18 February 2022: Clinical Research
Static Balance in Participants with Temporomandibular Joint Disc Displacement without Reduction Versus Healthy Participants: A Cross-Sectional Study
Ling Zhang1ACEF, Lili Xu2ACD, Junlan Lu2DF, Bin Cai2DG, Shuai Fan2ACEG*DOI: 10.12659/MSM.934593
Med Sci Monit 2022; 28:e934593
Abstract
BACKGROUND: There is no consensus on the association between body posture and temporomandibular disorders (TMDs). This study aimed to assess differences in static balance between healthy participants and patients with temporomandibular joint disc displacement without reduction.
MATERIAL AND METHODS: Sixteen patients with temporomandibular joint disc displacement without reduction and 14 healthy participants were included. Static balance tests were performed in the rest and “cotton rolls” (participants biting 2 cotton rolls with their upper and lower teeth) mandibular positions. The mean body’s center of gravity (COG) sway velocity was tested in each mandibular position on a firm surface with and without eyes open and on a foam surface with and without eyes open.
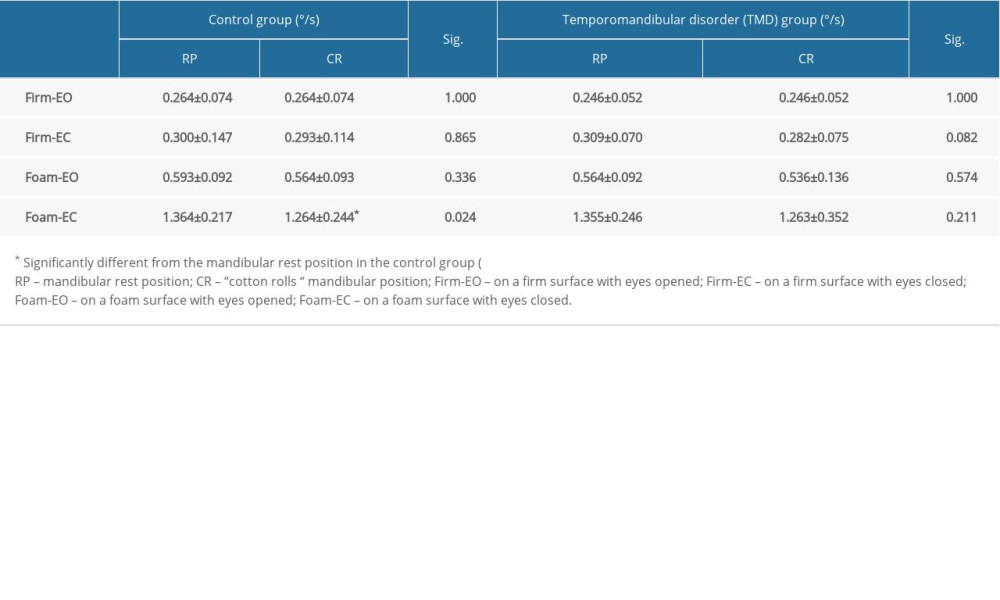
RESULTS: The COG sway velocity did not differ between the TMD and healthy groups regarding mandibular position or testing condition (P>0.05). However, in the control group, the COG sway velocity in the mandibular rest position was significantly higher than that in the “cotton rolls” mandibular position when standing on a foam surface with the eyes closed (P=0.024). In the TMD group, there was no difference in the COG sway velocity between the 2 mandible positions under any condition (P>0.05).
CONCLUSIONS: This study provides new evidence for static balance alterations in patients with temporomandibular joint disc displacement without reduction. Further studies are needed to investigate postural control changes in patients with arthrogenous TMDs. This study was registered in the Chinese Clinical Trial Registry (no. ChiCTR1800018369).
Keywords: chronic pain, Mandible, Physical and Rehabilitation Medicine, postural balance, Temporomandibular Joint Disorders, Adult, Cross-Sectional Studies, Female, healthy volunteers, Humans, Joint Dislocations, Male, Physical Therapy Modalities, Temporomandibular Joint Disc
Background
Body posture is the orientation and positioning of various body segments and the relationships between these segments [1] and is determined by the influences of bone structures, muscles, ligaments, and fascia covering the entire body. Postural adjustments occur based on somatosensory, visual, and vestibular inputs, which then integrate into a complex regulatory system [2]. Recently, the influence of the stomatognathic system on postural stability has been increasingly discussed [3,4].
Temporomandibular disorders (TMDs) are a group of clinical conditions affecting the stomatognathic system, particularly the temporomandibular joints (TMJs) and the masticatory muscles [5]. However, the etiology of TMD remains unclear as it is multidimensional, with several associated risk factors, such as age, hyperlaxity, parafunctional habits, stress, anxiety, and body postural changes [6]. Some reports indicate that a better understanding of the relationship between postural stability, mandible position, and TMD is critical to interpret the possible diagnostic and therapeutic implications of TMD [7,8]. Also, recent claims on correcting abnormal body posture during the management of TMD according to such relationships were based on questionable theories [8].
The relationship between body posture, mandible position, and TMD has been widely investigated [9–11]. Several studies demonstrated peculiar postural features in patients with TMD [8,12]. Armijo-Olivo et al [13] compared the head and cervical postures of patients with myogenous TMD with healthy individuals and reported craniocervical posture changes in these patients. Kittel et al [12] found that patients with TMD had greater postural asymmetry and hypothesized that cervical pain was associated with postural abnormalities. Manfredini et al [8] concluded that the presence of TMD pain is not related to postural abnormalities, and there is a lack of evidence for the existence of a predictable relationship between mandible position and postural features. Currently, studies investigating the relationship between postural balance and TMD mainly focus on myogenous patients with TMD, and few studies investigated the relationship between mandible position and postural features in patients with TMD. A systematic review by Chaves et al [14] found strong evidence of postural changes in myogenous TMD and moderate evidence of postural misalignment in arthrogenous TMD. Rocha et al [15] assessed the postural features of patients with TMD affected by disc displacement, with and without reduction, and observed no significant differences in body posture between the 2 groups. To date, the findings regarding postural characteristics in patients with arthrogenous TMD vary, and few studies have reported on alternations in postural balance in patients with TMJ disc displacement without reduction. To the best of our knowledge, the relationship between postural stability, mandible position, and TMD is still unclear.
Therefore, this study compared static balance between different mandible positions in healthy participants and patients with TMJ disc displacement without reduction. We hypothesized a significant difference in static balance control between patients with TMD and healthy participants and a significant difference in static balance between different mandible positions in both groups.
Material and Methods
STUDY POPULATION:
This cross-sectional study conformed to the STROBE statement, was approved by the Ethics Committee, and followed the Declaration of Helsinki guidelines (approval no. 2018-96-T87). The clinical trial was registered in the Chinese Clinical Trial Registry (
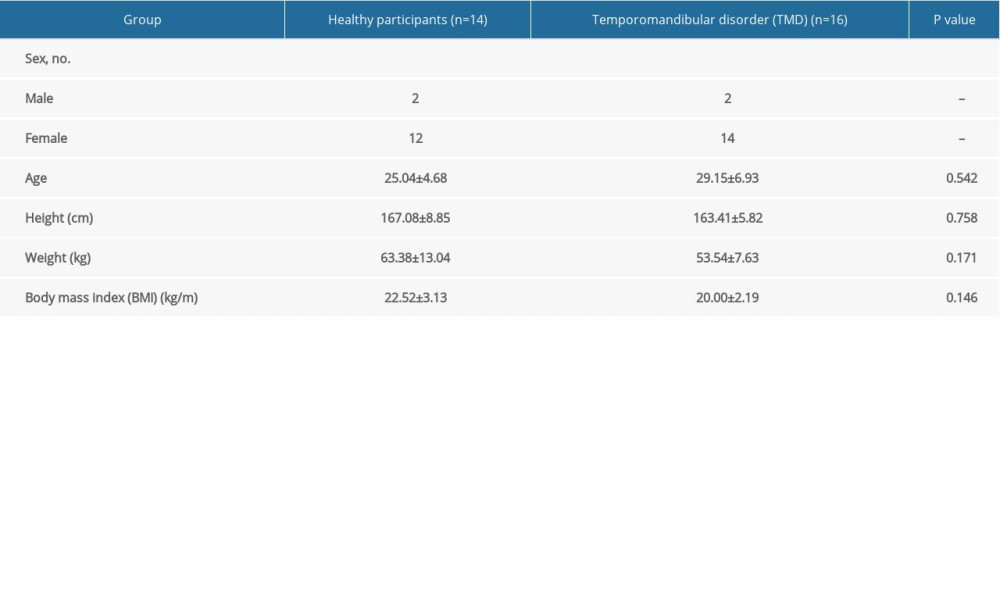
All patients who visited the hospital Rehabilitation Department between January 2019 and January 2020 were screened for eligibility. The study included 16 patients with TMD (2 men, 14 women; mean age 29.15±6.93 years; mean height 163.41±5.82 cm; mean weight 53.54±7.63 kg; 8 unilateral and 8 bilateral) and 14 healthy participants (2 men, 12 women; mean age 25.04±4.68 years; mean height 167.08±8.85 cm; mean weight 63.38±13.04 kg).
All participants were examined by the same physician (F.S.), a TMD expert, to determine dental occlusion abnormalities or TMD according to the Diagnostic Criteria for TMD (DC/TMD) protocols during their first outpatient visit [16]. Patients were included in the TMD group if they were between 18 to 45 years old, clinically diagnosed with TMJ disc displacement without reduction with an MRI-confirmed disc displacement, and had restricted mouth opening. Patients with TMJ disc displacement without reduction caused by misalignment of teeth, a habit of biting on 1 side, stress, and a cheek cane were excluded. Patients were also excluded from the TMD group if they had fewer than 32 teeth, a history of facial trauma, the absence of a crossbite, or vestibular or visual problems or if they had received TMD-related treatment in the past 2 weeks, such as physical therapy, medication, and joint injections. Participants with trauma or any disorder that influenced posture, ongoing or previous orthodontic treatment, and prior orthognathic surgery were also excluded. Individuals with no signs or symptoms of TMD according to the DC/TMD protocol were included in the healthy control group [16]. The healthy control group participants had no joint sounds during jaw movements and were recruited from the hospital interns.
INSTRUMENTATION AND TEST PROCEDURE:
Static balance was assessed using the NeuroCom Balance Manager (NeuroCom, Clackamas, OR, USA). This device includes a computer processing system and a whole force-plate structure with 4 transducers oriented vertically and 1 transducer oriented horizontally. The system sampled at a 100 Hz frequency, with the center of gravity (COG) movement parameters conveyed to the host every 10 s. This device was previously tested for reliability and validity [17]. During the testing procedure, the force plate was fixed.
The demographic data of all participants were collected before testing. Static balance tests were performed in 2 mandible positions: a mandibular rest position, a relaxed condition of the masticatory muscles without tooth contact [18], and a “cotton rolls” mandibular position, in which the participant bit 5-mm thick by 35-mm long cotton rolls placed from the canines to the molars between the 2 dental arches. Static balance control was measured on firm and foam surfaces, and the test was repeated with eyes open and closed. During testing, participants were barefoot and were instructed to stand in a designated location and remain as stable as possible, with feet separated comfortably, hands rested on their hips, and facing the wall without concentrating on 1 point. All participants were allowed 3 min of practice before testing and received the same verbal instructions during testing. The trial was discarded and repeated if participants lifted their heels from the platform, changed foot position relative to the platform, or lost their balance during testing.
Static balance was first assessed in the mandibular rest position and then in the cotton rolls mandibular position. In each mandibular position, participants were tested on a firm surface with and without eyes open and on a foam surface with and without eyes open. Each participant underwent 8 tests in total, and the COG sway velocities were recorded. One test consisted of three 10-s trials, and the mean COG sway velocity (measured in degrees per s) was calculated as the primary outcome measure. The static balance test was performed by the same researcher, who did not know the research group or the study hypothesis.
STATISTICAL METHODS:
First, a preliminary analysis was conducted with PASS version 15 (NCSS LLC, Kaysville, Utah, USA) to determine the necessary sample size based on an anticipated standard deviation of 0.04 and a group difference of 0.05, according to pre-experimental results. A minimum of 12 participants were required per group (power=80%; 1-sided α=0.05).
Demographic data and COG sway velocities are reported as the mean±standard deviation based on the group and the test condition. Data normality was assessed using the Shapiro-Wilk test. An independent
Results
Participant age, height, and weight did not differ significantly between the TMD and healthy control groups (
The reported
Discussion
This study assessed static balance control in patients with TMJ disc displacement without reduction compared with that in healthy participants. Contrary to our hypothesis, there was no significant difference between TMD and healthy participants regarding static balance. Body balance control of healthy participants on an unstable surface was significantly better when dental occlusion was in the cotton rolls mandibular position. However, there was no difference in static balance between the mandible positions in the arthrogenous TMD group.
This study focused on static balance control in patients with TMJ disc displacement without reduction, and there were no significant differences compared with healthy individuals. Inconsistent with our findings, some studies suggested atypical static body posture features or postural control patterns in patients with TMD [11,14], which may be explained based on sample selection differences. Patients in previous studies had myogenous TMD diagnosed according to the DC/TMD protocol, while the present study included patients diagnosed on the basis of symptoms and signs of arthrogenous TMD. Additionally, we performed static balance analysis using the body’s COG sway velocity, but other studies primarily quantified the ability to maintain balance based on the center of pressure excursion measurements [14]. Rocha et al [15] reported similar findings to ours and concluded that patients with TMJ disc displacement with reduction did not have body postural misalignment, indicating that there may be differences in the regulation of balance control between myogenic and arthrogenous patients with TMD.
Our results showed that in healthy participants, the mandible position contributed to static balance control in an unstable condition but had no effect in a stable condition. Specifically, the COG sway velocity was significantly higher in the mandibular rest position than the cotton rolls mandibular position when standing on a foam surface, suggesting an improvement in static balance control when dental occlusion was in the cotton rolls mandibular position. Until recently, the mandible position mechanisms of action were not well understood. Pallegama et al [19] reported that the stomatognathic system can affect balance control via the relationship between the cervical and masticatory muscles, acting through periodontal pressoreceptor feedback that takes control of the elevator mandibular muscles. In short, different mandible positions alter the masticatory muscle pattern, which can influence cervical chains, presumably resulting in postural control changes. Recent studies investigated the effect of sub-maximum jaw clenching on postural control and found that concurrent muscle activation while clenching the jaw significantly improved postural control compared with habitual standing [9,20–22]. Jaw and neck muscles co-contract at the sub-maximum bite force generated during jaw clenching to improve proprioception and balance control [20,23]. Furthermore, our findings indicated that surface conditions can contribute differently to postural balance regulation. Reports showed that dental occlusion affected balance control differently according to the stability condition [24], perhaps owing to the trigeminal nerve to vestibular nuclei link which may be responsible for equilibrium control and masticatory function. When standing on a firm surface, afferent signals used in the postural balance process primarily come from somatosensory information, whereas the sensory information from the visual and vestibular systems increases when standing on a foam surface [21,25]. These results suggest that in clinical practice, the physiotherapist should take the mandible position and the surface condition into consideration during balance training for patients with TMD.
Mandibular movement related to cervical movement becomes interconnected through postural synergies, which have a sensitive proprioceptive feedback system feeding into the center of the brain [20,26]. The cotton rolls placed between the 2 arches distributes the occlusal load onto several teeth, resulting in reduced precision of the proprioceptive periodontal information [25]. However, in this study, mandible position did not affect static balance in the arthrogenous TMD group. Therefore, static balance may be associated with imbalanced muscle co-contraction, impaired orofacial functions, and abnormal proprioception [27].
Joint sense reduction in patients with TMD could result in abnormal proprioception and poor postural balance [9]. Additionally, neuroanatomical connections between the cervical and masticatory muscles can influence postural imbalances in patients with TMD [19,20]. Increasing evidence suggests a clinical improvement in TMD symptoms when the mandible is permitted to function from the mandible rest position [22,28]. Our results support the positive outcomes of some manual therapies and therapeutic exercises, such as joint mobilization and chiropractic and jaw exercises. Notably, although no difference was seen in static balance between patients with TMJ disc displacement without reduction and healthy participants, arthrogenous TMD resulted in sensorial input changes linked to dental occlusion for balance control, which requires further investigation.
There are limitations to this study. First, a relatively small number of participants were included. Second, the patients with TMJ disc displacement without reduction included in the study were those who wanted to receive physical therapy. Male patients who visited the outpatient clinic had milder symptoms than female patients, chose self-management more often, and failed to participate in the study, which affected the sex ratio of included participants. Although sex differences in body posture for patients with TMD have not been previously reported, there was too large a difference in the number of male and female participants enrolled in this study. Future studies should include more male participants, and explore sex differences in body posture for patients with TMD. Third, this study included only patients with TMJ disc displacement without reduction. Future studies should assess differences in body posture between patients with TMD affected by TMJ disc displacement without reduction and those affected by TMJ disc displacement with reduction. Fourth, although the NeuroCom Balance Manager has good reliability and validity for the balance test [17], the balance function results from several factors, and the instrument can only reflect the balance function in certain ways. Because this study was performed in China, its applicability to other populations and countries is limited. Although this study showed no postural changes in participants with arthrogenous TMD compared with the healthy group, the findings are not definitive or generalizable since it is a cross-sectional study. Large-scale, experimental studies are needed in the future.
Conclusions
This study showed no significant differences in static balance control between healthy participants and patients with TMJ disc displacement without reduction. In healthy individuals, the mandible position contributed to the static balance control in an unstable condition but did not affect static balance in arthrogenous patients with TMD. A thorough understanding of postural balance is critical for developing more effective rehabilitation programs for TMD, and these results provide new evidence for static balance alterations in patients with disc displacement without reduction. Future studies should evaluate the effects of dental malocclusion on postural stability in patients with arthrogenous TMD.
References
1. Köhler AA, On temporomandibular disorders: Time trends, associated factors, treatment need and treatment outcome: Swed Dent J Suppl, 2012; 227(21); 111-19
2. Lee MY, Lee HY, Yong MS, Characteristics of cervical position sense in participants with forward head posture: J Phys Ther Sci, 2014; 26(7); 1741-43
3. Lee WY, Okeson JP, Lindroth J, The relationship between forward head posture and temporomandibular disorders: J Orofac Pain, 1995; 9(3); 161-67
4. Olivo SA, Bravo J, Magee DJ, The association between head and cervical posture and temporomandibular disorders: A systematic review: J Orofac Pain, 2006; 20(42); 9-23
5. Manfredini D, Arveda N, Guarda-Nardini L, Distribution of diagnoses in a population of patients with temporomandibular disorders: Oral Surg Or Med Or Pa, 2012; 114(11); 342-48
6. März K, Adler W, Matta RE, Can different occlusal positions instantaneously impact spine and body posture: A pilot study using rasterstereography for a three-dimensional evaluation: J Orofac Orthop, 2017; 78(3); 221-32
7. Anastassaki Köhler A, Hugoson A, Magnusson T, Prevalence of symptoms indicative of temporomandibular disorders in adults: Cross-sectional epidemiological investigations covering two decades: Acta Odontol Scand, 2012; 70(3); 213-23
8. Manfredini D, Castroflorio T, Perinetti G, Dental occlusion, body posture and temporomandibular disorders: Where we are now and where we are heading for: J Oral Rehab, 2012; 39(6); 463-71
9. Peterka RJ, Sensorymotor integration in human postural control: J Neurophysiol, 2002; 88(3); 1097-118
10. Strini PJ, Machado NA, Gorreri MC, Postural evaluation of patients with temporomandibular disorders under use of occlusal splints: J Appl Oral Sci, 2009; 17(8); 539-43
11. Nota A, Tecco S, Ehsani S, Postural stability in participants with temporomandibular disorders and healthy controls: A comparative assessment: J Electromyogr Kinesiol, 2017; 37(4); 21-24
12. Kittel R, Fausto B, Analysis of the postural stability in individuals with or without signs and symptoms of temporomandibular disorder: Braz Oral Res, 2008; 22(9); 378-83
13. Armijo-Olivo S, Rappoport K, Fuentes J, Head and cervical posture in patients with temporomandibular disorders: J Orofac Pain, 2011; 25(3); 199-209
14. Chaves TC, Turci AM, Pinheiro CF, Static body postural misalignment in individuals with temporomandibular disorders: A systematic review: Braz J Phys Ther, 2014; 18(6); 481-501
15. Rocha T, Castro MA, Guarda-Nardini L, Participants with temporomandibular joint disc displacement do not feature any peculiar changes in body posture: J Oral Rehab, 2017; 44(7); 81-89
16. Schiffman E, Ohrbach R, Truelove E, Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group: J Oral Facial Pain Headache, 2014; 28(56); 6-27
17. Harro CC, Garascia C, Reliability and validity of computerized force platform measures of balance function in healthy older adults: J Geriatr Phys Ther, 2019; 42(26); 57-66
18. Yilmaz G, Uginčius P, Sebik O, Tonic activity of the human temporalis muscle at mandibular rest position: Arch Oral Biol, 2015; 60(15); 887-93
19. Pallegama R, Ranasinghe A, Weerasinghe V, Influence of masticatory muscle pain on electromyographic activities of cervical muscles in patients with myogenous temporomandibular disorders: J Oral Rehab, 2004; 31(21); 423-29
20. Giannakopoulos NN, Hellmann D, Schmitter M, Neuromuscular interaction of jaw and neck muscles during jaw clenching: J Orofac Pain, 2013; 27(78); 61-71
21. Ringhof S, Leibold T, Hellmann D, Postural stability and the influence of concurrent muscle activation – Beneficial effects of jaw and fist clenching: Gait Posture, 2015; 42(9); 598-600
22. Heit T, Derkson C, Bierkos J, The effect of the physiological rest position of the mandible on cerebral blood flow and physical balance: An observational study: Cranio, 2015; 33(3); 195-205
23. Ferreira CL, Machado BC, Borges CG, Impaired orofacial motor functions on chronic temporomandibular disorders: J Electromyogr Kinesiol, 2014; 24(4); 565-71
24. Grosdent S, O’Thanh R, Domken O, Dental occlusion influences knee muscular performances in asymptomatic females: J Strength Cond Res, 2014; 28(25); 492-98
25. Julià-Sánchez S, Álvarez-Herms J, Gatterer H, Dental occlusion influences the standing balance on an unstable platform: Motor Control, 2015; 19(7); 341-54
26. Lee JH, Effects of forward head posture on static and dynamic balance control: J Phys Ther Sci, 2016; 28(4); 274-77
27. Yong MS, Lee HY, Lee MY, Correlation between head posture and proprioceptive function in the cervical region: J Phys Ther Sci, 2016; 28(67); 857-60
28. Tingey EM, Buschang PH, Throckmorton GS, Mandibular rest position: A reliable position influenced by head support and body posture: Am J Orthod Dentofacial Orthop, 2001; 120(8); 614-22
In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952