22 February 2023: Review Articles
Necessity and Importance of Developing AI in Anesthesia from the Perspective of Clinical Safety and Information Security
Bijia Song1ABCDE, Ming Zhou2AB, Junchao Zhu1ABCDEFG*DOI: 10.12659/MSM.938835
Med Sci Monit 2023; 29:e938835
Abstract
ABSTRACT: The rapid development of artificial intelligence (AI) technology is due to the significant progress in big data, databases, algorithms, and computing power, and medical research is a vital application direction of AI. The integrated development of AI and medicine has improved medical technology, and the efficiency of medical services and equipment has enabled doctors to better serve patients. The tasks and characteristics of the anesthesia discipline also make AI necessary for its development, and AI has also been initially applied in different fields of anesthesia. Our review aims to clarify the current situation and challenges of AI application in anesthesiology to provide clinical references and guide the future development of AI in anesthesiology. This review summarizes progress in the application of AI in perioperative risk assessment and prediction, deep monitoring and regulation of anesthesia, essential anesthesia skills operation, automatic drug administration systems, and teaching and training in anesthesia. Also discussed herein are the accompanying risks and challenges of applying AI in anesthesia: patient privacy and information security, data sources, and ethical issues, lack of capital and talent, and the “black box” phenomenon.
Keywords: Anesthesia, Artificial Intelligence, Humans, Anesthesiology, Algorithms, Big Data
Background
Artificial intelligence (AI) is a new technical science to research and develop theories, methods, technologies, and application systems for simulating and extending human intelligence, mainly using algorithms for reasoning about problems and performing tasks. Since the Dartmouth Conference in 1956, AI has been developed for more than 60 years and has experienced different development stages, including computing intelligence, perceptual intelligence, and cognitive intelligence. AI technologies include learning methods such as machine learning (ML) and deep learning (DL), natural language processing, speech and image recognition, and expert systems [1,2]. DL includes convolutional neural networks (CNNs), artificial neural networks (ANNs), and recurrent neural networks (RNNs) (Figure 1). CNNs are characterized by utilizing filters to extract features and then correlating features in its different layers by utilizing convolutions rather than general matrix multiplication. Image processing, computer vision, and pattern recognition are applications of CNNs [3]. ANNS, usually simply called neural networks (NNs) or neural nets, are computing systems inspired by the biological neural networks that constitute animal brains. Application areas include system identification and control (vehicle control, trajectory prediction, process control, natural resource management), quantum chemistry, general game playing, and pattern recognition (eg, radar systems, face identification, signal classification, and medical diagnosis). ANNs have been used to diagnose several types of cancers and to distinguish highly invasive cancer cell lines from less invasive lines using only cell shape information [4]. RNNs are a class of artificial neural networks where connections between nodes can create a cycle, allowing output from some nodes to affect subsequent input to the same nodes. This allows it to exhibit temporal dynamic behavior. Applications of RNNs include machine translation, robot control, time series prediction, speech recognition, speech synthesis, and brain–computer interfaces. There are several prediction tasks in the area of business process management and prediction in medical care pathways [5].
AI has been applied to various aspects of medicine, from numerous diagnostic applications in radiology and pathology to more therapeutic and interventional applications in cardiology and surgery [6–9]. The 2017 State Council development Plan for a New Generation of Artificial Intelligence and the 2018 Government Work Report highlighted the application of AI in the medical field [10]. Anesthesiology as a field is positioned on multiple elements of clinical care, including perioperative and intensive care, pain management, and drug delivery and discovery [11]. The application of AI in the field of anesthesia is also thriving, including in airway management, ultrasonic-assisted diagnosis, intelligent drug infusion systems, accurate intraoperative monitoring and early warning, perioperative complications, and fatality prediction and intensive care treatment; this can change clinical anesthesia practice, optimize treatment processes, and improve patient prognosis. Thus, mastering AI technology is crucial to providing safe, efficient, and cost-effective clinical anesthesia [12]. In addition, with the development and maturity of AI systems in the medical field, AI will be widely used in clinical work. This could also impact traditional medical models, thus causing new social, economic, and legal problems. Dealing with the many issues brought about by AI and ensuring its safe and controllable development is also a crucial problem. Therefore, in this review, the current situation of AI in the field of anesthesia is summarized, the prospects and challenges of AI in anesthesia are discussed, and relevant policy suggestions for the application and development of AI in anesthesia are presented.
Basics of AI and Its Characteristics in the Development of Anesthesia
AI is a vast field where machine learning (ML) forms a subfield. ML is a good form of AI best suited to the predictive analytics required for clinical decision-making [13]. ML focuses on developing computer systems that can learn from big data (or data of such volume, collection velocity, or complexity that it is difficult or impossible to process using traditional methods) [14], identifying patterns, and making decisions with minimal human intervention [15].
Over the last half century, improvements in short-acting drugs and patient monitoring have sparked interest in anesthesia administration as a target for automation [16]. In the field of anesthesia, AI and ML have penetrated many health areas, and the application of both in anesthesia is booming. Large amounts of medical and health data can be generated in electronic medical records, perioperative monitoring devices, or portable electronics worn by patients. Meanwhile, AI and ML have significant advantages in airway management, ultrasound-assisted diagnosis, intelligent drug infusion systems, accurate intraoperative monitoring and early warning, perioperative complications, fatality prediction, intensive care treatment, and others. It can change clinical anesthesia practice, optimize the treatment process, and improve patient prognosis. Therefore, mastering AI technology is crucial to providing safe, efficient, and cost-effective clinical anesthesia.
Prospect of AI in the Development of Anesthesia
ROLE OF ARTIFICIAL INTELLIGENCE IN PREOPERATIVE MEDICINE:
Comprehensive and accurate preoperative evaluation is an integral part of the work of clinical anesthesiologists; it can identify risk factors, screen patients at high risk, and help them to improve their preoperative preparation. Active intervention to reduce risks guarantees improved quality of anesthesia management and reduced incidence of perioperative complications and mortality.
Anticipating difficulty airway assessment has been the focus of preoperative anesthesia evaluation for many years, perhaps since the advent of anesthesia. Existing methods typically use a combination of history and physical examination to estimate the challenge of airway management [17,18]. Several AI methods use objective measures, such as body mass index and thyroid distance, as predictive features, whereas others also use computerized facial analysis and photographs [19–21]. The latter approach may prove beneficial, as many preoperative clinical assessments have been partially or fully converted to telemedicine modalities, driven by the COVID-19 pandemic. Automatic generation of challenging airway alerts can allow preoperative physicians to discuss potential airway management techniques with patients, including risks and benefits, and inform intraoperative clinicians to prepare appropriate airway equipment [22,23]. Moreover, perioperative hypotension is an independent risk factor for adverse postoperative outcomes.
Early identification of high-risk groups, optimized induction, maintenance, and recovery regimens improve patient outcomes. Kendale et al [24] analyzed the occurrence of induced hypotension in 13 323 patients by taking preoperative comorbidities, preoperative medication, induction medication, and intraoperative vital signs as clinical characteristics. Logistic regression, random forest, support vector machine, Naive Bayes, k-nearest neighbors, linear discriminant analysis, neural network, and gradient boosting were used for modeling. The model was optimized, and the results confirmed that the ML algorithm could successfully predict the occurrence of hypotension after general anesthesia. Hatib et al [25] determined the compensatory ability of the circulatory system and created a hypotension prediction model according to the characteristics of the invasive arterial pressure waves (eg, arterial pressure wave time, wave amplitude, area under the curve, slope features, Flotrac algorithm features, CO-Trek features, baroreflex features). The advantage of the model is that the probability of hypotension occurrence can be predicted 15 min before its onset, with a sensitivity of 88% and a specificity of 87%. This will provide clinicians with a high-value warning with sufficient time to correct the potentially life-threatening dysfunction and prevent the occurrence of severe hypotension. For the risk assessment of perioperative complications, traditional risk estimation methods mainly rely on carefully constructed cohorts or case-controls to reduce bias, using hypothesis testing and logistics regression to speculate on the relationship between outcome and risk factors. However, in the field of big data, the data structure is often incomplete, and the traditional statistical methods are relatively limited (such as being sensitive to missing values, requiring at least 10–15 events per study variable, and not including too many variables). In these cases, ML shows a great advantage [26,27]. Thottakkara et al [28] used logistic regression and a generalized additive model, Naive Bayes, to support vector machine, and other ML methods to analyze 50 318 high-dimensional clinical data files from the University of Florida Health database to establish postoperative sepsis and acute kidney injury prediction models. Compared with logistic regression, the generalized additive model and support vector machine algorithm significantly improved the prediction performance. Another study, by Corey et al, analyzed 194 clinical characteristics (patient demographics, comorbidities) of 66 370 patients who underwent 99 755 invasive procedures to create and validate an ML model for identifying high-risk surgical patients. Additionally, this tool has been shown to outperform the ACS NSQUIP calculator [29].
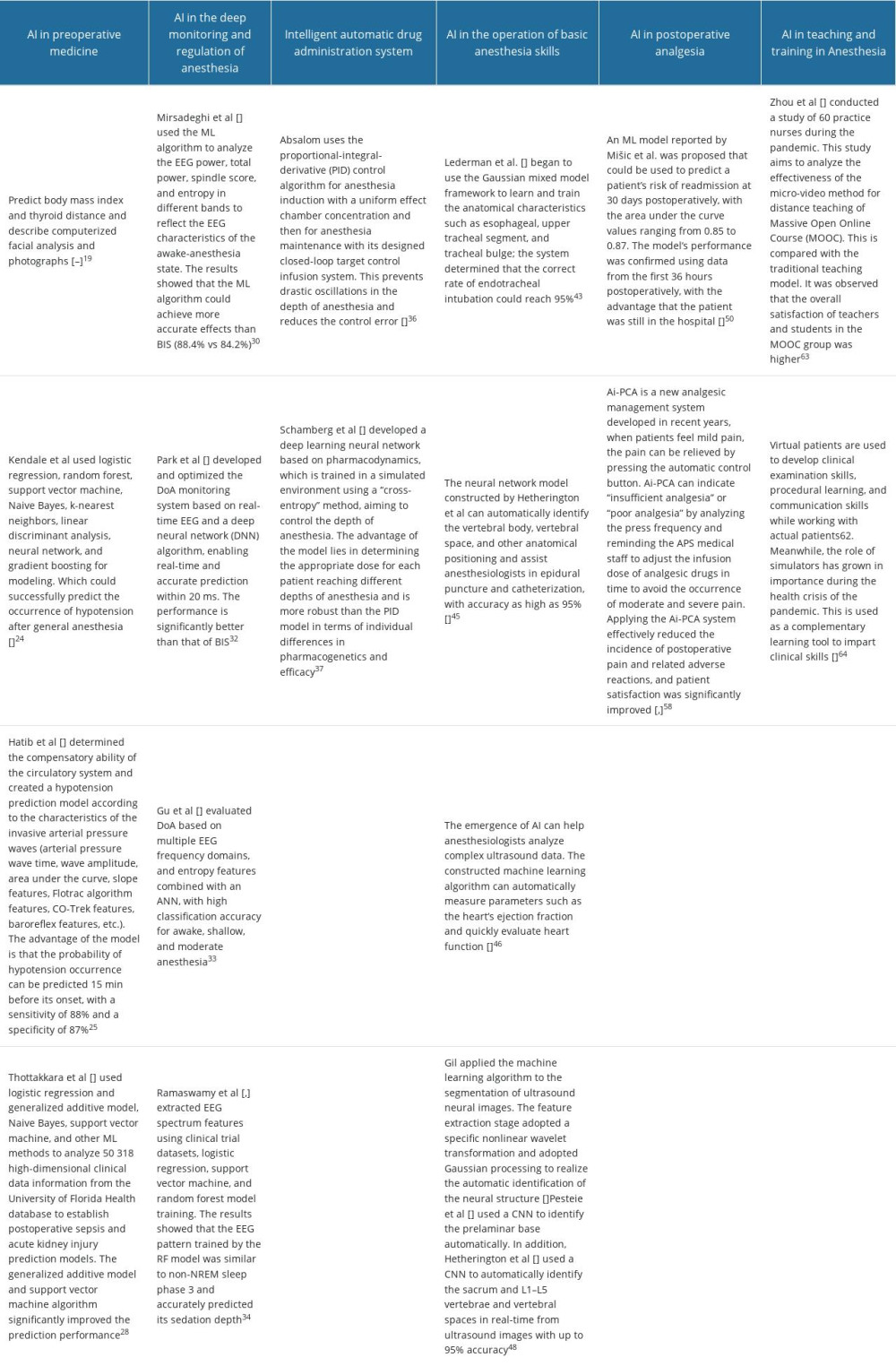
Successful integration of AI into surgical decision-making requires data standardization, efficiently interpretable models, accuracy of clinical monitoring, and attention to ethical challenges. However, the direct doctor–patient relationship and the role of human intuition in the decision-making process must be maintained. When appropriately applied, AI has the potential to optimize different stages of the perioperative pathway, from surgical indications and the informed consent process to the management of risk factors and adverse events (Table 1).
APPLICATION OF AI IN THE DEEP MONITORING AND REGULATION OF ANESTHESIA:
The depth of anesthesia (DoA) is the response to the central nervous systems between the inhibition of anesthetic drugs and the irritation of nociceptive stimuli. In recent years, many studies have shown that anesthesia that is too deep is closely related to postoperative mortality, whereas that which is too shallow increases the risk of patients suffering intraoperative awareness. Close monitoring and timely adjustment of the depth of anesthesia is the core work of clinical anesthesiologists and the essential requirement of accurate anesthesia. The clinical anesthetic depth monitoring method is mainly based on analysis of EEG signals, among which the bispectral index (BIS) is the most widely used. However, its stability and anti-interference ability still need to be improved, the correlation with nociceptive stimulation is also poor. A more comprehensive and accurate anesthetic depth monitoring method is still a subject of significant clinical research.
One of the advantages of AI is its strong data processing ability and self-learning ability. The computer can perform statistical analysis of redundant and repeated monitoring data or input signals in the anesthesia machine and monitor. Multiple studies have confirmed that ML models built through AI can be used for perioperative anesthesia management. ML is very suitable for analyzing complex data streams like EEG, which can build advanced models using multiple linear and nonlinear data to better reflect the drugs’ quantity-effect response. Mirsadeghi et al [30] used the ML algorithm to analyze the EEG power, total power, spindle score, and entropy in different bands to reflect the EEG characteristics of the awake-anesthesia state. The results showed that the ML algorithm could achieve more accurate effects than BIS (88.4% vs 84.2%). Shalbaf et al [31] targeted multiple characteristics of the EEG, using the ML algorithm to study the characteristic changes of the EEG at different anesthetic depths. The results show that the accuracy of the machine learning algorithm can reach 92.91%, much higher than the entropy index (77.5%). Furthermore, the effect of EEG by different general anesthesia states or drugs on EEG varies significantly, evaluating the DoA efficacy based on a single feature. Moreover, AI can strengthen EEG anesthesia and consciousness transition characteristics, which makes it suitable for analyzing complex EEG data streams.
A growing number of studies are conducting DoA monitoring of the direct analysis of EEG signals through AI and spectrum analysis to optimize clinical anesthesia management. Park et al [32] developed and optimized the DoA monitoring system based on real-time EEG and a deep neural network (DNN) algorithm, enabling real-time and accurate prediction within 20 ms. The performance is significantly better than that of BIS. Gu et al [33] evaluated DoA based on multiple EEG frequency domains, and entropy features combined with an ANN, with high classification accuracy for awake, shallow, and moderate anesthesia. Ramaswamy et al [34,35] extracted EEG spectrum features using clinical trial datasets, logistic regression, support vector machine, and random forest model training. The results showed that the EEG pattern trained by the RF model was similar to non-NREM sleep phase 3 and accurately predicted its sedation depth. In conclusion, an AI model based on EEG features can be used for accurate prediction of DoA, in which nonlinear dynamic brain function monitoring indicators (such as entropy) are better than in traditional BIS, while ML through multiple parameter EEG features is better than that through single features. Through the optimization of AI algorithm performance, prediction accuracy will be improved, and AI will play an essential role in the development and application of DoA monitoring systems (Table 1).
INTELLIGENT AUTOMATIC DRUG ADMINISTRATION SYSTEM:
The mechanism by which general anesthetic drugs induce the reversible loss of consciousness is still an urgent scientific problem in anesthesia. As early as the 1950s, scientists, according to the pharmacokinetic and pharmacodynamic models of anesthetics, adjusted the infusion speed of anesthetics, controlled the depth of anesthesia, and designed an automated anesthetic drug infusion system so that the anesthetics would maintain a stable target blood concentration. Recently, the target-controlled infusion technique has been widely used in clinical anesthesia. However, a computer cannot dynamically regulate the plasma target concentration or the effector compartment to achieve a new balance once the patient’s hemodynamic changes. This single closed-loop system limits the application of an automatic delivery system.
AI can build mathematical models using various linear or nonlinear data through deep learning and calculate the drug’s quantity–effect relationship according to the pharmacodynamics and its characteristics. AI can guide and optimize the target control of the drug infusion according to the input monitoring data, such as heart rate, blood pressure, and BIS. Absalom [36] used the proportional-integral-derivative (PID) control algorithm for anesthesia induction with a uniform effect chamber concentration and then for anesthesia maintenance with its designed closed-loop target control infusion system. This prevents drastic oscillations in the depth of anesthesia and reduces the control error. Schamberg et al [37] has developed a deep learning neural network based on pharmacodynamics, which is trained in a simulated environment using a “cross-entropy” method, aiming to control the depth of anesthesia. The algorithm first conducts the batch simulation according to specific rules to obtain the point error and decide the following direction according to the error information. After multiple learning, the neural network gradually learns the correspondence between the anesthetic state and propofol concentration. The advantage of the model lies in determining the appropriate dose for each patient reaching different depths of anesthesia and is more robust than the PID model in terms of individual differences in pharmacogenetics and efficacy. However, the automatic drug administration system is imperfect. The following are some of its limitations: 1) Module composition is relatively simple, mainly composed of sedation, analgesia, and muscle relaxation single modules, whereas the advanced automatic drug delivery system should be composed of sedation, analgesia, muscle relaxation, fluid management, blood pressure control, and other modules [38]. 2) The accuracy of the pharmacodynamics feedback index needs improvement. Many studies have reflected the variability of the BIS value, which makes researchers question the current use of the BIS value as a feedback index. Some people suggest using new parameters, such as the nociception index, as an analgesic parameter [39]. 3) Lack of uniform standards – different device manufacturers use various literature searches and consultants to develop their products independently. Having other models for the same intravenous anesthetic may confuse anesthesiologists unfamiliar with pharmacology and limit the spread of this technology [40] (Table 1).
APPLICATION OF AI IN THE OPERATION OF BASIC ANESTHESIA SKILLS:
With the successful development of the Da Vinci robot-assisted surgical system, many scholars have introduced the concept of the intelligent robotic arm to the essential operation related to anesthesia to realize the intelligent and remote management of anesthesia. In 2010, Tighe of the University of Florida School of Medicine reported using a Da Vinci robot to perform endotracheal intubation on a simulated patient [41]. In 2012, MacGill University successfully performed tracheal intubation using its Kepler intubation system (KIS) in 12 patients. However, the Kepler intubation system is the same as Da Vinci, so it is still not real automation [42]. In 2011, Lederman et al began to use the Gaussian mixed model framework to learn and train anatomical characteristics such as esophageal, upper tracheal segment, and tracheal bulge; the system determined that the correct rate of endotracheal intubation could reach 95% [43]. The real-time image recognition function and active visual tracking technology based on machine learning provide a big step toward automation for the development of tracheal intubation robots. REALITI is an automated airway intubation robot based on laryngeal images, developed by the University of Zurich in Switzerland, which can be operated manually or systematically operated automatically. The system recognizes the first anatomical sign, encouraging the operator to convert the mode to the automatic mode. The prompt box appears around the identified anatomy, and the front end of the endoscope will move toward the glottal opening. Once it enters the glottis, the structural image of the tracheal cavity will be provided, and the operator will be prompted for manual confirmation [44]. Furthermore, a nerve block is one of the critical techniques in clinical anesthesia. In the past 20 years, more guiding techniques and methods have been applied in nerve blocks, from the initial method of abnormal sensation to the current nerve stimulator and ultrasound guidance techniques. In recent years, nerve block guidance technology has dramatically developed with regard to medical image fusion technology and AI identification for medical imaging.
The application of AI in perioperative ultrasound can help anesthesiologists identify ultrasound images efficiently and quickly, improve the accuracy of perioperative ultrasound, and reduce the time needed to analyze and judge the results. For example, the neural network model constructed by Hetherington et al can automatically identify the vertebral body, vertebral space, and other anatomical positioning and assist anesthesiologists in epidural puncture and catheterization, with accuracy as high as 95% [45]. In addition, the emergence of AI can help anesthesiologists analyze complex ultrasound data. The constructed machine learning algorithm can automatically measure parameters such as the heart’s ejection fraction and quickly evaluate heart function. The accuracy of the results is equivalent to that of a cardiologist and they are more reproducible than those of a sonologist [46]. Meanwhile, driven by the concept of enhanced recovery after surgery, ultrasound-guided nerve block has also been widely promoted as an essential operation in the discipline of anesthesia. However, there are many difficulties in acquiring and maintaining the skill sets involved in anatomical recognition and needle guidance, limiting clinicians’ confidence in performing ultrasound-guided regional anesthesia. Currently, most peripheral nerve blocks are performed by a small number of experts [47]. ML has been proved to have significant advantages in image recognition. In 2015, Gil applied the machine learning algorithm to the segmentation of ultrasound neural images. The feature extraction stage adopted a specific nonlinear wavelet transformation and used Gaussian processing to realize the automatic identification of the neural structure [48]. In addition to detecting images of specific structures in ultrasound, the researchers used neural networks to help identify vertebral levels and other anatomical landmarks for epidural placement. Pesteie et al [49] used a CNN to identify the prelaminar base automatically. In addition, Hetherington et al [45] used a CNN to automatically identify the sacrum and L1–L5 vertebrae and vertebral spaces in real-time from ultrasound images, with up to 95% accuracy (Table 1).
APPLICATION OF AI IN POSTOPERATIVE ANALGESIA:
AI technology can provide helpful surgical patient management tools even in the postoperative stage. The decision to discharge is a delicate one that often requires analysis of multiple factors simultaneously; understanding how to identify the most vulnerable patients is the basis for research into differentiated surveillance pathways. An ML model reported by Mišic et al was proposed that could be used to predict a patient’s risk of readmission at 30 days postoperatively, with the area under the curve values ranging from 0.85 to 0.87. The model’s performance was confirmed using data from the first 36 h postoperatively, with the advantage that the patient was still in the hospital [50].
Postoperative pain is a common complication during the perioperative phase, and more than 60% of surgical patients have moderate to severe acute pain after surgery [51]. Dolin et al [52] also noted that 41% of surgical patients had moderate to severe postoperative pain, and 24% had inadequate pain relief. Incomplete postoperative analgesia can cause acute pain to develop into chronic pain, leading to hyperalgesia and neuropathic pain and affecting postoperative rehabilitation and quality of life. The incidence of chronic postsurgical pain (CPSP) was 3% to 80%. Pain caused during the perioperative period is a physiological trauma for patients and an essential psychological stressor [53]. Every 10% increase in severe pain time within 24 h resulted in a 1/3 increase in the incidence of postoperative CPSP [54]. Effective pain assessment is necessary to assess the pain level and determine the appropriate time to give patients an individualized treatment regimen. Patients can use patient-controlled analgesia (PCA) technology to continuously press the additional key (Bolus) according to their pain degree, owing to the significant individual differences in pain. In theory, postoperative PCA has its advantages, and the application of PCA should be better than the traditional analgesic methods. It may improve the postoperative analgesic effect, which is widely used [55]. However, PCA also has disadvantages: long PCA treatment cycle, incomplete information feedback, high incidence of incomplete analgesia, high call back rate, and frequent clinical complaints [56].
Because of these issues of PCA, clinicians are forced to find ways to innovate. With the help of AI technologies, AI patient-controlled analgesia (Ai-PCA) technology has emerged. Ai-PCA is a new analgesic management system developed in recent years. Based on the traditional PCA, it integrates the Internet of Things (IoT) technology and AI operation, which helps to improve the work efficiency of acute pain service (APS) [57]. The Ai-PCA system can analyze and prompt relevant adverse events (eg, insufficient or poor analgesia, nausea and vomiting, excessive sedation, itching, dizziness, and respiratory inhibition through abnormal automatic critical pressing frequency) to facilitate the early detection and treatment of APS doctors and nurses in a timely and effective manner. For example, when patients feel mild pain, the pain can be relieved by pressing the automatic control button. Ai-PCA can indicate “insufficient analgesia” or “poor analgesia” by analyzing the press frequency and reminding the APS medical staff to adjust the infusion dose of analgesic drugs in time to avoid the occurrence of moderate and severe pain. When patients have nausea, vomiting, itching, dizziness, and other adverse reactions, they can reduce drug infusions by blocking the PCA lines. At this time, the APS medical staff can detect such patients early through a “blocking” alarm. In addition, the central analgesia monitoring platform can also classify the real-time alarm to help medical personnel distinguish and prevent the bedside alarm sound from bothering patients. This study showed that applying the Ai-PCA system effectively reduced the incidence of postoperative pain and related adverse reactions, and patient satisfaction was significantly improved [58,59]. Current PCA devices are still not intelligent enough. These systems are not equipped with “brains” that can think and make decisions independently. These devices have yet to break through the traditional sense of “intended or required” pain relief, providing salvage rather than preventive pain relief. Prophylactic analgesia is a broader perioperative pain management strategy aimed at preventing the induction of central sensitization, thereby reducing pain intensity and analgesic consumption [60,61] (Table 1).
AI IN TEACHING AND TRAINING IN ANESTHESIA:
Owing to the outbreak of the COVID-19 pandemic, online executive teaching practices have replaced classroom teaching methods. Students need to develop their clinical knowledge continuously, even when real patient contact is limited. Hence, intelligent technologies are reliable to cultivate skills and knowledge [62]. Technology-based learning includes audio recordings, video tutorials, online chatting, and mannequin simulators. This is possible with the help of online teaching apps such as Google meet, Zoom, Cisco Webex, Massive Open Online Course, and National Digital Library of India (NDLI). Zhou et al conducted a study of 60 practice nurses during the pandemic to analyze the effectiveness of the micro-video method for distance teaching of Massive Open Online Course (MOOC) compared with the traditional teaching model. It was observed that the overall satisfaction of teachers and students in the MOOC group was higher [63]. Virtual patients are used to develop clinical examination skills, procedural learning, and communication skills while working with actual patients [64]. Meanwhile, the role of simulators has grown in importance during the health crisis of the pandemic. This is used as a complementary learning tool to impart clinical skills.
Because demand outweighs resource availability, simulation focuses on executing programs efficiently. Therefore, resources can be fully utilized, and the best patient care can be provided. Singh et al reviewed an article based on anesthesiology simulators. Simulators can be device-based, patient-based, or environment-based. Simulator-based training can target multiple skills, such as chest compressions, central venous intubation, tracheal intubation, tracheostomy, and cricothyrotomy. Research shows that residents who undergo a 6-week simulation training program demonstrate better skills than traditional residents. Anesthesiologists proficient in video technology find it easier to handle video laryngoscopy procedures. Proper hand–eye coordination can be achieved through this simulation-based training program. Another perspective of AI-based simulation training can be used to assess the safety of new devices before entering the market [65] (Table 1).
Challenges of AI in Anesthesiology Development
PATIENT PRIVACY AND INFORMATION SECURITY:
“Privacy security” is one of the most important topics; in traditional medical activities, patient privacy is mainly manifested as a kind of physical privacy, and the right to patient privacy means that patients have the right to protect their private parts, medical history, physical defects, unique experiences, encounters, and so on, from unauthorized access. However, AI, sensor technology, and the IoT have realized the interaction between patients and medical staff, medical institutions, and medical equipment, making medical services intelligent.
While data-driven intelligent medicine brings better medical services, data also faces the risk of disclosure in the process of collection, sharing, and use [66]. The medical information security of AI + smart hospitals is mainly reflected in network security. Once a virus attacks the network, or there are security loopholes, patient privacy information and medical information will be leaked. Under the premise of various countries’ GDPR and data security laws, using patient data legally and in compliance has become a considerable challenge for intelligent medicine [67]. Some scholars use desensitization technology to desensitize patient data and then make it public, after which it can be used in various big data studies such as precision medicine. Desensitization refers to deleting sensitive information in patient data (such as name, ID number, and mobile phone number) to hide the patient’s identity. However, attackers can also find the corresponding patient ID by comparing it with the public database, leading to information disclosure [68,69]. To address this problem, some scholars have used differential privacy technology to ensure that the patient data in use are processed before sharing. Patient data adds Gaussian noise, preventing a third party from checking the patient information during the sharing process. Still, privacy technologies need to make a trade-off between security and accuracy. The more noise added to the patient data, the less accurate the machine learning algorithm becomes. This does not fit into the precision medicine scenario (Figure 2B) [70,71]. Faced with this problem, some scholars have proposed homomorphic encryption to protect the patients’ original data. The patients’ data with each institution are encrypted and shared with a third party in this process. The third party receives the data and uses them as training data for the AI technology and ML model. Homomorphic encryption technology ensures data operations of addition, subtraction, multiplication, and division under the ciphertext state are equal to state the same operation so that the homomorphic encryption technology can achieve non-destructive training. In addition, it can ensure the safety of patient data. However, the ciphertext operation in homomorphic encryption technology consumes a lot of time, which needs to be improved for medical treatment with high real-time requirements (Figure 2C) [72,73].
In response to these problems, the proposal of federated learning provides new ideas for healthcare and intelligent medical care. Under the framework of federated learning, each institution locally uses patient data to train a local model, which is aggregated and generated by sharing the local model. The global model achieves the purpose of training the model. In this way, patient data does not go out of the institution and does not need to be shared with other users, so the privacy of patient information is guaranteed. By sharing local models, patient data from various institutions can be used to improve the accuracy of prediction and provide the primary conditions for precision medicine (Figure 2A) [74,75].
LIMITED NUMBER OF DL PROGRAMS WITH EXTERNAL VALIDATION:
DL is a data-driven AI technology that requires a large amount of relevant data to train a good model to help relevant workers perform classification or decision-making tasks. At present, deep learning has a large number of applications in intelligent recommendation, speech recognition, transportation, and medical fields. In terms of medical care, the deep learning model can infer abnormal lesions or disease risks by analyzing and modeling the medical data workload. An external validation study on assistive AI for ultrasound image interpretation in regional anesthesia assessed the use of ScanNav™ (Intelligent Ultrasound, Cardiff, UK), an artificial intelligence-based device that produces a color overlay on real-time ultrasound images to highlight anatomical structures of interest. The device showed high true-positive/true-negative and low false-positive/false-positive rates in identifying key anatomical structures for the performance of 9 peripheral nerve blocks [76]. Zhang et al’s study reported on the first deep-learning segmentation model to apply consensus definitions for the detection, classification, and quantification of geographic atrophy and its constituent features on optical coherence tomography and to assess potential clinical utility through high performance in a real-life external validation [77]. However, at this stage, due to personal data privacy concerns and the constraints of laws and regulations, data of the same structure cannot be used interchangeably, and the sample size of isolated data is not enough to support a high-precision model. First, patient data in medical institutions exist in isolation, and in some special studies, such as the sample size of rare diseases, it still cannot meet the large sample size required for deep learning model training. Therefore, the small sample size has become one of the biggest challenges facing artificial intelligence technology at this stage [78]. Second, the quality of training data is the most important issue determining whether the model is reliable or not. DL relies on a large amount of labeled data, and the quality of image-labeled data determines the results of DL model training. At present, the quality of domestic image annotation has not yet reached a unified standard, and the quality of data is uneven and varied, which will definitely affect the accuracy of the model [79]. Third, for the model, strong generalization is another criterion to measure the quality of a model. Generalization means that the model obtained on the training set has the same good effect under different external data tests. Especially for rigorous disciplines such as clinical medicine, strict external verification is needed to ensure the correctness of decision-making results [80].
DATA SOURCES AND ETHICAL ISSUES:
Research on AI + smart hospitals relies on big data, but domestic medical big data is challenging to share owing to the problem of ownership confirmation, and it is challenging to apply owing to the large amount of poor-quality data. The depth and breadth of electronic medical records are insufficient in practical application, and there is a large construction gap in medical treatment and medical management. Furthermore, it is challenging to ethically obtain medical data. Information fragmentation is still a problem; however, experts should annotate high-quality data accurately. The quantity and quality of annotation directly affect the whole data set. In addition, each unit has its database, and the data and form of each disease are different. There is no unified standard to integrate it, and there is a lack of an extensive public database system [81]. In the process of AI and medical big data construction, many ethical issues arise, including informed consent of subjects, personal information privacy security, the fairness of data open sharing. Only with full protection of the security of personal information it is possible to promote the standard governance of big data, the effective use of data to improve medical science, promote public health safety, and develop industrial applications.
Moreover, with the advent of AI medical care, many companies actively provide their developed products to hospitals for a free trial to collect a large amount of clinical trial data. The ethics committee of the AI medical device review notes should pay attention to fair benefits, unemployment, patient privacy, medical safety, division of responsibilities, and supervision. However, the incomplete establishment of the database itself, hidden algorithmic bias, and lack of legislation and regulation make the ethical review difficult [82]. There is a famous saying that “to cure, sometimes; to relieve, often; to comfort, always.” A hundred years from now, looking back, people cannot say, “We have gone so fast, we have gone so far, so we forget why we started.” The future will be an era of human–computer interaction. Artificial intelligence will push medicine to unprecedented heights. Physicians will be transformed into knowledge managers with more time to communicate, care for patients, and advise decision-making. The process looks simple, but it is not. Numerous medical ethics and legal issues continue to emerge. Nevertheless, in the final analysis, “patient interests” should be the essential starting point to successfully start the ground-breaking journey and effectively promote the development of medical big data.
LACK OF CAPITAL AND TALENT:
The development of AI in medicine cannot be separated from the training of talents. In particular, it involves 2 major disciplines – AI and medicine – which are specific interdisciplinary disciplines and require skills to be proficient in these 2 aspects. However, AI engineers have less understanding of medical problems and are unfamiliar with the clinical complexity, which will inevitably affect the research and development of AI systems. Doctors with medical backgrounds lack an understanding of engineering algorithms, and the system’s development process is challenging, which will also affect the standardization of AI products [83–85]. However, many medical staff believe that AI may threaten their survival and lead to job loss. Thus, their resistance hinders the active application of AI. In addition, intelligent medical treatment faces many challenges, including the fact that some personnel are not good at operating intelligent equipment [86].
“BLACK BOX” PHENOMENON:
The ML algorithm’s analysis ability is very high, better than classical statistics and modeling methods. However, its main disadvantage is the black box problem: ML algorithm data analysis is based on mathematical functions, algorithms, or models. Understanding the ML algorithm to obtain the mechanical answer to the problem is challenging [87]. For example, in a neural network, a single neuron receives input signals from multiple neurons. After the weighted sum is summed, these signals are passed to subsequently connected neurons, and subsequent neurons again receive signal input from the previous layer of neurons. Repeating these steps, layers of operations between the input and output ports will be created. It makes it challenging for anesthesiologists to understand the internal mechanisms of ML. Despite the success of ML algorithms in various trials, it is difficult for clinicians to determine whether errors occur within the “black box,” thus, it may be challenging for ML algorithms to obtain independence. Although ML can predict the results from variables, it cannot give the reason for the results; people cannot understand the mechanism of the results, that is, ML cannot answer how the results are generated. Finally, the prerequisite for ML algorithms is to collect large amounts of high-fidelity physiological monitoring data from patients. If data are incomplete, unstable, biased, or incorrect in the training process, it may produce false results and lead doctors to make the bad decisions [88]. Therefore, the opacity and irrationality of the ML model operation mode will significantly limit its application.
Future Directions
In conclusion, AI algorithms have not surpassed human performance; however, AI’s ability to quickly and accurately sift through large amounts of data and discover correlations and patterns imperceptible to human cognition will make it an invaluable tool for clinicians. ML algorithms play a vital role in developing AI, and they play a critical role in image analysis, evaluation and prediction, decision-making assistance, and AI. The automation advantages will bring huge opportunities for the development of anesthesiology. In addition, most of the current applications of AI are limited to data analysis, saving doctors time otherwise spent on repetitive and low-tech operations. More research is still needed to explore AI’s application in anesthesia in the future. Anesthesiologists who keep pace with the times should enjoy the convenience brought by AI and explore more development possibilities of AI in the field of anesthesia and become pioneers of anesthesia. They also should continue to partner with data scientists and engineers to provide valuable clinical insight into the development of AI to ensure that the technology will be clinically applicable, that the data used to train algorithms are valid and representative of a broad population of patients, and that the interpretations of the data are clinically meaningful [89]. At the same time, in the process of AI design, manufacture, and application, the developers should always adhere to the concept of being people-oriented, respect the autonomy of subjects, and fully protect personal privacy under the premise of ensuring security, actively promote the accessibility of technology, and establish and improve relevant laws and ethical norms to ensure the ethical application of AI in the medical industry.
Figures
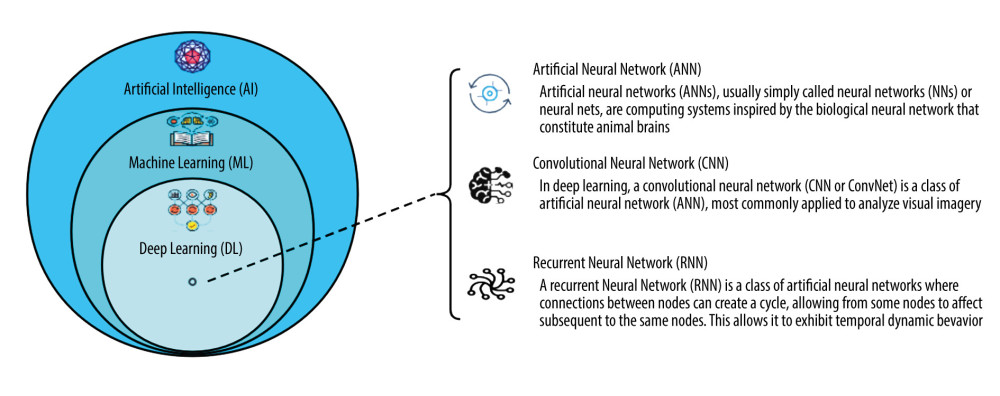 Figure 1. The relationship of AI, ML, and DL. (Software: ProcessOn, https://www.processon.com/view/link/638acc2d1e08536bffa302e4).
Figure 1. The relationship of AI, ML, and DL. (Software: ProcessOn, https://www.processon.com/view/link/638acc2d1e08536bffa302e4). 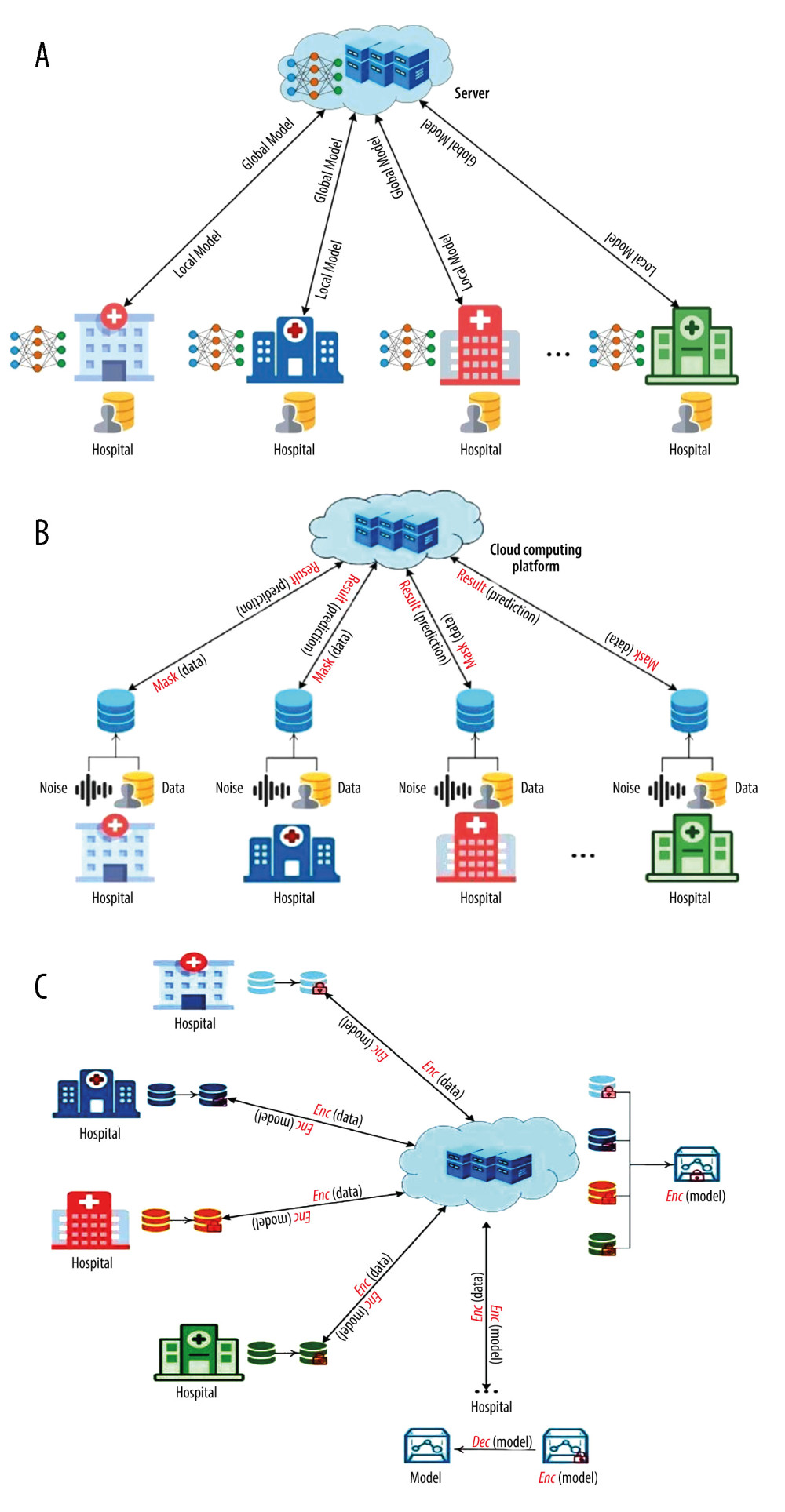 Figure 2. (A) Federated learning technology in the patient’s privacy protection. (B) Differential privacy technology in the patient’s privacy protection. (C) Homomorphic encryption technology in the patient’s privacy protection. (Software: Microsoft Office Visio 2019).
Figure 2. (A) Federated learning technology in the patient’s privacy protection. (B) Differential privacy technology in the patient’s privacy protection. (C) Homomorphic encryption technology in the patient’s privacy protection. (Software: Microsoft Office Visio 2019). References
1. Hashimoto DA, Witkowski E, Gao L, Artificial intelligence in anesthesiology: Current techniques, clinical applications, and imitations: Anesthesiology, 2020; 132(2); 379-94
2. Turing AM, Computing machinery and intelligence: Mind, 1950; 59(236); 433-60
3. Valueva MV, Nagornov NN, Lyakhov PA, Application of the residue number system to reduce hardware costs of the convolutional neural network implementation: Mathematics and Computers in Simulation, 2020; 177; 232-43
4. Yang ZR, Yang Z: Comprehensive biomedical physics, 2014; 1, Karolinska Institute Stockholm, Sweden, Elsevier
5. Dupond S, A thorough review on the current advance of neural network structures: Annual Reviews in Control, 2019; 14; 200-30
6. Thrall JH, Li X, Li Q, Artificial intelligence and machine learning in radiology: Opportunities, challenges, pitfalls, and criteria for success: J Am Coll Radiol, 2018; 15(3 Pt B); 504-8
7. Salto-Tellez M, Maxwell P, Hamilton P, Artificial intelligence-the third revolution in pathology: Histopathology, 2019; 74; 372-76
8. Deo RC, Machine learning in medicine: Circulation, 2015; 132; 1920-30
9. Hashimoto DA, Rosman G, Rus D, Meireles OR, Artificial intelligence in surgery: Promises and perils: Ann Surg, 2018; 268; 70-76
10. The State Council: The 2018 Government Work Report [EB/OL] 03 05, 2018 [2021-05-09]. http://www.gov.cn/zhuanti/2018lh/2018zfgzbg/zfgzbg.htm
11. Kudsk-Iversen S, Shamambo N, Bould MD, Strengthening the anesthesia workforce in low- and middle-income countries: Anesth Analg, 2018; 126(4); 1291-97
12. Gambus PL, Jaramillo S, Machine learning in anesthesia: Reactive, proactive predictive: Br J Anaesth, 2019; 123(4); 401-3
13. Diao JA, Kohane IS, Manrai AK, Biomedical informatics and machine learning for clinical genomics: Hum Mol Genet, 2018; 27; R29-34
14. Suleiman D, Al-Zewairi M, Naymat G, An empirical evaluation of intelligent machine learning algorithms under big data processing systems: Procedia Computer Science, 2017; 113; 539-44
15. Chen PC, Liu Y, Peng L, How to develop machine learning models for healthcare: Nat Mater, 2019; 18; 410-14
16. Alexander JC, Joshi GP, Anesthesiology, automation, and artificial intelligence: Proc (Bayl Univ Med Cent), 2018; 31; 117-19
17. Nørskov AK, Wetterslev J, Rosenstock CV, Effects of using the simplified airway risk index vs usual airway assessment on unanticipated difficult tracheal intubation – a cluster randomized trial with 64,273 participants: Br J Anaesth, 2016; 116; 680-89
18. L’Hermite J, Nouvellon E, Cuvillon P, The Simplified Predictive Intubation Difficulty Score: A new weighted score for difficult airway assessment: Eur J Anaesthesiol, 2009; 26; 1003-9
19. Moustafa MA, El-Metainy S, Mahar K, Defining difficult laryngoscopy findings by using multiple parameters: A machine learning approach: Egypt J Anaesth, 2017; 33; 153-58
20. Aguilar K, Alférez GH, Aguilar C, Detection of difficult airway using deep learning: Mach Vis Appl, 2020; 31; 1-11
21. Cuendet GL, Schoettker P, Yüce A, Facial image analysis for fully automatic prediction of difficult endotracheal intubation: IEEE Trans Biomed Eng, 2016; 63; 328-39
22. Mihalj M, Carrel T, Gregoric ID, Telemedicine for preoperative assessment during a COVID-19 pandemic: Recommendations for clinical care: Best Pract Res Clin Anaesthesiol, 2020; 34; 345-51
23. Galvez JA, Rehman MA, Telemedicine in anesthesia: An update: Curr Opin Anaesthesiol, 2011; 24; 459-62
24. Kendale S, Kulkarni P, Rosenberg AD, Wang J, Supervised machine-learning predictive analytics for prediction of postinduction hypotension: Anesthesiology, 2018; 129(4); 675-88
25. Hatib F, Jian Z, Buddi S, Machine-learning algorithm to predict hypotension based on high-fidelity arterial pressure waveform analysis: Anesthesiology, 2018; 129(4); 663-74
26. Mann CJ, Observational research methods. Research design II: Cohort, cross sectional, and case-control studies: Emerg Med J, 2003; 20(1); 54-60
27. Kruppa J, Liu Y, Diener HC, Probability estimation with machine learning methods for dichotomous and multicategory outcome: Applications: Biom J, 2014; 56(4); 564-83
28. Thottakkara P, Ozrazgat-Baslanti T, Hupf BB, Application of machine learning techniques to high-dimensional clinical data to forecast postoperative complications: PLoS One, 2016; 11(5); e0155705
29. Corey KM, Kashyap S, Lorenzi E, Development and validation of machine learning models to identify high-risk surgical patients using automatically curated electronic health record data (Pythia): A retrospective, single-site study: PLoS Med, 2018; 15(11); e1002701
30. Mirsadeghi M, Behnam H, Shalbaf R, Characterizing awake and anesthetized states using a dimensionality reduction method: J Med Syst, 2016; 40(1); 13
31. Shalbaf A, Saffar M, Sleigh JW, Monitoring the depth of anesthesia using a new adaptive neurofuzzy system: IEEE J Biomed Health Inform, 2018; 22(3); 671-77
32. Park Y, Han SH, Byun W, A real time depth of anesthesia monitoring system based on deep neural network with large EDO tolerant EEG analog front end: IEEE Trans Biomed Circuits Syst, 2020; 14(4); 825-37
33. Gu Y, Liang Z, Hagihira S, Use of multiple EEG features and artificial neural network to monitor the depth of anesthesia[J/OL]: Sensors (Basel), 2019; 19(11); 2499
34. Ramaswamy SM, Weerink MAS, Struys MMRF, Dexmedetomidine induced deep sedation mimics non rapid eye movement stage 3 sleep: Large scale validation using machine learning[J/OL]: Sleep, 2021; 44(2); zsaa167
35. Ramaswamy SM, Kuizenga MH, Weerink MAS, Frontal electroencephalogram based drug, sex, and age independent sedation level prediction using non linear machine learning algorithms: J Clin Monit Comput, 2020; 36(1); 121-30
36. Absalom AR, Sutcliffe N, Kenny GN, Closed-loop control of anesthesia using Bispectral index: Performance assessment in patients undergoing major orthopedic surgery under combined general and regional anesthesia: Anesthesiology, 2002; 96(1); 67-73
37. Schamberg G, Controlling level of unconsciousness by titrating propofol with deep reinforcement learning: Artificial Intelligence in Medicine, 2020; 26-36, Minneapolis, Springer
38. Guen MLE, Liu N, Chazot T, Closed-loop anesthesia: Minerva Anestesiol, 2016; 82(5); 573-81
39. Struys MM, De Smet T, Glen JI, The history of target-controlled infusion: Anesth Analg, 2016; 122(1); 56-69
40. Hemmerling TM, Robots will perform anesthesia in the near future: Anesthesiology, 2020; 132(2); 219-20
41. Tighe PJ, Badiyan SJ, Luria I, Robot-assisted airway support: A simulated case: Anesth Analg, 2010; 111(4); 929-31
42. Hemmerling TM, Taddei R, Wehbe M, First robotic tracheal intubations in humans using the Kepler intubation system: Br J Anaesth, 2012; 108(6); 1011-16
43. Lederman D, Endotracheal intubation confirmation based on video image classification using a parallel GMMs framework: A preliminary evaluation: Ann Biomed Eng, 2011; 39(1); 508-16
44. Biro P, Hofmann P, Gage D, Automated tracheal intubation in an airway manikin using a robotic endoscope: A proof of concept study: Anesthesia, 2020; 75(7); 881-86
45. Hetherington J, Lessoway V, Gunka V, SLIDE: Automatic spine level identification system using a deep convolutional neural network: Int J Comput Assist Radiol Surg, 2017; 12; 1189-98
46. Chen X, Owen CA, Huang EC, Artificial intelligence in echocardiography for anesthesiologists: J Cardiothorac Vasc Anesth, 2021; 35(1); 251-61
47. Turbitt LR, Mariano ER, El-Boghdadly K, Future directions in regional anesthesia: Not just for the cognoscenti: Anesthesia, 2020; 75; 293-97
48. Gil González J, Álvarez MA, Orozco ÁA, Automatic segmentation of nerve structures in ultrasound images using Graph Cuts and Gaussian processes: Annu Int Conf IEEE Eng Med Biol Soc, 2015; 2015; 3089-92
49. Pesteie M, Lessoway V, Abolmaesumi P, Rohling RN, Automatic localization of the needle target for ultrasound-guided epidural injections: IEEE Trans Med Imaging, 2018; 37; 81-92
50. Mišić VV, Gabel E, Hofer I, Machine learning prediction of postoperative emergency department hospital readmission: Anesthesiology, 2020; 132(5); 968-80
51. Kehlet H, Jensen TS, Woolf CJ, Persistent postsurgical pain: Risk factors and prevention: Lancet, 2006; 367(9522); 1618-25
52. Dolin SJ, Cashman JN, Bland JM, Effectiveness of acute postoperative pain management: I. Evidence from published data: Br J Anaesth, 2002; 89(3); 409-23
53. Hannan AQ, Roshni R, Lauren MM, Burnout phenomenon in U. S. plastic surgeons: Risk factors and impact on quality of life: Plast Reconstr Surg, 2015; 135(2); 619-26
54. Poleshuck EL, Katz J, Andrus CH, Risk factors for chronic pain following breast cancer surgery: A prospective study: J Pain, 2010; 7(5); 626-34
55. She S, Xu X, Xiao J, Effect of continuous epidural infusion on morphine PCA consumption: Chinese Journal of Anesthesia, 2000; 20(9); 570-71
56. She S, Huang Y, Review of patient controlled analgesia and clinical strategy in China: Journal of Practical Pain, 2018; 4(14); 247-49
57. Wang Q, Cao H, Xiong L, PCA intelligence and improves the quality of postoperative analgesia: Chinese Journal of Anesthesia, 2018; 38(3); 257-58
58. Wang R, Wang S, Dian N, From patient-controlled analgesia to artificial intelligence-assisted patient-controlled analgesia: Practices and perspectives: Fron Med, 2020; 7(4); 145-49
59. Wang S, Duan N, Li X, Effect of intelligent patient-controlled analgesia on adverse reactions and satisfaction of postoperative analgesia patients: Guangdong Medicine, 2020; 41(11); 1097-110
60. Kissin I, A call to reassess the clinical value of preventive (preemptive) analgesia: Anesth Analg, 2011; 113(5); 977-78
61. Katz J, Clarke H, Review article: Preventive analgesia: Quo vadimus?: Anesth Analg, 2011; 113(5); 1242-53
62. Echelard JF, Méthot F, Nguyen HA, Pomey MP, Medical student training in eHealth: Scoping review: JMIR Med Educ, 2020; 6; e20027
63. Zhou T, Huang S, Cheng J, Xiao Y, The distance teaching practice of combined mode of massive open online course micro-video for interns in Emergency Department during the COVID-19 epidemic period: Telemed J E Health, 2020; 26; 584-88
64. Sahi PK, Mishra D, Singh T, Medical education amid the COVID-19 pandemic: Indian Pediatr, 2020; 57; 652-57
65. Singh PM, Kaur M, Trikha A, Virtual reality in anesthesia “simulation”: Anesth Essays Res, 2012; 6; 134-39
66. Alexander JC, Joshi GP, Anesthesiology, automation, and artificial intelligence: Proc (Bayl Univ Med Cent), 2018; 31(1); 117-19
67. Voigt P, Von dem Bussche A: The EU general data protection regulation (gdpr) A Practical Guide, 2017; 10(3152676); 10.5555, Cham, Springer International Publishing
68. Li Y, Wang Y, Wan J, Privacy protection for medical image management based on blockchain: International Conference on Database Systems for Advanced Applications, 2021; 414-28, Cham, Springer
69. Wu F, Cui L, Feng J, Data privacy protection based on feature dilution in cloud services; 1-6, IEEE
70. Lv Z, Piccialli F, The security of medical data on internet based on differential privacy technology: ACM Transactions on Internet Technology, 2021; 21(3); 1-18
71. Xiong A, Wang T, Li N, Towards effective differential privacy communication for users’ data sharing decision and comprehension; 392-410, IEEE
72. Boulemtafes A, Derhab A, Braham NAA, PReDIHERO-privacy-preserving remote deep learning inference based on homomorphic encryption and reversible obfuscation for enhanced client-side overhead in pervasive health monitoring; 1-8, IEEE
73. Kumari KA, Sharma A, Chakraborty C, Preserving health care data security and privacy using carmichael’s theorem-based homomorphic encryption and modified enhanced homomorphic encryption schemes in edge computing systems: Big Data, 2021
74. Liu ZY, Shi ZW, Liang CHPromoting the application of federated learning in medical imaging artificial intelligence: Zhonghua Yi Xue Xa Xhi, 2022; 102(5); 318-20 [in Chinese]
75. Sharma S, Kesarwani A, Maheshwari S, Federated learning for data mining in healthcare: Federated Learning for IoT Applications; 243
76. Bowness JS, Burckett-St Laurent D, Hernandez N, Assistive artificial intelligence for ultrasound image interpretation in regional anesthesia: An external validation study: Br J Anaesth, 2022 [Online ahead of print]
77. Zhang G, Fu DJ, Liefers B, Clinically relevant deep learning for detection and quantification of geographic atrophy from optical coherence tomography: A model development and external validation study: Lancet Digit Health, 2021; 3(10); e665-75
78. Lopez-Jimenez F, Attia Z, Arruda-Olson AM, Artificial intelligence in cardiology: present and future: Mayo Clin Proc, 2020; 5; 1015-39
79. Whang SE, Lee JG, Data collection and quality challenges for deep learning: Proceedings of the VLDB Endowment, 2020; 13(12); 3429-32
80. Echle A, Rindtorff NT, Brinker TJ, Deep learning in cancer pathology: A new generation of clinical biomarkers: Br J Cancer, 2021; 124(4); 686-96
81. Wang DF, Liu D, Artificial intelligence promotes medical big data to help ensure people’s health: Chinese Critical Care Medicine, 2020; 32(10); 1155-59
82. Zhou J, Li H, Yang Y, Elements for ethical review of artificial intelligence medical device: Medicine and Philosophy, 2020; 41(6); 35-39
83. Chen XR, Li GZ, Cui YD, Analysis of the development trend of the application of global artificial intelligence technology in the medical and health field based on patent measurement: Science and Technology Management Research, 2021; 41(3); 139-47
84. Zhang J, The application of human comprehensive development theory and deep learning in innovation education in higher education: Front Psychol, 2020; 11; 1605
85. Cyranoski D, China enters the battle for AI talent: Nature, 2018; 553(7688); 260-62
86. Wang H, Meng X, Liu Y, Study of the testing strategy of artificial intelligence methods in medical devices: Medical Equipment in China, 2016; 31(10); 67-70
87. Connor CW, Artificial intelligence and machine learning in anesthesiology: Anesthesiology, 2019; 131(6); 1346-59
88. Sassenscheidt J, Jungwirth B, Kubitz JC, Machine learning in anesthesiology: Anesthesist, 2020; 69(8); 535-43
89. Weber GM, Mandl KD, Kohane IS, Finding the missing link for big biomedical data: JAMA, 2014; 311; 2479-800
Figures
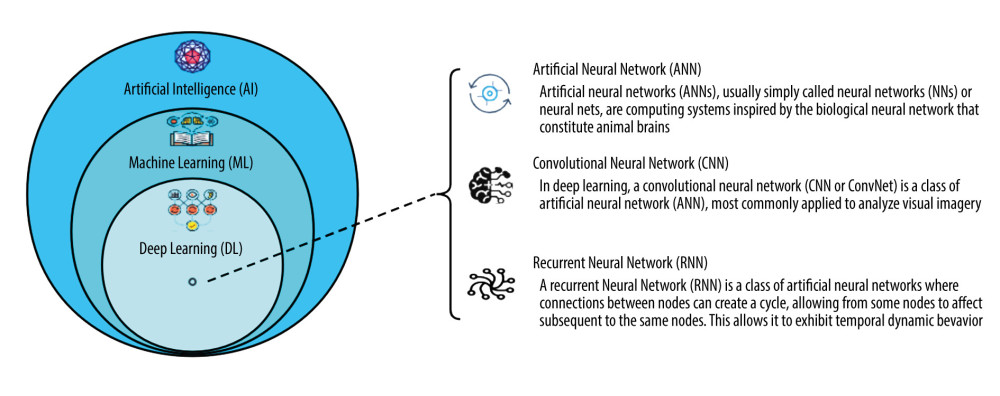 Figure 1. The relationship of AI, ML, and DL. (Software: ProcessOn, https://www.processon.com/view/link/638acc2d1e08536bffa302e4).
Figure 1. The relationship of AI, ML, and DL. (Software: ProcessOn, https://www.processon.com/view/link/638acc2d1e08536bffa302e4).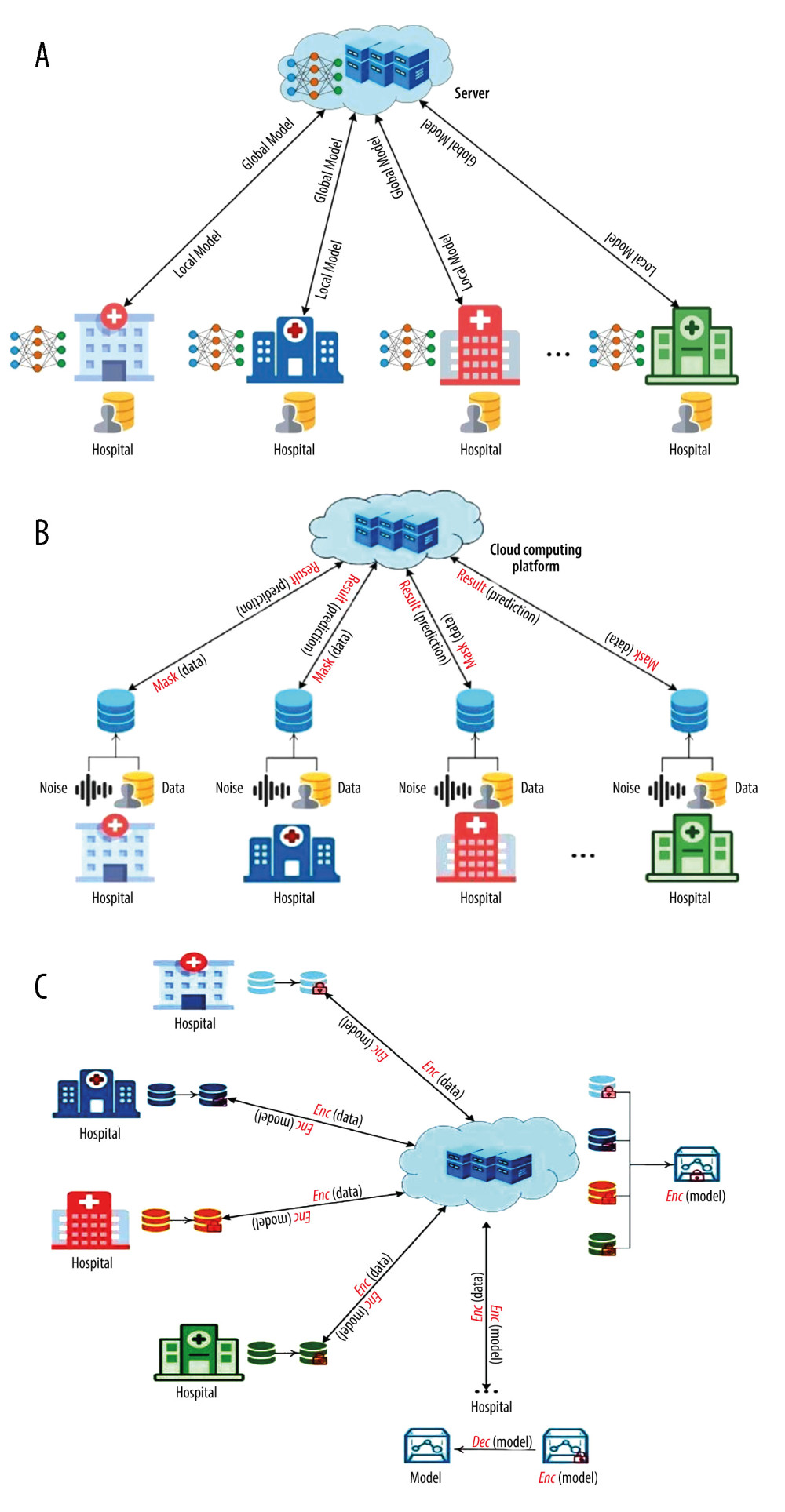 Figure 2. (A) Federated learning technology in the patient’s privacy protection. (B) Differential privacy technology in the patient’s privacy protection. (C) Homomorphic encryption technology in the patient’s privacy protection. (Software: Microsoft Office Visio 2019).
Figure 2. (A) Federated learning technology in the patient’s privacy protection. (B) Differential privacy technology in the patient’s privacy protection. (C) Homomorphic encryption technology in the patient’s privacy protection. (Software: Microsoft Office Visio 2019). In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952