11 May 2021: Review Articles
A Review of the Global Impact of the COVID-19 Pandemic on Public Mental Health, with a Comparison Between the USA, Australia, and Poland with Taiwan and Thailand
Katarzyna M. Bliźniewska-KowalskaDOI: 10.12659/MSM.932220
Med Sci Monit 2021; 27:e932220
Abstract
ABSTRACT: Coronavirus may have a negative impact not only on physical, but also on mental wellbeing. Despite the different approaches of countries to stop the spread of the virus and different infection rates, the dynamically developing pandemic has already affected the entire world. The consequences of the coronavirus for our mental health can be divided into those related to strategies for the prevention of infection, like isolation, quarantine, limitation of social contacts, and remote work, and those related to the direct impact of infection on our nervous system. This review aims to highlight the global effects of the Coronavirus Disease 2019 (COVID-19) pandemic on public mental health following social restrictions, to identify how infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may have direct neurophysiological effects and to compare the impact on public mental health between the USA, Australia, and Poland with Taiwan and Thailand.
Keywords: COVID-19, Mental Health, Neurosciences, Australia, COVID-19, Pandemics, Poland, Public Health, Taiwan, Thailand, United States
Background
At the beginning of 2020, when the Coronavirus Disease 2019 (COVID-19) pandemic broke out worldwide, we were unaware of the potentially serious implications of the coronavirus on global mental health. We now know that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection may have negative effects not only on physical, but also mental wellbeing [1]. These psychiatric and psychological consequences can be divided into those related to the prevention of infection, like isolation, quarantine, limitation of social contacts, or remote work, and those related to the direct impact of infection on the nervous system [1]. Therefore, this review aims to highlight the global effects of the COVID-19 pandemic on public mental health following social restrictions, to identify how infection with SARS-CoV-2 may have direct neurophysiological effects, and to compare the impact on public mental health in the USA, Australia, and Poland with Taiwan and Thailand.
Psychological and Psychiatric Consequences of Prevention Strategies
To stop the spread of the virus, authorities worldwide undertook drastic preventive measures that have affected the everyday life of their citizens to a greater or lesser degree. These measures have included the recommendation of social distancing, variably introduced and enforced curfews, quarantines, and isolation of affected individuals. Some nonessential stores and facilities, like gyms or theaters, were closed. Such actions affected many sectors of the overall economy. Many people had to switch to remote work. School and universities began on-line classes. Many aspects of our lives moved to the internet. Although lockdown has been partially successful in slowing the spread of the COVID-19 pandemic, its mental health consequences are significant. Economic stress, social isolation, and decreased access to medical help and community support are significant risk factors leading to a variety of psychological problems.
Several studies have been carried out to investigate the impact of quarantine and isolation on mental health. Brooks et al indicated that quarantine can be accompanied by stress associated with the duration of the quarantine, fear of infection, frustration, boredom, inadequate supplies, and inadequate information. These stressors can induce acute stress disorders, anxiety, irritability, poor concentration, indecisiveness, deteriorating work performance, post-traumatic stress symptoms, psychological distress, depressive symptoms, and insomnia [2]. The prevalence of depression during COVID-19 quarantine ranged from 16.5% [3] up to 37% [4] and the prevalence of anxiety from 12.9% [5] up to 35% [6,7]. Lei et al showed that there is a significant difference in depression and anxiety prevalence between individuals affected and those unaffected by quarantine (22.4% and 12.9% compared to 11.9% and 6.7%, respectively) [5]. Other studies have shown that subjects who were in COVID-19 quarantine were more likely to experience adverse mental health effects in comparison to those who were not quarantined [8,9]. However, the affected groups are heterogenous.
Wang et al revealed that frontline workers and individuals with previously-existing mental or physical issues, those infected or at risk of infection, and people with financial problems were more vulnerable to psychological stress in quarantine. Accepting the quarantine, taking part in usual work, and understanding information concerning the outbreak are the factors which act protectively and result in fewer mental problems [10]. Gualano et al also emphasize the role of predisposing and protective factors. Younger people had a greater likelihood of experiencing mood or anxiety disorders during quarantine [7]. A stable work situation and being in a relationship also reduced overall risk [7]. Women may be more likely to report mood or sleeping problems [11–14], although data are inconsistent [3,4,6].
The media have played a major role in the development of mental health-related problems during the pandemic. Media often use alarming messages that can increase the level of anxiety in the population. This in turn contributes to potential stigmatization of individuals and groups affected by the infection [15–18]. Youth who spend a lot of time on-line, have a strong need for social contacts with their peers, are more sensitive to stigma, and are in a less stable financial situations are particularly vulnerable to developing psychological stress reactions associated with the pandemic [19,20]. As previously mentioned, people with pre-existing mental disorders are more prone to developing COVID-19-related psychiatric problems. However, the question arises of whether psychiatric patients are more susceptible to SARS-CoV-2 infection?
The Evidence That Poor Mental Health Increases Susceptibility to Infection with SARS-CoV-2
Jeon et al concluded that psychiatric patients in general are not more likely to develop COVID-19. However, individuals with a schizophrenic disorder may be at higher risk of developing COVID-19 disease. Moreover, higher mortality due to infection with SARS-CoV-2 virus has been suggested in psychiatric patients [21]. There are several physical health risk factors for COVID-19, and many of these, such as diabetes, are more prevalent in people with psychiatric conditions than in the general population [22]. Taquet et al have shown that patients who were diagnosed with a psychiatric disorder in the year before the COVID-19 outbreak had a 65% increased risk of SARS-CoV-2 infection [22]. Indeed, mental illness per se may be a risk factor for COVID-19, regardless of the category of psychiatric diagnosis [22]. This finding is in line with the study conducted by Wang et al, who assessed the impact of a psychiatric diagnosis within the previous year on the risk of SARS-CoV-2 infection and related mortality [14]. Patients who have been recently diagnosed with mental health problems were at significant risk of COVID-19 and that was especially true for those with depression and schizophrenia. Women and African Americans had higher odds of SARS-CoV-2 infection. Elderly people had a lower risk than those aged 18–65 years, with the exception of people with schizophrenia. The mortality rate in this group is also higher than in those unaffected by mental illness (8.5% versus 4.7%) [14]. However, there are inconsistent data on the link between mental illness and the risk of developing COVID-19 [23]. Nevertheless, clinicians need to be aware that certain factors related to mental disorders may contribute to greater risk of developing COVID-19 disease. Patients with serious mental illness may have health literacy barriers and might encounter problems understanding and complying with health security measures, coping with stress related to social isolation, and recognizing and communicating symptoms or their health needs [24].
The Neuropsychiatric Effects of SARS-CoV-2 Infection
There are several neurobiological consequences of SARS-CoV-2 infection. In the first 2 weeks to 3 months after the diagnosis of COVID-19 was made, psychiatric disorders were diagnosed for the first time in 5–8% of patients [22]. This suggests that the risk of developing a psychiatric disorder for COVID-19 survivors almost doubles (5–8% versus 2.5–3.4% in comparison cohorts) [22]. However, these numbers may be an underestimate. Access to healthcare services during a pandemic is more difficult. Many people may be undiagnosed or simply not seek help from a specialist [22].
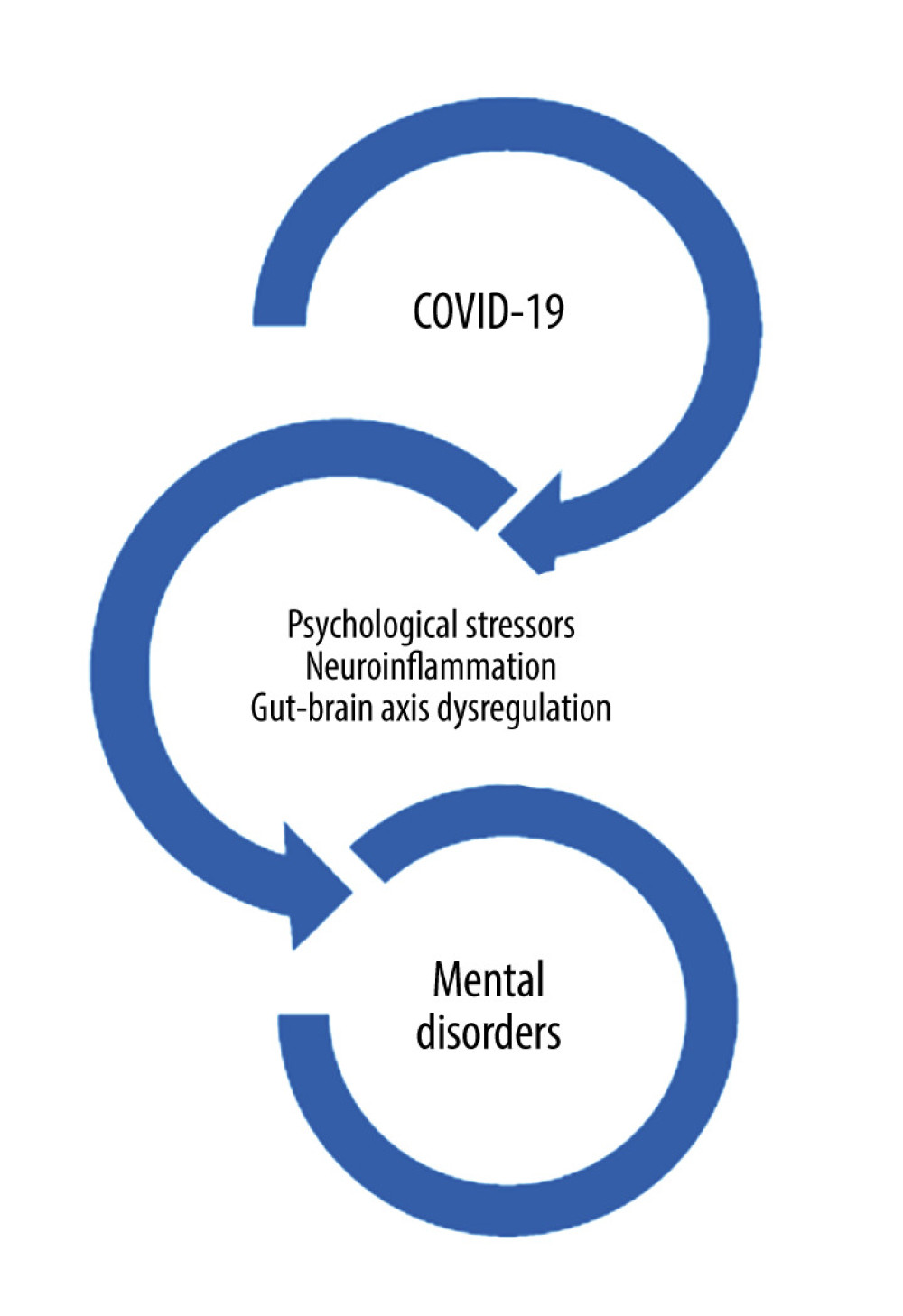
Coronavirus infection is primarily associated with anxiety, depression, trauma-related disorders, and insomnia. The mechanism linking the emergence of these disorders to COVID-19 is still unknown. Undoubtedly, psychological factors and stress play an important role. Attention should also be paid to the influence of infection on the central nervous system (CNS), particularly immune mechanisms (Figure 1).
Mao et al reported that 40 out of 88 hospitalized patients in Wuhan, China with severe coronavirus diseases (COVID-19) had neurological manifestations [25]. SARS-CoV-2 can penetrate the CNS from peripheral nerves via synapses, through the olfactory bulb, and through the systemic circulation, directly causing neuroinflammation [1,26–28]. Coronavirus can also affect the CNS indirectly by an increased cytokine release [1]. In a group of patients with CNS-related symptoms, lymphocyte counts were significantly lower [25,29,30]. The presence of the “cytokine storm” in severe cases of COVID-19 emphasizes the significance of immunological mechanisms in the pathophysiology of this disease [31,32]. Mindful of the inflammation theory of depression [33,34], elevated pro-inflammatory cytokines might be a nexus in the shared pathology of these diseases. Fetal and early childhood exposure to viral infections enhances the risk of developing psychiatric disorders [35,36]. Severance et al observed elevated levels of antibodies against 4 coronavirus strains in patients who had experienced psychotic episodes, suggesting a possible correlation between SARS-CoV-2 infections and psychosis [37]. Other potential mechanisms of neuropsychiatric manifestations in COVID-19 may involve gut microbial translocation and thus dysregulation of the gut-brain barrier [38,39].
The Global Effects of the COVID-19 Pandemic on Public Mental Health From SARS-CoV-2 Infection and Social Isolation
COVID-19 is a heterogeneous disease. Currently, more contagious mutations of the coronavirus are emerging, including B.1.1.7, first identified in the United Kingdom, and B.1.351, which was identified in South Africa. The course of infection can vary from asymptomatic to very severe. We do not yet know all the risk factors for the severity of the disease. There are countries that have dealt very well with the pandemic and countries where the epidemiological situation is poorly controlled. The restrictions in different parts of the globe are different. Access to vaccines also varies from country to country. Psychiatry experts from different parts of the globe commented on the situation in their countries.
The Effects of the COVID-19 Pandemic on Public Mental Health in the USA
The pandemic has profoundly affected nearly all aspects of life in the United States. The country continues to record the highest rates of new cases and deaths than any other country. This is in large part due the politicization of the pandemic with the intentional spread of misinformation by the government leadership and interference with the expeditious and universal implementation of mitigating strategies that had been deployed successfully in many other countries. These measures have proven effective and have effectively arrested the pandemic in many countries. Presently, the rapid pace of vaccination is beginning to show a beneficial effect on containing transmission and reducing the number of new cases and daily deaths. Mandatory wearing of face shields (masks) in public places, social distancing, restrictions in occupancy at restaurants and shopping areas, quarantining, and contact tracing, which are all measures that have been proven effective in most countries that have deployed them universally and consistently, are practiced in most but not all locations in the United States. With 3 proven safe and efficacious vaccines presently available in the United States and strong and mature leadership in the US government, the pace of vaccination expectedly will lead to herd immunity by late summer 2021. In the meantime, adherence to established mitigation strategies must be enforced across the country and the world. Unfortunately, mass media interfere negatively by spreading misinformation about vaccine safety, and a portion of the population is refusing to be vaccinated. The same misinformation driven by political motives undermines the implementation of mitigation strategies still essential to be practiced until at least 85% of the population has been vaccinated.
With respect to the psychiatric consequences of COVD-19, the high rates of anxiety (6.33% to 50.9%), depression (14.6% to 48.3%), post-traumatic stress disorder (7% to 53.8%), psychological distress (34.43% to 38%), and stress (8.1% to 81.9%) that have been reported in other countries also hold true for the United States. Risk factors include female gender, younger age (≤40 years), presence of chronic/psychiatric illnesses, unemployment, student status, and frequent exposure to social media/news concerning COVID-19 [40].
The pandemic has profoundly affected psychiatric patients and practice. Just as in the general population, psychiatric patients have to cope with isolation, loneliness, sudden bereavement following the loss of loved ones, loss of livelihood, and fear of possibly losing their own lives. Delivery of psychiatric care has been negatively impacted by the pandemic at a critical time when effective and prompt interventions are urgently needed. Services based on groups, such as partial hospital and intensive outpatient programs involving group therapies, were suspended indefinitely. In-office visits were replaced by telehealth sessions. Telehealth has been most useful under the pandemic and will likely remain a treatment option for years to come. Unquestionably, psychiatric telehealth, where appropriate, will likely make such care more easily accessible to remote parts of any country that lack provider and facility availability. It is entirely our responsibility as health care providers to inform health care policy makers and health care systems about the challenges and continued needs of financial and administrative support for psychiatric clinicians and mental health systems across any country.
Effects of the COVID-19 Pandemic on Public Mental Health in Australia
The number of COVID-19 cases reported in Australia remains low. The average daily number of cases in the last 2 weeks of February 2021 was 5, the same as in the previous 2 weeks. The total number of cases brought up to 28 937 and 909 deaths. Australia has started a COVID-19 vaccination program. By February 28th, 33 702 Australians had received 1 dose of the Pfizer vaccine. A total of 14% of all COVID-19 cases have been admitted to hospital since the start of the pandemic. According to sentinel surveillance data, 19% of hospitalized patients were admitted to the intensive care unit. The death rate in Australia remains steady at 3.1%, and no COVID-19-related deaths occurred in February 2021 [41].
There was great concern about the mental health consequences of the epidemic and risks of suicide. Demand for services has gone up, but whether that is related to consequences of COVID-19 or increases in public interest in mental health more generally is unclear. Unlike many other countries, mental health is a major political and election issue. The recent Victorian Royal Commission into mental health services has advocated for dramatically increased resourcing for the sector, but this is independent of COVID-19.
Effects of the COVID-19 Pandemic on Public Mental Health in Poland
In Poland, over 1.8 million cases of SARS-CoV2 infection have been recorded since the beginning of the pandemic. There have already been over 45 000 deaths due to COVID-19 [42]. A Polish study conducted at the beginning of the pandemic, in spring 2020, showed that 68% of respondents were worried about the COVID-19 pandemic. The main areas of concern were: death of loved ones (75%), severe illness in loved ones (72%), failure of healthcare (64%), and individual and social consequences of the pandemic (64% and 63%, respectively) [43]. Polish research indicates that 30% of respondents changed their alcohol drinking habits during the pandemic: 14% consume more alcohol and 16% consume less [44]. A study conducted on health care workers in Poland during the pandemic showed that as many as 70.7% present symptoms of depression, 64.4% suffer from anxiety, and 58% suffer from insomnia. The results of this study also indicate that people fighting on the front lines with a pandemic statistically significantly more often suffer from depression, anxiety, or insomnia [45]. Already in the spring of 2020, during the first lockdown, it was possible to grant reimbursed telephone psychiatric visits, which helped to assure continued therapy. The worst situation is with inpatient addiction treatment, which has not been functioning for a year. The pandemic is accelerating the trend of increasing amounts of prescribed antidepressants. In 2020, the number of prescriptions issued by doctors in general decreased by 8% YoY (year-over-year) whereas, by contrast, the number of prescriptions issued by psychiatrists increased by 3%. From March to April 2020, Poles spent 24% more on sedatives and sleeping pills than they did a year earlier and spent 33% more on antidepressants [46].
Effects of the COVID-19 Pandemic on Public Mental Health in Taiwan
On March 10, 2021, a total of 977 confirmed Taiwanese cases had been recorded and 10 people had died, making Taiwan one of the most unaffected countries worldwide [47]. Taiwan has achieved relative success against COVID-19 due to prudent action, rapid response, and early-stage containment policy, together with transparency and public trust with solidarity [48]. At the very beginning of the COVID-19 pandemic, Taiwan had commenced onboard quarantine measures for all direct flights arriving from Wuhan, China, and activated airport quarantine measures. From their experience with the SARS pandemic in 2003, people in Taiwan had already internalized the importance of wearing face masks and hand-washing to prevent infection; moreover, to ensure adequate domestic supplies of surgical masks and personal protective equipment, the Taiwan government encouraged the rapid ramping up of mask production and banned mask exportation [49]. Based on data of the National Health Insurance smart-card system, Taiwan had used big data analytics with smart contact tracing, automated alert messaging for self-restriction, and follow-up of the outcome [50,51]. Since January 22, 2020, the Taiwan Health and Welfare Minister has hosted a daily televised press conference to provide the public with a case-by-case update on the current status of the outbreak, seeking to maximize transparency and awareness and thereby minimize public anxiety.
Due to social isolation, hospitalized patients had limited time to meet with their family or to temporarily leave the hospital in Taiwan. We did not need to implement city lockdowns or mass screening, but we applied information technology and artificial intelligence to carry out precision disaster prevention and mitigation. Due to border control, quarantine, social distancing, and financial problems, the outpatients experienced more anxiety, insomnia, and stress.
Since November 2020, several COVID-19 vaccines, such as the Pfizer, Moderna, and Astra-Zeneca vaccines, have been approved and made available for clinical application [52–55]. The Taiwan government made recommendations for who should be offered COVID-19 vaccines first, including medical staff, essential government employees, soldiers, the elderly, and those at high risk of severe respiratory complications. At the same time, the Taiwan government continues to promote internalized healthy behaviors, such as wearing face masks, social distancing, and hand-washing.
Effects of the COVID-19 Pandemic on Public Mental Health in Thailand
On March 11th, 2021, Thailand registered a total of 26 598 COVID-19 cases, of whom 25 946 have recovered. Eighty-five deaths due to COVIC-19 have been registered. After a few months without any new infections, there was a second outbreak starting in January 2021 imported via migrant workers from Myanmar. Thailand was the first country to report a case of COVID-19 outside China; however, due to the strict comprehensive measures taken, such as tracing and quarantining contacts, there were no reported local transmissions during May and September 2020. Nevertheless, on March 11th 2021, 58 new cases were detected, consisting of 53 local infections (especially in Myanmar nationals) and 5 imported cases.
Researchers in Thailand now analyze new data on COVID-19, namely (a) epidemiologic studies that examined the association between COVID-19-associated stressors and new mental health problems; and (b) biomarkers of depression, anxiety, and fatigue symptoms during acute COVID-19 infection.
The first series of Thai epidemiologic studies show that isolation due to lockdown is accompanied by increased rates of stress and distress, depression, anxiety, panic, post-traumatic stress disorder, and suicidal ideation, especially in those who already suffered from depression. Likewise, the anxiety about being infected, or that a close family member is affected, is associated with increased rates of the same symptoms.
Scientists in Thailand and Iraq also established new biomarkers of acute COVID-19 infection, which have an accuracy of 100%, including interleukin-6, lowered calcium, C3, C4, angiotensin-converting enzyme 2, RAGEs, albumin, and thromboxane. Patients in the acute phase of COVID-19 show increased depression, anxiety, fatigue, and physio-somatic symptoms. The latter are strongly associated with the biomarkers of acute COVID-19 infection, including interleukin-6, CRP, albumin, and RAGEs.
As described above, there is a significant increase in mental health symptoms; however, the number of patients attending the clinic in Thailand did not increase, and overall severity of chronic patients with affective disorders or schizophrenia did not appreciably increase. On the other hand, there is probably a significant increase in suicides, but the hypothesis is that this may be the consequence of economic problems due to the lockdowns.
At the end of February 2021, Thailand had 200 000 Sinovac doses of COVID-19 vaccine. According to Prof. Michael Maes, Thailand is now the latest to receive vaccine deliveries, whereas all neighboring countries are already vaccinating. The current government was unable to secure more doses of vaccines at this point. They bought 20 million Astra-Zeneca doses and will produce Astra-Zeneca vaccine to have the whole population vaccinated by the end of the year. It appears that the Thai population is eager to get vaccinated as soon as possible.
Patients with COVID-19 infection should routinely be screened for major psychiatric symptoms; they should be prospectively followed because many of these patients will develop a post-COVID syndrome and chronic fatigue, and depression, which are cognitive impairments that are major features of this syndrome. The neuro-immune approach is warranted because: (a) the psychiatric symptoms during infection are associated with inflammation, immune disorders, and oxidative stress, and (b) increased autoimmunity is one of the features of COVID-19 infection [56], which is probably associated with the post-COVID-19 syndrome.
Conclusions
We have reviewed the literature and have confirmed that SARS-CoV-2-infected patients are at high risk of developing neuropsychiatric complications, suggesting that the “psychoneuroimmunity” (interaction between psychological processes, nervous system and immunity) model may be helpful in understanding the effect of the virus [57,58]. During the COVID-19 pandemic, the most common psychiatric symptoms both in patients and health providers [59] were anxiety and mood disorders as well as suicidal thoughts [60,61]. Lifestyle interventions are essential for using “psychoneuroimmunity” models against COVID-19 [62]. For example, poor sleep quality was also associated with a slow recovery and an increased need for intensive care [63]; while certain nutritional approaches, such as omega-3 fatty acids, could be beneficial in increasing psychological and physiological resilience against COVID-19 [64]. Among patients with mental disorders, the COVID-19 pandemic appeared to disrupt daily routines, sever social ties, and increase financial worries and fears about the future [65]. COVID-19 infection can cause a wide variety of nervous system symptoms, including acute cerebrovascular disease, headache, sleep disturbances, impaired consciousness, dizziness, and loss of taste and smell [1,59,66]. COVID-19 patients frequently presented with subjective neurological symptoms in their early stage of the disease; cutaneous hyperesthesia was also reported [67,68].
In addition to the newly administered vaccinations and the currently available supportive treatments for COVID-19, a healthy lifestyle, including physical activity [69] and psychological interventions, have the potential to enhance the immunity against the virus and improve mental health during the COVID-19 pandemic [57,58]. Furthermore, Kinoshita et al used the snowball sampling method within a global network of telepsychiatry experts and found that the COVID-19 pandemic accelerated the promotion of telemedicine [70]. There are several factors that may contribute to this trend. For example, psychiatric medicine is based on face-to-face interviews, and telemedicine can facilitate interviews without the need for exposure and infection risk; additionally, telemedicine can reduce the pressure for patients to go to the hospital, as well as improving access to psychotherapy.
This review has highlighted the global effects of the COVID-19 pandemic on public mental health following social restrictions and has also discussed how infection with SARS-CoV-2 may have direct neurophysiological effects. Comparison of the impact on public mental health between the USA, Australia, and Poland with Taiwan and Thailand has also shown that social restrictions during the COVID-19 pandemic have affected public mental health and that poor mental health increases the susceptibility to SARS-CoV-2 infection in all countries. However, lessons may be learned from the different public mental health measures and approaches in different countries as pandemic SARS-CoV-2 infection becomes endemic throughout the world.
References
1. Szcześniak D, Gładka A, Misiak B, The SARS-CoV-2 and mental health: From biological mechanisms to social consequences: Prog Neuropsychopharmacol Biol Psychiatry, 2021; 104; 110046
2. Brooks SK, Webster RK, Smith LE, The psychological impact of quarantine and how to reduce it: rapid review of the evidence: Lancet, 2020; 395(10227); 912-20
3. Wang C, Pan R, Wan X, Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China: Int J Environ Res Public Health, 2020; 17; 1729
4. Ahmed MZ, Ahmed O, Aibao Z, Epidemic of COVID-19 in China and associated Psychological Problems: Asian J Psychiatry, 2020; 51; 102092
5. Lei L, Huang X, Zhang S, Yang J, Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China: Med Sci Monit, 2020; 26; e924609
6. Huang Y, Zhao N, Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey: Psychiatry Res, 2020; 288; 112954
7. Gualano MR, Lo Moro G, Voglino G, Effects of COVID-19 lockdown on mental health and sleep disturbances in Italy: Int J Environ Res Public Health, 2020; 17(13); 4779
8. Daly Z, Slemon A, Richardson CG, Associations between periods of COVID-19 quarantine and mental health in Canada: Psychiatry Res, 2021; 295; 113631
9. Hossain MM, Sultana A, Purohit N, Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence: Epidemiol Health, 2020; 42; e2020038
10. Wang Y, Shi L, Que J, The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic: Mol Psychiatry, 2021; 22; 1-10
11. Mazza C, Ricci E, Biondi S, A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors: Int J Environ Res Public Health, 2020; 17; 3165
12. González-Sanguino C, Ausín B, Castellanos MÁ, Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain: Brain Behav Immun, 2020; 87; 172-76
13. Zhang C, Yang L, Liu S, Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak: Front Psychiatry, 2020; 11; 306
14. Wang Q, Xu R, Volkow ND, Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States: World Psychiatry, 2021; 20(1); 124-30
15. Ahmad AR, Murad HR, The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: Online questionnaire study: J Med Internet Res, 2020; 22; e19556
16. Gao J, Zheng P, Jia Y, Mental health problems and social media exposure during COVID-19 outbreak: PLoS One, 2020; 15; e0231924
17. Sell TK, Boddie C, McGinty EE, Media messages and perception of risk for Ebola virus infection, United States: Emerg Infect Dis, 2017; 23; 108-11
18. Garfin DR, Silver RC, Holman EA, The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure: Health Psychol, 2020; 39; 355-57
19. Singh S, Roy D, Sinha K, Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations: Psychiatry Res, 2020; 293; 113429
20. Elmer T, Mepham K, Stadtfeld C, Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland: PLoS One, 2020; 15(7); e0236337
21. Jeon H, Kwon J, Park S, Shin J, Association of mental disorders with SARS-CoV-2 infection and severe health outcomes: Nationwide cohort study: Br J Psychiatry, 2021 [Online ahead of print]
22. Taquet M, Luciano S, Geddes JR, Harrison PJ, Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA: Lancet Psychiatry, 2021; 8(2); 130-40 [Erratum in: Lancet Psychiatry. 2021;8(1): e1]
23. Lee SW, Yang JM, Moon SY, Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: A nationwide cohort study: Lancet Psychiatry, 2020; 7(12); 1025-31
24. Shinn AK, Viron M, Perspectives on the COVID-19 pandemic and individuals with serious mental illness: J Clin Psychiatry, 2020; 81; 20com13412
25. Mao L, Wang M, Chen S, Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study: JAMA Neurol, 2020; 77(6); 683-90
26. Li YC, Bai WZ, Hirano N, Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication: J Comp Neurol, 2013; 521; 203-12
27. Netland J, Meyerholz DK, Moore S, Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2: J Virol, 2008; 82(15); 7264-75
28. Baig AM, Khaleeq A, Ali U, Syeda H, Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms: ACS Chem Neurosci, 2020; 11; 995-98
29. Li Y, Li H, Fan R, Coronavirus infections in the Central nervous system and respiratory tract show distinct features in hospitalized children: Intervirology, 2017; 59; 163-69
30. Lagunas-Rangel FA, Neutrophil-to-Lymphocyte ratio and Lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis: J Med Virol, 2020; 2019; 2019-20
31. Huang KJ, Su IJ, Theron M, An interferon-γ-related cytokine storm in SARS patients: J Med Virol, 2005; 75; 185-94
32. Yang Y, Shen C, Li J, Exuberant elevation of IP-10, MCP-3 and IL-1ra during SARS-CoV-2 infection is associated with disease severity and fatal outcome: medRxiv, 2020; 2020; 20029975
33. Gałecka M, Bliźniewska-Kowalska K, Maes M, Update on the neurodevelopmental theory of depression: Is there any ‘unconscious code’?: Pharmacol Rep, 2021; 73(2); 346-56
34. Maes M, Major depression and activation of the inflammatory response system: Adv Exp Med Biol, 1999; 461; 25-46
35. Brown AS, Derkits EJ, Prenatal infection and schizophrenia: A review of epidemiologic and translational studies: Am J Psychiatry, 2010; 167; 261-80
36. Khandaker GM, Zimbron J, Dalman C, Childhood infection and adult schizophrenia: A meta-analysis of population-based studies: Schizophr Res, 2012; 139; 161-68
37. Severance EG, Dickerson FB, Viscidi RP, Coronavirus immunoreactivity in individuals with a recent onset of psychotic symptoms: Schizophr Bull, 2011; 37; 101-7
38. Troyer EA, Kohn JN, Hong S, Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms: Brain Behav Immun, 2020; 87; 34-39
39. Li N, Ma WT, Pang M, The commensal microbiota and viral infection: A comprehensive review: Front Immunol, 2019; 10; 1-16
40. Xiong J, Lipsitz O, Nasri F, Impact of COVID-19 pandemic on mental health in the general population: A systematic review: J Affect Disord, 2020; 277; 55-64
41. , COVID-19 Australia: Epidemiology report 6. Reporting period ending 28 February 2021: Commun Dis Intell, 2018 2021 45https://doi.org/10.33321/cdi.2021.45.14
42. : Data from the Polish Ministry of Health https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2
43. Gawrych M, Cichoń E, Kiejna A, COVID-19 pandemic fear, life satisfaction and mental health at the initial stage of the pandemic in the largest cities in Poland: Psychol Health Med, 2021; 26(1); 107-13
44. Chodkiewicz J, Talarowska M, Miniszewska J, Alcohol consumption reported during the COVID-19 pandemic: The initial stage: Int J Environ Res Public Health, 2020; 17(13); 4677
45. Wańkowicz P, Szylińska A, Rotter I, Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients: Int J Environ Res Public Health, 2020; 17(16); 5849
46. (data of the analytical company IQVIA. and )https://www.rynekaptek.pl/farmakologia/stosowanie-antydepresantow-w-polsce-rosnie-od-lat-pandemia-przyspiesza-ten-trend,42306.html
47. Wu WK, Liou JM, Hsu CC, Pandemic preparedness in Taiwan: Nat Biotechnol, 2020; 38(8); 932-33
48. Awandare G, André E, Corrales-Aguilar E, Science advisers around the world on 2020: Nature, 2020; 588(7839); 586-88
49. Feng S, Shen C, Xia N, Rational use of face masks in the COVID-19 pandemic: Lancet Respir Med, 2020; 8(5); 434-36
50. Chen CM, Jyan HW, Chien SC, Containing COVID-19 among 627,386 persons in contact with the diamond princess cruise ship passengers who disembarked in Taiwan: Big data analytics: J Med Internet Res, 2020; 22(5); e19540
51. Wang CJ, Ng CY, Brook RH, Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing: JAMA, 2020; 323(14); 1341-42
52. Polack FP, Thomas SJ, Kitchin N, Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine: N Engl J Med, 2020; 383(27); 2603-15
53. Ledford H, Moderna COVID vaccine becomes second to get US authorization: Nature, 2020 [Online ahead of print]
54. Baden LR, El Sahly HM, Essink B, Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine: N Engl J Med, 2021; 384(5); 403-16
55. Knoll MD, Wonodi C, Oxford-AstraZeneca COVID-19 vaccine efficacy: Lancet, 2021; 397(10269); 72-74
56. Vojdani A, Vojdani E, Kharrazian D, Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: Implications for autoimmune diseases: Front Immunol, 2021; 11; 617089
57. Wang SC, Su KP, Pariante CM, The three frontlines against COVID-19: Brain, behavior, and immunity: Brain Behav Immun, 2021; 93; 409-14
58. Kim SW, Su KP, Using psychoneuroimmunity against COVID-19: Brain Behav Immun, 2020; 87; 4-5
59. Nalleballe K, Reddy Onteddu S, Sharma R, Spectrum of neuropsychiatric manifestations in COVID-19: Brain Behav Immun, 2020; 88; 71-74
60. Liu T, Zheng Z, Sha X, Psychological impact in non-infectious disease specialists who had direct contact with patients with COVID-19: B J Psych Open, 2020; 7(1); e8
61. Fang X, Zhang J, Teng C, Depressive symptoms in the front-line non-medical workers during the COVID-19 outbreak in Wuhan: J Affect Disord, 2020; 276; 441-45
62. Lee SA, How much “Thinking” about COVID-19 is clinically dysfunctional?: Brain Behav Immun, 2020; 87; 97-98
63. Zhang J, Lu H, Zeng H, The differential psychological distress of populations affected by the COVID-19 pandemic: Brain Behav Immun, 2020; 87; 49-50
64. Chang JP, Pariante CM, Su KP, Omega-3 fatty acids in the psychological and physiological resilience against COVID-19: Prostaglandins Leukot Essent Fatty Acids, 2020; 161; 102177
65. Frank A, Fatke B, Frank W, Depression, dependence and prices of the COVID-19-Crisis: Brain Behav Immun, 2020; 87; 99
66. Kajani R, Apramian A, Vega A, Neuroleptic malignant syndrome in a COVID-19 patient: Brain Behav Immun, 2020; 88; 28-29
67. Krajewski PK, Szepietowski JC, Maj J, Cutaneous hyperesthesia: A novel manifestation of COVID-19: Brain Behav Immun, 2020; 87; 188
68. Liguori C, Pierantozzi M, Spanetta M, Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection: Brain Behav Immun, 2020; 88; 11-16
69. da Silveira MP, da Silva Fagundes KK, Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature: Clin Exp Med, 2021; 21(1); 15-28
70. Kinoshita S, Cortright K, Crawford A, Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions’ approaches to an evolving healthcare landscape: Psychol Med, 2020; 27; 1-8
In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952