27 September 2021: Database Analysis
Postoperative Neutrophil-to-Lymphocyte Ratio Is Associated with Mortality in Adult Patients After Cardiopulmonary Bypass Surgery: A Cohort Study
Yanhong Zhu1BCE, Wenyong Peng2BDF, Shuai Zhen2BEF, Xiaofeng Jiang2AC*DOI: 10.12659/MSM.932954
Med Sci Monit 2021; 27:e932954
Abstract
BACKGROUND: Cardiopulmonary bypass (CPB) contributes to the development of systemic inflammatory response after cardiothoracic surgery. As a measure of inflammation and immune reaction, the neutrophil-to-lymphocyte ratio (NLR) has been linked to poor outcomes in a variety of diseases. However, it remains to be seen whether postoperative NLR is associated with CPB patient mortality. The purpose of this research was to explore the prognostic role of the postoperative NLR in adult patients undergoing cardiothoracic surgery with cardiopulmonary bypass.
MATERIAL AND METHODS: This is an analysis of data stored in the databases of the MIMIC–III, which contains data of critically ill patients for over 50,000. The exposure of interest was postoperative NLR. The primary outcomeaThis study incorporates data from the MIMIC III database, which includes more than 50 000 critically ill patients. The variable of interest was postoperative NLR. The primary outcome was 30-day mortality and the secondary outcomes were 90-day mortality, length of intensive care unit stay, and length of hospital stay. was 30-day mortality, the secondary outcome was 90-day mortality, length of hospital stay and length of ICU stay.
RESULTS: We enrolled 575 CPB patients. The ROC curve for the postoperative NLR to estimate mortality was 0.741 (95% confidence interval [CI]: 0.636-0.847, P<0.001), and the critical value was 7.48. There was a significant difference between different postoperative NLR levels in the Kaplan-Meier curve (P=0.045). Furthermore, elevated postoperative NLR was associated with increased hospital mortality (hazard ratio [HR]: 1.1, 95% CI: 1.0-1.1, P=0.021). However, there was no important relationship in these patients between the postoperative NLR levels and 90-day mortality (HR: 1.1, 95% CI: 1.0-1.5, P=0.465).
CONCLUSIONS: Our findings suggest that higher postoperative NLR is associated with greater hospital mortality in adult patients undergoing cardiopulmonary bypass surgery.
Keywords: Cardiopulmonary Bypass, Hospital Mortality, Outcome Assessment, Health Care, Cohort Studies, Critical Care, Databases, Factual, Female, Humans, Length of Stay, Leukocyte Count, Lymphocyte Count, Postoperative Complications
Background
Cardiovascular disease and its associated risk factors are the leading cause of death worldwide [1]. Cardiothoracic surgery with cardiopulmonary bypass (CPB) is the criterion standard treatment for various serious heart diseases, and many studies have shown that CPB contributes to the development of systemic inflammatory response after cardiothoracic surgery [2–4]. Numerous studies have confirmed increased inflammatory mediators among several patients following CPB [5–8]. However, in clinical practice, there are no inflammatory biomarkers for outcome evaluation. Therefore, it is critical to identify early postoperative clinical factors associated with an increased risk of poor outcomes.
The neutrophil-to-lymphocyte ratio (NLR) is an innovative inflammatory biomarker derived from combined neutrophil and lymphocyte counts [9]. Non-specific inflammation triggers neutrophils, whereas a decreased lymphocyte count suggests that the body is under stress or has poor immunity. The NLR integrates these 2 opposing immune pathways [10]. Additionally, as an innovative inflammatory marker, the NLR has been associated with the severity and prognosis of various cardiovascular problems [11,12]. Moreover, prior to heart surgery, an elevated NLR is associated with decreased survival [13–15]. Despite this, the association between increased postoperative NLR and worse prognosis in adult patients after cardiothoracic surgery with CPB remains unclear. Therefore, the purpose of this study was to explore the prognostic role of postoperative NLR in adult patients undergoing cardiothoracic surgery with CPB.
Material and Methods
DATA SOURCE:
The Multiparameter Intelligent Monitoring in Intensive Care III (MIMIC III, V.1.4) database maintained by the Laboratory for Computational Physiology at the Massachusetts Institute of Technology’s Laboratory has extensive data on over 50 000 patients admitted to the critical care unit at Beth Israel Deaconess Medical Center over the years 2001 to 2012 [16]. For the purpose of applying for access to the database, we took the National Institutes of Health’s web-based course “Protecting Human Research Participants”.
Institutional review boards at both the Massachusetts Institute of Technology (Cambridge, MA) and Beth Israel Deaconess Medical Center (Boston, MA) gave their approval for the creation of the database. The data for this study were collected by the author Jiang after completing an online training course offered by the National Institutes of Health (certification number: 9322422).
POPULATION SELECTION CRITERIA:
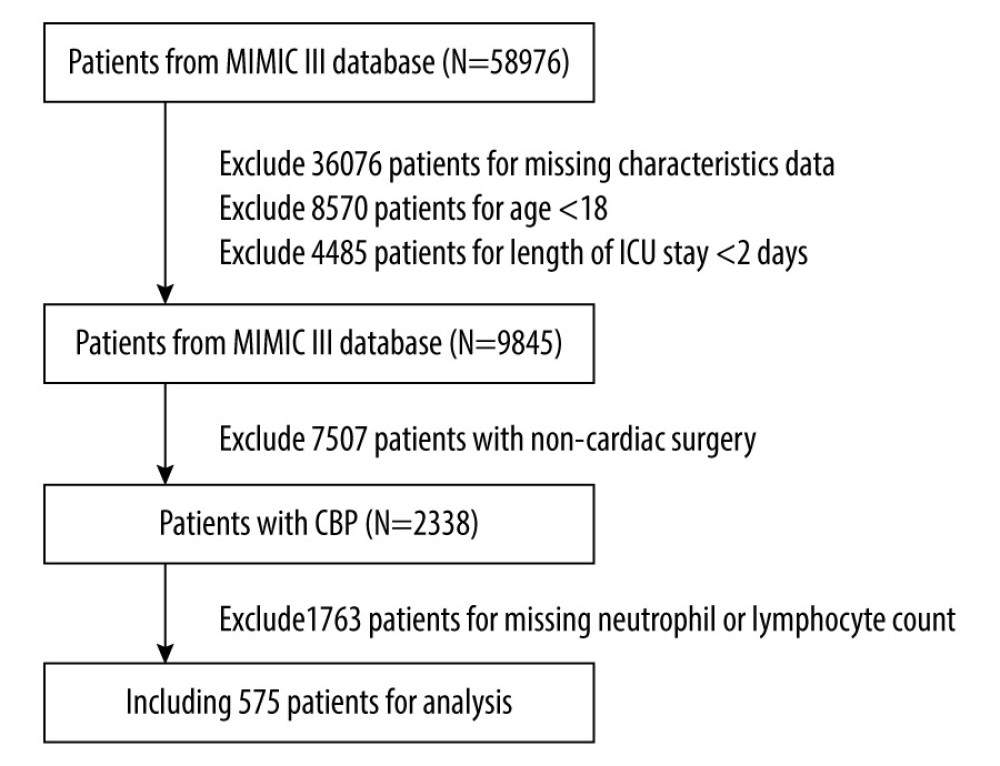
The MIMIC III database had information on 58 976 intensive care unit (ICU) patients in total. In these people, we included patients who underwent cardiac surgery utilizing cardiopulmonary bypass, were older than 18 years, and stayed in the ICU for at least 2 days. Patients were excluded if they had a missing neutrophil or lymphocyte count to calculate the NLR, had >1% missing data, or had been diagnosed with hematological disorders such as leukemia or lymphoma. Only data of the first ICU admission of the first hospitalization were used.
DATA EXTRACTION:
Data were extracted from the database using Structure query language (SQL). It included white blood cell (WBC) count, neutrophil, lymphocyte, and platelet count, hemoglobin, hematocrit, serum lactate, serum bicarbonate, anion gap, serum chloride, serum sodium, serum potassium, and serum glucose. NLR was calculated using complete neutrophil and lymphocyte counts. Since the patients had several measurements available, the arithmetic mean between the highest and the lowest value in the first 24 h postoperatively was used. The NLR in the first 24 h of the postoperative period was chosen because during this time as systemic inflammatory response is usually the most severe then.
Demographic parameters included age, sex, ethnicity (white, black, or other), height, weight, vital signs, comorbidities, and disease severity scores (Acute Physiology and Chronic Health Evaluation [APACHE] III) [17]. Measurements of vital signs, comorbidities, and disease severity scores were collected on the first day of ICU admission. The follow-up began on the day of admission to the ICU. The primary outcome was 30-day mortality and the secondary outcomes included 90-day mortality, length of intensive care unit stay (ICU LOS), and length of hospital stay (hospital LOS).
STATISTICAL ANALYSES:
The mean and standard deviation (SD) or median and interquartile ranges are presented in the tables for continuous variables. The
Results
Finally, 575 patients met the study’s criteria. Figure 1 depicts the data selection approach and data exclusion criteria. The demographic features of survivors and non-survivors are summarized in Table 1. NLR was significantly lower for survivors (9.1±9.2) than non-survivors (24.3±26.4) (
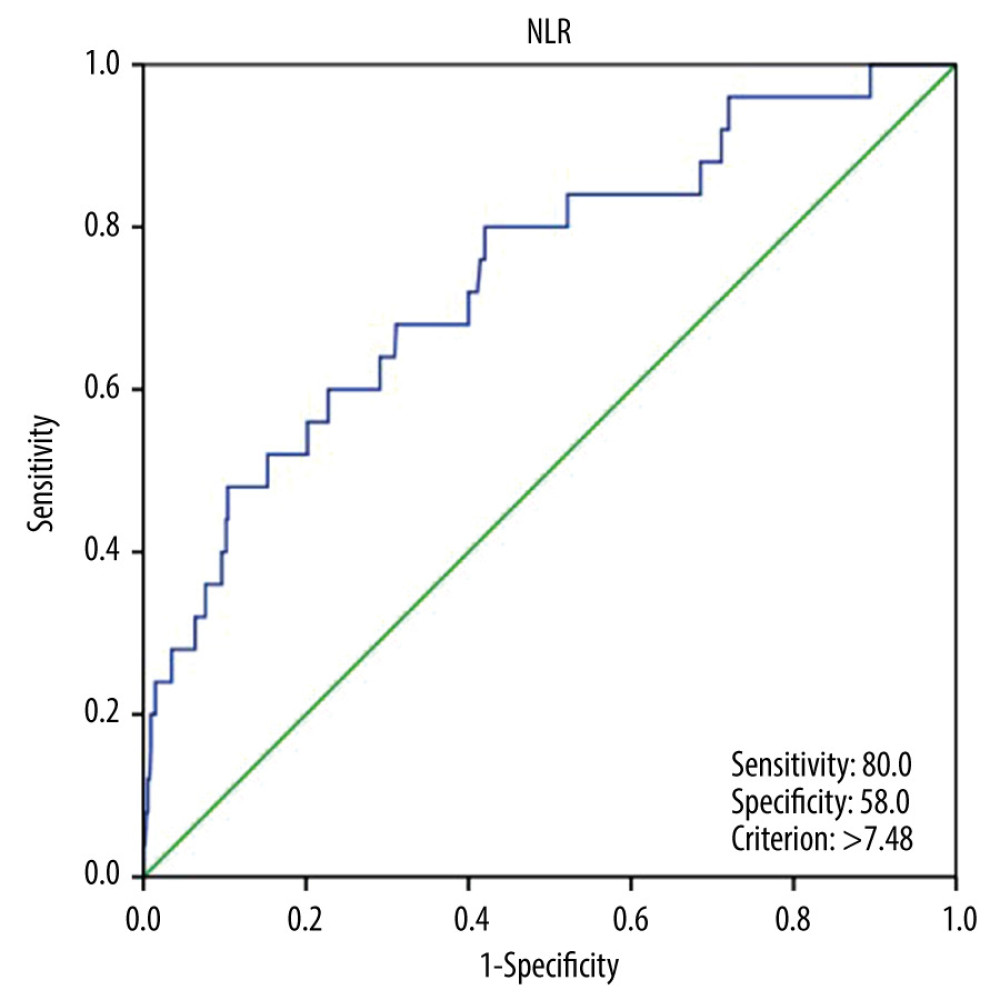
According to the ROC of the NLR (Figure 2), the critical value was 7.48, with an AUC of 0.741 (95% CI: 0.636–0.847,
According to the cut-off value, all patients were divided into 2 groups. Table 2 summarizes the postoperative outcomes for the 2 NLR categories. Observed hospital mortality and 90-day mortality were higher in the elevated NLR group compared with the non-elevated NLR group (
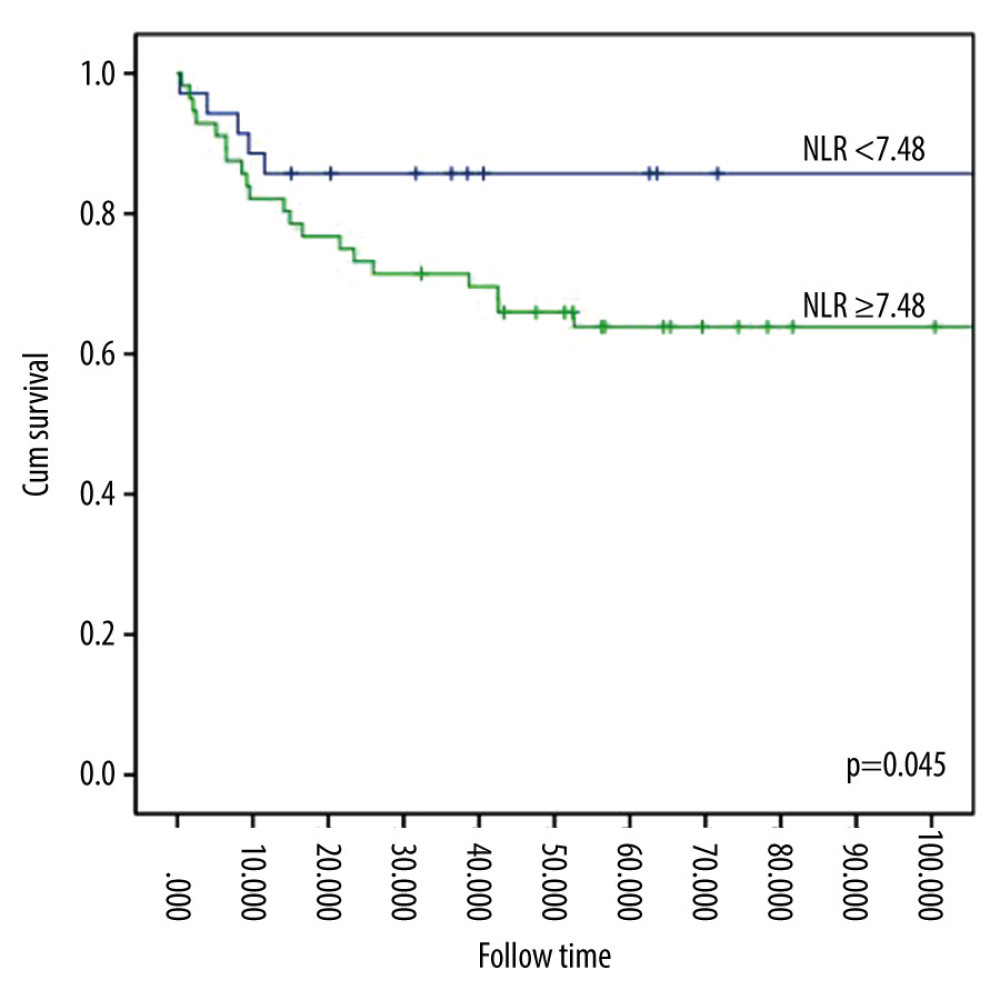
The Kaplan-Meier curve analysis revealed that all-cause mortality was significantly different between the different NLR levels (Figure 3). In contrast to patients with NLR lower than 7.48, those with NLR higher than 7.48 had higher mortality (
To determine potential predictors of hospital mortality and 90-day mortality in the study population, multivariate analysis was used (Table 3). The analysis showed that after adjusting for covariates, higher NLR was associated with higher hospital mortality (HR=1.1, 95% CI 1.0–1.1,
Discussion
Our study revealed that elevated postoperative NLR was an independent predictor of hospital mortality in adult patients undergoing cardiothoracic surgery with CPB. Hospital mortality increased with an increase in the NLR (HR=1.1,
Numerous studies have shown that CPB induces a systemic inflammatory response, likely due to blood components coming into contact with the artificial surface of the extracorporeal circuit. This contributes to the high mortality associated with heart surgery [3,18–20]. White blood cell count is a marker of systemic inflammation [21,22] and has also been associated with mortality after heart surgery [23,24]. However, the potential function of the absolute white blood cell count is limited by apparent confounding variables, and the association between increased white blood cell count and outcomes is non-linear [22,24]. Neutrophils are the most abundant type of white blood cell, and they respond rapidly to acute inflammation while being capable of killing invading pathogens [25]. Inflammation caused by CPB is primarily mediated by activated neutrophils, leading to systemic inflammation [26,27]. CPB initiates the complement cascade by activating neutrophils and inducing the secretion of polymorphonuclear elastase (PMN-E). The overactivation of PMN-E leads to cell damage and promotes the synthesis and release of IL-8 by IL-1 signaling, which indirectly enhances inflammatory reactions [28]. Furthermore, tissue and endothelial dysfunction are caused by neutrophil-driven enzymes such as elastase, myeloperoxidase, and reactive oxygen species, rendering patients vulnerable to organ damage. Activated neutrophils also directly stimulate endothelial cells, increasing perivascular edema and leukocyte migration to the extracellular matrix [29]. The development of cortisol and neuroendocrine stress was linked to lymphopenia after major operations [30], indicating that the body was stressed and the immune system was compromised. Therefore, the NLR reflects these 2 diametrically opposed immune pathways. One reflects unrestrained inflammation, while the other reflects a potential immune pathway. Furthermore, NLR is determined during a routine full blood count following surgery. Additional inspections are not necessary, and it is an inexpensive and readily available marker. Several studies have previously sought to link NLR with cardiac surgery mortality. The NLR levels were correlated with the outcomes of patients undergoing cardiac surgery with CPB [13–15,31,32]. Although most studies examined the relationship between preoperative or perioperative NLR and outcomes, few studies have examined the prognostic significance of postoperative NLR in patients undergoing cardiac surgery with CPB. In children with CPB, Xu et al [33] discovered a significant and positive association between early outcomes and postoperative NLR. Adult patients undergoing CPB had a weaker inflammatory response than pediatric patients [2]. According to our study, postoperative NLR was also associated with early prognosis in adult patients undergoing CPB.
Contrary to our study, the findings of a recent meta-analysis [31] and a study by Silberman et al (2018), in which 3027 adult patients who underwent CPB surgery were evaluated [15], the preoperative NLR and long-term mortality (>90 days) were strongly and positively associated. We propose a possible explanation for this finding. Elevated preoperative NLR reflects chronic background inflammation caused by chronic cardiovascular disease. Neutrophils are associated with the hypercoagulable state of coronary artery disease and the unstable atherosclerotic plaque state. These indicate patients with high cardiovascular risk [34]. The elevated postoperative NLR demonstrates the extent of myocardial injury and the degree of hypoperfusion caused by decreased cardiac output and ischemia-reperfusion syndrome [35]. However, these are temporary. Therefore, the association between postoperative NLR and long-term mortality (90-day mortality) was not significant. Additionally, a study by Wang et al [36] showed that the postoperative NLR with a cut-off value of 7.28 is an independent predictor of short survival. This finding is consistent with our results. However, they also found that postoperative NLR is positively associated with long-term mortality (90 days). This is in contrast to our results. We propose possible explanations for this finding. First, the NLR selected was different. Although NLR was determined in the first 24 h postoperatively, we used the arithmetic mean between the highest and lowest values. Wang et al [36] might have used the highest NLR value. Second, as this was a retrospective study, to process missing data, the analysis of the primary outcome was replicated after multiple imputations. This gave rise to an inevitable bias. Further investigations (including clinical trials) are necessary to explore the relationship between postoperative NLR and mortality in the future.
Our study has some limitations. First, we selected patients who stayed in the intensive care unit (ICU) for at least 2 days, as we aimed to select patients with severe illness and inflammatory reactions. However, the current findings cannot be applied to patients who were transferred from the ICU or those who died within the first 48 h. Second, as the datasets utilized in this analysis were from publicly available data, intraoperative variables such as CPB time, DHCA time, cross-clamping time, and the use of a balloon pump were not collected.
Conclusions
Elevated postoperative NLR is associated with increased hospital mortality, hospital length of stay (LOS), and ICU LOS in adult patients after CPB surgery. Owing to the simplicity of determining the NLR using complete blood count values, monitoring the postoperative NLR can predict the early outcome of adult patients undergoing CPB surgery.
References
1. GBD 2017 Causes of Death Collaborators, Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017 [editorial]: Lancet, 2018; 392(10159); 1736-88
2. Boehne M, Sasse M, Karch A, Systemic inflammatory response syndrome after pediatric congenital heart surgery: Incidence, risk factors, and clinical outcome: J Card Surg, 2017; 32(2); 116-25
3. Bronicki RA, Hall M, Cardiopulmonary bypass-induced inflammatory response: Pathophysiology and treatment: Pediatr Crit Care Med, 2016; 17(8 Suppl 1); S272-78
4. Kraft F, Schmidt C, Van Aken H, Zarbock A, Inflammatory response and extracorporeal circulation: Best Pract Res Clin Anaesthesiol, 2015; 29(2); 113-23
5. Allan CK, Newburger JW, Mcgrath E, The relationship between inflammatory activation and clinical outcome after infant cardiopulmonary bypass: Anesth Analg, 2010; 111(5); 1244-51
6. Ranucci M, Baryshnikova E, Inflammation and coagulation following minimally invasive extracorporeal circulation technologies: J Thorac Dis, 2019; 11(Suppl 10); S1480-88
7. Hall R, Identification of inflammatory mediators and their modulation by strategies for the management of the systemic inflammatory response during cardiac surgery: J Cardiothorac Vasc Anesth, 2013; 27(5); 983-1033
8. Souza AR, Lima RAG, Lopes LC, Biomarkers associated with postoperative cardiac surgery clinical outcomes in pediatric intensive care: Acta Paulista de Enfermagem, 2021; 34(eAPE00171); 1-13
9. Zahorec R, Ratio of neutrophil to lymphocyte counts – rapid and simple parameter of systemic inflammation and stress in critically ill: Bratisl Lek Listy, 2001; 102(1); 5-14
10. Azab B, Zaher M, Weiserbs KF, Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction: Am J Cardiol, 2010; 106(4); 470-76
11. Sari I, Sunbul M, Mammadov C, Relation of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio with coronary artery disease severity in patients undergoing coronary angiography: Kardiol Pol, 2015; 73(12); 1310-16
12. Yoon GS, Choi SH, Woo SI, Neutrophil-to-lymphocyte ratio at emergency room predicts mechanical complications of ST-segment elevation myocardial infarction: J Korean Med Sci, 2021; 36(19); e131
13. Weedle RC, Costa MD, Veerasingam D, Soo AWS, The use of neutrophil lymphocyte ratio to predict complications post cardiac surgery: Ann Transl Med, 2019; 7(23); 778
14. Gurbuz O, Kumtepe G, Ozkan H, Predictive value of neutrophil-lymphocyte ratio for long-term cardiovascular event following coronary artery bypass grafting: Braz J Cardiovasc Surg, 2020; 35(3); 274-84
15. Silberman S, Abu-Yunis U, Tauber R, Neutrophil-lymphocyte ratio: Prognostic impact in heart surgery. Early outcomes and late survival: Ann Thorac Surg, 2018; 105(2); 581-86
16. Johnson A, Pollard TJ, Shen L, MIMIC-III, a freely accessible critical care database: Sci Data, 2016; 3; 160035
17. Metnitz P, Rui PM, Almeida E, SAPS 3 - From evaluation of the patient to evaluation of the intensive care unit. Part 1: Objectives, methods and cohort description: Intensive Care Med, 2005; 31(10); 1336-44
18. Zhang Z, Wu Y, Zhao Y, Dynamic changes in HMGB1 levels correlate with inflammatory responses during cardiopulmonary bypass: Exp Ther Med, 2013; 5(5); 1523-27
19. Madhok AB, Ojamaa K, Haridas V, Cytokine response in children undergoing surgery for congenital heart disease: Pediatr Cardiol, 2006; 27(4); 408-13
20. Gessler P, Schmitt B, Prètre R, Latal B, Inflammatory response and neurodevelopmental outcome after open-heart surgery in children: Pediatr Cardiol, 2009; 30(3); 301-5
21. Pearson TA, Mensah GA, Alexander RWCenters for Disease Control and Prevention; American Heart Association, Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association: Circulation, 2003; 107(3); 499-511
22. Madjid M, Awan I, Willerson JT, Leukocyte count and coronary heart disease: Implications for risk assessment: J Am Coll Cardiol, 2004; 44(10); 1945-56
23. Brown JR, Landis RC, Chaisson K, Preoperative white blood cell count and risk of 30-day readmission after cardiac surgery: Int J Inflam, 2013; 2013; 781024
24. Mahmood E, Knio ZO, Mahmood F, Preoperative asymptomatic leukocytosis and postoperative outcome in cardiac surgery patients: PLoS One, 2017; 12(9); e0182118
25. Leliefeld P, Wessels CM, Leenen L, The role of neutrophils in immune dysfunction during severe inflammation: Crit Care, 2016; 20(1); 1-9
26. Prabhu A, Sujatha DI, Ninan B, Neutrophil gelatinase associated lipocalin as a biomarker for acute kidney injury in patients undergoing coronary artery bypass grafting with cardiopulmonary bypass: Ann Vasc Surg, 2010; 24(4); 525-31
27. Herbert C, Patel M, Nugent A, Serum cystatin c as an early marker of neutrophil gelatinase-associated lipocalin-positive acute kidney injury resulting from cardiopulmonary bypass in infants with congenital heart disease: Congenit Heart Dis, 2015; 10(4); E180-88
28. Kohira S, Oka N, Inoue N, Effect of the neutrophil elastase inhibitor sivelestat on perioperative inflammatory response after pediatric heart surgery with cardiopulmonary bypass: A prospective randomized study: Artif Organs, 2013; 37(12); 1027-33
29. Nourshargh S, Alon R, Leukocyte migration into inflamed tissues: Immunity, 2014; 41(5); 694-707
30. Dupont G, Flory L, Morel J, Postoperative lymphopenia: An independent risk factor for postoperative pneumonia after lung cancer surgery, results of a case-control study: PLoS One, 2018; 13(10); e0205237
31. Tan TP, Arekapudi A, Metha J, Neutrophil-lymphocyte ratio as predictor of mortality and morbidity in cardiovascular surgery: A systematic review: ANZ J Surg, 2015; 85(6); 414-19
32. Gibson PH, Cuthbertson BH, Croal BL, Usefulness of neutrophil/lymphocyte ratio as predictor of new-onset atrial fibrillation after coronary artery bypass grafting: Am J Cardiol, 2010; 105(2); 186-91
33. Xu H, Sun Y, Zhang S, The relationship between neutrophil to lymphocyte ratio and clinical outcome in pediatric patients after cardiopulmonary bypass surgery: A retrospective study: Front Pediatr, 2019; 7; 308
34. Danesh J, Collins R, Appleby P, Peto R, Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: Meta-analyses of prospective studies: JAMA, 1998; 279(18); 1477-82
35. Turkmen K, Guney I, Yerlikaya FH, Tonbul HZ, The relationship between neutrophil-to-lymphocyte ratio and inflammation in end-stage renal disease patients: Ren Fail, 2012; 34(2); 155
36. Wang Q, Li J, Wang X, The neutrophil-lymphocyte ratio is associated with postoperative mortality of cardiac surgery: J Thorac Dis, 2021; 13(1); 67-75
Figures
Tables
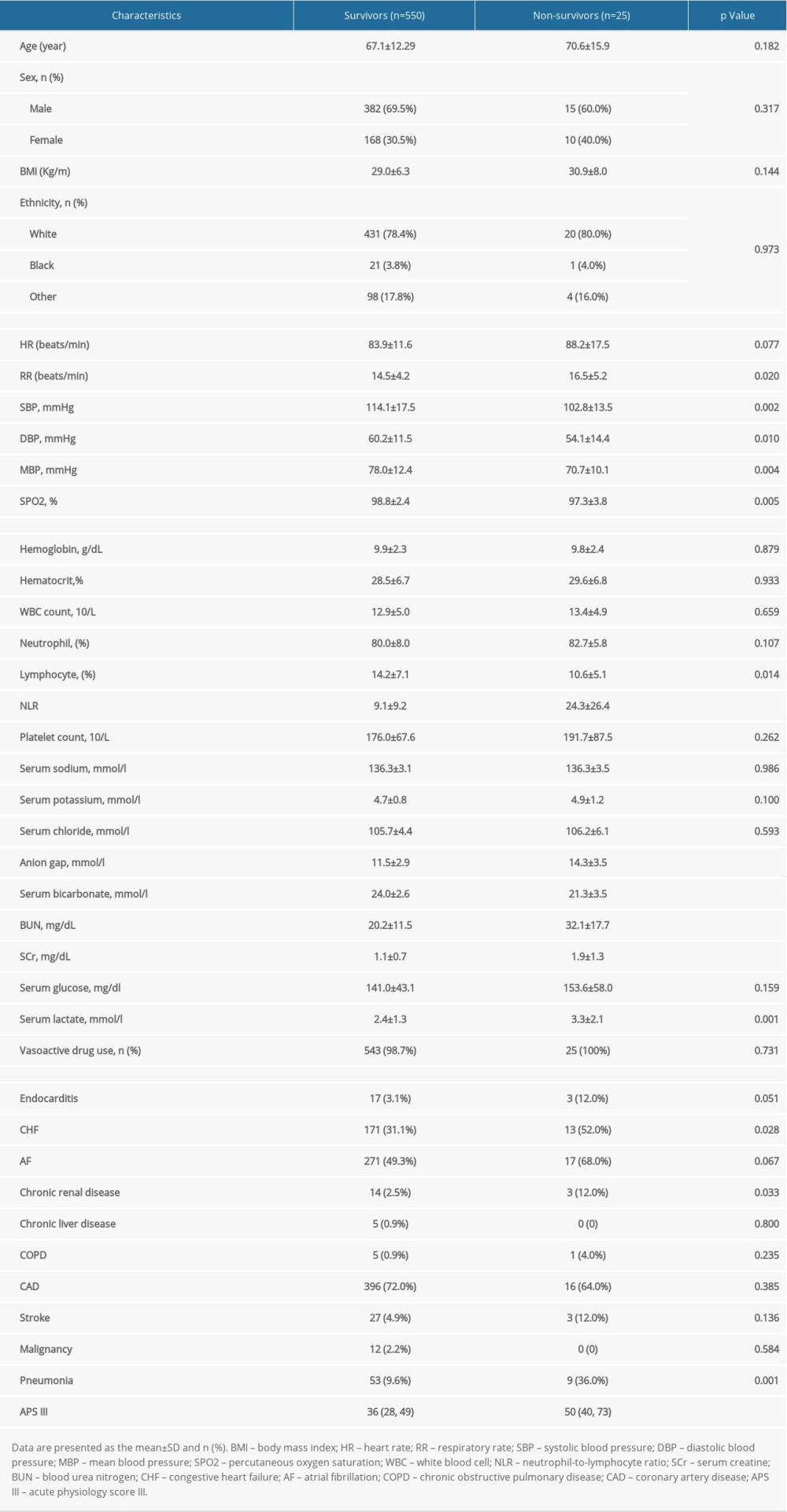 Table 1. Comparisons of demographics between survivors and non-survivors.
Table 1. Comparisons of demographics between survivors and non-survivors.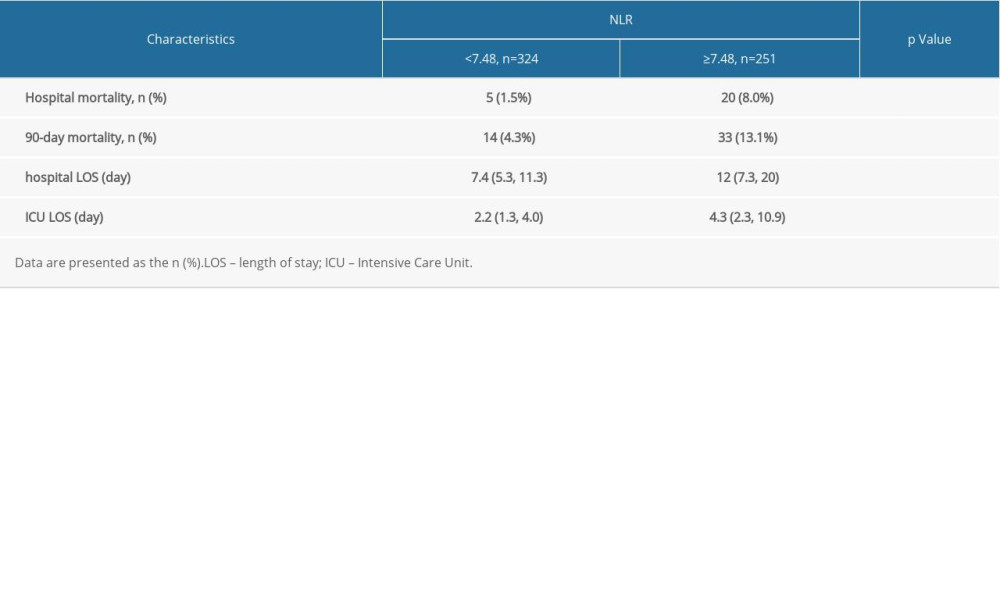 Table 2. Postoperative outcomes by the quartile of the neutrophil-to-lymphocyte ratio.
Table 2. Postoperative outcomes by the quartile of the neutrophil-to-lymphocyte ratio.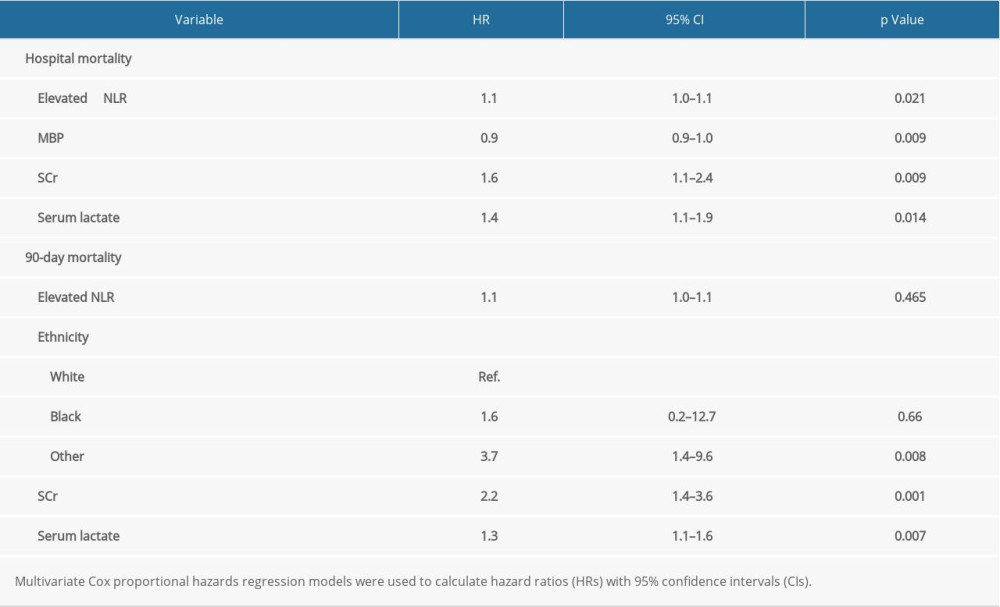 Table 3. Multivariate Cox hazard model NLR (adjusted HRs) for the possible predictors of outcomes in the study population.
Table 3. Multivariate Cox hazard model NLR (adjusted HRs) for the possible predictors of outcomes in the study population.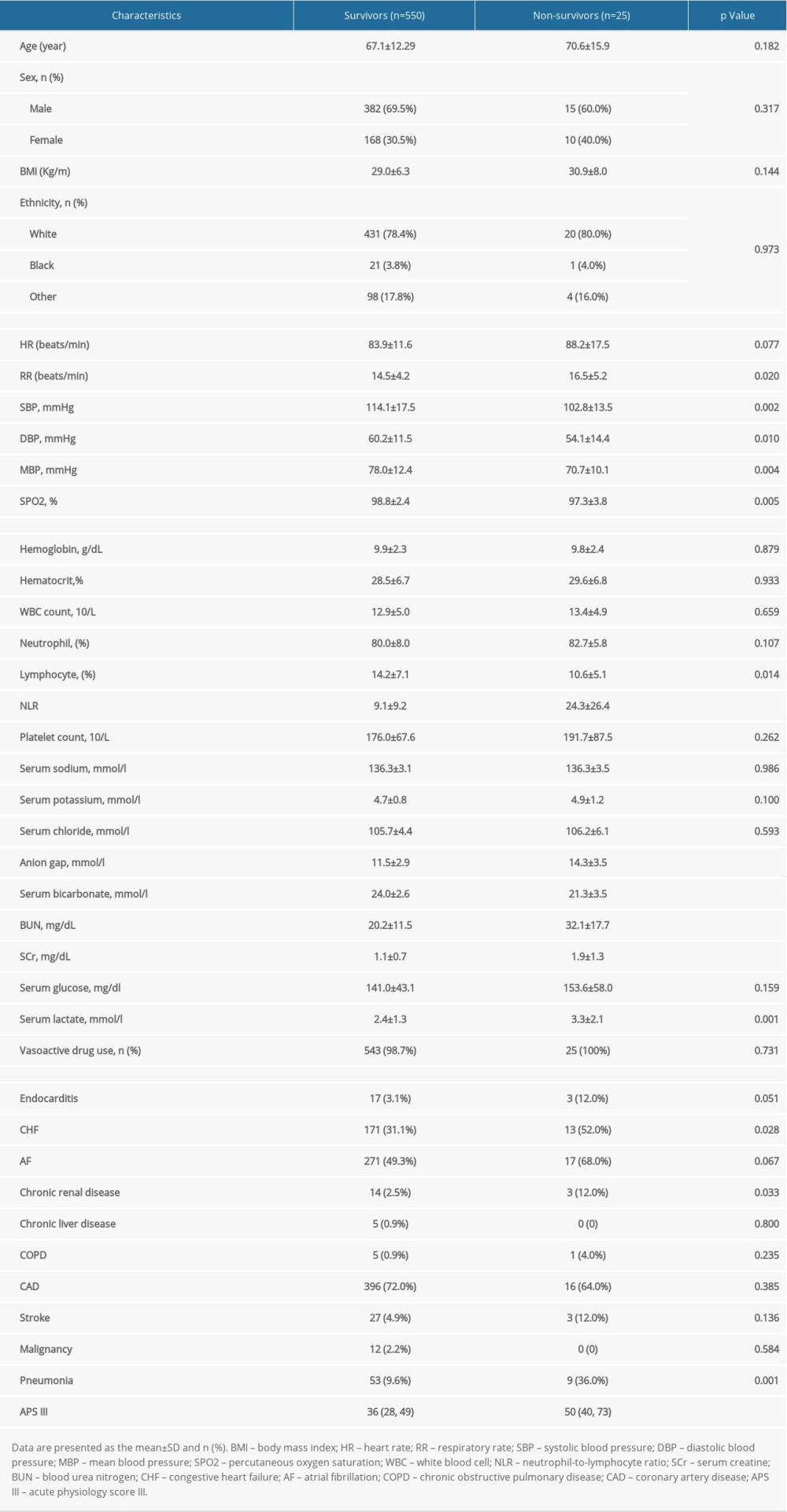 Table 1. Comparisons of demographics between survivors and non-survivors.
Table 1. Comparisons of demographics between survivors and non-survivors.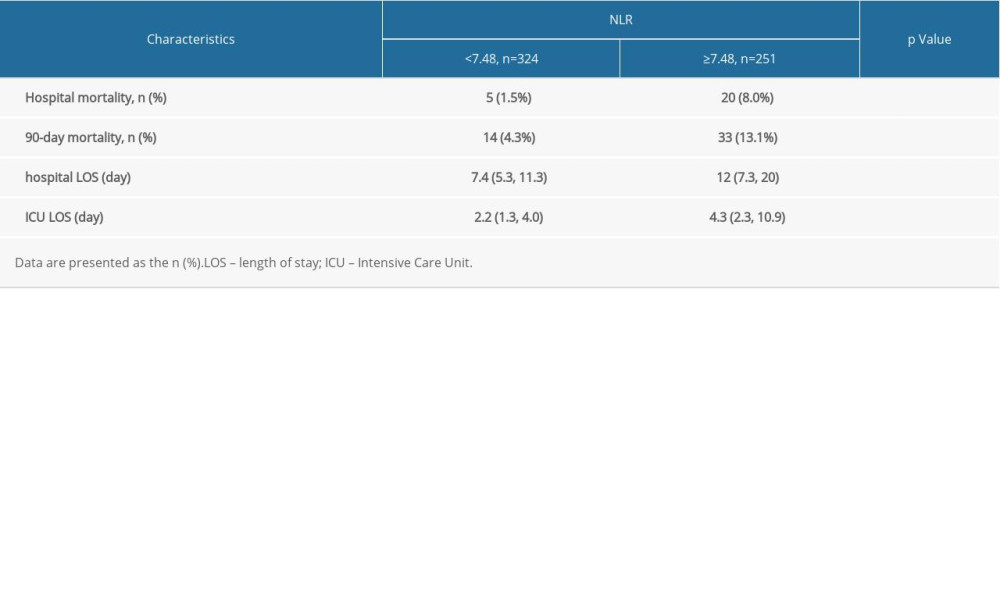 Table 2. Postoperative outcomes by the quartile of the neutrophil-to-lymphocyte ratio.
Table 2. Postoperative outcomes by the quartile of the neutrophil-to-lymphocyte ratio.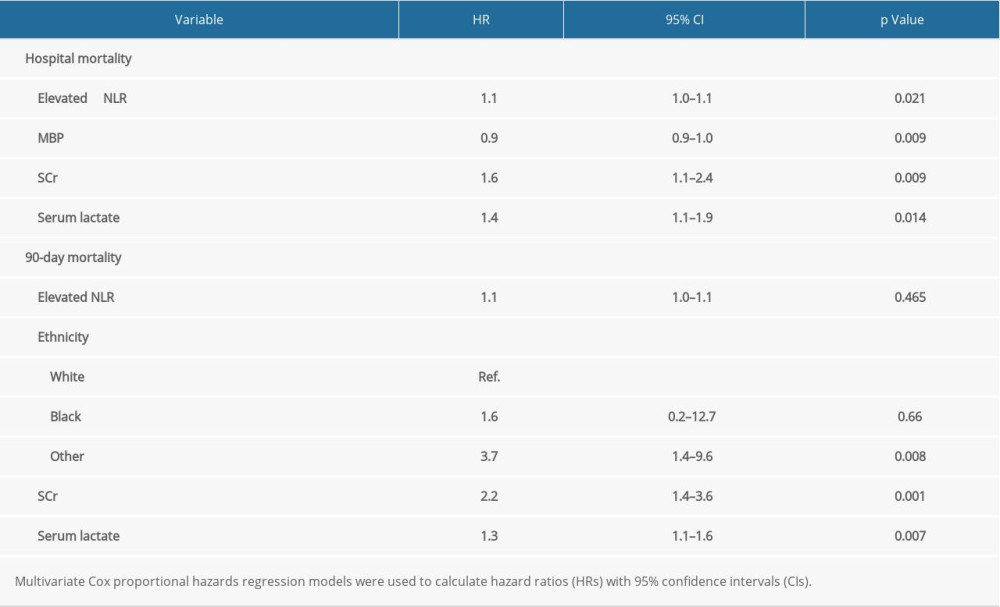 Table 3. Multivariate Cox hazard model NLR (adjusted HRs) for the possible predictors of outcomes in the study population.
Table 3. Multivariate Cox hazard model NLR (adjusted HRs) for the possible predictors of outcomes in the study population. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952