20 April 2023: Clinical Research
Low Prealbumin Levels Were Associated with Increased Frequency of Hepatic Encephalopathy in Hepatitis B Virus (HBV)-Related Decompensated Cirrhosis
Jiani Li12ABCDEFG, Minghao Du2EF, Hao Li1CEF, Peng Wu3CD, Mengying Sun12CDE, Min Guan12CEF, Shanhong Tang12A*DOI: 10.12659/MSM.937772
Med Sci Monit 2023; 29:e937772
Abstract
BACKGROUND: The role of nutritional parameter prealbumin in predicting the incidence of hepatic encephalopathy (HE) remains unclear. This study was designed to assess the diagnostic performance of prealbumin in predicting the incidence of HE in hepatitis B virus (HBV)-related decompensated liver cirrhosis patients.
MATERIAL AND METHODS: A retrospective cohort of 262 patients with HBV-related decompensated liver cirrhosis was involved in this study. Prealbumin, albumin, and other indicators were collected at admission, and independent factors were identified by logistic regression analysis. The Mann-Whitney U test and receiver operating characteristic (ROC) curves were used to compare the groups and indicators.
RESULTS: A total of 262 patients were enrolled in the study, including 197 men and 65 women. In patients with HBV-related decompensated liver cirrhosis accompanied by HE, the model for end-stage liver disease (MELD) scores, and prothrombin time (PT) and international normalized ratio (INR) values were significantly increased, while prealbumin and albumin levels were significantly decreased. Multivariate analysis showed that only serum prealbumin level (P=0.014) was independently related to the incidence of HE. Moreover, prealbumin level was negatively correlated with MELD (r=-0.63, P<0.001) and Child-Turcotte-Pugh (r=-0.35, P<0.001) scores. ROC curves were performed, and prealbumin showed the highest area under the ROC curve (0.781) compared with MELD and Child-Turcotte-Pugh scores.
CONCLUSIONS: Low prealbumin levels were associated with increased frequency of hepatic encephalopathy in HBV-related decompensated cirrhosis, which showed better performance than traditional models.
Keywords: hepatic encephalopathy, Liver Cirrhosis, Prealbumin, Male, Humans, Female, Hepatitis B virus, Retrospective Studies, End stage liver disease, Severity of Illness Index, Albumins, ROC Curve, Prognosis
Background
Liver cirrhosis is a global health burden with high morbidity and mortality, and many measures have been performed to solve this problem [1]. Hepatic encephalopathy (HE) is one of the most common and serious complications of liver cirrhosis, with a high mortality risk of 35% to 94% [2]. Currently, HE is mainly diagnosed by clinical symptoms, blood ammonia concentration, and imaging, which have poor specificity and sensitivity. Therefore, simple and accurate markers are urgently needed to improve the diagnosis and monitoring of HE.
Liver function loss and abnormal shunting are the main causes of HE. Patients with end-stage liver disease often have malnutrition due to insufficient liver synthesis. Malnutrition is a common complication of liver cirrhosis, is an independent predictor of poor prognosis in cirrhotic patients, and is associated with liver failure, infection, HE, and ascites. The prevalence of sarcopenia in patients with liver cirrhosis is about 40% to 70%, which is similar to the incidence of HE, and the occurrence of HE is closely related to cirrhotic sarcopenia [3]. Recent research showed that sarcopenia and muscle lipid metabolism were both risk factors for HE [4,5]. Serum albumin is the most objectively applicable nutritional index, but it is unsuitable to represent the instant liver function owing to its long half-life [6]. To assess the severity of liver function, Child-Turcotte-Pugh (CTP) and model for end-stage liver disease (MELD) scores are commonly used [7,8]. Compared with serum albumin, prealbumin is an indicator with a shorter half-life and faster synthesis speed, which has certain value in evaluating liver function and nutritional status [9,10]. As a precursor of albumin, prealbumin is hardly affected by exogenous supplements [11]. Recent research showed that prealbumin was associated with liver cirrhosis, hepatocellular carcinoma, and other disease [12–15]. However, the role of prealbumin in predicting the incidence of HE has not been reported.
This study was a single-center retrospective study designed to assess the diagnostic performance of prealbumin, CTP, and MELD scores in predicting the incidence of HE in patients with HBV-related decompensated liver cirrhosis (HBV-DeCi).
Material and Methods
STUDY DESIGN:
A total of 339 adults with HBV-DeCi (≥18 years old) involved in this study were hospitalized in the General Hospital of Western Theater Command from January 2014 to August 2019. A total of 262 patients were ultimately enrolled. Decompensated liver cirrhosis was identified by the Guidelines for Diagnosis and Treatment of Liver Cirrhosis 2019, which states that based on liver cirrhosis there are complications of portal hypertension, such as ascites, esophageal gastric varices bleeding, sepsis, hepatic encephalopathy, and hepatorenal syndrome [16]. Diagnosis of HE was confirmed by qualified physicians using standard criteria previously described when the patients were admitted [17]. Participants who had any of the following conditions were excluded; (i) above 70 years old; (ii) malignancies, such as hepatocellular carcinoma; (iii) pregnancy; (iv) incomplete data; (v) simultaneous hepatitis C virus infection, hepatitis D virus infection, HIV infection, or other liver disease; (vi) chronic diseases such as chronic kidney disease, chronic obstructive pulmonary disease, congestive heart failure, and malignant tumors other than hepatocellular carcinoma; and (vii) lost to follow-up for 3 months. All patients received antiviral therapy and standard care as recommended by the guideline. All laboratory examinations were performed according to an established laboratory routine. Prealbumin level was determined by immunoturbidimetry. The MELD score was calculated as: R=3.78×ln (total bilirubin, mg/dL)+11.2×ln (international normalized ratio [INR])+9.57×ln (creatinine, mg/dL)+6.43.
This study was approved by the Ethics Committee of the General Hospital of Western Theatre Command (2020ky032). All procedures were in accordance with the guidelines of the 1975 Declaration of Helsinki. As the study was retrospective, informed consent was not required.
STATISTICAL ANALYSIS:
All statistical analyses were performed using SPSS 23.0 and GraphPad Prism 8. Distribution was verified by the Kolmogorov-Smirnov test. Comparisons of categorical data were done using the χ2 test. Group comparisons were done using the
Results
COHORT DESCRIPTION:
After applying the exclusion criteria, a total of 262 patients were enrolled in the study. Of these patients, 75.2% (197/262) were men, and 24.8% (65/262) were women. The average age was 52.09±10.94 years. Of the 262 patients evaluated, the median MELD score was 10.79±4.65; patients were divided into CTP-A (93/262, 35.5%), CTP-B (124/262, 47.3%), and CTP-C (45/262, 17.2%) groups.
DIAGNOSTIC PERFORMANCE OF PREALBUMIN IN PREDICTING THE INCIDENCE OF HE:
The biochemical characteristics of patients with HBV-DeCi with or without HE is shown in Table 1. As demonstrated in the table, INR and MELD were significantly higher in patients with HE. Prealbumin and albumin levels were significantly lower in patients with HE, which meant that patients with lower prealbumin and albumin were more likely to have HE. In HBV-DeCi patients with HE, the MELD, prothrombin time, and INR values were significantly increased, while prealbumin and albumin were significantly decreased. No differences were observed in sex and age between patients with and without HE. To determine the risk factors for HE in patients with HBV-DeCi, we performed logistic regression analysis, as shown in Table 2. According to the univariate analysis, MELD (OR 1.126, [95% CI 1.032, 1.229], P=0.008), prealbumin (OR 0.975, [95% CI 0.961, 0.989], P=0.001), total bilirubin (OR 1.008, [95% CI 1.002, 1.014], P=0.014), prothrombin time (OR 1.302, [95% CI 1.102, 1.538], P=0.002), and INR (OR 17.192, [95% CI 2.898, 101.993], P=0.002) values were associated with the incidence of HE in HBV-DeCi patients. Multivariate analysis showed that only serum prealbumin level (OR 0.978, [95% CI 0.962, 0.995], P=0.014) was independently related to the incidence of HE in HBV-DeCi patients. To assess the diagnostic performance of prealbumin, ROC curves were performed, and prealbumin had the highest AUC (0.781) compared with MELD and CTP scores (Figure 1). Additionally, the sensitivity, specificity, and AUCs are showed in Table 3. Applying the cut-off value of 82.6 mg/L, the sensitivity and specificity were 0.900 and 0.521, respectively. Of the 3 parameters, prealbumin had the highest sensitivity at 0.900, and the highest specificity was 0.595, for CTP score.
PREALBUMIN WAS NEGATIVELY CORRELATED WITH MELD AND CTP SCORES:
Additionally, a significantly lower average prealbumin level (P<0.001) was present in the patients graded CTP-C (82.61 mg/L) compared with those graded CTP-A (95.46 mg/L) and CTP-B (87.90 mg/L), as shown in Figure 2. The patients were divided into 2 groups based on the MELD cut-off value of 10.94. The prealbumin level in patients with MELD >10.94 was significantly lower than that of those with MELD <10.94 (P<0.0001). As shown in Figure 3, prealbumin was significantly negative correlated with MELD score (r=−0.35, P<0.001) and CTP score (r=−0.63, P<0.001). It could be inferred that prealbumin was closely linked to the severity of liver cirrhosis.
Discussion
In this study, we found the serum prealbumin level was negatively correlated with the incidence of HE in patients with HBV-DeCi. Prealbumin was significantly decreased in HBV-DeCi patients with HE, and was negatively correlated with traditional score models, including MELD and CTP. Moreover, univariate and multivariate analysis showed that only serum prealbumin level was independently related to the incidence of HE and the predictive utility of prealbumin was better than that of MELD or CTP scores.
Generally, the main physiological mechanism of HE is hyperammonemia [18]. In the case of liver cirrhosis and liver dysfunction, liver metabolism of NH3 is impaired. When portal hypertension exists and transjugular intrahepatic portosystemic shunt is conducted, NH3 is shunted into the systemic circulation without detoxification, which in turn leads to brain dysfunction and HE [19]. It has been suggested that ammonia can interfere with protein remodeling itself to cause sarcopenia in patients with liver cirrhosis, thereby creating a vicious circle, in which sarcopenia will promote HE and hyperammonemia, and hyperammonemia will further aggravate sarcopenia [20]. Malnutrition is associated with the survival rate and complications in liver cirrhosis [21]. In addition, weakness is a common complication of liver cirrhosis, especially in patients with ascites or HE, and it is also an independent factor of pre-transplant mortality [4,22] As reported before, muscle lipid metabolism and muscle loss in patients with liver cirrhosis are independently associated with HE. The quality and quantity of muscle are both important risk factors for HE [23]. Protein malnutrition is especially important in this relationship.
Prealbumin is one of the most widely used parameters for monitoring and evaluating malnutrition [24]. Also, prealbumin is closely related to sarcopenia, and higher body mass index and prealbumin levels can be protective factors for sarcopenia [25]. In addition, compared with albumin, prealbumin is a more sensitive predictor of liver synthesis and the short-term prognosis of the osteoporosis [24,26]. At the same time, the theory of inflammatory mediators and the role of other toxic substances have also received increasing attention [27]. Generally, the most common cause of HE is infection, including abdominal cavity, intestinal, urinary tract, and respiratory tract infections. It can be seen from previous research that prealbumin is a negative acute phase protein because its synthesis is suppressed in the inflammatory setting, in which cytokines stimulate hepatic production of acute-phase proteins [26]. Therefore, prealbumin may serve as a comprehensive marker of inflammation and malnutrition. Our previous studies have shown that prealbumin was significantly negatively correlated with the MELD score. During the golden window period, prealbumin is independently related to the prognosis of acute on chronic liver failure. Therefore, prealbumin can be used as a simple indicator of liver function in patients with acute on chronic liver failure [28]. Because prealbumin can reflect nutritional status well, we believed that it could be used as a quantitative variable to evaluate the nutritional status of patients. Huang et al reported that postoperative liver function insufficiency is associated with advanced age and lower serum prealbumin level. A serum prealbumin level <170 mg/dL is still a predictor of liver function insufficiency after hepatectomy [12]. However, in these studies, prealbumin was considered to be a marker of prognosis, rather than a marker of the incidence of complications. It is now known that both HE and prealbumin are independently related to the nutritional status of liver cirrhosis patients with sarcopenia, and whether prealbumin is related to the incidence of HE in HBV-DeCi patients has not been reported. It must be mentioned that there are few studies on prealbumin and decompensated liver cirrhosis. Significant differences in prealbumin level were found in the CTP classification. Prealbumin has been found to have potential clinical value for HE, which is consistent with our research results [29].
In this study, serum prealbumin was not only an independent predictor of HE, but also showed a strong ability to predict risk. A previous study explored the CTP score as the most widely used model to evaluate liver function in patients with cirrhosis. We extended their data to clarify the relationship between prealbumin and CTP and MELD scores in patients with HE [30]. We excluded patients with hepatocellular carcinoma, other causes of liver disease, and pre-terminal comorbidities. However, due to a lack of utility and specificity, there is no generally accepted cut-off value for serum prealbumin. Our study confirmed that prealbumin level can effectively distinguish between HBV-DeCi with or without HE. Our results showed that the frequency of HE should be considered, especially when the prealbumin level is lower than 82.60. In addition, the indicators assessing liver function including MELD and CTP are not directly related to the causes of HE (eg, infection, sarcopenia, ammonia). Therefore, as an indicator of nutritional status and hepatic synthesis, serum prealbumin requires adequate attention.
There were some limitations that could not be avoided in our research. First, this was a retrospective study and it was difficult to avoid biases. Second, a single center may be affected by institutional issues, which will affect the external validity of the research. Third, in this study, we were unable to determine the relationship between the cumulative incidence of HE and the dynamic change of prealbumin. Further research is needed to determine whether the dynamic changes of prealbumin can be used as a predictor of the subsequent incidence of HE in patients with HBV-DeCi.
Conclusions
In brief, we determined that serum prealbumin levels were decreased during the deterioration of liver cirrhosis, and serum prealbumin levels might help predict the incidence of HE in patients with HBV-DeCi. Measuring serum prealbumin levels could facilitate decision making regarding prophylaxis, treatment, and surveillance intervals, ultimately improving the management of patients with HBV-DeCi.
Figures
![Receiver operating characteristic curves (ROC) for prealbumin, model for end-stage liver disease (MELD), and Child-Turcotte-Pugh (CTP) scores in predicting incidence of hepatic encephalopathy in patients with HBV-related decompensated liver cirrhosis. (Using the SPSS 23.0 software [IBM Corp, Armonk, NY, USA]).](https://jours.isi-science.com/imageXml.php?i=medscimonit-29-e937772-g001.jpg&idArt=937772&w=1000) Figure 1. Receiver operating characteristic curves (ROC) for prealbumin, model for end-stage liver disease (MELD), and Child-Turcotte-Pugh (CTP) scores in predicting incidence of hepatic encephalopathy in patients with HBV-related decompensated liver cirrhosis. (Using the SPSS 23.0 software [IBM Corp, Armonk, NY, USA]).
Figure 1. Receiver operating characteristic curves (ROC) for prealbumin, model for end-stage liver disease (MELD), and Child-Turcotte-Pugh (CTP) scores in predicting incidence of hepatic encephalopathy in patients with HBV-related decompensated liver cirrhosis. (Using the SPSS 23.0 software [IBM Corp, Armonk, NY, USA]). ![Serum prealbumin level among groups in sub-classification of (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).](https://jours.isi-science.com/imageXml.php?i=medscimonit-29-e937772-g002.jpg&idArt=937772&w=1000) Figure 2. Serum prealbumin level among groups in sub-classification of (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).
Figure 2. Serum prealbumin level among groups in sub-classification of (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]). ![Negative correlation between prealbumin and traditional score models including (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).](https://jours.isi-science.com/imageXml.php?i=medscimonit-29-e937772-g003.jpg&idArt=937772&w=1000) Figure 3. Negative correlation between prealbumin and traditional score models including (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).
Figure 3. Negative correlation between prealbumin and traditional score models including (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]). Tables
Table 1. Clinical characteristics of patients HBV-related decompensated liver cirrhosis with or without hepatic encephalopathy at admission. Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP).
Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP).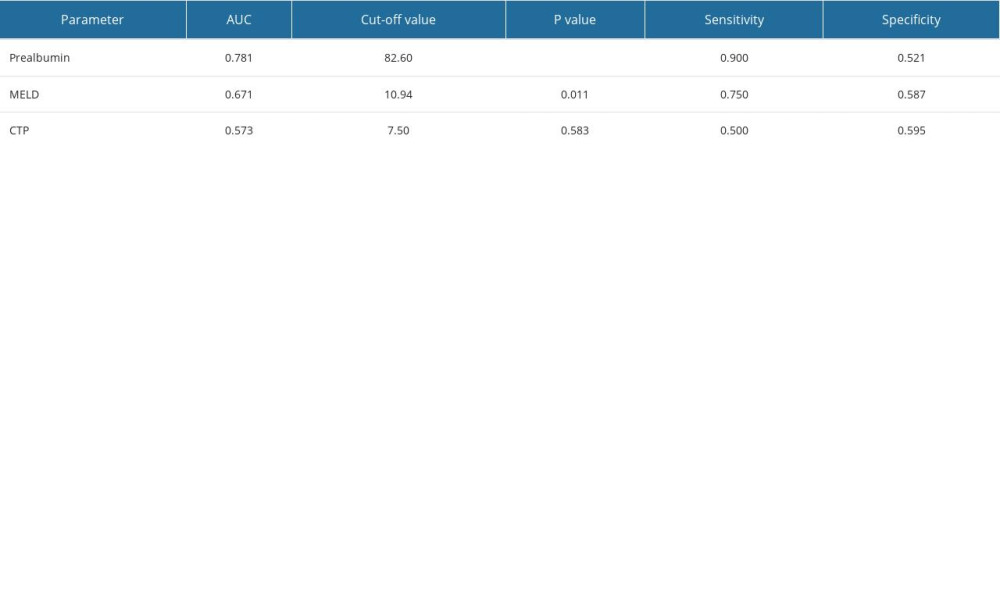 Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy.
Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy.
References
1. Mokdad AA, Lopez AD, Shahraz S, Liver cirrhosis mortality in 187 countries between 1980 and 2010. A systematic analysis: BMC Med, 2014; 12; 145
2. Jepsen P, Ott P, Andersen PK, Clinical course of alcoholic liver cirrhosis: A Danish population-based cohort study: Hepatology, 2010; 51(5); 1675-82
3. Kim G, Kang SH, Kim MY, Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis: PLoS One, 2017; 12(10); e0186990
4. Fallahzadeh MA, Rahimi RS, Hepatic encephalopathy and nutrition influences: A narrative review: Nutr Clin Pract, 2020; 35(1); 36-48
5. Nardelli S, Lattanzi B, Merli M, muscle alterations are associated with minimal and overt hepatic encephalopathy in patients with liver cirrhosis: Hepatology, 2019; 70(5); 1704-13
6. Lin MY, Liu WY, Tolan AM, Aboulian A, Preoperative serum albumin but not prealbumin is an excellent predictor of postoperative complications and mortality in patients with gastrointestinal cancer: Am Surg, 2011; 77(10); 1286-89
7. Pugh RN, Murray-Lyon IM, Dawson JL, Transection of the oesophagus for bleeding oesophageal varices: Br J Surg, 1973; 60(8); 646-49
8. Kamath PS, Wiesner RH, Malinchoc M, A model to predict survival in patients with end-stage liver disease: Hepatology, 2001; 33(2); 464-70
9. Saito M, Seo Y, Yano Y, Short-term reductions in non-protein respiratory quotient and prealbumin can be associated with the long-term deterioration of liver function after transcatheter arterial chemoembolization in patients with hepatocellular carcinoma: J Gastroenterol, 2012; 47(6); 704-14
10. Liu F, Cai LY, Zhong L, Model for end-stage liver disease combined with serum prealbumin to predict the prognosis of patients with decompensated liver cirrhosis: J Dig Dis, 2010; 11(6); 352-57
11. Dellière S, Cynober L, Is transthyretin a good marker of nutritional status?: Clin Nutr, 2017; 36(2); 364-70
12. Liao YY, Teng CL, Peng NF, Serum prealbumin is negatively associated with survival in hepatocellular carcinoma patients after hepatic resection: J Cancer, 2019; 10(13); 3006-11
13. Huang L, Li J, Yan JJ, Prealbumin is predictive for postoperative liver insufficiency in patients undergoing liver resection: World J Gastroentero, 2012; 18(47); 7021-25
14. Huo RR, Liu HT, Deng ZJ, Dose-response between serum prealbumin and all-cause mortality after hepatectomy in patients with hepatocellular carcinoma: Front Oncol, 2021; 10; 596691
15. Liu F, Cai LY, Zhong L, Model for end-stage liver disease combined with serum prealbumin to predict the prognosis of patients with decompensated liver cirrhosis: J Dig Dis, 2010; 11(6); 352-57
16. Chinese guidelines on the management of liver cirrhosis: Zhonghua Gan Zang Bing Za Zhi, 2019; 27(11); 846-65 [in Chinese]
17. Xu XY, Ding HG, Li WGChinese Society of Hepatology, Chinese Medical Association, Chinese guidelines on management of hepatic encephalopathy in cirrhosis: World J Gastroenterol, 2019; 25(36); 5403-22
18. Romero-Gómez M, Montagnese S, Jalan R, Hepatic encephalopathy in patients with acute decompensation of cirrhosis and acute-on-chronic liver failure: J Hepatol, 2015; 62(2); 437-47
19. Wijdicks EF, Hepatic encephalopathy: N Engl J Med, 2016; 375(17); 1660-70
20. Dasarathy S, Merli M, Sarcopenia from mechanism to diagnosis and treatment in liver disease: J Hepatol, 2016; 65(6); 1232-44
21. Child CG, Turcotte JG, Surgery and portal hypertension: Major Probl Clin Surg, 1964; 1; 1-85
22. Lai JC, Rahimi RS, Verna EC, Frailty associated with waitlist mortality independent of ascites and hepatic encephalopathy in a multicenter study: Gastroenterology, 2019; 156(6); 1675-82
23. Bhanji RA, Moctezuma-Velazquez C, Duarte-Rojo A, Myosteatosis and sarcopenia are associated with hepatic encephalopathy in patients with cirrhosis: Hepatol Int, 2018; 12(4); 377-86
24. Li XS, Zhang JR, Zhao YL, Reduced prealbumin is associated with bone mineral density in women with osteoporosis: Nutrition, 2017; 33; 338-32
25. Chen Q, Hao Q, Ding Y, Dong B, The association between sarcopenia and prealbumin levels among elderly Chinese inpatients: J Nutr Health Aging, 2019; 23(2); 122-27
26. Beck FK, Rosenthal TC, Prealbumin: A marker for nutritional evaluation: Am Fam Physician, 2002; 65(8); 1575-78 [Erratum in: Am Fam Physician 2002;66(12):2208]
27. Aldridge DR, Tranah EJ, Shawcross DL, Pathogenesis of hepatic encephalopathy: Role of ammonia and systemic inflammation: J Clin Exp Hepatol, 2015; 5(Suppl 1); S7-S20
28. Wang X, Tang S, Yang D, The value of prealbumin changes in the evaluation of liver function in acute-on-chronic liver failure: Medical Journal of National Defending Forces in Southwest China, 2019; 29(7); 760-62
29. Ampuero J, Montoliú C, Simón-Talero M, Minimal hepatic encephalopathy identifies patients at risk of faster cirrhosis progression: J Gastroenterol Hepatol, 2018; 33(3); 718-25
30. Djiambou-Nganjeu H, Hepatic encephalopathy in liver cirrhosis: J Transl Int Med, 2017; 5(1); 64-67
Figures
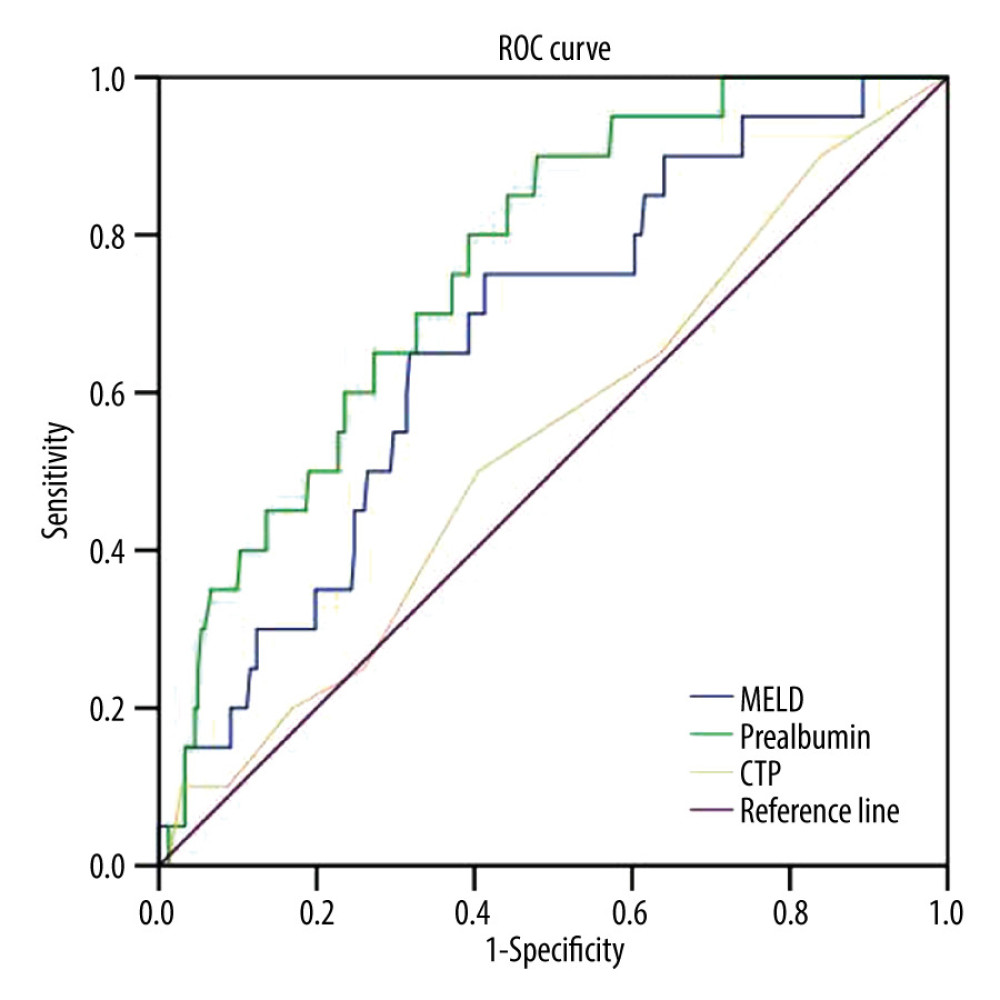 Figure 1. Receiver operating characteristic curves (ROC) for prealbumin, model for end-stage liver disease (MELD), and Child-Turcotte-Pugh (CTP) scores in predicting incidence of hepatic encephalopathy in patients with HBV-related decompensated liver cirrhosis. (Using the SPSS 23.0 software [IBM Corp, Armonk, NY, USA]).
Figure 1. Receiver operating characteristic curves (ROC) for prealbumin, model for end-stage liver disease (MELD), and Child-Turcotte-Pugh (CTP) scores in predicting incidence of hepatic encephalopathy in patients with HBV-related decompensated liver cirrhosis. (Using the SPSS 23.0 software [IBM Corp, Armonk, NY, USA]).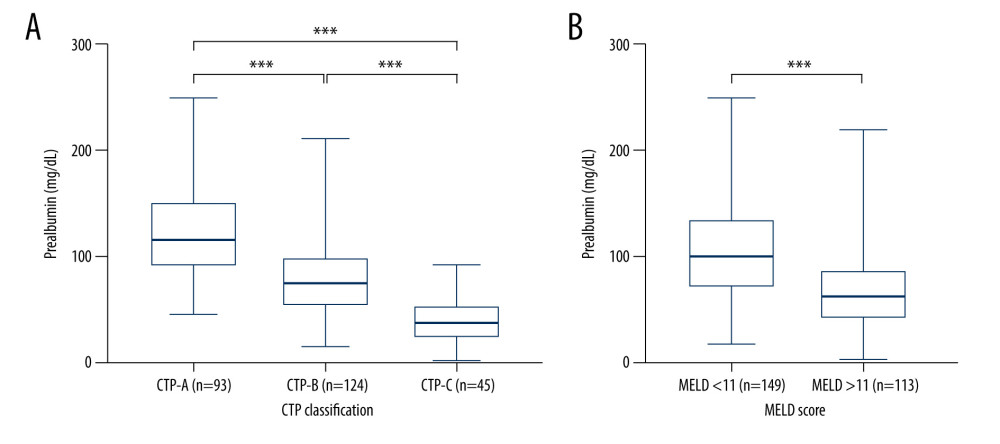 Figure 2. Serum prealbumin level among groups in sub-classification of (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).
Figure 2. Serum prealbumin level among groups in sub-classification of (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).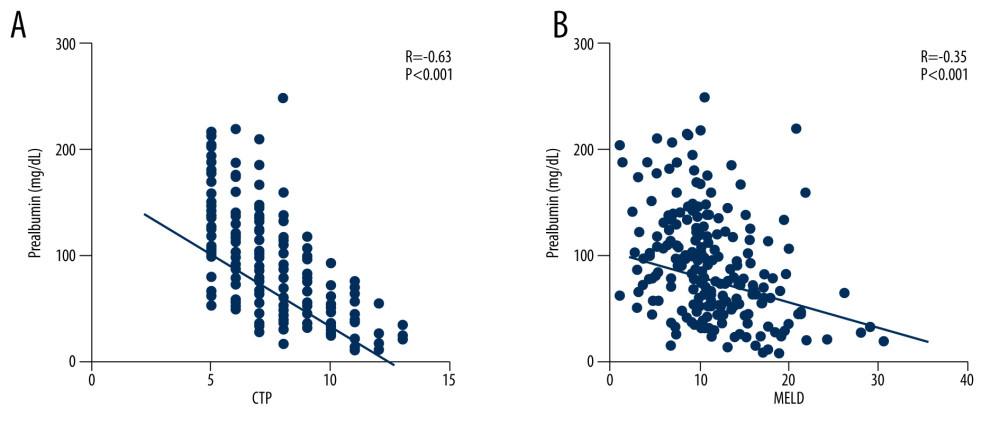 Figure 3. Negative correlation between prealbumin and traditional score models including (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]).
Figure 3. Negative correlation between prealbumin and traditional score models including (A) Child-Turcotte-Pugh (CTP) and (B) model for end-stage liver disease (MELD) scores. (Using Prism 8 software [GraphPad Software Inc.]). Tables
 Table 1. Clinical characteristics of patients HBV-related decompensated liver cirrhosis with or without hepatic encephalopathy at admission.
Table 1. Clinical characteristics of patients HBV-related decompensated liver cirrhosis with or without hepatic encephalopathy at admission.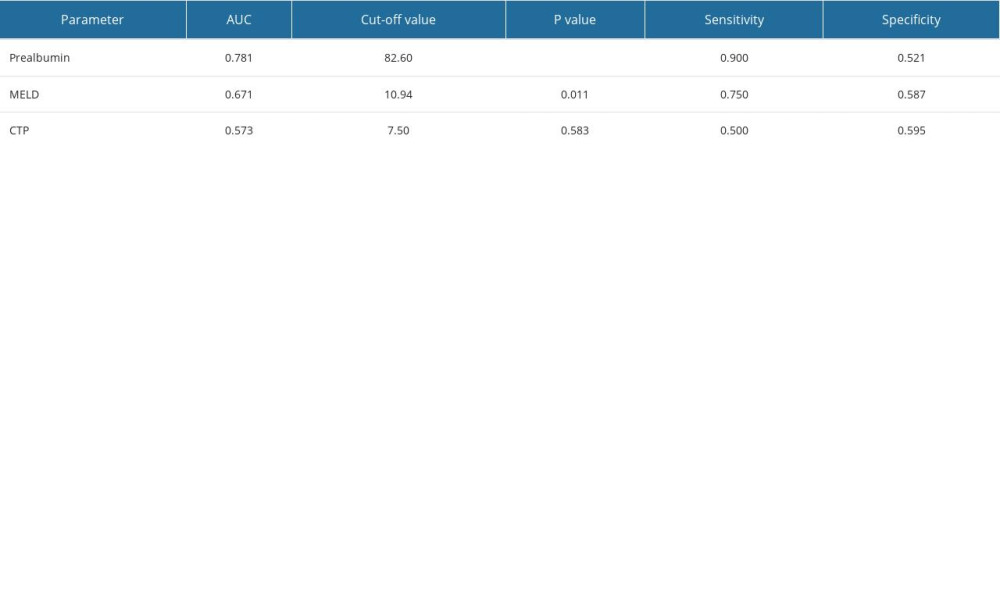 Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP).
Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP). Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy.
Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy. Table 1. Clinical characteristics of patients HBV-related decompensated liver cirrhosis with or without hepatic encephalopathy at admission.
Table 1. Clinical characteristics of patients HBV-related decompensated liver cirrhosis with or without hepatic encephalopathy at admission.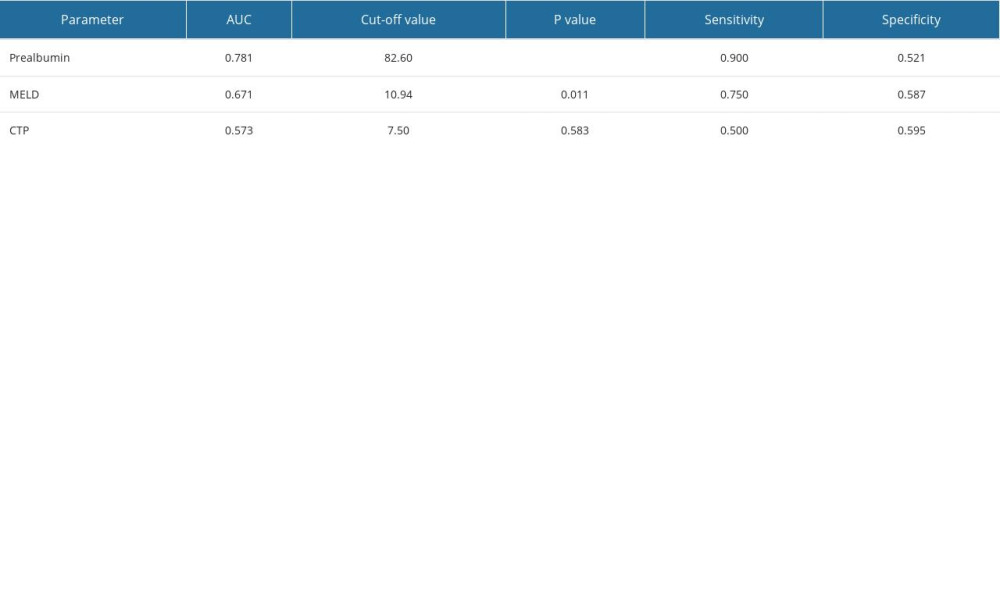 Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP).
Table 2. Area under the receiver operating characteristic curve (AUC) analysis of prealbumin, model for end-stage liver disease (MELD) and Child-Turcotte-Pugh (CTP). Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy.
Table 3. Univariate and multivariate analysis to identify potential predictors of hepatic encephalopathy. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








