15 July 2023: Clinical Research
Enhanced Rehabilitation Outcomes of Robotic-Assisted Gait Training with EksoNR Lower Extremity Exoskeleton in 19 Stroke Patients
Agnieszka Wiśniowska-SzurlejDOI: 10.12659/MSM.940511
Med Sci Monit 2023; 29:e940511
Abstract
BACKGROUND: Stroke is a leading cause of long-term disability, often resulting in impaired mobility and gait abnormalities, necessitating effective rehabilitation approaches. Robotic-assisted gait training (RAGT) offers precise control and intensive, task-specific training. The EksoNR exoskeleton shows potential in facilitating gait recovery. This study assesses the efficacy and tolerability of RAGT using EksoNR in the rehabilitation of 19 stroke patients.
MATERIAL AND METHODS: A prospective nonrandomized, observational study design was employed with a single group convenience sample. The study included 19 individuals post-stroke, who underwent a 4-week rehabilitation program. Baseline and post-rehabilitation assessments were conducted using selected International Classification of Functioning, Disability and Health (ICF) codes, gait exoskeleton parameters (number of steps, walking time, time of verticalization) obtained during the exoskeleton sessions, and the Timed Up and Go Test (TUG).
RESULTS: The study revealed statistically significant improvements in all analyzed ICF categories, except for D530 Toileting, indicating enhanced functioning. The most notable improvements in activity and participation were observed in the categories of D410 Changing basic body position (-0.84±0.60) and D450 Walking (-0.84±0.60). Additionally, gait analysis demonstrated significant enhancements in the number of steps (difference of 506.79±252.49), walking time (13.02±7.91), and time of verticalization (11.82±9.21) (p>0.001). The TUG test also showed a statistically significant improvement in mobility (p=0.005).
CONCLUSIONS: This study supports previous findings, demonstrating that RAGT using the EksoNR lower extremity exoskeleton improves gait and functional status in stroke patients, while being well tolerated. The results highlight the potential of this approach for improved rehabilitation outcomes.
Keywords: Exoskeleton Device, ICF05016, neurological rehabilitation, Physical Therapy Modalities, Humans, stroke rehabilitation, Prospective Studies, postural balance, Robotic Surgical Procedures, Time and Motion Studies, Stroke, Exercise Therapy, Treatment Outcome, Gait, Lower Extremity
Background
Stroke is one of the most common causes of disability and is the second most common cause of death in the world [1]. According to the Global Stroke Factsheet, over the last 17 years the risk of stroke over a whole lifetime has increased by 50% [2]. According to the World Stroke Organization (WSO), between 1990 and 2019, the incidence of strokes worldwide increased by 70%, resulting in a 143% increase in the number of years with disability as a result of stroke [3].
Deficits in patients after stroke are most often of a motor nature, related to mobility, gait, and balance [4,5]. Mobility deficits in patients after stroke are associated with an increased risk of falls and fall-related injuries, not only increasing the cost and time of treatment, but also causing a greater risk of death [6–8]. As has been shown in many scientific studies so far, limitations in motor functions may negatively affect functional efficiency in the performance of basic and complex activities of daily living, social participation, and the perception of overall quality of life [9,10]. According to the results of research conducted by Lord et al, 75% of patients after stroke consider independence in movement to be one of the most important factors determining independence in their own home after hospitalization [11]. According to Veerbeek et al, the ability to walk without orthopedic aids is a factor associated with the ability to regain ADL function within 3 months after a stroke incident [12]. According to reports from many scientific studies, the main goal of physiotherapy in patients after stroke should therefore be to strive to support their mobility in order to maintain or improve independence and autonomy in everyday functioning [13,14]. Therefore, a comprehensive and intensified rehabilitation program is of particular importance for creating sustainable changes in motor system networks and motor learning that underlie the re-education of gait in stroke patients [15].
Effective methods supporting the standard neuro-rehabilitation process in gait and mobility disorders in patients after stroke, based on the use of virtual reality, biofeedback, or assistive robotic devices, have been sought for several years [16,17]. The benefits of using robotic-assisted gait training (RAGT) in the re-education of gait in stroke patients have been described in many previous publications. As pointed out by Masiero et al, robots effectively improve traditional post-stroke physiotherapy, enabling multiple repetitions of movement in the same pattern and without signs of fatigue [18]. According to Poli et al, robotic systems used in gait training in stroke patients allow for a more complex multisensory stimulation of the patient than conventional physiotherapy. Thus, they enable the stimulation of non-walking people with a “real” sensomotor stimulus associated with gait activity [19]. In addition, using robotic systems, it is possible to measure individual kinematic parameters during walking, which allows a more objective assessment of the patient’s progress in therapy [20]. This is particularly important from the perspective of the reliability of the tools available to assess gait in stroke patients. As demonstrated in a review of the literature by Ferrarello et al, out of 5 tools dedicated to assessing gait in stroke patients – Gait Assessment and Intervention Tool (GAIT), Hemiplegic Gait Analysis Form (HGAF), New York Medical School Orthotic Gait Analysis (NYMSOGA), Rivermead Visual Gait Assessment (VGA), and Wisconsin Gait Scale (WGS) – only the GAIT scale was characterized by high reliability [21]. This confirms the need to implement additional parameters to assess the patient’s gait in everyday practice, which is now possible thanks to robotic systems.
Depending on the functional condition of the patient and the degree of motor deficits, static robots such as Lokomat or Gait Trainer and dynamic robots such as wearable exoskeletons or soft exoskeletons are available, which allow the patient a greater degree of independent movement [22]. The ExoNR exoskeleton (Ekso Bionics, San Rafael, CA, USA) is attached to the lower limbs on both sides, allowing automatic control of the mobility of the patient’s hip and knee joints. The device enables gait therapy according to 3 modes, which are selected depending on the degree of mobility deficits in the patient. The first of these, FirstStep, involves a fully external initiation of movement of the lower limbs. In the ProStep mode, steps are performed by transferring the body weight to one of the limbs, which initiates motion of the unloaded limb. In the ProStep Plus mode, the patient takes a step by himself, transferring their bodyweight not only to the side, but also to the front [23,24].
Gait therapy with the use of an exoskeleton supports the achievement of a gait pattern similar to the physiological one in terms of time and spatial parameters. It also supports the control of posture in walking with the patient’s conscious involvement [25]. Molteni et al showed beneficial changes in gait function after 12 sessions of gait training using an exoskeleton in patients after a stroke [26]. In the Longatelli et al study, in stroke patients, activation of proximal muscles of the lower limbs was observed after 20 sessions of gait training using an exoskeleton [27]. As Chen et al emphasized, the benefits of exoskeleton training, in addition to supporting gait re-education, also contribute to mitigating the secondary consequences of immobilization [28]. Beneficial effects of gait therapy with the use of the EksoNR exoskeleton (Ekso Bionics, San Rafael, CA, USA) have also been demonstrated in studies by Zhu et al, Louie et al, and Infarinato et al [29–31].
As Geroin et al emphasized in their work, assessment of the effectiveness of any intervention using modern technologies should be carried out on the basis of the International Classification of Functioning, Disability and Health (ICF), which is the basis for assessing a patient’s individual resources and limitations. According to the authors, the assessment of the gait function of patients with neurological conditions should be supplemented with the aspect of activity and participation in order to assess the holistic impact of a given therapy on the patient’s functioning [32]. According to Ármannsdóttir et al, an approach to evaluating the effectiveness of exoskeleton technology, consistent with the ICF concept and focused on the user, is also very important from the perspective of engineers and clinicians working to improve this technology [33].
Despite the fact that there are reports in the literature on the effectiveness of using exoskeleton-assisted therapy to improve mobility and gait function in patients with neurological conditions, there are few studies that take into account the aspect of functioning in the ICF concept. Therefore, this study aimed to describe and evaluate the method of robotic-assisted gait training – RAGT – in the rehabilitation of 19 patients following stroke using the EksoNR lower-extremity exoskeleton.
Material and Methods
ETHICS:
The study was approved by the Bioethics Committee of the University of Rzeszów (No. 2022/059). In accordance with the Declaration of Helsinki, all subjects were informed about the purpose and procedure of the study and gave their informed consent to participate in the study.
STUDY DESIGN AND PARTICIPANTS:
A prospective, nonrandomized, observational study design with 2 repeated measures (pre- and post-intervention) was performed using a single-group convenience sample.
The study included people after stroke. Patients were qualified on the basis of the diagnosis of the underlying disease from post-hospital medical records.
The inclusion criteria for participation in the study included: 1) 18 years and older, 2) after a stroke that took place not earlier than 1 year before enrolment in the study, 3) cognitive functioning status enabling the execution of commands and answering questions (the Abbreviated Mental Test Score, AMTS >6 points), 4) height from 1.6 m to 1.8 m, 5) body weight less than 100 kg, 6) ability to independently maintain a sitting position, 7) ability to independently transfer from a wheelchair, 8) physician’s consent for rehabilitation, 9) informed consent of the examined person to participate in the project. The exclusion criteria were: 1) second or subsequent stroke, 2) severe concomitant diseases (infections, diseases of the circulatory system, heart, lungs), 3) lower limb fracture in the last 2 years, 4) neurogenic periarticular ossifications of the lower limbs, 5) pressure sores or wounds within the lower limbs, 6) spasticity >4 on the Ashworth scale, 7) significant limitations in the range of motion and pain (of the hip, knee or ankle joints) that make it difficult to move.
SETTING:
The study was carried out at the Regional Rehabilitation Center.
QUALIFICATION PROCEDURE FOR INTERVENTION:
After patients were assessed according to the inclusion and exclusion criteria, a specialist physician conducted qualifications for the rehabilitation program.
The qualification of patients for therapy using the Ekso NR exoskeleton was performed by a certified physiotherapist who operated the equipment.
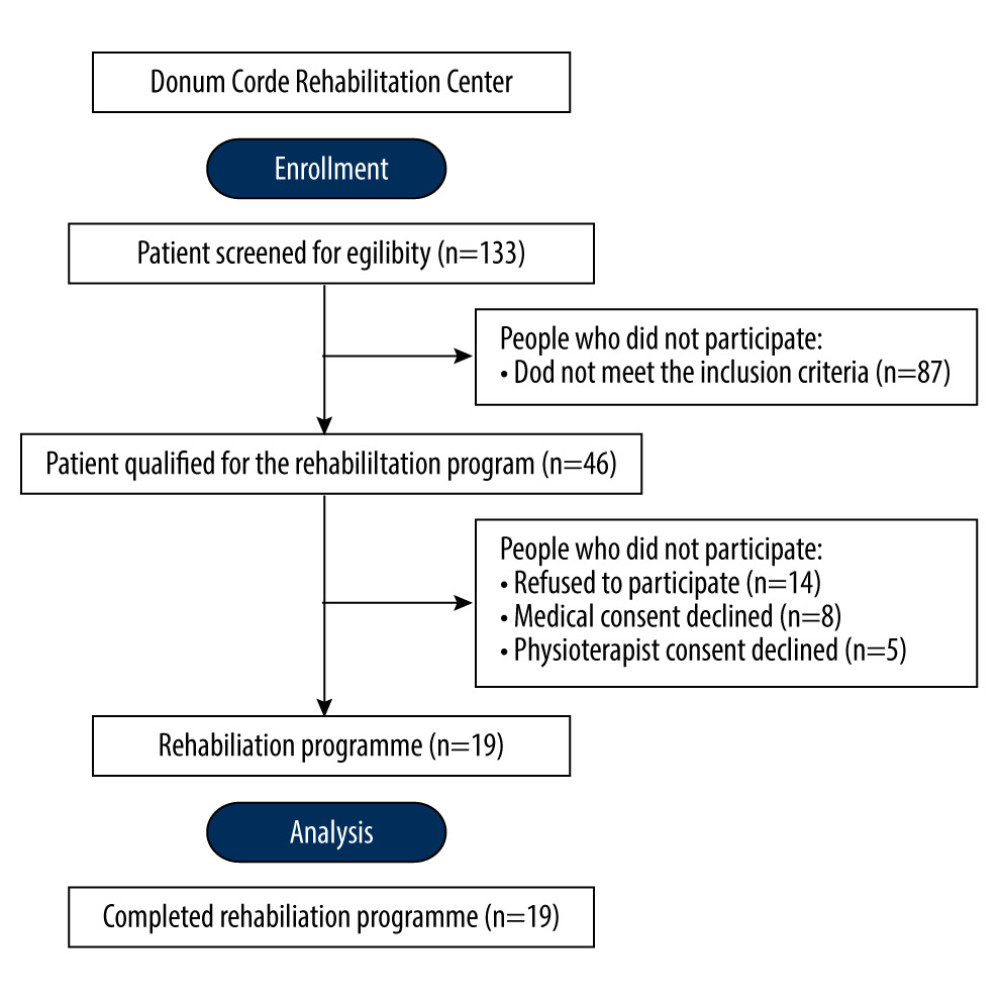
All patients who were admitted to the Donum Corde Rehabilitation Center from January to October 2022 and met the inclusion criteria were eligible for the rehabilitation program; 46 patients were qualified for the program, of which 19 patients ultimately underwent intervention (Figure 1). The preliminary nature of the project influenced the decision to create 1 research group and provide support to all eligible patients submitted to the project.
DATA COLLECTION:
Using an interview questionnaire, information concerning socioeconomic variables was collected: age, gender, and place of residence. An abbreviated version of the AMTS questionnaire was used to assess cognitive status [34].
FUNCTIONING AND DISABILITY ASSESSMENT:
The functional status assessment was carried out using the ICF classification. To assess the area related to the activity and participation of the subjects, 10 ICF of the following categories were selected for the study: D410 Changing basic body position, D415 Maintaining a body position, D420 Transferring oneself, D445 Hand and arm use, D450 Walking, D510 Washing oneself, D530 Toileting, D540 Dressing, D550 Eating. According to the ICF, the categories studied are described with the prefix “D”. In accordance with the principles of applying the ICF qualifications, each category was assessed using qualifiers defining the severity of the patient’s health problem according to the following scale: xxx.0 NO; xxx.1 MILD; xxx.2 MODERATE; xxx.3 SEVERE; xxx.4 COMPLETE [35].
ASSESSMENT OF THE PROGRESS IN THE ABILITY TO WALK WITH THE EKSO NR EXOSKELETON:
In the study group, the functions monitored by the Ekso NR exoskeleton (Ekso Bionics, Inc. Richmond, CA, USA) were measured during the therapy. The number of steps, walking time, and verticalization time during the first and last therapeutic sessions with the use of the exoskeleton were used for the analysis. The parameters obtained from the measurements indicated progression in the ability to walk with the exoskeleton. Each of the measurement and training sessions lasted 50 min [36] (Table 1).
MOBILITY ASSESSMENT:
Mobility was assessed using the Timed Up and Go (TUG) test. The TUG test was performed as follows: the participant stood up (from a sitting position on a chair), walked a distance of 3 m, turned around (180°), walked the 3 m back to the starting position, and resumed the sitting position. The final result was the average time of 3 attempts [37].
REHABILITATION PROGRAM:
The rehabilitation program was performed for 4 weeks and consisted of the following elements: 100 minutes a day of individual physiotherapy, 50 minutes a day of verticalization from Monday to Friday, 5 days a week, and a 50-minute gait training session using the Ekso NR exoskeleton 3 times a week (Monday, Wednesday, and Friday).
Individual physiotherapy included the normalization of muscle tone, stretching exercises for the upper and lower body, facilitating support on the upper and lower limbs on the paretic side, trunk stabilization exercises in low and high positions, static or dynamic balance training in a standing or sitting position, and gait re-education.
Verticalization was performed with the use of assistive devices (SMART dynamic standing frame). During verticalization, the physiotherapists supervised the correct stabilization of the trunk and pelvis, as well as the evenness of the load on the lower limbs. During the session, the parameters of arterial blood pressure, pulse, and saturation were monitored.
EXOSKELETON SESSION:
The gait training was conducted using the Ekso NR exoskeleton (Ekso Bionics, Inc. Richmond, CA, USA). EksoNR is a robotic exoskeleton specifically designed to be used in a rehabilitation setting to support neuro-rehab patients so they can walk out of the device and back into their communities. Before starting the gait training, each subject underwent a thorough diagnostic process to individually adjust the bionic skeleton (hip width, hip abduction, length of orthoses for the shin and thigh, stiffness and resting angle of the ankle joint). The next stage was to fix the subject in the exoskeleton using a system of pelottes, belts, and harnesses. After entering the patient’s data into the device’s software, the physiotherapist selected the optimal training parameters (step length, step height, transfer time, hip and knee flexion, lateral and frontal tilt). Training with the use of the exoskeleton began with the transfer of the patient to a chair on which the previously fitted exoskeleton (with properly adjusted lengths for the thighs and lower legs) was located. The device was then attached to the patient’s body and a change in the body position, from sitting to standing, was carried out. After assuming the vertical position, gait training began. It took place on a flat surface, along a corridor in the Rehabilitation Center. As the patient made progress during the training, the therapist updated the exoskeleton settings on an ongoing basis, so that the training was best suited to the subject’s current abilities. The following types of gait and activity were used during subsequent training sessions: First Step, Pro Step, and Pro Step Plus. Robotic Exoskeleton gait training with a physical therapist is shown in Figure 2.
Individual exercise programs were performed by qualified physiotherapists with a minimum of 3 years of experience in working with a neurological patient. Therapy using the exoskeleton was carried out by a certified physiotherapist with permission to operate the exoskeleton. The rehabilitation process was carried out under the supervision and with the consent of a specialist physician.
STATISTICAL ANALYSIS:
The obtained data were analyzed using Statistica (data analysis software system) version 13 from TIBCO Software Inc. (2017)
Results
PARTICIPANTS:
The study group consisted of 19 patients: 11 women and 8 men. The mean age in the study group was 44.10 years (SD=17.20). Most of the subjects lived in urban areas (68.42%). The highest levels of activity and participation limitations according to the ICF classification were found in the categories: D450 Walking (2.89 ±0.57), D420 Transferring oneself (2.42±0.69), and D410 Changing basic body position (2.37±0.90). The lowest level of disability was found in the D550 Eating category (1.68±1.45). Before the intervention, the average level of mobility in the study group expressed by the result of the Timed Up and Go test was 48.79±24.60s. The characteristics of the study group are shown in Table 2.
OUTCOME RESULTS:
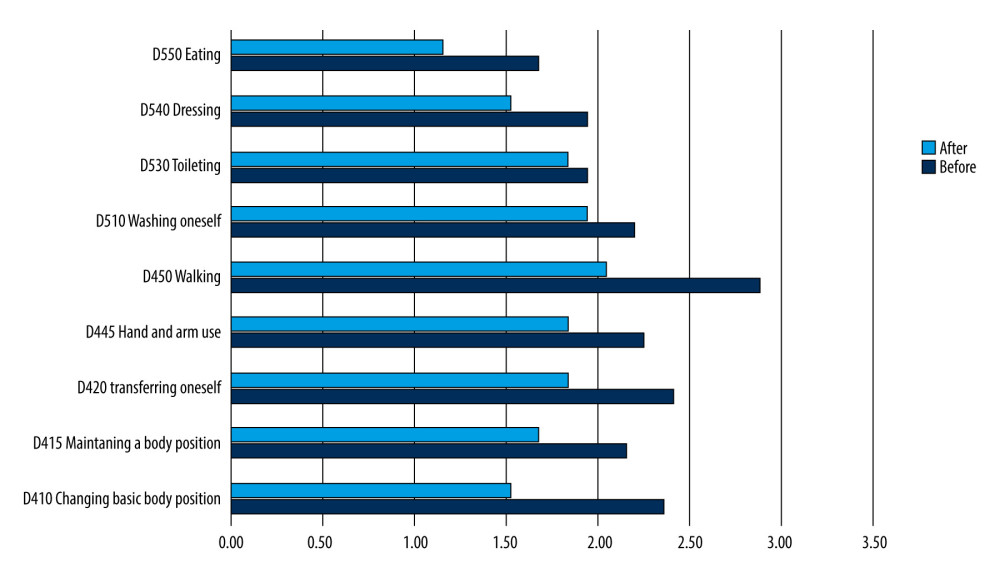
As a result of the rehabilitation program with the use of an exoskeleton, a statistically significant improvement in the level of functioning was found in all of the analyzed ICF categories, with the exception of D530 Toileting. The greatest difference in the assessment of disability after the completion of the physiotherapy program was shown in the categories: D410 Changing basic body position (−0.84±0.60) and D450 Walking (−0.84±0.60). The final study also showed a statistically significant improvement in the number of steps (difference 506.79±252.49), walking time (13.02±7.91), and time of verticalization 11.82±9.21). A statistically significant improvement in the mobility of the examined people was found, expressed in the result of the Timed Up and Go test (difference −10.32±14.59) (Table 3).
ICF EVALUATION DISPLAY:
To enable the comparability of the collected data, 10 ICF classification codes were selected for the assessment of activity and participation, which were numerically and graphically recorded. Figure 3 presents the data in the form of ICF qualifiers before and after the rehabilitation program. The ICF Evaluation Display contains visual presentations of the functional limitations of the persons included in the study.
Discussion
There have been recent developments in robotic-assisted methods for patient rehabilitation following acute neurological disability. This study aimed to describe and evaluate the method of robotic-assisted gait training – RAGT – in the rehabilitation of 19 patients following stroke using the EksoNR lower-extremity exoskeleton.
In our own study, a statistically significant improvement in mobility was demonstrated, expressed in the time of performing the TUG test with the use of an exoskeleton after the end of the rehabilitation program. Naves et al, in retrospective studies, analyzed data from stroke patients who underwent rehabilitation with RAGT for improved gait function. The results showed that the use of RAGT may improve clinically relevant aspects of walking function, as assessed TUG [38]. Loro et al, in a systematic review and meta-analysis of 18 randomized clinical trials, which confirmed the efficacy of RAGT, as well as the effects of traditional therapy, also suggest a combination of both therapies as the most clinically and functionally effective [39]. Some reports also confirm the positive impact of training with the use of an exoskeleton on improving the mobility of patients after a stroke [18,40].
Individuals with stroke have significant ambulatory deficits resulting in reduced mobility and activities of daily living. Our study also showed a statistically significant increase in the number of steps performed during a single walking session using an exoskeleton, as well as an increase in the time of maintaining an upright position in the study group. Karunakaran et al focused their study on improving movement ability with RAGT among stroke patients. The results suggest that the use of the exoskeleton increases the patient’s mobility and distance during the session 2-fold as compared to conventional physiotherapy. Improvement of functional gait measurements showed a positive correlation with the increase in the number of gait training sessions RE [36]. Similarly, Nolan et al noted in their research that robotic exoskeletons (RE) training in post-stroke rehabilitation can provide increased dosing of gain training [41]. Tomida et al also showed that gait training with RAGT for 4 weeks improved the walking ability of patients with subacute stroke. RAGT contributes to early improvement in walking ability possibly by assisting knee flexion during the swing phase on the paralyzed side, thereby increasing training volume, and by a finely adjustable stance/swing assist mechanism for the paralyzed limb, which optimizes the training difficulty [42]. Studies by Longatelli et al indicate the importance of restoring a symmetrical gait pattern; they assessed the muscular activation profiles of patients by comparing the impact of therapy using the exoskeleton with the results of conventional therapy. Both interventions improved the gait of post-stroke patients, while only those in the exoskeleton group improved their gait pattern to a more regular one. The achieved improvement in functional gait became a motivation to systematic exercises [27]. The results of our studies are consistent with the results of Zhu et al, who showed that the use of RAGT affects the improvement of gait pattern and neuromuscular coordination as well as increasing the distance travelled among people after a stroke [29].
The most important observations from this study were that the physiotherapy program supported by exoskeleton gait training had a beneficial effect on improving the activity and participation of the subjects, defined according to selected ICF categories. Similar results were obtained by Rojek et al, who showed that training with the use of an exoskeleton is associated with the improvement of functional efficiency in a greater number of everyday activities than in the case of using only conventional physiotherapy [43]. Morone et al showed that robot therapy combined with conventional therapy may be more effective than conventional therapy alone in patients with greater motor impairment during stationary post-stroke rehabilitation [44]. Poli et al also noted that gait training with RAGT in stroke patients has an effect on a more complex multisensory stimulation of the patient than in conventional therapy [19]. Lexell and Brogårdh emphasized that the work on the development of the ICF classification in recent decades has enabled it to be used as a standard framework in the neurorehabilitation process, for medical documentation, creating rehabilitation plans and objective measurement of results [45]. According to Mayr et al, improving locomotion and independence in activities of daily living are the most important goals of physiotherapy for patients with neurological conditions. The authors emphasized that the number of studies assessing the impact of physiotherapy with robot-assisted devices on functional status is still insufficient [46].
Our own study showed that the physiotherapy program supported by gait training with the use of an exoskeleton had the greatest impact on the improvement of the functional status in the ICF categories corresponding to the change of body position and walking. Some of the reports indicate that this may be related to the more symmetrical activation of the lower-limb muscles induced by the exoskeleton, which is comparable to the physiological gait and may stimulate the re-education of the correct gait pattern to a greater extent [47,48].
The improvement of functional efficiency in terms of changes in position may be related to the improvement of balance in patients undergoing therapy with the use of an exoskeleton, as demonstrated in some previous studies. It should be emphasized, however, that the assessment of balance in most of the studies conducted so far has been carried out using the Berg Balance Scale, which suggests the need to confirm the obtained results in balance studies on a stabilometric platform [49].
In the conducted exoskeleton-assisted rehabilitation, an improvement in activity, participation and mobility in people after stroke was noticed. However, the study also has some limitations. The first of these is the small size of the group studied. As the study was preliminary, the justification for the size of the group was based on the feasibility of a pilot study. The study participants were all persons meeting the inclusion criteria: 1) 18 years and older, 2) after a stroke or ruptured aneurysm incident that took place not earlier than 1 year before enrolment in the study, 3) cognitive functioning status enabling the execution of commands and answering questions (the Abbreviated Mental Test Score, AMTS >6 points), 4) height from 1.6 m to 1.8 m, 5) body weight less than 100 kg, 6) ability to independently maintain a sitting position, 7) ability to independently transfer from a wheelchair, 8) physician’s consent for rehabilitation, 9) informed consent of the examined person to participate in the project), who were given rehabilitation therapy in the Rehabilitation Center during the 10 months of the project. Another limitation of this study is the absence of a control group that would allow a comparative analysis. This limitation is due to the fact that all patients of the rehabilitation center receive treatment, therefore we were not able to select a control group of people not affected by intervention. However, in order to partially compensate for this limitation, we are in the process of performing the third follow-up, 2 months after discharge from the rehabilitation center, which will allow us to assess the long-term effects of post-hospital rehabilitation.
Conclusions
Conventional neurorehabilitation combined with gait re-education with the use of an exoskeleton may improve activities, participation, and mobility in patients with neurological conditions. The findings from this study support those of previous studies and showed that RAGT using the EksoNR lower-extremity exoskeleton improved patient gait and was well tolerated by patients following stroke. However, there is a need for further research on a larger group of people and with the use of a control group.
References
1. Katan M, Luft A, Global burden of stroke: Semin Neurol, 2018; 38(2); 208-11
2. Feigin VL, Brainin M, Norrving B, World Stroke Organization (WSO): Global stroke fact sheet 2022: Int J Stroke, 2022; 17(1); 18-29
3. World Stroke Organization (WSO): Global stroke fact sheet 2022, 2022, Geneva, World Stroke Organization (cited 2023, 18 April). Available from: https://www.world-stroke.org/assets/downloads/WSO_Global_Stroke_Fact_Sheet.pdf
4. Whitiana GD, Vitriana V, Cahyani A, Level of activity daily living in post stroke patients: Althea Med J, 2017; 4(2); 261-66
5. Hatem SM, Saussez G, Della Faille M, Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery: Front Hum Neurosci, 2016; 10; 442
6. Homann B, Plaschg A, Grundner M, The impact of neurological disorders on the risk for falls in the community dwelling elderly: A case-controlled study: BMJ Open, 2013; 3(11); e003367
7. Stevens JA, Lee R, The potential to reduce falls and avert costs by clinically managing fall risk: Am J Prev Med, 2018; 55(3); 290-97
8. Heshmatollah A, Darweesh SKL, Dommershuijsen LJ, Quantitative gait impairments in patients with stroke or transient ischemic attack: a population-based approach: Stroke, 2020; 51(8); 2464-71
9. Wuehr M, Huppert A, Schenkel F, Independent domains of daily mobility in patients with neurological gait disorders: J Neurol, 2020; 267(1); 292-300
10. Jung H, Tanaka S, Iwamoto Y, Yamasaki M, Tanaka R, Relationship between mobility-related activities of daily living and health-related quality of life among healthy older adults: A cross-sectional study using structural equation modeling: Gerontol Geriatr Med, 2021; 7; 23337214211013166
11. Lord SE, McPherson K, McNaughton HK, Community ambulation after stroke: how important and obtainable is it and what measures appear predictive?: Arch Phys Med Rehabil, 2004; 85(2); 234-39
12. Veerbeek JM, Kwakkel G, van Wegen EE, Early prediction of outcome of activities of daily living after stroke: A systematic review: Stroke, 2011; 42(5); 1482-88
13. Hassett L, van den Berg M, Lindley RI, Digitally enabled aged care and neurological rehabilitation to enhance outcomes with Activity and MObility UsiNg Technology (AMOUNT) in Australia: A randomised controlled trial: PLoS Med, 2020; 17(2); e1003029
14. Mang CS, Peters S, Advancing motor rehabilitation for adults with chronic neurological conditions through increased involvement of kinesiologists: A perspective review: BMC Sports Sci Med Rehabil, 2021; 13(1); 132
15. Kleim JA, Jones TA, Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage: J Speech Lang Hear Res, 2008; 51(1); S225-39
16. Rodriguez J, Del-Valle-Soto C, Gonzalez-Sanchez J, Affective states and virtual reality to improve gait rehabilitation: A preliminary study: Int J Environ Res Public Health, 2022; 19(15); 9523
17. Payedimarri AB, Ratti M, Rescinito R, Effectiveness of platform-based robot-assisted rehabilitation for musculoskeletal or neurologic injuries: A systematic review: Bioengineering (Basel), 2022; 9(4); 129
18. Masiero S, Poli P, Rosati G, The value of robotic systems in stroke rehabilitation: Expert Rev Med Devices, 2014; 11(2); 187-98
19. Poli P, Morone G, Rosati G, Masiero S, Robotic technologies and rehabilitation: New tools for stroke patients’ therapy: Biomed Res Int, 2013; 2013; 153872
20. Warutkar V, Dadgal R, Mangulkar UR, Use of robotics in gait rehabilitation following stroke: A review: Cureus, 2022; 14(11); e31075
21. Ferrarello F, Bianchi VA, Baccini M, Tools for observational gait analysis in patients with stroke: A systematic review: Phys Ther, 2013; 93(12); 1673-85
22. Morone G, Paolucci S, Cherubini A, Robot-assisted gait training for stroke patients: Current state of the art and perspectives of robotics: Neuropsychiatr Dis Treat, 2017; 13; 1303-11
23. : Ekso Bionics (cited 2023, 18 April) Available from: https://eksobionics.com
24. : Egzoszkielet EKSO GT/NR (cited 2023, 16 April). Available from: [in Polish]www.ekso.technomex.pl
25. Vaughan-Graham J, Brooks D, Rose L, Exoskeleton use in post-stroke gait rehabilitation: A qualitative study of the perspectives of persons post-stroke and physiotherapists: J Neuroeng Rehabil, 2020; 17(1); 123
26. Molteni F, Gasperini G, Gaffuri M, Wearable robotic exoskeleton for overground gait training in sub-acute and chronic hemiparetic stroke patients: Preliminary results: Eur J Phys Rehabil Med, 2017; 53(5); 676-84
27. Longatelli V, Pedrocchi A, Guanziroli E, Robotic exoskeleton gait training in stroke: An electromyography-based evaluation: Front Neurorobot, 2021; 15; 733738
28. Chen G, Chan CK, Guo Z, Yu H, A review of lower extremity assistive robotic exoskeletons in rehabilitation therapy: Crit Rev Biomed Eng, 2013; 41(4–5); 343-63
29. Zhu F, Kern M, Fowkes E, Effects of an exoskeleton-assisted gait training on post-stroke lower-limb muscle coordination: J Neural Eng, 2021; 18(4); abf0d5
30. Louie DR, Mortenson WB, Durocher M, Efficacy of an exoskeleton-based physical therapy program for non-ambulatory patients during subacute stroke rehabilitation: A randomized controlled trial: J Neuroeng Rehabil, 2021; 18(1); 149
31. Infarinato F, Romano P, Goffredo M, Functional gait recovery after a combination of conventional therapy and overground robot-assisted gait training is not associated with significant changes in muscle activation pattern: An EMG preliminary study on subjects subacute post stroke: Brain Sci, 2021; 11(4); 448
32. Geroin C, Mazzoleni S, Smania NItalian Robotic Neurorehabilitation Research Group, Systematic review of outcome measures of walking training using electromechanical and robotic devices in patients with stroke: J Rehabil Med, 2013; 45(10); 987-96
33. Ármannsdóttir AL, Beckerle P, Moreno JC, Assessing the involvement of users during development of lower limb wearable robotic exoskeletons: A survey study: Hum Factors, 2020; 62(3); 351-64
34. Piotrowicz K, Romanik W, Skalska A, The comparison of the 1972 Hodkinson’s Abbreviated Mental Test Score (AMTS) and its variants in screening for cognitive impairment: Aging Clin Exp Res, 2019; 31(4); 561-66
35. World Health Organization (WHO): World Health Organization: International Classification of Functioning, Disability and Health (ICF), 2001, Geneva, World Health Organization
36. Karunakaran KK, Gute S, Ames GR, Effect of robotic exoskeleton gait training during acute stroke on functional ambulation: Neurorehabilitation, 2021; 48(4); 493-503
37. Christopher A, Kraft E, Olenick H, The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review: Disabil Rehabil, 2021; 43(13); 1799-813
38. Neves MVM, Furlan L, Fregni F, Robotic-Assisted Gait Training (RAGT) in stroke rehabilitation: A pilot study: Arch Rehabil Res Clin Transl, 2023; 5(1); 100255
39. Loro A, Borg MB, Battaglia M, Balance rehabilitation through robot-assisted gait training in post-stroke patients: A systematic review and meta-analysis: Brain Sci, 2023; 13(1); 92
40. Louie DR, Eng JJ, Powered robotic exoskeletons in post-stroke rehabilitation of gait: A scoping review: J Neuroeng Rehabil, 2016; 13(1); 53
41. Nolan KJ, Karunakaran KK, Chervin K, Robotic exoskeleton gait training during acute stroke inpatient rehabilitation: Front Neurorobot, 2020; 14; 581815
42. Tomida K, Sonoda S, Hirano S, Randomized controlled trial of gait training using Gait Exercise Assist Robot (GEAR) in stroke patients with hemiplegia: J Stroke Cerebrovasc Dis, 2019; 28(9); 2421-28
43. Rojek A, Mika A, Oleksy Ł, Effects of exoskeleton gait training on balance, load distribution, and functional status in stroke: A randomized controlled trial: Front Neurol, 2020; 10; 1344
44. Morone G, Bragoni M, Iosa M, Who may benefit from robotic-assisted gait training? A randomized clinical trial in patients with subacute stroke: Neurorehabil Neural Repair, 2011; 25(7); 636-44
45. Lexell J, Brogårdh C, The use of ICF in the neurorehabilitation process: Neurorehabilitation, 2015; 26(1); 5-9
46. Mayr A, Kofler M, Quirbach E, Prospective, blinded, randomized crossover study of gait rehabilitation in stroke patients using the Lokomat gait orthosis: Neurorehabil Neural Repair, 2007; 21(4); 307-14
47. Coenen P, van Werven G, van Nunen MP, Robot-assisted walking vs overground walking in stroke patients: An evaluation of muscle activity: J Rehabil Med, 2012; 44(4); 331-37
48. Husemann B, Müller F, Krewer C, Effects of locomotion training with assistance of a robot-driven gait orthosis in hemiparetic patients after stroke: A randomized controlled pilot study: Stroke, 2007; 38(2); 349-54
49. Hornby TG, Campbell DD, Kahn JH, Enhanced gait-related improvements after therapist- versus robotic-assisted locomotor training in subjects with chronic stroke: A randomized controlled study: Stroke, 2008; 39(6); 1786-92
Figures
Tables
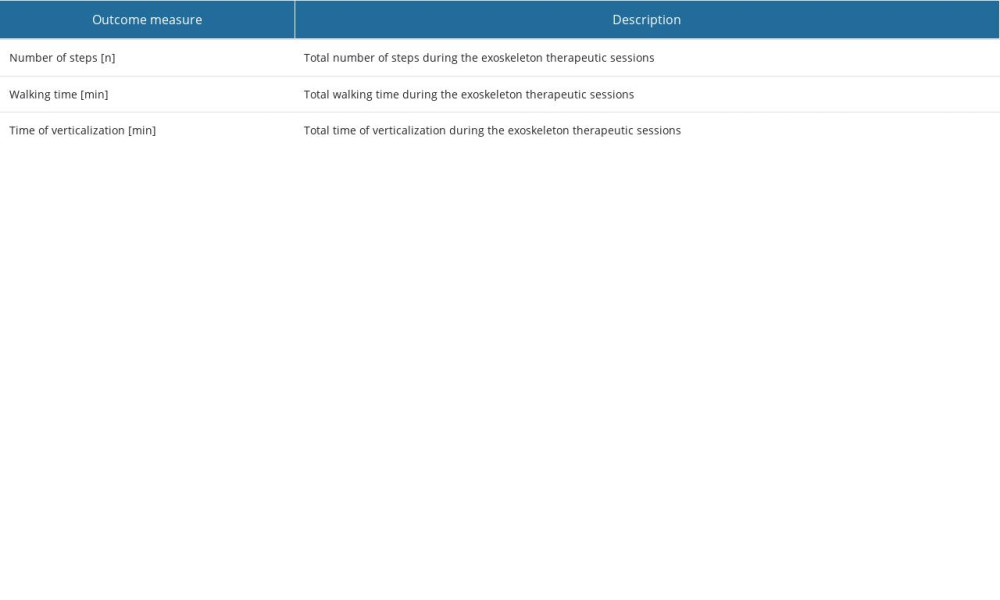 Table 1. Exoskeleton outcome measures.
Table 1. Exoskeleton outcome measures.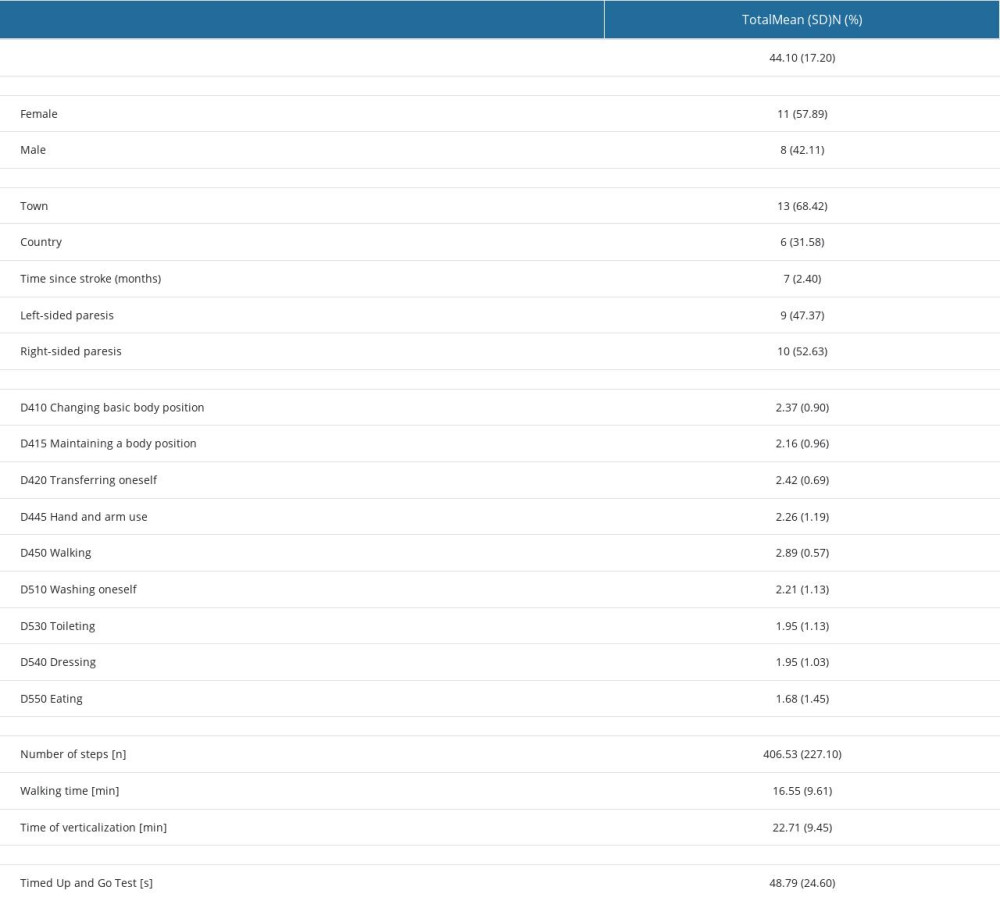 Table 2. Participant characteristics (n=19).
Table 2. Participant characteristics (n=19).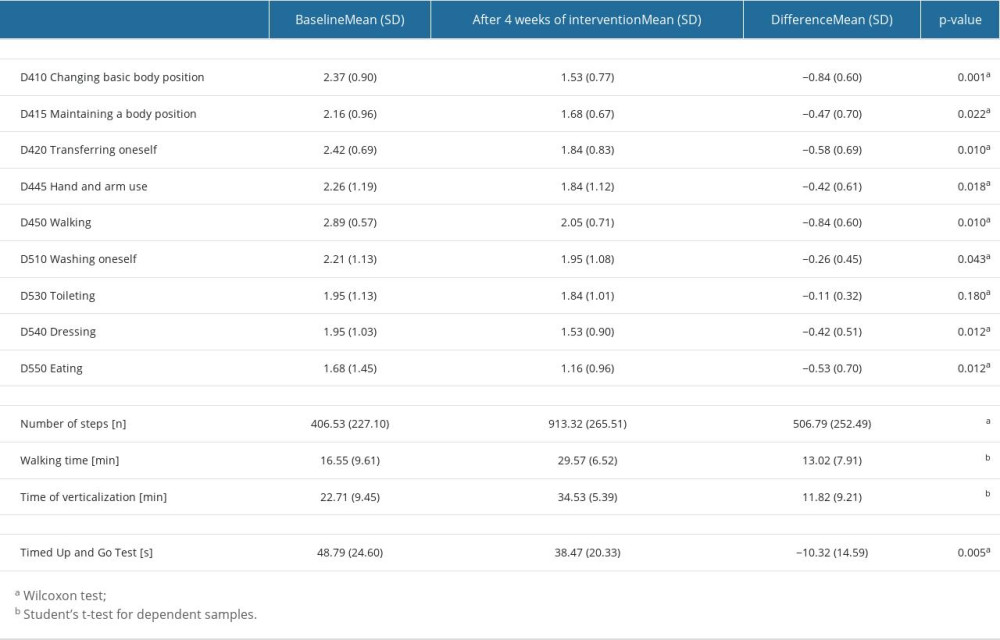 Table 3. The effects of a physiotherapy program with the use of an exoskeleton on the functional efficiency and mobility of people with neurological conditions (n=19).
Table 3. The effects of a physiotherapy program with the use of an exoskeleton on the functional efficiency and mobility of people with neurological conditions (n=19).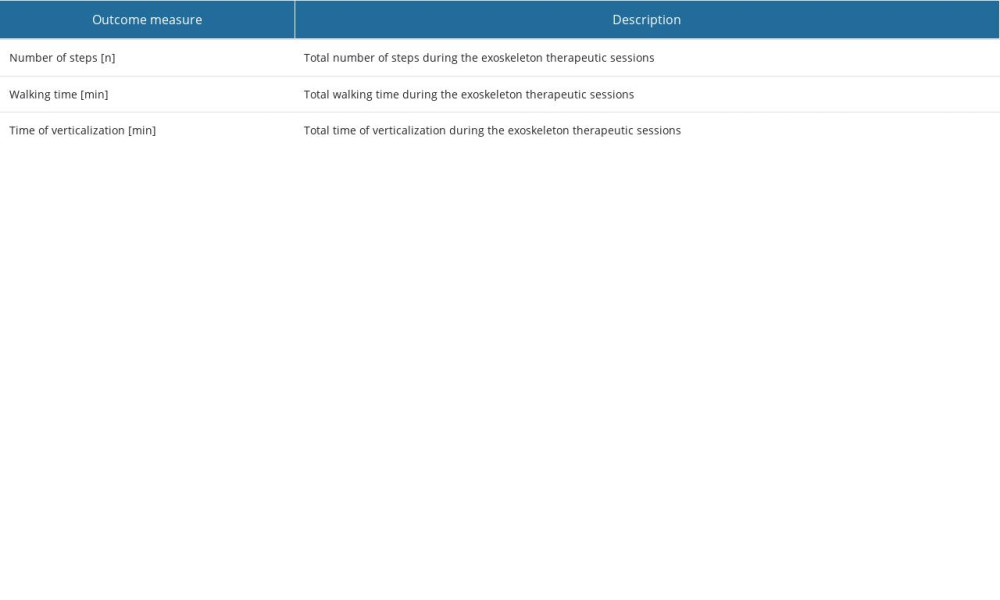 Table 1. Exoskeleton outcome measures.
Table 1. Exoskeleton outcome measures.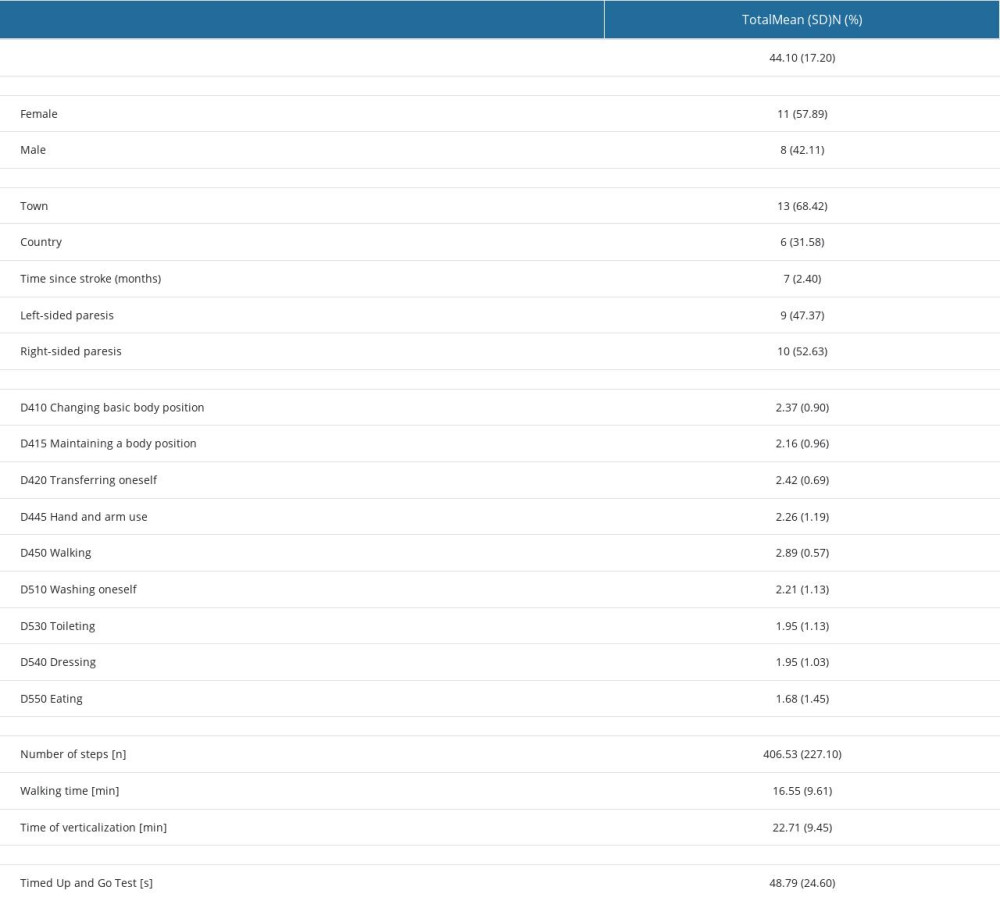 Table 2. Participant characteristics (n=19).
Table 2. Participant characteristics (n=19).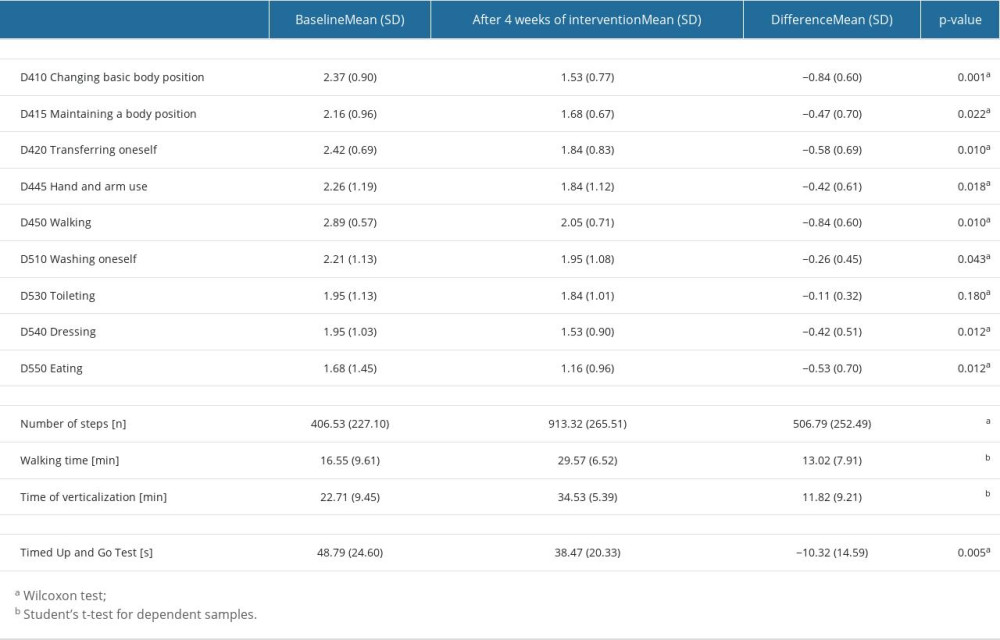 Table 3. The effects of a physiotherapy program with the use of an exoskeleton on the functional efficiency and mobility of people with neurological conditions (n=19).
Table 3. The effects of a physiotherapy program with the use of an exoskeleton on the functional efficiency and mobility of people with neurological conditions (n=19). In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952