15 March 2022: Clinical Research
Development of a Predictive Nomogram for Estimating Medication Nonadherence in Hemodialysis Patients
Ying Wang1BCDE, Yinhui Yao1BCF, Junhui Hu1BC, Yingxue Lin1BF, Chunhua Cai2B, Yanwu Zhao1AG*DOI: 10.12659/MSM.934482
Med Sci Monit 2022; 28:e934482
Abstract
BACKGROUND: Medication compliance in hemodialysis patients affects the therapeutic effect of treatment and patient survival. Therefore, we aimed to explore the influencing factors of medication adherence in hemodialysis patients and develop a nomogram model to predict medication adherence.
MATERIAL AND METHODS: Data from questionnaires on medication adherence in hemodialysis patients were collected in Chengde from May 2020 to December 2020. The least absolute selection operator (LASSO) regression model and multivariable logistic regression analysis were used to analyze the risk factors for medication adherence in hemodialysis patients, and then a nomogram model was established. The bootstrap method was applied for internal validation. The concordance index (C-index), area under the receiver operating characteristic (ROC) curve (AUC), decision curve analysis (DCA), calibration curve, net reclassification improvement (NRI) index, and integrated discrimination improvement (IDI) index were used to evaluate the degree of differentiation and accuracy of the nomogram model, and clinical impact was used to investigate the potential clinical value of the nomogram model.
RESULTS: In total, 206 patients were included in this study, with a rate of medication nonadherence of 41.75%. Eight predictors were identified to build the nomogram model. The C-index, AUC, DCA, calibration curve, NRI, and IDI showed that the model had good discrimination and accuracy. The clinical impact plot showed that the nomogram of medication adherence in hemodialysis patients had clinical application value.
CONCLUSIONS: We developed and validated a nomogram model that is intuitive to apply for predicting medication adherence in hemodialysis patients.
Keywords: nomograms, Predictive Value of Tests, Renal Dialysis, Treatment Adherence and Compliance, Decision Support Techniques, Female, Follow-Up Studies, Humans, Kidney Failure, Chronic, Male, medication adherence, SEER Program
Background
End-stage renal disease is one of the major causes of mortality worldwide, with approximately 1 million people dying of this disease every year, and the prevalence rate is increasing by 7% annually [1]. Hemodialysis is the main method of renal replacement therapy in end-stage renal disease patients, and a large amount of oral medicine is required, which leads to treatment complexity, poor medication adherence, and the occurrence of adverse drug events [2]. Hemodialysis patients not only need daily dialysis but also face a certain economic burden associated with drug costs. Commonly used drugs and supplements in hemodialysis patients include folic acid, calcium, vitamin D, antihypertensive drugs, antidiabetic drugs, erythropoietic agents, iron supplements, and other drugs [1,3].
Drug compliance refers to how consistent patients are with adhering to medication and medical advice, while from the perspective of drug therapy, drug compliance refers to the degree to which patients follow drug therapy plans [4]. Patients may be noncompliant at different stages of disease treatment [5]. Poor medication adherence can be intentional or unintentional, and factors that lead to poor drug adherence are likely to cause complications, directly leading to poor prognosis and avoidable medical and health care costs [6,7].
Studies show that approximately 50% of chronic disease patients do not adhere to their medication regimens [8]. This figure includes chronic hemodialysis patients [1]. Recent studies of medication compliance in hemodialysis patients have mainly assessed the relationship between patients’ preferences, such as dietary intake, and chelating agents [9,10]. Our study analyzed clinical data related to hemodialysis patients, discussed the factors influencing patient medication compliance, and established a nomogram model to predict poor medication compliance in patients undergoing hemodialysis; this nomogram provides a simple and effective tool for identifying high-risk hemodialysis patients with poor medication compliance. The findings may provide evidence for more targeted intervention methods and further improve the therapeutic effect of drugs in hemodialysis patients.
Material and Methods
PATIENTS:
This research was approved by the Medical Ethics Committee of Chengde Medical University Affiliated Hospital (ethics number: LL2020013). This study was conducted at the Chengde Medical University Affiliated Hospital, Shuangluan Hospital, and Yingshouyingzi Hospital from May 2020 to December 2020. The inclusion criteria were as follows: (1) patients who were older than 18 years old and (2) patients who underwent hemodialysis 3 times a week for 4 h each time and who were on maintenance hemodialysis for more than 3 months. Patients who were illiterate, had severe cognitive impairment, or had severe physical limitations were excluded. The collected characteristics of the hemodialysis patients included sex, age, disease duration, smoking history, alcohol consumption history, marital status, occupation, income, type of medical insurance, residential region, history of disease, complications, types of drugs used, insulin use, number of oral drugs used and use of traditional Chinese medicine (TCM), and cause of renal disease.
ADHERENCE ASSESSMENT:
Medication adherence in hemodialysis patients was assessed by using the Morisky Medication Adherence Questionnaire-8 (MMAS-8) [11]. Patients were asked to answer 8 questions from the MMAS-8, which were used to calculate an adherence score. In our study, an adherence score greater than or equal to 6 was defined as adherence, whereas a score less than 6 was defined as nonadherence.
PSYCHOLOGICAL DATA:
In all the participants, psychological data were acquired with the Hospital Anxiety and Depression Scale (HADS), which consists of 14 items to assess anxiety and depression. The HADS scores ranged from 0 to 21. Scores greater than 8 indicated that the patient had anxiety/depression [12,13].
AGE-ADJUSTED CHARLSON COMORBIDITY INDEX (ACCI):
The age-adjusted Charlson Comorbidity Index (ACCI) creates a single indicator that takes into account both age and comorbidity. The ACCI was used to measure the health status of all the patients included in this study [14].
STATISTICAL ANALYSIS:
Least absolute selection operator (LASSO) analysis was used to screen potential risk factors for nonadherence in patients on hemodialysis. Then, combined with the potential risk factors for nonadherence identified by LASSO regression analysis, logistic multivariate regression analysis was conducted to further screen relevant factors for the establishment of a model. However, taking into account factors related to medication adherence, some potential risk factors were included to develop a prediction model in this study [15,16].
After all potential predictors were included in the risk prediction model for poor medication adherence, the corresponding nomogram was displayed. To evaluate the differentiation ability of the nomogram, we used the concordance index (C-index) and the area under the receiver operating characteristic curve (AUC) [17]. Calibration plots were used to evaluate calibration ability. The net reclassification improvement (NRI) and integrated discrimination improvement (IDI) indexes were calculated to assess the risk prediction model. Decision curve analysis (DCA) and clinical influence curve analysis were used to demonstrate the potential clinical value of the nomogram [18].
All the data in this study were analyzed using R software (version 4.0.3).
Results
CHARACTERISTICS OF THE HEMODIALYSIS PATIENTS:
A total of 206 patients (100 males and 106 females) with an average age of 58.50 (48.25, 66.75) years, who met the inclusion criteria and completed the questionnaire from May 2020 to December 2020 were included. According to the MMAS-8 score, the patients were divided into 2 groups: the medication adherence (120 patients) and medication nonadherence (86 patients) groups. The ACCI scores for the whole cohort ranged from 2 to 9, with a median of 4.46. The median disease duration for all the patients was 3.50 (1.50, 6.50) years. The demographic characteristics, comorbidities, ACCI scores, and drug treatment characteristics of the 2 groups are detailed in Table 1.
NOMOGRAM VARIABLE SCREENING AND CONSTRUCTION:
In terms of the demographics, medication compliance, therapeutic drug characteristics, and patient psychological characteristics, the 206 patients had a total of 23 characteristics, which were reduced to 8 potential nonzero coefficient predictors associated with medication nonadherence in the LASSO regression analysis (Figure 1A, 1B). These potential risk factors included education, residential region, job, hospital level, depression, TCM use, income, and ACCI score. The results of multivariate logistic regression analysis of the above characteristics are shown in Figure 1C. These 8 factors were incorporated into the model to construct a nomogram for predicting medication nonadherence in hemodialysis patients (Figure 1D).
CALIBRATION OF THE NOMOGRAM:
The C-index and AUC were 0.83, indicating favorable discrimination by the medication nonadherence risk nomogram (Figure 2A). The calibration curve also showed good nomogram agreement in this study (Figure 2B). The changes in the NRI and IDI indexes were used to compare the accuracy between the nomogram and a model including hospital level and education. The NRI and IDI indexes were 0.041 and 0.033, respectively (all P<0.01). In addition, the AUC of the nomogram was higher than that of the model (0.83 vs 0.78, P<0.05). These indicators demonstrate that the nomogram showed greater accuracy than the model.
CLINICAL USE OF THE NOMOGRAM:
The DCA of the nomogram for medication nonadherence in hemodialysis patients is shown in Figure 2C. The DCA showed that the implementation of the nomogram for medication nonadherence in this study population would be more beneficial than implementing an all-patient intervention or no intervention regimen with threshold probabilities of 0.07–0.95. Furthermore, a clinical impact plot showed that the number of predicted high-risk patients was always greater than the number of patients who were actually nonadherent, which appeared to be accompanied by an acceptable cost-benefit ratio (Figure 2D). These results suggest that the nomogram has a high potential for clinical application to predict medication nonadherence in hemodialysis patients.
Discussion
The rate of nonadherence has not improved for decades, a phenomenon that has prompted the World Health Organization (WHO) to call nonadherence a “hidden epidemic” [1]. Existing studies retrospectively investigating the influencing factors of medication nonadherence in hemodialysis patients through drug therapy, dialysis nursing, diet and other aspects are limited [19–22], and no effective prediction model has been established and verified. Therefore, combined with the questionnaire results and clinical data related to medication compliance of hemodialysis patients in our hospital, this study analyzed the influencing factors of medication noncompliance in dialysis patients and used 8 readily available variables to build a nomogram model. The nomogram model combines risk factors related to demographics, disease characteristics, and medication characteristics to help individualize the prediction of medication compliance in hemodialysis patients.
Nomograms have been widely used in the field of prognosis and diagnosis, especially in oncology [23–25] and have also been successfully applied in the field of medication nonadherence prediction [26]. Our study is the first to apply a nomogram to predict medication adherence in hemodialysis patients. The results of our study showed that 41.75% of hemodialysis patients exhibited medication nonadherence. In the analysis of risk factors for medication nonadherence, education level, region, income, occupation, hospital level, depression, ACCI score, and TCM use were closely related to medication compliance in hemodialysis patients. The nomogram uses these 8 risk factors as key individual factors for determining the risk of nonadherence in hemodialysis patients. The calibration curve for the nomogram showed good identification and calibration capabilities. Both the C-index and AUC were 0.83, which confirmed that the nomogram model could effectively predict medication nonadherence of hemodialysis patients. Clinical decision curves and clinical impact curves were incorporated to investigate the advantages of the nomogram results. The results further confirmed the clinical usability and high benefit of the nomogram model.
As in previous studies [27,28], education level was found to be one of the factors affecting medication nonadherence in hemodialysis patients. Hemodialysis patients with low education levels tend to have a higher risk of medication nonadherence, which means that such patients are more likely to not take drugs as prescribed by doctors or even stop taking their medication. The hospital level of hemodialysis patients was an important factor affecting medication nonadherence. At present, compared with hospital level II in China, hospital level III has well-equipped hemodialysis facilities and higher-quality medical personnel, which can provide better medical services to patients and reduce the risk of medication nonadherence. Patients with depression have a higher risk of medication nonadherence. Patients with possible depression are less concerned about drug-related problems [29–31]. In our study, low income was one of the risk factors for medication nonadherence among hemodialysis patients. This finding shows that patients will consider their personal economic level when taking medication. Similarly, related to the abovementioned factors of economic income level, rural patients have a higher risk of medication nonadherence than urban residents. In terms of drug use, we considered the use of TCM, and studies have shown that patients who use TCM have a lower risk of noncompliance than those who do not use TCM. In the investigation, we found that the TCM used by clinicians was mainly for the regulation of patients’ creatinine level (such as the drug cordycepin). In terms of occupation, the adherence of retired elderly individuals was worse that of individuals with other occupations, which may be related to the memory of elderly individuals; therefore, it is necessary for pharmacists to patiently guide the elderly population in regard to medication use.
The ACCI quantifies comorbidities based on patients’ age, number of comorbidities, and severity of disease. In clinical practice, the ACCI is mainly used to evaluate the treatment plan and treatment results affected by organ function impairment, such as the prediction of the occurrence of perioperative complications and the prediction value of long-term prognosis for patients with various malignant tumors [32,33]. In our study, a nomogram was established for the first time by combining the ACCI scores of patients in the adherence and nonadherence groups. The results showed that the risk of nonadherence was the lowest when the score was 4, and the risk was the highest when the score was 8.
Good medication adherence contributes to the treatment of disease, improves the quality of life of patients, and reduces the economic burden on patients and society, and patients with good medication compliance often achieve better treatment results [34,35]; therefore, the development of prediction tools to help determine a patient’s individual risk for treatment noncompliance can improve the prognosis of patients [26]. We established a nomogram to help clinicians and pharmacists identify dialysis patients at high risk of noncompliance early. At the same time, the predictive tool can also be used in clinical trials to guide researchers to exclude patients with poor medication compliance and to screen out patients with good medication compliance. In addition, this nomogram could be useful for early interventions for patients at high risk of noncompliance; these interventions could include encouraging the use of automatic reminders, monitoring drug compliance, and strengthening the model of home medication services. These methods can improve drug noncompliance and the effectiveness of treatment. It is even helpful to combine drug management interventions with occupational therapy, which can improve patients’ self-perception and generate new drug management behaviors [36].
This study has some limitations. First, the sample size was relatively small. The generalizability of the results of this study is not clear, and a study needs to be done in a wider population for external validation. Second, the analysis of the potential risk factors did not include all the factors associated with medication nonadherence.
Conclusions
A nomogram model was developed to estimate medication nonadherence in hemodialysis patients. This nomogram can help health care workers identify hemodialysis patients at high risk for noncompliance at the beginning of clinical treatment and thus allow health care workers to make an individual risk assessment of patients’ medication compliance. This model can also be a convenient tool for encouraging doctor- or pharmacist-initiated interventions for patients to obtain the best effect of drug treatment. However, further external validation is needed to determine the individual prediction effect of the nomogram model and the intervention treatment effect.
Figures
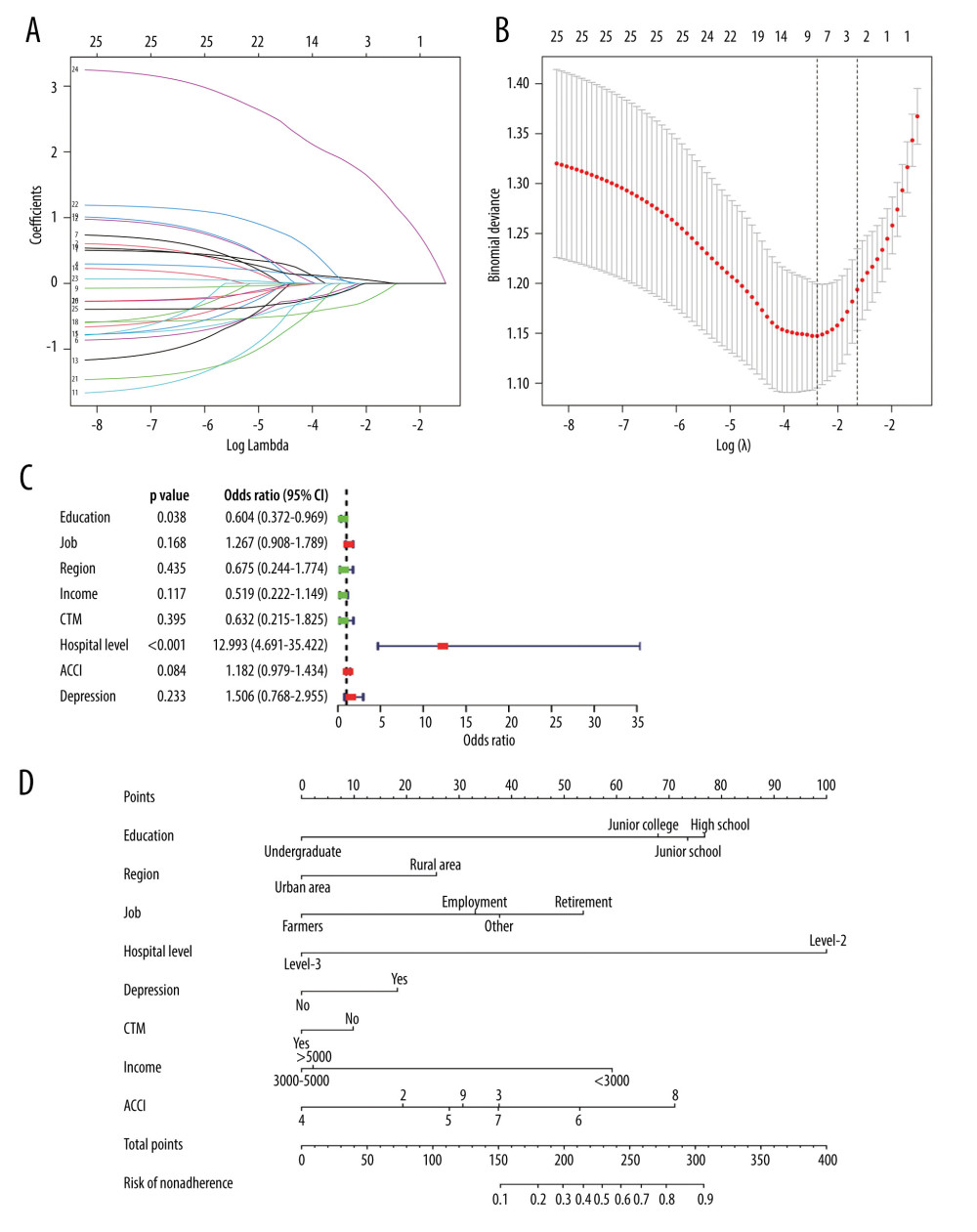 Figure 1. Prediction factors for medication nonadherence were selected, and a medication nonadherence nomogram was developed in hemodialysis patients. (A, B) Least absolute shrinkage and selection operator (LASSO) coefficient profiles of the 8 prediction factors. (C) Logistic regression analyses of the 8 prediction factors in hemodialysis patients. (D) Nomogram prediction of medication nonadherence in hemodialysis patients. (R software, version 4.0.3)
Figure 1. Prediction factors for medication nonadherence were selected, and a medication nonadherence nomogram was developed in hemodialysis patients. (A, B) Least absolute shrinkage and selection operator (LASSO) coefficient profiles of the 8 prediction factors. (C) Logistic regression analyses of the 8 prediction factors in hemodialysis patients. (D) Nomogram prediction of medication nonadherence in hemodialysis patients. (R software, version 4.0.3) 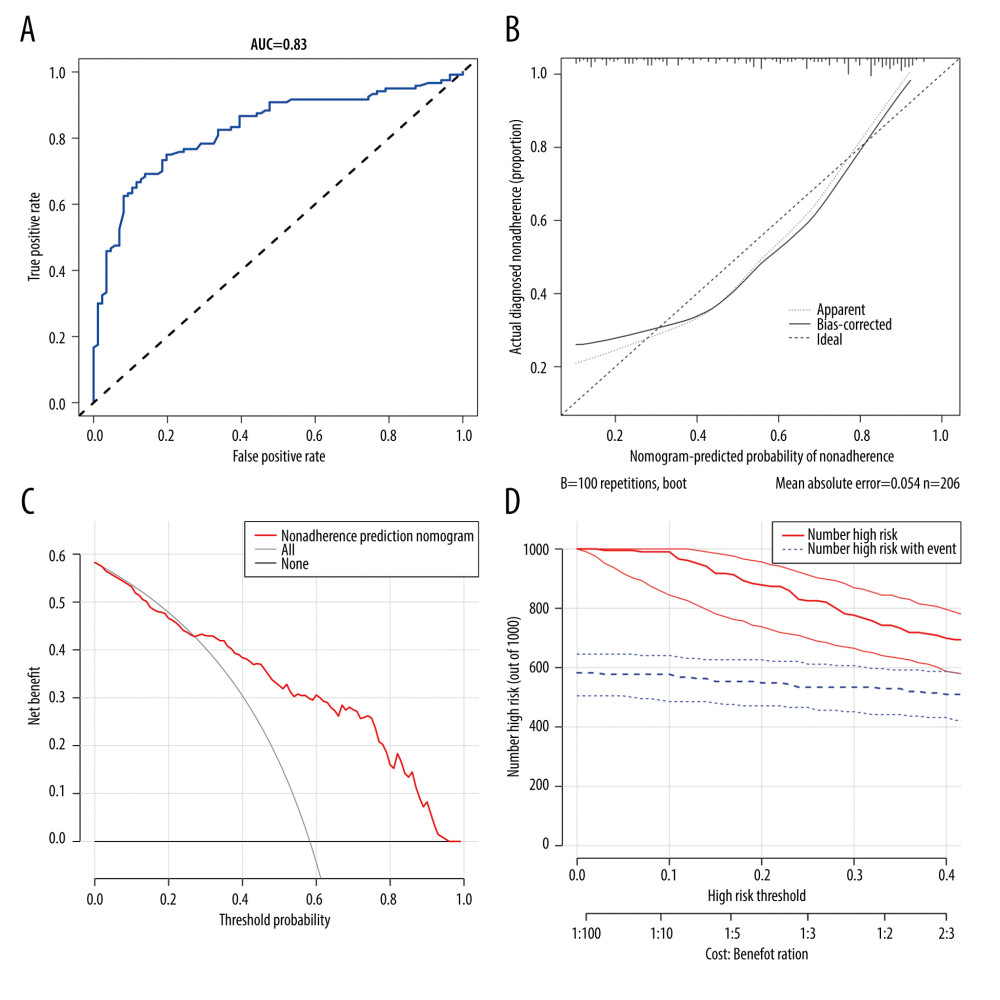 Figure 2. Medication nonadherence of nomogram evaluation and clinical use in hemodialysis patients. (A) ROC curve based on the predictive nomogram for medication nonadherence in hemodialysis patients. (B) Calibration plots for predicting patient medication nonadherence. (C) Decision curve analysis for the nonadherence nomogram in hemodialysis patients. (D) Clinical impact plot for predicting patient medication nonadherence. (R software, version 4.0.3)
Figure 2. Medication nonadherence of nomogram evaluation and clinical use in hemodialysis patients. (A) ROC curve based on the predictive nomogram for medication nonadherence in hemodialysis patients. (B) Calibration plots for predicting patient medication nonadherence. (C) Decision curve analysis for the nonadherence nomogram in hemodialysis patients. (D) Clinical impact plot for predicting patient medication nonadherence. (R software, version 4.0.3) References
1. Ghimire S, Castelino RL, Lioufas NM, Nonadherence to medication therapy in haemodialysis patients: A systematic review: PLoS One, 2015; 10(12); e0144119
2. Mason NA, Polypharmacy and medication-related complications in the chronic kidney disease patient: Curr Opin Nephrol Hypertens, 2011; 20(5); 492-97
3. Ohya M, Iwashita Y, Kunimoto S, An analysis of medication adherence and patient preference in long-term stable maintenance hemodialysis patients in Japan: Intern Med, 2019; 58(18); 2595-603
4. Hugtenburg JG, Timmers L, Elders PJ, Definitions, variants, and causes of nonadherence with medication: A challenge for tailored interventions: Patient Prefer Adherence, 2013; 7; 675-82
5. Vrijens B, De Geest S, Hughes DA, A new taxonomy for describing and defining adherence to medications: Br J Clin Pharmacol, 2012; 73(5); 691-705
6. Chao CT, Huang JW, Geriatric syndromes are potential determinants of the medication adherence status in prevalent dialysis patients: PeerJ, 2016; 4; e2122
7. Saunders J, Ahmadzadeh S, Bush M, Improving patient experience and treatment adherence in the adult, outpatient hemodialysis population: J Nurs Care Qual, 2019; 34(4); 330-36
8. Neri L, Martini A, Andreucci VE, Regimen complexity and prescription adherence in dialysis patients: Am J Nephrol, 2011; 34(1); 71-76
9. Wileman V, Farrington K, Wellsted D, Medication beliefs are associated with phosphate binder non-adherence in hyperphosphatemic haemodialysis patients: Br J Health Psychol, 2015; 20(3); 563-78
10. Tao X, Zhang H, Yang Y, Daily dietary phosphorus intake variability and hemodialysis patient adherence to phosphate binder therapy: Hemodial Int, 2019; 23(4); 458-65
11. Morisky DE, Ang A, Krousel-Wood M, Ward HJ, Predictive validity of a medication adherence measure in an outpatient setting: J Clin Hypertens (Greenwich), 2008; 10(5); 348-54
12. Brennan C, Worrall-Davies A, McMillan D, The Hospital Anxiety and Depression Scale: A diagnostic meta-analysis of case-finding ability: J Psychosom Res, 2010; 69(4); 371-78
13. Zigmond AS, Snaith RP, The hospital anxiety and depression scale: Acta Psychiatr Scand, 1983; 67(6); 361-70
14. Charlson M, Szatrowski TP, Peterson J, Gold J, Validation of a combined comorbidity index: J Clin Epidemiol, 1994; 47(11); 1245-51
15. Sauerbrei W, Royston P, Binder H, Selection of important variables and determination of functional form for continuous predictors in multivariable model building: Stat Med, 2007; 26(30); 5512-28
16. Kidd AC, McGettrick M, Tsim S, Survival prediction in mesothelioma using a scalable Lasso regression model: Instructions for use and initial performance using clinical predictors: BMJ Open Respir Res, 2018; 5(1); e000240
17. Pencina MJ, D’Agostino RB, Overall C as a measure of discrimination in survival analysis: Model specific population value and confidence interval estimation: Stat Med, 2004; 23(13); 2109-23
18. Vickers AJ, Cronin AM, Elkin EB, Gonen M, Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers: BMC Med Inform Decis Mak, 2008; 8; 53
19. Gilad L, Haviv YS, Cohen-Glickman I, Chronic drug treatment among hemodialysis patients: A qualitative study of patients, nursing and medical staff attitudes and approaches: BMC Nephrol, 2020; 21(1); 239
20. Suzuki H, Uchida S, Kashiwagura Y, Impact of community pharmacist-led intensive education on the control of serum phosphate levels in haemodialysis patients: Int J Clin Pharm, 2021; 43(1); 220-28
21. Al-Abdelmuhsin L, Al-Ammari M, Babelghaith SD, Pharmacist-led medication counseling for patients undergoing hemodialysis: A path to better adherence: Int J Environ Res Public Health, 2020; 17(7); 2399
22. Pretto CR, Winkelmann ER, Hildebrandt LM, Quality of life of chronic kidney patients on hemodialysis and related factors: Rev Lat Am Enfermagem, 2020; 28; e3327
23. Zhang Q, Ning G, Jiang H, 15-lncRNA-based classifier-clinicopathologic nomogram improves the prediction of recurrence in patients with hepatocellular carcinoma: Dis Markers, 2020; 2020; 9180732
24. Badakhshi H, Wang ZM, Li RJ, Ismail M, Kaul D, Survival and prognostic nomogram for primary gastrointestinal melanoma (PGIM): A population-based study: Anticancer Res, 2021; 41(2); 967-74
25. Balasubramanian D, Subramaniam N, Missale F: Head Neck, 2021; 43(4); 1043-55
26. Wang H, Zhang L, Liu Z, Predicting medication nonadherence risk in a Chinese inflammatory rheumatic disease population: Development and assessment of a new predictive nomogram: Patient Prefer Adherence, 2018; 12; 1757-65
27. Alkatheri AM, Alyousif SM, Alshabanah N, Medication adherence among adult patients on hemodialysis: Saudi J Kidney Dis Transpl, 2014; 25(4); 762-68
28. Tayebi A, Einollahi B, Rahimi A, Sirati-Nir M, Non-adherence to treatment among Iranian dialysis patients, a systematic review: Iran J Kidney Dis, 2019; 13(6); 347-61
29. Rosenthal Asher D, Ver Halen N, Cukor D, Depression and nonadherence predict mortality in hemodialysis treated end-stage renal disease patients: Hemodial Int, 2012; 16(3); 387-93
30. Theofilou P, Medication adherence in Greek hemodialysis patients: The contribution of depression and health cognitions: Int J Behav Med, 2013; 20(2); 311-18
31. Ossareh S, Tabrizian S, Zebarjadi M, Joodat RS, Prevalence of depression in maintenance hemodialysis patients and its correlation with adherence to medications: Iran J Kidney Dis, 2014; 8(6); 467-74
32. Kahl A, du Bois A, Harter P, Prognostic value of the age-adjusted Charlson comorbidity index (ACCI) on short- and long-term outcome in patients with advanced primary epithelial ovarian Cancer: Ann Surg Oncol, 2017; 24(12); 3692-99
33. Jian Xian L, Ying Qi H, Jian Wei X, Age-adjusted Charlson Comorbidity Index (ACCI) is a significant factor for predicting survival after radical gastrectomy in patients with gastric cancer: BMC Surg, 2019; 19; 53
34. van Heuckelum M, van den Ende CHM, The effect of electronic monitoring feedback on medication adherence and clinical outcomes: A systematic review: PLoS One, 2017; 12(10); e0185453
35. Nieuwlaat R, Wilczynski N, Navarro T, Interventions for enhancing medication adherence: Cochrane Database Syst Rev, 2014; 2014(11); CD000011
36. Schwartz JK, Grogan KA, Mutch MJ, Intervention to improve medication management: qualitative outcomes from a phase I randomized controlled trial: Am J Occup Ther, 2017; 71(6); 7106240010p-17106240010p10
Figures
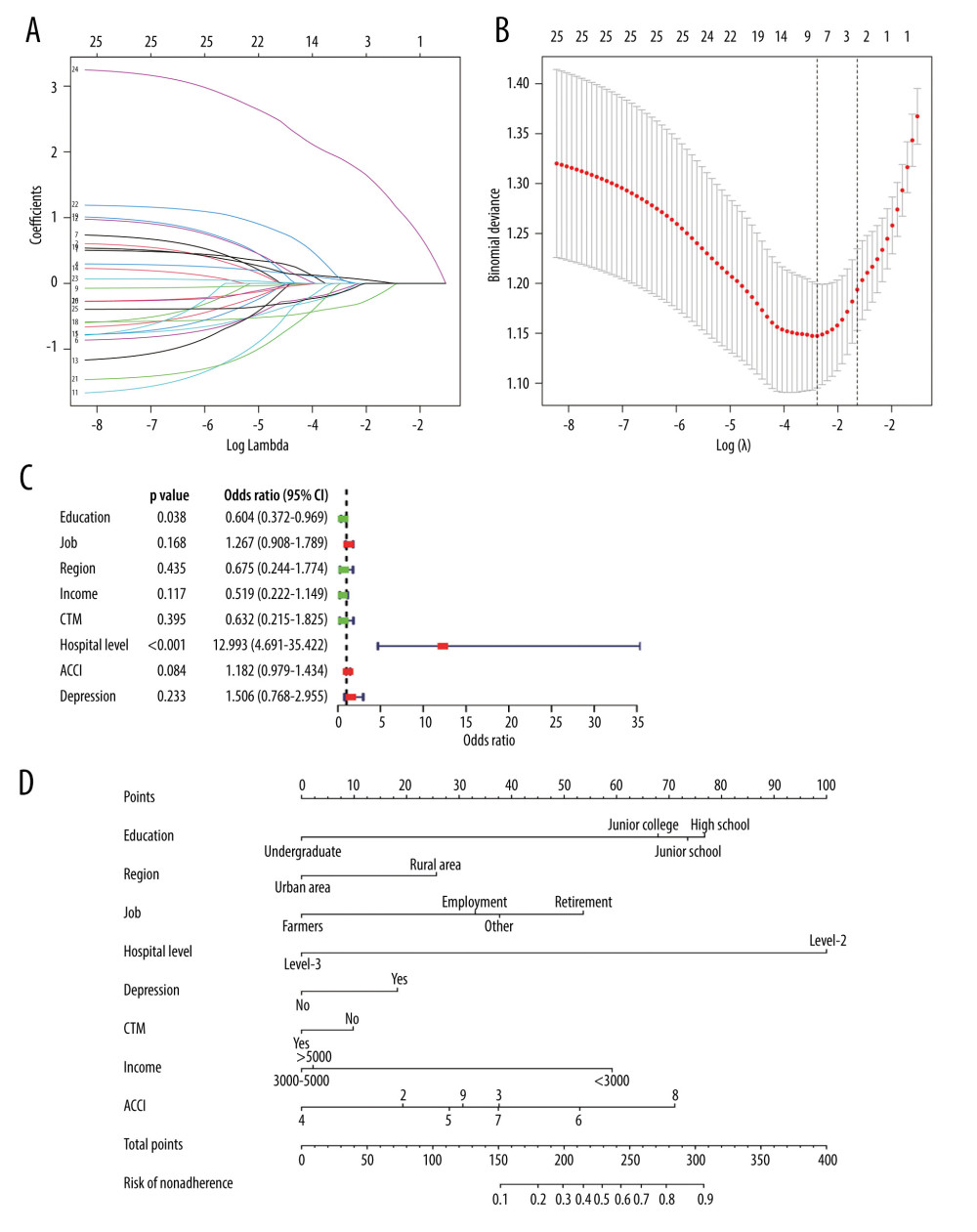 Figure 1. Prediction factors for medication nonadherence were selected, and a medication nonadherence nomogram was developed in hemodialysis patients. (A, B) Least absolute shrinkage and selection operator (LASSO) coefficient profiles of the 8 prediction factors. (C) Logistic regression analyses of the 8 prediction factors in hemodialysis patients. (D) Nomogram prediction of medication nonadherence in hemodialysis patients. (R software, version 4.0.3)
Figure 1. Prediction factors for medication nonadherence were selected, and a medication nonadherence nomogram was developed in hemodialysis patients. (A, B) Least absolute shrinkage and selection operator (LASSO) coefficient profiles of the 8 prediction factors. (C) Logistic regression analyses of the 8 prediction factors in hemodialysis patients. (D) Nomogram prediction of medication nonadherence in hemodialysis patients. (R software, version 4.0.3)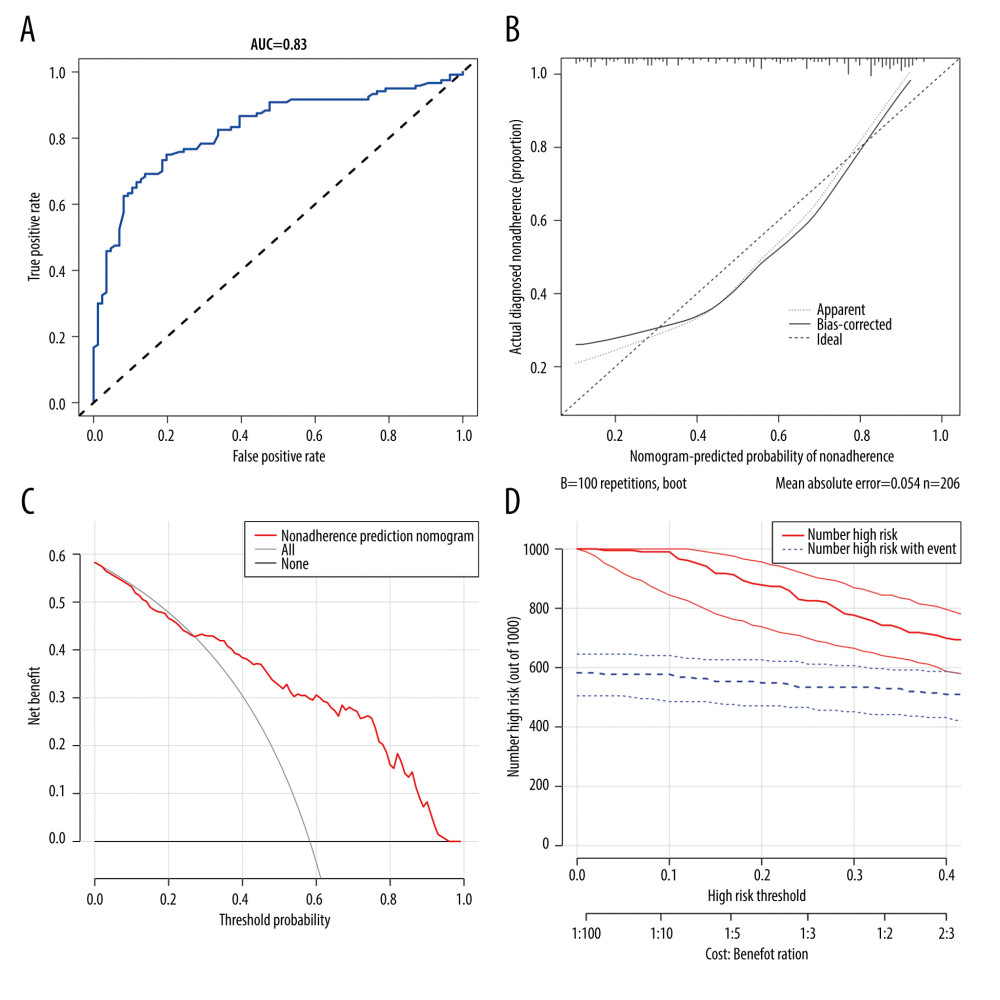 Figure 2. Medication nonadherence of nomogram evaluation and clinical use in hemodialysis patients. (A) ROC curve based on the predictive nomogram for medication nonadherence in hemodialysis patients. (B) Calibration plots for predicting patient medication nonadherence. (C) Decision curve analysis for the nonadherence nomogram in hemodialysis patients. (D) Clinical impact plot for predicting patient medication nonadherence. (R software, version 4.0.3)
Figure 2. Medication nonadherence of nomogram evaluation and clinical use in hemodialysis patients. (A) ROC curve based on the predictive nomogram for medication nonadherence in hemodialysis patients. (B) Calibration plots for predicting patient medication nonadherence. (C) Decision curve analysis for the nonadherence nomogram in hemodialysis patients. (D) Clinical impact plot for predicting patient medication nonadherence. (R software, version 4.0.3) In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









