02 May 2023: Clinical Research
Clinical Results of Decortication with Bone Grafting Method versus Extracorporeal Shock Wave Treatment in Long-Bone Pseudoarthrosis
Mehmet Ata Gökalp1ABEFG*, Seyyid Şerif Ünsal2BCDF, Savaş Güner3AEFG, Tülin Türközü1BCEFG, Necip Güven1BDFDOI: 10.12659/MSM.939395
Med Sci Monit 2023; 29:e939395
Abstract
BACKGROUND: Despite advanced treatment methods, the treatment of pseudoarthrosis still poses a significant challenge for orthopedists. In this study, we aimed to assess the clinical results of decortication and bone grafting and extracorporeal shock wave treatment (ESWT) in long-bone pseudoarthrosis.
MATERIAL AND METHODS: Between 2007 and 2015, 68 fractures of 66 patients treated for long-bone pseudoarthrosis were evaluated retrospectively. ESWT was used in 36 extremities and decortication and iliac bone grafting was used in 32. The treatment results of these patients were evaluated and compared with rates in the literature.
RESULTS: The mean patient age was 43.9 years (range, 21-69). The mean interval between the occurrence of the fracture and treatment with bone grafting or ESWT was 8.6 months and the mean interval between the procedure and achievement of union was 6.9 months. The patients were followed up for a mean period of 25.2 months. After the mean follow-up period, bone union had occurred in all 32 patients (100%) in the decortication and bone grafting group and in 28 (78%) of the 36 patients in the ESWT group (P=0.023).
CONCLUSIONS: This study shows that extracorporeal shock wave treatment should be considered the first option in treatment of pseudoarthrosis as it is a non-invasive method and also provides good rates of union. In patients that do not heal with ESWT, decortication and bone grafting remains the criterion standard therapy.
Keywords: Extracorporeal Shockwave Therapy, Bones of Lower Extremity, Pseudarthrosis, Ilium, Humans, young adult, Adult, Middle Aged, Aged, Fractures, Ununited, Bone Transplantation, Retrospective Studies, Fracture Healing, Fractures, Bone, Treatment Outcome
Background
Long-bone fractures of the lower extremity are injuries that cause significant physical problems [1]. These fractures usually occur after high-energy traumas and lead to important movement disorders, malunion, delayed union, and non-union [2]. Non-union of fractures causes chronic pain, functional and psychological disorders, impairs quality of life, and increases treatment costs [3]; 9–10% of lower-extremity fractures result in non-union. In open fractures, depending on the severity of the fractures type, non-union rates can reach 50% [4,5]. The treatment of pseudoarthrosis is mechanical stabilization and biological stimulation [6].
Debridement of the necrotic tissue and removing devitalized bone fragments from the pseudoarthrosis site and inserting autologous cancellous bone grafting between the fracture ends and fixation is considered the criterion standard treatment of pseudoarthrosis [7,8]. This treatment is still considered the first option for treating pseudoarthrosis, and success rates of 85–95% are reported [7]. However, up to 8.6% of patients treated with this method have major complications (eg, infection, prolonged wound drainage, hematomas, advanced surgery, and permanent pain) and up to 20% have minor complications (eg, superficial wound infection, temporary loss of sensation, mild pain) [9]. Non-union and delayed union fractures are treated with surgical stabilization with or without bone graft reinforcement. High-energy focused extracorporal shock wave therapy (ESWT), on the other hand, has emerged as a non-invasive, cost-effective, and similarly successful method [10].
ESWT is a non-invasive outpatient procedure to biologically stimulate fracture healing in non-unions [11]. For the last 30 years, ESWT has been used in orthopedics and traumatology for the treatment of plantar fasciitis, lateral humeral epicondylitis, non-union and delayed union of fractures, calcified shoulder tendinitis, aseptic necrosis of the femoral head, achilles tendinitis, patellar tendinitis, and osteochondritis dissecans [12]. Since Valchanou and Michailov reported a success rate of 85% in the treatment of pseudoarthrosis in 1991, ESWT has been used widely in orthopedics and traumatology for treatment of fractures and pseudoarthrosis [13].
Until the present work, no study had compared both methods in the literature.Therefore, a comparative study was planned with the hypothesis that ESWT could be an alternative to traditional surgical methods in the treatment of biologically active pseudoarthrosis of the lower-extremity long bone.
Material and Methods
DECORTICATION AND AUTOLOGOUS BONE GRAFTING SURGICAL TECHNIQUE:
In decortication and bone grafting, after the pseudoarthrosis field is opened, the fibrotic and necrotic bone tissues on the fracture line are removed, then the sclerotic bones with no nutrition at the fracture ends are refreshed until punctate bleeding spots are seen.Then, the iliac crest is opened and grafts obtained from the spongious portion are placed in the fracture line and are stabilized with appropriate fixation material. After stabilization, the periosteum is closed, covering the graft, the tissues are closed in standard fashion, and the operation is completed. In patients undergoing decortication and iliac bone grafting for tibial pseudoarthrosis, an additional fibula osteotomy is also performed (Figures 1, 2).
ESWT APPLICATION:
All patients were treated under either general or regional anesthesia. ESWT was performed with the Siemens brand device. Non-union was visualized by X-ray and the level was marked on the skin. Anatomical structures such as arteries, veins and nerves were spared by the shock waves. All patients received high-energy ESWT (0.6 mJ/mm2) with 3000 impulses administered to 3–4 different foci in 1 session. Cold therapy was applied to the procedure site in all patients within the first 24 hours (Figures 3, 4).
EVALUATION:
The mean intervention times was the same in both groups, the mean time to union was 6.6 months in the decortication and bone grafting group and 7.3 months in the ESWT group, the mean follow-up period was 20.9 months in the decortication and bone grafting group and 29.6 months in ESWT group, and union rates were evaluated. After the intervention, physical examination and two-view radiographic union findings were evaluated monthly in the first 3 months, then 3 and 6 months later, then annually. Painless palpation and weight bearing, no crepitations on the fracture line, no pathological movements, and the presence of calluses in 3 of the 4 bone cortexes in two-view radiographs were considered supportive of union after this evaluation. The Cech and Weber vascular-avascular pseudoarthrosis classification was used to identify the type of the pseudoarthrosis (Table 1) [14]. The Stewart-Hundley and Hammer classification was used to evaluate clinical and radiological healing [15].
STATISTICAL ANALYSES:
Among the features assessed, the defining statistics of continuous variables were expressed as means, standard deviations, and minimum and maximum values, and the categorical variables were expressed as numbers and percentages. For continuous variables, the
Results
The mean age of the patients was 44.1 years (range, 24–69 years) in the decortication and bone grafting group and 43.8 (range, 21–62) in the ESWT group. There were 26 males and 6 females in the decortication and bone grafting groups, and 28 males and 8 females in the ESWT group. There was no statistically significant difference between the 2 groups in terms of age and sex (
According to the Cech Weber pseudoarthrosis classification, 4 fractures were classified as elephant’s foot, 20 fractures as horse’s hoof, and 44 fractures as oligotrophic pseudoarthrosis. The classification of patients according to the Cech and Weber vascular pseudoarthrosis classification is given in Table 1.
After the mean follow-up period, bone union had occurred in all 32 patients (100%) in the decortication and bone grafting group and in 28 (78%) of 36 patients in the ESWT group (
In respect to the fixation material used, 38 fractures were fixated with intramedullary nail and 22 fractures were fixated with external fixators. Infections developed in 12 fractures that were initially being treated with the internal fixation method. The internal stabilization was ended and external fixation was started. Eight fractures were treated with plate osteosynthesis fixation. The stabilization materials used in the initial surgeries are listed in Table 4.
The etiology of the fractures was high-energy trauma in all patients. The etiologic causes are listed in Table 5. In the decortication and bone grafting group, no complications such as wound problem or vascular-nerve injury were observed.
Discussion
The causes of delayed union or non-union include passage of soft tissue between fracture fragments, the severity of the trauma, bone loss, inadequate fixation, early mobilization, infections, presence of concomitant diseases, nonsteroidal anti-inflammatory drugs use, vitamin or protein deficiencies, hormonal disorders, presence of osteoporosis, age, and smoking [16].
A precise definition of non-union is difficult. Although it varies among sources, situations where clinical and radiological union does not occur in 6 months or one in which there is a failure of progression towards union over the previous 3 months are regarded as pseudoarthrosis [8,14,15]. However, Cech and Weber have stated that all cases believed to have no potential to heal without further intervention should be regarded as pseudoarthrosis independent of duration [17,18]. In our study, it was observed that intervention was done if pseudoarthrosis signs persisted for an average of 8.7 months in the decortication and bone grafting group and 8.6 months in the ESWT group.
Femoral and tibial fractures are seen in the young, active age group with rates of 75% and occur more frequently after high-energy traumas (eg, traffic accident, falling from height) [19]. Out of 66 patients enrolled in the study, 52 were male and 14 were female, 56 patients were 50 years old or younger, and the mean age was 43.9 years. In addition, the etiology was high-energy trauma in all patients. With these features, our cases are consistent with studies in the literature in respect to average age, sex distribution, and etiology.
For the last 30 years, ESWT has been used in orthopedics and traumatology for treatment of plantar fasciitis, lateral humeral epicondylitis, non-union and delayed union of fractures, calcified shoulder tendinitis, aseptic necrosis of the femoral head, Achilles tendinitis, patellar tendinitis, and osteochondritis dissecans [12]. Since Valchanou and Michailov reported success rates of 85% in the treatment of pseudoarthrosis in 1991, ESWT has been used widely in orthopedics and traumatology [13].
Schoellner performed ESWT under regional anesthesia in 43 patients 9 months after surgery and reported that the bone union rate after an average of 4–6 months was 75% [20]. Alvarez performed ESWT in 34 fractures in 32 metatarsal non-union patients at an average of 23 weeks after injury and reported the bone union rate as 89% after an average follow-up of 1 year [21]. Josef et al performed ESWT in 17 long-bone (tibia-femur) pseudoarthrosis patients and had a bone union rate of 64.7% [22]. Zelle reported had a 76% bone union rate, which was higher in the hypertrophic pseudoarthrosis in the 10 studies including 924 delayed unions treated with ESWT they reviewed to assess the efficacy of ESWT [23]. In our cases, we performed ESWT in single doses on 36 fractures (22 femurs, 14 tibias) after an average of 8.6 months and our bone union rate was 78% after an average of 7.3 months. When compared with rates in the literature, our union rates are similar, but our time to union was slightly longer. We attributed this to our small number of cases and the presence of fractures of lower-extremity long bones, where healing is difficult, whereas studies in the literature included fractures of nearly every bone in various regions.
Debridement of the necrotic tissue and removing devitalized bone fragments from the pseudoarthrosis site and inserting spongious bone between the fracture ends and fixation is considered the criterion standard in the treatment of pseudoarthrosis, and success rates of 85–95% are reported [7,8].
Niedzwiedzki et al mixed the graft obtained from the iliac crest with heparin and injected it into the fracture line in a case series of 92 patients. In these patients, the mean age was 36.6 years, 24 of these were new fractures, 42 were delayed unions, and 30 were pseudoarthrosis. It was reported that bone union was achieved in an average of 2.8, 3.2 and 3.4 months respectively in all of these patients [24]. The same authors reported that they treated 17 femoral or tibial pseudoarthrosis cases (mean age 48 years) with reamed locking intramedullary nails; union was achieved in 15 cases and the spreading of the bone graft on the fracture line during reaming positively affected the bone union [25]. Pawel et al performed decortication and iliac bone grafting in 56 patients with long-bone pseudoarthrosis; union was achieved in 51 cases and the time to bone union was 5 months [26]. In our case series, 32 fractures (18 femurs, 14 tibias) were present in the decortication and bone grafting group. Procedures were performed an average of 8.7 months later and union was achieved in all patients after an average of 6.6 months. Our results are consistent with the literature in respect to union outcomes and time to achieve union.
When we compared the groups with each other in the aspects of average age, sex distribution, extremity involvement, fracture etiology, fracture type (open or closed), presence of segmental fractures, presence of additional fractures, postoperative fracture reduction status, fixation material used, and the mean intervention times, the results were statistically similar.
Although factors that cause delays in union, such as high rates of fragmentation at the fracture line, a high number of patients with vascular injuries, a high number of smokers, a high number of patients with additional fractures, and a history of infection, were more common in the decortication and bone grafting group, a statistically significant difference was not identified between groups. Comorbidities (eg, protein deficiencies, diabetes mellitus, steroid use, osteoporosis) were less frequent in the ESWT group than in the decortication and bone grafting group, but the difference was not statistically significant. We believe that the differences mentioned would affect the results but did not reflect on the statistics because the patient number in the sample was low. Our mean follow-up period was longer in the ESWT group and the mean duration of bone union was lower in the decortication and bone grafting group, but these differences were not statistically significant.
While union was achieved in all of the 32 fractures in the decortication and bone grafting group, union was only achieved in 28 of the 36 patients in the ESWT group (
This study has some limitations. First of all, the number of cases was small. However, the choice of 2 different comparative treatments and the use of the same ESWT device in a single center are important factors in terms of the number of cases. Another limitation of the study is that it was retrospective. In addition, we did not perform cost analysis of the 2 treatment methods.
Conclusions
We believe that decortication and bone grafting is the first choice and best treatment method for pseudoarthrosis surgery, esespecially in defective fractures, atrophic pseudoarthrosis, inadequate fixation, and if there are reduction losses. Extracorporeal shock wave treatment can be used in non-defective fractures, in situations with adequate fixation and no reduction loss, and in all kinds of early fractures that are believed to have no potential to heal. ESWT should be considered the first option in the treatment of pseudoarthrosis as it is a non-invasive method and also provides good union rates. In patients that do not heal with this method, decortication and bone grafting remains to the criterion standard.
Figures
 Figure 1. 45-year-old male tibial fracture A) postoperative 8th month radiography B) postoperative 8th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 18th month after decortication – Bone Grafting application radiograph.
Figure 1. 45-year-old male tibial fracture A) postoperative 8th month radiography B) postoperative 8th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 18th month after decortication – Bone Grafting application radiograph. 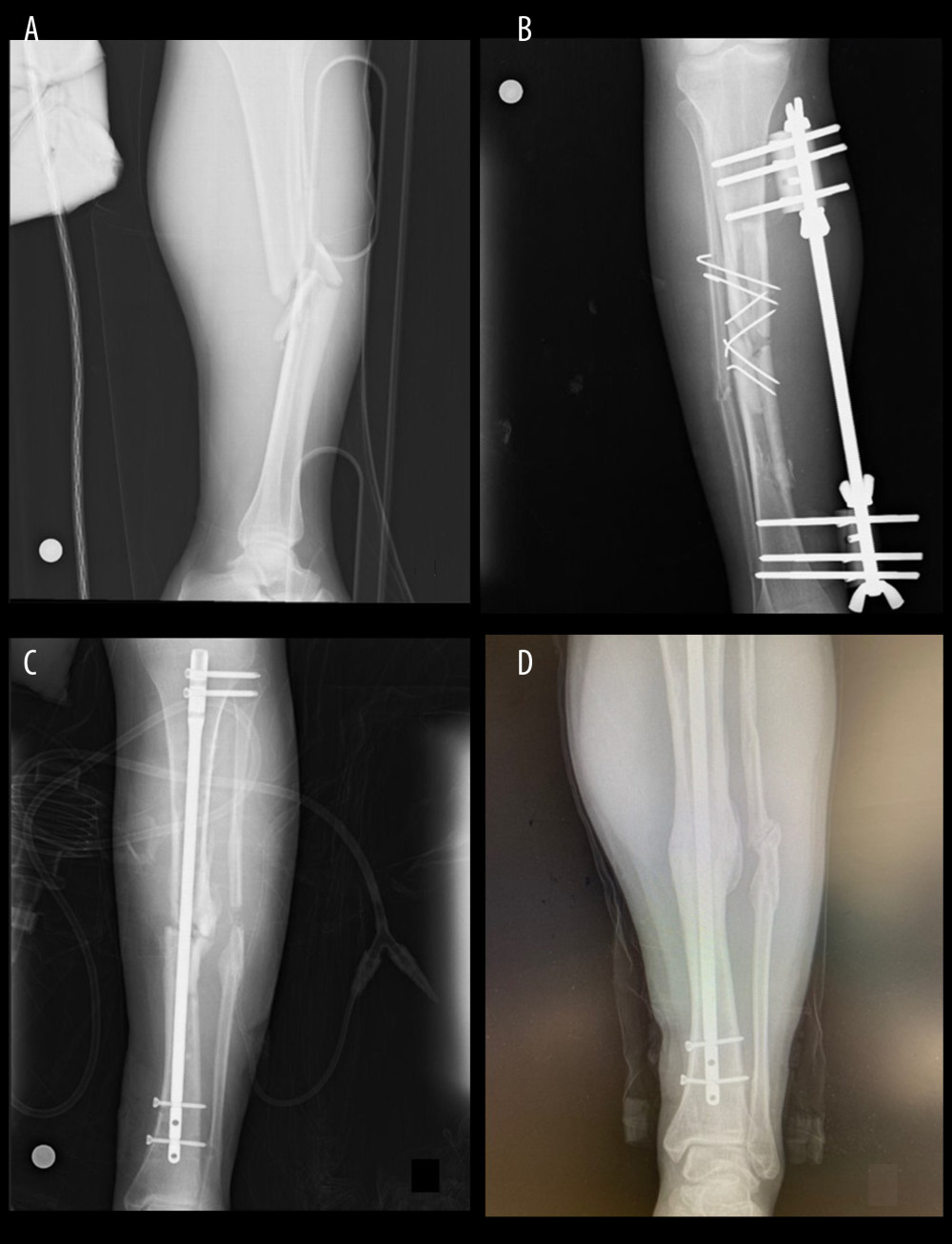 Figure 2. 43-year-old male femur fracture A) fracture radiography B) postoperative 11th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 14th month after decortication – Bone Grafting application radiograph.
Figure 2. 43-year-old male femur fracture A) fracture radiography B) postoperative 11th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 14th month after decortication – Bone Grafting application radiograph.  Figure 3. 21-year-old male femur fracture A) fracture radiography B) post-operative radiography C) post operative 12th month radiographic ESWT applied D) post-operative 18th month after ESWT application radiograph.
Figure 3. 21-year-old male femur fracture A) fracture radiography B) post-operative radiography C) post operative 12th month radiographic ESWT applied D) post-operative 18th month after ESWT application radiograph.  Figure 4. 30-year-old male tibial fracture A) fracture radiography B) postoperative radiography C) post operative 10th month radiographic ESWT applied D) post-operative 22th month after ESWT application radiograph.
Figure 4. 30-year-old male tibial fracture A) fracture radiography B) postoperative radiography C) post operative 10th month radiographic ESWT applied D) post-operative 22th month after ESWT application radiograph. Tables
Table 1. The Cech and Weber vascular pseudoarthrosis classification.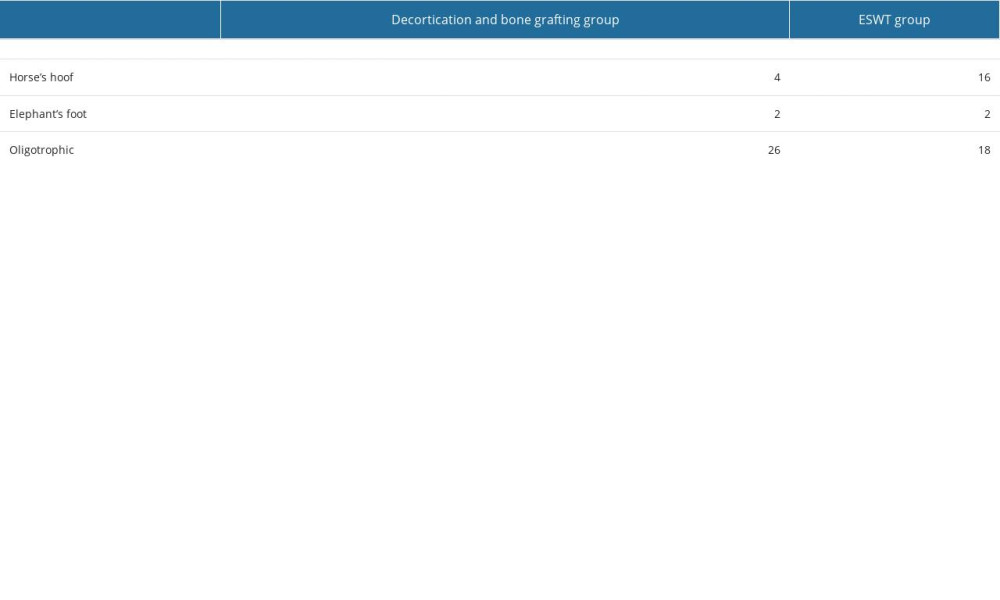 Table 2. The properties of patients fractures.
Table 2. The properties of patients fractures.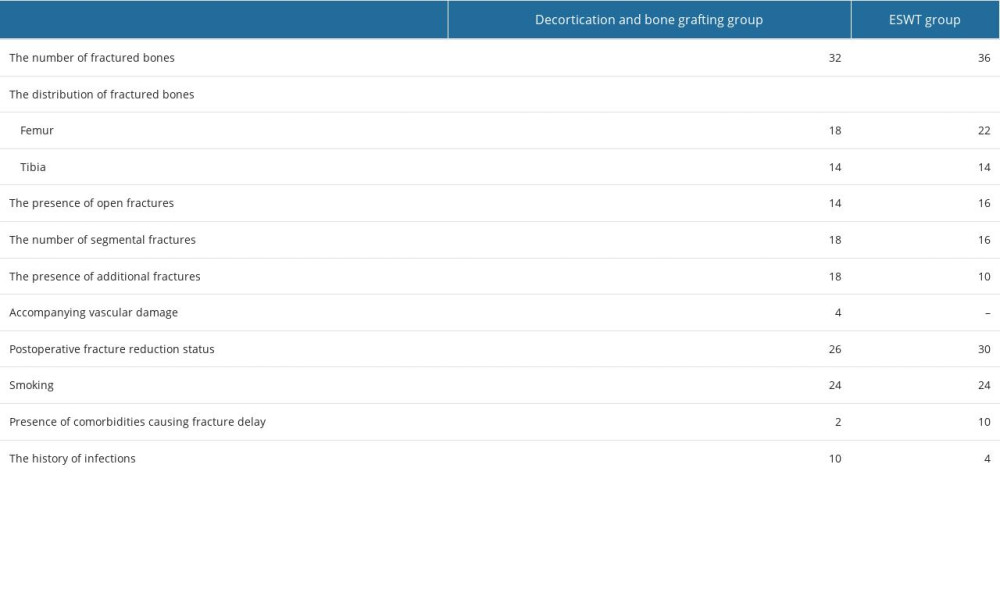 Table 3. The mean intervention time, union times, follow up period and union rate.
Table 3. The mean intervention time, union times, follow up period and union rate. Table 4. The stabilization material used in the initial surgeries of the patients.
Table 4. The stabilization material used in the initial surgeries of the patients.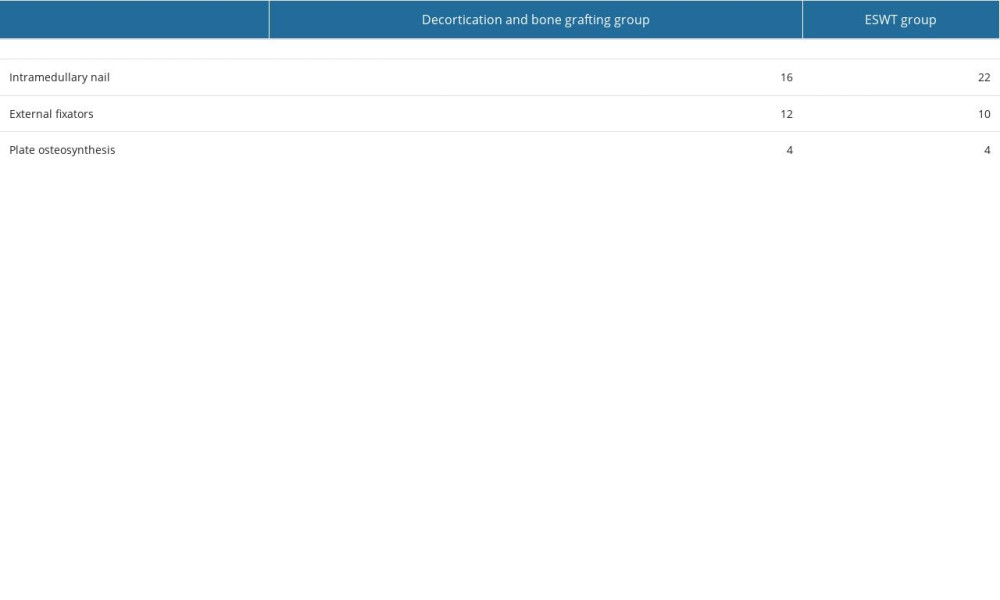 Table 5. The etiologic causes of fractures.
Table 5. The etiologic causes of fractures.
References
1. Markus R, Christoph B, Matthäus B, Diaphyseal long bone nonunions – types, aetiology, economics, and treatment recommendations: Int Orthop, 2018; 42(2); 247-58
2. Cleveland KB: Delayed union and non-union of fractures, 2013, Philadelphia, Canale & Beaty
3. Polyzois VD, Papakostas I, Stamatis ED, Current concepts in delayed bone union and non-union: Clin Podiatr Med Surg, 2006; 23; 445-53
4. Ekegren CL, Edwards ER, de Steiger R, Gabbe BJ, Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture: Int J Environ Res Public Health, 2018; 15; 2845
5. Mills LA, Aitken SA, Simpson AHRW, The risk of non-union per fracture: Current myths and revised figures from a population of over 4 million adults: Acta Orthop, 2018; 88; 434-39
6. Thomas F, Josef S, Philipp AM, Effect of bone morphogenetic protein-2 in the treatment of long bone non-unions: J Clin Med, 2021; 10(19); 4597
7. Thein E, Chevalley F, Borens O, Pseudoarthrosis of the long bones: Rey Med Suisse, 2013; 18(411); 2390-96
8. Calori GM, Mazza E, Colombo M, Ripamonti C, The use of bone-graft substitutes in large bone defects: Any specific needs ? Injury, 2011; 42(Suppl 2); 56-63
9. Younger EM, Chapman MW, Morbidity at bone graft donor sites: J Orthop Trauma, 1989; 3; 192-95
10. Kwok IHY, Ieong E, Aljalahma MA, Haldar A, Welck M, Extracorporeal shock wave treatment in foot and ankle fracture non-unions – a review: Foot (Edinb), 2022; 51; 101889
11. Georg TKG, Everding J, Stolberg J, Möglichkeiten der nicht operativen: Behandlung von Pseudarthrosen, 2019; 35; 252-61
12. Baloğlu İ, Özsoy MH, Aydınok H, Lök V, The use of shock wave therapy in orthopaedics and traumatology: Journal of Turkish Association of Orthopaedics and Traumatology, 2005; 4; 1-2
13. Valchanou VD, Michailov P, High energy shock waves in the treatment of delayed and nonunion of fractures: IntOrthop, 1991; 15(3); 181-84
14. Dijkman BG, Spraque S, Schemitsch EH, Bhandari M, When is a fracture healed? Radiographic and clinical criteria revisited: J Orthop Trauma, 2010; 24(Suppl 1); 76-80
15. Hammer R, Hammerby S, Lindholm B, Accuracy of radiologic assessment of tibial shaft fracture union in humans: ClinOrthop, 1985; 199; 233-38
16. Zura R, Xiong Z, Einhorn T, Epidemiology of fracture nonunion in 18 human bones: JAMA Surg, 2016; 151(11); 1-12
17. Johner R, Wrush O, Classification of tibial shaft fractures and correlation with result after rigid internal fixation: Clin Orthop Relat Res, 1983(178); 7-25
18. Chapman MW: Principles of treatment of nonunions and malunions, 2001; 847-85, Philadelphia, Lippincott Williams & Wilkins
19. Sudhir K, Kataria H, Boruah T, Expandable self-locking nail in the management of closed diaphyseal fractures of femur and tibia: Indian J Orthop, 2009; 43(3); 264-70
20. Schollner C, Rompe JD, Decking J, Heine J, High energy extra corporeal shock wave therapy (ESWT) in pseudoarthrosis: Orthopade, 2002; 31(7); 658-62
21. Alvarez RG, Cincere B, Channappa C, Extracorporeal shock wave treatment of non- or delayed union of proximal metatarsal fractures: Foot Ankle Int, 2011; 32(8); 746-54
22. Josef S, Thomas F, Moritz F, Addition of shock wave therapy to nail dynamization increases the chance of long bone non union healing: J Orthop Traumatol, 2022; 23; 4
23. Zelle BA, Gollwitzer H, Zlowodzki M, Bühren W, Extra corporeal shock wave therapy. Current evidence: J Orthop Trauma, 2010; 24(Suppl 1); 66-70
24. Niedzwiedzki T, Effect of bone marrow on healing of fractures, delayed unions and pseudoarthrosis of long bone: Chir Narzadow Ruchu Ortop Pol, 1993; 58(3); 194-204
25. Niedzwiedzki T, Szuscik M, Niedzwiedzki L, Interlocking intramedullary nail with reaming of bone marrow cavity in treatment of tibia and femur pseudoarthrosis: Acta Chir Orthop Traumatol Cech, 2001; 68(2); 109-11
26. Pawel R, Roman R, Krzysztof Z, Outcome treatment of pseudoarthrosis of long bones with decortication method, depends on osteosynthesis: Chir Narzadow Ruchu Ortop Pol, 2007; 72(3); 175-79
Figures
 Figure 1. 45-year-old male tibial fracture A) postoperative 8th month radiography B) postoperative 8th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 18th month after decortication – Bone Grafting application radiograph.
Figure 1. 45-year-old male tibial fracture A) postoperative 8th month radiography B) postoperative 8th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 18th month after decortication – Bone Grafting application radiograph.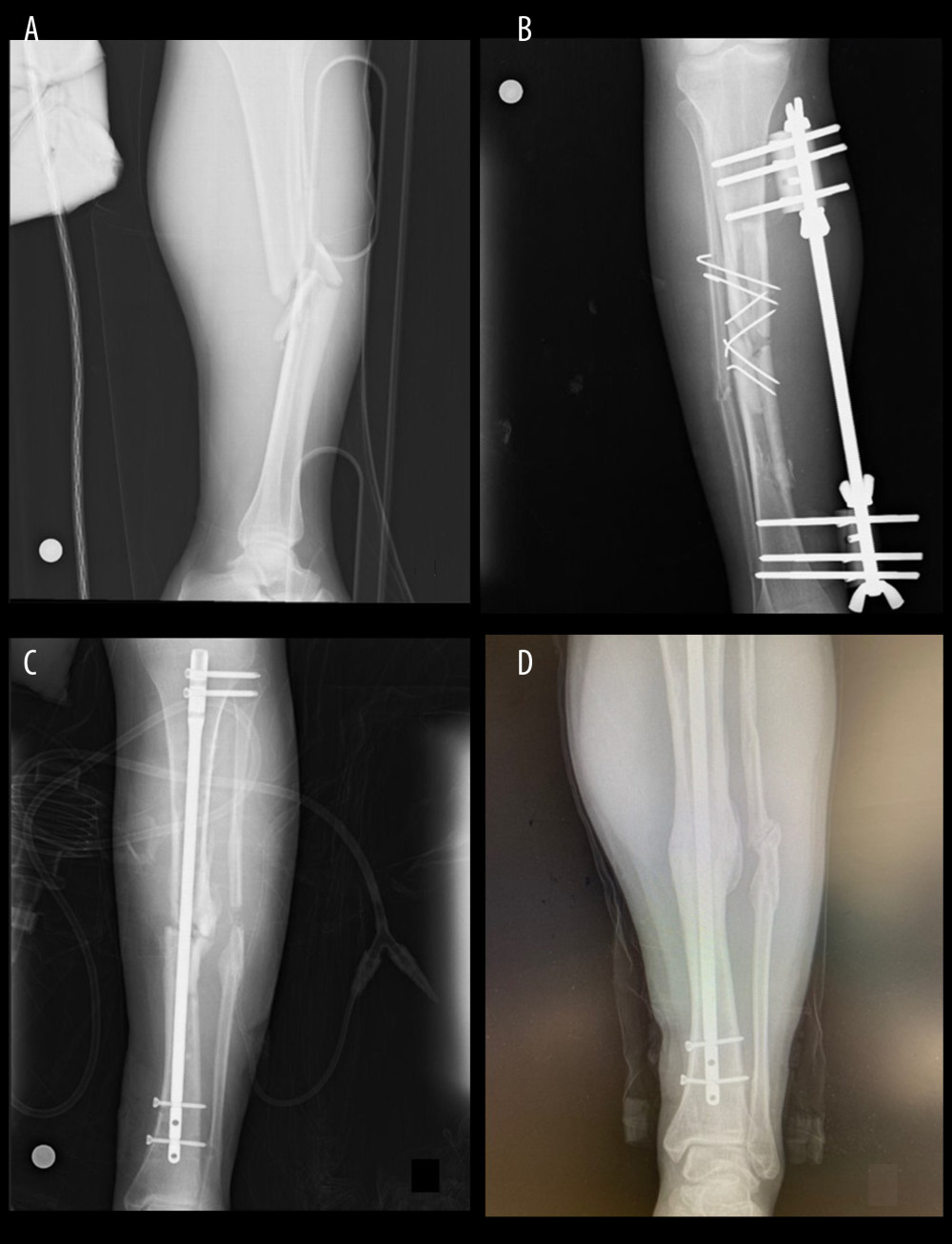 Figure 2. 43-year-old male femur fracture A) fracture radiography B) postoperative 11th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 14th month after decortication – Bone Grafting application radiograph.
Figure 2. 43-year-old male femur fracture A) fracture radiography B) postoperative 11th month radiography C) Decortication – Bone Grafting Method application postoperative radiograph D) postoperative 14th month after decortication – Bone Grafting application radiograph. Figure 3. 21-year-old male femur fracture A) fracture radiography B) post-operative radiography C) post operative 12th month radiographic ESWT applied D) post-operative 18th month after ESWT application radiograph.
Figure 3. 21-year-old male femur fracture A) fracture radiography B) post-operative radiography C) post operative 12th month radiographic ESWT applied D) post-operative 18th month after ESWT application radiograph. Figure 4. 30-year-old male tibial fracture A) fracture radiography B) postoperative radiography C) post operative 10th month radiographic ESWT applied D) post-operative 22th month after ESWT application radiograph.
Figure 4. 30-year-old male tibial fracture A) fracture radiography B) postoperative radiography C) post operative 10th month radiographic ESWT applied D) post-operative 22th month after ESWT application radiograph. Tables
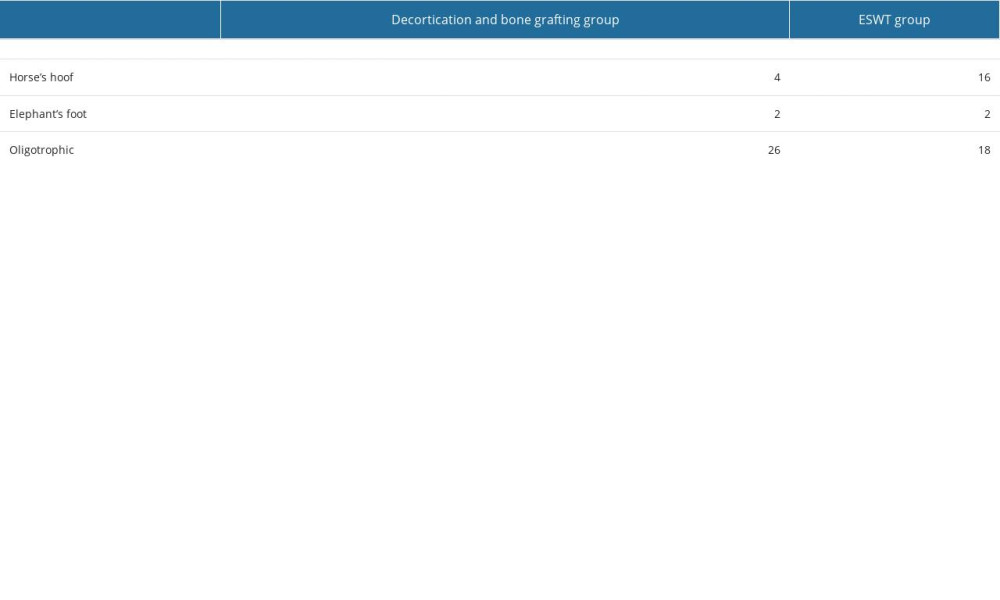 Table 1. The Cech and Weber vascular pseudoarthrosis classification.
Table 1. The Cech and Weber vascular pseudoarthrosis classification.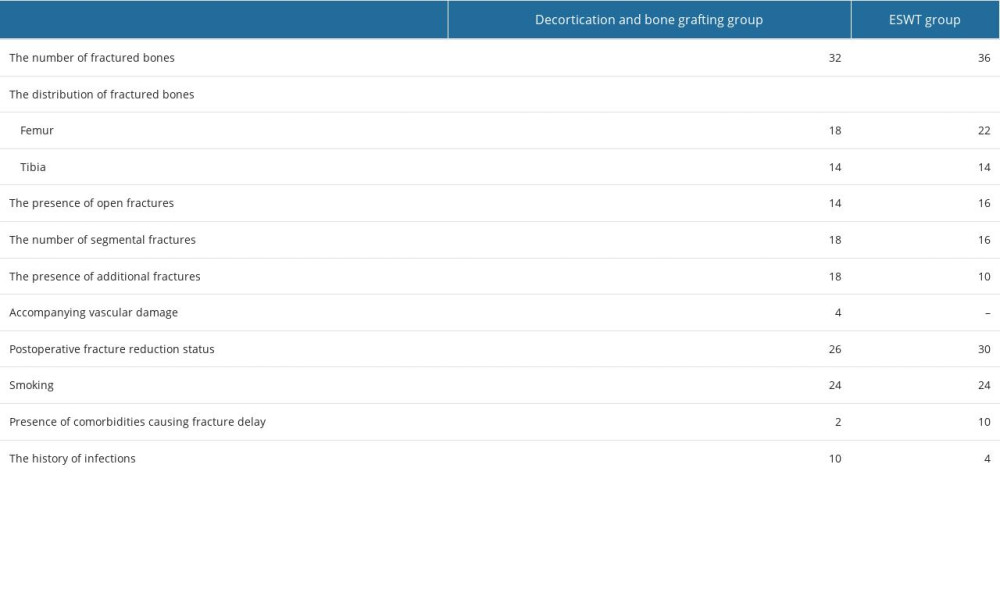 Table 2. The properties of patients fractures.
Table 2. The properties of patients fractures. Table 3. The mean intervention time, union times, follow up period and union rate.
Table 3. The mean intervention time, union times, follow up period and union rate.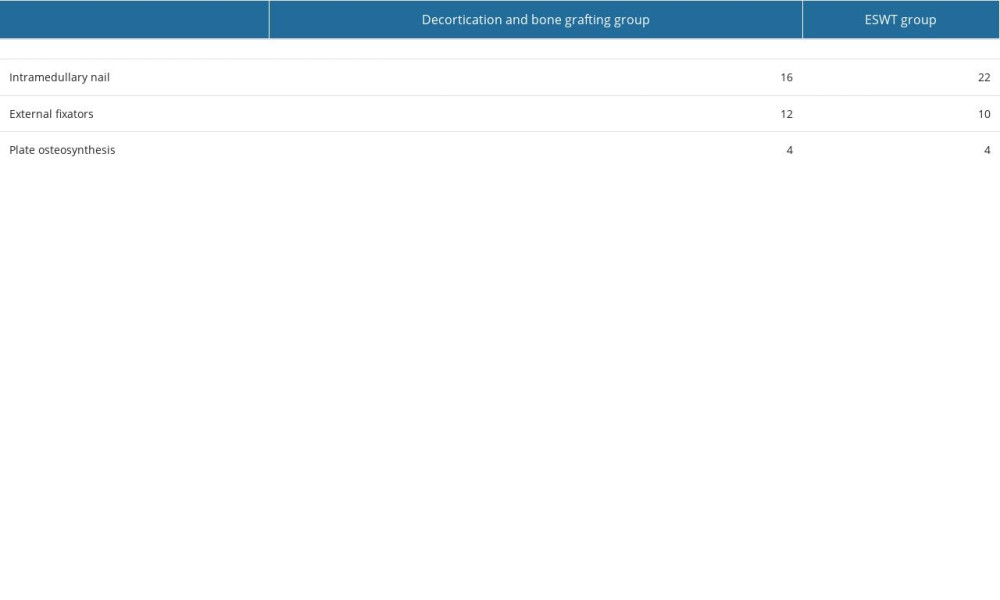 Table 4. The stabilization material used in the initial surgeries of the patients.
Table 4. The stabilization material used in the initial surgeries of the patients. Table 5. The etiologic causes of fractures.
Table 5. The etiologic causes of fractures.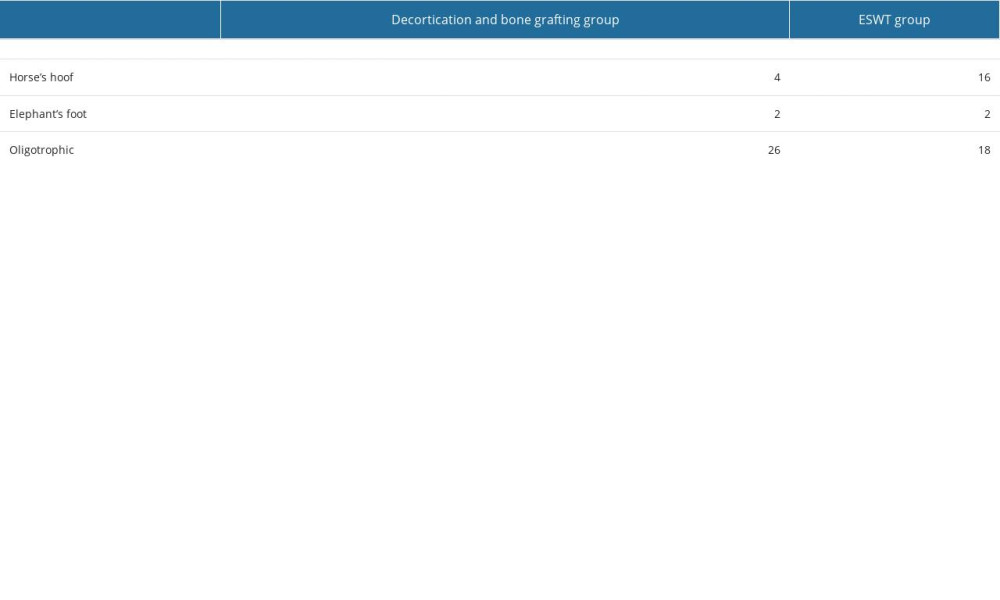 Table 1. The Cech and Weber vascular pseudoarthrosis classification.
Table 1. The Cech and Weber vascular pseudoarthrosis classification.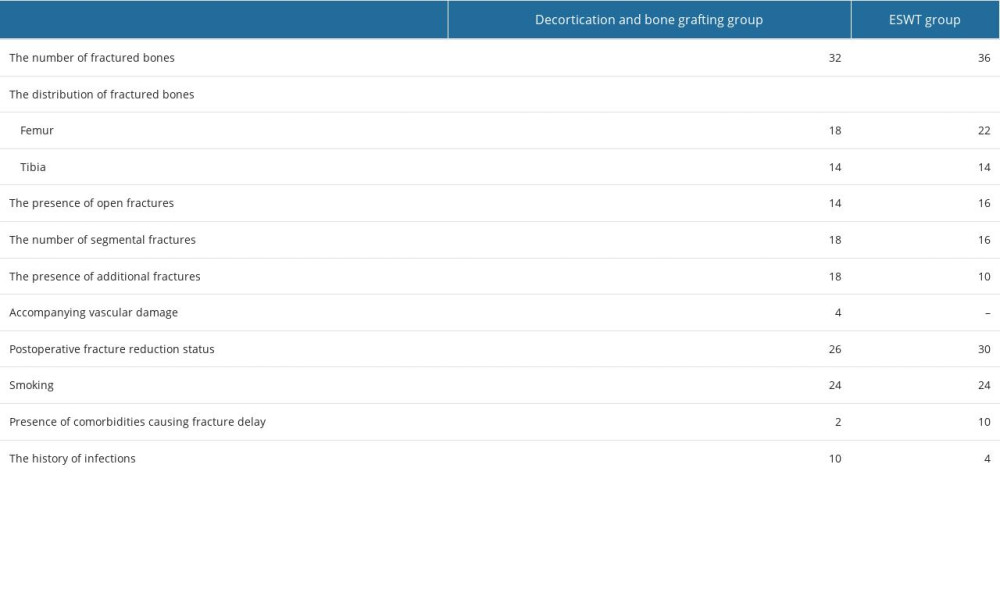 Table 2. The properties of patients fractures.
Table 2. The properties of patients fractures. Table 3. The mean intervention time, union times, follow up period and union rate.
Table 3. The mean intervention time, union times, follow up period and union rate.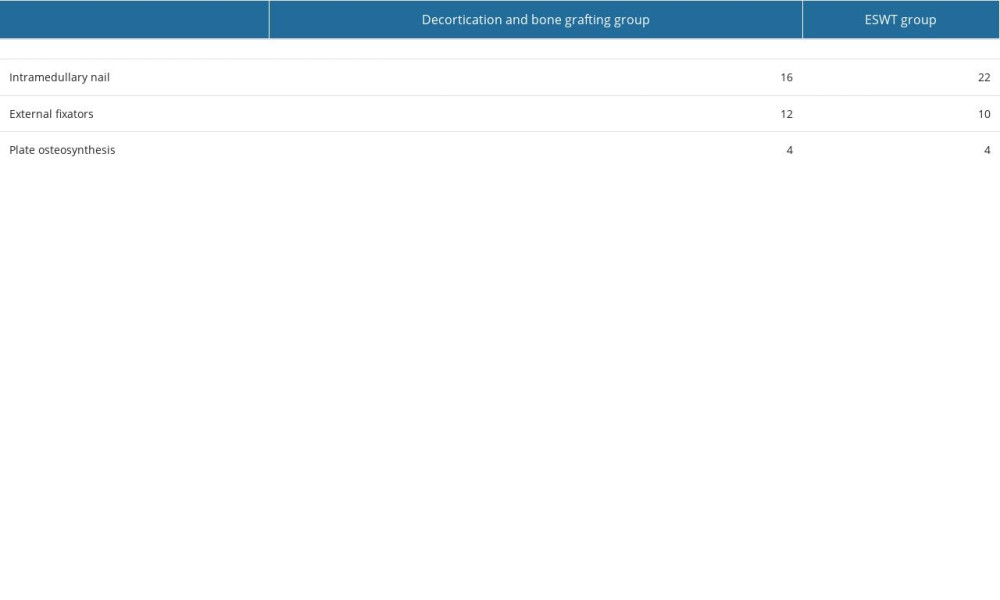 Table 4. The stabilization material used in the initial surgeries of the patients.
Table 4. The stabilization material used in the initial surgeries of the patients. Table 5. The etiologic causes of fractures.
Table 5. The etiologic causes of fractures. In Press
05 Mar 2024 : Clinical Research
Muscular Function Recovery from General Anesthesia in 132 Patients Undergoing Surgery with Acceleromyograph...Med Sci Monit In Press; DOI: 10.12659/MSM.942780
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








