11 November 2021: Clinical Research
Endovascular Repair of Thoracic Aorta Injury: 17 Years of Single-Center Experience
Václav ProcházkaDOI: 10.12659/MSM.934479
Med Sci Monit 2021; 27:e934479
Abstract
BACKGROUND: Traumatic thoracic aortic transection is one of the most severe complications of high-energy injuries, but patients rarely receive treatment, and it is fatal in the vast majority of cases. Due to the complexity of surgical revision for transection, endovascular repair with stent graft implantation is the preferred approach.
MATERIAL AND METHODS: We retrospectively analyzed the short-term and long-term treatment results for 31 patients (29 men, 2 women) treated at the Interventional Radiology Department, University Hospital Ostrava, for the isthmus part of a descending thoracic aorta injury between 2004 and 2020.
RESULTS: The median patient age was 48 years (interquartile range [IQR]: 28-63 years). The most common causes of injury were traffic accidents and falls or jumps, with the trauma location at the Ishimaru zones 2 to 4 of the aortic isthmus. Aortic stent grafts were successfully implanted in all patients; 13% of patients had complications and 10% died due to the trauma severity. The median procedure duration was 30 min (IQR: 25-43 min) and the median hospital stay was 29 days (IQR: 28-63 days).
CONCLUSIONS: Aortic stent graft implantation appears to be a safe and effective method for dealing with thoracic aorta injury, with a low complication rate and high patient survival. The endovascular approach is the method of choice for treating this severe disease, and a multidisciplinary approach for emergency medical treatment with a comprehensive trauma protocol is essential.
Keywords: Advanced Trauma Life Support Care, Aortic Diseases, endovascular procedures, Aorta, Thoracic, Czech Republic, Female, Humans, Male, Thoracic Injuries
Background
Traumatic thoracic aortic transection is one of the most severe complications of polytrauma. It most commonly arises during blunt trauma due to shear forces, typically in car accidents or falls from heights [1,2]. The aorta is mostly injured in the area of the aortic isthmus (“loco typico”), which is the weakest point of the aortic arch. The severity of this injury is characterized by less than 25% of patients surviving pre-hospital care [1,3]. One-third to one-half of patients die soon after hospital admission [1,4]. This aortic injury usually presents with significant hemodynamic instability or hemorrhagic shock with unconsciousness. Chest pain, paraplegia, or dyspnea can also be observed [5]. Associated injuries can also significantly worsen overall patient status. Urgent surgical revision through attempting a provisional suture, graft interposition, or thoracic aortic replacement used to be the only therapeutic option. However, in patients with polytrauma, this is a high-risk procedure with a mortality rate of up to 42% [6,7]. Recently, implantation of a stent graft in the damaged part of the thoracic aorta, a rapidly developing endovascular therapy known as thoracic endovascular aortic repair (TEVAR), has become the standard of care. This treatment creates a lower burden for the patient, with a lower risk of mortality [8] and complications [9]. However, because of the relatively few patients treated in this way, extensive descriptive studies are lacking in the literature. Here, we evaluate and analyze our experience with TEVAR for traumatic thoracic aortic transection in our center.
Material and Methods
This study analyzed data collected from patients who were admitted to the University Hospital Ostrava between 2004 and 2020 for thoracic aorta injury and were treated with the stent graft TEVAR procedure. All patients received standard pre-hospital care, and further treatment was organized via the hospital Emergency Department. Vital functions were stabilized according to the emergency trauma protocol. The baseline clinical evaluation and relevant blood analyses were recorded in the University Hospital Ostrava clinical research database, including blood pressure, Glasgow Coma Scale (GCS) score, blood cell count, and hemoglobin, aspartate aminotransferase, alanine aminotransferase, urea, creatinine, myoglobin, procalcitonin, and C-reactive protein levels. A whole-body computed tomography (CT) scan with CT angiography was completed before the endovascular therapy. Immediately after the verification of diagnosis and urgent clinical stabilization were completed, patients were transported to the radiology operating room for the endovascular aortic repair, with a self-expanding stent graft covering the aortic blunt trauma site.
After preparing the groin and inserting a 10F Terumo sheath into the common femoral artery, the aortic arch was carefully catheterized using a Vertebral 4F catheter (Merit Medical, Salt Lake City, UT, USA) and a Cordis STORQ guidewire (Cardinal Health, Dublin, Ireland). After verifying the aortic injury anatomy, location, and extension with digital subtraction angiography, a.035-inch wide/260-cm long Amplatz Super Stiff guidewire (Boston Scientific, Marlborough, MA, USA) was inserted into the ascending aorta. Subsequently, under angiographic road-map control or 3D navigation, the appropriate thoracic stent graft, most commonly a Zenith TAA endovascular graft (ZTEG), Zenith TX2 dissection endovascular graft (ZDEG, Cook Medical LLC, Bloomington, IN, USA), or earlier Valiant thoracic stent graft (Boston Scientific) was inserted.
The aortic injury near the left subclavian artery origin was covered with the stent graft positioned between the left common carotid artery and left subclavian artery. After implantation, the accurate positioning and sealing of the stent graft were controlled by the final angiography. The vascular access site was sutured percutaneously or surgically, and further monitoring was done at the cardiac surgical Intensive Care Unit (ICU). The procedure data (length, complication, stent graft type, length, and diameter, and distance from the left subclavian artery) were recorded in the database (Figure 1).
After stent graft implantation, all patients received standard intensive care and were followed during subsequent hospitalization and at the outpatient clinic after discharge from the hospital. The follow-up data included the blood transfusion volume, necessity of a follow-up CT scan, and overall and specific patient mortality count. We did not have any exclusion criteria for this treatment approach. Due to the emergency conditions of polytrauma, no informed consent was obtained before this life-saving procedure and aortic repair were performed. After stabilization, all surviving patients signed an informed consent for further follow-up. The local Ethics Committee of the University Hospital Ostrava approved the entire study.
For statistical analysis, numerical variables are expressed as the median and interquartile range (IQR, lower and upper quartile). Categorical variables are presented as absolute frequencies and relative frequencies. All statistical analyses were performed using R software (version 4.0.3, www.r-project.org).
Results
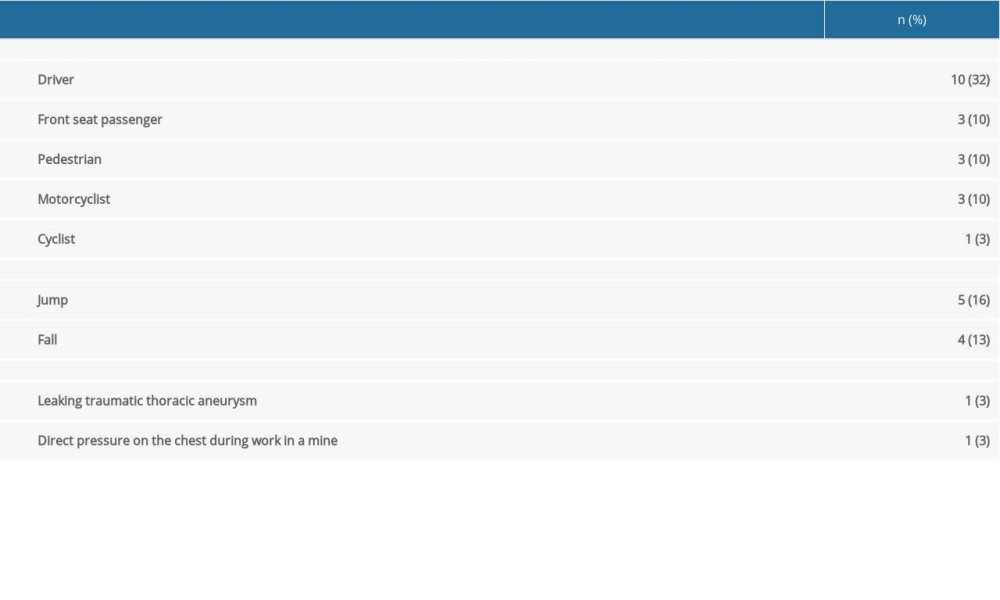
During a period of 17 years, 31 patients were treated with endovascular stent graft implantation at the University Hospital Ostrava. Car accidents were the most common cause of trauma (Table 1), followed by falls or jumps (accidental or suicidal). Rare causes of transection included 1 case of leaking post-traumatic thoracic aortic aneurysm and 1 case of aortic trauma at work in a mine.
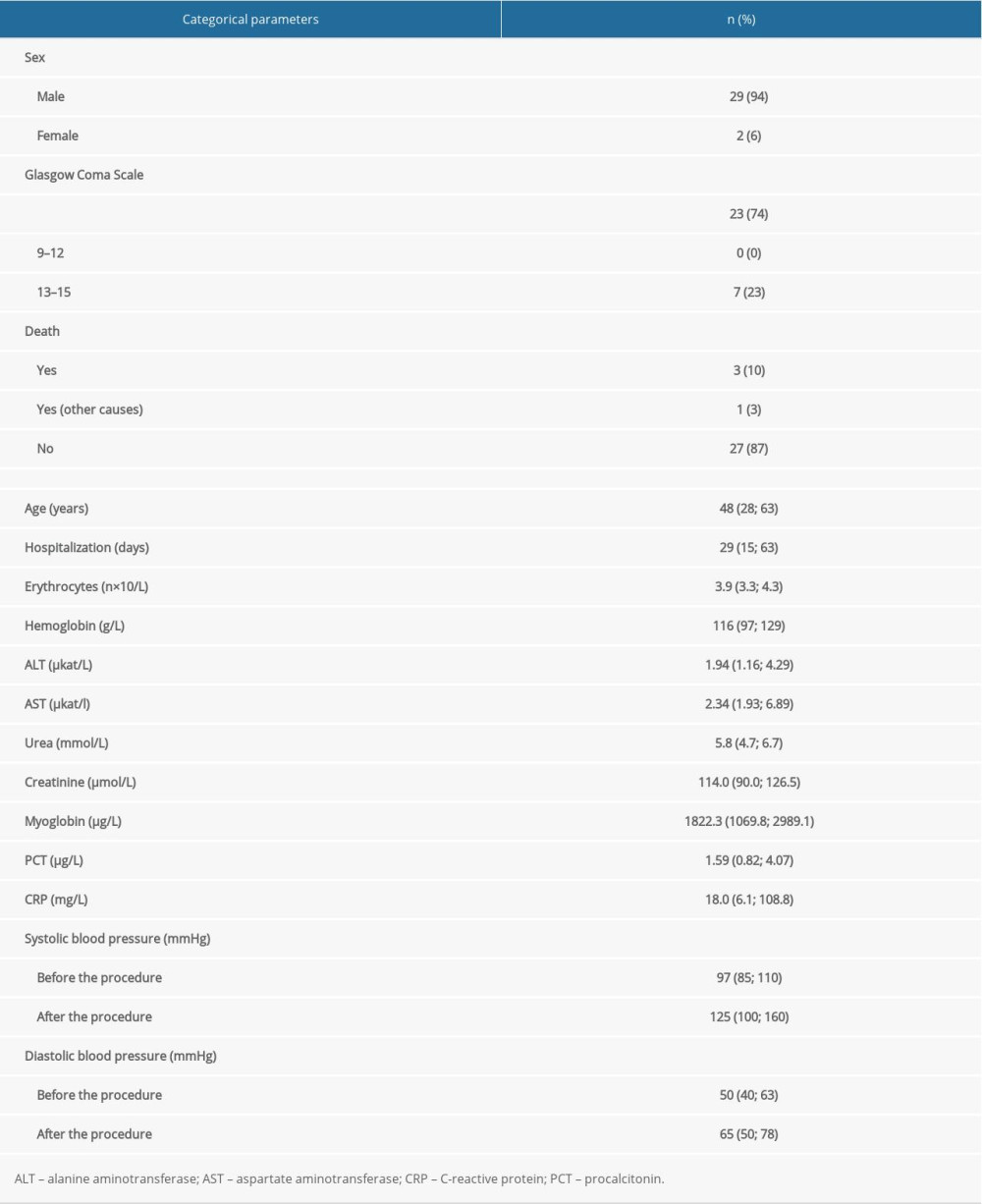
Table 2 shows the detailed patient information. Owing to the nature of the injury, most patients were unconscious and already intubated during pre-hospital care. Only 23% of patients had a GCS score between 13 and 15 and did not require essential life support. Patients in our cohort had severe hypotension, with a median blood pressure of 97/50 mmHg, when arriving at the Emergency Department. None of the patients showed laboratory signs of severe anemia. Trauma was always accompanied by mild hepatopathy and elevated myoglobin. Patients received red blood cell units during the first day of hospitalization, with a median dose of 2 (IQR: 1–8) units, and plasma at a median dose of 3 (IQR: 0–6) units. At admission, all patients underwent an initial CT scan according to the polytrauma protocol; 2 patients underwent 2 or more CT scans due to multiple complex lesions.
All patients underwent endovascular thoracic stent graft implantation. The most common device types used were the ZTEG (65%) and ZDEG (32%) (Cook Medical). In 1 (3%) earlier case, the Valiant thoracic stent graft (Boston Scientific) was implanted. Stent graft length ranged from 115 mm to 210 mm (median 142 mm) with a diameter of 24 mm to 38 mm (median 28 mm). The aortic injury location was in the Ishimaru zones 2 to 4 of the aortic isthmus, and the implantation position was 1 mm to 75 mm (median 14 mm) from the left subclavian artery origin in left subclavian artery (LSA) non-covering procedures (Figure 2). In a total of 4 patients, complications occurred during the procedure. One patient with tension hemothorax (Figure 1) had significant hemodynamic instability during the treatment course. The procedure was completed immediately after the stent graft placement with hemothorax drainage. In 1 patient, the stent graft was placed suboptimally, and subsequent PTA balloon remodeling was necessary for stent graft folding. Another patient required proximal stent graft extension after transposition of the supra-aortic vessels due to proximal leakage into the false lumen. One patient required additional extension implantation to anchor the distal thoracic aorta injury site. The implantation was performed 2 weeks after the primary procedure to prevent aortic rupture at the distal part of the original stent graft. In 22 patients (71%), the LSA was covered to achieve optimal placement of the stent graft. These procedures were performed after verification of the second vertebral artery patency on CT angiography. None of the patients developed the long-term difficulties after LSA overlay that are described in the literature. The procedure parameters are summarized in Table 3.
Overall, 27 patients (87%) recovered and were discharged from the hospital. Three patients (10%) died in the ICU as a result of concomitant injuries. Another patient died of cancer after discharge from the hospital. Within 1 month after the procedure, the stent graft position was verified by follow-up CT. Most patients were followed up at regular intervals (1, 6, and 12 months) with CT and ultrasound. No later complications were observed. The average follow-up period was 61.3 months after the procedure.
Discussion
Traumatic transection of the thoracic aorta is a life-threatening complication of high-energy injuries. Shear forces result in various degrees of aortic wall rupture, typically at the level of the aortic isthmus [10]. Owing to the nature of the injury, urgent management of the transection is necessary. In the latest guidelines from the Society for Vascular Surgery, endovascular treatment of aortic transection is preferred to open surgery [8]. The principal risks of open surgery are paraplegia (up to 25.5%), respiratory distress, and infectious complications (24–65%) [5,11–14]. The endovascular stent graft procedure is currently the first-line approach used immediately after resolution of any injuries that are potentially more life-threatening than aortic rupture [15–17]. In addition, definitive surgical management is possible only after the patient’s general condition has been stabilized. Conservative management is a possibility but is an outdated approach with worse results than open surgical and endovascular treatment (10-year survival 72.3% vs 77.2% and 85.7%, respectively). In contrast to the targeted therapy, conservative treatment is often associated with the development of life-threatening complications related to the aorta in 38% of cases [18]. Given the superior results of endovascular therapy, our data also confirm that successful stent graft implantation can rapidly stabilize circulation and normalize blood pressure.
Modern low-profile stent grafts usually support percutaneous access through the common femoral artery. In some patients (massive atherosclerosis in 0–14.3%), however, the external iliac artery must be used, typically with a retroperitoneal approach [15,16,19]. In both cases, surgical preparation of the access site is necessary as part of the intervention. In our study, we used a common femoral artery in all patients. A percutaneous approach with the subsequent use of a suturing device for artery sutures is often used for stent graft placement. Implanting a shorter stent graft with smaller diameters is typically recommended; some publications argue for lengths of less than 150 mm and diameters ranging from 20 mm to 30 mm [15]. Such stent grafts are more appropriate for younger patients without thoracic aortic dilatation, in whom a larger stent graft size can cause device collapse, bearing a risk of life-threatening complications and the need for repeated intervention [20]. In the present study, we predominantly used larger diameter stent grafts (24–38 mm), which did not increase the frequency of mechanical complications. The long-term follow-up of patients did not detect stent graft malposition. Some authors also recommend using endovascular ultrasonography or transesophageal echocardiography for exact sizing of the device. Stent graft selection based on measurements by CT angiography tends to underestimate the proper dimensions by 1 mm to 2 mm for the aortic arch size because of severe hypovolemia or hypotension [21].
Aortic stent graft implantation can occlude some arteries, most commonly the LSA or multiple intercostal arteries, presenting a specific issue. In our series, occlusion of the LSA was necessary in 71% of patients; none developed left upper extremity or arm claudication symptoms or ischemia. However, sufficient collateralization by the contralateral vertebral artery was always verified by CT angiography. Other studies have reported the need for LSA overlap in 23% to 50% of cases [2,15–17,19,22]; the main reason is a short distance (<20 mm) between the LSA ostium and the injury site.
In most cases, targeted LSA bypass surgery is unnecessary owing to the excellent collateral circulation of the upper left hand and brain supply [19]. Should the patient develop any upper limb claudication, these conditions can be treated successfully by the bypass procedure later. In some patients, the left common carotid artery also needs to be occluded. This situation can be resolved by implanting a branched stent graft or using the chimney technique. Other options are hybrid procedures, such as carotid-carotid crossover bypass or the complete debranching method with bifurcated bypass to the brachiocephalic trunk and the left common carotid artery, with subsequent stent graft placement in the aortic arch.
Another relatively frequent complication is an endoleak of the stent graft. We found this situation in 1 of our patients. It is often caused by dislocation or improper anchoring of the proximal part of the stent graft. The complication frequency is reported to be up to 14.3% and can be solved by stent graft extension [22,24]. Compared with surgery, endovascular stent graft implantation has a significantly lower risk of paraplegia (2.6% vs 9.9%, odds ratio 0.328) [9,25,26]. This is also influenced by the length of the spinal ischemia [3]. Another possible complication of endovascular treatment is aortic-bronchial fistula, which is often a dramatic event with high mortality [22,23]. Serious complications that have been observed are stent graft collapse or folding, which can obstruct the aortic lumen and usually require repeated endovascular intervention. Collapse can be solved by stent graft reimplantation or balloon angioplasty [2,10,20]. We can also encounter bronchial atelectasis [19], mesenteric ischemia [27], or vertebral artery occlusion in the context of LSA covering or an aortic arch of vertebral artery origin [23]. We did not observe these complications in our patients. All general complications, including ruptures or avulsions of the arteries, iatrogenic dissection, and pseudoaneurysm, can develop after the aortic repair. In general, the exact incidence of individual complications (except for LSA overlap, endoleak, and paraplegia) can only be estimated because of their low frequency and occurrence in all patient care units. Due to the excellent results of TEVAR, practically all authors of the above-mentioned studies recommend emergency stent graft implantation as the method of choice for all injuries because the patient is not directly endangered by other injuries causing hemodynamic instability. This recommendation is mainly supported by low patient mortality and a relatively low incidence of complications, as complications associated with implantation of the stent graft itself are rare [28]. This claim is supported by the high technical success rate of stent graft implantation [22,27]. Even relatively larger groups report a 30-day hospital mortality of 0% to 18% [2,15,17,18,24,29], consistent with the 10% hospital mortality in the present study.
Conclusions
The main limitation of this study is the retrospective evaluation of the collected data. However, our cohort presents the long-term results of patient follow-up after stent graft implantation. TEVAR is currently the method of choice for treating traumatic transection of the thoracic aorta, providing a shorter performance time, lower risk of complications, and high percentage of long-term patient survival, compared with surgical therapy. A multidisciplinary approach for emergency medical treatment with a comprehensive trauma protocol is essential.
Figures
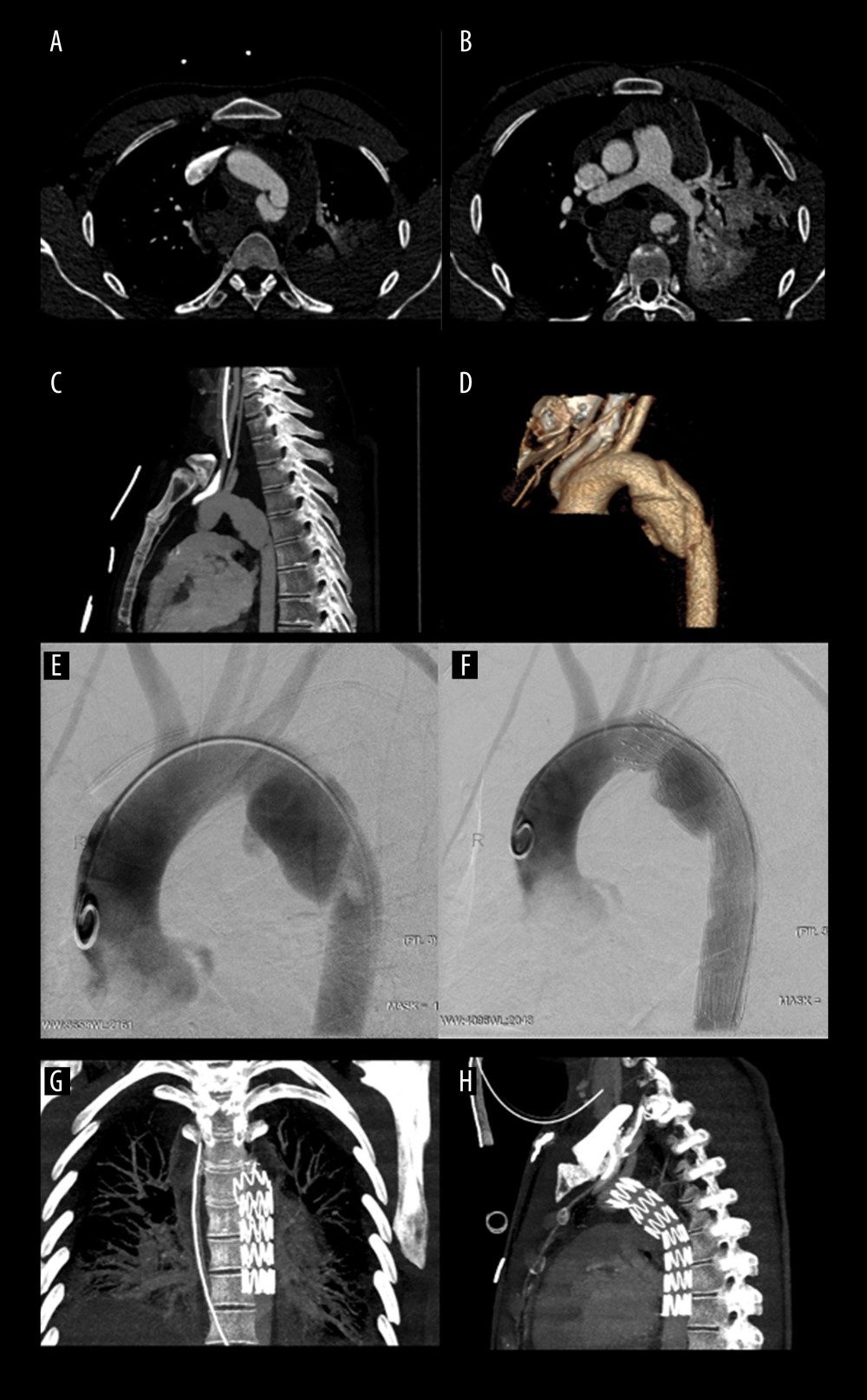 Figure 1. Thoracic aortic injury with active bleeding(A) Computed tomography (CT) angiogram of the axial maximum intensity projection (MIP) reconstruction with aortic trauma in loco typico. (B) CT showing left hemothorax, pulmonary trauma, and active bleeding. (C) CT MIP sagittal projection with aortic grade IV trauma. (D) CT volume rendering technique reconstruction of the aortic wall trauma grade IV. (E) Digital subtraction angiography with active contrast agent leakage. (F) ZDEG (Cook) stent graft implantation before the origin of the left vertebral artery with left subclavian artery coverage. (G) CT follow-up in coronal projection. (H) CT follow-up in sagittal projection.
Figure 1. Thoracic aortic injury with active bleeding(A) Computed tomography (CT) angiogram of the axial maximum intensity projection (MIP) reconstruction with aortic trauma in loco typico. (B) CT showing left hemothorax, pulmonary trauma, and active bleeding. (C) CT MIP sagittal projection with aortic grade IV trauma. (D) CT volume rendering technique reconstruction of the aortic wall trauma grade IV. (E) Digital subtraction angiography with active contrast agent leakage. (F) ZDEG (Cook) stent graft implantation before the origin of the left vertebral artery with left subclavian artery coverage. (G) CT follow-up in coronal projection. (H) CT follow-up in sagittal projection. 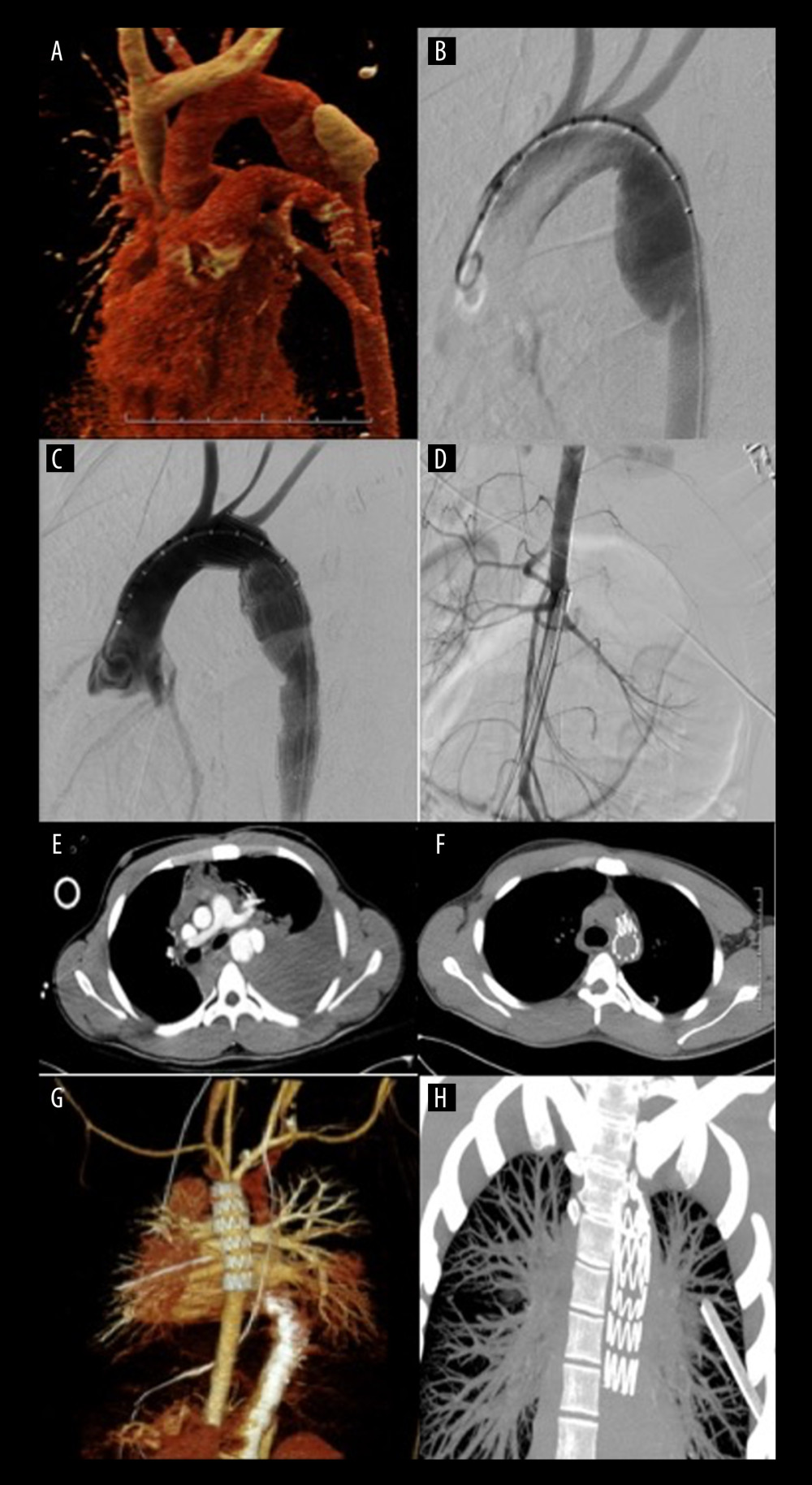 Figure 2. Tension hemothorax after thoracic aortic transection(A) Computed tomography (CT) angiogram volume rendering technique (VRT) reconstruction with contrast agent leakage. (B) Digital subtraction angiography showing dissection in loco typico. (C) ZDEG (Cook) stent graft implantation. (D) Abdominal aorta hypovolemia. (E) CT showing severe hemothorax and aortic injury. (F) CT follow-up after stent graft and hemothorax drainage. (G) CT angiogram follow-up 3D VRT reconstruction after stent graft placement. (H) CT follow-up maximum intensity projection after hemothorax drainage.
Figure 2. Tension hemothorax after thoracic aortic transection(A) Computed tomography (CT) angiogram volume rendering technique (VRT) reconstruction with contrast agent leakage. (B) Digital subtraction angiography showing dissection in loco typico. (C) ZDEG (Cook) stent graft implantation. (D) Abdominal aorta hypovolemia. (E) CT showing severe hemothorax and aortic injury. (F) CT follow-up after stent graft and hemothorax drainage. (G) CT angiogram follow-up 3D VRT reconstruction after stent graft placement. (H) CT follow-up maximum intensity projection after hemothorax drainage. References
1. Hiller RJ, Mikocka-Walus AA, Cameron PA, Aortic transection: Demographics, treatment, and outcomes in Victoria, Australia: Emerg Med J, 2010; 27(5); 368-71
2. Steuer J, Björck M, Sonesson B, Editor’s Choice – Durability of endovascular repair in blunt traumatic thoracic aortic injury: Long-term outcome from four tertiary referral centers: Eur J Vasc Endovasc Surg, 2015; 50(4); 460-65
3. Fabian TC, Richardson JD, Croce MA, Prospective study of blunt aortic injury: J Trauma Inj Infect Crit Care, 1997; 42(3); 374-83
4. Jamieson WRE, Janusz MT, Gudas VM, Traumatic rupture of the thoracic aorta: Third decade of experience: Am J Surg, 2002; 183(5); 571-75
5. Jahromi AS, Kazemi K, Safar HA, Traumatic rupture of the thoracic aorta: Cohort study and systematic review: J Vasc Surg, 2001; 34(6); 1029-34
6. Cardarelli MG, McLaughlin JS, Downing SW, Management of traumatic aortic rupture: A 30-year experience: Ann Surg, 2002; 236(4); 465-70
7. Cowley RA, Turney SZ, Hankins JR, Rupture of thoracic aorta caused by blunt trauma. A fifteen-year experience: J Thorac Cardiovasc Surg, 1990; 100(5); 652-60 discussion 660–61
8. Lee WA, Matsumura JS, Mitchell RS, Endovascular repair of traumatic thoracic aortic injury: Clinical practice guidelines of the Society for Vascular Surgery: J Vasc Surg, 2011; 53(1); 187-92
9. Xenos ES, Abedi NN, Davenport DL, Meta-analysis of endovascular vs open repair for traumatic descending thoracic aortic rupture: J Vasc Surg, 2008; 48(5); 1343-51
10. Czerny M, Schmidli J, Adler S, Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: An expert consensus document of the European Association for Cardio-Thoracic Surgery (EACTS) and the European Society for Vascular Surgery (ESVS): Eur J Cardiothorac Surg, 2019; 55; 133-62
11. Attar S, Cardarelli MG, Downing SW, Traumatic aortic rupture: Recent outcome with regard to neurologic deficit: Ann Thorac Surg, 1999; 67(4); 959-64
12. Von Oppell UO, Dunne TT, De Groot MK, Zilla P, Traumatic aortic rupture: Twenty-year metaanalysis of mortality and risk of paraplegia: Ann Thorac Surg, 1994; 58(2); 585-93
13. Razzouk AJ, Repair of traumatic aortic rupture: Arch Surg, 2000; 135(8); 913
14. Gammie JS, Shah AS, Hattler BG, Traumatic aortic rupture: Diagnosis and management: Ann Thorac Surg, 1998; 66(4); 1295-300
15. Alsac J-M, Boura B, Desgranges P, Immediate endovascular repair for acute traumatic injuries of the thoracic aorta: A multicenter analysis of 28 cases: J Vasc Surg, 2008; 48(6); 1369-74
16. Hoornweg LL, Dinkelman MK, Goslings JC, Endovascular management of traumatic ruptures of the thoracic aorta: A retrospective multicenter analysis of 28 cases in The Netherlands: J Vasc Surg, 2006; 43(6); 1096-102
17. Bent CL, Matson MB, Sobeh M, Endovascular management of acute blunt traumatic thoracic aortic injury: A single center experience: J Vasc Surg, 2007; 46(5); 920-27
18. Mosquera VX, Marini M, Lopez-Perez JM, Role of conservative management in traumatic aortic injury: Comparison of long-term results of conservative, surgical, and endovascular treatment: J Thorac Cardiovasc Surg, 2011; 142(3); 614-21
19. Marcheix B, Dambrin C, Bolduc J-P, Endovascular repair of traumatic rupture of the aortic isthmus: Midterm results: J Thorac Cardiovasc Surg, 2006; 132(5); 1037-41
20. Muhs BE, Balm R, White GH, Verhagen HJM, Anatomic factors associated with acute endograft collapse after Gore TAG treatment of thoracic aortic dissection or traumatic rupture: J Vasc Surg, 2007; 45(4); 655-61
21. Wallace GA, Starnes BW, Hatsukami TS, Intravascular ultrasound is a critical tool for accurate endograft sizing in the management of blunt thoracic aortic injury: J Vasc Surg, 2015; 61(3); 630-35
22. Azizzadeh A, Ray HM, Dubose JJ, Outcomes of endovascular repair for patients with blunt traumatic aortic injury: J Trauma Acute Care Surg, 2014; 76(2); 510-16
23. McBride CL, Dubose JJ, Miller CC, Intentional left subclavian artery coverage during thoracic endovascular aortic repair for traumatic aortic injury: J Vasc Surg, 2015; 61(1); 73-79.e1
24. Neschis DG, Moainie S, Flinn WR, Endograft repair of traumatic aortic injury – a technique in evolution: Ann Surg, 2009; 250(3); 377-82
25. Orend KH, Pamler R, Kapfer X, Endovascular repair of traumatic descending aortic transection: J Endovasc Ther, 2002; 9(5); 573-78
26. Dake MD, Miller DC, Mitchell RS, The “first generation” of endovascular stent-grafts for patients with aneurysms of the descending thoracic aorta: J Thorac Cardiovasc Surg, 1998; 116(5); 689-704
27. Melnitchouk S, Pfammater T, Kadner A, Emergency stent-graft placement for hemorrhage control in acute thoracic aortic rupture: Eur J Cardio-Thoracic Surg, 2004; 25(6); 1032-38
28. Zipfel B, Chiesa R, Kahlberg A, Endovascular repair of traumatic thoracic aortic injury: Final results from the relay endovascular registry for thoracic disease: Ann Thorac Surg, 2014; 97(3); 774-80
29. Botta L, Russo V, Savini C, Endovascular treatment for acute traumatic transection of the descending aorta: Focus on operative timing and left subclavian artery management: J Thorac Cardiovasc Surg, 2008; 136(6); 1558-63
Figures
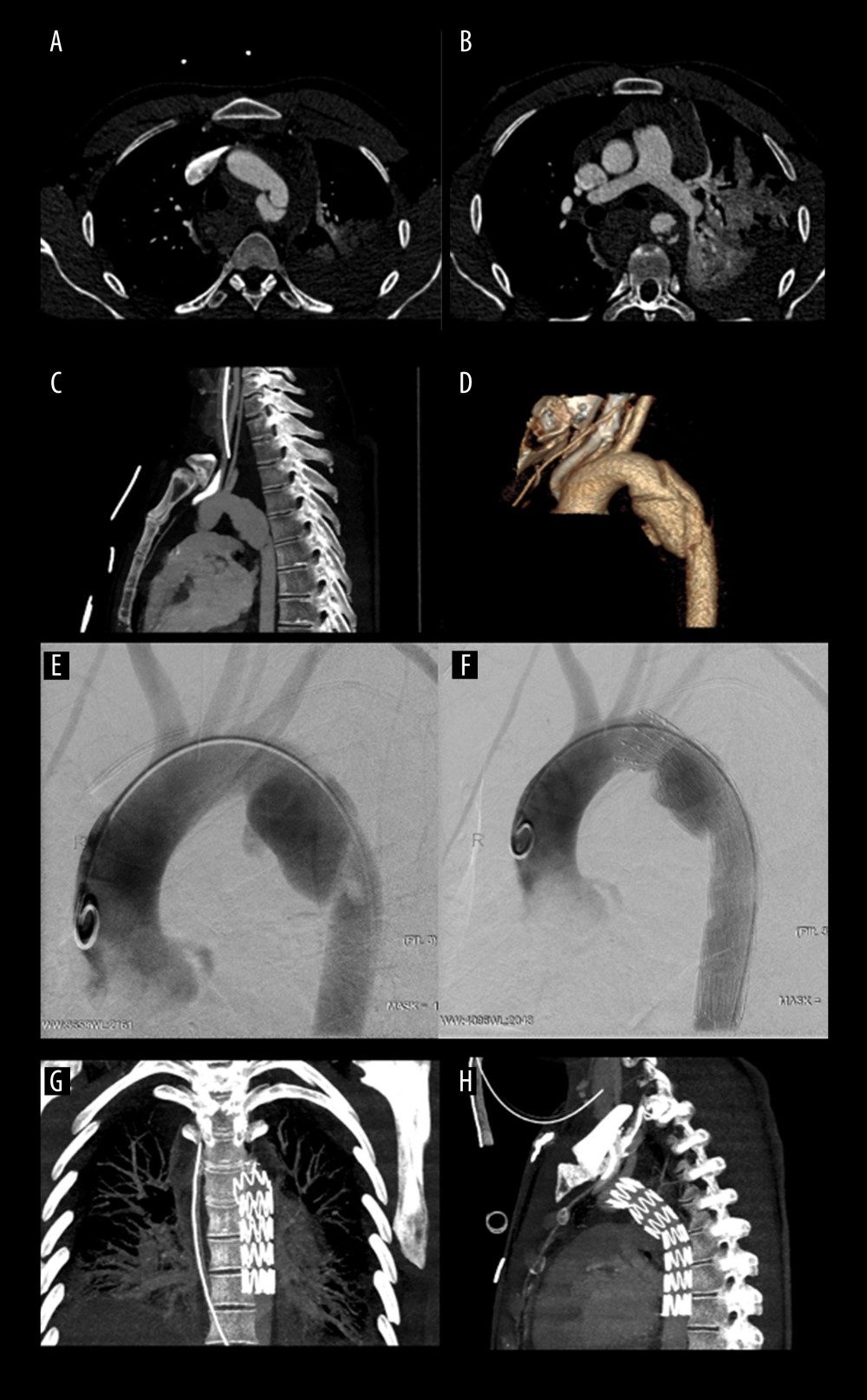 Figure 1. Thoracic aortic injury with active bleeding(A) Computed tomography (CT) angiogram of the axial maximum intensity projection (MIP) reconstruction with aortic trauma in loco typico. (B) CT showing left hemothorax, pulmonary trauma, and active bleeding. (C) CT MIP sagittal projection with aortic grade IV trauma. (D) CT volume rendering technique reconstruction of the aortic wall trauma grade IV. (E) Digital subtraction angiography with active contrast agent leakage. (F) ZDEG (Cook) stent graft implantation before the origin of the left vertebral artery with left subclavian artery coverage. (G) CT follow-up in coronal projection. (H) CT follow-up in sagittal projection.
Figure 1. Thoracic aortic injury with active bleeding(A) Computed tomography (CT) angiogram of the axial maximum intensity projection (MIP) reconstruction with aortic trauma in loco typico. (B) CT showing left hemothorax, pulmonary trauma, and active bleeding. (C) CT MIP sagittal projection with aortic grade IV trauma. (D) CT volume rendering technique reconstruction of the aortic wall trauma grade IV. (E) Digital subtraction angiography with active contrast agent leakage. (F) ZDEG (Cook) stent graft implantation before the origin of the left vertebral artery with left subclavian artery coverage. (G) CT follow-up in coronal projection. (H) CT follow-up in sagittal projection.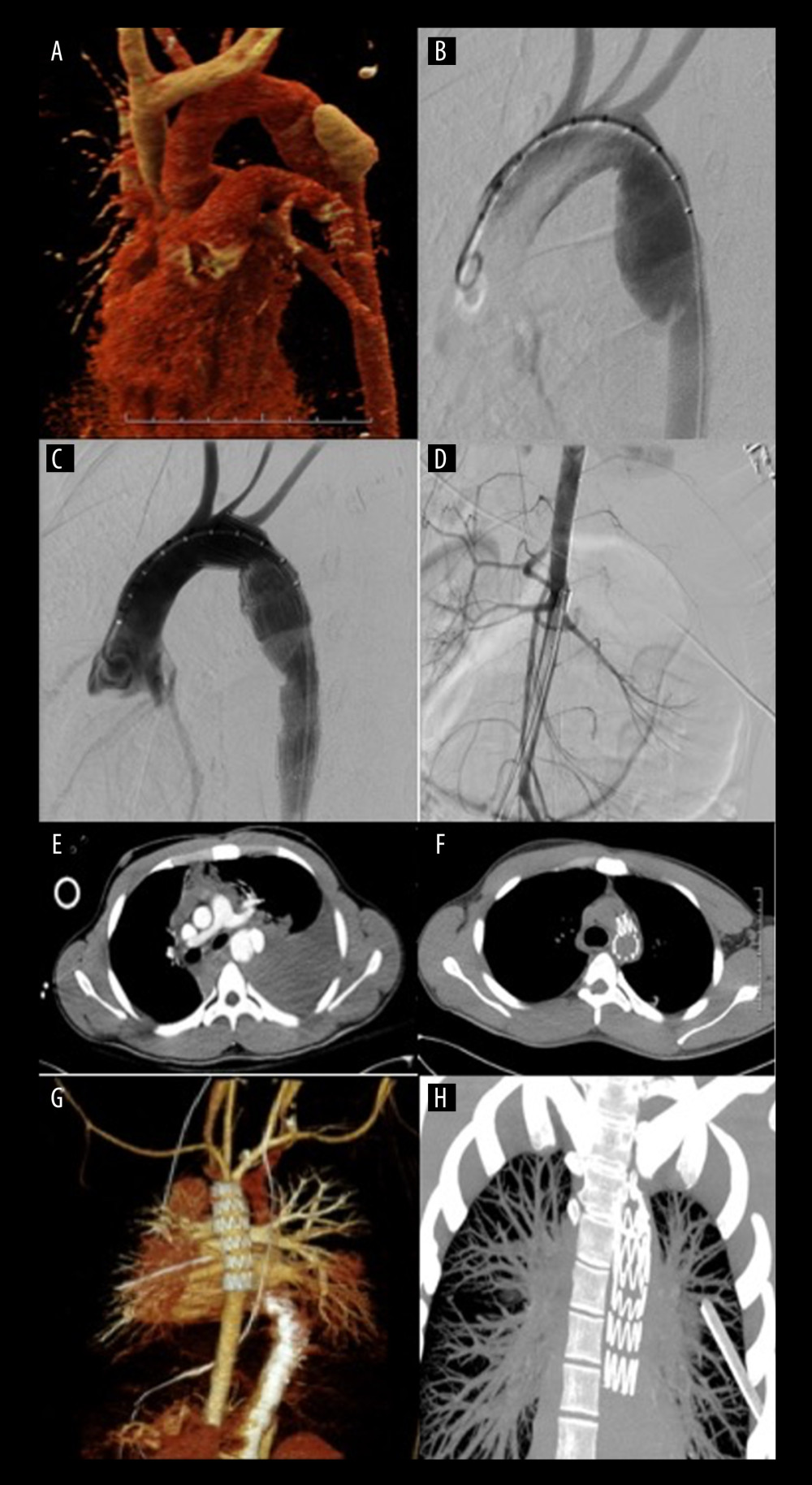 Figure 2. Tension hemothorax after thoracic aortic transection(A) Computed tomography (CT) angiogram volume rendering technique (VRT) reconstruction with contrast agent leakage. (B) Digital subtraction angiography showing dissection in loco typico. (C) ZDEG (Cook) stent graft implantation. (D) Abdominal aorta hypovolemia. (E) CT showing severe hemothorax and aortic injury. (F) CT follow-up after stent graft and hemothorax drainage. (G) CT angiogram follow-up 3D VRT reconstruction after stent graft placement. (H) CT follow-up maximum intensity projection after hemothorax drainage.
Figure 2. Tension hemothorax after thoracic aortic transection(A) Computed tomography (CT) angiogram volume rendering technique (VRT) reconstruction with contrast agent leakage. (B) Digital subtraction angiography showing dissection in loco typico. (C) ZDEG (Cook) stent graft implantation. (D) Abdominal aorta hypovolemia. (E) CT showing severe hemothorax and aortic injury. (F) CT follow-up after stent graft and hemothorax drainage. (G) CT angiogram follow-up 3D VRT reconstruction after stent graft placement. (H) CT follow-up maximum intensity projection after hemothorax drainage. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952