26 December 2021: Clinical Research
A Retrospective Evaluation of Operative and Postoperative Outcomes in Patients with Spinal Metastases from a Single Center to Compare Vertebrectomy with Combined Vertebrectomy and Radiofrequency Ablation
Xiuxin Han1DEFG, Chao Zhang1ABCD, Lili Li1FG, Yulin Ma1DEFG*, Guowen Wang1AEFGDOI: 10.12659/MSM.932995
Med Sci Monit 2021; 27:e932995
Abstract
BACKGROUND: This retrospective study was conducted at a single center and aimed to evaluate operative and postoperative outcomes in patients with spinal metastases using vertebrectomy and combined vertebrectomy and radiofrequency ablation (RFA).
MATERIAL AND METHODS: Patients diagnosed with spinal metastases between April 2009 and March 2016 (n=49) included patients who underwent vertebrectomy (n=26) and patients who underwent combined vertebrectomy and RFA (n=23). The characteristics of the 2 groups were similar in primary tumor types, comorbidities, Tomita score, vertebral involvement, preoperative bone pain, and neurologic deficit.
RESULTS: The results showed for the both groups that the visual analog scale (VAS) pain score was significantly decreased (P<0.05) and the neurological status was improved after treatment. Compared with the control group (vertebrectomy only), the combination group (combined vertebrectomy and RFA) had less intraoperative blood loss (P=0.002) and shorter operation time (P<0.001). The recurrence rate was lower (P=0.003) in the patients who received combined treatment, and the period of local recurrence was prolonged (P=0.030) in the combination group.
CONCLUSIONS: This retrospective study showed that the selective use of combined vertebrectomy and RFA significantly reduced surgical time and blood loss, improved recovery of neurologic deficit, and reduced the tumor recurrence rate in patients with spinal metastases.
Keywords: Orthopedic Procedures, radiofrequency ablation, Spine, Back Pain, Blood Loss, Surgical, Breast Neoplasms, Female, Humans, Kidney Neoplasms, Lung Neoplasms, Male, metastasectomy, operative time, Pedicle Screws, Progression-Free Survival, Prostatic Neoplasms, Spinal Neoplasms, Thyroid Neoplasms, vertebral body
Background
For the arterial system and the valveless venous plexus of Batson, 36–55% of patients with primary cancers such as breast cancer, lung cancer, prostate cancer, renal cancer, thyroid cancer, gastrointestinal cancer, or multiple myeloma develop spine diseases, resulting in spinal column involvement or intramedullary spinal cord metastases [1–4]. Patients with metastatic spinal tumors usually show symptoms of bone pain, spinal cord compression, pathologic fracture, hypercalcemia, and progressive deformity. In addition to creating neurologic deficits, the symptoms seriously worsen the quality of life and reduce survival [5]. The rate of spinal cord compression due to epidural metastases is approximately 5–10%. About 10–20% of these patients develop symptomatic spinal cord compression, and this number is projected to increase [6]. Therefore, it is very urgent to develop a new therapeutic strategy to manage pain and neurologic deficit of spinal metastases.
Clinical treatment options available for spinal metastases include medical therapy, radiation, and surgery [7]. Surgical resection appears to be the most effective therapy strategy [8]. The major goals of the operation are to relieve pain and neurologic symptoms, improve neurologic function, stabilize the spine, restrain local tumor recurrence, and prolong survival time [9,10]. The indications for surgical treatment include intractable pain, severe neural compression, obvious spinal instability and deformity, and ongoing radiation failure. However, there are substantial potential complications, including recurrence of primary malignancy caused by incomplete resection, which may be due to uncertain tumor margin, massive blood loss, cerebrospinal fluid fistulas, and new neurologic compromise [11]. Thus, it is essential to develop a complementary strategy to eliminate or alleviate these potential complications. The main indications include mechanical instability and high spinal cord compression. Surgery can significantly improve the quality of life and functional status of appropriate patients.
Surgical trends include minimally invasive surgery, emphasizing durable local control and spinal stability [12]. Recently, minimally invasive techniques such as RFA have received increasing attention due to their superiority in treating painful bone lesions [13,14]. With a sufficiently high focal temperature, RFA can destroy tumor tissue and exhibits a promising effect for pain palliation of bone metastasis patients [15,16]. Moreover, RFA combined with cementoplasty has been proved to be a safe and powerful technique for metastatic pain relief. The conditions of spinal metastases patients were improved and major goals of treatment were achieved, including pain management, as well as reduction of complications and tumors recurrence [17,18].
For patients with spinal metastases, it is extremely difficult to achieve a balance between complete tumor clearance and preserving spinal stability. Radical ventral tumor resection was found to be effective only for solitary metastases patients with a favorable long-term prognosis [19]. Multi-level spondylectomy can achieve complete tumor clearance, but at the cost of high risk of spinal instability and neurological deterioration, which may result in poor long-term oncological outcomes [20]. Tomita et al [21] originally proposed that total en-bloc spondylectomy (TES) to achieve oncological complete tumor resection was generally not recommended for multiple spinal metastatic lesions. In this case, radiotherapy was considered as the primary treatment for multiple spinal metastases in the absence of an acute neurological deficit [1]. In fact, palliative surgery (decompression) is often performed for multiple spinal metastases to alleviate symptom [22].
Surgical resection and RFA have their own merits in management of spinal metastases. Therefore, this retrospective study was conducted at a single center and aimed to evaluate operative and postoperative outcomes in patients with spinal metastases using vertebrectomy and combined vertebrectomy and RFA.
Material and Methods
STUDY PATIENTS:
A total of 49 spinal metastases patients were identified. Written informed consent was obtained from each patient. Approval of the hospital and institutional review board was obtained before acquiring and analyzing patients’ information from our institutional database. The participants were recruited and received treatment according their own wishes during April 2009 and March 2016. Data were collected, including demographics information, preoperative investigations, operation details, and postoperative evaluations. The control group consisted of 26 patients (12 males and 14 females) who underwent vertebrectomy alone. The combination group consisted of 23 patients (12 males and 11 females) who underwent combined vertebrectomy and RFA. Each patient was diagnosed with 1 kind of primary malignancy and metastatic osseous disease. All the patients had a pain problem that was considered to be partially or totally refractory to analgesic medications. Moreover, patients were required to have neurologic impairment due to metastatic epidural spinal cord compression (MESCC). The inclusion criteria were adult patients whose survival was expected to be more than 3 months, with a diagnosis of spinal metastatic tumors, and a vertebral lesion generating spinal compression symptoms or pain could be accurately defined. Patients with severe cardiopulmonary dysfunction or cerebrovascular disease who could not tolerate anesthesia or surgery were excluded.
PRE-TREATMENT EVALUATION:
Before undergoing treatment, the pain level of all the patients was strictly evaluated by VAS, which contains a 11-point scale ranging from 0 (no pain) to 10 (the most severe pain), as previously described by the Brief Pain Inventory [17]. The Frankel scale was used for assessment of neurological symptoms [2]. In addition, all patients had detailed cross-sectional imaging by either CT or MRI.
SURGICAL PROCEDURE:
For the combination group, vertebrectomy and RFA were sequentially performed via posterior approaches, which had 2 steps for a single operation in the same sitting position. RFA was first performed for the normal vertebrae and then the involved vertebrae were treated guided by preoperative radiographic findings. To expose vertebrae involvement under direct visualization, the surgical approach was posterior midline exposure under local infiltration anesthesia with 0.25~0.5% lidocaine. The success rate was 100% (53 of 53 treatments) in 13 patients. According to preoperative radiographic findings (including X-rays, CT, and MRI), RFA was first administered into the exposed normal vertebrae. For the vertebrae involved, an 11G or 13G bone puncture needle was then introduced into a Rita UniBlate unipolar needle. This step was aimed to create the desired radius of ablation based on tumor size through modulating the unipolar needle by protuberating 1.0 cm~2.0 cm. Radiofrequency temperature was maintained at 70°C to 80°C and 1 application of 10-min ablation was utilized. The whole process was monitored during RFA, and the location of the unipolar needle was quickly modified if the patient had severe pain or chest distress. After RFA was accomplished, the surgical region was temporarily closed.
In the next step, vertebrectomy was performed under general anesthesia. After extraskeletal soft tissue tumor mass was removed, the vertebral elements were resected by posterolateral approach. The anterolateral vertebral body was then exposed and the tumor located in the vertebral body was removed. Segmental pedicle screw fixation was also performed as surgical fixation for the spinal column. The collapsed spinal column was repaired and reconstructed using an artificial vertebral body in the circumstance that more than 2/3 of the vertebral body was destroyed. In addition, vertebral augmentations were created by injecting bone cement, and vertebroplasty was also performed in several segmental jumping lesions.
POST-TREATMENT FOLLOW-UP:
Assessment of pain (VAS score) was carried out at 1 month and 6 months after procedures. Neurologic recovery was assessed by the Frankel scale. Routine X-rays, contrast-enhanced CT, and MRI were performed to confirm ablation by visualizing necrosis between the soft tissue and the bone, and to identify possible complications. Local recurrence was ascertained by histological evidence or radiographic imaging. The recurrence period was calculated as the time from treatment to appearance of recurrence evidence.
STATISTICAL ANALYSIS:
Data are presented as mean±SD. The Frankel scale and local recurrence rate between the 2 groups were calculated by Pearson chi-square tests. Statistical analyses were performed using SPSS 16.0 version software (SPSS, Inc., Chicago, IL, USA), and
Results
BASIC FEATURES OF THE STUDY SUBJECTS:
The mean age of the recruited patients was 62.35±8.02 years for the control group and 63.26±7.70 years for the combination group. In the control group, the primary malignances included 7 lung cancers, 4 breast cancers, 5 prostate cancers, 6 renal cancers, 3 thyroid cancer, and 1 unknown primary malignancy. There were 60 vertebral involvements including 27 thoracic spine, 30 lumbar spine, and 3 sacrum spine. In the combination group, the primary malignances included 6 lung cancers, 4 breast cancers, 2 prostate cancers, 6 renal cancers, and 5 thyroid cancers. There were 53 vertebral involvements, including 25 thoracic spine, 27 lumbar spine, and 1 sacrum spine. Patients with spinal metastases were evaluated by Tomita score. In the control group, 6 patients scored 4, 5 patients scored 5, 7 patients scored 6, and 8 patients scored 7. In the combination group, 5 patients scored 4, 5 patients scored 5, 6 patients scored 6, and 7 patients scored 7. The 2 groups were similar in characteristics of primary tumors, comorbidities, Tomita score, and preoperative findings such as bone pain and neurologic deficit. The average procedure time of RFA was 7.35±1.75 min.
COMPARISON OF TREATMENT OUTCOMES:
Combined vertebrectomy and RFA alleviated pain and improved neurological status. As shown in Figure 1, the pain scale rating was significantly reduced in both groups. In the control group, the VAS score was reduced from 7.96±1.51 before surgery to 4.92±1.41 at 1 month after surgery and 2.0±1.69 at 6 months after surgery (P=0.0002, 0.016). In the combination group, the VAS score was reduced from 7.39±1.37 to 4.52±1.56 at 1 month after surgery, and 2.3±1.66 at 6 month after surgery, respectively (P=0.0007, 0.005). However, there was no statistically significant difference between the 2 groups (P=0.690, at 6 months after surgery).
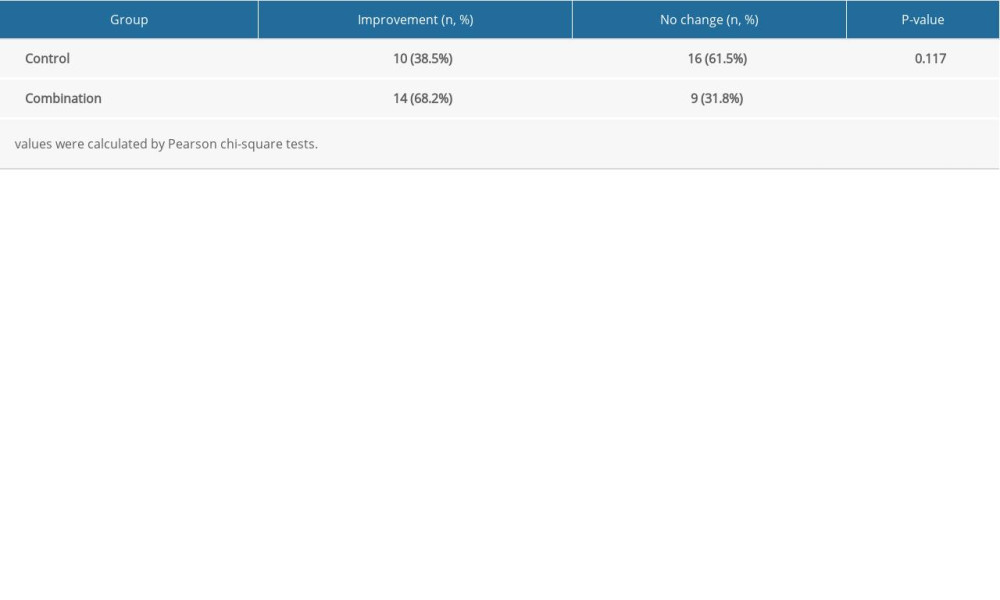
In the control group, 38.5% (10/26) of patients showed improved postoperative Frankel grade, and 61.5% (16/26) of patients had no changes in Frankel grade. No patients had reduced Frankel grade. In addition, 64.3% (9/14) of patients who were Frankel C before surgery became ambulatory after surgery, changing to Frankel D grade, and 8.3% (1/12) of patients who were Frankel D grade before surgery improved to Frankel E grade. In the combination group, 60.9% (14/23) of patients showed improved postoperative Frankel grade, and 39.1% (9/23) of patients had no changes in Frankel grade. No patients had reduced Frankel grade. In addition, 84.6% (11/13) of patients who were Frankel C before surgery became ambulatory after surgery, changing to Frankel D grade. One patient who was nonambulatory Frankel B grade before surgery improved to Frankel D grade after surgery, and 22.2% (2/9) of patients who were Frankel D before surgery improved to Frankel E after surgery. Neurological function was improved in both groups, and there was no statistically significant difference between the 2 treatment groups (P=0.117) (Table 1).
Combined vertebrectomy and RFA improved surgical outcome. The average blood loss was 1088.7±429.9 ml per patient in the combination group, which was less compared with 1601.9±610.3 ml per patient in the control group (Figure 2, P=0.002). The operation time was shortened from 309.42±89.72 min in the control group to 207.39±88.02 min in the combination group (Figure 3, P<0.001).
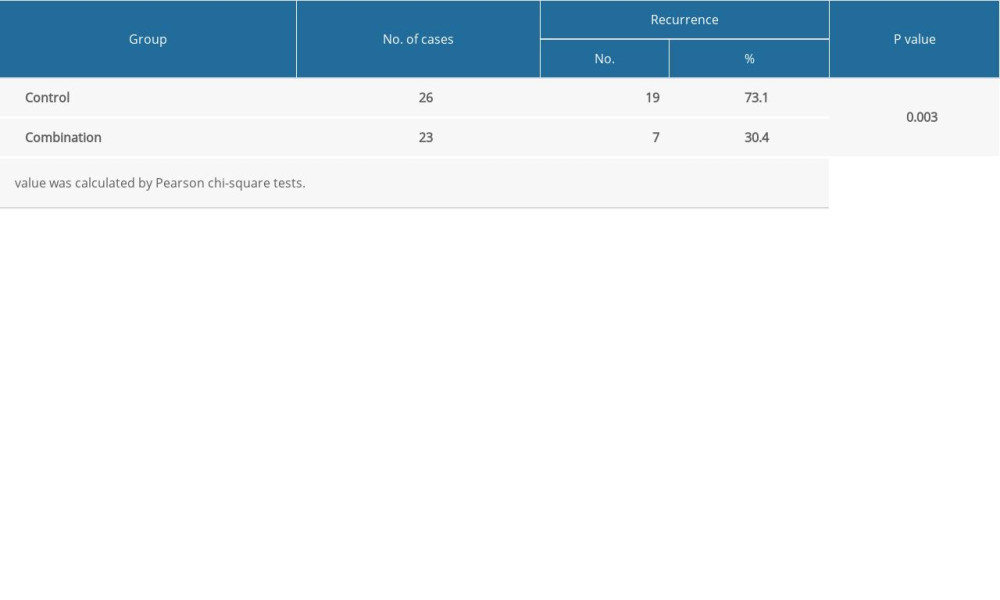
Combined vertebrectomy and RFA decreased recurrence incidence and prolonged the recurrence-free period. As shown in Table 2, 19 patients (73%) in the control group developed recurrence at the end of the study, whereas 7 patients (30.4%) developed recurrence in the combination group. The 2 groups showed a statistically significant difference in recurrence rate (P=0.003). Moreover, the recurrence period in the control group was 9.84±2.93 months, whereas the mean recurrence period in the combination group was 14.00±2.24 months. The period between treatment and recurrence was significantly longer in the combination group than in the control group (Figure 4, P=0.002).
Discussion
Previous studies found that RFA combined with PVP is mainly used in the treatment of spinal metastases to alleviate pain and strengthen the stability of vertebrae, but pain relief is limited [2,13,17,18]. The present retrospective study showed that the selective use of combined vertebrectomy and RFA significantly reduced surgical time and blood loss, improved recovery of neurologic deficit, and reduced the tumor recurrence rate in patients with spinal metastases.
The management of spinal metastases has been evolving in past decade [5,24]. Surgical resection remains a standard palliative treatment [2]. However, the limited efficacy of laminectomy and its associated complications such as spinal instability increasingly give rise to a notion that surgery cannot be the primary treatment for metastatic spinal disease [25,26]. Therefore, surgical techniques, implants, and expertise have evolved, and circumferential decompression and stabilization have been developed and are becoming more widely used in managing metastatic spine disease [27,28]. RFA is a recently emerging modality which is considered to be safe, effective, and repeatable, and with low morbidity and mortality [14]. Minimally invasive targeted RFA with cement augmentation of spinal metastatic lesions is an effective treatment for patients with vertebral body metastases [29].
In this study, we compared the clinical outcomes of patients receiving vertebrectomy alone and those receiving combined vertebrectomy and RFA for treating spinal metastases. Our observations demonstrated the combined vertebrectomy and RFA is expected to be an available therapeutic modality for managing spinal metastases. Combined vertebrectomy and RFA could effectively alleviate intractable metastatic pain, improve surgical outcomes, decrease recurrence rate, and prolong the recurrence-free period.
Previous studies have reported that surgery could relieve intractable metastatic pain and improve neurologic function [22]. A recently published randomized controlled trial showed the effectiveness of surgery in improving neurologic function in patients with metastatic spinal disease [22]. Surgical resection in negative tumor margin could provide significant relief of bone pain, improve neurologic function, and increase postoperative survival for patients with solitary spinal metastases [30]. These findings are consistent with the results of the present study (Figure 1). RFA was also reported to be effective for pain relief [31]. In the present study, 38.5% (10/26) of patients showed improved postoperative Frankel grade in the control group, and 60.9% (14/23) of patients showed improved postoperative Frankel grade in the combination group. However, combined vertebrectomy and RFA did not further enhance the effects of pain relief or improvement of neurologic function by vertebrectomy.
Massive blood loss and longer operation time may pose additional challenges to surgical resection [32]. We found that combined vertebrectomy and RFA could effectively reduce blood loss and shorten the operation time (Figures 2, 3) compared with vertebrectomy alone, which was similar to previous reports [21,33]. RFA has been proved to be highly effective in achieving coagulation necrosis in tumors [3,34], and thus reduces intratumoral microvessel density and blood concentration [15]. Accordingly, vertebrectomy is expected to minimize bleeding and shorten the operation time. During surgery, we also observed that RFA created several confluent areas of necrosis in all cases, and the subsequent tumor masses were remarkably decreased. Our study demonstrated RFA is an important complementary treatment for surgical resection, especially when there are no definite tumor margins or abundant blood supply. In those cases, resection might lead to a bleeding problem, especially for those patients with thrombocytopenia and coagulopathy.
Local recurrence can prevent recovery of neurological function and worsen long-term outcomes, affecting the prognosis of spinal metastases patients. In this novel treatment, large tumors with neurological compromise due to metastatic epidural spinal cord compression were first ablated and then removed by vertebrectomy, while single small ones without neurologic deficit were directly ablated. RFA can result in necrosis of tumor tissue and promote tumor cell death, so RFA should be able to facilitate curative vertebrectomy and prevent recurrence. Our findings suggest that combined vertebrectomy and RFA can decrease recurrence rates (Table 2) and prolong the recurrence-free interval (Figure 4).
For treating spinal metastases, we found that in some situations the combination approach may be easier. First of all, RFA under direct visualization can ablate tumors and achieve complete tumor clearance with lower risk, especially when the tumor is extremely close to an important anatomical structure such as a major vessel, nerve root, or spinal cord. Secondly, it is much safer to use RFA when mobilizing the spine, while resection may lead to bleeding problems. These findings, together with previous evidence, strongly support that RFA is an appealing complementary treatment for vertebrectomy [1,14,31].
The limitation of this study is the small sample size in a single center, and larger samples and multicenter clinical research are needed to confirm the clinical value of combined vertebrectomy and RFA. Radiofrequency ablation has been widely used to treat spinal metastases in the last 10 years, but the most suitable working parameters need to be explored, and there are some differences between different types of probes. RFA can cause coagulation necrosis and apoptosis of vertebral tumors, but the specific mechanism still needs to be further studied.
Conclusions
This study showed that the selective use of combined vertebrectomy and RFA significantly reduced surgical time and blood loss, improved recovery of neurologic deficit, and reduced the recurrence rate in patients with spinal metastases.
Figures
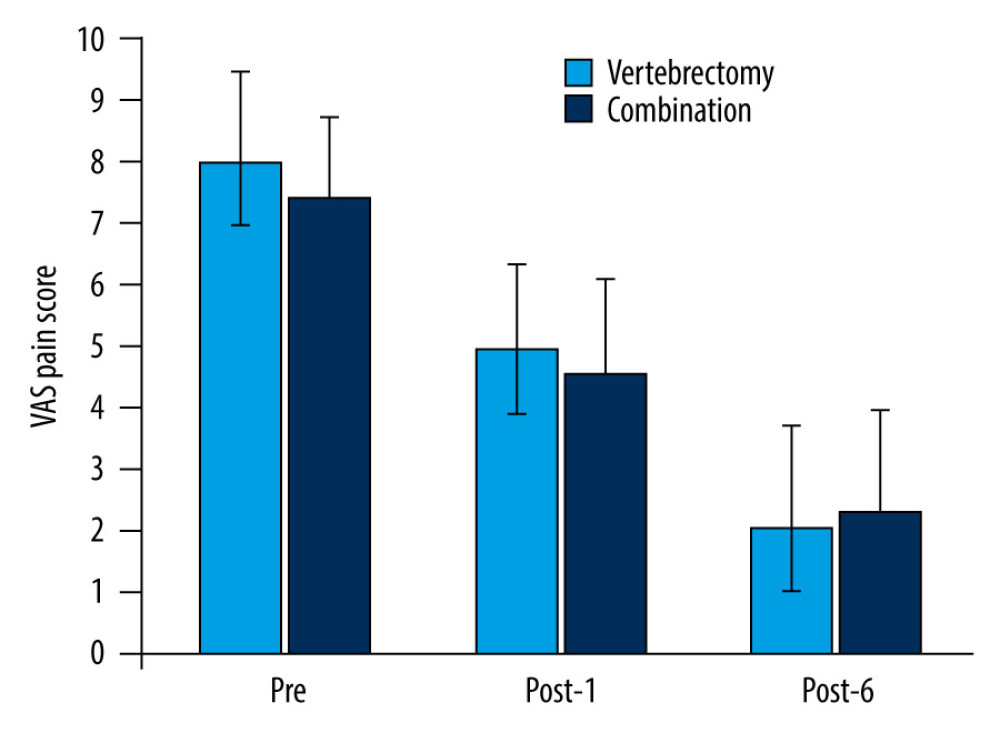 Figure 1. VAS in both groups. There was a statistically significant decrease (P=0.0002, 0.016) in the control group, while in the combination group there was a statistically more significant decrease (P=0.0007, 0.005). However, there was no statistically significant difference between the 2 groups (P=0.690, at 6 months after surgery). Pre – pre-treatment; Post-1 – 1 month after surgery; Post-6 – 6 months after surgery. Data are presented as mean±SD. VAS – visual analog scale.
Figure 1. VAS in both groups. There was a statistically significant decrease (P=0.0002, 0.016) in the control group, while in the combination group there was a statistically more significant decrease (P=0.0007, 0.005). However, there was no statistically significant difference between the 2 groups (P=0.690, at 6 months after surgery). Pre – pre-treatment; Post-1 – 1 month after surgery; Post-6 – 6 months after surgery. Data are presented as mean±SD. VAS – visual analog scale. 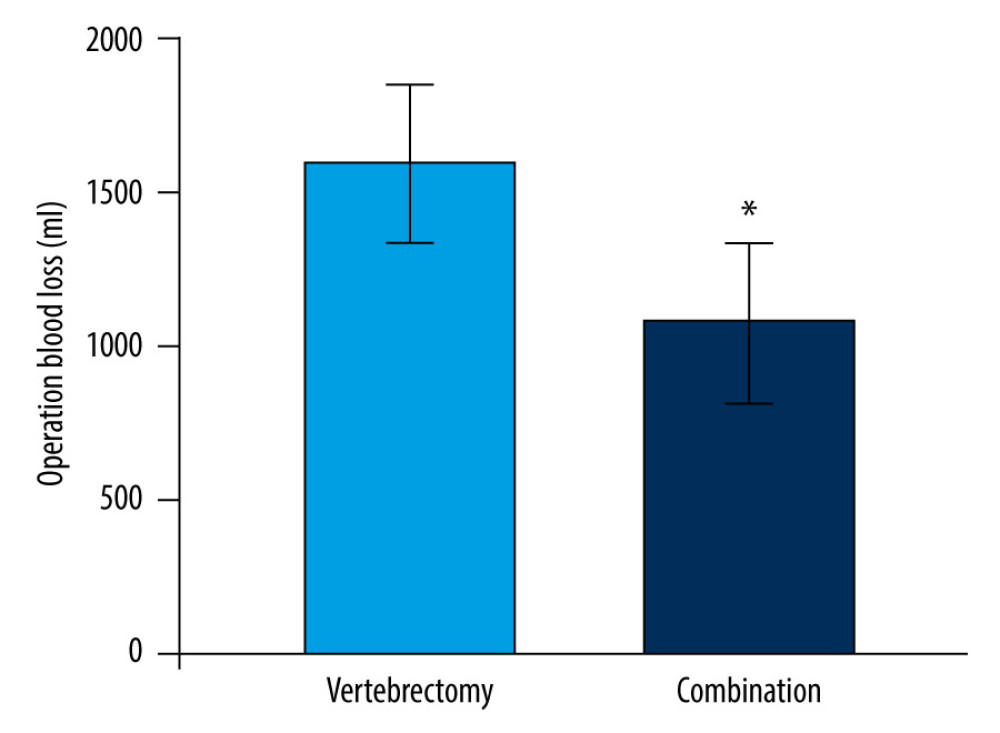 Figure 2. Surgical blood loss in both groups. There was a significant difference between the 2 groups (* P=0.034). Data are presented as mean±SD.
Figure 2. Surgical blood loss in both groups. There was a significant difference between the 2 groups (* P=0.034). Data are presented as mean±SD. 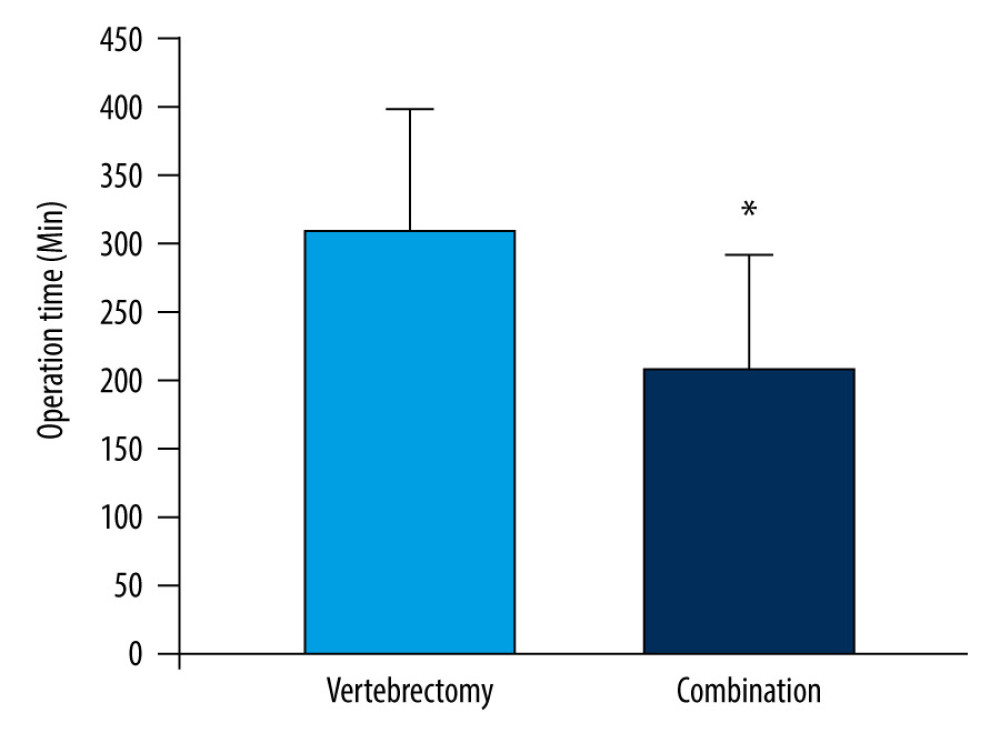 Figure 3. The operation time in both groups. There was a significant difference between the 2 groups (* P=0.025). Data are presented as mean±SD.
Figure 3. The operation time in both groups. There was a significant difference between the 2 groups (* P=0.025). Data are presented as mean±SD. 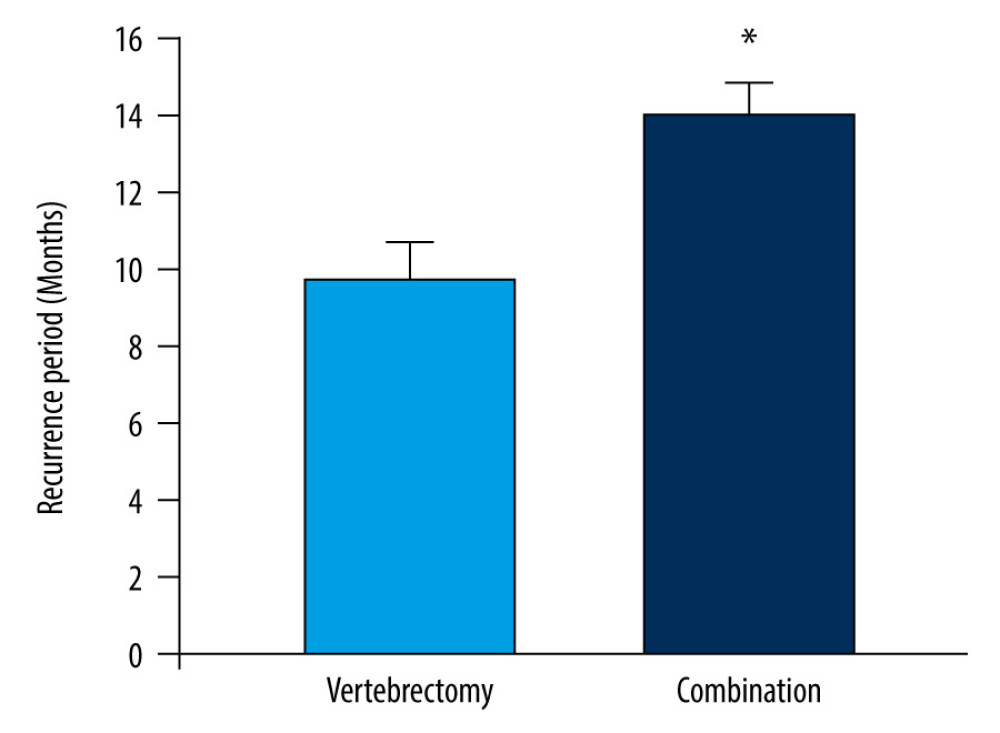 Figure 4. The recurrence-free period in both groups. The period between treatment and recurrence tended to be significantly longer in the combination group than in the control group (* P=0.030). Data are presented as mean±SD.
Figure 4. The recurrence-free period in both groups. The period between treatment and recurrence tended to be significantly longer in the combination group than in the control group (* P=0.030). Data are presented as mean±SD. References
1. Chen B, Xiao S, Tong X, Comparison of the therapeutic efficacy of surgery with or without adjuvant radiotherapy versus radiotherapy alone for metastatic spinal cord compression: A meta-analysis: World Neurosurg, 2015; 83(6); 1066-73
2. Quraishi NA, Arealis G, Salem KM, The surgical management of metastatic spinal tumors based on an Epidural Spinal Cord Compression (ESCC) scale]: Spine J, 2015; 15(8); 1738-43
3. Zhang C, Han X, Li L, Posterior decompression surgery and radiofrequency ablation followed by vertebroplasty in spinal metastases from lung cancer: Med Sci Monit, 2020; 26; e925169
4. Han XX, Tao F, Wang GW, Effect of combined treatment including surgery and postoperative adjuvant therapy on spinal metastases of Tomita type 7: Clin Neurol Neurosurg, 2019; 181; 112-18
5. Tai P, Dubey A, Salim M, Diagnosis and management of spinal metastasis of glioblastoma: Can J Neurol Sci, 2015; 42(6); 410-13
6. Thibault I, Al-Omair A, Masucci GL, Spine stereotactic body radiotherapy for renal cell cancer spinal metastases: analysis of outcomes and risk of vertebral compression fracture: J Neurosurg Spine, 2014; 21(5); 711-18
7. Bate BG, Khan NR, Kimball BY, Stereotactic radiosurgery for spinal metastases with or without separation surgery: J Neurosurg Spine, 2015; 22(4); 409-15
8. Bohm P, Huber J, The surgical treatment of bony metastases of the spine and limbs: J Bone Joint Surg Br, 2002; 84(4); 521-29
9. Jiang L, Liu XG, Wang C, Surgical treatment options for aggressive osteoblastoma in the mobile spine: Eur Spine J, 2015; 24(8); 1778-85
10. Barzilai O, Laufer I, Yamada Y, Integrating evidence-based medicine for treatment of spinal metastases into a decision framework: Neurologic, oncologic, mechanicals stability, and systemic disease: J Clin Oncol, 2017; 35(21); 2419-27
11. Tomita K, Kawahara N, Kobayashi T, Surgical strategy for spinal metastases: Spine (Phila Pa 1976), 2001; 26(3); 298-306
12. Barzilai O, Boriani S, Fisher CG, Essential concepts for the management of metastatic spine disease: What the surgeon should know and practice: Global Spine J, 2019; 9(1 Suppl); 98S-107S
13. Hoffmann RT, Jakobs TF, Trumm C, Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease: J Vasc Interv Radiol, 2008; 19(3); 419-25
14. Sheehan JP, Shaffrey CI, Schlesinger D, Radiosurgery in the treatment of spinal metastases: Tumor control, survival, and quality of life after helical tomotherapy: Neurosurgery, 2009; 65(6); 1052-61
15. Kim YS, Rhim H, Lim HK, Coagulation necrosis induced by radiofrequency ablation in the liver: Histopathologic and radiologic review of usual to extremely rare changes: Radiographics, 2011; 31(2); 377-90
16. Goetz MP, Callstrom MR, Charboneau JW, Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: A multicenter study: J Clin Oncol, 2004; 22(2); 300-6
17. Lane MD, Le HB, Lee S, Combination radiofrequency ablation and cementoplasty for palliative treatment of painful neoplastic bone metastasis: Experience with 53 treated lesions in 36 patients: Skeletal Radiol, 2011; 40(1); 25-32
18. Munk PL, Rashid F, Heran MK, Combined cementoplasty and radiofrequency ablation in the treatment of painful neoplastic lesions of bone: J Vasc Interv Radiol, 2009; 20(7); 903-11
19. Joaquim AF, Powers A, Laufer I, An update in the management of spinal metastases: Arq Neuropsiquiatr, 2015; 73(9); 795-802
20. Luzzati AD, Shah S, Gagliano F, Multilevel en bloc spondylectomy for tumors of the thoracic and lumbar spine is challenging but rewarding: Clin Orthop Relat Res, 2015; 473(3); 858-67
21. Tomita K, Kawahara N, Murakami H, Total en bloc spondylectomy for spinal tumors: Improvement of the technique and its associated basic background: J Orthop Sci, 2006; 11(1); 3-12
22. Walter J, Reichart R, Waschke A, Palliative considerations in the surgical treatment of spinal metastases: Evaluation of posterolateral decompression combined with posterior instrumentation: J Cancer Res Clin Oncol, 2012; 138(2); 301-10
23. Kam NM, Maingard J, Kok HK, Combined vertebral augmentation and radiofrequency ablation in the management of spinal metastases: An update: Curr Treat Options Oncol, 2017; 8(12); 74
24. Garfin SR, Yuan HA, Reiley MA, New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures: Spine (Phila Pa 1976), 2001; 26(14); 1511-15
25. Liang T, Wan Y, Zou X, Is surgery for spine metastasis reasonable in patients older than 60 years?: Clin Orthop Relat Res, 2013; 471(2); 628-39
26. Bartels RH, van der Linden YM, van der Graaf WT, Spinal extradural metastasis: Review of current treatment options: Cancer J Clin, 2008; 58(4); 245-59
27. Patchell RA, Tibbs PA, Regine WF, Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised trial: Lancet, 2005; 366(9486); 643-48
28. Akbar M, Ayache A, Eichler MManagement of spinal metastases, strategies and surgical indications: Orthopade, 2012; 41(8); 632-39 [in German]
29. Sayed D, Jacobs D, Sowder T, Spinal radiofrequency ablation combined with cement augmentation for painful spinal vertebral metastasis: A single-center prospective study: Pain Physician, 2019; 22(5); E441-49
30. Gasbarrini A, Li H, Cappuccio M, Efficacy evaluation of a new treatment algorithm for spinal metastases: Spine (Phila Pa 1976), 2010; 35(15); 1466-70
31. Wallace AN, Greenwood TJ, Jennings JW, Radiofrequency ablation and vertebral augmentation for palliation of painful spinal metastases: J Neurooncol, 2015; 124(1); 111-18
32. Wood TJ, Racano A, Yeung H, Surgical management of bone metastases: Quality of evidence and systematic review: Ann Surg Oncol, 2014; 21(13); 4081-89
33. Liu W, Zhou S, Wang S, Application of percutaneous vertebroplasty in the treatment of multiple thoracic metastases: Oncol Lett, 2015; 9(6); 2775-80
34. Goldberg SN, Kruskal JB, Oliver BS, Percutaneous tumor ablation: increased coagulation by combining radio-frequency ablation and ethanol instillation in a rat breast tumor model: Radiology, 2000; 217(3); 827-31
Figures
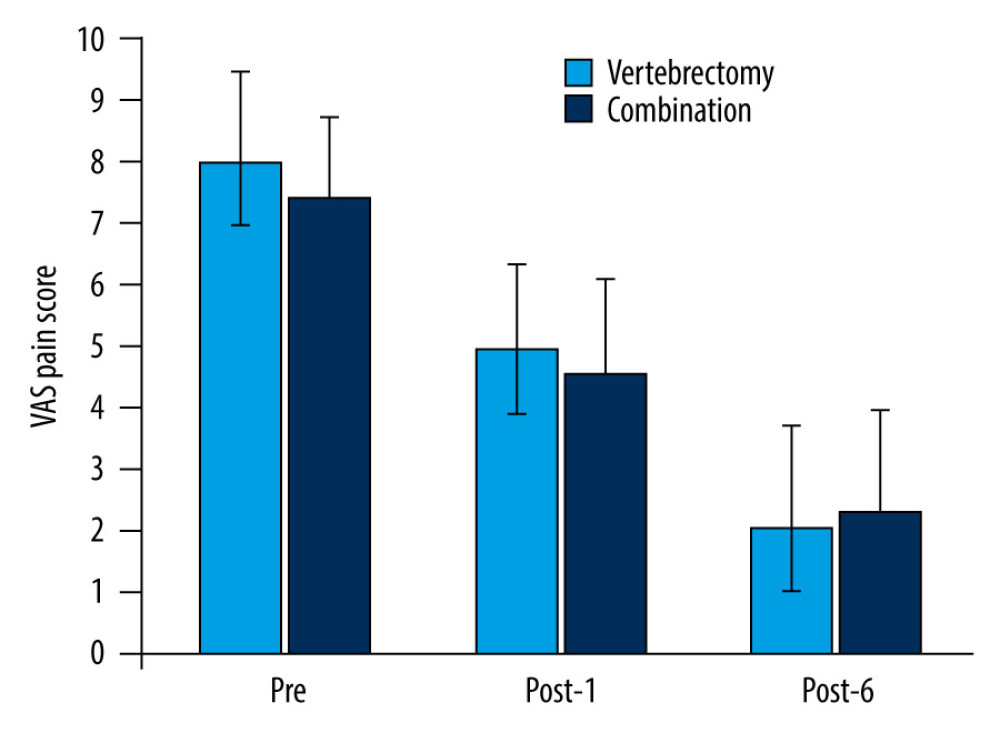 Figure 1. VAS in both groups. There was a statistically significant decrease (P=0.0002, 0.016) in the control group, while in the combination group there was a statistically more significant decrease (P=0.0007, 0.005). However, there was no statistically significant difference between the 2 groups (P=0.690, at 6 months after surgery). Pre – pre-treatment; Post-1 – 1 month after surgery; Post-6 – 6 months after surgery. Data are presented as mean±SD. VAS – visual analog scale.
Figure 1. VAS in both groups. There was a statistically significant decrease (P=0.0002, 0.016) in the control group, while in the combination group there was a statistically more significant decrease (P=0.0007, 0.005). However, there was no statistically significant difference between the 2 groups (P=0.690, at 6 months after surgery). Pre – pre-treatment; Post-1 – 1 month after surgery; Post-6 – 6 months after surgery. Data are presented as mean±SD. VAS – visual analog scale.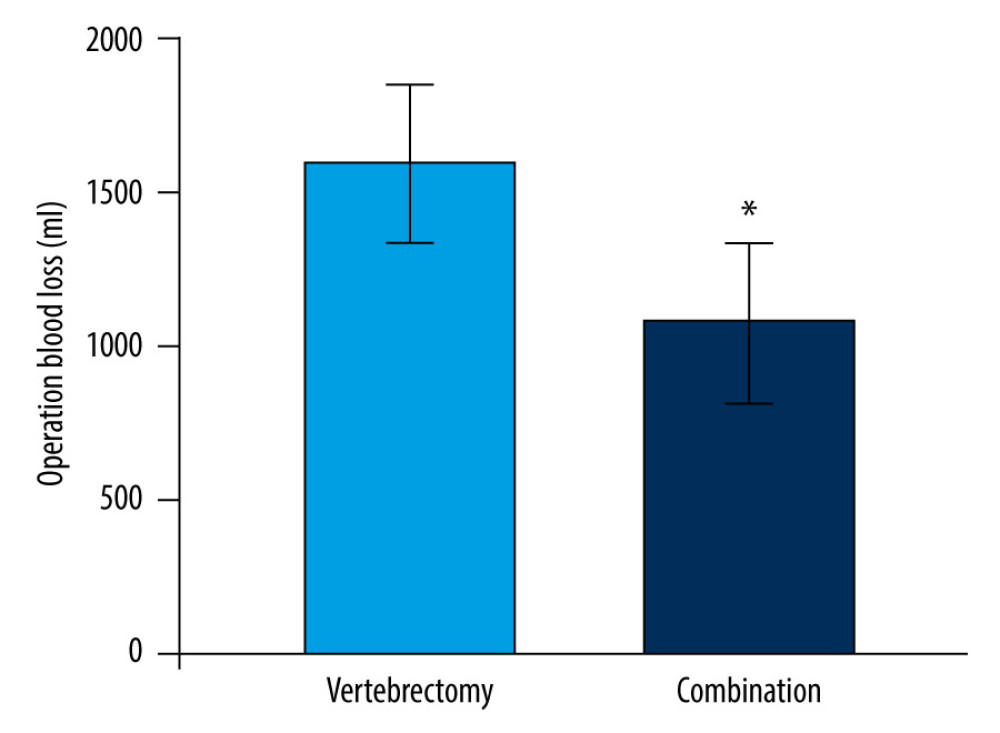 Figure 2. Surgical blood loss in both groups. There was a significant difference between the 2 groups (* P=0.034). Data are presented as mean±SD.
Figure 2. Surgical blood loss in both groups. There was a significant difference between the 2 groups (* P=0.034). Data are presented as mean±SD.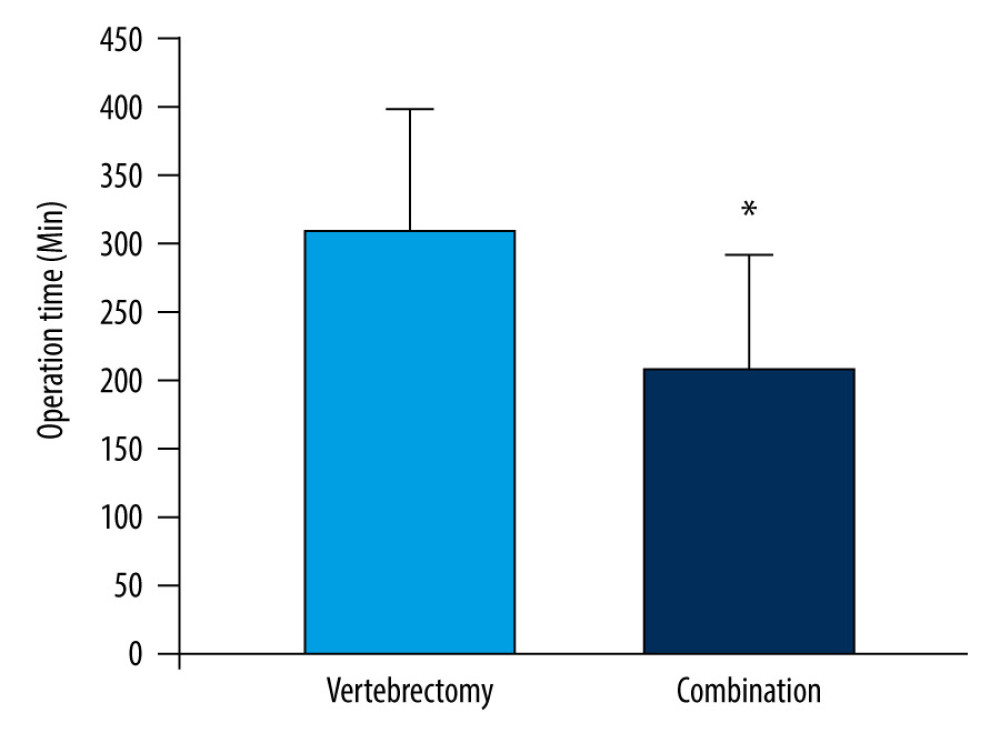 Figure 3. The operation time in both groups. There was a significant difference between the 2 groups (* P=0.025). Data are presented as mean±SD.
Figure 3. The operation time in both groups. There was a significant difference between the 2 groups (* P=0.025). Data are presented as mean±SD.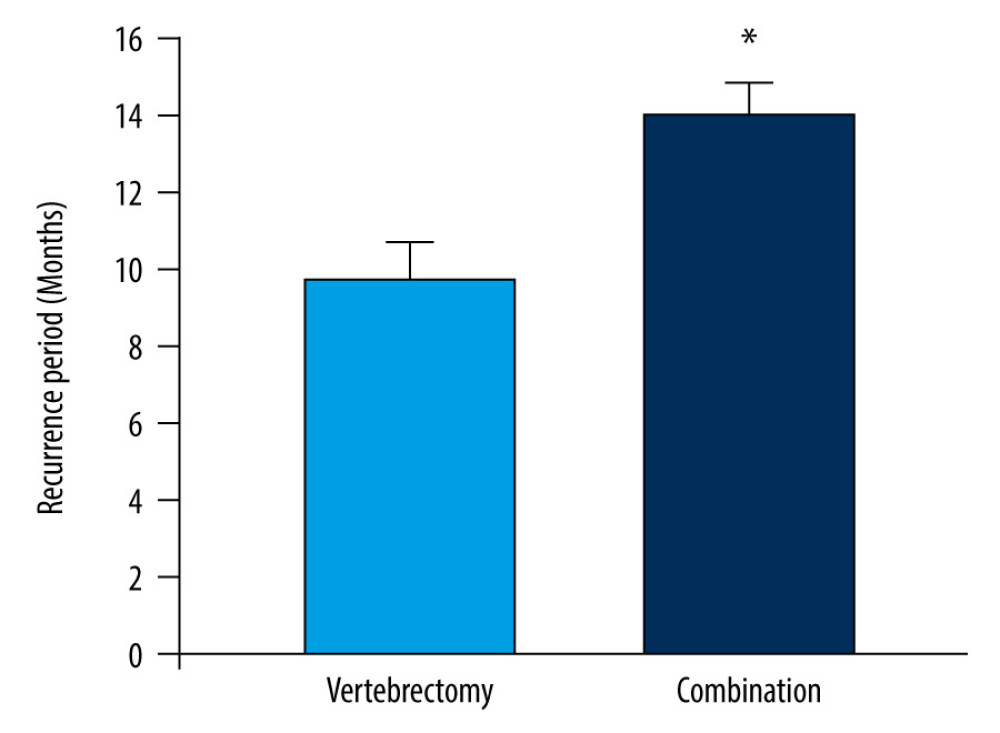 Figure 4. The recurrence-free period in both groups. The period between treatment and recurrence tended to be significantly longer in the combination group than in the control group (* P=0.030). Data are presented as mean±SD.
Figure 4. The recurrence-free period in both groups. The period between treatment and recurrence tended to be significantly longer in the combination group than in the control group (* P=0.030). Data are presented as mean±SD. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952