18 September 2023: Clinical Research
Comparative Analysis of Physical Examination, CT Scan, and Three-Dimensional Gait Analysis in Evaluating Lower Extremity Torsion Deformities in Children with Cerebral Palsy
Sheng Jin1DEG, Chunxin Xu2EF, Haiqing Cai1D, Cen Chen2BC, Yangyang Lu2BC, Zhigang Wang1A*, Min Shen2ADOI: 10.12659/MSM.940948
Med Sci Monit 2023; 29:e940948
Abstract
BACKGROUND: The aim of this study was to analyze the correlation and the accuracy of lower-extremity torsion deformities measured by physical examination, CT scan, and three-dimensional gait analysis in children with CP.
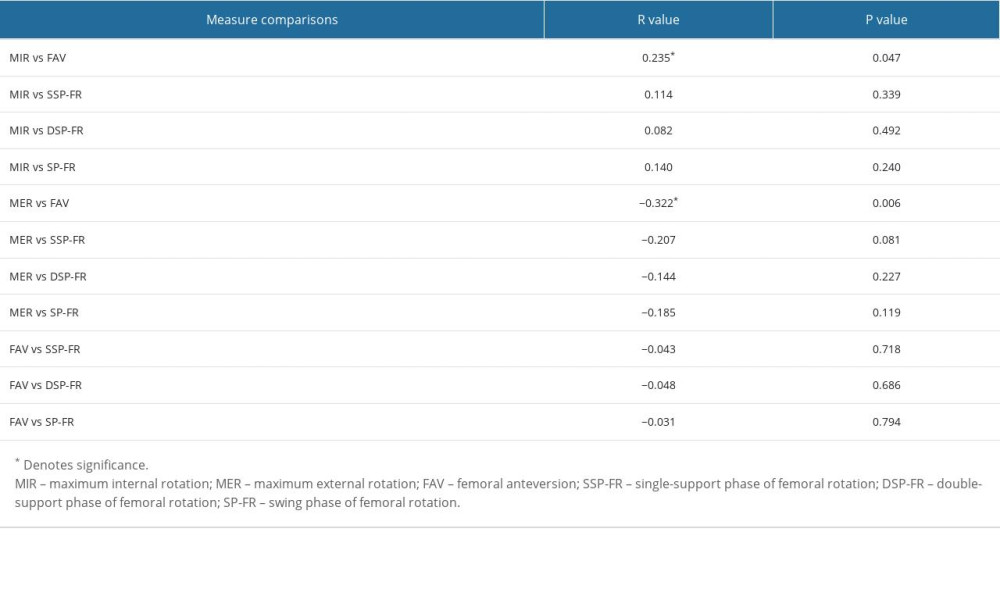
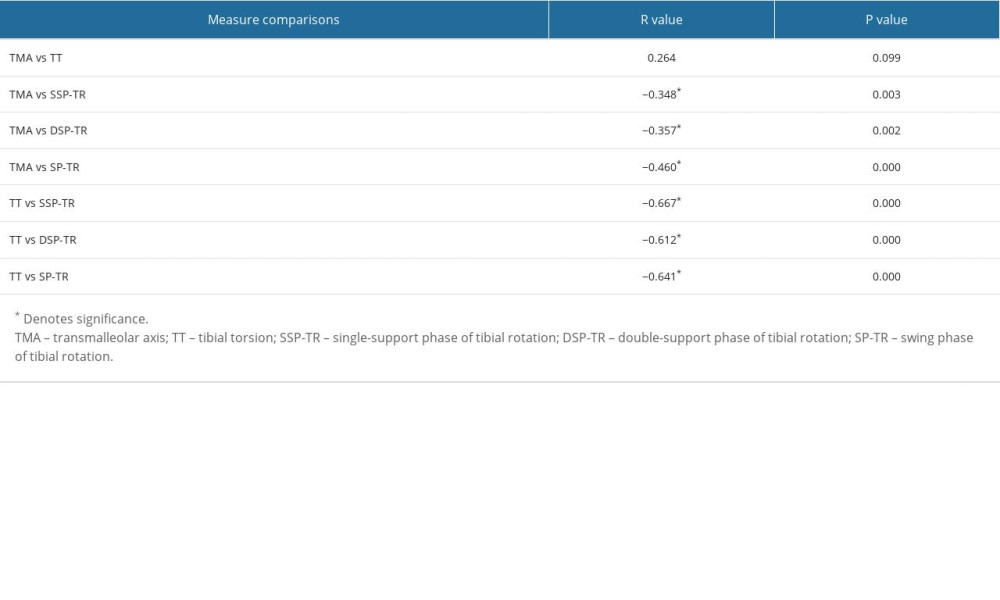
MATERIAL AND METHODS: The study group included 72 children with CP with lower-extremity torsion deformities. All subjects were assessed by: 1. physical examination: maximum internal rotation (MIR), maximum external rotation (MER) for hip joint torsion, and transmalleolar axis (TMA) for tibial torsion; 2. CT scanning: femoral anteversion (FAV) and tibial torsion (TT); 3. three-dimensional gait analysis kinematic parameters: single-support phase of femoral rotation, double-support phase of femoral rotation, swing phase of femoral rotation and single-support phase of tibial rotation, double-support phase of tibial rotation, and swing phase of tibial rotation. Statistical analysis was performed using the Pearson correlation test. A significance level of P<0.05 was set.
RESULTS: In femurs, MIR and MER were correlated with FAV, and the correlation of MER was higher, while physical examination and FAV were not correlated with any kinematic data in gait analysis. In tibias, there was no correlation between TMA and TT, but both TMA and TT were correlated with the gait analysis kinematic data, and the correlation of TT was higher. TMA was more correlated with tibial rotation during swing phase, while TT was more correlated with tibial rotation in single-support phase.
CONCLUSIONS: Three-dimensional gait analysis can analyze the tibial rotation of children with cerebral palsy, which is highly correlated with CT and physical examination. However, femoral rotation was not associated with CT and physical examination.
Keywords: Cerebral Palsy, gait analysis, Lower Extremity, Torsion Abnormality, Child, Humans, Physical Examination, Tomography, X-Ray Computed
Background
Torsion deformities of the lower extremities are very common in children with cerebral palsy (CP), which are manifested as in-toeing or out-toeing gait pattern. The prevalence of in-toeing gait is higher than that of out-toeing gait. In patients with CP, the incidence of in-toeing gait pattern was reported to be 64%, and was mainly caused by increased femoral anteversion and internal tibial torsion [1], while out-toeing gait was more often related to femoral retroversion, external tibial torsion, and foot deformity such as pes planovalgus [2].
Derotation osteotomy surgery of the femur or tibia is considered an essential treatment for the severe rotation deformity of the lower extremities. It is important to accurately evaluate the derotation angle before the surgery. At present, multiple methods are available to analyze the torsion degree of the lower extremities, including physical examination, CT or MRI imaging, and three-dimensional (3D) gait analysis. However, there have been controversies among some scholars regarding the accuracy of the results measured by different methods and whether there are correlations between them. Previous studies demonstrated that physical examination is often subjective and inaccurate, and may not be correlated to the femoral anteversion (FAV) and tibial torsion (TT) measured by CT [3–5]. Likewise, a study by Aktas found that CT measurements of FAV failed to accurately evaluate the hip rotation during the gait cycle [6].
3D gait analysis is also currently applied to assess torsion of the lower extremities. Previous studies reported that the correlation between physical examination and 3D gait analysis are in conflict due to different parameters analyzed [7–9]; therefore, dynamic data vary among different phases of the gait cycle [8].
These inconsistent results often make it difficult for orthopedic surgeons to determine the accuracy of derotation angle in the surgical process, which generates hardship in making clinical decisions and selecting surgical strategies. The purpose of this study was to analyze the correlation and the accuracy of lower-extremity torsion deformities measured by physical examination, CT, and 3D gait analysis in children with CP, in order to provide a precise and referential analysis for planning orthopedic surgery.
Material and Methods
PHYSICAL EXAMINATION:
We measured the maximum internal and maximum external rotation (MIR and MER, respectively) of the hip joint to reflect hip joint torsion, and the transmalleolar axis (TMA) was measured to reflect tibial torsion. All procedures were performed with patients in the prone position with the tested side’s hip completely extended, the knee flexed 90°, and the ankle in neutral position. Details of measurements were as follows: (1) MIR/MER: When the hip was in the maximum internal or external rotation position, by using a line perpendicular to the longitudinal axis of the thigh as a reference, the angle between this perpendicular line and the long axis of the shank was measured (Figure 1). The normal range of internal hip joint torsion is about 10–50 degrees, while external hip joint torsion is about 30–60 degrees; (2) TMA: We measured the angle between the line of the longitudinal axis of the thigh and the line perpendicular to the axis that connected the most prominent point of the medial and lateral malleolus [11] (Figure 2). The normal range of TMA is about 5–20 degrees. A negative value means internal rotation and a positive value means external rotation. All measurements were performed using a standard goniometer by the same trained orthopedics resident and the same gait lab staff.
CT IMAGING EXAMINATION:
We used the CT scanner (Toshiba 320-row CT Aquilion ONE) to measure the rotation of the lower limbs in each patient. Patients were in a supine position with bilateral patella upwards when the CT scan was performed. The pelvis and lower extremities were immobilized during scanning. Four transverse planes were selected for measurement. The first plane was the one containing the longest femoral neck axis on the transverse section. The second plane included both medial and lateral condyles of the distal femoral. The third plane was the proximal tibial condyle, while the fourth plane included the most prominent part of both the medial and lateral malleolus.
All CT scans data was measured by the same experienced radiographer. For measuring femoral torsion, the first angle was measured between a horizontal baseline and a long axis through the center of the femoral neck, while the second angle was measured between a horizontal baseline and a tangent to the posterior surface of the medial and lateral condyles of the distal femur [4] (Figure 3). Femoral anteversion (FAV) angle was calculated by subtraction of the first and second angle when they were in the same direction, and was calculated as the sum of the 2 angles if they were in the opposite direction [12]. The normal range of FAV is about 6–24 degrees [13]. For measuring tibial torsion (TT), the first angle was measured between a horizontal baseline and the tangent to the posterior aspects of the tibial plateau, while the second angle was measured between a horizontal baseline and the bimalleolar axis at the distal tibia [14] (Figure 4). The same as we calculated the FAV, TT was defined as difference between 2 angles if they were in the same direction. On the contrary, TT was the sum of 2 angles if they were in the opposite direction. The normal range of TT is about 24.5–38 degrees [13].
3D GAIT ANALYSIS:
Each patient was asked to walk barefoot, at a self-selected speed on an 8-m walking board. A minimum of 20 gait cycles were collected for each lower limb to evaluate consistency. Kinematics data were motion-captured using a 20-camera infrared motion analysis system (Santa Rosa, California, Motion Analysis Corp, USA). A modified Calibrated Anatomical System Technique (CAST) retroreflective marker set was placed on the subjects, including 38 markers. The placement of all patients’ markers was performed by the same examiner. Marker placements were as follows: left and right anterior superior iliac spine, left and right posterior superior iliac spine, lateral epicondyle of femur, medial epicondyle of femur, tibial trochanter, lateral malleolus, medial malleolus, Achilles insertion on calcaneus, dorsal margin of first metatarsal head, dorsal margin of second metatarsal head, and dorsal margin of fifth metatarsal head. The cortex served as an integrated software interface for data recording. According to the conventional gait models (CGM), Visual 3D was used for data processing, and a virtual coordinate system [15] was constructed for the pelvis, hip joint, knee joint, and ankle joint to ensure the accuracy of the analysis of rotation data.
The rotation of the hip joint was defined as the rotation of the rigid body on the horizontal plane constructed by the anterior superior iliac spine marker, the thigh wand marker, and the lateral knee marker. The rotation of the tibia was defined as the rotation of the rigid body on the horizontal plane constructed by the lateral knee marker, the shank wand marker, and the lateral ankle marker.
The rotation angles of the hip joint and tibia were considered in the different static (stance) and dynamic (swing) states. The stance also included the single-support phase and the double-support phase. Therefore, we recorded the average rotation angles of both the hip joint and tibia in the static standing phase, single-support phase, and swing phase, which included single-support phase of femoral rotation (SSP-FR), double-support phase of femoral rotation (DSP-FR), swing phase of femoral rotation (SP-FR) and single-support phase of tibial rotation (SSP-TR), double-support phase of tibial rotation (DSP-TR), swing phase of tibial rotation (SP-TR).
Pearson correlation testing was conducted for both the femoral group and the tibial group. The correlations between the torsion angles measured by physical examination, the CT scan, and the kinematic data obtained by 3D gait analysis were statistically evaluated in each group. SPSS for Windows (version 20.0, SPSS, Inc., Chicago, IL, USA) was used for determining the significance based on the validated
Results
The study included 72 patients from November 2020 to December 2021. The included subjects were all in line with the body mass index (BMI) standards of the corresponding age groups of the Chinese population. In each patient, physical examination, CT, and 3D gait analysis were completed sequentially within 1 week, and the results of each measurement were recorded separately. IBM SPSS 23.0 statistical software was used for analysis.
For the femur, physical examination showed the mean MIR was 53.0±4.5° (range, 25–89), and the mean MER was 46.1±9.0° (range, 18–80). CT scans showed the mean FAV was 33.9±11.7° (range, 12.7–55.9). 3D gait analysis showed the mean hip joint rotation angle was 3.2±2.8° (range, −27.5 to 52.5) in the static standing phase, 6.4±5.1° (range, −19.7 to 46.4) in the single-support phase and 5.1±2.9° (range, −17.7 to 46.9) in the swing phase. Both MIR and MER were correlated with FAV, and the correlation between MER and FAV was higher (MIR: R=0.235,
For tibias, the mean TMA was 14.9±3.5° (range, −14 to 41), the mean TT was 31.3±6.0° (range, 11.2 to 49.7), and the mean tibial rotation angle was −18.7±2.1° (range, −67.9 to 26.0) in the static standing phase, −14.9±4.2° (R=−57.9–26.1) in the single-support phase and −17.1±3.9° (range, −56.7 to 14.3) in the swing phase. There was no correlation between TMA and TT, but both TMA and TT were correlated with the kinematic data of tibial in gait analysis, and the correlation between TT and 3D gait analysis was higher (Table 2). The correlation between TMA and TT and kinematic data was analyzed. TMA was more correlated with tibial rotation during the swing phase (R=−0.460,
Discussion
As reported by Rodda [16], children with spastic diplegia based on sagittal plane gait patterns can be divided into 5 types: true equinus, jump gait, apparent equinus, crouch gait, and asymmetrical gait. Crouch gait is the most typical gait pattern of spastic diplegia and is part of the natural history of children with cerebral palsy. Children with crouch gait also usually have excessive adduction and pronation of the hip, excessive external torsion of the tibia, and pes valgoplanus deformity, which are typical manifestations of lever arm dysfunction in children with spastic diplegia. Our study results confirmed that children with spastic diplegia usually have rotation deformities of the lower extremities in horizontal plane, including excessive internal rotation of the hip, excessive internal or external torsion of the tibia, and excessive external and internal rotation of the foot relative to the tibia. We also confirmed that children with spastic diplegia usually have rotation deformities of the lower extremities in horizontal plane, including excessive internal rotation of the hip, excessive internal or external torsion of the tibia, and excessive external and internal rotation of the foot relative to the tibia. As reported by O’Sullivan [17], femoral rotation is associated with femoral anteversion, hip flexor tightness, imbalance of hip rotators, and hamstring and adductor tightness. As reported by Aiona [18], the tibial rotation arises from the complex interaction between the growing human skeleton and the abnormal forces applied by the spastic muscles acting across growth plates, joints, and connective tissue.
For children with cerebral palsy who have severe deformity in rotation of the lower extremities, derotation osteotomy of the femur or tibia can serve as an effective treatment to correct rotation deformity, improve gait, and improve energy efficiency in walking [19]. Accurate evaluation of rotation correction angle before surgery is the key to successful operation. Although this has been reported in the relevant literature before, and the conclusion is not unanimous, and the results in our study are different from those reported in these previous studies. In addition to analyzing the correlation between 3 different measurement methods of lower-limb rotation – physical examination, CT, and 3D gait analysis – we also compared the measurement data of physical examination and CT with the kinematic data measured in the single-support phase, double-support phase, and swing phase of 3D gait analysis. The correlations among the 3 measurement methods in different gait phases were further analyzed.
In terms of the femur, we found that both the maximum internal rotation (MIR) and the maximum external rotation (MER) on physical examination were correlated with the femoral anteversion (FAV) on CT; the correlation between MER and FAV was higher, while both MIR and MER were not correlated with the kinematic data of the hip joint in gait analysis. We believe that there are 2 reasons for this. First, iliopsoas and adductor spasm, hip abductor dysplasia, and poor acetabular coverage are the 3 main characteristics of the hip in children with spastic CP [20]. The traction of adductor spasticity can affect the development of the hip abductor muscle, and then reduce the stimulation of the greater trochanter; the development of the greater trochanter is affected, the formation of femoral neck anteversion is blocked, and the femoral neck appears valgus, resulting in the abnormality of femoral anteversion. At the same time, the adductor muscle spasm leads to adduction of the thigh, which makes the acetabulum not cover the femoral head adequately, and the acetabulum also suffers from dysplasia due to abnormal stress [21]. Therefore, on physical examination, there is a significant increase in MIR of the hip joint, and the majority of children with spastic cerebral palsy also have an increase in FAV, which leads to excessive internal rotation of the hip joint (internal rotation >80°). In children with spastic CP at a young age, because the musculoskeletal ligaments are not yet mature and the joint ligaments still have some flexibility, the MER of the hip joint may not be abnormal. Gait abnormalities in children with CP can affect movement at the hip, knee, and ankle, and across multiple joints. Spasticity of the hip adductors and flexors in children with CP, accompanied by weakness of the hip abductors and hip extensors, results in abnormal hip rotation [22]. Second, in each gait cycle, both femurs have an internal rotation radian and the same external rotation radian. During the initial landing, the bone structures of the pelvis and thigh are fixed, indicating a neutral position of the lower limbs. The peak internal rotation of the thigh occurs at the end of the loading response, while the peak external rotation occurs at the beginning of the early swing, and the average total horizontal arc of femoral motion during walking is 8° [23]. In the supporting phase, the main muscles controlling the hip joint are the hip extensor and hip abductor muscles. In the swing phase the hip flexor dominates. The adductor muscle group is often involved in the transition between swinging and supporting phases during movement. The deep external rotation muscle group cannot be separated to determine the timing of its participation in exercise. When these muscles perform their main functions, the function of the internal rotation muscle group plays a subordinate role [24]. Therefore, we believe that the relatively small range of hip joint movement radian in the horizontal plane and the subordinate role of adductor muscle group during walking lead to the irrelevant correlation between MIR and MER and the kinematic data of hip joint in gait analysis.
Lower-extremity muscle spasticity and muscle tension imbalance are common problems in children with cerebral palsy, and are also the main causes of tibial torsion [25]. Abnormal torsion of the tibia can change the normal alignment of the human body. The change of alignment will result in some corresponding compensations. The support stability of children with CP with abnormal tibial torsion is decreased while standing, and the unstable factors are increased during walking [26]. In terms of the tibia, we found that there was no correlation between TMA and CT tibial rotation (TT) on physical examination, while both TMA and TT were correlated with kinematic data of the tibial rotation in gait analysis, and TT had a higher correlation with kinematics captured by 3D gait analysis. The basic movement pattern of the tibia, femur, and pelvis in the normal human body during walking is determined by the way the bones are connected; they move in different directions and the amplitude of motion is different. There is a “locking mechanism” of the knee joint that is active in the process of walking. The final extension of the knee joint in the process of walking is often accompanied by external rotation of the tibia relative to the femur, and the corresponding knee joint begins to flex, together with internal rotation of the tibia relative to the femur [27]. In the process of walking, the amplitude and direction of the knee joint are changing. In the loading response phase, the tibia is 4–8° relative to the femur internal rotation; in the single-support phase, the tibia reaches the peak external rotation; in the end of the support phase and early swing phase, the tibia is about 1° relative to the femur internal rotation [28]. Children with spastic CP, especially spastic diplegic CP, also often have foot deformities, among which flat valgus foot deformities are particularly common. In the process of natural standing or walking, due to the presence of flat valgus foot in children with spastic diplegia CP, the ground reaction force acts on the lateral edge of the foot, leading to the lever arm dysfunctions of increased tibial external torsion, increased femoral internal rotation, increased knee flexion angle, and increased hip flexion adduction [29]. A small number of children with spastic diplegia and hemiplegia cerebral palsy develop simple tibial over rotation while walking or standing due to bilateral varus foot deformity [30]. In conclusion, with the increase of age in children with spastic CP, the tibia will produce outward or inward torsion deformity due to the “locking mechanism” of the lower limbs, and the evaluation of excessive torsion deformity of the tibia in or outward should be carried out under the condition of weight bearing (standing and walking). Both TMA and TT in physical and CT examination can determine the tibial rotation under static condition. However, there are many confounding factors in the TMA evaluation process, such as whether the child cooperated with the examination and the level of experience of the examiner. The tibial rotation of CT scan can accurately assess the tibial rotation of children. However, this examination method may not take into account the biomechanical factors of the lower extremities because the subject is static and non-weight-bearing. However, 3D gait analysis examination can analyze the bone connection movement mode of tibia, femur, and pelvis in detail, thus providing accurate kinematics of rotation.
Through a previous literature review, we found that most of the literature reported the rotation of the support phase of femur and tibia in physical examination, CT or EOS, and 3D gait analysis. In a complete gait cycle, the rotation of the femur and tibia occurs all the time. Therefore, the present study not only assessed the rotation of the femur and tibia in support phase, but also studied the correlation between the rotation of the double-support phase and the swing phase, which is an innovation.
There are some limitations in our study that should be considered. First, the rotation of the foot relative to the tibia during walking was not reported in this paper, which is also an important index in clinical gait analysis. However, the rotation of the foot relative to the tibia could not be measured in CT examination. Therefore, EOS examination will be used to improve the relevant research in the future. Second, both swing and stance phases can be divided into at least 3 important gait events. However, in this study, the kinematic data were recorded by the average measure of each gait phase in both swing and stance phases. These data may be inaccurate because of the average measures used, which may have affected our results. We will conduct further research on this in the future to make the conclusions more accurate.
Conclusions
Compared with CT and X-ray, 3D gait analysis technology have the advantage of being radiation-free. According to the findings of this study, 3D gait analysis can analyze the tibial rotation of children with CP, which is highly correlated with the results of CT and physical examination. However, femoral rotation, because of its small arc of motion during walking and low subordinate role of muscle groups, was not associated with CT and physical examination findings.
Figures
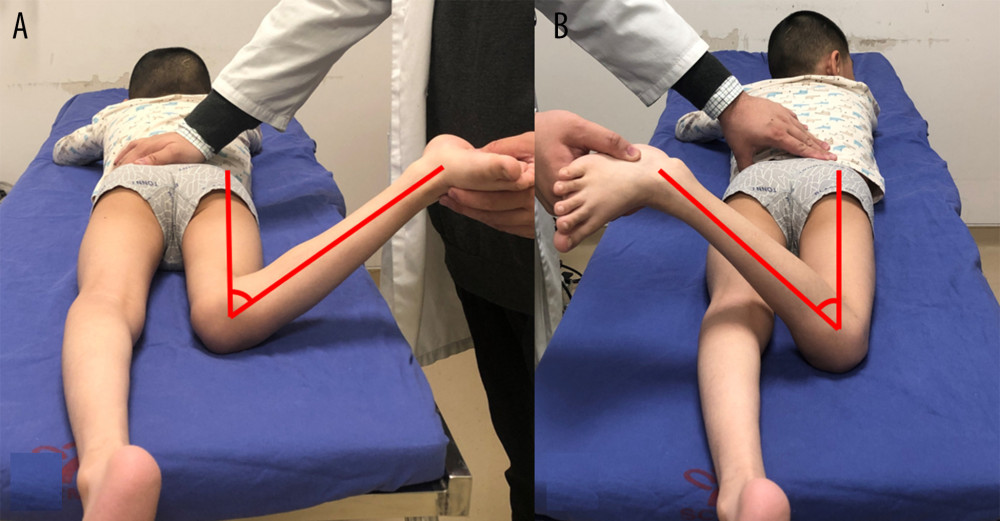 Figure 1. Clinical measurement of maximum internal rotation (MIR) (A) and maximum external rotation (MER) (B).
Figure 1. Clinical measurement of maximum internal rotation (MIR) (A) and maximum external rotation (MER) (B). 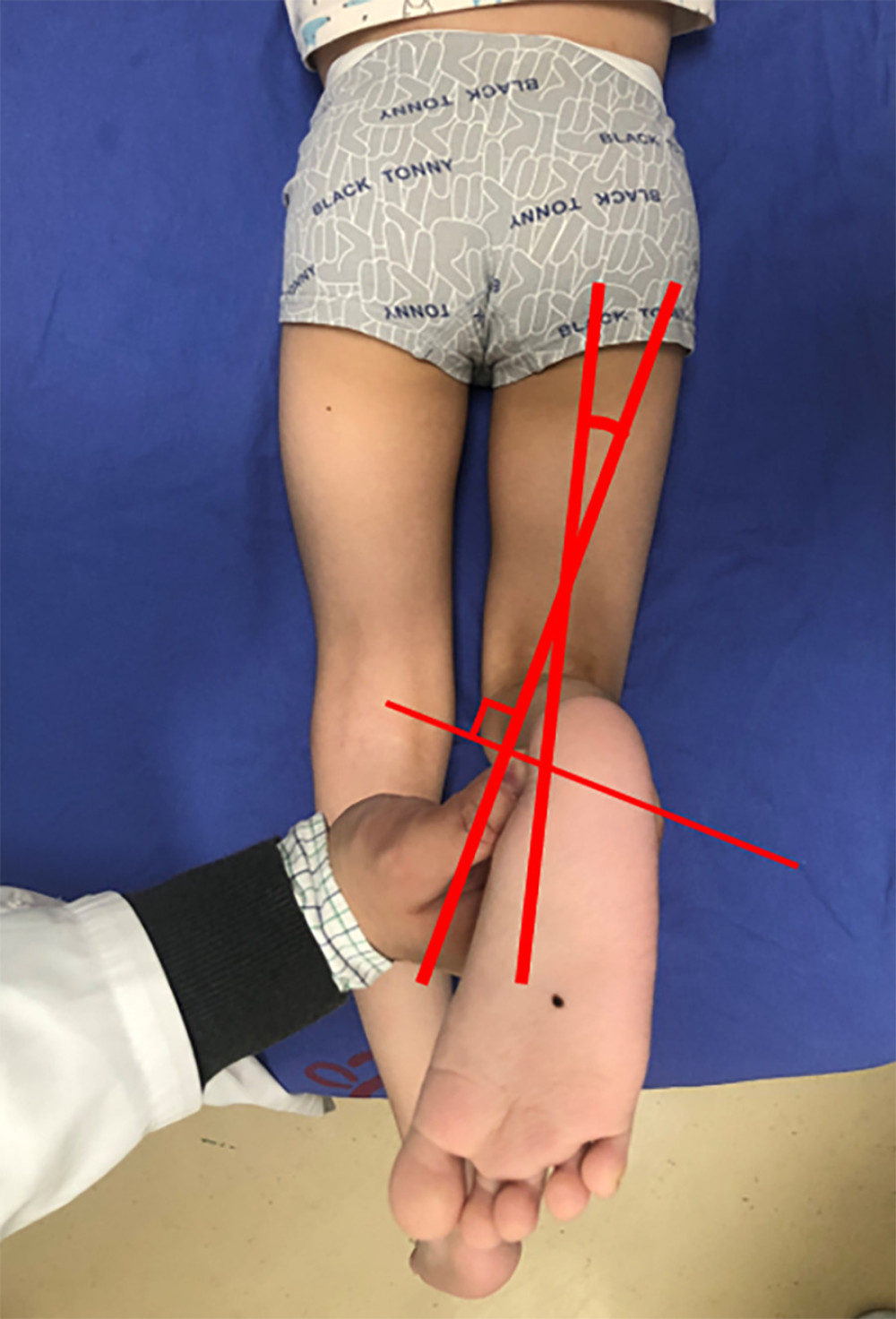 Figure 2. Clinical measurement of the tibial torsion by using the transmalleolar axis (TMA).
Figure 2. Clinical measurement of the tibial torsion by using the transmalleolar axis (TMA). 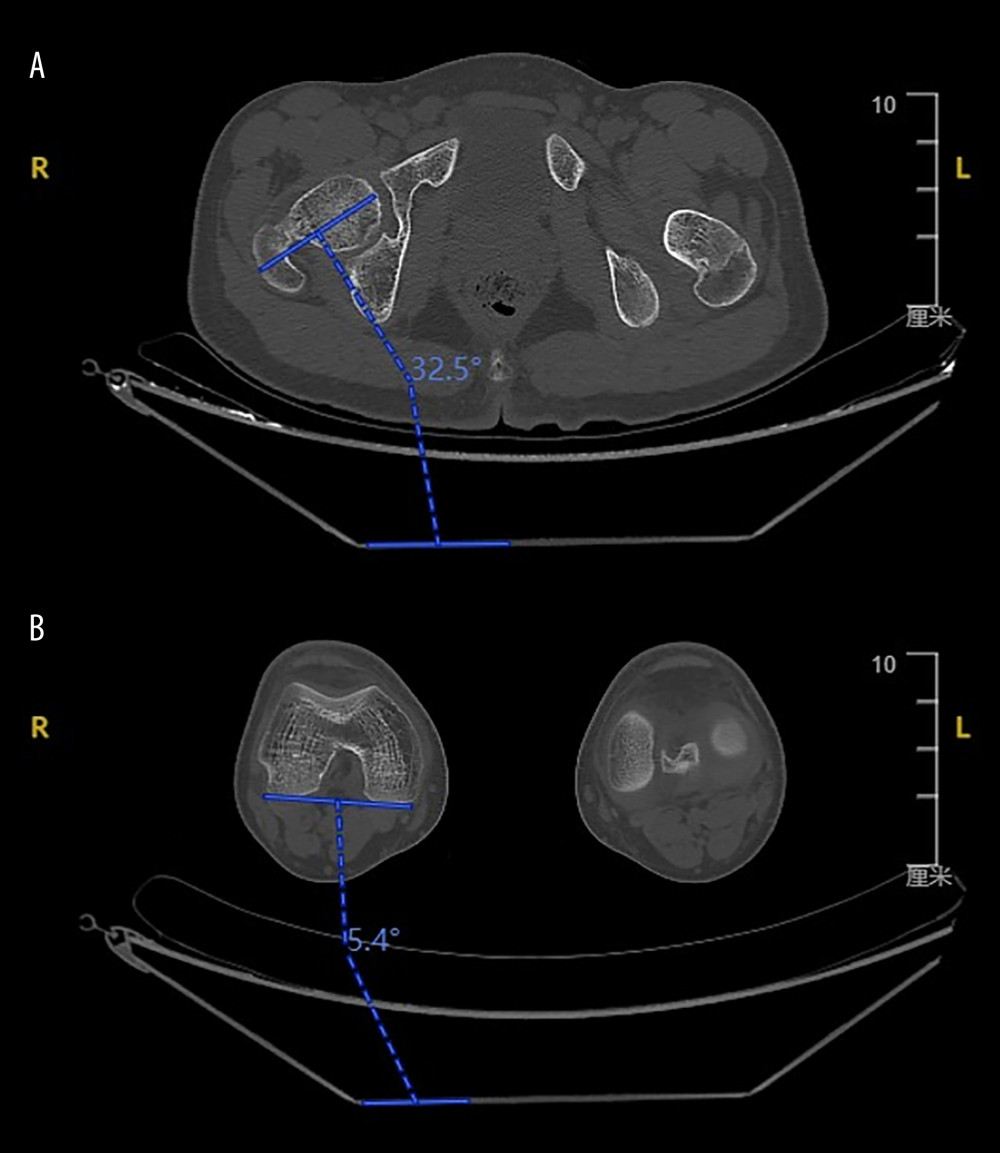 Figure 3. (A) The angle between a horizontal baseline and a long axis through the center of the femoral neck. (B) The angle between a horizontal baseline and a tangent to the posterior surface of the medial and lateral condyles of the distal femur.
Figure 3. (A) The angle between a horizontal baseline and a long axis through the center of the femoral neck. (B) The angle between a horizontal baseline and a tangent to the posterior surface of the medial and lateral condyles of the distal femur. 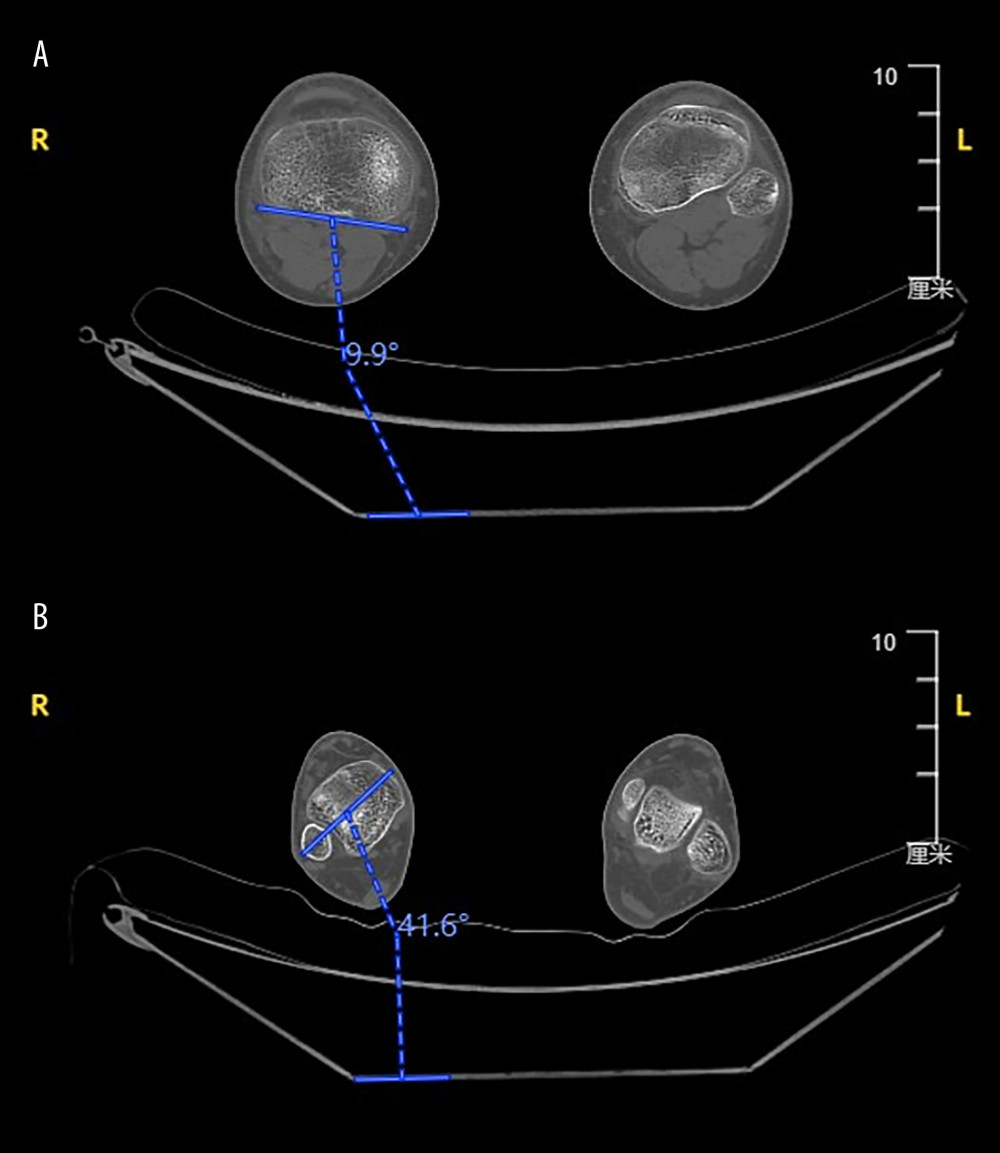 Figure 4. (A) The angle between a horizontal baseline and the tangent to the posterior aspects of the tibial plateau. (B) The angle between a horizontal baseline and the bimalleolar axis at the distal tibia.
Figure 4. (A) The angle between a horizontal baseline and the tangent to the posterior aspects of the tibial plateau. (B) The angle between a horizontal baseline and the bimalleolar axis at the distal tibia. 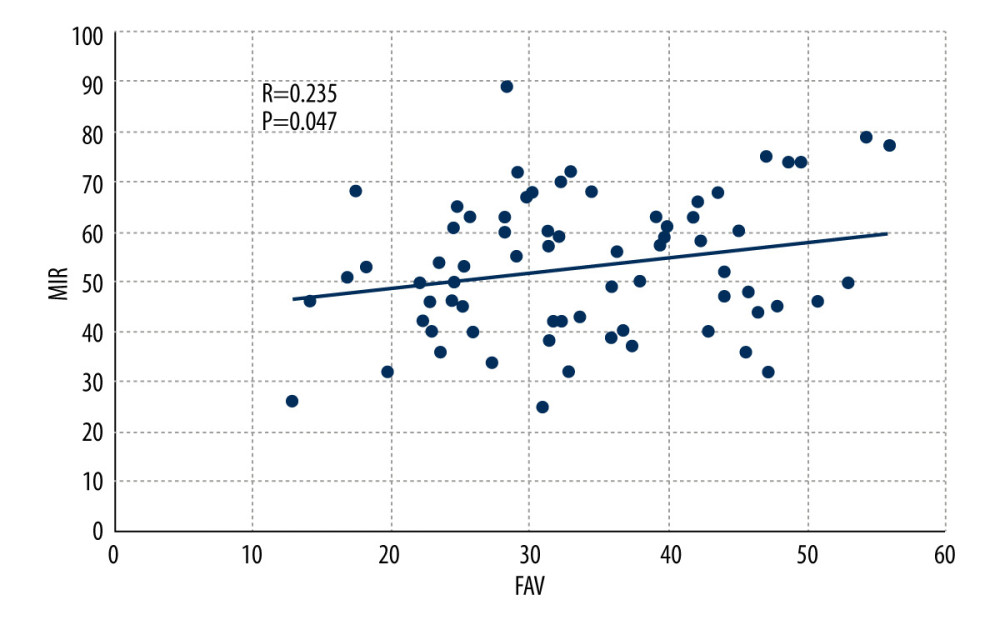 Figure 5. Scatter plot showing the correlation between maximum internal rotation (MIR) and femoral anteversion (FAV) by Pearson correlation test.
Figure 5. Scatter plot showing the correlation between maximum internal rotation (MIR) and femoral anteversion (FAV) by Pearson correlation test. 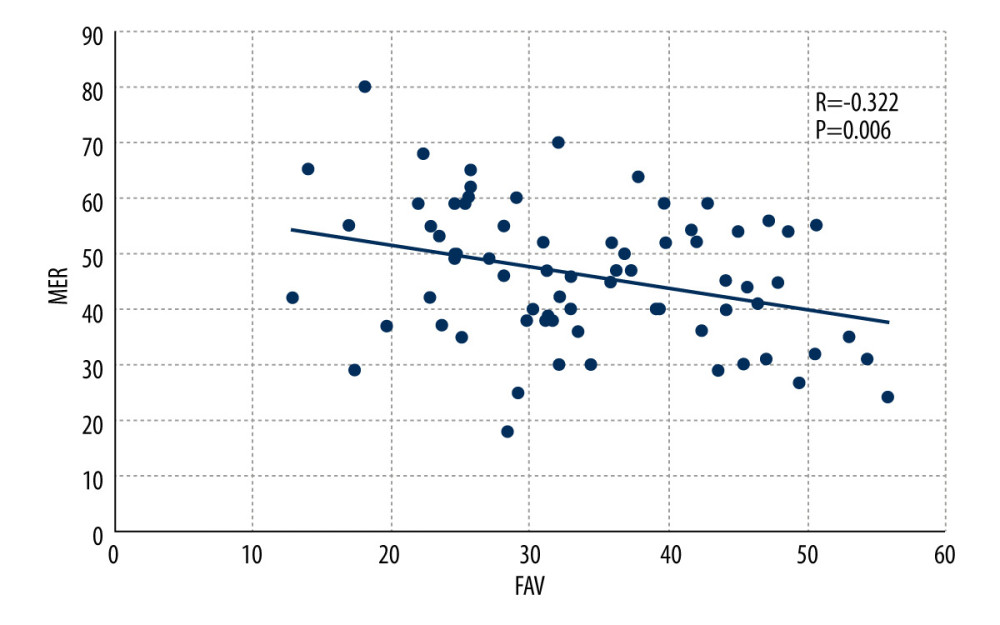 Figure 6. Scatter plot showing the correlation between maximum external rotation (MER) and femoral anteversion (FAV) by Pearson correlation test.
Figure 6. Scatter plot showing the correlation between maximum external rotation (MER) and femoral anteversion (FAV) by Pearson correlation test. 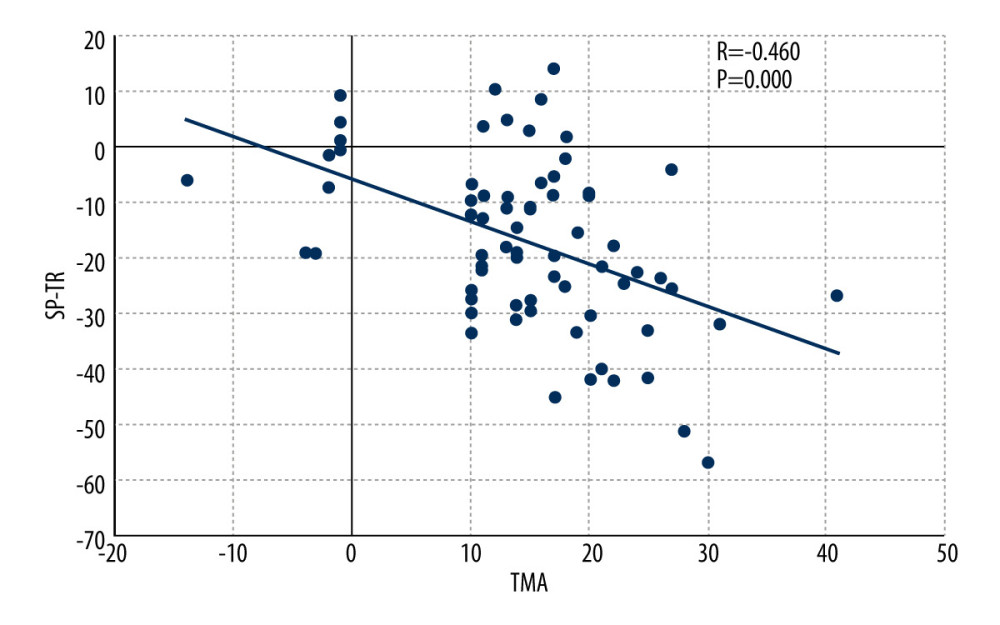 Figure 7. Scatter plot showing the correlation between transmalleolar axis (TMA) and swing phase of tibial rotation (SP-TR) by Pearson correlation test.
Figure 7. Scatter plot showing the correlation between transmalleolar axis (TMA) and swing phase of tibial rotation (SP-TR) by Pearson correlation test. 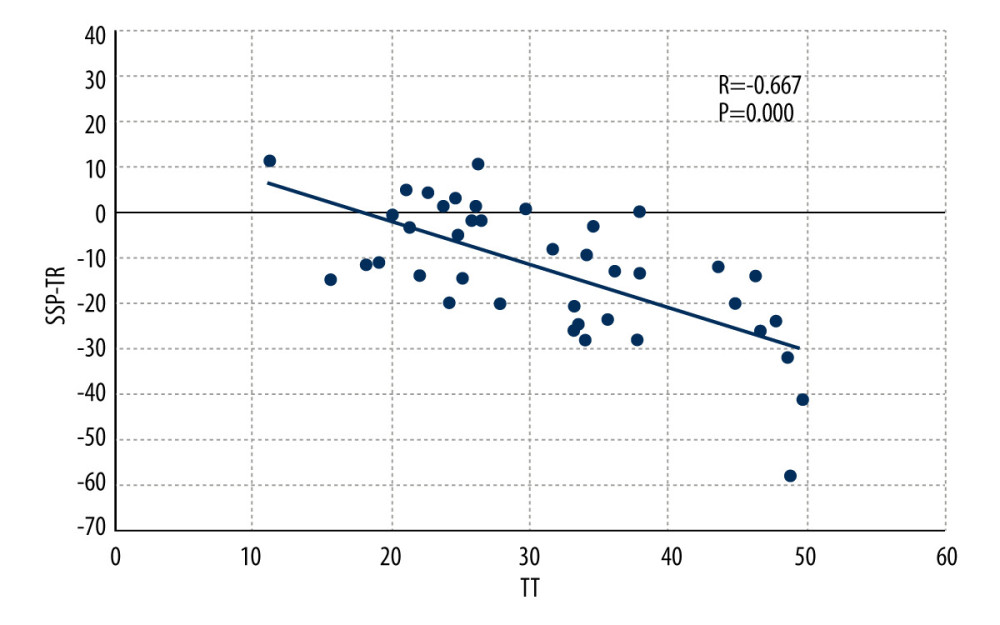 Figure 8. Scatter plot showing the correlation between tibial torsion (TT) and single-support phase of tibial rotation (SSP-TR) by Pearson correlation test.
Figure 8. Scatter plot showing the correlation between tibial torsion (TT) and single-support phase of tibial rotation (SSP-TR) by Pearson correlation test. References
1. Wren TA, Rethlefsen S, Kay RM, Prevalence of specific gait abnormalities in children with cerebral palsy: Influence of cerebral palsy subtype, age, and previous surgery: J Pediatr Orthop, 2005; 25; 79-83
2. Westberry DE, Wack LI, Davis RB, Femoral anteversion assessment: Comparison of physical examination, gait analysis, and EOS biplanar radiography: Gait Posture, 2018; 62; 285-90
3. Sangeux M, Mahy J, Graham HK, Do physical examination and CT-scan measures of femoral neck anteversion and tibial torsion relate to each other?: Gait Posture, 2014; 39; 12-16
4. Radler C, Kranzl A, Manner HM, Torsional profile versus gait analysis: Consistency between the anatomic torsion and the resulting gait pattern in patients with rotational malalignment of the lower extremity: Gait Posture, 2010; 32; 405-10
5. Carriero A, Zavatsky A, Stebbins J, Correlation between lower limb bone morphology and gait characteristics in children with spastic diplegic cerebral palsy: J Pediatr Orthop, 2009; 29; 73-79
6. Aktas S, Aiona MD, Orendurff M, Evaluation of rotational gait abnormality in the patients cerebral palsy: J Pediatr Orthop, 2000; 20; 217-20
7. Lee KM, Chung CY, Kwon DG, Reliability of physical examination in the measurement of hip flexion contracture and correlation with gait parameters in cerebral palsy: J Bone Joint Surg Am, 2011; 93; 150-58
8. Desloovere K, Molenaers G, Feys H, Do dynamic and static clinical measurements correlate with gait analysis parameters in children with cerebral palsy?: Gait Posture, 2006; 24; 302-13
9. Kerr AM, Kirtley SJ, Hillman SJ, The mid-point of passive hip rotation range is an indicator of hip rotation in gait in cerebral palsy: Gait Posture, 2003; 17; 88-91
10. Palisano R, Rosenbaum P, Walter S, Development and reliability of a system to classify gross motor function in children with cerebral palsy: Dev Med Child Neurol, 1997; 39; 214-23
11. McMulkin ML, Gulliford JJ, Williamson RV, Correlation of static to dynamic measures of lower extremity range of motion in cerebral palsy and control populations: J Pediatr Orthop, 2000; 20; 366-69
12. Byun HY, Shin H, Lee ES, The availability of radiological measurement of femoral anteversion angle: Three-dimensional computed tomography Reconstruction: Ann Rehabil Med, 2016; 40; 237-43
13. Gruskay JA, Fragomen AT, Rozbruch SR, Idiopathic rotational abnormalities of the lower extremities in children and adults: JBJS Rev, 2019; 7; e3
14. Eckhoff DG, Johnson KK, Three-dimensional computed tomography reconstruction of tibial torsion: Clin Orthop Relat Res, 1994; 302; 42-46
15. Wu G, Siegler S, Allard P, Standardization and Terminology Committee of the International Society of Biomechanics. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion – part I: Ankle, hip, and spine: J Biomech, 2002; 35; 543-48
16. Rodda JM, Graham HK, Carson L, Sagittal gait patterns in spastic diplegia: J Bone Joint Surg Br, 2004; 86; 251-58
17. O’Sullivan R, Walsh M, Hewart P, Factors associated with internal hip rotation gait in patients with cerebral palsy: J Pediatr Orthop, 2006; 26; 537-41
18. Aiona M, Calligeros K, Pierce R, Coronal plane knee moments improve after correcting external tibial torsion in patients with cerebral palsy: Clin Orthop Relat Res, 2012; 470; 1327-33
19. Kim HY, Cha YH, Chun YS, Correlation of the torsion values measured by rotational profile, kinematics, and CT study in CP patients: Gait Posture, 2017; 57; 241-45
20. Miller SD, Juricic M, Hesketh K, Prevention of hip displacement in children with cerebral palsy: A systematic review: Dev Med Child Neurol, 2017; 59; 1130-38
21. Helenius IJ, Viehweger E, Castelein RM, Cerebral palsy with dislocated hip and scoliosis: What to deal with first?: J Child Orthop, 2020; 14; 24-29
22. Chambers HG, Treatment of functional limitations at the knee in ambulatory children with cerebral palsy: Eur J Neurol, 2001; 8; 59-74
23. Levens AS, Inman VT, Blosser JA, Transverse rotation of the segments of the lower extremity in locomotion: J Bone Joint Surg Am, 1948; 30A; 859-72
24. Sheldon JD, Adkesson MJ, Allender MC: PLoS One 25, 2019; 14; e0220468
25. Fox AS, Carty CP, Modenese L, Simulating the effect of muscle weakness and contracture on neuromuscular control of normal gait in children: Gait Posture, 2018; 61; 169-75
26. Min JJ, Kwon SS, Kim KT, Evaluation of factors affecting external tibial torsion in patients with cerebral palsy: BMC Musculoskelet Disord, 2021; 22; 684
27. Nene A, Byrne C, Hermens H, Is rectus femoris really a part of quadriceps? Assessment of rectus femoris function during gait in able-bodied adults: Gait Posture, 2004; 20(1); 1-13
28. Anderson FC, Goldberg SR, Pandy MG, Contributions of muscle forces and toe-off kinematics to peak knee flexion during the swing phase of normal gait: An induced position analysis: J Biomech, 2004; 37; 731-37
29. Theologis T, Lever arm dysfunction in cerebral palsy gait: J Child Orthop, 2013; 7; 379-82
30. Lee KM, Chung CY, Sung KH, Femoral anteversion and tibial torsion only explain 25% of variance in regression analysis of foot progression angle in children with diplegic cerebral palsy: J Neuroeng Rehabil, 2013; 10; 56
Figures
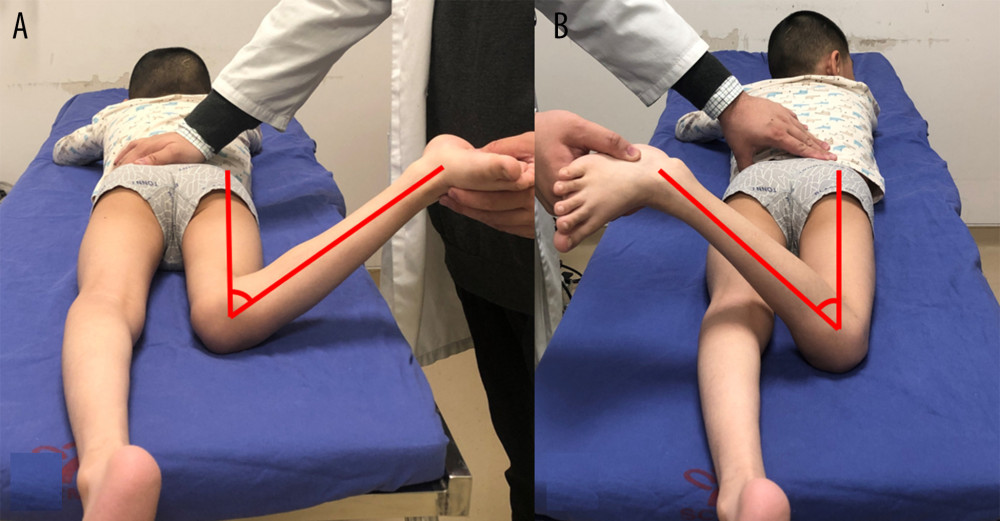 Figure 1. Clinical measurement of maximum internal rotation (MIR) (A) and maximum external rotation (MER) (B).
Figure 1. Clinical measurement of maximum internal rotation (MIR) (A) and maximum external rotation (MER) (B).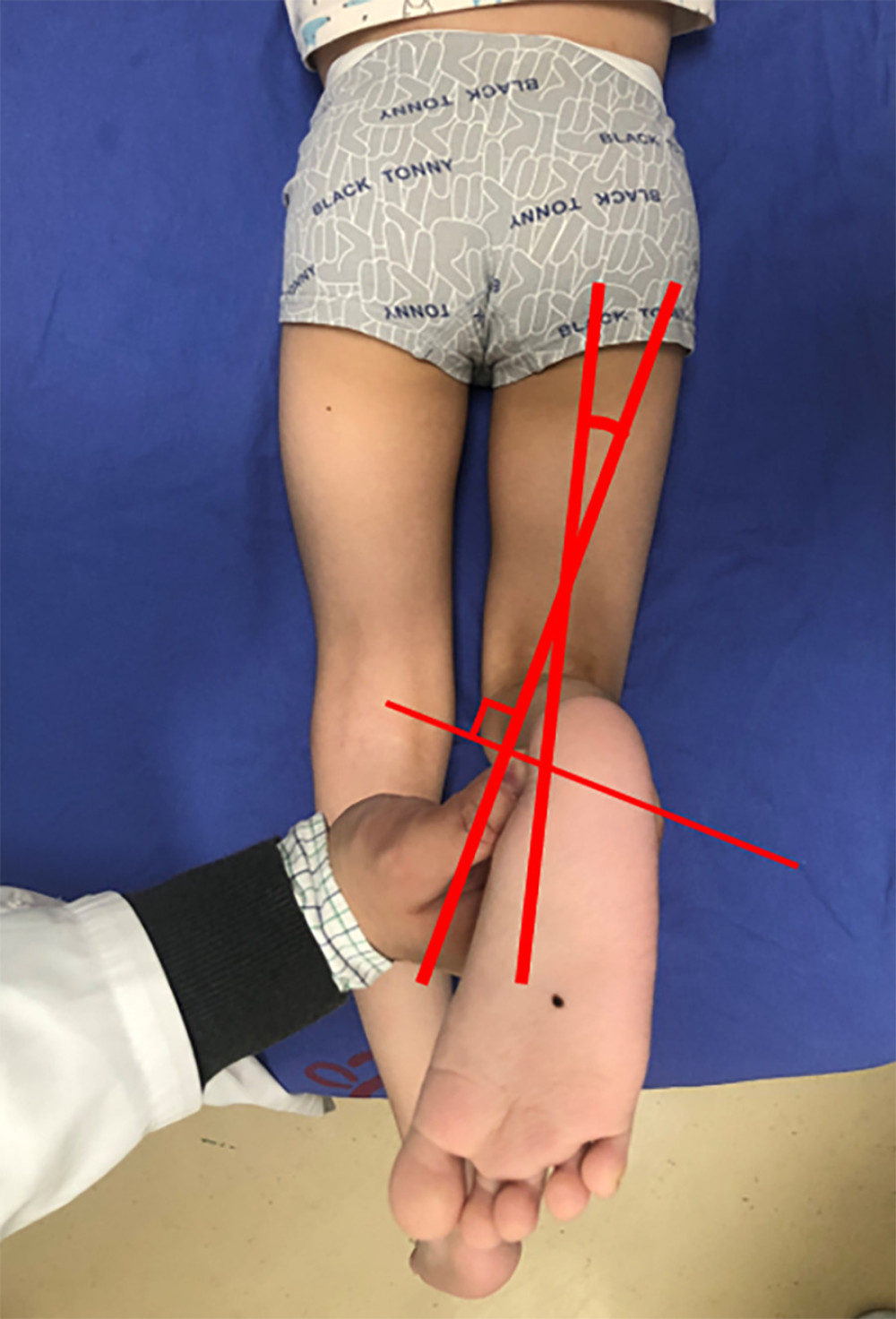 Figure 2. Clinical measurement of the tibial torsion by using the transmalleolar axis (TMA).
Figure 2. Clinical measurement of the tibial torsion by using the transmalleolar axis (TMA).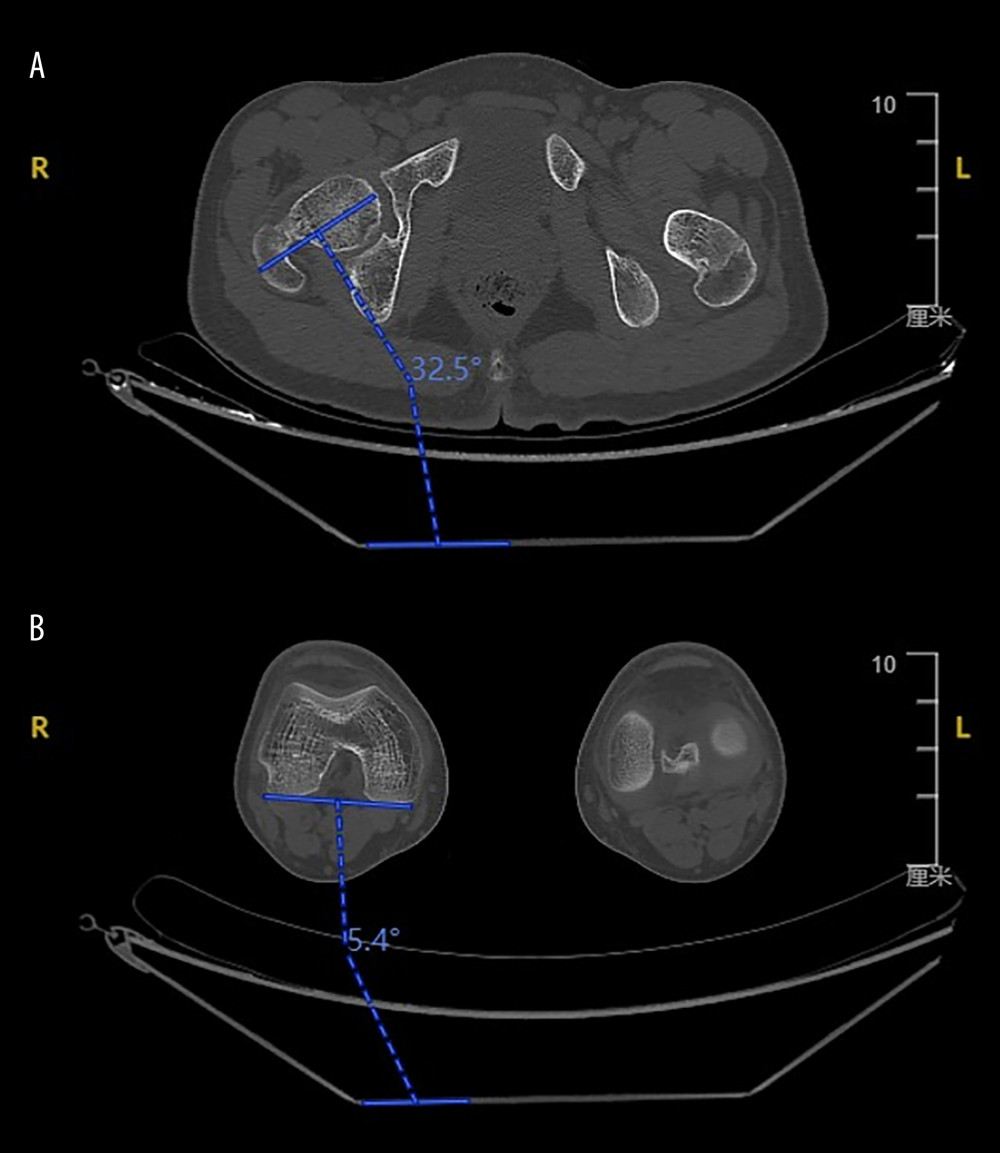 Figure 3. (A) The angle between a horizontal baseline and a long axis through the center of the femoral neck. (B) The angle between a horizontal baseline and a tangent to the posterior surface of the medial and lateral condyles of the distal femur.
Figure 3. (A) The angle between a horizontal baseline and a long axis through the center of the femoral neck. (B) The angle between a horizontal baseline and a tangent to the posterior surface of the medial and lateral condyles of the distal femur.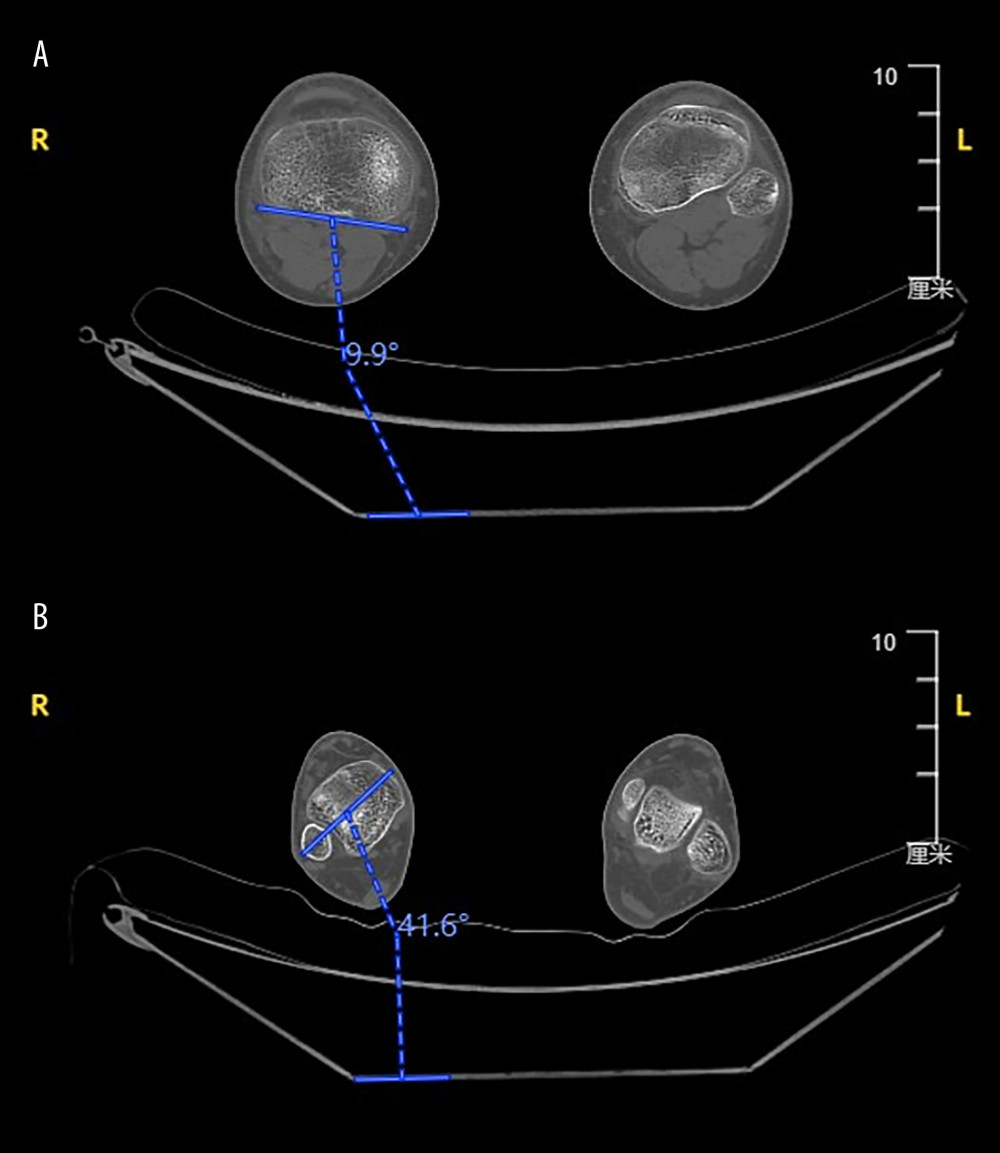 Figure 4. (A) The angle between a horizontal baseline and the tangent to the posterior aspects of the tibial plateau. (B) The angle between a horizontal baseline and the bimalleolar axis at the distal tibia.
Figure 4. (A) The angle between a horizontal baseline and the tangent to the posterior aspects of the tibial plateau. (B) The angle between a horizontal baseline and the bimalleolar axis at the distal tibia.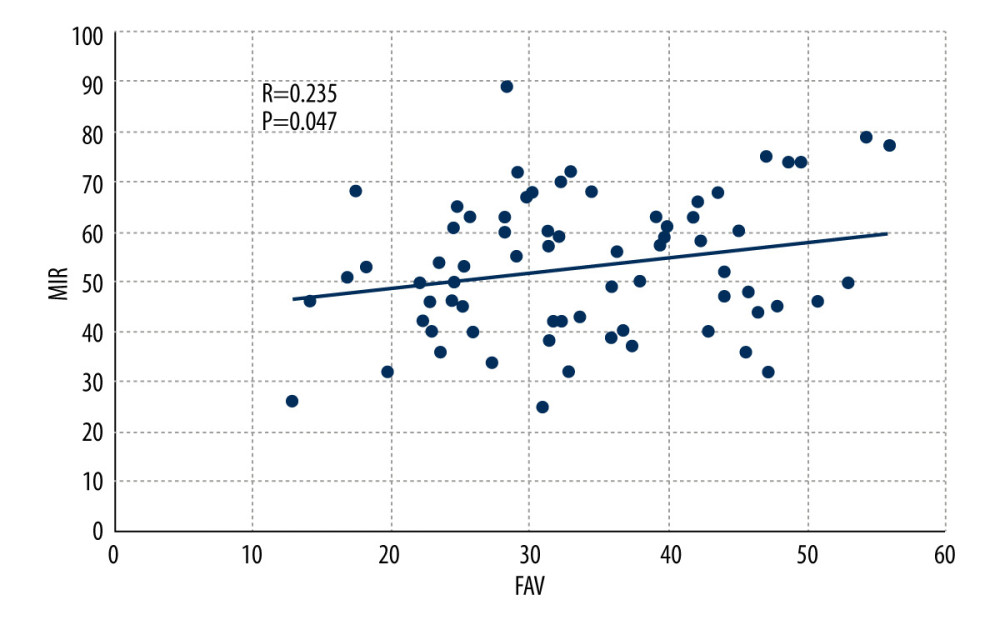 Figure 5. Scatter plot showing the correlation between maximum internal rotation (MIR) and femoral anteversion (FAV) by Pearson correlation test.
Figure 5. Scatter plot showing the correlation between maximum internal rotation (MIR) and femoral anteversion (FAV) by Pearson correlation test.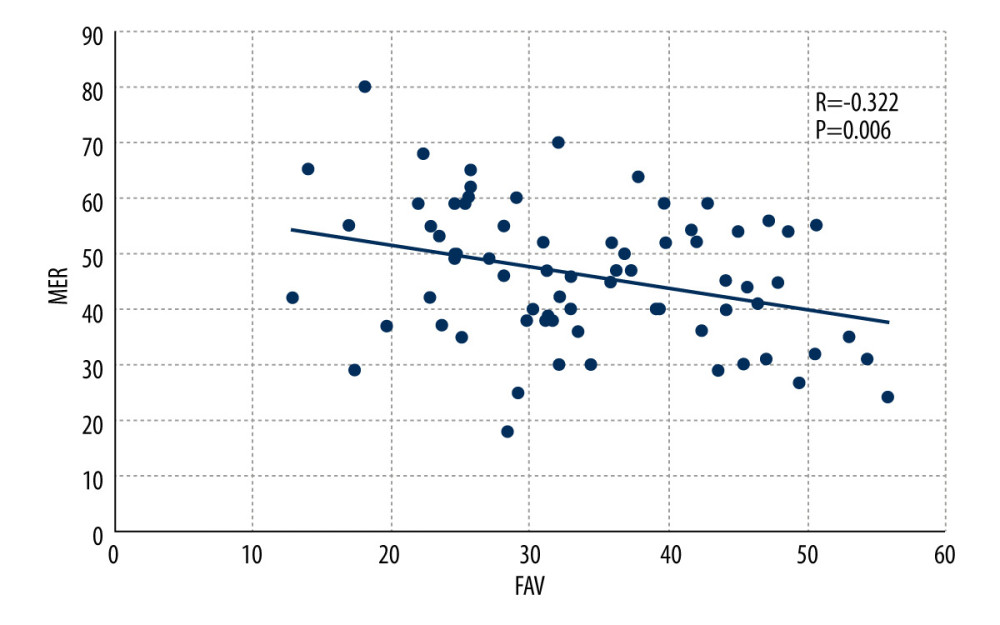 Figure 6. Scatter plot showing the correlation between maximum external rotation (MER) and femoral anteversion (FAV) by Pearson correlation test.
Figure 6. Scatter plot showing the correlation between maximum external rotation (MER) and femoral anteversion (FAV) by Pearson correlation test.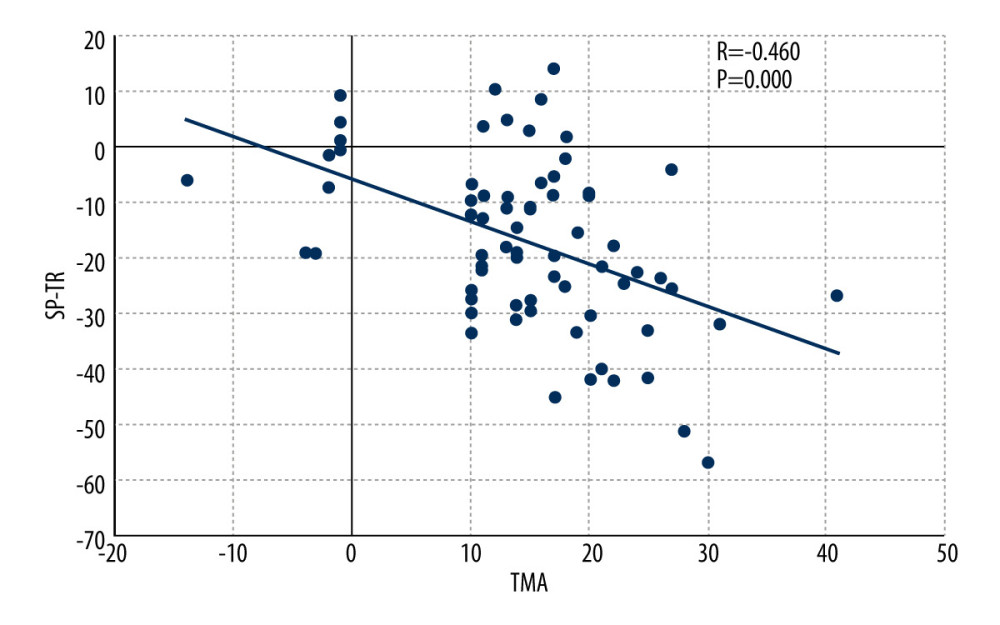 Figure 7. Scatter plot showing the correlation between transmalleolar axis (TMA) and swing phase of tibial rotation (SP-TR) by Pearson correlation test.
Figure 7. Scatter plot showing the correlation between transmalleolar axis (TMA) and swing phase of tibial rotation (SP-TR) by Pearson correlation test.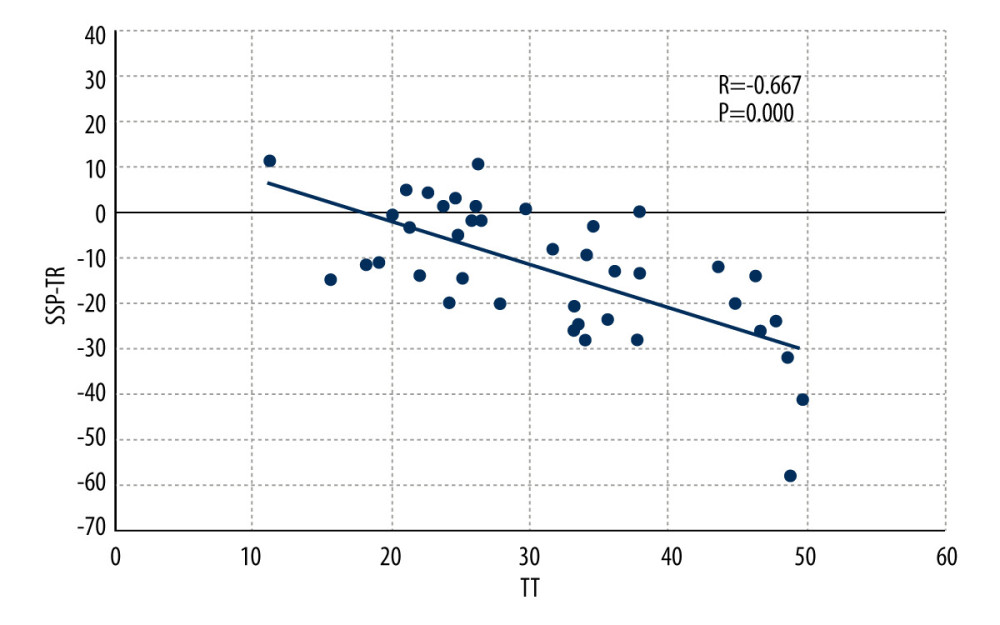 Figure 8. Scatter plot showing the correlation between tibial torsion (TT) and single-support phase of tibial rotation (SSP-TR) by Pearson correlation test.
Figure 8. Scatter plot showing the correlation between tibial torsion (TT) and single-support phase of tibial rotation (SSP-TR) by Pearson correlation test. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952