01 December 2021: Clinical Research
Comparison of the Effects of Myotherapy in Patients with Myofascial Pain with and without Self-Reported Sleep Bruxism Using The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) Axis I Questionnaire
Małgorzata Gałczyńska-RusinDOI: 10.12659/MSM.934917
Med Sci Monit 2021; 27:e934917
Abstract
BACKGROUND: This study aimed to compare the effects of myotherapy using sublingual relaxation splints and stretching exercises in 110 patients with myofascial pain with and without self-reported sleep bruxism using The Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) Axis I Questionnaire.
MATERIAL AND METHODS: The study involved 110 patients with myofascial pain. The diagnosis was based on the RDC/TMD questionnaire. The number of painful muscle sites (PMS) and the range of maximum mouth opening (MMO) were assessed 2 times – at the first visit and after 3 months. Then, the influence of possible bruxism on the treatment was assessed.
RESULTS: The mean age of the patients was 26.8 years (SD 5.4); 89% of the subjects were women; and 60.9% of the patients reported bruxism. Each patient was instructed to perform muscle stretching at the first visit and after 1 week all patients received a sublingual relaxation splint. The number of PMS decreased and the range of MMO increased in both groups after a period of 3 months of treatment (P<0.05). Significant differences were observed in the obtained treatment effects between the patients with and without possible bruxism.
CONCLUSIONS: This study evaluated the effectiveness of the sublingual relaxation splint and stretching exercises in patients with myofascial pain. Patients at a single center in Poland who reported myofascial pain that was not associated with self-reported sleep bruxism had a significantly better response to myotherapy when compared to patients with self-reported sleep bruxism.
Keywords: bruxism, Myofascial Pain Syndromes, Occlusal Splints, Temporomandibular Joint Dysfunction Syndrome, Female, Humans, Male, Myofunctional Therapy, pain management, self report, Sleep Bruxism, Surveys and Questionnaires
Background
Pain is the most common reason for patients with temporomandibular disorders (TMD) to seek treatment [1]. Patients with the muscular form of TMD more often report the coexistence of other ailments and stronger pain than those with the joint form [2]. Myalgia of orofacial muscles is defined as pain of muscular origin, which is influenced by the movements of the mandible and the normal function and parafunction of the temporomandibular joint [3]. The severity of the muscle pain is directly related to the functional activity of the muscles involved, which can also cause fatigue and increased tenderness [1].
There are many possible causes of the pain-related form of TMD. One of the factors that may influence the development of TMD is bruxism [4]. Bruxism is defined as repetitive activity of the masticatory muscles, characterized by clenching and grinding of the teeth, and bracing or thrusting of the mandible [5]. Sleep bruxism (SB) and awake bruxism (AB) are distinguished [5]. In the international classification, a three-level assessment of this condition has been adopted: possible bruxism is assessed on the basis of complaints reported by the patient in the questionnaire or in the history; probable bruxism is assessed on the basis of physical examination in a patient with or without symptoms; and definite bruxism is assessed on the basis of polysomnography (SB) or electromyography (AB) in both symptomatic and symptom-free patients with positive or negative clinical examination [6].
It has been proved that the use of both therapeutic exercises and occlusal splints brings significant effects in terms of reducing pain in patients with the pain-related form of TMD [7–11]. Exercises used in the treatment of myalgia are designed to reduce pain, improve the coordination of masticatory muscles, reduce muscle spasm and hyperactivity, as well as strengthening the muscles and supporting tissue regeneration [12].
In the literature there are many studies comparing the effectiveness of therapeutic exercises with the use of occlusal splints [10,11,13], while few reports describe the use of non-occluding sublingual splints [14,15].
The aim of the study was to compare the efficacy of myofascial pain treatment using stretching exercises and the sublingual relaxation splint in patients with and without possible bruxism.
Material and Methods
PATIENT SELECTION:
The research involved patients who presented to the Department of Temporomandibular Disorders at the Poznań University of Medical Sciences with a pain-related form of TMD. Among these patients (n=157), people suffering from isolated myofascial pain were selected (n=133). 110 patients completed the entire study (27 missed the follow-up visit).
A total of 110 people were examined, who were then divided into a group of patients with possible bruxism and a group of patients who did not report bruxism. Written consent was obtained from each patient that participate in the study.
The study included patients over 18 years of age who were diagnosed with myofascial pain or myofascial pain with limited mouth opening (IA/IB) on the basis of the Research Diagnostic Criteria for Temporomandibular Disorders Questionnaire (RDC/TMD) Axis I. The study excluded patients with an RDC/TMD diagnosis of IIA, IIB, IIC and IIIA, IIIB, IIIC; people after recent injuries; people with general diseases that may affect the functioning of TMJ (eg, RA); and people over 40 years of age.
STUDY DESIGN:
At the first visit, the patients were instructed to perform muscle stretching exercises (SE) and the nature of bruxism was explained to them. In accordance with the guidelines of the international consensus on the assessment of bruxism [6], after explaining what awake and sleep bruxism is, the patients were asked to self-observe (teeth grinding, teeth clenching, bracing or thrusting of the mandible) and to obtain information from their partners about possible teeth grinding during sleep. During this visit, impressions were also taken for the sublingual relaxation splint.
At the second visit, the sublingual relaxation splint was put in place and the correctness of the prescribed stretching exercises was checked. Each patient again answered the following RDC/TMD questions:
Have you been told or do you notice that you grind your teeth or clench your jaw while sleeping at night?
Do you grind your teeth or clench your jaw during the day?
Based on their responses to the above questions, the studied patients were divided into those with and those without possible bruxism.
A follow-up visit was scheduled after 4 weeks. During the visit the correctness of performing the stretching exercises was checked, and questions were asked about any problems connected with using the sublingual relaxation splint. After a period of 3 months another follow-up visit was held, at which muscle tenderness and the maximum comfortable mouth opening were reassessed.
RESEARCH DIAGNOSTIC CRITERIA FOR TEMPOROMANDIBULAR DISORDERS (RDC/TMD) – AXIS I:
The clinical examination of patients was based on the RDC/TMD questionnaire, which was adapted into Polish by Osiewicz et al [16]. This examination makes it possible to assign patients to the following TMD groups: group I – muscular disorders; group II – disc displacement; group III – arthralgia, osteoarthritis and osteoarthrosis. Axis I of the questionnaire was used in the study [17].
The examination of painful muscle sites (PMS) was performed on the basis of the muscle sites determined by RDC/TMD (10 sites on the right side and 10 sites on the left side). These sites are the posterior, middle and anterior part of the temporalis muscle; the upper, middle and lower part of the masseter muscle (with 1 kg palpation pressure); the posterior mandibular region; the submandibular region; the lateral pterygoid area; and the temporalis muscle tendon (with 0.5 kg palpation pressure). During palpation, the patient’s mandible was in a rest position, with the teeth out of contact. Before examining the above-mentioned muscle sites, the examiner calibrated the pressure force 3 times using an electronic scale. In the statistical analysis, the number of painful sites was counted before the treatment and after the 3-month treatment period.
The range of the maximum mouth opening (MMO) was also assessed. Each patient was asked to open their mouth as wide as it was possible without any pain, and the distance between the incisal edge of the maxillary central incisor (tooth 11) and the incisal edge of the mandibular central incisor of the mandible (tooth 41) was measured. The value of the vertical overlap of the incisors was added to the obtained result.
METHODS OF MYOTHERAPY:
At the first visit all the patients were instructed to perform stretching and relaxation exercises. The stretching exercises consisted of performing slow movements of the mandible, including maximum opening, laterotrusion and protrusion without resistance, and then performing the above movements against some resistance. Exercises had to be performed 3 times a day for a minimum of 10 minutes. Relaxation exercises according to Bae were also recommended [8]. This exercise involves placing the front one-third of the tongue on the roof of the mouth and applying a light force to the tip of the tongue with the tip not touching the teeth. The patient holds this position for as long as possible. Relaxation exercises were recommended after performing a series of stretching exercises and before going to bed. Each patient received detailed written instructions on how to perform the above exercises.
Sublingual relaxation splint (SRS). At the second visit all the patients received a sublingual relaxation splint. The correctness of the stretching exercises was also checked. SRS was recommended to be used during the night. This splint is designed for the lower dental arch; its frontal part runs along the edges of the incisors and canines, then at the level of the anatomic equator of the lateral teeth, and descends behind the last molar. SRS does not cover the occlusal surfaces of the teeth; therefore, it does not alter occlusal contacts and does not affect the vertical dimension. A detailed description of SRS can be found in Gawriołek et al [14].
STATISTICAL ANALYSIS:
Statistical calculations were conducted using SPSS v23 software. Descriptive statistics were used for determining mean values and standard deviations (SD). The Kolmogorov-Smirnov test was used to test the normality of distribution of continuous variables. For testing differences between independent groups, the
ETHICAL STATEMENT:
The research was approved by the Poznań University of Medical Sciences Bioethics Committee nr 1198/17. All patients gave informed consent to participate in the study.
Results
STUDY GROUP:
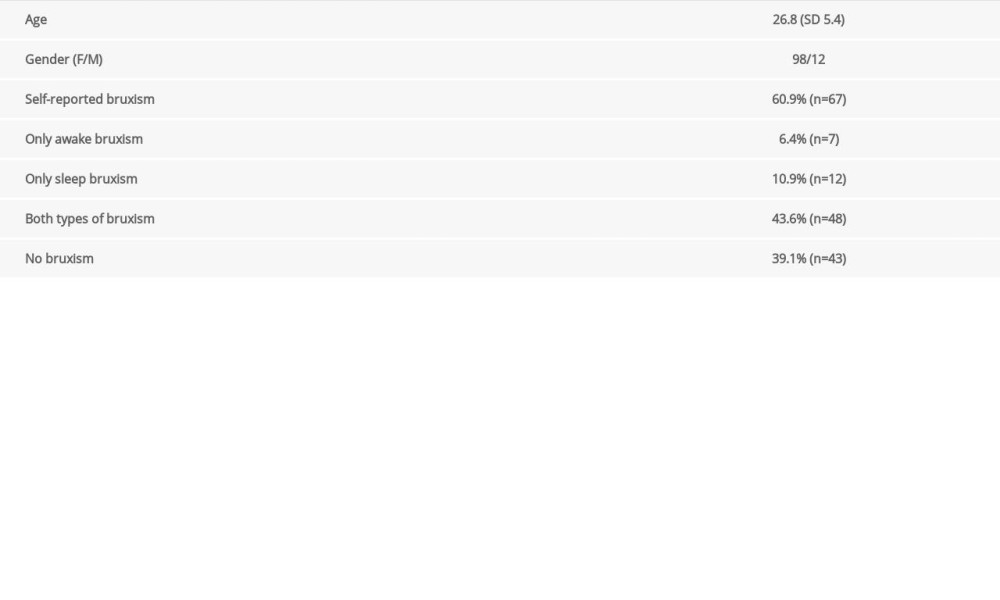
The study included 110 patients. The mean age was 26.8 years (SD 5.4); 89% of the patients were women; and 60.9% of the patients reported bruxism. The description of the study group is presented in Table 1.
MAXIMAL MOUTH OPENING AND PAINFUL MUSCLE SITES BEFORE AND AFTER THE 3-MONTH THERAPY IN PATIENT GROUPS:
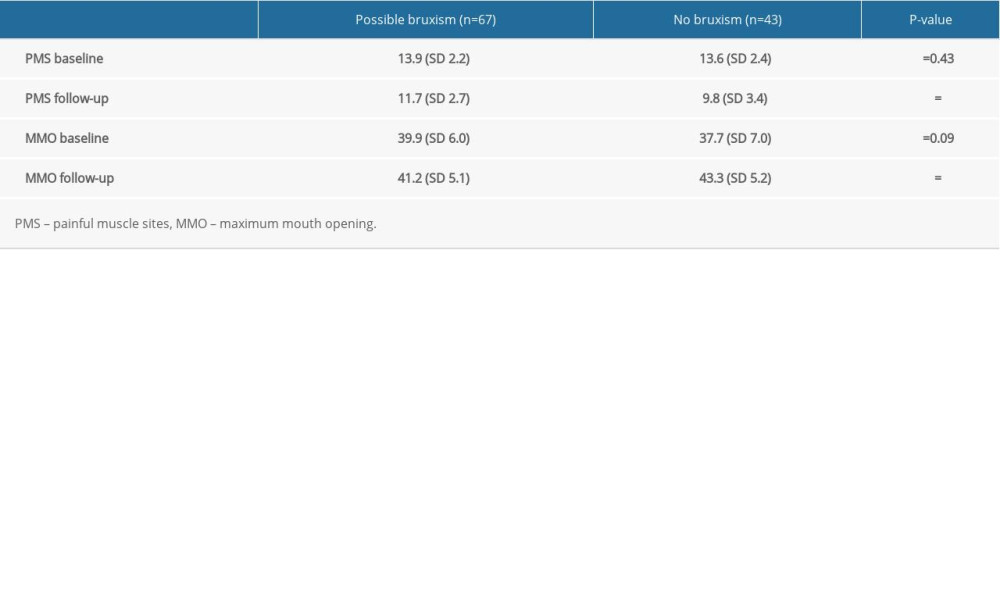
The MMO and PMS were assessed at the beginning of the treatment and after 3 months. The results for patients with and without possible bruxism are presented in Table 2. There was a statistically significant difference between the MMO ranges and the number of PMS recorded at the start of the study and those obtained after the 3-month period (P<0.05). This finding clearly indicates the positive effects of the applied therapy.
COMPARISON OF DIFFERENCES AT THE BEGINNING AND AFTER 3 MONTHS OF TREATMENT IN GROUPS OF PATIENTS WITH POSSIBLE BRUXISM AND WITH NO BRUXISM:
Then the study checked whether there were any differences between the specific groups of patients. The results are presented in Table 3. The obtained treatment effects were compared for the patients with possible bruxism and those without bruxism. No statistically significant differences were found at the beginning of the study, but statistically significant differences were observed after the period of 3 months. There was significant difference in PMS (P=0.01) and in MMO (P=0.03) between patients with self-report bruxism and without it, which indicates that possible bruxism had an impact on the obtained therapeutic effect.
Discussion
In this study, patients with myofascial pain in the masticatory region received a combination therapy which involved a splint and therapeutic exercises.
Therapeutic jaw exercises are often used in the treatment of TMD, primarily because they are simple, cheap and actively involve the patient in the healing process. Exercises are recommended in cases of myalgia, chronic degenerative disease of TMJ, and limited mouth opening due to hyperactivity of the mandibular muscles or disc displacement without reduction. Jaw exercises are contraindicated, however, in acute painful arthritis [9]. Many studies have proved the effectiveness of exercises performed by patients in reducing pain associated with TMD [8,10,18]. Our study recommended stretching and relaxation exercises, which are often used in patients with muscle pain. The stretching exercises are similar to those proposed by Lindfors [9]. Similar stretching exercises were used in the research by Katyayan, achieving a reduction in muscle tenderness, a reduction in pain on the VAS scale, and an increase in mandibular mobility [10]. Relaxation exercises according to Bae and Park were also recommended. In their study they achieved a significant reduction in pain, an increased range of mandibular mobility and a reduction in mandibular deviation in the group of patients who performed exercises compared to the control group [8]. Although there is no doubt as to the efficacy of therapeutic exercises, there has been no consensus so far in standardizing the recommendations for patients with the muscular form of TMD [9]. An international group of specialists agreed that in cases involving catching/temporary locking of the jaw due to disc displacement, patients should be recommended exercises according to Yoda et al [9,19].
In addition to the prescribed exercises, the patients also received a sublingual relaxation splint. The splint was placed in the mandible, not covering the occlusal surfaces of teeth. Most non-occluding splints described in the literature are placebo splints that are used in comparative studies. They are designed in such a way that they cover the palate, have clasps on the molars, and do not affect the occlusal relationships in any way. [11,20–22] Nillson found no statistically significant difference in terms of reducing TMD pain, physical functioning, emotional functioning and headache over a 12-month period between patients using a non-occluding palatal splint and the group using a resilient appliance [22]. Dao obtained similar results when comparing a hard occlusal splint with a palatal splint not covering the occlusal surfaces. In both groups of patients with myofascial pain he achieved a reduction in pain and an increase in the quality of life, with no significant differences observed between the groups [11]. On the other hand, after a 10-week observation of patients with muscle pain, Ekberg found that the stabilization splint was more effective in relieving signs and symptoms in patients with TMD of mainly myogenous origin than the non-occlusal splint used in the control group. It should be noted, however, that in both groups there was a reduction in pain symptoms [20].
An appliance similar to the sublingual relaxation splint used in this study, the ELIBA lingual elevator, has recently been described in the literature. This splint was originally used in orthodontic treatment to maintain the correct position of the tongue in patients suffering from abnormal swallowing after speech therapy. It covers the lingual surfaces of the mandibular incisors, canines and premolars, ending with clasps on the molars. It does not cover the occlusal surfaces and does not alter occlusal relationships. Its manufacture requires taking an impression of the sublingual space [15].
Both Gawriołek and Pietropaoli observed a reduction in TMD symptoms and an increase in the range of MMO as a result of using sublingual splints [14,15]. However, it should be remembered that the placement of a sublingual splint on the soft tissues may cause some discomfort in the form of mucosal trauma in the initial period of use [14].
In studies which used non-occluding splints as a placebo the results are inconclusive. Wassel compared a lower stabilizing splint and a sublingual control splint, which was described as an acrylic lingual flange extending from the occlusal or incisal surfaces into the lingual sulcus. In both groups of patients, the applied treatment produced similar results. Thus, he concluded that the presence of the lingual flange could have an impact on the position of the tongue and oral perception [23].
We also assessed the influence of possible bruxism on the obtained treatment effects. The diagnosis of possible bruxism was based on 2 questions from the RDC/TMD questionnaire. This approach is used in many scientific studies [24–26]. According to the guidelines, after a thorough explanation of the nature of bruxism, all the patients were instructed to self-monitor for a week for the occurrence of clenching, grinding and thrusting of the mandible. This is important because while people with awake bruxism are usually aware of their condition, people with sleep bruxism should pay attention to the symptoms which occur after waking up and obtain information from their partners about possible symptoms occurring during sleep [27]. In our study, 60.9% of people with myofascial pain reported the occurrence of bruxism, and 43.6% reported both forms (awake and sleep bruxism). To compare, Osiewicz found possible bruxism in 67% of patients diagnosed with TMD; and in Reissmann’s study, 84% of patients with the pain-related form of TMD reported bruxism, with 54% reporting both forms [24,25].
Since only a small percentage of the studied patients reported the occurrence of isolated awake or sleep bruxism, regardless of the reported type, all the patients were combined into one group of patients with bruxism.
In our study, we obtained a significant reduction in the number of PMS and an increase in the MMO range both in the patients with and in those without bruxism after 3 months of therapy. Patients in the group without bruxism had on average 3.8 fewer painful muscle points compared to 1.3 in the group with bruxism, and the maximum mouth opening increased by an average of 3.8 mm compared to 2.2 mm in the group with possible bruxism.
We examined a group of people whose primary diagnosis was the presence of myofascial pain within the muscles of the masticatory organ. Michelotii proved that daily clenching or grinding of the teeth is a significant risk factor for the occurrence of myofascial pain [28]. Ohlmann, on the other hand, believes that myofascial pain cannot be explained only on the basis of a simple cause-effect relationship between sleep bruxism and myalgia [4]. There is no doubt, however, that both awake bruxism and sleep bruxism are largely associated with the pain-related form of TMD, and their total effect is greater than the sum of the individual effects [25,27]. At the same time, the 2 types of bruxism are not independent: they interact with each other because the risk of one type of bruxism is modified by the presence of the other type [25].
Our study revealed significant differences in the treatment effects between people with possible bruxism and those not reporting the symptoms of bruxism. Although in both groups there was a reduction in the number of PMS and an increase in the MMO range, the differences between the groups of patients with and without possible bruxism were statistically significant. Therefore, it can be concluded that the occurrence of self-reported bruxism has an impact on the achieved treatment effects.
These findings require further studies on a larger group of patients, which will make it possible to more accurately assess the prevalence of bruxism and more precisely divide patients into those with sleep bruxism, those with awake bruxism, and those with both types of bruxism.
In this study we used the RDC/TMD questionnaire to diagnose myofascial pain. However, for several years a newer version has been available to researchers – the DC/TMD questionnaire [3]. Because its Polish translation was not available when the study was being done, we used the older version. This is a certain limitation of the present study because due to the growing number of publications using the DC/TMD version, it will not be possible to fully relate the obtained results to those obtained by studies using the improved version of the questionnaire. It should be noted that in RDC/TMD the diagnosis of myofascial pain with limited mouth opening was considered to be of no clinical utility and was eliminated in the new DC/TMD. The remaining primary RDC/TMD diagnosis of myofascial pain has been reorganized in the new DC TMD into 2 new disorders: myalgia (as a subclass of muscle pain disorders) and myofascial pain with referral (as a type of myalgia) [3].
The efficacy of the sublingual relaxation splint used in our study to reduce pain and improve the range of pain-free mouth opening among patients with myofascial pain has been proved. In further studies, the observation period should be extended and the size of patient groups should be increased. The study did not include a control group of people with myalgia who would not receive any treatment as we believe it would have been unethical not to provide any help to patients who experienced pain.
In our study, the majority of patients were women. This is consistent with other studies as it has been proven that the female gender poses a greater risk of developing painful-TMD than the male gender [24].
The diagnosis of sleep bruxism was not confirmed using polysomnography, which is a major limitation of the study. In the present study, bruxism was assessed as possible based on the patients’ responses, a method which is commonly used in the literature [24–27], but also sometimes questioned [4]. It was decided not to define bruxism as probable because there are no clear guidelines as to how many symptoms of bruxism would have to occur simultaneously (tooth wear, linea alba, scalloped tongue, muscle hypertrophy, damage to prosthetic work, damage to dental fillings) in order to be able to make this diagnosis. In our opinion, making a diagnosis of probable bruxism based on the occurrence of only one of the above-mentioned symptoms is unreliable. However, it should be emphasized that to date there are no clear criteria for assessing the occurrence of bruxism. A consensus is being created to standardize and systematize the diagnosis [29].
Although the literature recommends a separate analysis of patients with sleep bruxism and awake bruxism [26], it was decided to combine the people reporting possible bruxism due to the small number of people with isolated sleep or awake bruxism (a greater number of patients reported both types).
Conclusions
This study evaluated the efficacy of sublingual relaxation splints and stretching exercises in patients with myofascial pain. The obtained results show the effectiveness of this combination therapy in the treatment of myalgia. Patients who reported myofascial pain that was not associated with self-reported sleep bruxism had a significantly better response to myotherapy when compared with patients with self-reported sleep bruxism.
Further studies are recommended that include confirmation of sleep bruxism using polysomnography and the use of the Polish translation of the updated Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Questionnaire.
References
1. Okeson JP: Management of temporomandibular disorders and occlusion, 2020, St Louis, Elsevier Inc
2. Klasser GD, Bassiur J, de Leeuw R, Differences in reported medical conditions between myogenous and arthrogenous TMD patients and its relevance to the general practitioner: Quintessence Int, 2014; 45(2); 157-67
3. Schiffman E, Ohrbach R, Truelove E, Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group: J Oral Facial Pain Headache, 2014; 28(1); 6-27
4. Ohlmann B, Waldecker M, Leckel M, Correlations between sleep bruxism and temporomandibular disorders: J Clin Med, 2020; 9(2); 611
5. Lobbezoo F, Ahlberg J, Glaros AG, Bruxism defined and graded: An international consensus: J Oral Rehabil, 2013; 40(1); 2-4
6. Lobbezoo F, Ahlberg J, Raphael KG, International consensus on the assessment of bruxism: Report of a work in progress: J Oral Rehabil, 2018; 45(11); 837-44
7. McNeely ML, Armijo Olivo S, Magee DJ, A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders: Phys Ther, 2006; 86(5); 710-25
8. Bae Y, Park Y, The effect of relaxation exercises for the masticator muscles on temporomandibular joint dysfunction (TMD): J Phys Ther Sci, 2013; 25(5); 583-86
9. Lindfors E, Arima T, Baad-Hansen L, Jaw exercises in the treatment of temporomandibular disorders-an international modified delphi study: J Oral Facial Pain Headache, 2019; 33(4); 389-98
10. Katyayan PA, Katyayan MK, Shah RJ, Patel G, Efficacy of appliance therapy on temporomandibular disorder related facial pain and mandibular mobility: A randomized controlled study: J Indian Prosthodont Soc, 2014; 14(3); 251-61
11. Dao TTT, Lavigne GJ, Charbonneau A, The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: A controlled clinical trial: Pain, 1994; 56(1); 85-94
12. da Moraes AR, Sanches ML, Therapeutic exercises for the control of temporomandibular disorders: Dental Press J Orthod, 2013; 18(5); 134-39
13. Niemelä K, Korpela M, Raustia A, Efficacy of stabilisation splint treatment on temporomandibular disorders: J Oral Rehabil, 2012; 39(11); 799-804
14. Gawriołek K, Azer SS, Gawriołek M, Piotrowski PR, Mandibular function after Myorelaxation Therapy in temporomandibular disorders: Adv Med Sci, 2015; 60(1); 6-12
15. Pietropaoli D, Cooper BC, Ortu E, Monaco A, IAPNOR , A device improves signs and symptoms of TMD [published correction appears in Pain Res Manag. 2020;2020:9465080]: Pain Res Manag, 2019; 2019; 5646143
16. Osiewicz MA, Lobbezoo F, Loster BW, Research diagnostic criteria for temporomandibular disorders (RDC/TMD) – The Polish version of a dual-axis system for the diagnosis of TMD. RDC/TMD form: J Stoma, 2013; 66(5); 576-649
17. Dworkin SF, LeResche L, Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique: J Craniomandib Disord, 1992; 6(4); 301-55
18. Magnusson T, Syrén M, Therapeutic jaw exercises and interocclusal appliance therapy. A comparison between two common treatments of temporomandibular disorders: Swed Dent J, 1999; 23(1); 27-37
19. Yoda T, Sakamoto I, Imai H, A randomized controlled trial of therapeutic exercise for clicking due to disk anterior displacement with reduction in the temporomandibular joint: Cranio, 2003; 21(1); 10-16
20. Ekberg E, Vallon D, Nilner M, The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial: J Orofac Pain, 2003; 17(2); 133-39
21. Zhang FY, Wang XG, Dong J, Effect of occlusal splints for the management of patients with myofascial pain: A randomized, controlled, double-blind study: Chin Med J (Engl), 2013; 126(12); 2270-75
22. Nilsson H, Vallon D, Ekberg EC, Long-term efficacy of resilient appliance therapy in TMD pain patients: A randomised, controlled trial: J Oral Rehabil, 2011; 38(10); 713-21
23. Wassell RW, Adams N, Kelly PJ, Treatment of temporomandibular disorders by stabilising splints in general dental practice: results after initial treatment: Br Dent J, 2004; 197(1); 35-51
24. Osiewicz M, Lobbezoo F, Ciapała B, Pain predictors in a population of temporomandibular disorders patients: J Clin Med, 2020; 9(2); 452
25. Reissmann DR, John MT, Aigner A, Interaction between awake and sleep bruxism is associated with increased presence of painful temporomandibular disorder: J Oral Facial Pain Headache, 2017; 31(4); 299-305
26. Wetselaar P, Vermaire EJH, Lobbezoo F, Schuller AA, The prevalence of awake bruxism and sleep bruxism in the Dutch adult population: J Oral Rehabil, 2019; 46(7); 617-23
27. Sierwald I, John MT, Schierz O, Association of temporomandibular disorder pain with awake and sleep bruxism in adults: J Orofac Orthop, 2015; 76(4); 305-17
28. Michelotti A, Cioffi I, Festa P, Oral parafunctions as risk factors for diagnostic TMD subgroups: J Oral Rehabil, 2010; 37(3); 157-62
29. Manfredini D, Ahlberg J, Aarab G, Towards a standardized tool for the assessment of bruxism (STAB) – overview and general remarks of a multidimensional bruxism evaluation system: J Oral Rehabil, 2020; 47(5); 549-56
In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952