29 April 2024: Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety and Efficacy Evaluation
Mehmet Zafer Sabuncuoglu1ABCDEF, Isa Sozen1AE, İsmail Zihni1ABF*, Girayhan Celik1EF, Bilal Turan2CD, Serdar Acar3D, İsa Karaca3BD, Demet Gunduz4ADEDOI: 10.12659/MSM.944127
Med Sci Monit 2024; 30:e944127
Abstract
BACKGROUND: Chronic anal fissure is a common condition that causes pain and discomfort and has a significant impact on quality of life. When conservative management fails, surgical sphincterotomy can be successful. This retrospective study from a single center in Turkey included 188 patients with chronic anal fissures and aimed to compare outcomes from open and closed sphincterotomy.
MATERIAL AND METHODS: This retrospective study included 188 patients treated with lateral internal sphincterotomy (LIS) for chronic anal fissure between January 2015 and December 2021 in our hospital. Open LIS procedure was performed in 91 patients and closed LIS was performed in 97 patients. Demographic characteristics, postoperative complications, and recurrence were compared for these 2 methods.
RESULTS: Of the 188 patients included in the study, 47.9% were women and 52.1% were men. The mean age was 42.9 (20-84) years. In the open LIS group, recurrence occurred in 2 patients (2.19%), and no incontinence was observed. In the closed LIS group, recurrence occurred in 3 patients (3%; P=0.703), and incontinence developed in 5 patients (5.15%; P=0.035).
CONCLUSIONS: Comparing the 2 methods used in chronic anal fissure surgery, and considering the recurrence and risk of incontinence, the most feared outcome by the patient and surgeon, open LIS stands out as a superior technique, especially in young male patients.
Keywords: Fissure in Ano, Lateral Internal Sphincterotomy, sphincterotomy
Introduction
Anal fissure is a superficial tear in the anal canal distal to the dentate line. Anal fissure is a common anorectal disease involving approximately 10% of all proctologic patients [1]. Anal fissures can be acute, lasting less than 6 weeks, or chronic, lasting longer than 6 weeks, and are characterized by bleeding and painful longitudinal tears from the dentate line to the squamous epithelium of the anal canal. They manifest as severe perianal pain, typically exacerbated by defecation.
The pathogenesis and etiology of anal fissures remain unclear. Hypertonia, fibrosis, local trauma, and ischemia have been suggested as causes of anal fissures. Anal fissure is a common disease affecting all age groups, with equal frequency in both sexes. The diagnosis of an anal fissure is primarily clinical. Several treatment options exist, including medical management and surgical options [1].
International guidelines state that the treatment of chronic anal fissure should first require a trial of medical treatment. However, the efficacy of these agents is limited by adverse effects, variability in administration technique, and dependence on patient compliance. In addition, the effects of medical treatment are generally temporary, and the recurrence rate is reported to be greater than 50% [2].
Lateral internal sphincterotomy (LIS) is considered the criterion standard treatment for chronic anal fissure and relieves symptoms with a high cure rate and less than 10% recurrence. However, this optimal treatment is associated with a risk of postoperative anal incontinence, which can reach a rate of 30% (or more) and become permanent [3–5]. Recent studies have suggested that the surgical technique, whether surgery is open or closed, can affect incontinence rates after sphincterotomy. This study was designed to compare efficacy, recurrence rates, and complications, especially incontinence, after open and closed LIS.
Material and Methods
ETHICS:
Ethical approval was granted by the local Medical Research Ethics Committee of Gaziantep Islamic Science and Technology University Clinical Research (Ref: 2023). Our center obtained their respective approvals according to local and institutional requirements. All participants gave their written informed consent. The data were subsequently collated and analyzed centrally in Suleyman Demirel University.
STUDY DESIGN:
In this retrospective study, 245 patients who were operated on for anal fissures in the Suleyman Demirel University General Surgery Clinic between January 2015 and December 2021 were included. A total of 57 patients, who had either missing medical records or were lost to follow-up, were excluded from the study. In total, 188 patients were followed up regularly and could be reached and were therefore included in the study. Two surgical techniques were used in the study: open LIS and closed LIS. The open LIS procedure was performed in 91 patients and the closed LIS procedure was performed in 97 patients (Figure 1).
DATA COLLECTION AND STUDY POPULATION:
Data of patients’ demographic findings and preoperative and postoperative variables were collected. The study assessed preoperative characteristics, including demographics, operation type, and sex differences. Postoperative outcomes were evaluated at least 6 months following surgery and included recurrence rates, fecal and float incontinence, pain levels, and any surgical complications. Short-term incontinence was defined as the involuntary loss of gas, fluid, or fecal material at the 6-week follow-up, and long-term incontinence was involuntary loss of gas, fluid, or fecal material at the 12-month follow-up. Incontinence data were assessed through the validated Wexner scoring system, in which solid, liquid, and gas incontinence are rated separately on a 5-point grading system.
INCLUSION AND EXCLUSION CRITERIA:
The study included patients who were 18 years of age or older, had undergone LIS, and had no prior perineal surgery or recurrent chronic anal fissure.
DEFINITIONS AND OUTCOMES:
The primary outcomes were surgery-related parameters, recurrence, pain, and perioperative complications. Postoperative complications were categorized according to open and closed surgery groups and were recorded within the same hospitalization.
Unhealed fissures were considered as treatment failure. Incontinence data were assessed through the validated Wexner scoring system.
SURGICAL PROCEDURES:
All procedures were performed under regional anesthesia by 2 experienced colorectal surgeons with more than 10 years of coloproctology experience. Each surgeon performed the single surgical technique they preferred. There was no randomization.
CLOSED LIS:
After spinal anesthesia, the patient was placed in the lithotomy position. The surgeon palpated the internal sphincter muscle by inserting the left index finger into the anal canal. The intersphincteric groove was identified, and a 1-cm incision was made. While the internal sphincter was controlled with the left index finger, one-half to one-third of the internal sphincter was divided with a scalpel. After bleeding was controlled, the incision was closed with a sterile dressing, without suturing.
OPENED LIS: With the patient under regional anesthesia and in the lithotomy position, the anal canal was retracted with a Parks retractor to expose the internal sphincter muscle. Similar to the closed method, the surgeon identified the intersphincteric groove and made a 1-cm incision. Artery forceps were used to carefully separate the muscle fibers from the underlying mucosa, and one-half to one-third of the internal sphincter muscle was divided with a scalpel. After bleeding was controlled, the incision was closed with a sterile dressing, without suturing (Figure 2).
FOLLOW-UP:
Patients who were followed up for at least 6 months were included in the study.
STATISTICAL EVALUATION:
Data were transferred to SPSS.23 (IBM Corp, Armonk, NY, USA) and analyzed. Before we proceeded to the statistical analysis, controls were made regarding the absence of data entry errors and whether the parameters were within the expected range. Normality assumptions of continuous variables were assessed with the Kolmogorov-Smirnov and Shapiro-Wilk tests, and homogeneity of variance was examined with the Levene test. Mean and standard deviation values were given for continuous variables, and frequency (n) and percentage (%) values were given for categorical variables. The Mann-Whitney U test was used for 2-level comparisons, where the data were not normally distributed, and the Kruskal-Wallis H test was used for comparisons with 3 or more levels. Relationships between categorical variables were examined with the chi-square test. A value of
Results
DEMOGRAPHIC FINDINGS OF STUDY POPULATION:
Of the patients included in the study, 98 (52.1%) were men, and 90 (47.9%) were women. The age range of patients was 20 to 84 years, and the mean age was 42.87±13.13 years. Open LIS was performed in 91 (48.4%) patients, and closed LIS was performed in 97 (51.6%) patients.
The mean age of the patients who underwent open surgery was 40.98±19.73 years. The mean age of the patients who underwent closed surgery was 44.64±13.63 years. There was no statistically significant relationship between the age of the patients and surgical method (
RESULTS OF PROCEDURES AND FOLLOW-UP:
The mean follow-up period of the patients was 27.63±15.50 months. The number of patients operated on by year was as follows: 29 patients in 2015; 25 patients in 2016; 42 patients in 2017; 34 patients in 2018; 22 patients in 2019; 8 patients in 2020; 19 patients in 2021; and 9 patients in 2022. Complications were seen in 39 patients: abscess was observed in 1, pain in 12, leakage in 4, fecal incontinence in 5, constipation in 1, bleeding in 7, itching in 2, recurrence in 5, and tenesmus in 2 patients (Figure 3).
The mean follow-up period of patients who underwent open surgery was 19.73±13.36 days, and for those who underwent closed surgery, 35.05±13.63 days. The mean follow-up period of patients who underwent the closed surgical method was statistically significantly longer than those who underwent the open method (P<0.001) (Table 1).
COMPLICATIONS:
Complications developed in 16 of the patients who underwent open surgery and in 23 of the patients who underwent closed surgery. Of the patients who underwent open surgery, 8 (50%) had pain, 2 (12.5%) had leakage, 3 (1.8%) had bleeding, 1 (6.3%) had itching, and recurrence was observed in 2 (12.5%). No cases of tenesmus, constipation, fecal incontinence, and gas incontinence occurred in the open LIS group. Complications seen in patients who underwent closed LIS were gas incontinence in 1 (4.3%), pain in 5 (21.7%), discharge in 2 (8.7%), fecal incontinence in 4 (17.4%), constipation in 1 (4.3%), bleeding in 4 (17.4%), itching in 1 (4.3%), tenesmus in 2 (8.7%), and recurrence in 3 (13%). There was no statistically significant relationship between the development of complications and the type of surgery (P>0.05) (Figure 4).
While no constipation was observed in male patients, the most common complications in male patients were discharge, pain, and bleeding. While discharge, gas incontinence, and itching were not observed in female patients, the most common complications in female patients were pain, bleeding, and recurrence. There was no statistically significant relationship between sex and complication types (P>0.05) (Table 2).
The mean age of patients with tenesmus was higher than that of patients with other complications. Patients with pain complications had the youngest mean age. No statistically significant correlation was observed between the types of complications and mean age (
Short-term incontinence was defined as the involuntary loss of gas, fluid, or fecal material at the 6-week follow-up, and long-term incontinence was involuntary loss of gas, fluid, or fecal material at the 12-month follow-up. Incontinence data were assessed through the validated Wexner scoring system, in which solid, liquid, and gas incontinence are rated separately on a 5-point grading system (Table 3).
Discussion
The aim of our study was to determine the effectiveness of open LIS and closed LIS in chronic anal fissure, complications of the surgeries, and factors affecting the complications. Of the patients who underwent open surgery, 8 (50%) had pain, 2 (12.5%) had leakage, 3 (1.8%) had bleeding, 1 (6.3%) had itching, and 2 (12.5%) had recurrence. The complications seen in patients who underwent closed surgery were gas incontinence in 1 (4.3%), pain in 5 (21.7%), discharge in 2 (8.7%), fecal incontinence in 4 (17.4%), constipation in 1 (4.3%), bleeding in 4 (17.4%), itching in 1 (4.3%), tenesmus in 2 (8.7%), and recurrence in 3 (13%). Our primary outcome measures were recurrence and postoperative incontinence. Recurrence was defined as the presence of anal pain or anal fissure identified on physical examination at follow-up, with or without a temporary improvement in symptoms following the initial procedure. In the literature, LIS has already been established as the standard treatment method, being both permanent and the most effective treatment.
Notaras described subcutaneous LIS in 1971. The main purpose of sphincterotomy is to increase blood flow to the anoderm by reducing the maximum anal sphincter pressure by 18% to 50%. This technique provides successful treatment in between 82% and 100% of cases [6,7]. Despite the high success rate in fissure treatment after sphincterotomy, the recurrence rate can be between 1.6% and 6% [7–10]. The most common cause of recurrence is inadequate sphincterotomy. The length of the internal sphincter incision of LIS varies depending on the surgeon’s discretion and skill, as the procedure has not been standardized; this is the main cause of recurrence and incontinence [11]. In our study, this rate was found to be 2.65%, with 5 cases, which is compatible with the literature. The mean age of the patients with relapse was 37.6 years. This can be explained by insufficient sphincterotomy due to strong pelvic muscles. In addition, there was no statistically significant difference between open LIS and closed LIS regarding recurrence (2.19%–3.0%). Regardless of an experienced surgeon’s method, recurrence does not fall below a certain rate.
This study consisted of 188 patients; 91 (48.4%) patients underwent open LIS surgery, and 97 (51.6%) patients underwent closed LIS surgery. The mean age of the patients was 42.87 (20–84) years. In some series, the average age ranges between 30 and 44.8 years [2,12,13]. In the present study, a patient population compatible with that described in the literature was operated on.
A wide variation in sex of studied populations exists in different studies. Although there are studies stating a male: female ratio of 3: 1, 6: 1, and 7: 1, publications with equal ratios are more common. Of the patients included in our study, 98 (52.1%) were men, and 90 (47.9%) were women [2,14,15].
Studies evaluating preoperative and postoperative pain relief at 1, 4, and 6 weeks with the visual analog scale in patients who underwent LIS found the rate of pain varied between 91.4% and 100% [7]. Although this rate was 93.1% in our study, it was observed that, in most cases, pain was relieved after 6 weeks. Although the pain rate (8.7%) in our patients who underwent open LIS was higher than the pain rate (5.1%) in patients who underwent closed LIS, it was observed to be 50% lower in the closed method, although there was no statistically significant difference.
In the present study, the mean age of patients with pain was 34.3 years. This was thought to be related to the muscle strength of young patients. In addition, the incidence of pain was higher in female patients than in male patients in our study (30.7–69.3%). This difference can be explained by the lower pain threshold in female patients. Therefore, greater caution should be exercised in analgesic treatment during the first month in female patients. While a previous meta-analysis [4] did not find a statistical difference in pain by patient sex and age, it is important to consider that young female patients can require more analgesics. Further research may be necessary to explore potential sex and age-related variations in pain perception and analgesic needs after LIS surgery [4].
Garcia-Granero et al demonstrated that 90% of patients with symptomatic fissure recurrence had an incomplete internal sphincterotomy on endorectal ultrasound examination. We believe this is a consequence of the non-standardized, or unstandardized, sphincterotomy procedure. The idea of decreasing or increasing the size of the internal sphincterotomy is complex, and the different results in the literature reflect this complexity [16,17]. The recent meta-analysis also found a higher recurrence rate with the closed LIS technique [4]. However, in our study, no statistically significant difference was found between the 2 techniques.
The incidence of postoperative incontinence, mostly gas incontinence, varies in the literature, and its duration is reported as temporary. However, it remains controversial whether minor incontinence is a symptom of chronic anal fissure or the result of the LIS procedure [18,19]. In our study, gas (1 patient) and fecal incontinence (4 patients) was observed in 5 (2.65%) patients (4 patients’ Wexner scores [10]: 1 patient, 2; 3 patients, 3), which resolved after 8 months without any intervention. One case (0.8%), in a patient with a Wexner score of 12, was considered permanent. Later, it was observed that the clinical picture of the patient who underwent a perineoplasty operation was partially improved. The meta-analysis reported that open LIS surgery led to more incontinence than did closed LIS surgery. However, there are some crucial points, including allocation concealment and blinding of participants or personnel, that need careful consideration in interpreting these findings [4]. Further research is needed.
According to the meta-analysis conducted with botulinum toxin, the overall incontinence rate was 5.01%. An important point to note is that most patients experienced only transient flatus or mucus incontinence, which lasted up to 8 weeks postoperatively and resolved spontaneously [20].
A meta-analysis found that the success rate of LIS for treating chronic anal fissures was 90.2% (90.1% for the closed method and 90.3% for the open method). Our study had similar results. These success rates of open and closed LIS in our study and the meta-analysis are higher than that of conservative management, with success rates of 65% to 75%. In the comparative study of botulinum toxin and LIS, LIS provided a faster, more stable, and permanent effect [22]. The success rate of the botulinum toxin group dropped to 75.4%, whereas it remained stable in the LIS group (94%) at 12 months. As a result, the authors suggested that botulinum toxin injection is not superior to LIS treatment. However, they reported an anal incontinence rate of 16% of varying degrees after surgery [20]. Patients can sometimes present with a triad syndrome, which includes a hypertrophic anal papilla on the proximal part of the fissure, a sentinel pile on the distal part of the fissure, and a chronic anal fissure. Some studies describe the excision of a skin tag and hypertrophic papilla during LIS to be associated with reduced pain, irritation during defecation, decreased foreign body sensation, and reduced itching [4].
Anal incontinence is a frightening result for both the surgeon and patient. Arroyo et al reported a recovery rate of 92.5% in patients undergoing LIS surgery. However, the rate of procedure-related anal incontinence was 5% [8]. Sánchez et al observed this complication in 5% of patients [18]. In contrast, some studies have shown a higher prevalence of this morbidity [7,10]. Gas/liquid incontinence was observed in 8 cases (1.8%) in the study by Acar et al. All patients who developed permanent incontinence were women with a history of vaginal delivery [7]. Especially in patients with a history of vaginal delivery, to avoid increasing the risk of permanent or temporary incontinence, we should consider a more controlled sphincterotomy or prioritize medical treatment first.
The potential risk of fecal incontinence after LIS seems to be variable, according to many factors, such as age, anatomical differences between men and women, pregnancy and vaginal delivery, history of pelvic surgery, surgeon inexperience, and inappropriate technique. However, of the 5 patients that developed incontinence in our study, 4 were men, and 1 was a woman. The mean age was 46.40 years. There was 1 case of gas incontinence and 4 of fecal incontinence among the patients. It is noteworthy that all the cases were in the closed LIS group, although there was no statistical difference between groups. In our study, while the overall mean was 2.65% in terms of incontinence, the risk of incontinence was 5.15% in those who had closed LIS. Even though there was no statistically significant difference, relatively uncontrolled sphincterotomy performed in the closed technique increased the risk of incontinence. Additionally, in our series, we attribute the higher incidence of incontinence in men to the mistaken perception of high anal tone, due to elevated pelvic muscle tone, and excessive sphincterotomy after the procedure. Furthermore, the observed higher incidence of incontinence in male patients in our study has not been explicitly emphasized in the literature.
Night et al found fecal incontinence in 21.3% of open LIS cases and in 4.3% of closed LIS cases [13]. Incontinence following LIS is a complex condition directly related to sphincterotomy rather than sex, age, or other operations combined with LIS (hemorrhoidectomy) or birth-related vaginal trauma, and it will have better continence rates when sphincterotomy attempts are more limited. The issues in which postoperative outcomes are evaluated are complex, and studies advocating the continence superiority of the closed LIS method by comparing open LIS and closed LIS techniques should be viewed with some skepticism [5,7,21,22].
Although the findings regarding continence in our study were not statistically significant, no incontinence was observed in patients who underwent open LIS, while gas/fecal incontinence was observed in 5 patients who underwent closed LIS. Controlled sphincterotomy in open LIS cases may be the result of more limited incision of the internal anal sphincter, and the open method seems to be more advantageous in terms of continence (Figure 5). In addition, anal fissure in patients progressed with a low recurrence rate, at recurrence rates similar to that in the literature. We argue that performing sphincterotomy based on the degree of anal tone during surgery can lead to misdirection, especially for male patients, and result in excessive muscle cutting that could increase the risk of incontinence. We advocate for a standardized, specific sphincterotomy for each patient.
While previous studies have reported higher rates of gas incontinence with the open method, they failed to specify the sex and age distribution of the incontinent cases. It is important to consider that sphincterotomy performed based on anal tone in the closed LIS method can lead to a higher incidence of incontinence, especially in young male patients. We believe that our study, which evaluated patients with a balanced sex and age distribution, yielded more accurate results than previous studies. Recent studies support balanced open sphincterotomy to reduce potential complications [11,23]. Although one study reported no cases of incontinence or recurrence, the description of the closed sphincterotomy technique in that study was stated as “partial sphincterotomy was performed.” This is a non-standardized definition and is similarly described in many closed sphincterotomy techniques [24].
In addition, complications such as wound infection, hematoma, abscess, and anal fistula can develop after LIS [25]. In our study, apart from recurrence, pain, and incontinence, complications such as abscess, discharge, constipation, bleeding, itching, and tenesmus also developed at a low rate; however, no statistically significant relationship was found between the development of complications and the type of surgery (
Abscess drainage was performed in 1 patient, who developed an abscess after closed LIS, while other complications mostly resolved clinically in the long term. Abscess formation is rare in open LIS, as any collection will most likely decompress from the surgical incision. In addition, suturing or leaving the wound open in the LIS did not affect the clinical outcome [20].
While the mean age of the patients who developed complications was between 34 and 43 years, tenesmus developed postoperatively in 2 patients with a relatively higher mean age of 55 years and who underwent closed LIS. The youngest mean age was for patients with pain complications; however, no statistically significant correlation was observed between the types of complications and mean age (
The most important limitations of this study are its retrospective and single-centered design and the procedures having been performed by different surgeons. In addition, anal canal pressure was not known, because anal manometry was not performed. However, despite being a single-center study, we believe that our objectively shared LIS results will significantly contribute to surgeons interested in anorectal surgery.
Conclusions
LIS procedures are considered the criterion standard in treatment of anal fissures and should be regarded as the definitive treatment. No difference was found between the open and closed techniques in terms of recurrence, itching, or bleeding. Open LIS emerged as a superior technique in relation to incontinence, which is major concern for both patients and surgeon, particularly in regard to young male patients.
Figures
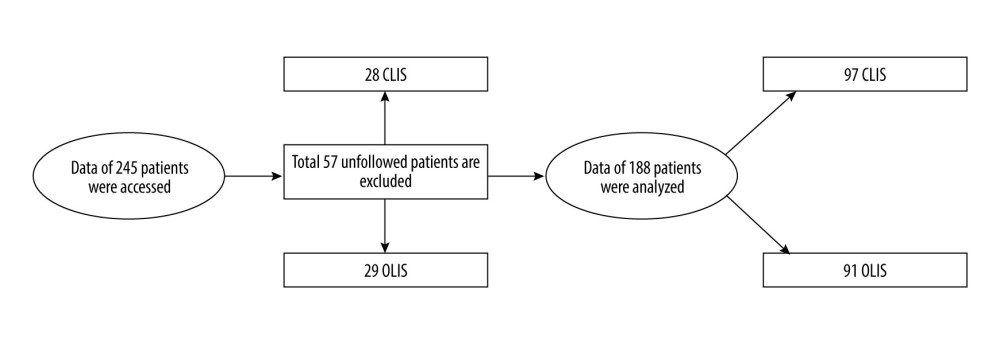 Figure 1. Flow chart of patients included in the study.
Figure 1. Flow chart of patients included in the study.  Figure 2. View of internal sphincter.
Figure 2. View of internal sphincter. 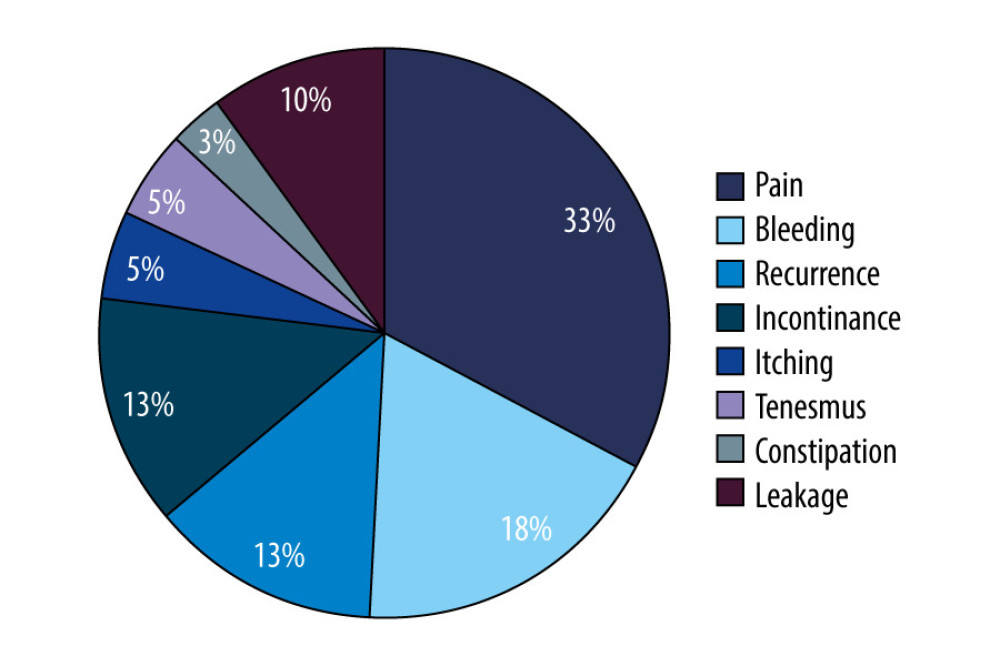 Figure 3. Distribution of complication types of patients.
Figure 3. Distribution of complication types of patients. 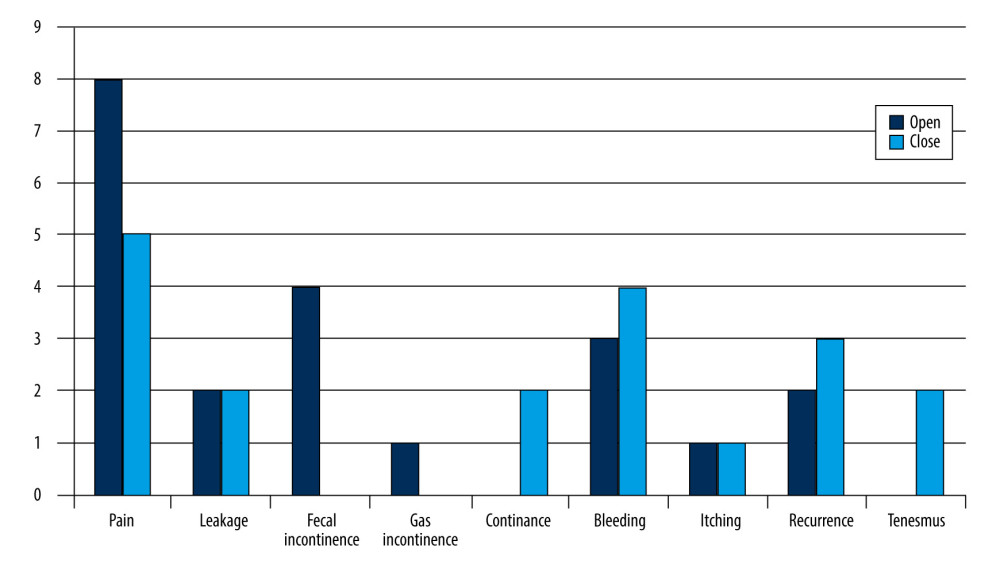 Figure 4. Distribution of complication types according to open lateral internal sphincterotomy (LIS) and closed LIS groups of patients. Dark blue column shows open LIS, light blue column shows closed LIS.
Figure 4. Distribution of complication types according to open lateral internal sphincterotomy (LIS) and closed LIS groups of patients. Dark blue column shows open LIS, light blue column shows closed LIS.  Figure 5. Sphincterotomy.
Figure 5. Sphincterotomy. References
1. Wienert V, Raulf F, Mlitz H: Anal fissure: Symptoms, diagnosis and therapies, 2017, Chan, Switzerland, Springer International Publishing AG
2. De Robles MS, Young CJ, Real world outcomes of lateral internal sphincterotomy vs botulinum toxin for the management of chronic anal fissures: Asian J Surg, 2022; 45(1); 184-88
3. Madalinski MH, Identifying the best therapy for chronic anal fissure: World J Gastrointest Pharmacol Ther, 2011; 2(2); 9-16
4. Asefa Z, Awedew anal fissure. Comparing closed versus open lateral internal sphincterotomy for management of chronic anal fissure: Systematic review and meta-analysis of randomised control trials: Sci Rep, 2023; 13(1); 20957
5. Wiley M, Day P, Rieger N, Open vs. closed lateral internal sphincterotomy for idiopathic fissure-in-ano: A prospective, randomized, controlled trial: Dis Colon Rectum, 2004; 47(6); 847-52
6. Notaras MJ, The treatment ofanal fissure by lateral subcutneous internal sphincterotomy – a technique and results: Br J Surg, 1971; 58(2); 96-100
7. Acar T, Acar N, Güngör F, Treatment of chronic anal fissure: Is open lateral internal sphincterotomy (LIS) a safe and adequate option?: Asian J Surg, 2019; 42(5); 628-33
8. Arroyo A, Pérez F, Serrano P, Surgical versus chemical (botulinum toxin) sphincterotomy for chronic anal fissure: Long-term results of a prospective randomized clinical and manometric study: Am J Surg, 2005; 189(4); 429-34
9. Whatley JZ, Tang SJ, Glover PH, Management of complicated chronic anal fissures with high-dose circumferential chemodenervation (HDCC) of the internal anal sphincter: Int J Surg, 2015; 24(Pt A); 24-26
10. Jorge JM, Wexner SD, Etiology and management of fecal incontinence: Dis Colon Rectum, 1993; 36(1); 77-97
11. Sungurtekin U, Ozgen U, Sungurtekin H, Prospective, randomized, controlled trial of ultra-modified internal sphincterotomy vs closed lateral internal sphincterotomy for chronic fissure-in-ano: Am Surg, 2022; 88(9); 2388-96
12. Farouk R, Monson JR, Duthie GS, Technical failure of lateral sphincterotomy for the treatment of chronic anal fissure: a study using endoanal ultrasonography: Br J Surg, 1997; 84(1); 84-85
13. Ghayas N, Younus SM, Mirani AJ, Frequency of post-operatıve faecal ıncontınence ın patıents wıth closed and open ınternal anal sphıncterotomy: J Ayub Med Coll Abbottabad, 2015; 27(4); 878-82
14. Danish KF, Chaudhry AR, Khan SS, Intractable headache as a side effect of topical nitroglycerine ointment: Rawal Med J, 2008; 33(1); 15-17
15. Ali M, Akhtar R, Mirza TI, Chronic anal fissure; Comparison of lateral anal sphincterotomy (closed method) versus anal dilatation: Professional Med J, 2011; 18(2); 215-21
16. García-Granero E, Sanahuja A, García-Botello SA, The ideal lateral internal sphincterotomy: clinical and endosonographic evaluation following open and closed internal anal sphincterotomy: Colorectal Dis, 2009; 11(5); 502-7
17. Liratzopoulos N, Efremidou EI, Papageorgiou MS, Lateral subcutaneous internal sphincterotomy in the treatment of chronic anal fissure: Our experience: J Gastrointestin Liver Dis, 2006; 15(2); 143-47
18. Sánchez Romero A, Arroyo Sebastián A, Pérez Vicente F, Open lateral internal anal sphincterotomy under local anesthesia as the gold standard in the treatment of chronic anal fissures. A prospective clinical and manometric study: Rev Esp Enferm Dig, 2004; 96(12); 856-63
19. Sharp FR, Patient selection and treatment modalities for chronic anal fissure: Am J Surg, 1996; 171(5); 512-15
20. Bobkiewicz A, Francuzik W, Krokowicz L, Botulinum toxin injection for treatment of chronic anal fissure: Is there any dose-dependent efficiency? a meta-analysis: World J Surg, 2016; 40(12); 3064-72 Erratum in: World J Surg. 2016;40(12):3063
21. Elsebae MM, A study of fecal incontinence in patients with chronic anal fissure: Prospective, randomized, controlled trial of the extent of internal anal sphincter division during lateral sphincterotomy: World J Surg, 2007; 31(10); 2052-57
22. Shanmugaiah A, Pandian S, Prospective randomized study between open vs closed lateral anal internal sphincterotomy in patients with chronic fissure in ano: Acad J Surg, 2020; 3(1); 167-71
23. Gupta V, Rodrigues G, Prabhu R, Ravi C, Open versus closed lateral internal anal sphincterotomy in the management of chronic anal fissures: A prospective randomized study: Asian J Surg, 2014; 37(4); 178-83
24. Garg P, Garg M, Menon GR, Long-term continence disturbance after lateral internal sphincterotomy for chronic anal fissure: A systematic review and meta-analysis: Colorectal Dis, 2013; 15(3); e104-17
25. Alva S, Chinn B, Yanar TF: Kolon rektum cerrahisi; Anorektal ameliyatlar, 2015; 17; 163-69, İstanbul, İstanbul Tıp Kitabevi
Figures
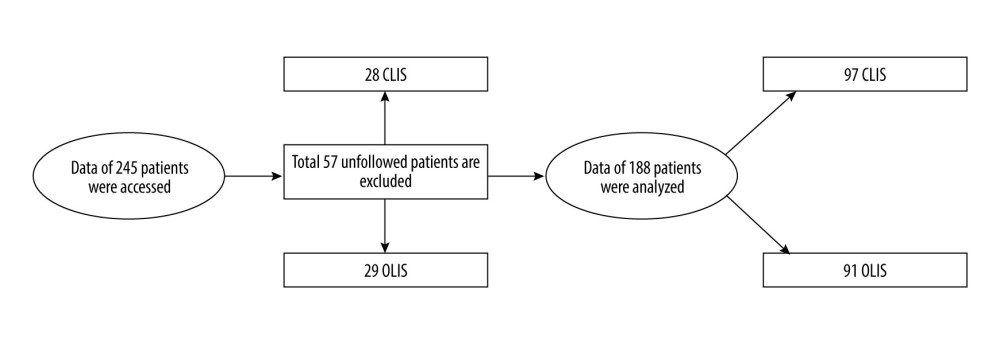 Figure 1. Flow chart of patients included in the study.
Figure 1. Flow chart of patients included in the study. Figure 2. View of internal sphincter.
Figure 2. View of internal sphincter.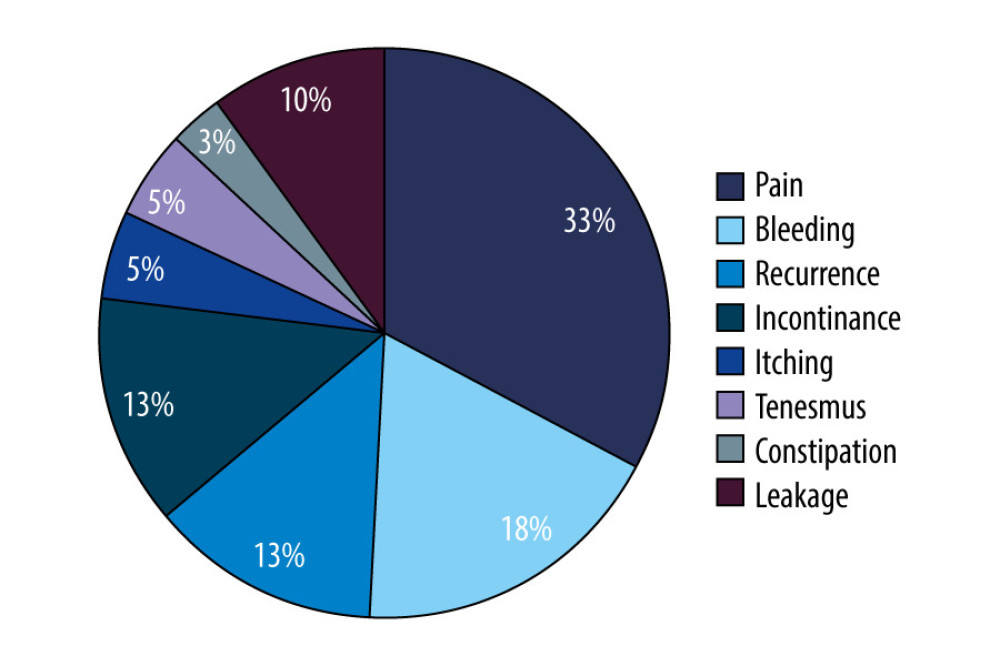 Figure 3. Distribution of complication types of patients.
Figure 3. Distribution of complication types of patients.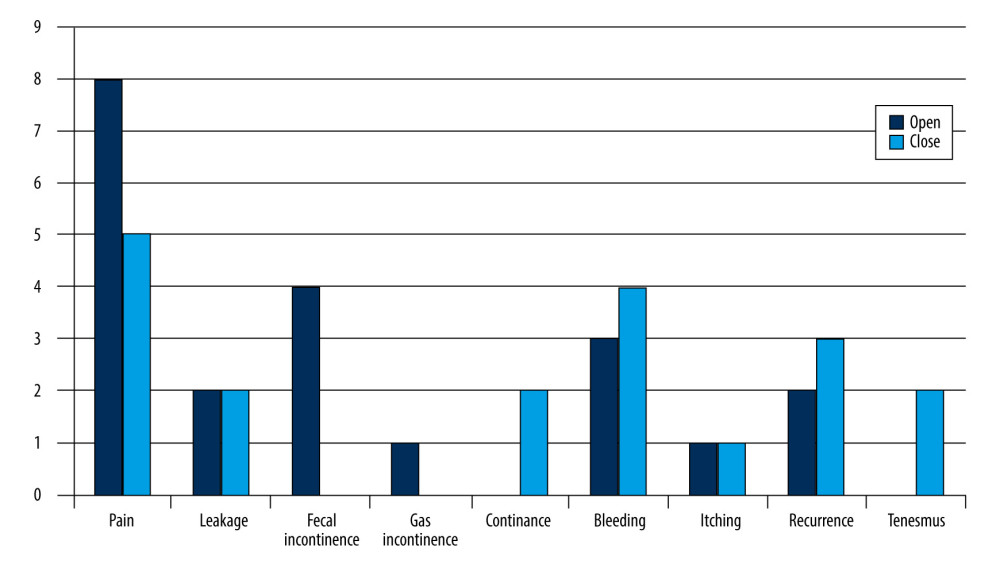 Figure 4. Distribution of complication types according to open lateral internal sphincterotomy (LIS) and closed LIS groups of patients. Dark blue column shows open LIS, light blue column shows closed LIS.
Figure 4. Distribution of complication types according to open lateral internal sphincterotomy (LIS) and closed LIS groups of patients. Dark blue column shows open LIS, light blue column shows closed LIS. Figure 5. Sphincterotomy.
Figure 5. Sphincterotomy. Tables
 Table 1. Comparison of follow-up time, age, and complications according to open and closed lateral internal sphincterotomy surgery groups of patients.
Table 1. Comparison of follow-up time, age, and complications according to open and closed lateral internal sphincterotomy surgery groups of patients.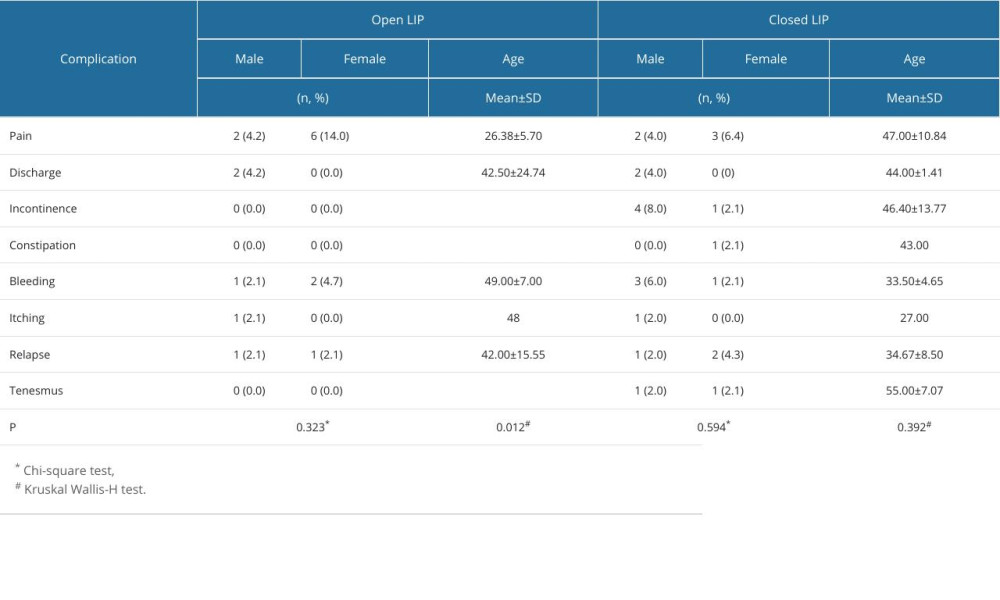 Table 2. Comparison of complications according to sex and age of patients.
Table 2. Comparison of complications according to sex and age of patients.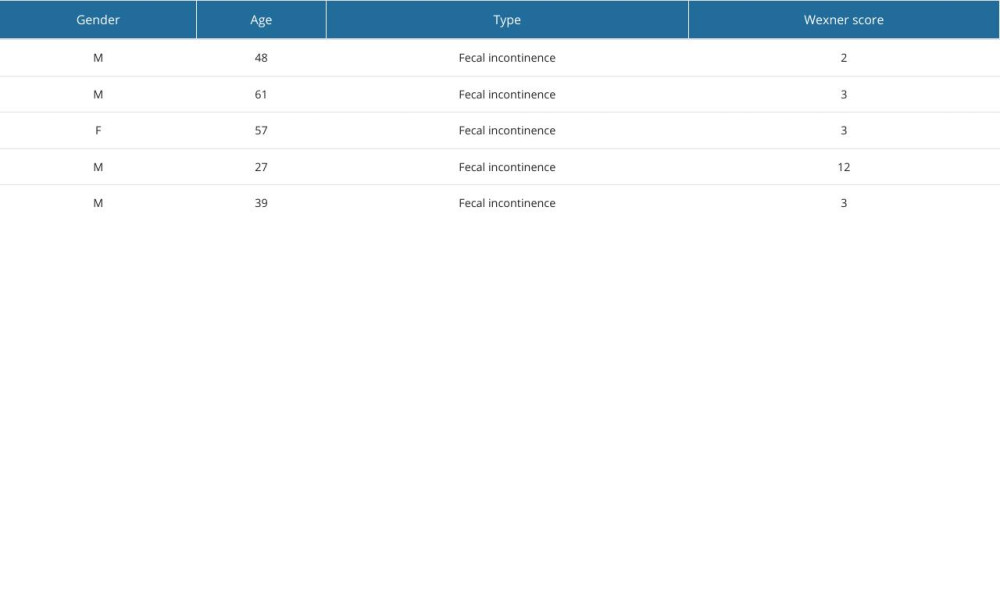 Table 3. Characteristics if incontinence complications.
Table 3. Characteristics if incontinence complications. Table 1. Comparison of follow-up time, age, and complications according to open and closed lateral internal sphincterotomy surgery groups of patients.
Table 1. Comparison of follow-up time, age, and complications according to open and closed lateral internal sphincterotomy surgery groups of patients.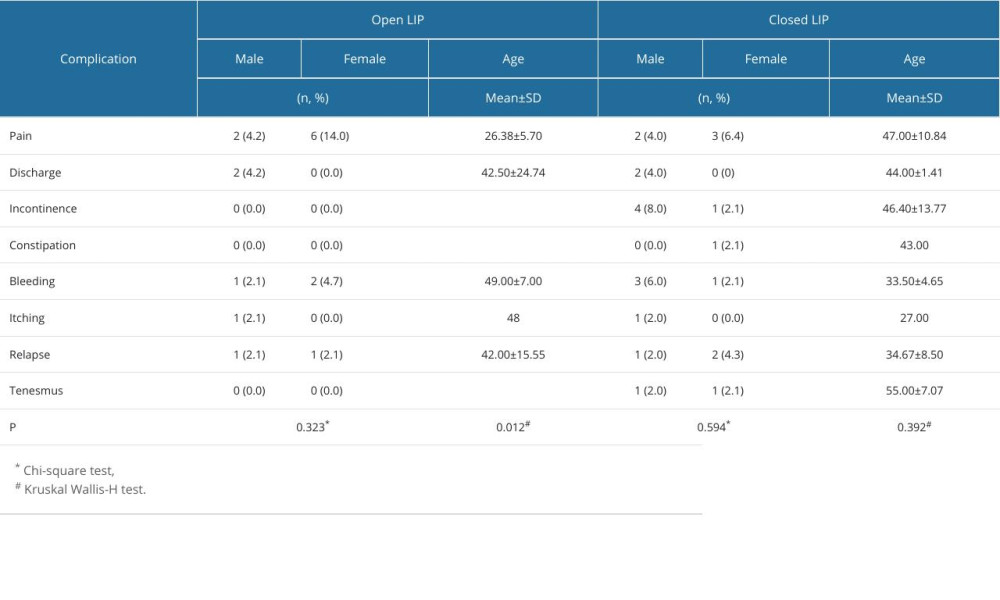 Table 2. Comparison of complications according to sex and age of patients.
Table 2. Comparison of complications according to sex and age of patients.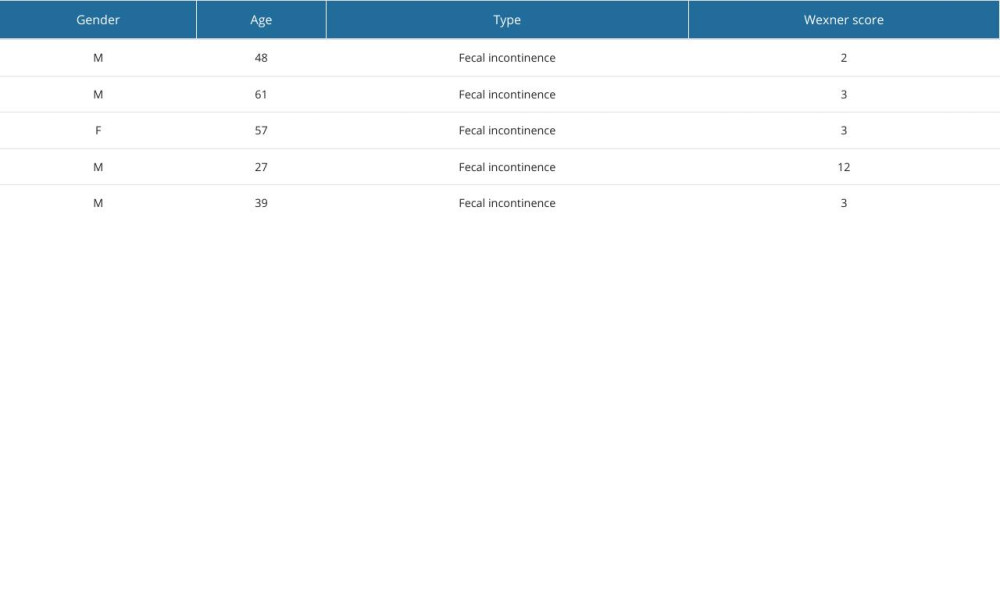 Table 3. Characteristics if incontinence complications.
Table 3. Characteristics if incontinence complications. In Press
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








