12 October 2022: Review Articles
Effects of Physiotherapy on Rehabilitation and Quality of Life in Patients Hospitalized for COVID-19: A Review of Findings from Key Studies Published 2020–2022
Samire Beqaj12ABCDEF*, Amra Mačak Hadžiomerović1ABEF, Arzija Pašalić1DEF, Amila Jaganjac1DEFDOI: 10.12659/MSM.938141
Med Sci Monit 2022; 28:e938141
Abstract
ABSTRACT: The estimated percentage of individuals with COVID-19 due to infection with SARS-CoV-2 in need of hospitalization mostly increases proportionally with age, reaching almost 10% for those older than 60 years. Among hospitalized patients, one-fifth require treatment in the intensive care unit (ICU) due to acute respiratory distress syndrome, multiorgan failure, or hypoxemic respiratory insufficiency. Patients with moderate and severe COVID-19 who were hospitalized during the early stages of the pandemic and who continue to be hospitalized report fatigue, muscle weakness, joint stiffness, reduced mobility, increased risk of falls, and impaired quality of life. Physiotherapy is recognized to be important in the rehabilitation of COVID-19 patients requiring hospitalization. The current physiotherapy guidelines and recommendations for individuals with COVID-19, which include treatment methods and outcome measures for evaluation of the effects on respiratory and physical function and quality of life, are those established from the pre-COVID-19 era. The available extant scientific literature mainly reported the effect of physiotherapy in patients with COVID-19 in the acute, hospitalization courses of the disease, while there is a lack of quality primary, experimental studies on the effects of physiotherapy in rehabilitation of post-COVID-19 patients after hospitalization. This review aims to present an update on the effects of physiotherapy on rehabilitation and quality of life in patients hospitalized for COVID-19 and the findings from key studies published between 2020 and 2022.
Keywords: COVID-19, Physical Therapy Modalities, Rehabilitation, review, SARS-CoV-2, Hospitalization, Humans, Middle Aged, Quality of Life
Background
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) is a new coronavirus that appeared in year 2019 and causes coronavirus disease 2019 (COVID-19) [1]. The World Health Organization declared the COVID-19 epidemic a global health emergency on January 30, 2020 [2]. Shortly afterwards, on March 11, 2020, COVID-19 was declared a global pandemic, the first declaration since the H1N1 flu pandemic in 2009 [1].
The incidence of new COVID-19 cases continues to rise, with over 581 million cases confirmed worldwide [3]. Clinical presentation of the disease is often reported to be flu-like with a mild respiratory tract infection including fever (89%), cough (68%), fatigue (38%), sputum production (34%), and/or difficulty breathing (19%). Some patients require additional oxygen and have variable clinical outcomes after antiretroviral treatment [4,5].
Existing reports estimate that 80% of cases are asymptomatic or mild; 15% are serious (infection with need for oxygen), and 5% are critical (with requirement of ventilation and life support) [1]. The estimated percentage of infected individuals in need of hospitalization mostly varies by age, starting from 0.4% for those younger than 40 years to 9.2% for those older than 60 years [6]. Among hospitalized patients, 20% require treatment in the intensive care unit (ICU), often due to acute respiratory distress syndrome [7]. These patients can also experience multiorgan failure [8] and hypoxemic respiratory insufficiency [1].
Patients in the ICU may develop several complications due to prolonged immobilization and many hours spent lying down [9], including neuromuscular complications, muscle weakness and fatigue, joint stiffness, dysphagia, psychological problems, decreased mobility, severely impaired quality of life, frequent falls, and even quadriparesis [10]. Immobilization, joint pain, and stiffness have also been observed in elderly patients with moderate to severe COVID-19 and in younger adults with critical forms of the disease [11].
The Global Rehabilitation Alliance considers rehabilitation an integral part of the response to the COVID-19 pandemic [12]. Vitacca et al (2020) classify respiratory rehabilitation into 3 groups of patients with COVID-19: the first in the acute phase, when critical respiratory impairment is present (emergency service, first aid, ICU); the second in the acute phase where there is severe respiratory damage (department of internal medicine, respiratory, infectious diseases or other departments); and the third in the post-acute phase (other units, subacute wards) [13]. According to Lew et al [14], complications caused by COVID-19 can be reduced by providing interdisciplinary rehabilitation that begins early and continues during the hospital stay, providing education to patients/families on self-care after discharge from hospital rehabilitation in acute or subacute wards, and continuous rehabilitation care in outpatient and home settings through either in-person therapy or telehealth.
In the current literature, 2 points of view regarding COVID-19 respiratory rehabilitation were observed. The first is based on principles of early respiratory rehabilitation, including mobilization and psychological support to be initiated during the acute phase of the disease. From another point of view, based on the experiences of countries that faced severe COVID-19 early in the pandemic and experienced a crisis in rehabilitation services, such as China and Italy, early respiratory rehabilitation is not recommended for critically ill patients during the possible progressive deterioration [15].
Dasgupta et al [16] draws attention to the observation that previous “members of the same family” of coronavirus (Severe Acute Respiratory Syndrome - SARS and Middle-East Respiratory Syndrome - MERS), which have caused 2 major epidemics in the past, although much smaller, resulted in long-term consequences of cardiopulmonary, glucometabolic and neuropsychiatric complications. Therefore, it is considered necessary to prepare the health system for such challenges that may arise after the end of the acute phase of the disease [17]. According to Halpin et al [17], early mobilization and exercise with the active participation of a physiotherapist are vital after hospitalization.
It is evident that in the extant scientific literature there is a lack of quality primary, experimental studies on the effects of physiotherapy in rehabilitation of patients with COVID-19 [18]. The recent literature reported the effect of physiotherapy in patients with COVID-19 in all courses of the disease, ie, in settings of inpatient intensive and non-intensive units, as well as outpatient or home care, with most studies focusing on the acute, hospitalization phase of COVID-19 patients [19]. One recently published review study which focused on post-COVID-19 patients discharged from hospital examined the outcome of exercise training on functional and psychological changes [20]. This review aims to present an update on the effects of physiotherapy on rehabilitation and quality of life in patients hospitalized for COVID-19 and the findings from key studies published between 2020 and 2022.
Main Methods used in Physiotherapy
Based on the physical impairment and difficulty physiotherapeutic interventions can be applied for treatment and prevention purposes which mainly include education and advice, mobility and exercise, and manual therapy [21]. It was demonstrated that experienced physiotherapists frequently approach patients’ problems by providing information about their condition, taking into account their perceptions, educating them on proper posture and movement, as well as self-management and problem-solving strategies [22].
Therapeutic exercise programs include movement prescribed for maintenance of physical fitness and health, correction of impairment, or improvement/re-establishment of musculoskeletal function. Such therapeutic exercises include aerobic, resistance, flexibility, and neuromotor exercise training [23,24].
Impairments related to mobility restrictions resulting from restorative limitations in joint motion are treatable by manual therapy, which encompasses joint-specific techniques for restoration of normal joint motion [25]. According to the recommendations for physiotherapy in patients with COVID-19 developed by the Royal Dutch Society for Physical Therapy (KNGF) [26], physiotherapeutic treatment should involve activities of daily living and therapeutic exercises such as those for gradual enhancement of muscle strength, balance, endurance, breathing, and relaxation. Patient’s health status and preferences should be taken into account to secure an optimal patient-tailored physiotherapeutic treatment program encompassing patient education regarding frequency, intensity, type, and duration of each activity/exercise [26]. It is implied that for the successful implementation of rehabilitation, it is necessary to establish appropriate measures to assess the physical, functional, cognitive, and emotional state of patients who have survived COVID-19 [27].
Methods Used to Evaluate the Physical and Functional Outcomes of Physiotherapy
The most common outcome parameters used for assessment of aerobic capacity and endurance in the current available literature in COVID-19 patients are the Six Minute Walking Test (6MWT) [28] and the Endurance Shuttle Walk Test (ESWT) [29]. The 6MWT, which measures the distance covered over a time of 6 min, was recommended by KNGF guidelines [26], considering the requirement for larger space to conduct the test. The American Physical Therapy Association recommended the 2-minute step test [30] as a COVID-19 core outcome measure for endurance [31].
The most frequently used outcome measures for functional mobility and balance are the Short Physical Performance Battery (SPPB) [32] and Tinetti balance test [33,34]. The SPPB is recommended as a core measure of functional mobility allowing the assessment of gait speed, balance ability, and a 5 times sit-to-stand performance in 10 min [26,31]. It is preferred that muscle strength is objectively evaluated using dynamometry [35]. For determination of upper limb strength, handgrip force is usually utilized [36], while for the lower limbs, quadriceps isometric force is used [37]. For evaluation of functional status, established measures such as Barthel Index (BI) [38], the Functional Independence Measure (FIM) [39], and the Patient-Specific Functional Scale (PSFS) [40] have been widely used.
Methods Used to Evaluate Pulmonary Function Following Physiotherapy
Pre- and post-respiratory physiotherapy pulmonary function are mainly assessed clinically using the forced vital capacity (FVC) [41], forced vital capacity in one second (FEV1) [41], total lung capacity (TLC) [41], diffusion capacity for carbon monoxide (DLCO) [41], and maximum inspiratory pressure (MIP-cmH2O) [42]. The modified Borg dyspnea scale is the most frequently used outcome measure for subjective perception of dyspnea intensity [43,44].
Methods Used to Evaluate Quality of Life Following Physiotherapy
For assessment of quality of life and cognitive and emotional state, the EQ-5D-5L [45,46] and the 36-Item Short Form Survey (SF-36) [47] are most utilized. EQ-5D-5L is recommended as a core outcome measure for assessment of health-related quality of life, along with PROMIS-Global-10, which was adapted from SF-36 and EQ-5D [31,48]. Additionally, in clinical practice, the Feeling Thermometer (FT) [49], the Hospital Anxiety and Depression scale (HADS) [50], the Generalized Anxiety Disorder-7 (GAD-7) score [51], and the Patient Health Questionnaire (PHQ-9) [52] are often used.
Findings from 10 Key Studies Published Between 2020 and 2022
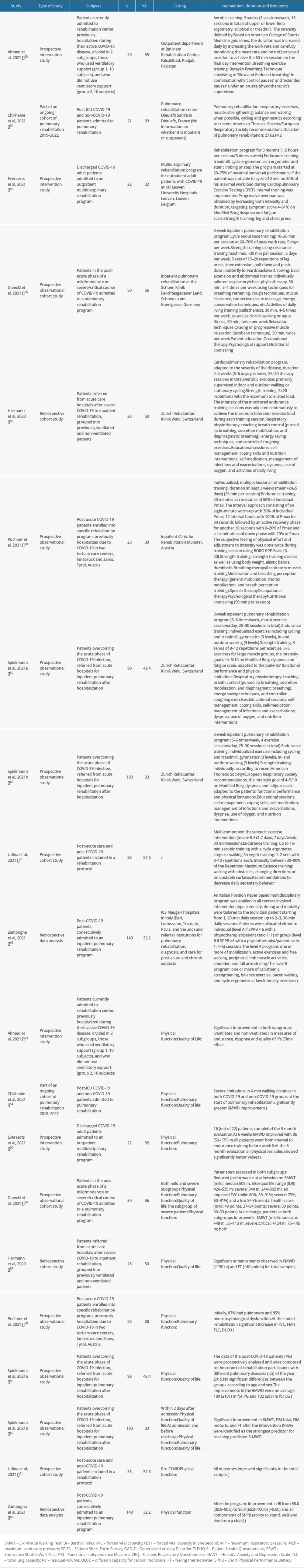
SUMMARY OF INCLUDED STUDIES:
A total of 10 studies [53–62] were included in this review, all of which were non-randomized intervention studies. Table 1 provides a summary of the characteristics of the included studies. Of note, 2 studies by Spielmanns et al [59,60] were identified. Upon reading, it was evident they reported different patient sample sizes, thus both papers were retained. All included studies were published in the English language between the years 2020 and 2022. They were conducted in Pakistan (1), France (1), Belgium (1), Germany (1), Switzerland (3), Austria (1), and Italy (1), while 1 study had no location information. Sample sizes ranged from n=20 to n=183. Two studies made comparisons between 2 subgroups of patients – those who did and those who did not use ventilatory support during the active course of the disease [53]. One study [54], besides post-ICU COVID-19 patients, included also post-ICU non-COVID-19 patients hospitalized due to respiratory failure. Also, 1 study compared the performance of post-ICU patients and those admitted to non-ICU wards [61].
Puchner et al [58] reported that 87% of patients had at least 1 underlying comorbidity. Six studies [54,56–60] assessed the comorbidities of patients upon admission to respective intervention programs, among whom 21–54% presented with arterial hypertension, 0–29% were smokers, 5–28% had diabetes, 5–48% had an established coronary artery disease, and 22–30% were previously diagnosed with pulmonary disease. According to Gloeckl et al [56], patients with a severe/critical form of COVID-19 had a higher percentage of comorbidities at baseline assessment in comparison to those with mild/moderate course of the disease. The Cumulative Illness Rating Scale (CIRS) score assessed in the studies of Spielmann et al [59,60] ranged from 12.74 (±5.54) to 14.18 (±5.92) (maximum possible points 56 corresponding to extremely severe problems in all items of the scale).
There was a wide range of intervention reporting. One study lacked a detailed description [54]. However, the majority of studies (n=9, 90%) provided elaborate explanations. Intervention programs ranged from 8 days to 3 months. Seven studies employed interventions in inpatient rehabilitation institutions, while the remaining 3 were in outpatient departments.
Rehabilitation programs mainly encompassed aerobic/endurance training, pulmonary/chest physiotherapy including breathing exercises, and resistance training. Surprisingly, balance training was involved only in 2 studies [54,61]. In 5 studies, besides the aforementioned training, interventions additionally included 1 or more of the following sessions: patient education, relaxation techniques, occupational therapy, activities of daily living, psychological support, nutritional counseling, self-management, coping skills, self-medication, management of infections and exacerbations, dyspnea, use of oxygen, and speech therapy [56–60].
Intervention therapy frequencies differed between the studies: every day [61,62], 5–6×/week [56,57,59,60], and 3×/week [53,55]. Duration of daily rehabilitation training sessions varied among studies, ranging from 20 to 90 min per day. No specific intervention frequency was provided in the studies of Chikhanie et al [54] and Puchner et al [58], while the overall length of the intervention program was not depicted by Zampogna et al [62].
In the majority of studies (n=8, 80%), the intensity of aerobic/endurance training was defined by either or both 50–70% of heart rate (HR) maximum according to the age of patients and rate of perceived exertion between 4 and 6 (Modified Borg dyspnea scale). For the resistance training components, most studies (n=9, 90%) utilized a mixture of upper and lower body exercises.
AEROBIC AND ENDURANCE TRAINING:
For the endurance training, patients were mainly engaged in 1 or more of the following exercises: upper or lower limb cycle ergometry [53,55,61,62], elliptical trainer [53], treadmill [53,55,59,60], stair climbing [55], stepper [55,61], indoor and outdoor walking [53,56,57,59–62], and ‘gymnastics’ [53,59,60].
All 10 studies reported outcomes related to aerobic capacity and endurance, 9 of which used the Six Minute Walk Distance (6MWD) as a measure of effect. All interventions resulted in significant increase in aerobic capacity when pre- and post-training performances were compared, with P values ranging from 0.05 to 0.001. Gloeckl et al [56] were the only ones who used both the 6MWTand the ESWT, a constant-load exercise capacity test which was performed at 85% of the maximum walking speed. There was a significant pre-post intervention change in duration, from 460 s to 1200 s (P=0.001), with 14 (54%) patients reaching the test duration maximum of 20 min.
In several studies, total samples were separated into subgroups based on previous severity of the disease for further inter-group comparisons to better understand the intervention effect in different courses of COVID-19. In the prospective intervention study of Ahmed et al [53] (N=20), the subgroup of patients who used ventilatory support during hospitalization due to COVID-19 showed a higher increase in exercise tolerance by performing a longer 6MWD after 5 weeks of training (pre-post mean difference (95% CI)=98.7 (78.9–118.4)) compared to the subgroup who did not use ventilatory support (51.3 (21.4–81.1) (P=0.008). In contrast, in the retrospective cohort study of Hermann et al [57] (N=28), no significant differences were observed in 6MWD between ventilated and non-ventilated patients.
Zampogna et al [62] showed that previous use of non-invasive ventilation and baseline inability to perform 6MWT is significantly associated with the functional performance of lower extremities, ie, improvement above 1 point in SPPB total score, OR 3.0 (SE 1.1), P=0.002, and OR 2.3 (SE 0.9), P=0.001, respectively. The improvement in 6MWD (in meters/day) was negatively correlated with the number of days post-ICU (r=−0.59, P=0.01) [54].
The sample in the study of Chikhanie et al [54] consisted of 21 COVID-19 post-ICU patients, in which pulmonary rehabilitation outcomes were compared retrospectively to a non-COVID-19 post-ICU group of 21 patients who underwent a similar intervention program. Interestingly, COVID-19 patients had a significantly greater (P<0.001) 6MWD improvement (+205±121 m) compared to non-COVID-19 patients (+93±66 m).
The 6MWD results were better in patients who underwent intervention sooner after discharge from the ICU [54].
RESISTANCE TRAINING:
All studies other than Ahmed et al [53] employed strengthening exercises in their intervention training. In the study reported by Everaerts et al [55], rehabilitation program sessions included leg and chest press as a form of strengthening exercises, while Gloeckl et al [56] used leg press, knee extension, pull-down and push-down, butterfly forward/backward, rowing, back extension, and abdominal trainer exercises. Puchner et al [58] used strength-training devices, body weight, elastic bands, and dumbbells. Spielmanns et al [59,60] in both of their studies used strength training to improve patients’ functional performance and physical limitations, with an intensity goal of 4–5/10 on the Modified Borg dyspnea and fatigue scale by engaging large muscle groups. Similarly, Zampogna et al [60] reported that patients with an initial SPPB score ≥6 underwent progressive increase or decrease of the strengthening training workload until patients scored their dyspnea and/or leg fatigue as 4–5/10 on the Modified Borg scale. Chikhanie et al [54] and Hermann et al [57] did not provide detailed information on the modality of strengthening exercise they used.
Significant increase in the force of upper and/or lower extremities was reported in several reviewed studies. Accordingly, handgrip force improved from 18.1±8.0 to 23.5±8.5 (kg) (P<0.05) in the study of Chikhanie et al [54], 25 (18–35) to 30 (20–39) (kg, P=0.002) in the study of Gloeckl [56], and from 69% to 104% (96–112) (p<0.01) of predicted value in the study of Everaerts et al [55]. Quadriceps force increased from 14.2±10.6 to 25.5±11.7 (kg) (p<0.05) in the study of Chikhanie et al. [54], from 78.4% (48.6–98.1) to 99.6% (68.4–103.3) of predicted value (p=0.008) in the study of Gloeckl et al. [56], and from 61% to 74% (p<0.01) of predicted value in the study of Everaerts et al [55].
The functional performance of the lower extremities using the SPPB was evaluated in 2 studies – Udina et al [61] and Zampogna et al [62]. In the first study [61], the total score (0–12) which was 5.4±2.7 at baseline assessment, increased by 3.7±2.1 (P<0.05) at the end of intervention, with a mean duration of 8.2±1.7 days. All 3 sub-scores of SPPB, ie, balance, gait speed, and chair stance, also increased significantly at post-intervention assessment (P<0.05). In the same study, it was reported that post-ICU patients, who were younger than non-ICU ones, experienced greater improvement in SPPB (4.4±2.1 vs 2.5±1.7) (P<0.01), and gait speed, 0.4±0.2 vs 0.2±0.1 m/s (P<0.01). Enhancement in SPPB total and its 3 components’ scores was also reported by Zampogna et al [60]. SPPB total scores improved from 3.2±3.7 to 6.9±3.8 (P<0.00). Chikhanie et al [54] reported increased balance ability at the end of the rehabilitation program, which was measured by the Tinetti balance test, from 25.0±3.0 to 27.5±1.0 (P<0.05), respectively. Physical improvement seems more pronounced in patients who required intensive care during hospitalization. Although both post-ICU and non-post-ICU patients showed significant improvements, post-ICU patients experienced greater improvement in SPPB and gait speed [61].
BREATHING EXERCISES:
Pulmonary performance was reported in a few studies. In the study of Chikhanie et al [54], following pulmonary rehabilitation, FVC (% predicted) increased from 59.1±15.2 to 72.9±15.2 (P<0.05), FEV1 (% predicted) increased from 66.7±16.0 to 81.2±14.2 (P<0.05). Likewise, Gloeckl et al [56] reported significant improvement in the following respiratory parameters (% predicted): FVC in patients with mild/moderate course of COVID-19 increased from 80.0 (59.2–90.9) to 87.7 (67.0–98.9) (P<0.01), and in those with severe/critical COVID-19 from 75.1 (59.8–90.6) to 86.4 (67.6–96.3) (P<0.001), FEV1 in mild/moderate COVID-19 patients changed from 83.3 (65.5–101.1) to 95.1 (84.0–106.8) (P<0.001), and in severe/critical COVID-19 from 79.1 (65.8–99.7) to 94.8 (80.9–106.2) (P<0.001), and DLCO in the subgroup of severe/critical COVID-19 patients increased from 55.8 (37.2–63.0) to 59.5 (37.8–70.9) (P<0.001), while no significant inter-group (mild/moderate vs severe/critical) differences were found for any of the above respiratory parameters. Positive changes in pulmonary function parameters (% predicted) as a result of rehabilitation were also found by Puchner et al [58]: FVC improved from 74±15 to 79±15 (P=0.007), FEV1 from 2.5±0.7 to 2.7±0.6 (P=0.014), TLC from 92±17 to 98±19 (P=0.002), and DLCO from 55±15 to 66±18 (P=0.003). MIP-cmH2O increased from 54±25 to 78±30 (P<0.001).
SUPPORTIVE THERAPIES:
The Barthel Index, used for assessment of the ability to perform everyday tasks, such as personal hygiene, walking, and dressing (score range 0–100) had an increase of 18.5 (12.9) in addition to the baseline value 76.5 (17.4) in the study by Udina [61]. Correspondingly, a significant increase of the Barthel Index was found by Puchner et al [58], from mean value 83±18 to 97±7 (P<0.001), and the study of Zampogna et al [62], from median value 55 (30–90) to 95 (65–100) (P<0.001).
The FIM, which was used to identify changes in functional status of patients as an outcome of rehabilitation, had a significant pre-post intervention improvement of the total score in the studies of Spielmanns et al [59,60], from 100±15.1 to 111±15.0 (P<0.0001), and from 98.12±15.75 to 113.51±12.94 (P<0.001), respectively. In the second paper by Spielmanns et al [60], the FIM motoric score also significantly increased, from 68.68±12.89 to 81.22±10.75 (P<0.001).
Significant enhancements were observed in Feeling Thermometer (FT) (+40 points) for total sample (P<0.001) in the study by Hermann et al [57], with no significant differences between patients who were ventilated and non-ventilated during the active course of COVID-19. Likewise, positive changes in FT degrees were also encountered in both studies by Spielmanns et al [59,60], from 51.9±18.1 to 68.6±17.2 (P<0.0001), and from 53.79±16.99 to 75.18±13.14 (P<0.001), respectively.
EVALUATION OF QUALITY OF LIFE IN PATIENTS RECOVERING FROM SEVERE COVID-19:
Quality of life was measured in several studies. While Hermann et al [57] and Spielmanns et al [60] encountered no significant changes regarding anxiety and depression assessed using the HADS (normal values considered if <8), in the study of Chikhanie et al [54] significant improvement was found after pulmonary rehabilitation, from 6.9±4.6 to 2.2±3.2 and from 6.5±4.8 to 1.4±2.4 (P<0.05), respectively. In the study of Ahmad et al [53], the outcome of SF-36 health-related quality of life increased in all of its sub-scales: general health, physical function, role emotional, role physical, bodily pain, mental health, social function, and vitality (P<0.05-0.001). Gloeckl et al [56] did not find any significant change in the SF-36 physical component sum score, but the SF-36 mental component sum score had a significant increase after 3 weeks of inpatient pulmonary rehabilitation in patients with previous severe/critical course of COVID-19, from 38.5 (30.1–52.8) to 52.9 (32.0–58.2), (P<0.001), respectively. In the same study, the measures GAD-7 and PHQ-9 were additionally utilized for patients with severe/critical course of COVID-19. Surprisingly, there was a slight but significant worsening in GAD-7 outcome after completion of intervention, increased from score 4 (2–8) to 5 (1–7) (P=0.021) (cut-off points of 5, 10, and 15 interpreted as mild, moderate, and severe levels of anxiety, respectively), whereas PHQ-9 showed a positive change from mild to no depression, with a decrease in score from 7 (4–12) to 4 (2–10) (P=0.002), respectively.
DEFINING CANDIDATE PATIENTS FOR PHYSIOTHERAPY:
Quadriceps muscle weakness and decreased ability to exercise may define a good choice of patients for respiratory rehabilitation [63–65]. Gloeckl et al [56] found that patients on admission to pulmonary rehabilitation had a reduced performance on 6MWT, an impaired FVC, and a low SF-36 mental health score. Zampogna et al [62] also reported that only 42 (30.0%) subjects were able to perform the 6MWT at admission, while the activities of daily living were diminished (BI 55.0 (30.0–90.0) out of a maximum score 100). The ability to stand, walk, or rise from a chair without help was also reported as severely impaired upon admission, with 82 (58.6%) patients showing a SPPB score <3 (out of maximal score 12) in the study by Zampogna et al [62]. The values of 6MWD ≥130 m and FVC >83% predicted assessed at admission were described as the best predictors of reaching 6MWD predicted in the 3-week inpatient pulmonary rehabilitation of Spielmanns et al [60]. Also, previous use of non-invasive ventilation, the median SPPB total score <3, and inability to perform 6MWT at admission were significantly associated with the improvement of above 1 point in SPPB total score [62].
Future Recommendations
Many countries have issued national guidelines for one-to-one or self-management physiotherapy interventions for individuals with COVID-19. However, considering the novelty of SARS-CoV-2 and lack of randomized controlled clinical trials involving rehabilitation of COVID-19 patients, the current recommended treatment methods and outcome measures to evaluate the effects on respiratory and physical function and quality of life are those largely founded on the established evidence of other respiratory illnesses. Hence, research providing high-quality evidence-based data are warranted for development of international clinical guidelines for physiotherapy and rehabilitation support for patients who have been hospitalized for COVID-19. We recommend that future studies also include a more thorough evaluation of the effect of physiotherapy on quality of life of post-COVID-19 patients.
Conclusions
This review has highlighted the feasibility of physiotherapy in enhancement of aerobic endurance, strength, pulmonary capacity, activities of daily living, and functionality of post-COVID-19 patients after discharge from hospital. For stronger conclusions on the effectiveness of physiotherapy, randomized control trials and other research providing high-quality evidence-based data are warranted. It is also recommended that future studies include a more thorough evaluation of effect of physiotherapy on quality of life of post-COVID-19 patients.
Currently, the methods used for physiotherapy and the methods used to evaluate the effects on respiratory and physical function and quality of life are those established from the pre-COVID-19 era. Therefore, this review has also highlighted the need for controlled clinical studies to support physiotherapy guidelines as COVID-19 continues to affect patients worldwide, with some patients still requiring extended periods of hospitalization.
References
1. Wu C, Chen X, Cai Y, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China: JAMA Inter Med, 2020; 180(7); 934-43
2. World Health Organization: COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum Aug 6, 2022 Available at: https://bit.ly/34FnbLd
3. World Health Organization, Coronavirus disease 2019 (COVID-19): COVID-19 Weekly Epidemiological Update. Data as received by WHO from national authorities, as of 7 Sep 2022 Sep 7, 2022 Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---7-september-2022
4. Young B, Ong SWX, Kalimuddin S, Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore: JAMA, 2020; 323(15); 1488-94
5. Guan WJ, Ni ZY, Hu Y, Clinical characteristics of Coronavirus disease 2019 in China: N Engl J Med, 2020; 382(18); 1708-20
6. Menachemi N, Dixon BE, Wools-Kaloustian KK, How many SARS-CoV-2-infected people require hospitalization? Using random sample testing to better inform preparedness efforts: J Public Health Manag Pract, 2021; 27(3); 246-50
7. Simpson R, Robinson L, Rehabilitation following critical illness in people with COVID-19 infection: Am J Phys Med Rehabil, 2020; 99; 470-74
8. Brugliera L, Spina A, Castellazzi P, Rehabilitation of COVID-19 patients: J Rehabil Med, 2020; 52; jrm00046
9. Lazzeri M, Lanza A, Bellini R, Respiratory physiotherapy in patients with COVID-19 infection in acute setting: A Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR): Monaldi Arch Chest Dis, 2020; 90(1); 1285
10. Stam HJ, Stucki G, Bickenbach J, COVID-19 and post intensive care syndrome: A call for action: J Rehab Med, 2020; 52; jrm00044
11. Carda S, Invernizzi M, Bavikatte G, The role of physical and rehabilitation medicine in the COVID-19 pandemic: The clinician’s view: Ann Phys Rehabil Med, 2020; 63(6); 554-56
12. Gutenbrunner C, Stokes EK, Dreinhöfer K, Why Rehabilitation must have priority during and after the COVID-19-pandemic: A position statement of the Global Rehabilitation Alliance: J Rehabil Med, 2020; 52(7); jrm00081
13. Vitacca M, Carone M, Clini EM, Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: The Italian position paper: Respiration, 2020; 99; 493-99
14. Lew HL, Oh-Park M, Cifu DX, The war on COVID-19 pandemic: Role of rehabilitation professionals and hospitals: Am J Phys Med Rehabil, 2020; 99(7); 571-72
15. Demeco A, Marotta N, Barletta M, Rehabilitation of patients post-COVID-19 infection: A literature review: J Int Med Res, 2020; 48(8); 300060520948382
16. Dasgupta A, Kalhan A, Kalra S, Long term complications and rehabilitation of COVID-19 patients: J Pak Med Assoc, 2020; 70(Suppl 3(5)); S131-35
17. Halpin SJ, McIvor C, Whyatt G, Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation: J Med Virol, 2020; 93(2); 1013-22
18. Andrenelli E, Negrini F, de Sire AInternational Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action: Eur J Phys Rehabil Med, 2020; 56(4); 508-14
19. Debeuf R, Swinnen E, Plattiau T, The Effect of physical therapy on impairments in COVID-19 patients from intensive care to home rehabilitation: A rapid review: J Rehabil Med, 2022; 54; jrm00242
20. Ahmadi Hekmatikar AH, Ferreira JB, Shahrbanian S, Functional and psychological changes after exercise training in post-COVID-19 patients discharged from the hospital: A PRISMA-compliant systematic review: Int J Environ Res Public Health, 2022; 19(4); 2290
21. National Health System: Techniques-Physiotherapy Sep 06, 2022 Available at: https://www.nhs.uk/conditions/physiotherapy/how-it-works/
22. Forbes R, Mandrusiak A, Smith M, A comparison of patient education practices and perceptions of novice and experienced physiotherapists in Australian physiotherapy settings: Musculoskelet Sci Pract, 2017; 28; 46-53
23. Bielecki JE, Tadi P, Therapeutic exercise: StatPearls, 2022, Treasure Island (FL), StatPearls Publishing
24. Garber CE, Blissmer B, Deschenes MRAmerican College of Sports Medicine position stand, Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise: Med Sci Sports Exerc, 2011; 43(7); 1334-59
25. Placzek JD, Boyce DA: Orthopaedic physical therapy secrets, 2017, St Louis (MO), Elsevier
26. Royal Dutch Society for Physical Therapy (KNGF): Recommendations for physiotherapy in patients with COVID-19 Sep 07, 2022 Available at: https://www.https://bit.ly/3esY2Ir
27. Spruit MA, Holland AE, Singh SJ, COVID-19: Interim guidance on rehabilitation in the hospital and post-hospital phase from a European Respiratory Society and American Thoracic Society-coordinated International Task Force: Eur Respir J, 2020; 56(6); 2002197
28. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories, ATS statement: guidelines for the six-minute walk test: Am J Respir Crit Care Med, 2002; 166(1); 111-17
29. Revill SM, Morgan MD, Singh SJ, The endurance shuttle walk: A new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease: Thorax, 1999; 54(3); 213-22
30. Bohannon RW, Wang YC, Gershon RC, Two-minute walk test performance by adults 18 to 85 years: Normative values, reliability, and responsiveness: Arch Phys Med Rehabil, 2015; 96(3); 472-77
31. Wells CL, Kegelmeyer D, Mayer KP, APTA cross sections and academies recommendations for COVID-19 core outcome measures: J Acute Care Phys Ther, 2022; 13(2); 62-76
32. Guralnik JM, Simonsick EM, Ferrucci L, A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission: J Gerontol, 1994; 49(2); M85-94
33. Tinetti ME, Williams TF, Mayewski R, Fall risk index for elderly patients based on number of chronic disabilities: Am J Med, 1986; 80(3); 429-34
34. Berg KO, Wood-Dauphinee SL, Williams JI, Measuring balance in the elderly: Validation of an instrument: Can J Public Health, 1992; 83(Suppl 2); S7-11
35. Parry SM, Granger CL, Berney S, Assessment of impairment and activity limitations in the critically ill: A systematic review of measurement instruments and their clinimetric properties: Intensive Care Med, 2015; 41(5); 744-62
36. Innes E, Handgrip strength testing: A review of the literature: Australian Occupational Therapy Journal, 1999; 46; 120-40
37. Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, Functionally relevant thresholds of quadriceps femoris strength: J Gerontol A Biol Sci Med Sci, 2002; 57(4); B144-52
38. Mahoney FI, Barthel DW, functional evaluation: The Barthel Index: Md State Med J, 1965; 14; 61-65
39. Linacre JM, Heinemann AW, Wright BD, The structure and stability of the Functional Independence Measure: Arch Phys Med Rehabil, 1994; 75(2); 127-32
40. Stratford PW, Gill C, Westaway MD, Assessing disability and change on individual patients: A report of a patient specific measure: Physiother Can, 1995; 47; 258-62
41. Ranu H, Wilde M, Madden B, Pulmonary function tests: Ulster Med J, 2011; 80(2); 84-90
42. Wilson SH, Cooke NT, Edwards RH, Predicted normal values for maximal respiratory pressures in caucasian adults and children: Thorax, 1984; 39(7); 535-38
43. Borg GA, Psychophysical bases of perceived exertion: Med Sci Sports Exerc, 1982; 14(5); 377-81
44. Williams N, The Borg Rating of Perceived Exertion (RPE) scale: Occupational Medicine, 2017; 67(5); 404-5
45. Group TE, EuroQol – q new facility for the measurement of health-related quality of life: Health Policy, 1990; 16(3); 199-208
46. Herdman M, Gudex C, Lloyd A, Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L): Qual Life Res, 2011; 20; 1727-36
47. Ware JE, Sherbourne CD, The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection: Med Care, 1992; 30(6); 473-83
48. Hays RD, Bjorner JB, Revicki DA, Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items: Qual Life Res, 2009; 18(7); 873-80
49. Zavala-Rojas D, Thermometer scale (feeling thermometer): Encyclopedia of quality of life and well-being research, 2014; 6633-34, Dordrecht (Netherlands), Springer
50. Herrmann C, International experiences with the Hospital Anxiety and Depression Scale – a review of validation data and clinical results: J Psychosom Res, 1997; 42(1); 17-41
51. Spitzer RL, Kroenke K, Williams JB, A brief measure for assessing generalized anxiety disorder: The GAD-7: Arch Intern Med, 2006; 166(10); 1092-97
52. Kroenke K, Spitzer RL, Williams JB, The PHQ-9: Validity of a brief depression severity measure: J Gen Intern Med, 2001; 16(9); 606-13
53. Ahmed I, Inam AB, Belli S, Effectiveness of aerobic exercise training program on cardio-respiratory fitness and quality of life in patients recovered from COVID-19: Eur J Physiother, 2021; 2021; 1909649
54. Al Chikhanie Y, Veale D, Schoeffler M, Effectiveness of pulmonary rehabilitation in COVID-19 respiratory failure patients post-ICU: Respir Physiol Neurobiol, 2021; 287; 103639
55. Everaerts S, Heyns A, Langer D, COVID-19 recovery: Benefits of multidisciplinary respiratory rehabilitation: BMJ Open Respir Res, 2021; 8; e000837
56. Gloeckl R, Leitl D, Jarosch I, Benefits of pulmonary rehabilitation in COVID-19: A prospective observational cohort study: ERJ Open Res, 2021; 7(2); 00108-2021
57. Hermann M, Pekacka-Egli AM, Witassek F, Feasibility and efficacy of cardiopulmonary rehabilitation after COVID-19: Am J Phys Med Rehabil, 2020; 99(10); 865-69
58. Puchner B, Sahanic S, Kirchmair R, Beneficial effects of multi-disciplinary rehabilitation in postacute COVID-19: An observational cohort study: Eur J Phys Rehabil Med, 2021; 57(2); 189-98
59. Spielmanns M, Pekacka-Egli AM, Schoendorf S, Effects of a comprehensive pulmonary rehabilitation in severe post-COVID-19 patients: Int J Environ Res Public Health, 2021; 18(5); 2695
60. Spielmanns M, Buelow MM, Pekacka-Egli AM, Clinical and functional predictors of response to a comprehensive pulmonary rehabilitation in severe post-COVID-19 patients: Microorganisms, 2021; 9(12); 2452
61. Udina C, Ars J, Morandi A, Rehabilitation in adult post-COVID-19 patients in post-acute care with Therapeutic Exercise: J Frailty Aging, 2021; 10(3); 297-300
62. Zampogna E, Paneroni M, Belli S, Pulmonary rehabilitation in patients recovering from COVID-19: Respiration, 2021; 100(5); 416-22
63. Wang TJ, Chau B, Lui M, Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19: Am J Phys Med Rehabil, 2020; 99(9); 769-74
64. Huang S, Xiao Y, Yan L, Implications for online management: Two cases with COVID-19: Telemed J E Health, 2020; 26(4); 487-94
65. Mukaino M, Tatemoto T, Kumazawa N, Staying active in isolation: Telerehabilitation for individuals with the SARS-CoV-2 infection: Am J Phys Med Rehabil, 2020; 99; 478-79
In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952