13 February 2023: Clinical Research
Relationship Between Changes in Cranio-Cervical Extensor Muscles and Quality of Life: A Single-Center Study of 15 Patients with Chronic Tension-Type Headache
Xiaoman Min1ABCDEFG, Yongjun Huo2B, Ning Sun3BCEF, Hongwei Zhi4B, Haitao Li4F, Sishuo Zhang4B, Wenqiang Cui4ABCEFG, Yanlin Guo5B, Hongyun Wu4ABEG*DOI: 10.12659/MSM.938574
Med Sci Monit 2023; 29:e938574
Abstract
BACKGROUND: This single-center study of 15 patients with chronic tension-type headache aimed to compare the cranio-cervical extensor muscles between patients with chronic tension-type headache and healthy individuals and to explore the relationship between changes in cranio-cervical extensor muscles and quality of life (QoL).
MATERIAL AND METHODS: We recruited 15 patients with chronic tension-type headache and 15 healthy individuals. Patients with chronic tension-type headache were diagnosed by 2 neurologists according to the diagnostic criteria in the International Classification of Headache Disorders, 3rd edition (ICHD-3). Morphological changes in the cranio-cervical extensor muscle were detected using magnetic resonance imaging (MRI). QoL and the degree of neck dysfunction were assessed using the Headache Impact Test-6 (HIT-6) and Neck Disability Index (NDI), respectively.
RESULTS: The relative cross-sectional areas (rCSAs) of the rectus capitis posterior minor (RCPmin) were lower in patients with chronic tension-type headache than in healthy individuals. The HIT-6 scores (r=-0.93, P<0.001 and r=-0.85, P<0.001 for RCPmin right side and left side, respectively) and NDI scores (r=-0.75, P<0.001 and r=-0.70, P<0.001 for RCPmin right side and left side, respectively) were negatively associated with the rCSA of RCPmin in the chronic tension-type headache group.
CONCLUSIONS: Most patients with chronic tension-type headache experience RCPmin atrophy. The more evident the RCPmin atrophy, the worse the QoL of the patients with chronic tension-type headache.
Keywords: Cross-Sectional Studies, Magnetic Resonance Imaging, Muscular Atrophy, Quality of Life, Tension-Type Headache, Humans, Muscle, Skeletal, Headache, Atrophy
Background
Tension-type headache is the most common type of headache [1,2]. Among all the diseases registered by the Global Burden of Diseases, Injuries, and Risk Factors studies in 2016, tension-type headache has the highest prevalence [3], ranging from 36% to 78% [4]. Tension-type headache is more common in men than women and is more common in people aged 30–39 years [5]. Chronic tension-type headache is a disease that evolves from episodic tension-type headache, and its incidence rate is 2.2% [6]. Patients with chronic tension-type headache may experience anxiety, depression, or sleep disorders under the continuous influence of headaches, and the pain of patients with chronic tension-type headache has various negative effects on their daily activities, work, and family [7–9]. Tension-type headache can be treated with analgesics, preventive therapy, and antidepressants [10,11].
McPartland et al found that, compared with healthy subjects, subjects with chronic neck pain had atrophy of the rectus capitis muscle, which may indicate a relationship between chronic pain and muscle atrophy [12]. In a study on tension-type headache, Fernández-de-las-Peñas et al found that the rectus capitis posterior minor (RCPmin) and rectus capitis posterior major (RCPmaj) of patients with chronic tension-type headache were atrophied compared to healthy individuals [13]. The splenius capitis is atrophied in adolescents with tension-type headache [14]. Eunsang Lee et al found that after 2 weeks of biofeedback treatment, tension-type headache patients’ headache symptoms improved and their Headache Impact Test-6 (HIT-6) scores decreased significantly [15]. Wonho Choi found that the tension of suboccipital muscles, headache, and Neck Disability Index (NDI) scores of patients with tension-type headache decreased after performing cervical deep-muscle flexion exercises [16]. Therefore, we speculated that the neck muscles of patients with chronic tension-type headache may be atrophied, which may also be related to decreased quality of life (QoL) of patients with chronic tension-type headache.
With the continuous development of medicine, magnetic resonance imaging (MRI) has gradually become an important tool for detecting muscle atrophy [17]. Fernández-de-Las-Peñas et al used MRI to measure the cross-sectional areas (CSAs) of neck muscles, and the CSAs measured using this method are considered to be accurate [13]. We used MRI to detect the CSAs of the cranio-cervical extensor muscles of patients with chronic tension-type headache, including the RCPmin, semispinalis capitis, and splenius capitis. Therefore, this single-center study of 15 patients with chronic tension-type headache aimed to investigate the relationship between changes in cranio-cervical extensor muscles and QoL.
Material and Methods
ETHICS STATEMENT:
This study was approved by the Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine (registration number: ChiCTR2200058447, ethics approval number: 2020-018) and was performed in accordance with the Declaration of Helsinki. All participants reported that the MRI examination and other tests were acceptable and completed all tests. All participants signed an informed consent form prior to participation.
RECRUITMENT OF SUBJECTS: We recruited 22 subjects with chronic headache and 15 healthy subjects between November 2021 and April 2022. All subjects were recruited from the Affiliated Hospital of Shandong University of Traditional Chinese Medicine and were right-handed. All our subjects were formally recruited through registration and screening, excluding outpatients and inpatients. According to the diagnostic criteria of the chronic tension-type headache in the International Classification of Headache Disorders, 3rd edition (ICHD-3: Code 1.1, 2013) [18], patients with chronic tension-type headache were diagnosed by neurologists Professor Wu and Professor Li.
INCLUSION CRITERIA: For inclusion in this study, all patients had to meet the ICHD-3 diagnostic criteria of chronic tension-type headache [18]: mild or moderate nonpulsatile pain on both sides of the head, without photophobia, fear of sound, nausea, or vomiting. All cases evolved from episodic tension-type headache, but headache must last for at least 15 days per month for more than 3 months before it can be considered chronic headache. In addition, the severity of headache should not be affected by daily physical activity, and there should be no signs of secondary headache or medication-overuse headache.
Patients with chronic tension-type headache who were included in the examination could receive preventive or therapeutic treatment with pain-killing drugs with the doctors’ consent or when they have a headache.
Subjects in the healthy control group were required to be in a healthy state and have no headache within the last year, no medication in 1 month, and no family history of headache. The subjects did not consume alcohol, caffeine, or other substances for at least 3 days before MRI.
EXCLUSION CRITERIA:
The exclusion criteria for all subjects included the following: (1) subjects taking opioid analgesics, antipsychotics, or ergotamine, consuming alcohol, or abusing other drugs; (2) subjects complicated with serious primary or mental diseases, such as heart, brain, liver, kidney, and hematopoietic system diseases; (3) pregnant or lactating women; (4) subjects contraindicated to undergo MRI or unwilling to cooperate; (5) the body mass index (BMI) of the subjects was not within the normal range, or they were too weak to exercise normally.
After screening, 15 patients with chronic tension-type headache and 15 healthy individuals were recruited for this study. An MRI scan was performed during the interictal stage in the chronic tension-type headache group, at least 3 days after the chronic tension-type headache attack. MRI was performed on 1 healthy individual on the same day.
CLINICAL EVALUATION:
In addition to recording the subjects’ sex, age, and preferred hand, the height (m) and weight (kg) of each subject were also recorded to calculate their BMI, which was used to explore whether the BMI of the subjects had an effect on the changes in their muscles. The data of all subjects were obtained using the same measuring ruler and scale.
MRI-RELATED DATA: In this study, we used MRI to detect morphological changes in muscles [13]. All images were acquired using a SIGNA Pioneer 3.0T MRI scanner. The region of interest of the muscle was manually delineated using the area measurement function of the MRI machine.
The suboccipital muscles, including the RCPmaj, RCPmin, obliquus capitis superior, and obliquus capitis inferior, are considered to be closely related to chronic tension-type headache [19]. The obliquus capitis inferior is involved in ipsilateral neck rotation. The RCPmin, RCPmaj, and obliquus capitis superior can help extend the head, and unilateral contraction contributes to ipsilateral rotation and side bending of the head [20]. Similar to the RCPmin and RCPmaj, the semispinalis capitis and splenius capitis also participate in head extension. The semispinalis capitis can maintain the neck forward-bending posture. The splenius capitis helps with ipsilateral rotation of the head and leaning the head backward. After combining the previous research and careful consideration, we analyzed the following neck muscles: the RCPmin, semispinalis capitis, and splenius capitis [13,14].
The measurement parameters were as follows: 28 slices, 4-mm slice thickness, 200 mm field of view read, 520 ms repetition time, 20.0 ms echo time, 256×256 matrix size, and 15: 00 acquisition time.
CALCULATION OF NECK MUSCLES’ RELATIVE CROSS-SECTIONAL AREAS (RCSAS): Because the measured neck muscles can be observed on at least 2 cervical planes, to minimize the error between the chronic tension-type headache and control groups, we used the rCSA to standardize the data. Our method was optimized using Elliott’s method [21]. After the MRI examination, we obtained sagittal and axial slices of head and neck of each subject. Through their sagittal slices, we could locate specific levels of each cervical vertebra, then we chose the slices corresponding to the cervical vertebra we desired. Finally, we used axial images to measure the rCSAs of the neck extensor muscles at specific cervical levels. The rCSAs of both RCPmin muscles were measured using axial scans at the C1 and C2 levels (Figure 1A). The rCSAs of the semispinalis capitis and splenius capitis were measured once each in the C3 and C4 segments (Figure 1B, 1C). To ensure the accuracy of data, at least 2 professionals (Professor Cui, Professor Huo, or Professor Zhi) were present when measuring each group of data, none of them knew the subject’s diagnosis, and they all stated that they had no objection to the measured data values.
THE HIT-6 SCORE: The HIT-6 can be used to evaluate the effect of various types of headaches on QoL [22], so we used the HIT-6 to evaluate the effect of chronic tension-type headache on QoL. These 6 questions of the HIT-6 originate from the Internet-based Headache Impact Questionnaires, Migraine Disability Assessment Scale, and migraine-specific QoL questionnaires. These 6 questions are related to the degree of pain, social activities, daily activities, cognitive function, psychological state, and concentration of patients. The total score of the HIT-6 should be between 36 and 78, and the corresponding scores of each option are as follows: never, 6 points; rarely, 8 points; sometimes, 10 points; often, 11 points; and always, 13 points. The higher the score of the subjects, the greater the effect of headaches on QoL. The criteria for determining the effect of different total QoL scores are shown in Table 1 [23].
THE NDI SCORE: The NDI can be used to evaluate neck dysfunction in patients with neck pain and is widely used as a self-reported questionnaire for assessment of disability in patients with neck pain [24]. The NDI consists of 10 questions, including the intensity of neck pain, headache, attention loss, and other related symptoms and the impact of neck pain on daily life, such as lifting heavy objects, reading, work, driving, entertainment, and sleep. The corresponding scores for each option are as follows: 0 points, no effect, 1 point, occasionally affected; 2 points, slightly affected; 3 points, moderately affected; 4 points, severely affected; and 5 points, continuously affected. The neck function impairment index was calculated after obtaining the corresponding score for each subject. The calculation formula is as follows: neck function impairment index (%)=(total score of each item/number of items completed by the subject×5)×100%. The higher the neck function impairment index, the greater the effect of neck pain on QoL [25], so we used the NDI score to explore the influence of neck dysfunction on QoL of chronic tension-type headache patients.
STATISTICAL ANALYSIS:
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) statistical package (version 26.0; SPSS Inc.). Anthropometric data are expressed as the mean±standard deviation. The normal distribution of quantitative data was evaluated using the Kolmogorov-Smirnov test (
Results
PARTICIPANTS AND BASELINE CHARACTERISTICS:
Fifteen patients were included in this study, with a disease duration of more than 3 (7.60±2.41) months and an average attack duration of more than or equal to 15 (19.07±4.22) days. All patients with chronic tension-type headache in this study had symptoms of tension headache within 1 month before the test and lasted for more than 15 days. Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics, including sex, age, and dominant hand, are shown in Table 2. No significant differences were observed between the groups (P=1.00, 0.98, and 1.00, respectively).
COMPARISON OF LEFT AND RIGHT CRANIO-CERVICAL EXTENSOR MUSCLES: After the Kolmogorov-Smirnov test, the rCSA data did not have normal distribution range; thus, nonparametric analysis was selected. No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05). In all our subjects, the 4 pairs of muscles we tested were symmetrical. The result of the comparison of left and right muscles of subjects are displayed in Table 3.
COMPARISON OF CRANIO-CERVICAL EXTENSOR MUSCLES BETWEEN CHRONIC TENSION-TYPE HEADACHE PATIENTS AND HEALTHY CONTROLS: Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively, Table 4, Figure 2), indicating that the RCPmin in chronic tension-type headache patients are atrophic. However, at C3 and C4 levels, there were no significant differences in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4, Table 4). We did not find any significant difference between the semispinalis capitis and splenius capitis of patients with chronic tension-type headache and healthy individuals. Moreover, we did not find a direct correlation between BMI and rCSA values (P=0.244 >0.05). The rCSA values of subjects had no relationship with their height and weight.
HIT-6 OUTCOMES:
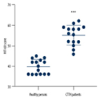
The HIT-6 scores of patients with chronic tension-type headache (55.07±4.83) were significantly higher than those of healthy volunteers (39.73±3.56) (Wilcoxon rank-sum test, P<0.001, Figure 3A), indicating that chronic tension-type headache had a significant negative effect on QoL. The proportion of patients whose QoL was affected was 87% (n=13), of whom 39% (n=5) were slightly affected, 46% (n=6) were moderately affected, and 15% (n=2) were seriously affected.
NDI OUTCOMES:
The neck function impairment index of patients with chronic tension-type headache (16.2±10.96%) was significantly higher than that of healthy volunteers (5.01±2.60%) (Wilcoxon rank-sum test, P<0.001, Figure 3B). The proportion of chronic tension-type headache patients with neck dysfunction was 27% (n=4), and the proportion of healthy individuals was 0%. This indicates that patients with chronic tension-type headache are more likely to have neck disability than healthy individuals, and that abnormal neck muscle function has a greater effect on their QoL.
CORRELATION BETWEEN THE HIT-6 SCORE AND THE RCSA OF RCPMIN IN THE CHRONIC TENSION-TYPE HEADACHE GROUP:
The results of Spearman correlation analysis showed that there was a significant negative correlation between the HIT-6 score and the rCSA of the RCPmin in the chronic tension-type headache group (r=−0.93 and
CORRELATION BETWEEN THE NDI SCORE AND THE RCSA OF RCPMIN IN THE CHRONIC TENSION-TYPE HEADACHE GROUP:
The NDI score and rCSA of the RCPmin in the chronic tension-type headache group were also negatively correlated (r=−0.75,
Discussion
In our study, we measured the rCSAs of patients with chronic tension-type headache and healthy individuals and analyzed the relationship between the rCSAs and QoL in patients with chronic tension-type headache. According to our results, compared with the healthy control group, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower, suggesting muscle atrophy, whereas the rCSAs of the semispinalis capital and splenius capital did not differ significantly between patients with chronic tension-type headache and healthy individuals. We did not find a clear correlation between the rCSA values of the subjects and their BMI index. Some patients with chronic tension-type headache had small rCSAs’ RCPmin values, not because of their low BMI index, but because their RCPmin had atrophied.
Our results suggest that chronic tension-type headache is closely associated with RCPmin atrophy. Deep-muscle atrophy in patients with musculoskeletal diseases has been reported in previous studies. The symptomatic side of patients with unilateral back pain shows spinal muscle atrophy [26]. The degree of pain in patients with chronic low back pain is negatively correlated with the degree of atrophy of the paraspinal muscle [27]. Furthermore, in a prior study related to tension-type headache, the RCPmin and RCPmaj of patients with chronic tension-type headache were more atrophied compared with those of healthy individuals [13]. In our study, consistent with previous findings, the RCPmin in patients with chronic tension-type headache also showed atrophy. The area around the RCPmaj is surrounded by the superior oblique muscle of the head, RCPmin, semispinalis capitis, and splenius capitis. The RCPmaj is at risk of unclear boundary, resulting in inaccurate data, and thus is not measured. This suggests that patients with chronic tension-type headache have experienced atrophy of the rectus capitis muscle, which may be an important factor leading to chronic pain. The splenius capitis also atrophies in adolescents with tension-type headache [14]. However, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and healthy controls in our study. We will recruit more subjects in the future and further observe the changes in these 2 muscles.
The current explanation for the decrease in rCSAs in the cervical muscles of patients with tension-type headache is mostly hypothetical. The RCPmin is connected to the cervical dura mater through a myodural bridge [28–30]. During normal head movement, it can prevent or limit inflection of the dura mater, which is sensitive to pain [29,31]. The RCPmin of patients with chronic headache tend to have a fatty infection (FI) [32]. FI can cause atrophy of the RCPmin, reduce its strength, and cause the RCPmin to be unable to maintain normal tension levels within the myodural bridge [33]. Therefore, FI is likely to lead to infolding of the dura mater in daily life and further cause headache and neck pain, which may also explain why osteopathic manipulative treatment techniques can alleviate some cranio-cervical disorders [30,31]. Headache can limit neck movement, and insufficient effective use of the neck may change the state of the neck muscles and lead to muscle atrophy [34,35], but the RCPmin may not substantially contribute to gross movements of the head [36]. Therefore, the restriction of neck movement by headache of chronic tension-type headache patients may not be closely related to the changes in RCPmin status.
In our study, as also reported by Eunsang Lee et al [15], we found that the degree of atrophy of the RCPmin in patients with chronic tension-type headache was negatively correlated with their HIT-6 scores. Moreover, the NDI scores of patients with chronic tension-type headache were negatively correlated with the degree of atrophy of their RCPmin, which was consistent with the findings of Wonho Choi [16]. The degree of atrophy of the RCPmin in patients with chronic tension-type headache affected their QoL. We hope that we can improve the QoL of patients with chronic tension-type headache by changing the state of the cranio-cervical extensor muscles.
The strength of our study is that the age of the patients we selected covered a relatively wide range. Our study has shown that the RCPmin in patients with chronic tension-type headache tend to be atrophied compared with healthy individuals. If we continue to recruit more subjects, the change trend of the RCPmin we found may help clarify the diagnosis of chronic tension-type headache in more patients of various ages with chronic tension-type headache. Each patient with chronic tension-type headache was accurately diagnosed by experts with high reliability. All rCSAs were measured by the same examiner, which reduces the data error as much as possible.
However, our study has some limitations. First, we only selected patients with chronic tension-type headache to participate in this study, rather than patients with other types of headaches. Therefore, our study results can only be applied to patients with chronic tension-type headache and not to those with other types of headache. Future studies should further explore whether other types of headaches are associated with neck muscle atrophy. Second, the sample size of the present study was relatively small, as only 15 patients with chronic tension-type headache and 15 healthy individuals were included. In the future, we can further expand the number of subjects to conduct multicenter observations with a large sample size to reduce the influence of regional factors on the experimental results and further clarify the relationship between muscle atrophy and chronic tension-type headache. Third, although our participants were systematically educated before the MRI examination, some subjects still have a short period of activity during MRI scanning, which may have had a slight impact on the results. We hope we can find a way to shorten the test time in the future. Fourth, the rCSA of muscle was manually delineated using the area measurement function of the MRI machine. Although our drawing process was very careful, there were still inevitable small errors. Finally, the muscle tissue around the RCPmaj is quite dense, which can easily produce large errors in measurement. We did not measure this muscle tissue. Efforts should be made to determine a measurement method suitable for the RCPmaj. In this way, we can have a more comprehensive understanding of the effect of changes in cranial neurological extension muscles in patients with chronic tension-type headache.
Conclusions
In our study, compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower. Our results show a change in the cranio-cervical extensor muscles in patients with chronic tension-type headache. With the decrease in rCSAs of the RCPmin in patients with chronic tension-type headache, their HIT-6 scores and NDI scores increased. The more evident the RCPmin atrophy, the worse the QoL of the patients with chronic tension-type headache. However, it remains unclear whether atrophy of the neck muscles leads to the occurrence of chronic tension-type headache or whether chronic tension-type headache leads to changes in the neck muscles. More experiments are required to explore the pathophysiology related to changes in the cervical extensor muscles to provide a basis for the clinical diagnosis and treatment of chronic tension-type headache.
Figures
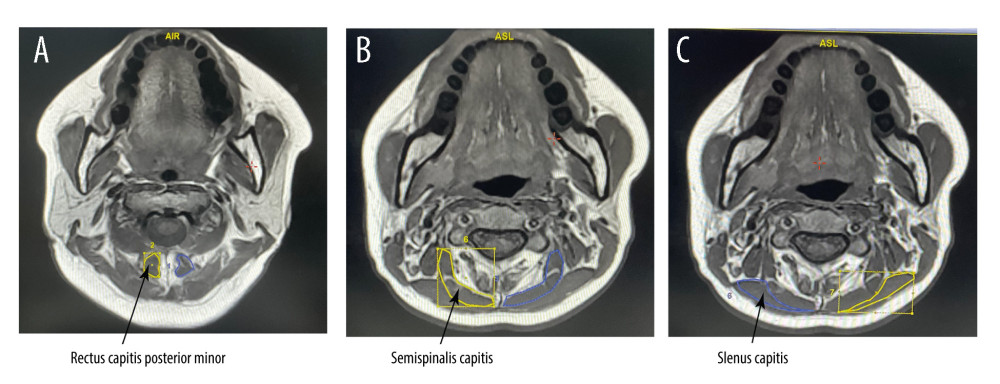 Figure 1. (A–C) Posterior cervical extensor muscles on magnetic resonance imagingIn this study we tested 3 muscles: the rectus capitis posterior minor, semispinalis capitis, and splenius capitis. The blue and yellow parts in the picture are the cross-sectional areas of the muscles we tested. This figure was created using Adobe Illustrator CC 2018 (Adobe).
Figure 1. (A–C) Posterior cervical extensor muscles on magnetic resonance imagingIn this study we tested 3 muscles: the rectus capitis posterior minor, semispinalis capitis, and splenius capitis. The blue and yellow parts in the picture are the cross-sectional areas of the muscles we tested. This figure was created using Adobe Illustrator CC 2018 (Adobe). 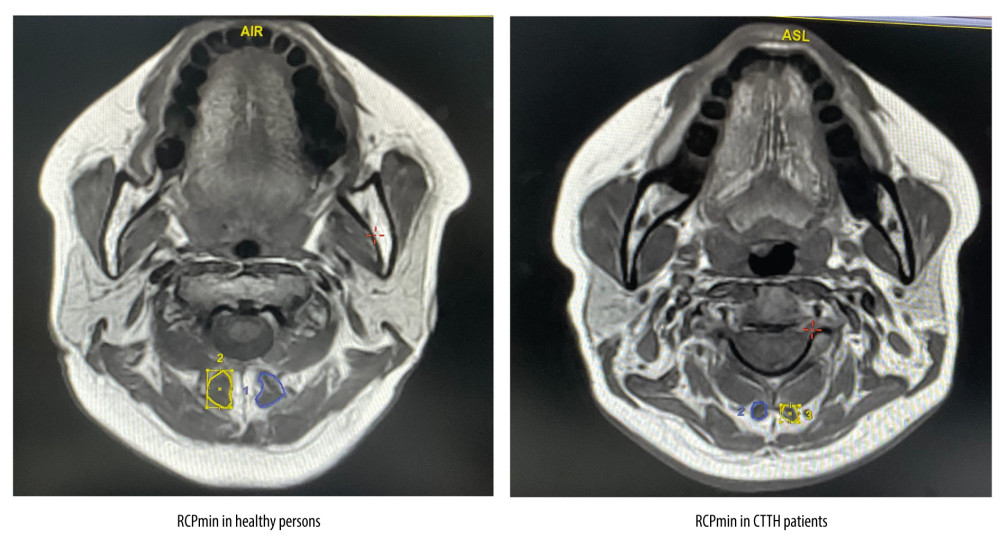 Figure 2. The rectus capitis posterior minor (RCPmin) in patients with chronic tension-type headache and healthy controlsThe blue and yellow parts in the picture are the cross-sectional areas of the RCPmin. Compared with the healthy controls, the RCPmin of CCTH patients was atrophic. This figure was created using Adobe Illustrator CC 2018 (Adobe).
Figure 2. The rectus capitis posterior minor (RCPmin) in patients with chronic tension-type headache and healthy controlsThe blue and yellow parts in the picture are the cross-sectional areas of the RCPmin. Compared with the healthy controls, the RCPmin of CCTH patients was atrophic. This figure was created using Adobe Illustrator CC 2018 (Adobe). 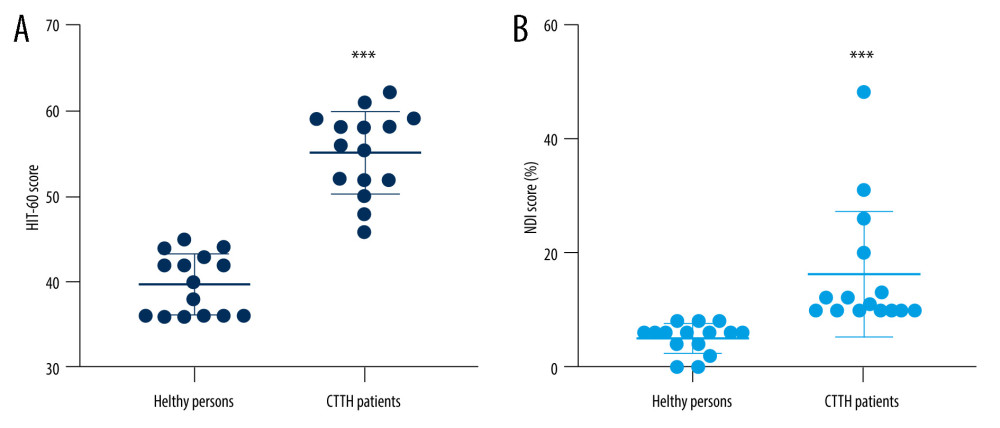 Figure 3. Comparison of Headache Impact Test-6 (HIT-6) and Neck Disability Index (NDI) scores between patients with chronic tension-type headache and healthy controlsThe scatter diagram of HIT-6 (A) and NDI (B) scores in the 2 groups. The HIT-6 scores of patients with chronic tension-type headache (55.07±4.83) were significantly higher than those of healthy volunteers (39.73±3.56). The neck function impairment index of patients with chronic tension-type headache (16.2±10.96%) was significantly higher than that of healthy volunteers (5.01±2.60%). This figure was created using GraphPad Prism version 6 (GraphPad Software). *** P<0.0001 compared with healthy controls (Wilcoxon rank-sum test).
Figure 3. Comparison of Headache Impact Test-6 (HIT-6) and Neck Disability Index (NDI) scores between patients with chronic tension-type headache and healthy controlsThe scatter diagram of HIT-6 (A) and NDI (B) scores in the 2 groups. The HIT-6 scores of patients with chronic tension-type headache (55.07±4.83) were significantly higher than those of healthy volunteers (39.73±3.56). The neck function impairment index of patients with chronic tension-type headache (16.2±10.96%) was significantly higher than that of healthy volunteers (5.01±2.60%). This figure was created using GraphPad Prism version 6 (GraphPad Software). *** P<0.0001 compared with healthy controls (Wilcoxon rank-sum test). Tables
Table 1. Criteria for determining the effect of the different Headache Impact Test-6 (HIT-6) scores on quality of life (QoL).The total score of the HIT-6 should be between 36 and 78. The higher the score of the subjects, the greater the effect of headaches on QoL.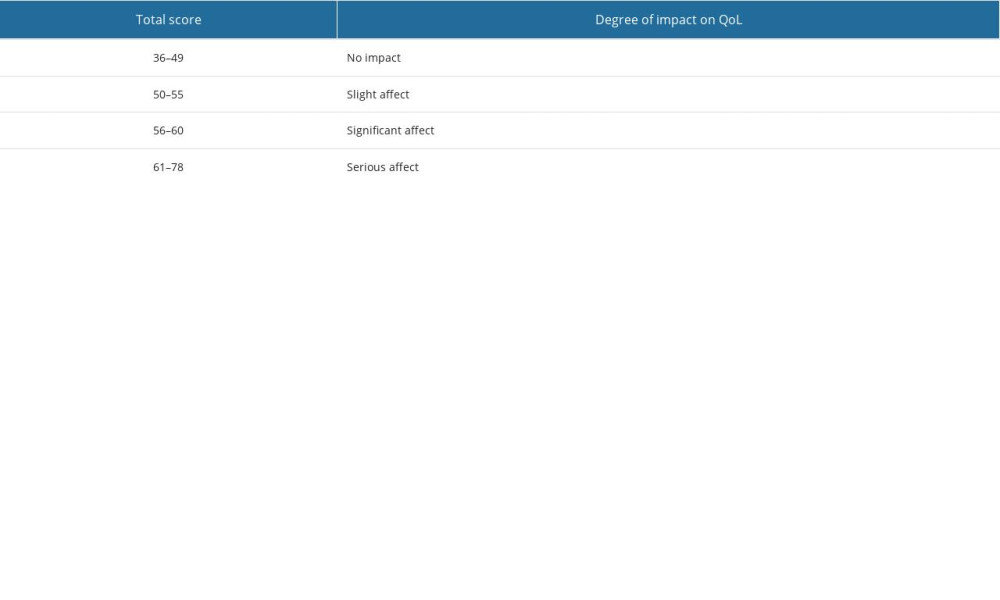 Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.
Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.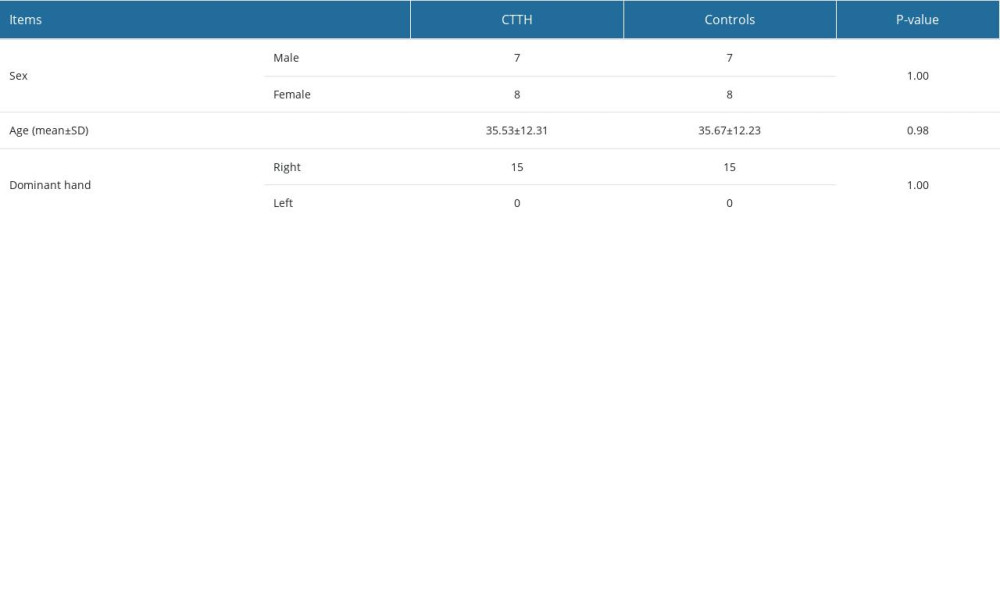 Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).
Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).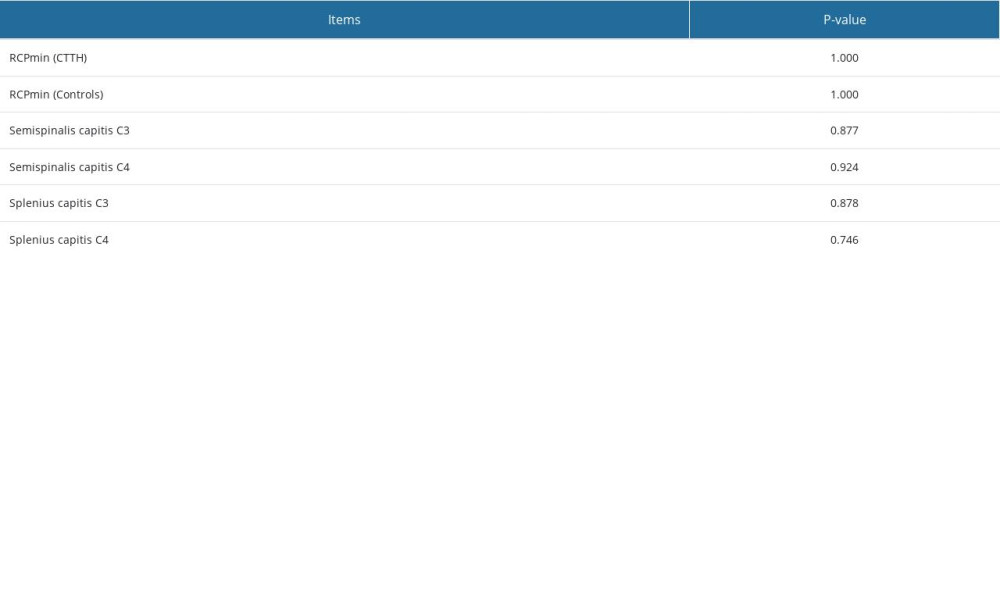 Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4).
Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4).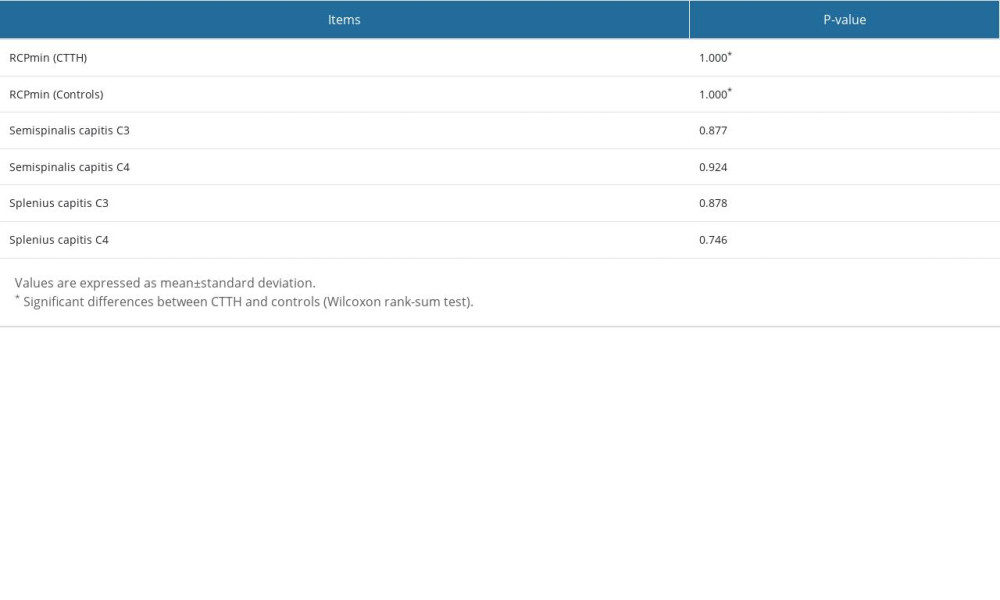
References
1. Speciali JG, Eckeli AL, Dach F, Tension-type headache: Expert Rev Neurother, 2008; 8(5); 839-53
2. Belyaeva II, Subbotina AG, Eremenko II, Pharmacogenetics in primary headache disorders: Front Pharmacol, 2022; 12; 820214
3. GBD 2016 Headache Collaborators, Global, regional, and national burden of migraine and tension-type headache, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016: Lancet Neurol, 2018; 17(11); 954-76
4. Rasmussen BK, Jensen R, Schroll M, Olesen J, Epidemiology of headache in a general population – a prevalence study: J Clin Epidemiol, 1991; 44(11); 1147-57
5. Crystal SC, Robbins MS, Epidemiology of tension-type headache: Curr Pain Headache Rep, 2010; 14(6); 449-54
6. Schwartz BS, Stewart WF, Simon D, Lipton RB, Epidemiology of tension-type headache: JAMA, 1998; 279(5); 381-83
7. Uhlig BL, Engstrøm M, Ødegård SS, Headache and insomnia in population-based epidemiological studies: Cephalalgia, 2014; 34(10); 745-51
8. Lampl C, Thomas H, Tassorelli C, Headache, depression and anxiety: Associations in the Eurolight project: J Headache Pain, 2016; 17; 59
9. Fuensalida-Novo S, Palacios-Ceña M, Fernández-Muñoz JJ, The burden of headache is associated to pain interference, depression and headache duration in chronic tension type headache: A 1-year longitudinal study: J Headache Pain, 2017; 18(1); 119
10. Lipton RB, Stewart WF, Cady R, 2000 Wolfe Award: Sumatriptan for the range of headaches in migraine sufferers: results of the Spectrum Study: Headache, 2000; 40(10); 783-91
11. Bendtsen L, Evers S, Linde M, EFNS guideline on the treatment of tension-type headache – report of an EFNS task force: Eur J Neurol, 2010; 17(11); 1318-25
12. McPartland JM, Brodeur RR, Hallgren RC, Chronic neck pain, standing balance, and suboccipital muscle atrophy – a pilot study: J Manipulative Physiol Ther, 1997; 20(1); 24-29
13. Fernández-de-Las-Peñas C, Bueno A, Ferrando J, Elliott JM, Magnetic resonance imaging study of the morphometry of cervical extensor muscles in chronic tension-type headache: Cephalalgia, 2007; 27(4); 355-62
14. Oksanen Airi, Erkintalo M, Metsähonkala L, Neck muscles’ cross-sectional area in adolescents with and without headache – MRI study: Eur J Pain, 2008; 12(7); 952-59
15. Lee E, Lee S, Impact of cervical sensory feedback for forward head posture on headache severity and physiological factors in patients with tension-type headache: A randomized, single-blind, controlled trial: Med Sci Monit, 2019; 25; 9572-84
16. Choi W, Effect of 4 weeks of cervical deep muscle flexion exercise on headache and sleep disorder in patients with tension headache and forward head posture: Int J Environ Res Public Health, 2021; 18(7); 3410
17. Tagliafico AS, Bignotti B, Torri L, Rossi F, Sarcopenia: How to measure, when and why: Radiol Med, 2022; 127(3); 228-37
18. Kaltseis K, Frank F, Bernar B, Primary headache disorders in adolescents in North- and South-Tyrol: Findings of the EVA-Tyrol-Study: Cephalalgia, 2022; 42(10); 993-1004
19. Escaloni J, Butts R, Dunning J, The use of dry needling as a diagnostic tool and clinical treatment for cervicogenic dizziness: A narrative review & case series: J Bodyw Mov Ther, 2018; 22(4); 947-55
20. Hallgren RC, Pierce SJ, Sharma DB, Rowan JJ, Forward head posture and activation of rectus capitis posterior muscles: J Am Osteopath Assoc, 2017; 117(1); 24-31
21. Elliott JM, Jull GA, Noteboom JT, Durbridge GL, Gibbon WW, Magnetic resonance imaging study of cross-sectional area of the cervical extensor musculature in an asymptomatic cohort: Clin Anat, 2007; 20(1); 35-40
22. Bae JY, Sung HK, Kwon NY, Cognitive behavioral therapy for migraine headache: A systematic review and meta-analysis: Medicina (Kaunas), 2021; 58(1); 44
23. Kosinski M, Bayliss MS, Bjorner JB, A six-item short-form survey for measuring headache impact: The HIT-6: Qual Life Res, 2003; 12(8); 963-74
24. Charalampidis A, Hejrati N, Ramakonar H, Clinical outcomes and revision rates following four-level anterior cervical discectomy and fusion: Sci Rep, 2022; 12(1); 5339
25. Vernon H, The Neck Disability Index: State-of-the-art, 1991–2008: J Manipulative Physiol Ther, 2008; 31(7); 491-502
26. Ploumis A, Michailidis N, Christodoulou P, Ipsilateral atrophy of paraspinal and psoas muscle in unilateral back pain patients with monosegmental degenerative disc disease: Br J Radiol, 2011; 84(1004); 709-13
27. Cankurtaran D, Yigman ZA, Umay E, Factors associated with paravertebral muscle cross-sectional area in patients with chronic low back pain: Korean J Pain, 2021; 34(4); 454-62
28. Hack GD, Koritzer RT, Robinson WL, Anatomic relation between the rectus capitis posterior minor muscle and the dura mater: Spine (Phila Pa 1976), 1995; 20(23); 2484-86
29. Nash L, Nicholson H, Lee AS, Configuration of the connective tissue in the posterior atlanto-occipital interspace: A sheet plastination and confocal microscopy study: Spine (Phila Pa 1976), 2005; 30(12); 1359-66
30. Palomeque-Del-Cerro L, Arráez-Aybar LA, Rodríguez-Blanco C, A systematic review of the soft-tissue connections between neck muscles and dura mater: The myodural bridge: Spine (Phila Pa 1976), 2017; 42(1); 49-54
31. Venne G, Rasquinha BJ, Kunz M, Ellis RE, Rectus capitis posterior minor: Histological and biomechanical links to the spinal dura mater: Spine (Phila Pa 1976), 2017; 42(8); E466-73
32. Uthaikhup S, Assapun J, Kothan S, Structural changes of the cervical muscles in elder women with cervicogenic headache: Musculoskelet Sci Pract, 2017; 29; 1-6
33. Scali F, Pontell ME, Enix DE, Marshall E, Histological analysis of the rectus capitis posterior major’s myodural bridge: Spine J, 2013; 13(5); 558-63
34. Hallgren RC, Greenman PE, Rechtien JJ, Atrophy of suboccipital muscles in patients with chronic pain: A pilot study: J Am Osteopath Assoc, 1994; 94(12); 1032-38
35. Madsen BK, Søgaard K, Andersen LL, Efficacy of strength training on tension-type headache: A randomised controlled study: Cephalalgia, 2018; 38(6); 1071-80
36. Nolan JP, Sherk HH, Biomechanical evaluation of the extensor musculature of the cervical spine: Spine (Phila Pa 1976), 1988; 13(1); 9-11
Errate
Figures
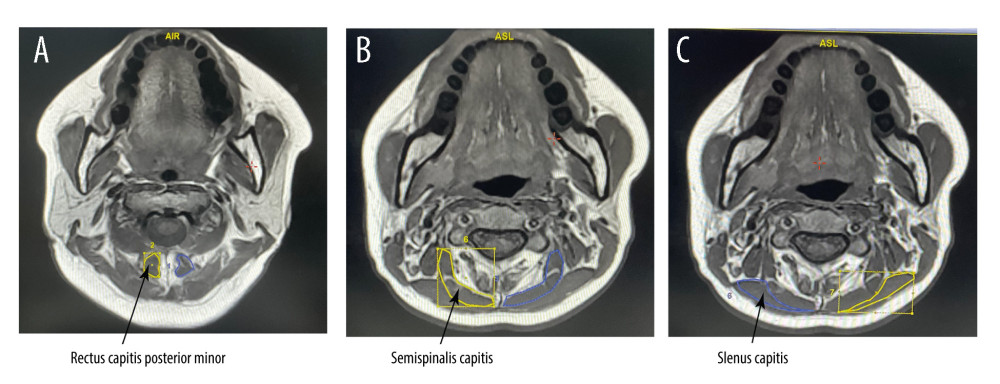 Figure 1. (A–C) Posterior cervical extensor muscles on magnetic resonance imagingIn this study we tested 3 muscles: the rectus capitis posterior minor, semispinalis capitis, and splenius capitis. The blue and yellow parts in the picture are the cross-sectional areas of the muscles we tested. This figure was created using Adobe Illustrator CC 2018 (Adobe).
Figure 1. (A–C) Posterior cervical extensor muscles on magnetic resonance imagingIn this study we tested 3 muscles: the rectus capitis posterior minor, semispinalis capitis, and splenius capitis. The blue and yellow parts in the picture are the cross-sectional areas of the muscles we tested. This figure was created using Adobe Illustrator CC 2018 (Adobe).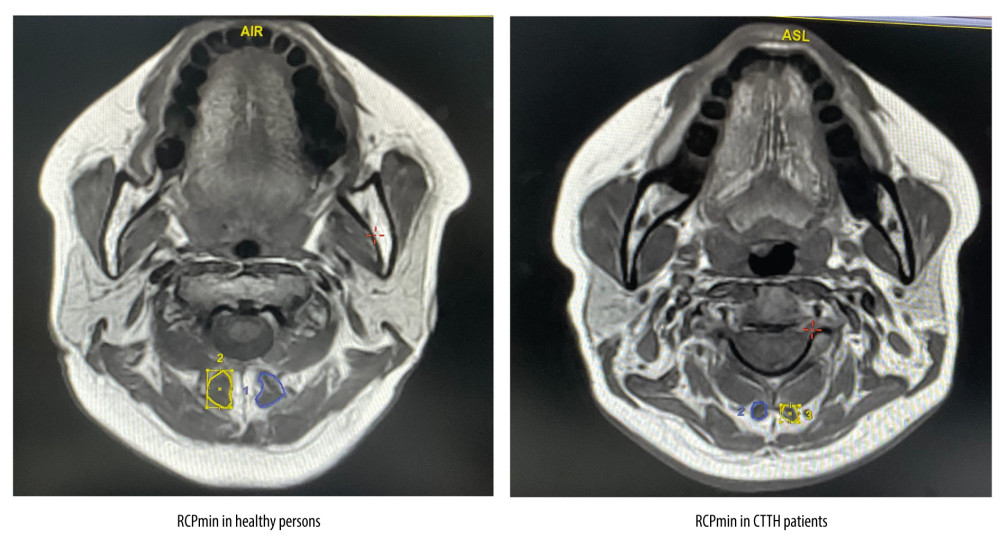 Figure 2. The rectus capitis posterior minor (RCPmin) in patients with chronic tension-type headache and healthy controlsThe blue and yellow parts in the picture are the cross-sectional areas of the RCPmin. Compared with the healthy controls, the RCPmin of CCTH patients was atrophic. This figure was created using Adobe Illustrator CC 2018 (Adobe).
Figure 2. The rectus capitis posterior minor (RCPmin) in patients with chronic tension-type headache and healthy controlsThe blue and yellow parts in the picture are the cross-sectional areas of the RCPmin. Compared with the healthy controls, the RCPmin of CCTH patients was atrophic. This figure was created using Adobe Illustrator CC 2018 (Adobe).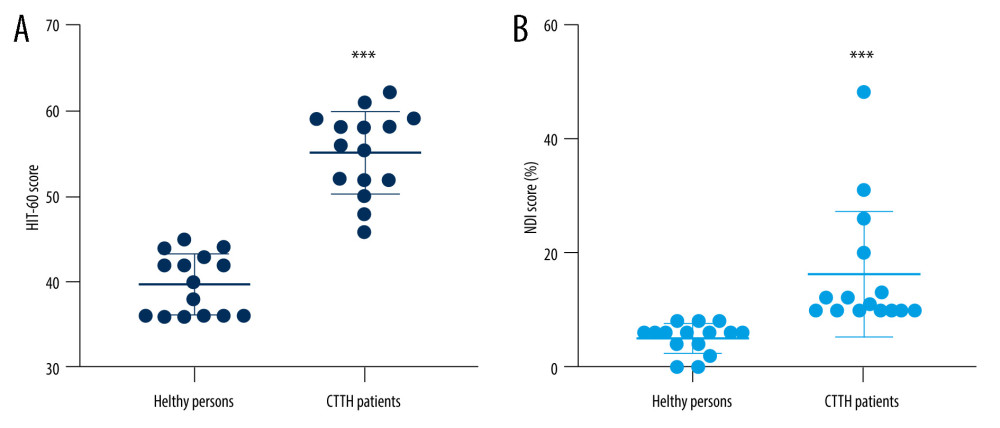 Figure 3. Comparison of Headache Impact Test-6 (HIT-6) and Neck Disability Index (NDI) scores between patients with chronic tension-type headache and healthy controlsThe scatter diagram of HIT-6 (A) and NDI (B) scores in the 2 groups. The HIT-6 scores of patients with chronic tension-type headache (55.07±4.83) were significantly higher than those of healthy volunteers (39.73±3.56). The neck function impairment index of patients with chronic tension-type headache (16.2±10.96%) was significantly higher than that of healthy volunteers (5.01±2.60%). This figure was created using GraphPad Prism version 6 (GraphPad Software). *** P<0.0001 compared with healthy controls (Wilcoxon rank-sum test).
Figure 3. Comparison of Headache Impact Test-6 (HIT-6) and Neck Disability Index (NDI) scores between patients with chronic tension-type headache and healthy controlsThe scatter diagram of HIT-6 (A) and NDI (B) scores in the 2 groups. The HIT-6 scores of patients with chronic tension-type headache (55.07±4.83) were significantly higher than those of healthy volunteers (39.73±3.56). The neck function impairment index of patients with chronic tension-type headache (16.2±10.96%) was significantly higher than that of healthy volunteers (5.01±2.60%). This figure was created using GraphPad Prism version 6 (GraphPad Software). *** P<0.0001 compared with healthy controls (Wilcoxon rank-sum test). Tables
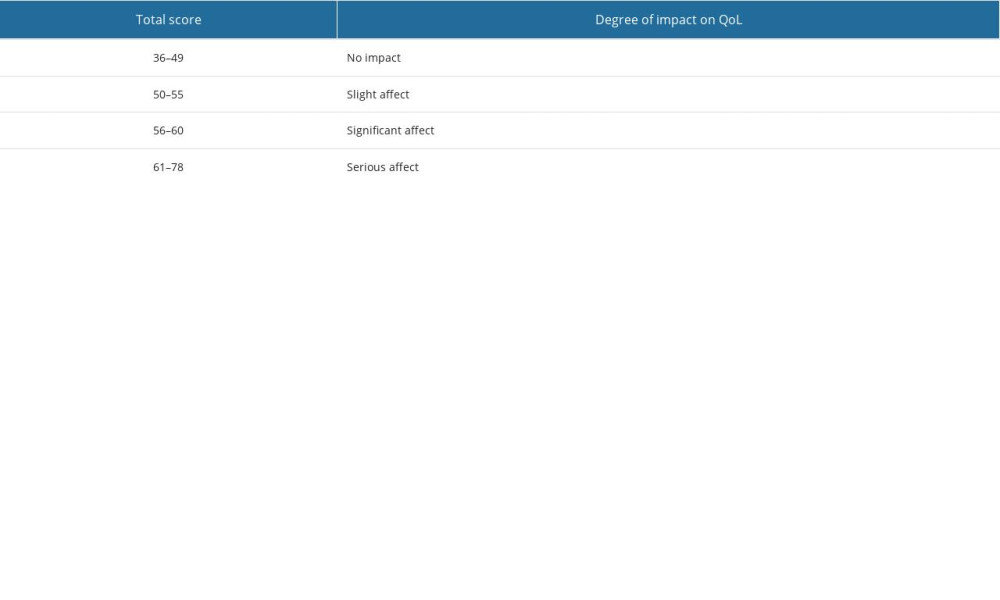 Table 1. Criteria for determining the effect of the different Headache Impact Test-6 (HIT-6) scores on quality of life (QoL).The total score of the HIT-6 should be between 36 and 78. The higher the score of the subjects, the greater the effect of headaches on QoL.
Table 1. Criteria for determining the effect of the different Headache Impact Test-6 (HIT-6) scores on quality of life (QoL).The total score of the HIT-6 should be between 36 and 78. The higher the score of the subjects, the greater the effect of headaches on QoL.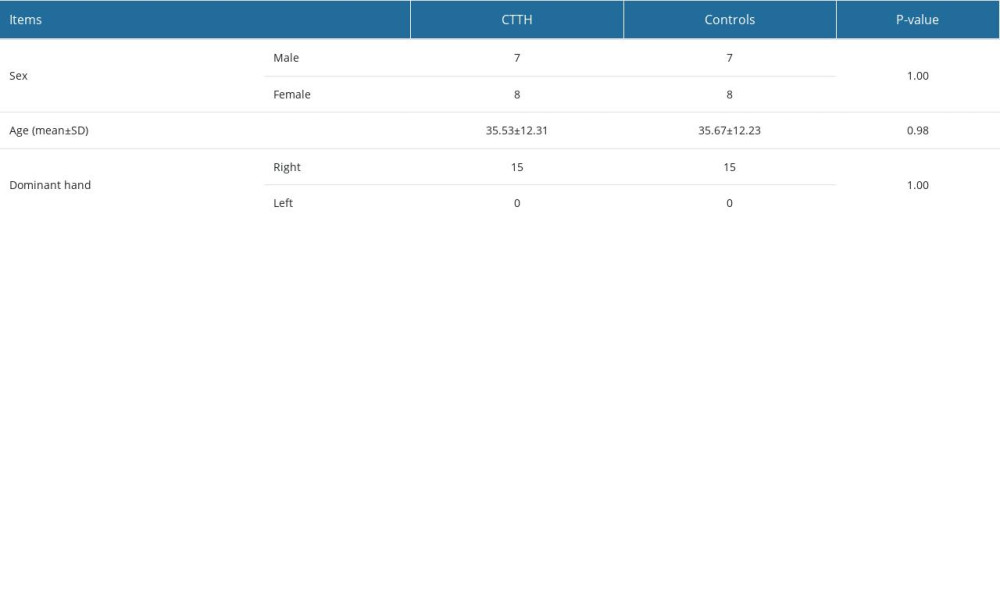 Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.
Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.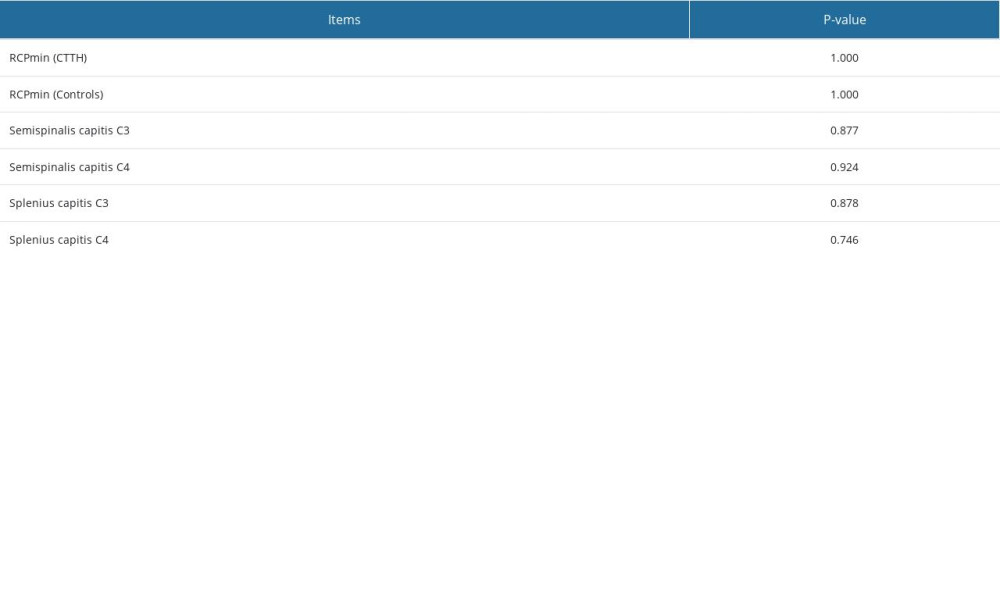 Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).
Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).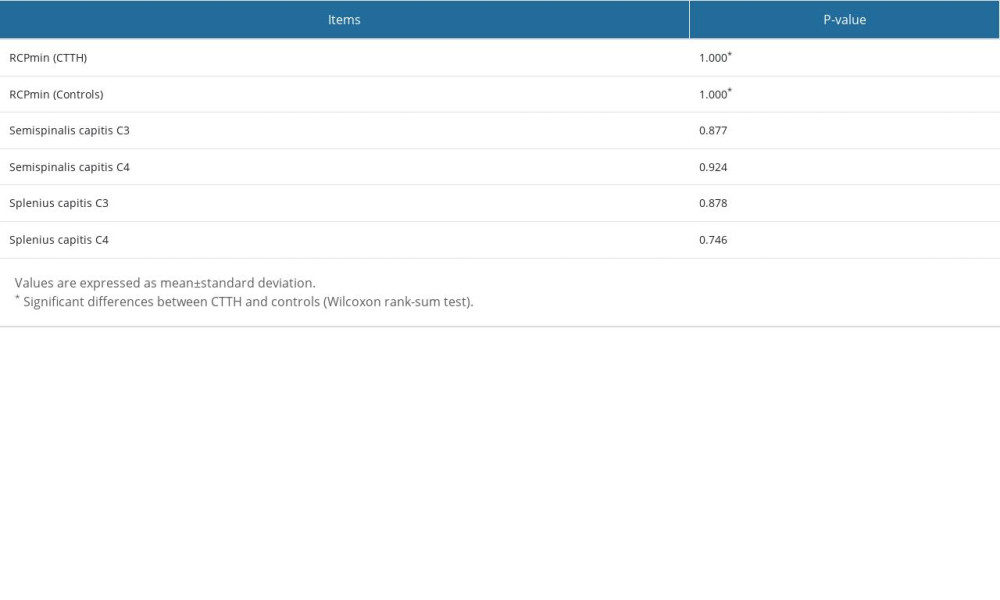 Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4).
Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4).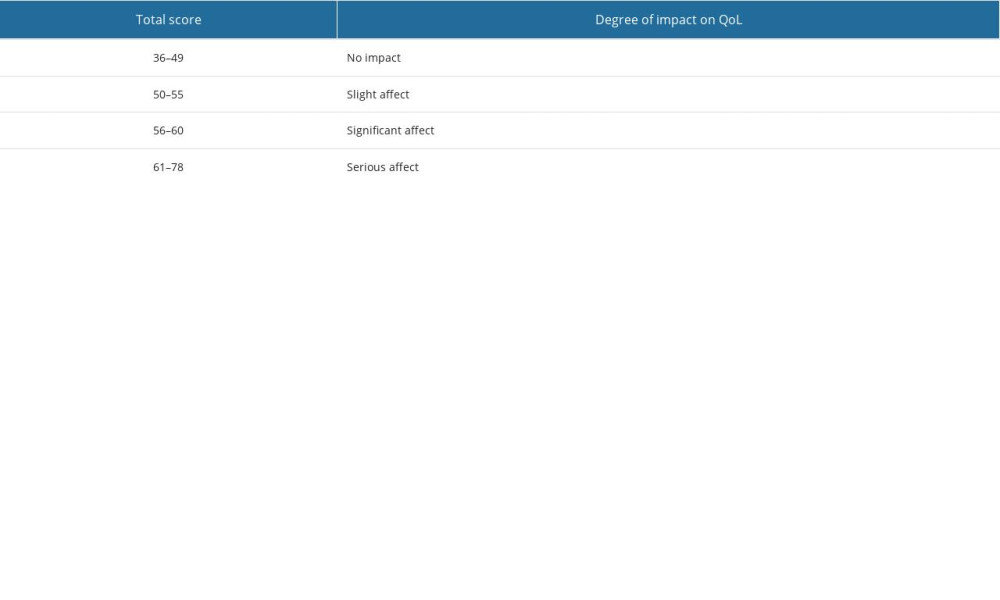 Table 1. Criteria for determining the effect of the different Headache Impact Test-6 (HIT-6) scores on quality of life (QoL).The total score of the HIT-6 should be between 36 and 78. The higher the score of the subjects, the greater the effect of headaches on QoL.
Table 1. Criteria for determining the effect of the different Headache Impact Test-6 (HIT-6) scores on quality of life (QoL).The total score of the HIT-6 should be between 36 and 78. The higher the score of the subjects, the greater the effect of headaches on QoL.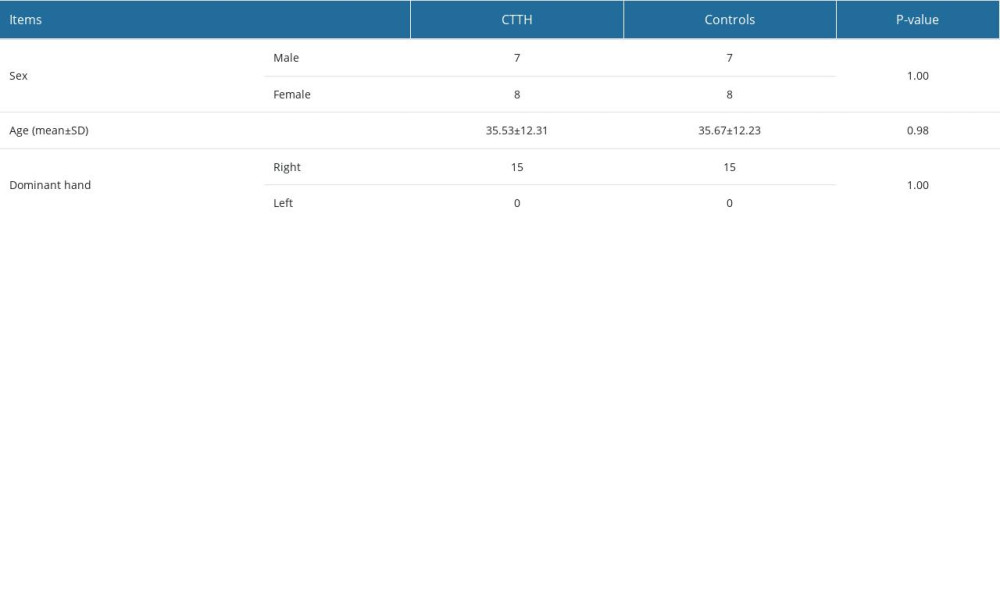 Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.
Table 2. Baseline characteristics of subjects.Fifteen age-, sex-, and dominant-hand-matched healthy controls were included in this study. The demographic characteristics included sex, age, and dominant hand.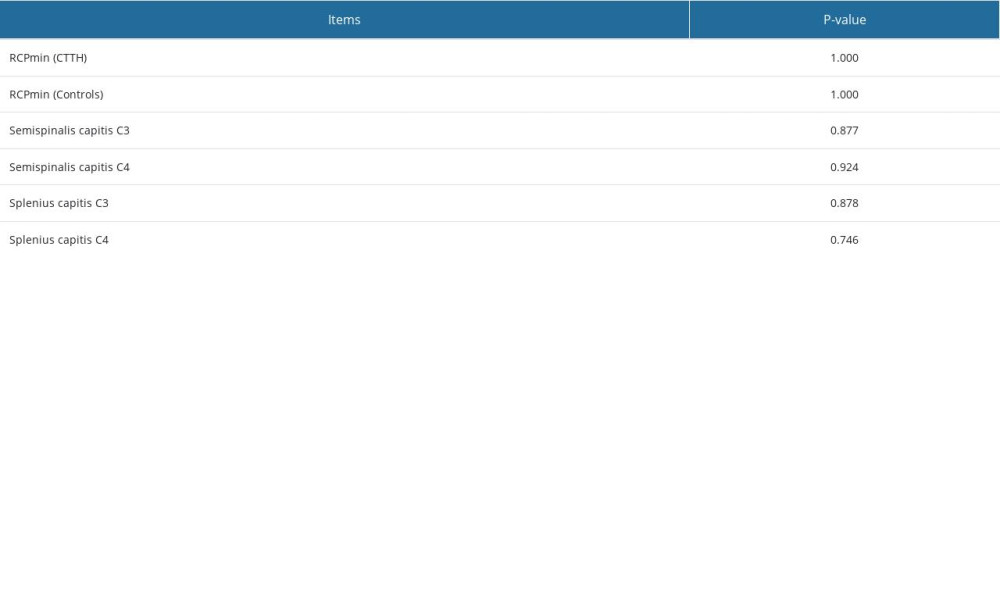 Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).
Table 3. Difference in relative cross-sectional area of the left and right muscles.No significant difference was found in the left and right muscles of each subject in all patients with chronic tension-type headache and healthy individuals (P>0.05).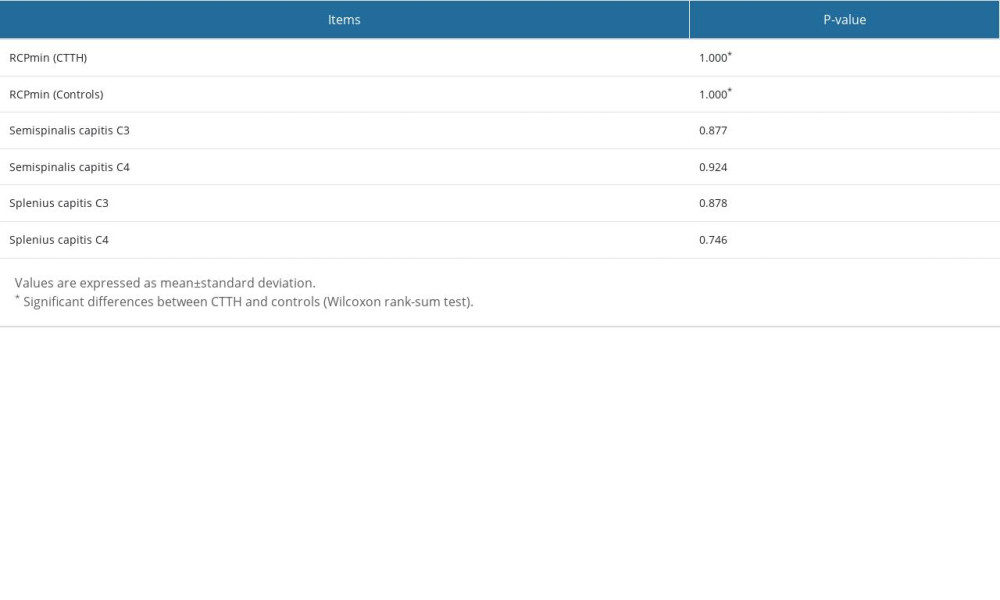 Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4).
Table 4. Differences in relative cross-sectional areas (rCSAs) between patients with chronic tension-type headache and healthy controls.Compared with healthy controls, the rCSAs of the RCPmin in patients with chronic tension-type headache were lower (P<0.001 and P<0.001 for RCPmin right side and RCPmin left side, respectively). At C3 and C4 levels, there was no significant difference in the rCSAs of the semispinalis capitis and splenius capitis between patients with chronic tension-type headache and controls (P>0.4). In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








