18 July 2022: Meta-Analysis
Comparison of Hysteroscopic Morcellation Versus Resectoscopy in Treatment of Patients with Endometrial Lesions: A Meta-Analysis
Fangying Ren1BEFG, Guannan Huang2BEF, Xue Wang3CDE, Xuehui Li4AD*, Jianning Cai5ACDDOI: 10.12659/MSM.936771
Med Sci Monit 2022; 28:e936771
Abstract
BACKGROUND: Hysteroscopic surgery has been widely used in clinical practice for more than 30 years due to its advantages of less trauma, less bleeding, and direct vision. The aim of this study was to compare hysteroscopic morcellation versus conventional resectoscopy for removal of endometrial lesions.
MATERIAL AND METHODS: For the database search, we used the keywords “morcellator,” “morcellators,” “morcellate,” “morcellation,” and “morcellated” combined with “hysteroscopy,” “hysteroscopy,” “uteroscope,” and “transcervical”. The last search was conducted on February 1, 2022. Randomized controlled trials (RCTs) were included in the meta-analysis.
RESULTS: According to our retrieval scheme and the inclusion and exclusion criteria, we found 6 studies including 565 patients. For enumeration data, we calculated the effect size as relative risk (RR) and 95% confidence interval (95% CI), while for quantitative data we used the weighted mean difference (WMD) and 95% confidence interval (95% CI). There was no significant difference between success rate of hysteroscopic morcellation and conventional resectoscopy (relative risk and 95% confidence interval 1.05(0.97,1.13); P=0.232). Procedure time was also shorter with hysteroscopic morcellation, the procedure time of the hysteroscopic morcellation group was 3.43 min shorter compared with the conventional resectoscopy group, and the operating time in the hysteroscopic morcellation group was 2.81 min shorter. In terms of fluid deficit, there was no statistically significant difference in fluid loss between the 2 groups (P=0.209).
CONCLUSIONS: Hysteroscopic morcellation is associated with a shorter procedure time and operative time among patients with endometrial lesions compared with resectoscopy.
Keywords: endoscopic mucosal resection, Morcellation, Uterine Diseases, Female, Humans, Hysteroscopy, operative time, Pregnancy
Background
Hysteroscopic surgery has been widely used in clinical practice for more than 30 years due to its advantages of less trauma, less bleeding, and direct vision. Hysteroscopy is used to determine the causes of abnormal uterine bleeding and infertility. Structural causes like submucosal fibroids, intrauterine adhesions, uterine septum, and intrauterine foreign bodies are easily treated with operative hysteroscope. Commonly used treatment methods include hysteroscopic resection, combined hysteroscopy and laparoscopy, laparoscopy alone, vaginal surgery, and open surgery. At present, hysteroscopic resection of endometrial polyps is widely used in clinical practice. This treatment method uses a hysteroscopic ring electrode, which can remove polyps directly under the microscope, with fewer residual roots and a relatively low recurrence rate. However, the recurrence of endometrial polyps after resection of endometrial polyps is still possible under certain conditions [1].
With the development of gynecological minimally invasive surgery, hysteroscopic resection of endometrial polyps has become the criterion standard of treatment. Traditional hysteroscopic electrotomy uses the ring electrode to remove polyps, and also can be electrocoagulated to stop blood flow. The postoperative recurrence rate is low, so it is widely used in clinical practice. In recent years, with the attention paid to fertility recovery after endometrial polypectomy, thermal radiation generated during electroresection has also been discussed, mainly because radiant heat can damage the deep muscle tissue of the lesion site and the surrounding normal endometrium [2]. The heat generated by electric resection can increase the temperature of the distention fluid and affect the endometrium, thus increasing the risk of intrauterine adhesion and reducing the postoperative pregnancy rate.
Monopolar resection was first used for clinical treatment of uterine cavity disease, but it required use of non-electrolyte glucose, mannitol, or sorbitol solution to distend the uterus. If the body absorbs too much uterine distention fluid during surgery, complications such as excessive circulating volume, hyponatremia, hyposmolarity, cerebral edema, and even death can occur [3]. With development of hysteroscopic surgical instruments, the electrode loops of hysteroscopic resection instruments have both working circuits and loop circuits, and plasma bipolar resection also uses normal saline as a uterine distension medium. This greatly improves the efficacy and safety, and provides a basis for clinical treatment of uterine cavity diseases. However, resection also has certain drawbacks. On the one hand, the electrothermal effect during resection can reduce the residual endometrial area and the secretion function of glands, which affects implantation of fertilized eggs. On the other hand, the air bubbles generated during the operation block the operative field of view, which also increases the possibility of complications such as uterine perforation and air embolism to a certain extent.
Compared with electrosurgery, hysteroscopic morcellation is accurate, effective, safe, and does not require hospitalization [4]. There is no scarring caused by thermal injury in hysteroscopic morcellation, which can maximize protection of the remaining normal endometrium and promote movement of the endometrium, thereby promoting recovery of the shape of the endometrium and uterine cavity. In addition, this surgical method can cut and suck polyp tissue at the same time, which not only reduces the formation of bubbles and the accumulation of excision tissue fragments, but also facilitates subsequent histological analysis [5,6]. However, hysteroscopic morcellation also has its own shortcomings – it is relatively difficult to perform when separating tough adhesion tissue, and it cannot quickly stop bleeding during separation.
These 2 treatment methods have clinical applications, but both of them have their own shortcomings. While studies have shown the feasibility of this new surgical approach, individual studies lack sufficient capacity to provide accurate estimates due to small sample sizes in terms of surgical success rate, duration of surgery, speed of surgery, and patient acceptability. In addition, the effectiveness and safety of the technology also need to be considered. At present, as the treatment of hysteroscopy is becoming more and more extensive, we should choose the most effective and safest treatment plan. Therefore, this study conducted systematic evaluation and meta-analysis of all eligible experimental studies collected in a quantitative way to compare the success rate (successful completion of the resection), surgical speed, and complications. This can provide more valid and credible evidence for the clinical selection of these 2 treatment options.
Material and Method
RETRIEVAL STRATEGY:
We performed a comprehensive systematic review and meta-analysis to evaluate the 2 surgical methods and searched PubMed, EMBASE, OVID, Medline, and BMJ. We employed the keywords “morcellator,” “morcellators,” “morcellate,” “morcellation,” and “morcellated” combined with “hysteroscopy,” “uteroscope,” and “transcervical”. The search was limited to English language publications. The last search was conducted on February 1, 2022.
DATA EXTRACTION:
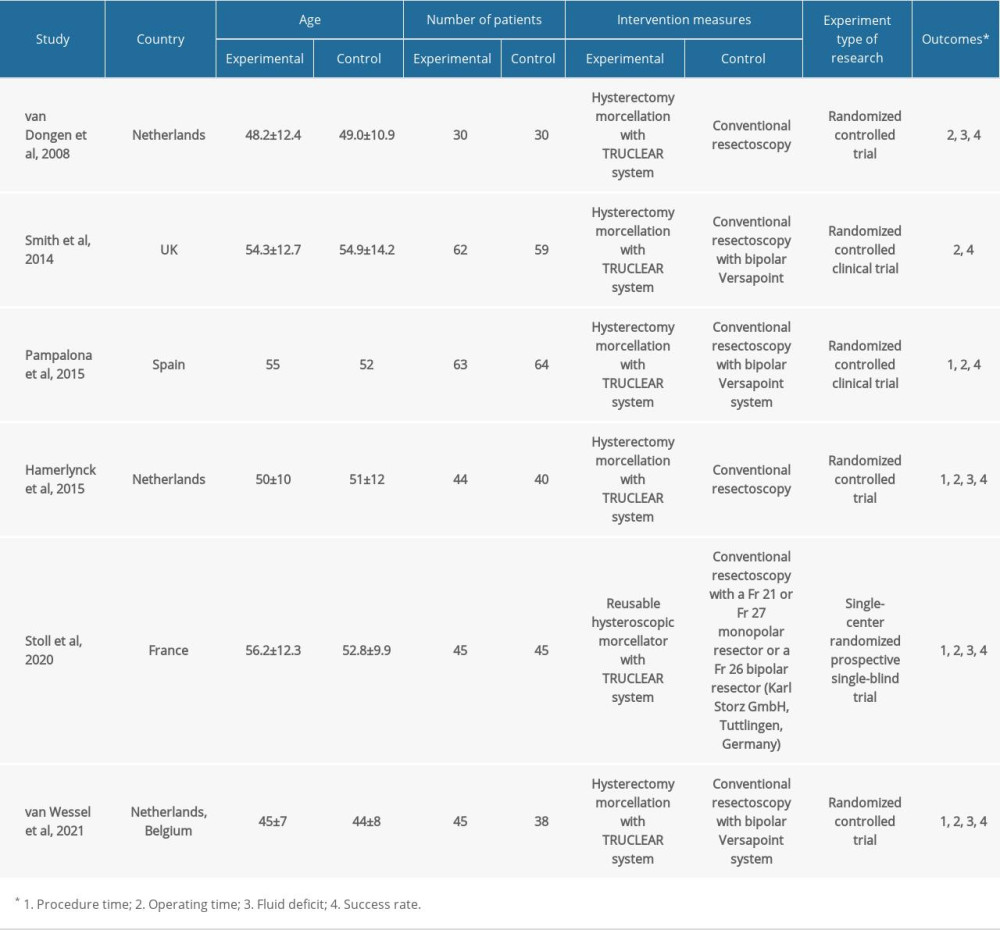
The data were extracted independently by 2 reviewers according to the prepared data sheet, and double-checked for review. The extracted data included the following aspects: (1) Basic information of the literature, including first author’s name, publication year, location of research object, research type, intervention measures, and research sample size; and (2) Measurement of outcome indicators, such as procedure time, operating time, fluid deficit, success rate.
LITERATURE QUALITY ASSESSMENT AND RISK ASSESSMENT:
In this study, 2 reviewers independently assessed the quality and risk of bias of the included RCTs according to the Cochrane Collaboration’s tool. Our assessment specifically included the following items: (1) Whether the grouping of subjects included in the study came from random assignment; (2) Whether allocation concealment was used before the subjects included in the study were allocated; (3) Whether the implementers and participants were double-blind, and whether the outcome measurers were blinded; (4) Whether the outcome data were complete; (5) Whether the included literature had selective reporting outcomes; and (6) Other biases.
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria of the literature were: (1) Research content: research literature on hysteroscopic electrosurgery and cold knife resection in the treatment of uterine cavity diseases; (2) Characteristics of included subjects: patients with uterine cavity disease who needed hysteroscopic treatment; (3) Study type: randomized controlled trials (RCTs) or case-control trials, whether blinded or not; (4) Evaluation indicators: to compare the differences in operation time, procedure time, fluid deficit, between the 2 treatments.
The exclusion criteria were: (1) Review and Meta literature; (2) The original data were incomplete, and supplementary data could not be obtained; (3) Duplicate articles in which the same experimental data were used in different articles.
STATISTICAL METHODS:
We used the
ETHICAL ISSUES:
This was a meta-analysis and did not involve any human or animal experiments, so there were no ethical issues involved. The studies we included all passed ethics review.
Results
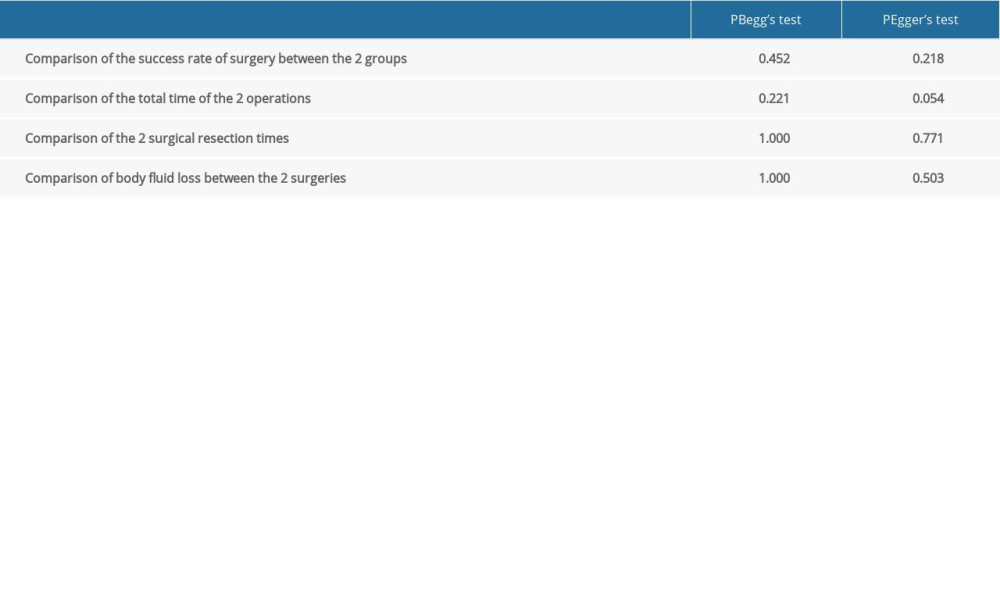
COMPARISON OF THE SUCCESS RATE OF SURGERY BETWEEN THE 2 GROUPS:
Heterogeneity testing showed I2=72.9% and P=0.002, so we combined the effect size using a random-effects model. Figure 2 is a comparison of the surgical success rates between the 2 groups, showing the overall RR value was 1.05 and the 95% CI was 0.97~1.13, so there was no significant difference in surgical success rates between the 2 groups (P=0.232). Sensitivity analysis showed that after excluding any one study, the combined effect size was consistent.
COMPARISON OF THE TOTAL TIME OF THE 2 OPERATIONS:
Through heterogeneity testing, we obtained the result of I2=9.8% and P=0.350, so the fixed-effects model was used to combine the effect size. Figure 3 shows the WMD value of the overall time of the 2 operations was −3.43, and the 95% CI was −4.63~−2.23. Therefore, the difference in the overall operation time between the 2 groups was statistically significant (P<0.001). The total operation time in the endoscopic group was 3.43 min shorter than in the traditional resection group. The results of sensitivity analysis showed that after excluding any one study, the combined effect size was consistent.
COMPARISON OF THE 2 SURGICAL RESECTION TIMES:
For the surgical resection time, the results of the heterogeneity test showed I2=0.0% and P=0.988, and we used a fixed-effects model to combine the effect sizes. As shown in Figure 4, the WMD value and the 95% CI of the 2 surgical resection times was −2.81(−4.08, −1.55), and the difference was statistically significant (P<0.001). The surgical resection time in the endoscopic group was 2.81 min shorter than in the traditional resection group. Sensitivity analysis after excluding any one study showed the combined effect size was consistent with the conclusion.
COMPARISON OF FLUID DEFICIT BETWEEN THE 2 SURGERIES:
The results of the heterogeneity test for fluid deficit showed I2=60.4% and P=0.08, so we used a random-effects model to combine the effect sizes. Figure 5 shows the WMD value and 95% CI of fluid deficit in the 2 operations were −141.41 (−361.95, 79.14) and P=0.209, and there was no statistically significant difference in fluid deficit between the 2 groups. Excluding any one study, the pooled effect size showed the conclusion was consistent.
PUBLICATION BIAS ANALYSIS AND PAPER QUALITY ASSESSMENT:
No publication bias was been found by Begg’s and Egger’s tests (Table 2). The results of quality evaluation are shown in Figure 6.
Discussion
In 2016, there was a meta-analysis that made a quantitative comparison between hysteroscopic morcellation and conventional resectoscopy [13], and its research results were different from our existing research. The results of our meta-analysis showed that there was no statistically significant difference in the surgical success rate between hysteroscopic morcellation and conventional resectoscopy in the management of endometrial lesions, and there was no statistically significant difference between the 2 in terms of body fluid deficit. This was quite different from previous studies [13]. As far as the 2 meta-analyses were concerned, our study included a comprehensive analysis of 565 patients by including 6 studies, while the previous study included only 382 patients, and the sample size was small [13]. Two new studies were added in our study (van Wessel et al 2021 [7] and Stoll et al 2021 [11]), which was more reliable than the conclusions of the previous studies.
The results of our meta-analysis showed that there was no statistical difference in the success rate of the 2 surgical approaches when treating endometrial lesions. As for hysteroscopic morcellation, the reasons for its failure were mainly based on the failure of entering the uterine cavity or the failure of complete resection due to the hardness of the fibroids, while the conventional resectoscopy was mainly due to the failure of complete resection of polyps or fibroids and the problem of insufficient visualization. In terms of surgical complications, both surgical approaches had complications. In fact, with the development of minimally invasive gynecological surgery, conventional resectoscopy of endometrial polyps has become the criterion standard for treatment, and its surgical success rate was also relatively high. For intrauterine tissue pulverization and suction technology, although the TRUCLEAN system overcame the problems of the electric cutting method, such as steam bubbles generated by electric heating of uterine dilatation fluid or excised tissue, and incomplete excision, which can lead to surgical failure, it has also created new problems that reduce the success rate of surgery, such as inability to enter the uterine cavity [14] and inability to use hysteroscopic morcellation for hard fibroids [2]. In terms of complications, life-threatening complications such as fluid overload, uterine perforation, and bleeding cannot be completely eliminated regardless of the surgical option, although these are uncommon with the use of hysteroscopic morcellation [15]. Therefore, this new technology is no better than the traditional resection in terms of surgical success rate in dealing with endometrial lesions.
Although our study did not find differences in the surgical success rate between this new surgical method and traditional electric resection, we found that hysteroscopic morcellation was associated with a shorter surgery in patients with endometrial lesions compared with conventional resectoscopy due to the following reasons. First, compared with traditional resectoscopy, the removal of intrauterine disease with hysteroscopic morcellation required less complicated operations. It can touch the lesion through a rotary cutting device, and then directly use the device to remove the corresponding tissue. There is no need to manually control the cutting of tissue by the cutting ring, as in traditional electrosurgery, mainly due to the lower number of hysteroscopic in and out of the uterus [6,16]. It can simultaneously cut and extract tissue from the uterine cavity directly under the hysteroscopic field of view [17], reducing time wasted by repeated insertion and removal of the hysteroscope to extract material through the endocervix during surgery [17]. It also reduced the damage to the uterus to a certain extent, which was more conducive to the subsequent recovery of the uterus.
Regarding fluid deficit, the absorption of dilatation fluid may increase with the prolongation of operation time [2], and compared with traditional electrosurgery, it was true that the hysteroscopic morcellation took less time during the operation, but we found no difference in fluid deficits between the 2 surgical approaches. On the one hand, with regard to the operation time, both procedures were related to abnormal intrauterine volume, and the larger the intrauterine lesion, the longer the time required, whether it was endometrial polyps or fibroids. On the other hand, although the use of the new technology has shortened the operation time to a certain extent, the shortened time may not cause statistical differences in the absorption of uterine distention fluid between patients with different surgical methods. Last but not least, there are many factors that affect the absorption of body fluids, not only the operation time [17], but also the intrauterine pressure, mean arterial pressure, the depth of myometrial penetration, and the size of the uterine cavity, which affect the absorption of body fluids [14]. However, these reasons have little to do with the choice of the 2 surgical methods. In summary, the difference in fluid deficit between the 2 methods was not statistically significant.
Hysteroscopic morcellation is a new surgical method. Compared with conventional resectoscopy, hysteroscopic morcellation has better accuracy, effectiveness, and safety [15]. Hysteroscopic morcellation will not cause electrical damage to the patient, no scar formation is caused by heat injury, can better protect the patient’s endometrium, can maximize the protection of the remaining normal endometrium and promote its movement, so as to promote the recovery of the endometrium and uterine cavity shape. This surgical method has fewer postoperative complications and better safety. Hysteroscopic morcellation does not rely on energy equipment, and the tissue can be sucked out quickly while crushing the tissue [15], so there the surgical field is not blocked during the separation of adhesive tissue, and the sucked out crushed tissue can be directly used for subsequent pathological examination [18]. In addition, under hysteroscopy, the field of vision is clear and the intimal vessels are clearly visible, so the separation process can effectively avoid the vessels during the operation, and there is little surgical trauma. Hysteroscopic surgery can not only completely preserve the patient’s reproductive function, but also improve the clinical treatment effect, reduce the incidence of adverse reactions, and improve the safety of clinical treatment. Compared with traditional electrosurgical resection, hysteroscopic morcellation requires a shorter learning time and it has a shorter learning curve [19].
Electrosurgical treatment has been used in clinical practice for a long time and its therapeutic effect is widely recognized, but its disadvantage is that its electrical and thermal conduction effect can easily damage the normal endometrial tissue around the lesion when the lesion is removed, and the electrothermal effect of electrosurgical technology on the endometrium is likely to cause re-adhesions [20]. When operating with electric instruments, low power and heat should be used, and the number of hysteroscopes inserted should be reduced as much as possible because burning causes more damage with heat transfer. In conventional resectoscopy, although the use of electrocautery can quickly stop bleeding, it is easy to generate air bubbles and eschar during the cutting process, which affects the surgical field of vision [21]. This technique can lead to potentially life-threatening complications such as excessive intravasation of distending fluid. Therefore, careful monitoring of the fluid is necessary to keep the balance in order to avoid fluid overload.
There are some shortcomings in this study. The individual indicators included in the studies were relatively heterogeneous and few articles were included. Further large-sample, multi-center, randomized, and prospective studies are needed to “increase” the calculation of the sample size and draw more positive conclusions to guide clinical decision making.
Conclusions
The removal of intrauterine disease with hysteroscopic morcellation requires less complex surgery than with conventional resectoscopy. In addition, it can directly attract the crushed tissue fragments in time, which can not only reduce the time of operation, but also avoid the crushed tissue blurring hysteroscopic vision. This reduces the damage to the uterus to a certain extent and is more conducive to the subsequent recovery of the uterus. Therefore, we need to have a more comprehensive grasp of surgical techniques and training in the use of new equipment.
Figures
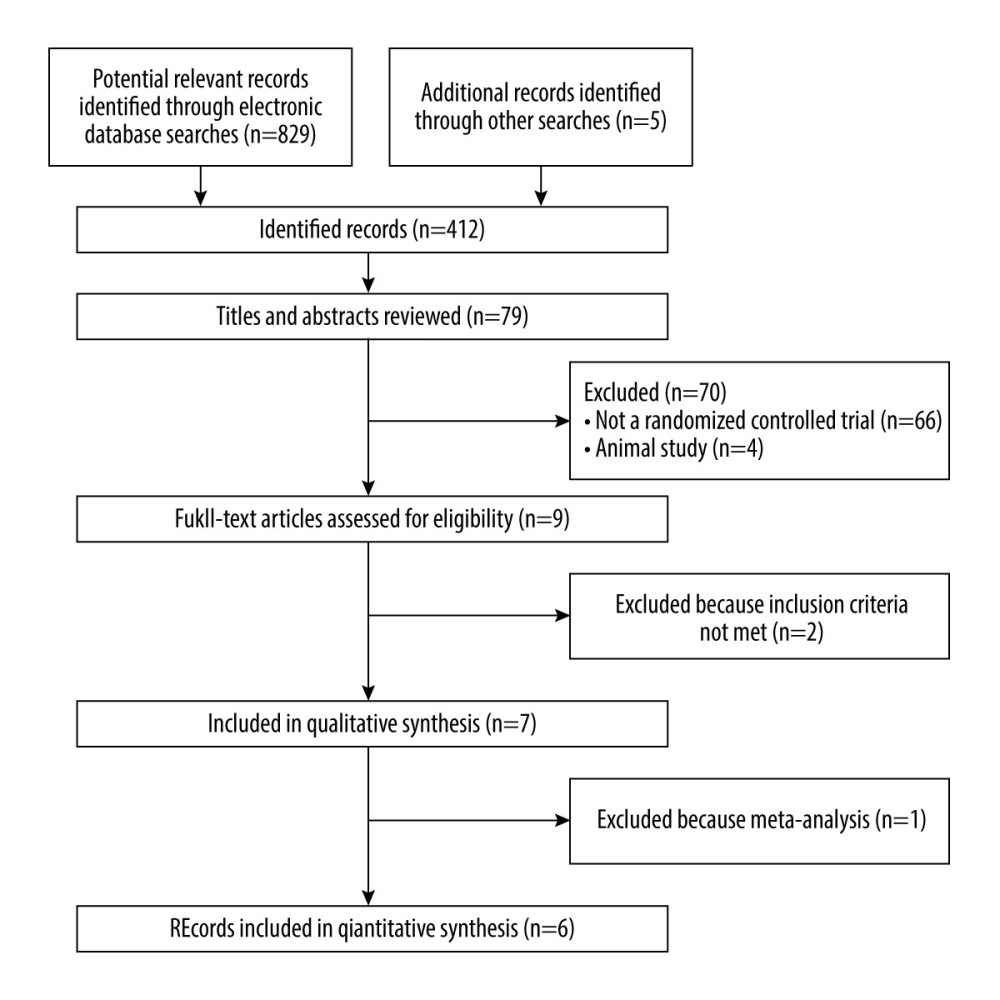 Figure 1. Document retrieval flow chart.
Figure 1. Document retrieval flow chart. 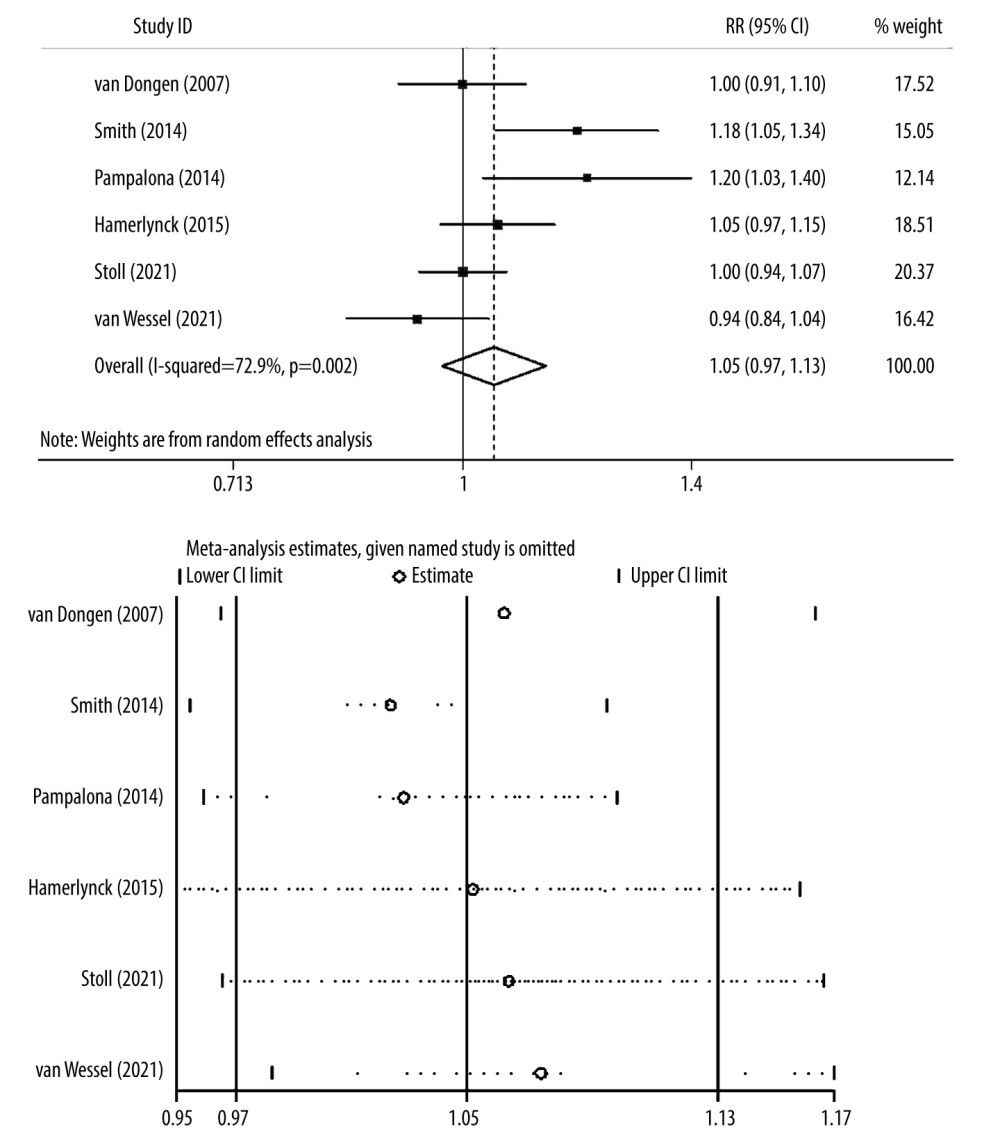 Figure 2. Forest plot and sensitivity analysis chart for the success rate of surgery between the 2 groups.
Figure 2. Forest plot and sensitivity analysis chart for the success rate of surgery between the 2 groups. 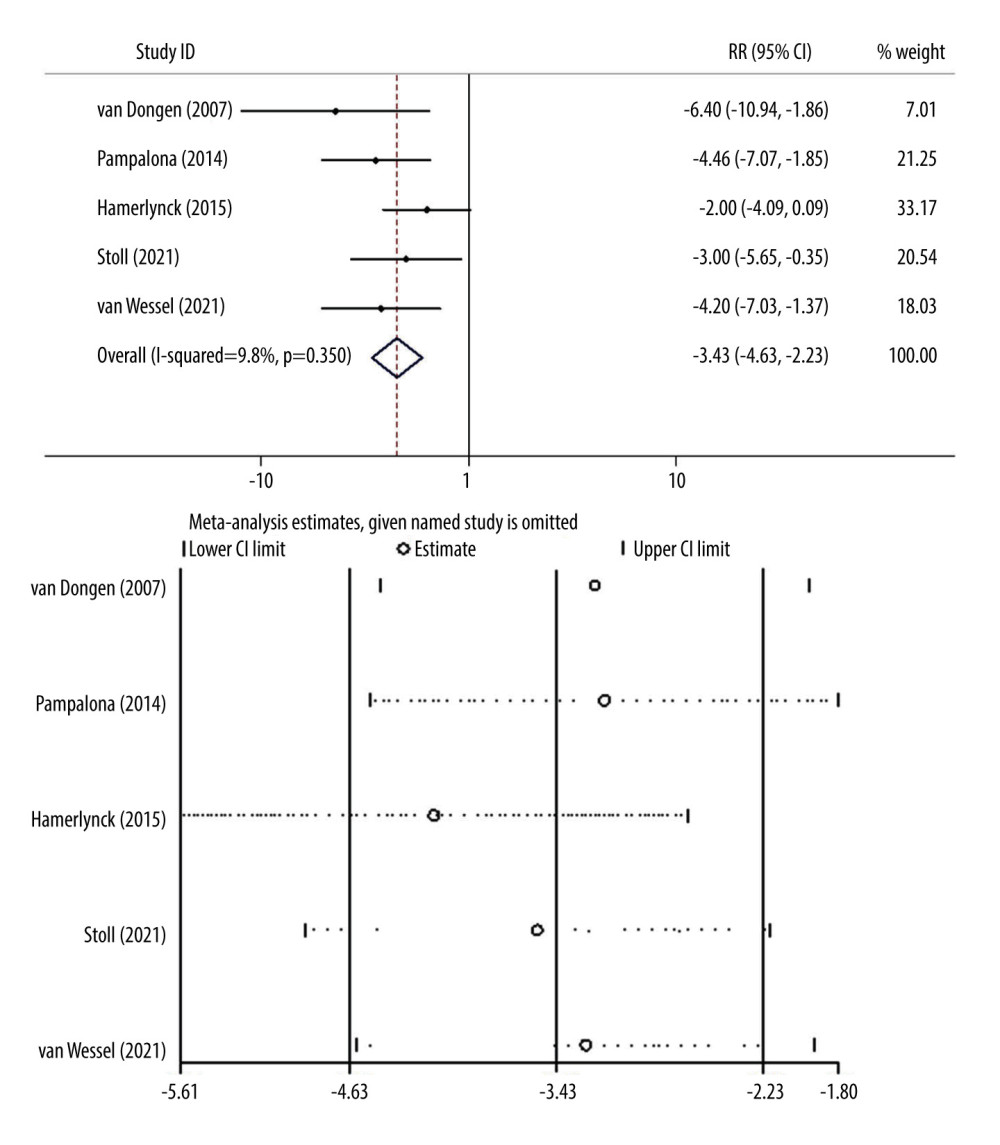 Figure 3. Forest plot and sensitivity analysis chart for the total time between the 2 groups.
Figure 3. Forest plot and sensitivity analysis chart for the total time between the 2 groups. 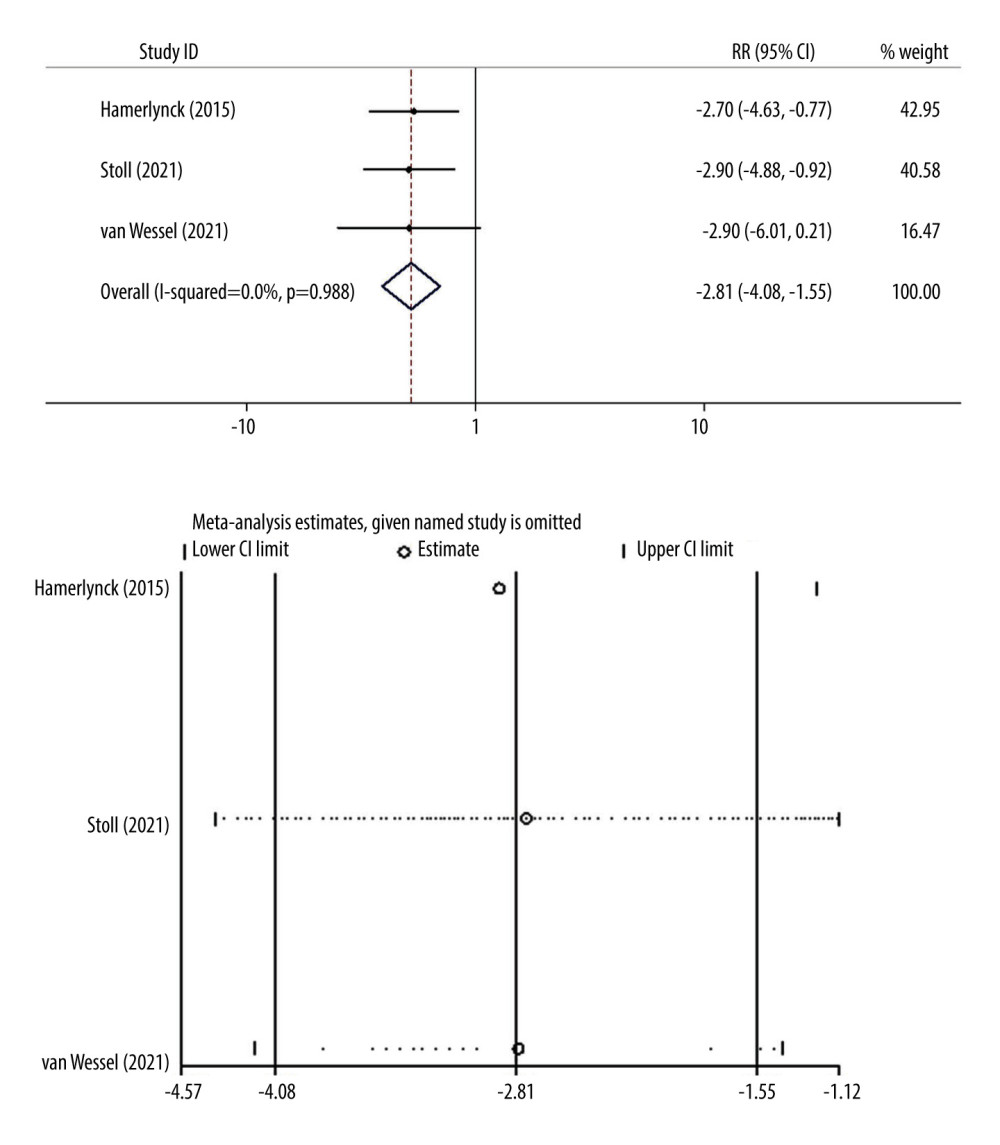 Figure 4. Forest plot and sensitivity analysis chart for the 2 surgical resection times.
Figure 4. Forest plot and sensitivity analysis chart for the 2 surgical resection times. 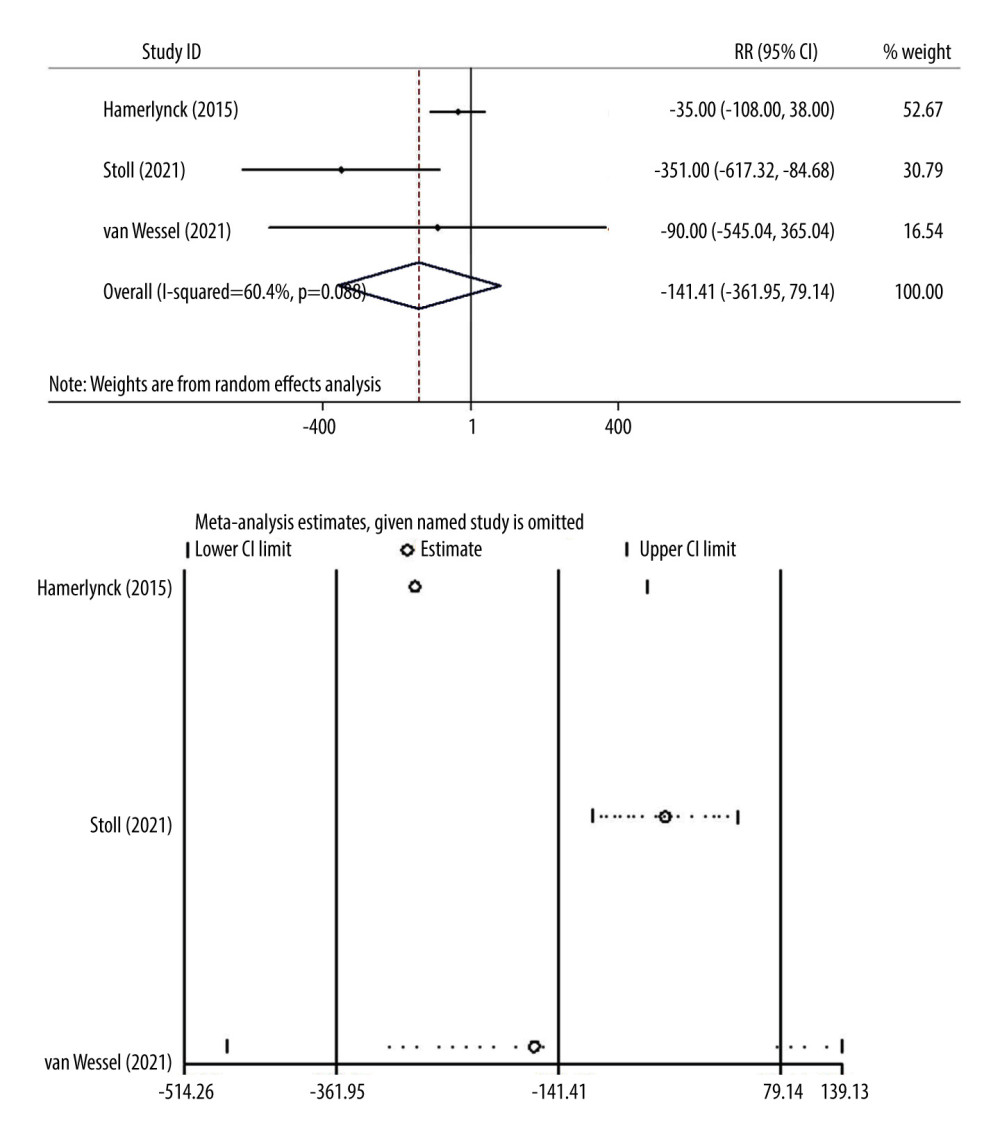 Figure 5. Forest plot and sensitivity analysis chart for the fluid deficit of surgery between the 2 groups.
Figure 5. Forest plot and sensitivity analysis chart for the fluid deficit of surgery between the 2 groups. 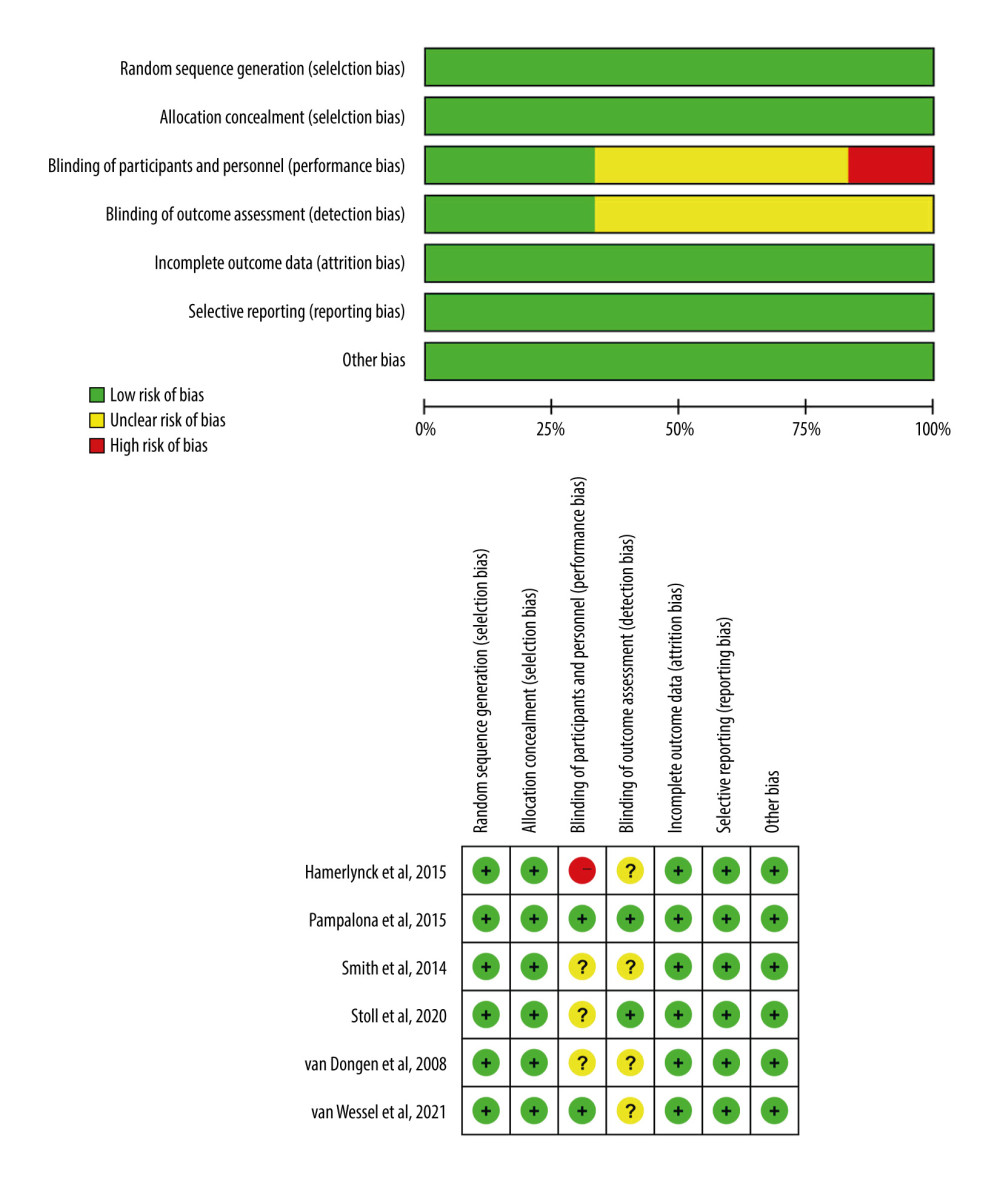 Figure 6. Summary of risk of bias for literature quality assessment.
Figure 6. Summary of risk of bias for literature quality assessment. References
1. Maheux-Lacroix S, Mennen J, Arnold A, The need for further surgical intervention following primary hysteroscopic morcellation of submucosal leiomyomas in women with abnormal uterine bleeding: Aust N Z J Obstet Gynaecol, 2018; 58(5); 570-75
2. Garbin O, Schwartz LNew in hysteroscopy: Hysteroscopic morcellators: Gynecol Obstet Fertil, 2014; 42(12); 872-76 [in French]
3. Cohen S, Greenberg JA, Hysteroscopic morcellation for treating intrauterine pathology: Rev Obstet Gynecol, 2011; 4(2); 73-80
4. Hamerlynck TWO, Blikkendaal MD, Schoot BC, An alternative approach for removal of placental remnants: Hysteroscopic morcellation: J Minim Invas Gyn, 2013; 20(6); 796-802
5. Meulenbroeks D, Hamerlynck TWO, Saglam-Kara S, Hysteroscopic tissue removal systems: A randomized in vitro comparison: J Minim Invas Gyn, 2017; 24(1); 159-64
6. Hamerlynck TW, van Vliet HA, Beerens AS, Hysteroscopic morcellation versus loop resection for removal of placental remnants: A randomized trial: J Minim Invasive Gynecol, 2016; 23(7); 1172-80
7. van Wessel S, van Vliet HAAM, Schoot BC, Hysteroscopic morcellation versus bipolar resection for removal of type 0 and 1 submucous myomas: A randomized trial: Eur J Obstet Gyn R B, 2021; 259; 32-37
8. Hamerlynck TWO, Schoot BC, van Vliet HAAM, Weyers S, Removal of endometrial polyps: Hysteroscopic morcellation versus bipolar resectoscopy, a randomized trial: J Minim Invas Gyn, 2015; 22(7); 1237-43
9. Pampalona JR, Bastos MD, Moreno GM, A comparison of hysteroscopic mechanical tissue removal with bipolar electrical resection for the management of endometrial polyps in an ambulatory care setting: Preliminary results: J Minim Invas Gyn, 2015; 22(3); 439-45
10. van Dongen H, Emanuel MH, Wolterbeek R, Hysteroscopic morcellator for removal of intrauterine polyps and myomas: A randomized controlled pilot study among residents in training: J Minim Invas Gyn, 2008; 15(4); 466-71
11. Stoll F, Lecointre L, Meyer N, Randomized study comparing a reusable morcellator with a resectoscope in the hysteroscopic treatment of uterine polyps: The RESMO study: J Minim Invas Gyn, 2021; 28(4); 801-10
12. Smith PP, Middleton LJ, Connor M, Clark TJ, Hysteroscopic morcellation compared with electrical resection of endometrial polyps: A randomized controlled trial: Obstet Gynecol, 2014; 123(4); 745-51
13. Li C, Dai Z, Gong Y, A systematic review and meta-analysis of randomized controlled trials comparing hysteroscopic morcellation with resectoscopy for patients with endometrial lesions: Int J Gynecol Obstet, 2017; 136(1); 6-12
14. Loddo A, Djokovic D, Drizi A, Hysteroscopic myomectomy: The guidelines of the International Society for Gynecologic Endoscopy (ISGE): Eur J Obstet Gyn R B, 2022; 268; 121-28
15. Haber K, Hawkins E, Levie M, Chudnoff S, Hysteroscopic morcellation: Review of the manufacturer and user facility device experience (MAUDE) database: J Minim Invas Gyn, 2015; 22(1); 110-14
16. Lee MMH, Matsuzono T, Hysteroscopic intrauterine morcellation of submucosal fibroids: Preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection: Hong Kong Med J, 2016; 22(1); 56-61
17. Tsuchiya A, Komatsu Y, Matsuyama R, Intraoperative and postoperative clinical evaluation of the hysteroscopic morcellator system for endometrial polypectomy: A prospective, randomized, single-blind, parallel group comparison study: Gynecol Minim Invasiv Ther, 2018; 7(1); 16-21
18. Hamidouche A, Vincienne M, Thubert THysteroscopic morcellation versus bipolar resection for endometrial polyp removal: Gynecol Obstet Fertil, 2015; 43(2); 104-8 [in French]
19. Noventa M, Ancona E, Quaranta M, Intrauterine morcellator devices: Reprod Sci, 2015; 22(10); 1289-96
20. Scheiber MD, Chen SH, A prospective multicenter registry of patients undergoing hysteroscopic morcellation of uterine polyps and myomas: J Gynecol Surg, 2016; 32(6); 318-23
21. Emanuel MH, New developments in hysteroscopy: Best Pract Res Clin Obstet Gynaecol, 2013; 27(3); 421-29
Figures
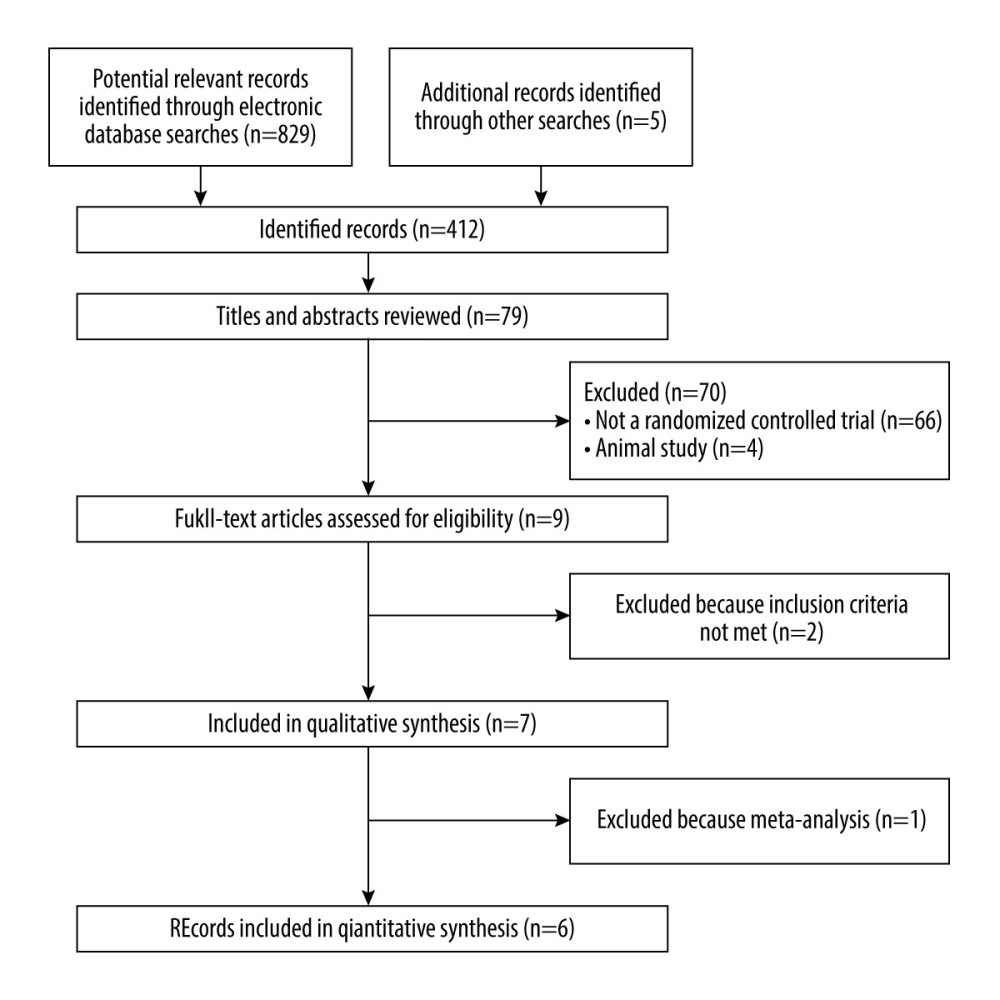 Figure 1. Document retrieval flow chart.
Figure 1. Document retrieval flow chart.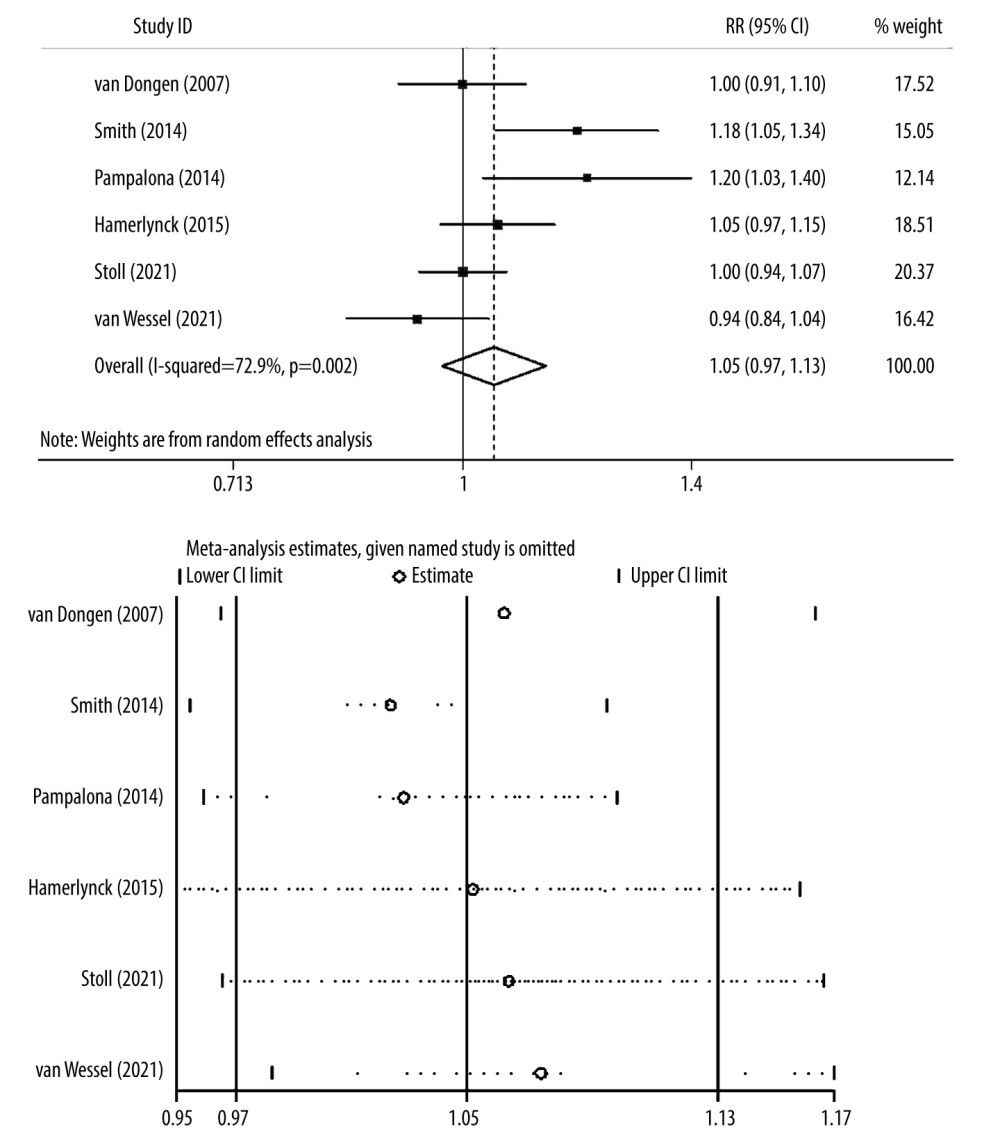 Figure 2. Forest plot and sensitivity analysis chart for the success rate of surgery between the 2 groups.
Figure 2. Forest plot and sensitivity analysis chart for the success rate of surgery between the 2 groups.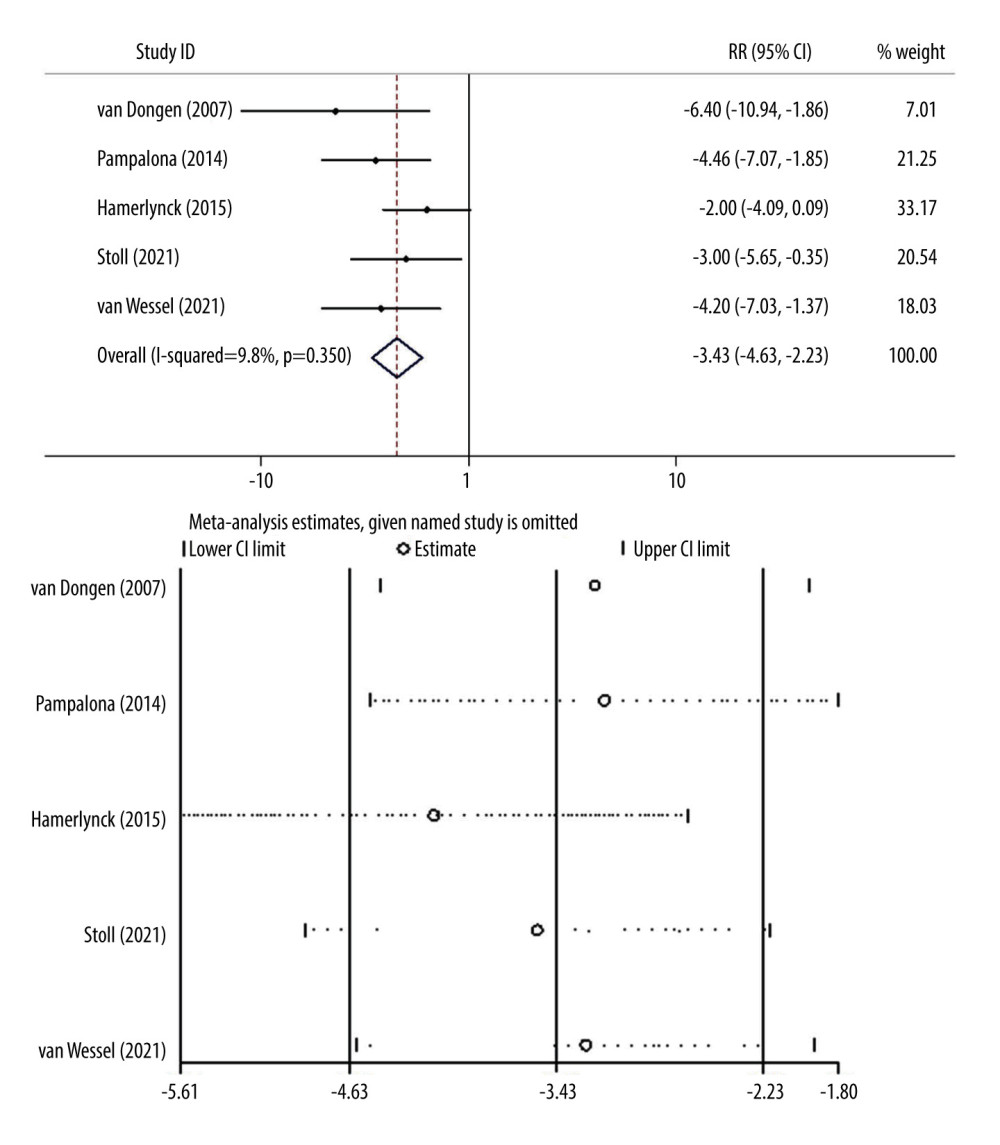 Figure 3. Forest plot and sensitivity analysis chart for the total time between the 2 groups.
Figure 3. Forest plot and sensitivity analysis chart for the total time between the 2 groups.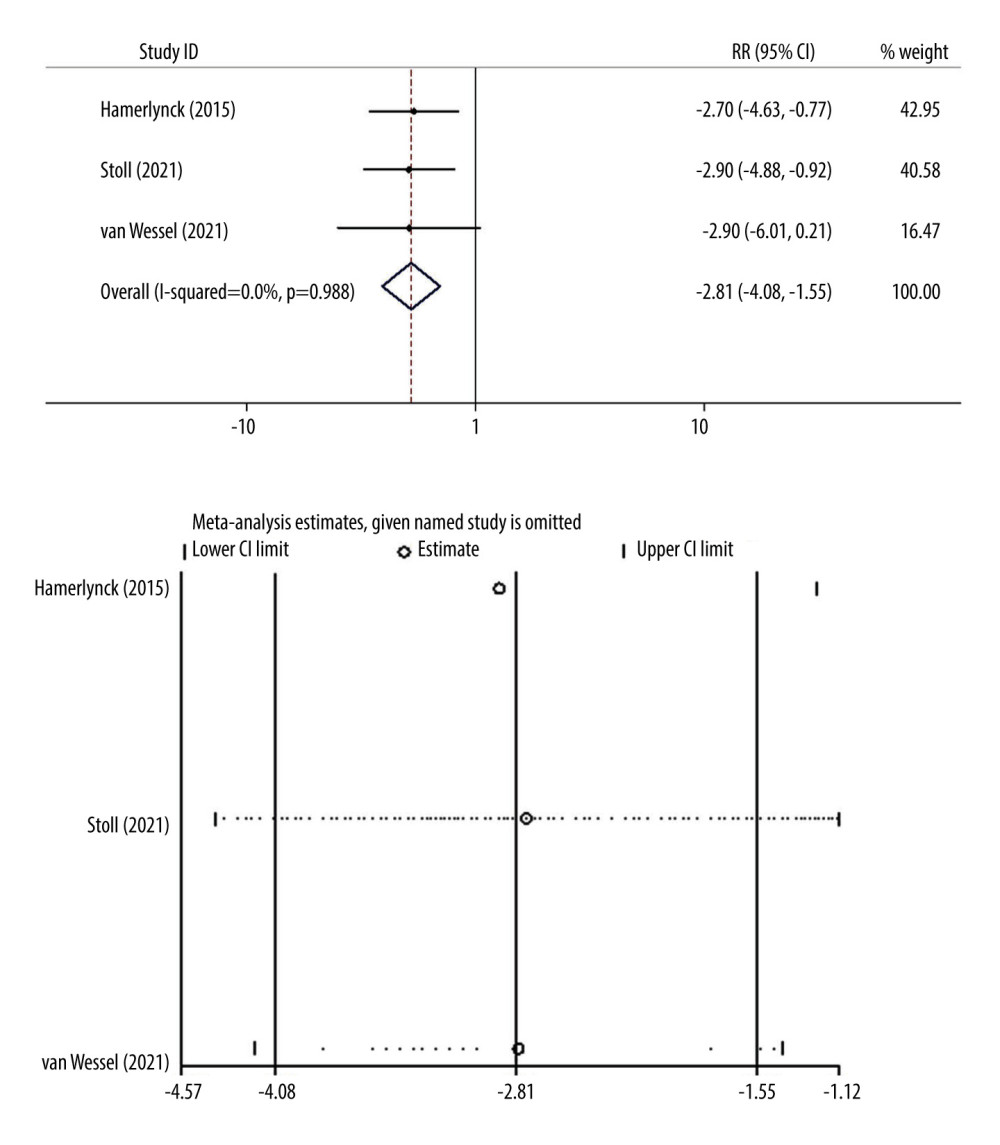 Figure 4. Forest plot and sensitivity analysis chart for the 2 surgical resection times.
Figure 4. Forest plot and sensitivity analysis chart for the 2 surgical resection times.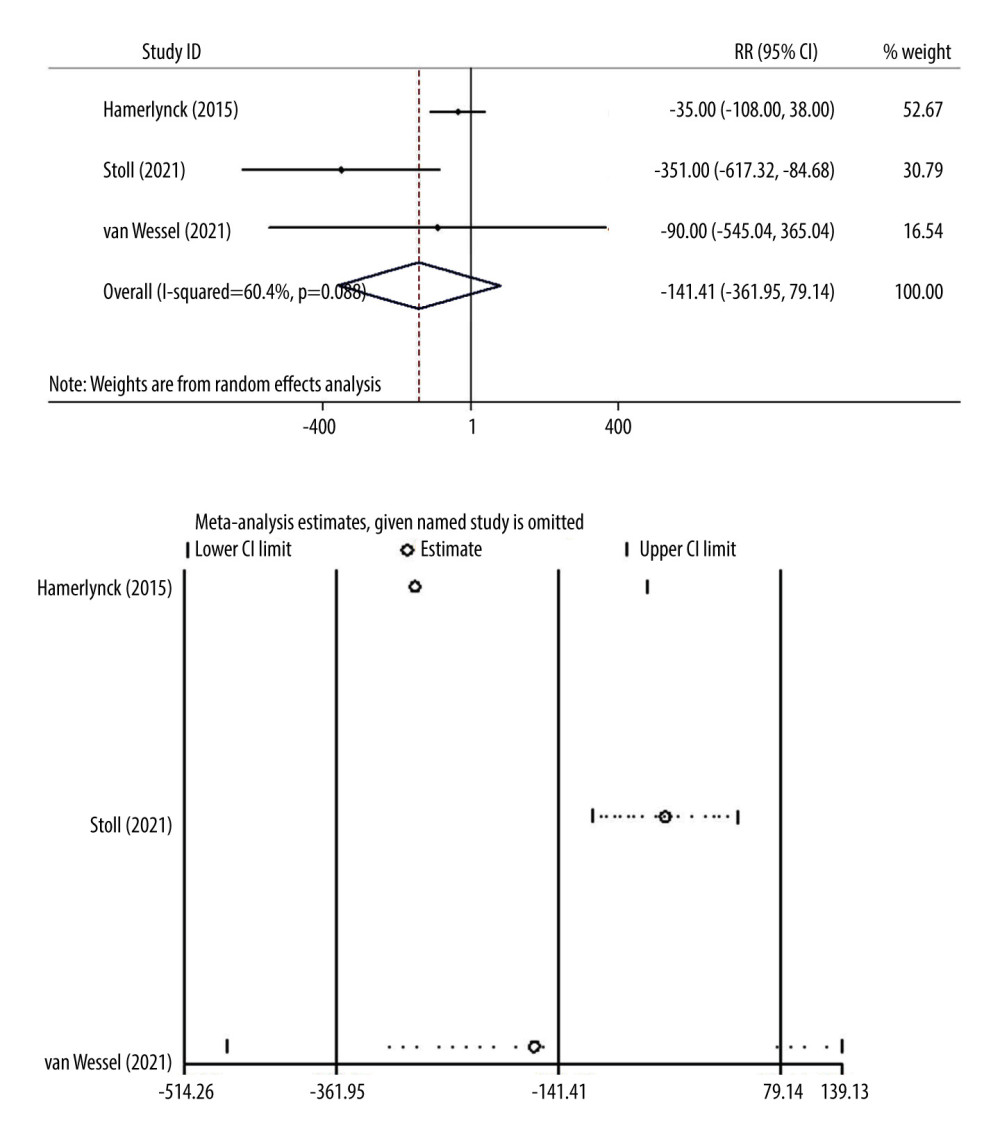 Figure 5. Forest plot and sensitivity analysis chart for the fluid deficit of surgery between the 2 groups.
Figure 5. Forest plot and sensitivity analysis chart for the fluid deficit of surgery between the 2 groups.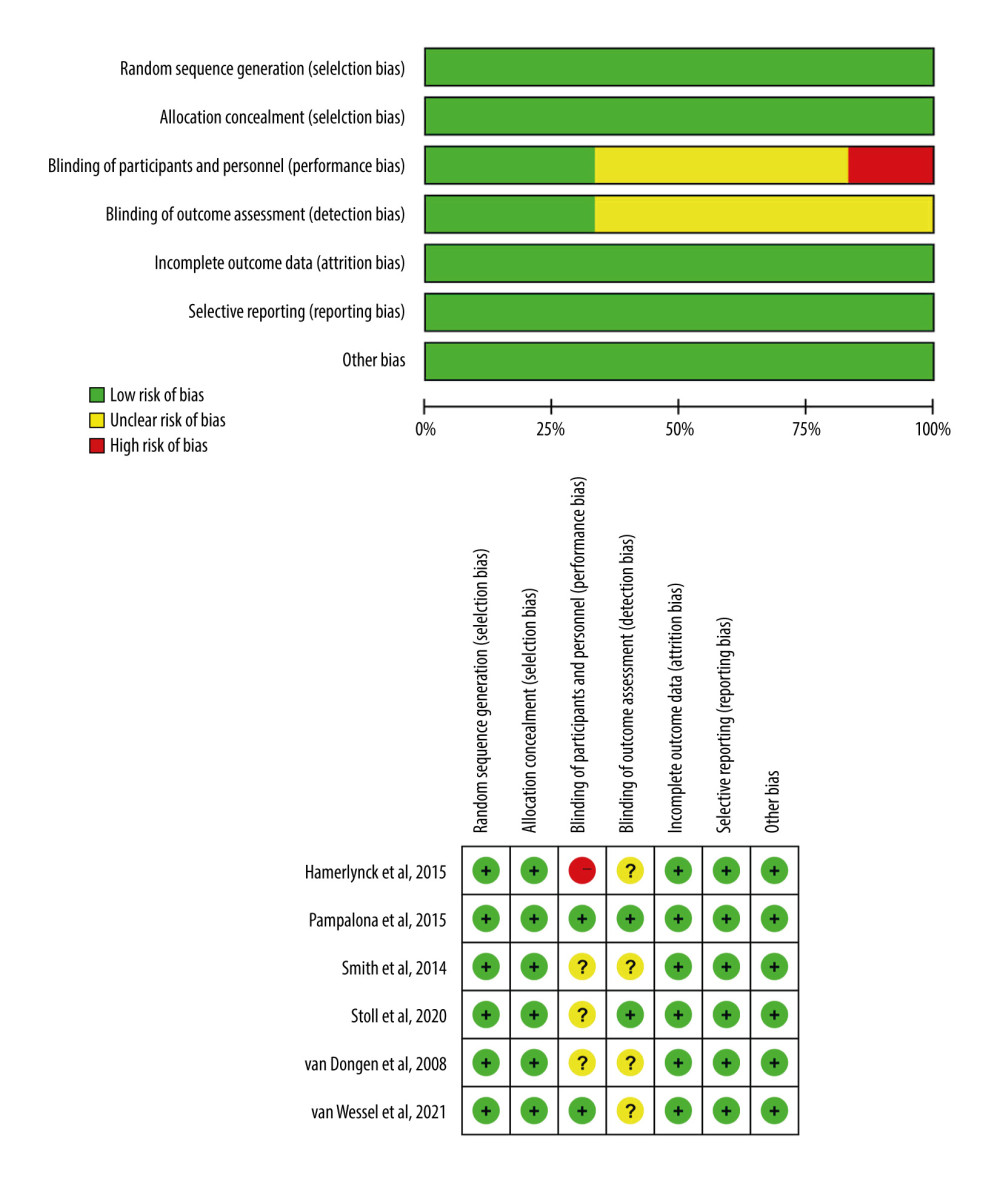 Figure 6. Summary of risk of bias for literature quality assessment.
Figure 6. Summary of risk of bias for literature quality assessment. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952