01 March 2022: Clinical Research
Serum Levels of N-Terminal Pro-Brain Natriuretic Peptide in Gestational Hypertension, Mild Preeclampsia, and Severe Preeclampsia: A Study from a Center in Zhejiang Province, China
Zhi Zheng12BEF, Xi Lin3CD, Xiaodong Cheng1AE*DOI: 10.12659/MSM.934285
Med Sci Monit 2022; 28:e934285
Abstract
BACKGROUND: Pre-eclampsia is one of the primary causes of maternal and newborn mortality. The pathogenesis of pre-eclampsia is still unclear. We aimed to investigate the link between serum N-terminal pro-brain natriuretic peptide (NT-proBNP) levels and pre-eclampsia.
MATERIAL AND METHODS: A total of 102 pregnant women with hypertensive disorders of pregnancy who were hospitalized and delivered in Wenzhou People’s Hospital from January 2019 to December 2019 were selected, including 43 patients with gestational hypertension, 32 patients with mild pre-eclampsia, and 27 patients with severe pre-eclampsia. Enzyme-linked fluorescence analysis was used to detect the serum NT-proBNP levels of the patients before delivery. We used the t test and ANOVA to compare differences between groups. Receiver operating curve (ROC) and the Youden index were used to evaluate the detection efficiency.
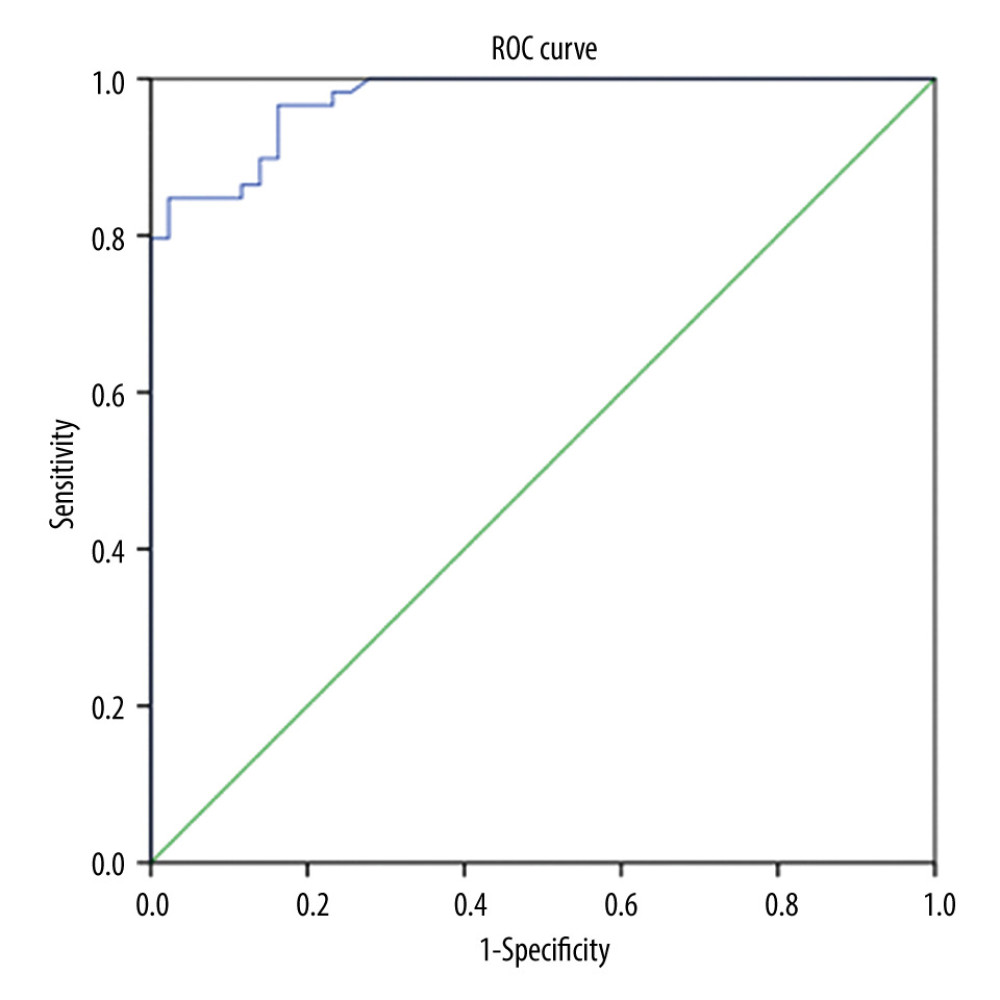
RESULTS: The average level of serum NT-proBNP in patients with mild pre-eclampsia was 197.12±105.80 pg/mL, which was significantly higher than that of patients with gestational hypertension (48.98±32.45 pg/mL) (P<0.05). Serum NT-proBNP in patients with severe pre-eclampsia (851.04±879.85 pg/mL) was higher than that in patients with moderate pre-eclampsia (P<0.05). The area under the ROC curve for diagnosing pre-eclampsia using NT-proBNP was 0.973, with NT-proBNP of 129.5 pg/mL as the cut-off value. The Youden index was 0.824, with a sensitivity for predicting pre-eclampsia of 84.7% and a specificity of 97.7%.
CONCLUSIONS: The level of serum NT-proBNP was as an effective indicator for predicting pre-eclampsia and judging the risk of pre-eclampsia.
Keywords: Hypertension, Pregnancy-Induced, Pre-Eclampsia, Pro-Brain Natriuretic Peptide (1-76), Adult, Blood Pressure, China, Female, Follow-Up Studies, Humans, Incidence, Infant, Newborn, Male, Natriuretic Peptide, Brain, Peptide Fragments, Pregnancy, Protein Precursors, ROC Curve, Severity of Illness Index
Background
Hypertensive disorders of pregnancy are one of the most common disorders in pregnant women, comprising gestational hypertension, pre-eclampsia, and eclampsia [1]. Pre-eclampsia is defined as the development of hypertension after 20 gestational weeks and is characterized by either proteinuria or signs of systemic disease, while gestational hypertension is defined as an elevated blood pressure after 20 gestational weeks [1]. Pre-eclampsia is a unique, multisystem-related disease of pregnant women, with an incidence of about 7% [2]. Also, it is currently among the most common causes of maternal and neonatal death. Studies have reported that pre-eclampsia is among the top 3 causes of maternal mortality in developing countries [3,4]. The number of pre-eclampsia cases is still growing worldwide [5,6]. Several studies have been conducted to identify the predictive factors of pre-eclampsia. However, to date, the pathogenesis of pre-eclampsia is still unclear. Early prediction and diagnosis of pre-eclampsia is important for improving maternal and infant prognosis. There is currently no reliable and practical method for predicting and judging the degree of pre-eclampsia.
The peptide hormone brain-type natriuretic peptide (BNP) and N-terminal (NT)-proBNP are produced in the ventricle as a response to increased blood volume and ventricle overload [7,8]. Heart failure can stimulate a sudden increase in BNP and NT-proBNP secretion. Recently, NT-proBNP was discovered as a new biomarker. Studies have shown that BNP and NT-proBNP can be used as effective biological indicators for the clinical diagnosis of congestive heart failure [9,10]. It has been reported that women with pre-eclampsia, one of the main contributing factors of heart burden, present with elevated serum levels of BNP and NT-proBNP [11,12]. By evaluating the serum NT-proBNP levels of 102 women with hypertensive disorders of pregnancy, we investigated the utility of NT-proBNP in the diagnosis and evaluation of pre-eclampsia.
Material and Methods
CLINICAL DATA:
From January 2019 to December 2019, 102 women diagnosed hypertensive disorders of pregnancy who were hospitalized and delivered at Wenzhou People’s Hospital were included in the study. Patients were divided into 3 groups according to the recent American College of Obstetricians and Gynecologists guidelines [1] as follows: 43 patients in the gestational hypertension group, 32 patients in the mild pre-eclampsia 32 group, and 27 patients in the severe pre-eclampsia group. Post hoc power analysis revealed a power of 1.0 (ηp2=0.354, α=0.05), which demonstrated that our sample size would be sufficient. The patients were 21 to 46 years old, with a median age of 28 years. The pregnant women included in the study were singleton pregnancies, with no previous organic diseases, kidney diseases, chronic hypertension, diabetes, systemic lupus erythematosus, and blood system diseases. We excluded patients who were using certain drugs during pregnancy and patients with severe infection during pregnancy. The Ethics Committee of our hospital approved this trial, and all patients gave their informed consent.
DETECTION OF NT-PROBNP:
After informed consent was obtained, about 2 mL of elbow venous blood was collected from each patient. The sample blood was added to an ethylene diamine tetraacetic acid-K2 anticoagulant tube. By centrifugation of blood at 3000 r/min for 15 min, serum was separated and was then stored in a refrigerator at −20 to be tested. Serum NT-proBNP was tested on an automatic immunoassay analyzer (VIDAS, Biomerieux, France) using enzyme-linked fluorescence analysis. Linearity was determined in the range of 20 000 to 25 000 pg/mL. Artificially synthesized NT-proBNP was used as the standard. All samples were measured in the same batch.
STATISTICAL ANALYSIS:
The data were analyzed by SPSS version 20.0 software (IBM Corp, Armonk, NY, USA). Measurement data are presented by the mean ± standard deviation. A
Results
GENERAL DATA:
The 3 groups had no statistically significant differences in age, number of pregnancies, and number of deliveries (P>0.05, Table 1).
COMPARISON OF SERUM NT-PROBNP LEVELS AMONG THE 3 GROUPS:
The level of serum NT-proBNP in patients with mild pre-eclampsia was 197.12±105.80 pg/mL, which was higher than that of patients with gestational hypertension (48.98±32.45 pg/mL) (P<0.05). Patients with severe pre-eclampsia had a serum NT-proBNP level of 851.04±879.85 pg/mL, which was higher than that of patients with mild pre-eclampsia (197.12±105.80 pg/mL) (P<0.05). With the development of hypertension during pregnancy, the level of serum NT-proBNP showed a gradual increase (Tables 2, 3).
ROC CURVE OF NT-PROBNP LEVELS IN BLOOD SERUM PREDICTED PRE-ECLAMPSIA:
We divided the 102 pregnant women into 2 groups: those with gestational hypertension and those with pre-eclampsia (including mild pre-eclampsia and severe pre-eclampsia), and the ROC curve was obtained (Figure 1). The AUC for NT-proBNP diagnosis of pre-eclampsia was 0.973. The optimal cut-off value for NT-proBNP was 129.5 pg/mL, with a sensitivity of 84.7% and a specificity of 97.7%. The Youden index was 0.824.
Discussion
Pre-eclampsia is a unique complication during pregnancy, with hypertension, edema, and proteinuria as the leading clinical manifestations and occurrence after the 20th week of gestation [13]. Pre-eclampsia can result in greater maternal and perinatal morbidity and mortality [14,15]. Severe cardiovascular dysfunction is common in pre-eclampsia. The reason for the increase in blood pressure is the increase in peripheral vascular resistance due to systemic arteriospasm, and the increase in peripheral vascular resistance aggravates the ventricular afterload in patients with pre-eclampsia, reducing the compliance of the ventricle. When evaluating the cardiac function of pregnant women with pre-eclampsia, echocardiography and clinical evaluation of ventricular function should be considered [16].
BNP is a neurohormonal from the ventricle that reflects dilated ventricular volume, overload, and increased wall tension [17]. BNP is commonly used to diagnose congestive heart failure, renal failure, and chronic liver disease [18]. Therefore, it is speculated that the serum BNP in patients with pre-eclampsia should be higher than normal, which is indicative of subclinical vascular disorders in these patients. It has been reported that patients with pre-eclampsia have elevated BNP and NT-proBNP levels as compared with those with normal pregnancies [12,19–21]. In the present study, through the detection of serum NT-proBNP in 102 pregnant women with hypertensive disorders of pregnancy, we discovered that the average level of blood NT-proBNP in patients with mild pre-eclampsia was higher than that of patients with gestational hypertension (
The early predictive value of BNP for pre-eclampsia has been reported. A case-control study by Resnik et al showed that the median BNP levels in healthy patients, patients with mild pre-eclampsia, and patients with severe pre-eclampsia were 17.8, 21.1, and 101 pg/mL, respectively [12]. A BNP cut-off of <40.6 pg/mL had a negative predictive value of 92% in excluding pre-eclampsia. In the present study, based on ROC curve results, the NT-proBNP level of 129.5 pg/mL was selected as the best cut-off value for predicting the onset of pre-eclampsia and an effective indicator of degree of severity. The cut-off value of NT-proBNP in the present study was similar to the that of a previously published study [12].
Serum levels of NT-proBNT in patients with pre-eclampsia have been poorly studied in the past. Our study showed that NT-proBNP in the blood correlated with the severity of pre-eclampsia. This study also had limitations. First, the sample size was relatively small, and additional studies with large sample sizes are required for further research. Second, we did not include a group of healthy pregnant women and lacked the follow-up of serum NT-proBNP levels after birth. Finally, whether the BNP value is related to pregnancy age, gestational week, and personal constitution needs further study. Therefore, further studies are needed to identify the correlation between NT-proBNP and pre-eclampsia.
Conclusions
Serum NT-proBNP was an effective indicator to evaluate pre-eclampsia, and the detection level has a good correlation with the grade of hypertension in pregnancy, which is helpful for the diagnosis and evaluation of pre-eclampsia.
References
1. , Gestational hypertension and preeclampsia: ACOG Practice Bulletin, Number 222: Obstet Gynecol, 2020; 135(6); e237-60
2. McGinnis R, Steinthorsdottir V, Williams NO, Variants in the fetal genome near FLT1 are associated with risk of preeclampsia: Nat Genet, 2017; 49(8); 1255-60
3. Hypertension in pregnancy, Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy Obstetrics and gynecology: Obstet Gynecol, 2013; 122(5); 1122-31
4. Creanga AA, Berg CJ, Syverson C, Pregnancy-related mortality in the United States, 2006–2010: Obstet Gynecol, 2015; 125(1); 5-12
5. Vousden N, Lawley E, Seed PT, Incidence of eclampsia and related complications across 10 low- and middle-resource geographical regions: Secondary analysis of a cluster randomised controlled trial: PLoS Med, 2019; 16(3); e1002775
6. Ghulmiyyah L, Sibai B, Maternal mortality from preeclampsia/eclampsia: Semin Perinatol, 2012; 36(1); 56-59
7. Nakagawa O, Ogawa Y, Itoh H, Rapid transcriptional activation and early mRNA turnover of brain natriuretic peptide in cardiocyte hypertrophy. Evidence for brain natriuretic peptide as an “emergency” cardiac hormone against ventricular overload: J Clin Invest, 1995; 96(3); 1280-87
8. Hunt PJ, Richards AM, Nicholls MG, Immunoreactive amino-terminal pro-brain natriuretic peptide (NT-PROBNP): A new marker of cardiac impairment: Clin Endocrinol (Oxf), 1997; 47(3); 287-96
9. Bhalla V, Willis S, Maisel AS, B-type natriuretic peptide: The level and the drug – partners in the diagnosis of congestive heart failure: Congest Heart Fail, 2004; 10(1 Suppl 1); 3-27
10. Chow SL, Maisel AS, Anand I, Role of biomarkers for the prevention, assessment, and management of heart failure: A scientific statement from the American Heart Association: Circulation, 2017; 135(22); e1054-91
11. Sadlecki P, Grabiec M, Walentowicz-Sadlecka M, Prenatal clinical assessment of NT-proBNP as a diagnostic tool for preeclampsia, gestational hypertension and gestational diabetes mellitus: PLoS One, 2016; 11(9); e0162957
12. Resnik JL, Hong C, Resnik R, Evaluation of B-type natriuretic peptide (BNP) levels in normal and preeclamptic women: Am J Obstet Gynecol, 2005; 193(2); 450-54
13. Mol BWJ, Roberts CT, Thangaratinam S, Pre-eclampsia: Lancet, 2016; 387(10022); 999-1011
14. Roberts JM, Cooper DW, Pathogenesis and genetics of pre-eclampsia: Lancet, 2001; 357(9249); 53-56
15. Burton GJ, Redman CW, Roberts JM, Pre-eclampsia: Pathophysiology and clinical implications: Br Med J, 2019; 366; l2381
16. Simmons LA, Gillin AG, Jeremy RW, Structural and functional changes in left ventricle during normotensive and preeclamptic pregnancy: Am J Physiol Heart Circ Physiol, 2002; 283(4); H1627-33
17. Fazlinezhad A, Rezaeian MK, Yousefzadeh H, Plasma brain natriuretic peptide (BNP) as an indicator of left ventricular function, early outcome and mechanical complications after acute myocardial infarction: Clin Med Insights Cardiol, 2011; 5; 77-83
18. Pimenta J, Paulo C, Gomes A, B-type natriuretic peptide is related to cardiac function and prognosis in hospitalized patients with decompensated cirrhosis: Liver Int, 2010; 30(7); 1059-66
19. James SK, Lindahl B, Siegbahn A, N-terminal pro-brain natriuretic peptide and other risk markers for the separate prediction of mortality and subsequent myocardial infarction in patients with unstable coronary artery disease: A Global Utilization of Strategies To Open occluded arteries (GUSTO)-IV substudy: Circulation, 2003; 108(3); 275-81
20. Kale A, Kale E, Yalinkaya A, The comparison of amino-terminal probrain natriuretic peptide levels in preeclampsia and normotensive pregnancy: J Perinat Med, 2005; 33(2); 121-24
21. Furuhashi N, Kimura H, Nagae H, Brain natriuretic peptide and atrial natriuretic peptide levels in normal pregnancy and preeclampsia: Gynecol Obstet Invest, 1994; 38(2); 73-77
Tables
 Table 1. Comparison of general data between the 3 groups.
Table 1. Comparison of general data between the 3 groups. Table 2. Comparison of serum NT-proBNP in the mild pre-eclampsia group and gestational hypertension group (pg/mL).
Table 2. Comparison of serum NT-proBNP in the mild pre-eclampsia group and gestational hypertension group (pg/mL). Table 3. Comparison of serum NT-proBNP in the mild pre-eclampsia group and severe pre-eclampsia group (pg/mL).
Table 3. Comparison of serum NT-proBNP in the mild pre-eclampsia group and severe pre-eclampsia group (pg/mL). Table 1. Comparison of general data between the 3 groups.
Table 1. Comparison of general data between the 3 groups. Table 2. Comparison of serum NT-proBNP in the mild pre-eclampsia group and gestational hypertension group (pg/mL).
Table 2. Comparison of serum NT-proBNP in the mild pre-eclampsia group and gestational hypertension group (pg/mL). Table 3. Comparison of serum NT-proBNP in the mild pre-eclampsia group and severe pre-eclampsia group (pg/mL).
Table 3. Comparison of serum NT-proBNP in the mild pre-eclampsia group and severe pre-eclampsia group (pg/mL). In Press
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952