12 September 2023: Clinical Research
Retrospective Evaluation of Short-Course versus Traditional Preoperative Chemotherapy in Thoracolumbar Spinal Tuberculosis Patients
Lin Chen1ABCDEFG, Jun Zhang1ABCDEFG*DOI: 10.12659/MSM.941003
Med Sci Monit 2023; 29:e941003
Abstract
BACKGROUND: Thoracolumbar spinal tuberculosis is a severe form of extrapulmonary tuberculosis requiring precise management strategies. Traditionally, patients undergo a 2-4 week course of preoperative quadruple chemotherapy before surgery. However, recent clinical practices have begun exploring the potential of a short-course (1-7 days) intensive preoperative chemotherapy regimen. This study aims to examine and compare the clinical effectiveness of both approaches, offering critical insights into the optimal preoperative chemotherapy duration.
MATERIAL AND METHODS: In this retrospective analysis, we examined the clinical data from 123 patients with surgically treated thoracolumbar spinal tuberculosis. Patients were categorized into two groups based on the duration of preoperative chemotherapy: the short-course intensive chemotherapy group (n=53, 1-7 days) and the traditional quadruple chemotherapy group (n=70, 2-4 weeks). We gathered and compared the pertinent clinical data from both groups to ascertain differences in clinical efficacy.
RESULTS: All 123 patients underwent follow-up for a duration averaging 2.8±0.7 years. Five patients experienced postoperative recurrence. Patients reported significant pain alleviation and overall good clinical outcomes. Among patients with neurological dysfunction, neurological symptoms were ameliorated, and the implanted devices were found to be effective. Bony fusion was observed in all the bone grafting regions.
CONCLUSIONS: For patients suffering from thoracolumbar spinal tuberculosis exhibiting progressive neurological deterioration, surgical intervention is deemed feasible after a brief period (usually 1-7 days) of intensive preoperative antitubercular therapy. This finding suggests that short-course intensive preoperative chemotherapy may serve as a viable approach in managing such cases.
Keywords: Spinal Diseases, Antitubercular Agents, preoperative period, Orthopedic Procedures, Humans, Retrospective Studies, Tuberculosis, Spinal, Bone Transplantation, Neoadjuvant Therapy
Background
Tuberculosis (TB) is one of the most common infectious diseases worldwide [1]. Spinal tuberculosis (STB) accounts for around 2% of all cases of TB and around 15% of extrapulmonary TB cases [2]. The preferred treatment for STB is still controversial. Some surgeons advocate medical therapy alone, while some recommend the combination of chemotherapy and surgery [3]. Hodgson and Stock reported radical surgery for STB, namely the “Hong Kong Operation,” which meant extirpation of the TB focus, posteriorly until the dura mater and cephalad caudad until healthy and bleeding cancellous bone was exposed [4]. Usually, if TB remains uncontrolled after conservative treatment, then surgery is considered as an effective treatment for patients affected by bone destruction, angular deformity, spinal instability, paraspinal or spine canal abscess, or nerve impairment. The thoracolumbar spine is a transition zone between the relatively stable thoracic vertebrae and the highly movable lumbar vertebrae. Thoracolumbar STB, in combination with the spinal canal abscess, can easily induce nerve damages caused by spinal cord compression [5]. For patients with STB who have surgical indications and need debridement, anti-TB drugs should be strictly administered for 2–4 weeks before surgery, but patients with spinal nerve dysfunction are indications for active surgical treatment, especially for spinal nerve function. For patients with progressive deterioration, if the neurological function cannot be rescued by surgical intervention as soon as possible under the protection of effective anti-TB drugs, it will cause irreversible damage to neurological function [6].
Before the advent of surgical treatment of STB, the length of preoperative anti-TB drug treatment has been a continuing problem for spine surgeons. The main concern is whether the lack of strict and standardized anti-tuberculosis treatment for 2–4 weeks before surgery can cause related postoperative complications. In this study, 53 patients with STB with neurological dysfunction were treated with short-course intensive chemotherapy after using an improved chemotherapy regimen since 2016; they then received surgical treatment. The relevant clinical data were collected and analyzed to assess the feasibility and necessity of preoperative short-course intensive chemotherapy in treating STB and to deepen the understanding of early and active surgical intervention for thoracolumbar STB.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria were as follows: (i) According to clinical data, the patient was diagnosed with thoracolumbar STB; diseased lesions involving the T11-L2) region; and lesions were localized within 2 vertebral bodies. The operation involved TB debridement and single-segment bone graft fusion and internal fixation; (ii). At least 1 of the following conditions should have been met: the symptoms of spinal cord or nerve compression were obvious or progressively aggravated, the spine was unstable, a large cavity and obvious sequestrum were formed; (iii) Patients with focus clearance, bone graft fusion and internal fixation only through a 1-stage anterior side approach; and (iv) The follow-up time for included patients was at least 2 years, and patients had complete clinical data.
The exclusion criteria were as follows: (i) Combination with other active TB; (ii) Combination with other spinal tumors and osteoporotic diseases; (iii) Inability to tolerate intensive chemotherapy and traditional chemotherapy; (iv) Postoperative recurrence of STB; (v) Presence of contraindications to surgery; (vi) Unwilling to undergo surgery; and (vii) Failure to complete the follow-up.
GENERAL PATIENT INFORMATION:
This study was approved by the Ethics Committee of the hospital, and written informed consent was obtained from all patients.
Data of 123 patients with thoracolumbar STB who were admitted to the Department of Spinal Surgery, Zunyi Medical University Affiliated Hospital from August 2016 to August 2018 were reviewed. Patients with STB, excluding related surgical contraindications, and who underwent TB debridement, bone graft fusion, and internal fixation and received >2 years of follow-up were divided into 2 groups: a short-course intensive chemotherapy group (1–7 days; n=53, mean age: 45.3 years, range: 14–75 years) according to the time of preoperative chemotherapy, with a mean duration of 5.35±1.27 days, and the traditional quadruple chemotherapy group (2–4 weeks; n=70, mean age: 46.4 years, range: 12–77 years), with a mean duration of 2.50±1.15 weeks. Patients in the traditional quadruple chemotherapy group had no neurological dysfunction. All preoperative anti-TB patients completed chemotherapy before surgery.
PREOPERATIVE PREPARATION:
The patients in the short-course intensive chemotherapy group (1–7 days) were treated with isoniazid (INR injection, 300 mg intravenous infusion/day); rifampicin (RFP injection, 600 mg intravenous infusion/day); and ethambutol (EMB, 15 mg/(kg·d) taken in the morning/day); pyrazinamide (PZA, 25 mg/(kg·d) taken in the morning/day), strengthen anti-TB effects before surgery. The medication time is based on preoperative-related inspections, generally 1–7 days. The traditional quadruple chemotherapy group received strict and standardized quadruple anti-tuberculosis treatment of oral INR (5 mg/(kg·d) taken in the morning/day), RFP (10 mg/(kg·d) taken in the morning/day), EMB (15 mg/(kg·d) taken in the morning/day), and PZA (25 mg/(kg·d) taken in the morning/day) for 2–4 weeks. Patients in both groups completed the relevant preoperative tests and had no contraindications for surgery. Surgical treatment was performed when the ill effects of tuberculosis poisoning had improved, hemoglobin had reached more than 100 g/L, ESR and CRP were in the declining or stable stage, and the general condition was good. In the preoperative preparation section, prophylactic antibiotic cefamandole was administered 30 min prior to surgery to prevent non-specific inflammation.
SURGICAL METHODS:
The anterior-lateral surgical approach was used for both study groups. After induction of general anesthesia, the patients were placed in the lateral decubitus position. C-arm (C-arm X-ray) fluoroscopy was performed to locate the vertebral body of the lesion. After routine disinfection with iodine and alcohol and following other standard operating room practices, the skin and subcutaneous tissue were incised along the markings, cutting through the fascia, latissimus dorsi, and inferior serratus posterior muscle with high-frequency electrocautery. The ribs were removed at the plane of the transverse process, then the extrapleural cavity and the extraperitoneal cavity were exposed and part of the diaphragm was cut off. The chest wall was opened with a distractor, the lateral side of the vertebral body was exposed, and the arteries and veins of the thoracic vertebral segments were exposed and ligated to fully expose the thoracic and lumbar vertebral bodies. The lesion tissue and pus were fully removed, and some tuberculous granulomas were collected as specimens. Rinsing was repeatedly performed with a large amount of INR injection and normal saline. After properly opening the intervertebral space, the bone graft bed was prepared with a high-speed drill. Next, the titanium cage and bone aid strips were measured and cut to the appropriate length; allogeneic bone and autologous rib particles mixed with streptomycin (SM) were placed into the titanium cage. The autologous rib strip and titanium cage mixed with SM were then implanted into the intervertebral space, and screws and plates of appropriate length were installed on the side of the thoracic vertebral body and locked. C-arm fluoroscopy showed that the positions of the plates, screws, and titanium cages were satisfactory. Exploration showed that the titanium cage plate and screws were stable and reliable, the spinal canal was unobstructed, and the dura was not compressed. A large amount of normal saline was used for rinsing. No active bleeding was found, and the operation area was rinsed with a collagen sponge. After a negative-pressure drainage tube was placed, the diaphragm was sutured, the peritoneal cavity and pleural cavity were closed, the muscle tissue was anastomosed, the incision was sutured layer-by-layer, and sterile dressing was bandaged for fixation. The postoperative specimens were sent for pathology and TB bacterial culture examination.
POSTOPERATIVE TREATMENT:
Postoperatively, symptomatic and supportive treatments such as primary care, electrocardiogram (ECG) monitoring, low-flow oxygen inhalation, anti-inflammatory therapy, hemostasis, and fluid replacement were given. Oral anti-TB drug treatment was continued for 9–12 months after surgery, and a brace was worn for 6–9 months beginning 1 week after surgery. The ESR and CRP levels were re-examined 3 days after the operation. The dressing was changed, and the catheter was extubated 3 days after the operation (determined according to the specific condition of the patient) to observe healing of the incision. It was crucial to quickly adjust the anti-tuberculosis drugs according to GeneXpert MTB/RIF, TB-DNA and the results of
FOLLOW-UP AND EVALUATION CRITERIA:
Clinical manifestations: symptoms of TB poisoning and local pain were evaluated by visual analog scale (VAS); the recovery of life and work ability was evaluated as previously described by Zhang Xifeng et al [7].
Pain relief: The VAS score (0–10) was used to evaluate pain relief, with 0 indicating no pain and 10 indicating the worst pain imaginable.
Efficacy evaluation: Using the evaluation criteria of Zhang Xifeng et al, efficacy was divided into 4 grades: excellent, good, moderate, and poor. Excellent: For moderate-to-heavy manual laborers, the ability to perform physical labor as before surgery, and for the elderly, frail, and weaker patients, the ability to regain self-care for daily living; Good: Although not able to restore the working ability as before the disease, patients could take care of themselves completely; Moderate: Lost the ability to work before surgery and can only maintain self-care, but no recurrence of TB; Poor: recurrence of TB.
Neurological function recovery and ASIA classification were used to evaluate the neurological function changes of postoperative patients.
The bone graft healing was observed by imaging, including thoracolumbar plain radiographs, and computed tomography (CT) scans. The inspection period was 1, 3, 6, 12, and 18 months after the operation. The bone graft healing was judged according to Moon’s standard [8].
Combining CT and radiographic findings according to Moon’s criteria resulted in no loss of correction power, no resorption of grafted bone, no resorption of the bone graft bed; significant bone remodeling occurred between the graft bed and the graft bone rearrangement of continuous trabecular bone and thick graft bone.
Healing of incision: The inspection period was 3 days, 1 week, and 2 weeks after the operation. Healing was based on the standard of delayed healing of the incision.
Criteria for delayed incision healing were: patients with postoperative incision redness, swelling, exudation, and incision that did not heal within 12 days were considered to have delayed incision healing.
The dissemination of M.tb was judged according to the clinical manifestations of tuberculous meningitis, tuberculous pleurisy, and tuberculous peritonitis after operation.
Recurrence of TB was checked at 1 month, 3 months, 6 months, and 12 months after the operation, and the recurrence of TB was based on the standard of TB recurrence.
Recurrence criteria of TB: patients with TB recovered well after surgery and the various clinical indicators returned to normal, but after a period of time, new TB lesions appeared in the original region or in other parts.
STATISTICAL ANALYSIS:
SPSS 23.0 statistical software (IBM Corporation, Armonk, NY, USA) was used to analyze and process clinically relevant data. The measurement data of the 2 groups were expressed as the mean±standard deviation (χ̄±s). The measurement data between the 2 groups were compared using the 2 independent samples
Results
From August 2016 to August 2018, a total of 123 patients underwent surgery and were followed-up for more than 2 years, with an average of 2.8±0.7 years. According to the duration of preoperative chemotherapy, patients were divided into the short-course intensive chemotherapy group (1–7 days, n=53) group (a 25-year-old woman with tuberculosis of the 10th and 11th thoracic vertebrae and paravertebral abscess, spinal cord lumbar enlargement and compression (AISA grade C) received preoperative chemotherapy for 5 days (Figures 1, 2 show the clinical data of patients receiving short-term intensive chemotherapy) and the traditional quadruple chemotherapy group (2–4 weeks, n=70). There was no significant difference in the general data of the patients between the groups with chemotherapy duration of 5 days and those with chemotherapy duration of 2–4 weeks (
Regarding surgical conditions, all 123 patients with thoracolumbar STB successfully completed the treatment of stage I TB debridement, bone graft fusion, and internal fixation. In the short-course intensive chemotherapy group, the operation time range was 195–478 min (mean time: 313 min). The volume of blood loss range was 50–1800 mL (mean volume: 338 mL). In the traditional quadruple chemotherapy group, the operation time range was 197–498 min (mean time: 327 min). The volume of blood loss range was 65–1500 mL (mean volume: 312 mL). There was no significant difference in operation time and intraoperative blood loss between the 2 groups (Table 1), and there was no instance of death or spinal cord injury during the operation. The diseased thoracic and lumbar vertebral bodies were fully exposed during surgery. Samples from the tuberculous granuloma were collected from both patient groups and sent for pathology and TB bacterial culture examination. The
Postoperatively, there was no delayed healing of the postoperative incision and no dissemination of M.tb. The anti-TB time for patients with no drug resistance of STB or no cultured M.tb was 12–18 months, and the anti-tuberculosis treatment time for patients with drug resistance of STB was at least 24 months after surgery, with regular monitoring of liver and kidney functions.
Among the 123 patients included, 118 discontinued medication 12–18 months after surgery, and the other 5 patients with TB recurrence were cured within 2 years after surgery. The VAS scores of the above 2 groups of patients decreased significantly with time, and there was no significant difference in the VAS scores between the 2 groups (
Discussion
In this study, the clinical efficacy and changes of related indicators of surgical treatment after short-course intensive therapy (1–7 days) and traditional quadruple chemotherapy (2–4 weeks) were analyzed and compared. Although the surgical treatment of STB has achieved satisfactory results in recent years, before the advent of surgical treatment of STB, the length of preoperative anti-TB drug treatment was a continuing problem for spine surgeons. The traditional point of view [10,11] is that anti-TB drugs should be strictly administered for 2–4 weeks before STB surgery, and surgery should be performed only after the patient’s ESR and CRP test indicators have decreased significantly and are trending toward normal. The purpose is to prevent TB caused by early surgery. Bacillus dissemination in vivo causes local recurrence of STB and sinus tracts, leading to delayed healing of surgical incisions. However, spinal nerve dysfunction in patients with STB is an indication for active surgical treatment, especially for patients with progressive deterioration of spinal nerve function. Irreversible damage to function requires a series of preoperative short-course chemotherapy regimens.
It is currently believed that the purpose of prescribing anti-TB drugs before STB surgery is to control the number of TB bacilli in the lesions, inhibit their growth, and avoid the spread of TB bacilli caused by surgery. The traditional preoperative quadruple anti-TB treatment is based on the plan formulated for bone and joint TB in China [12]: oral INR (300 mg/day), oral RFP (450 mg/day), oral EMB (750 mg/day), and oral PZA (750 mg/day) for 2–4 weeks. In recent years, in research on preoperative anti-TB effects of STB, Shibing and Yanzheng et al [13] reported that the shortest preoperative anti-TB treatment time in China was 2 weeks. Benli [14] reported 63 patients with Pott’s disease who were treated with anti-TB medication for 3 weeks prior to surgery, with the exception of patients with progressive neurologic deficits who required emergency decompression. Therefore, most scholars [10,11] believe that open pulmonary TB and acute miliary pulmonary TB should be excluded before performing TB debridement. After strict and standardized anti-TB drug chemotherapy for about 4 weeks, the symptoms of TB are relieved. When the clinical biochemical indicators of ESR and CRP are significantly reduced, the surgical treatment of STB is feasible, but there is no clear research to explain its necessity.
The traditional view is that anti-TB drugs should be strictly prescribed for 2–4 weeks before surgery, but in patients with spinal nerve dysfunction, active surgical treatment is indicated, especially for patients with progressive deterioration of spinal nerve function. Under the protection of anti-TB drugs, early surgical intervention to rescue neurological function will cause irreversible damage to neurological function; therefore, a series of preoperative short-course chemotherapy regimens have emerged. In a study on short-term preoperative anti-TB treatment, Zhang Hongqi [15] detected the DNA content of M.tb in the peripheral blood by PCR and found that no M.tb dissemination was detected in the patients who had undergone TB foci removal surgery. These patients received preoperative anti-TB medication less than 2 weeks before the surgery, and had a higher preoperative ESR than normal. Alici [16] conducted a retrospective analysis of 434 patients with vertebral TB treated by surgery, and focused on the analysis of the time of preoperative chemotherapy. Among them, 376 patients received regular anti-TB drug treatment for 4 weeks, and postoperative follow-up found that 2 patients relapsed. The remaining 58 patients received the same chemotherapy regimen and underwent surgery 6–18 h after admission to save neurological function, and no recurrence of STB occurred after surgery. Therefore, the preoperative chemotherapy time can be significantly shortened. With the gradual improvement of the professional knowledge of STB surgery, this scheme can be used for STB patients who have surgical indications except for nerve damage, allowing short-term chemotherapy followed by surgery. Xue Zhonglin [17] performed STB debridement in 16 patients with STB after 1 week of regular chemotherapy before surgery, and standardized anti-TB treatment for 1 year after surgery, and concluded that short-course anti-TB treatment before surgery had no significant effect on patient cure. However, it can reduce the length of time the patient suffers from the disease before surgery.
Ma et al [18] retrospectively analyzed 217 adult patients with thoracic and lumbar TB, with an average age of 39 years (16–67 years). Among them, 27 patients received regular anti-TB treatment within 6–18 h before surgery. No recurrence of STB occurred after surgery. Li Juan et al [19] treated patients with STB with standard anti-TB drugs for 1–2 weeks before surgery, and performed TB debridement when the general condition of the patients was good. The ESR and CRP were either stable or decreased, although there were a few cases of M.tb dissemination. Yin et al [20] treated 31 patients with STB who needed surgical treatment. Their patients received standardized anti-TB treatment for 3–17 days, and no dissemination of M.tb was found after surgery. In the above-mentioned studies, preoperative short-course chemotherapy regimens were proposed, but the chemotherapy regimens were mainly traditional quadruple regimens, which only shortened the preoperative anti-TB time. Our study is based on the clinical data of patients with STB in the Affiliated Hospital of Zunyi Medical University, who underwent preoperative short-course intensive anti-TB treatment followed by surgical treatment.
There was no significant difference in the VAS score between the 2 groups (
For drug-resistant TB patients, the factors and severity of drug resistance of M.tb have their own characteristics. Therefore, for patients with different characteristics, the clinical chemotherapy plans are different. It is necessary to fully evaluate the specific conditions of patients themselves and develop scientific and effective clinical treatment plans for patients on the basis of closely combining the drug sensitivity test results [21]. If it is difficult to carry out drug sensitivity testing or accurate test results cannot be obtained, the combination of anti-TB drugs can be carried out on the basis of comprehensive clinical judgment and prediction of drug resistance, referring to the relevant standards for the use of second-line anti-TB drugs, which is the so-called empirical treatment [22]. At present, in the treatment of multidrug-resistant spinal tuberculosis, we strictly follow the requirements of the WHO Guidelines [23] for the Treatment of Drug-Resistant Tuberculosis (2016 update) to guide drug use. The better clinical efficacy achieved in the short-course intensive chemotherapy group was closely related to early surgical removal of TB lesions, adequate decompression of spinal nerves, bone graft fusion, and strong internal fixation. Therefore, patients with progressive neurological deterioration should receive intensive anti-TB treatment before surgery, and after their general health improves, they should be actively treated with surgery.
Through the comparison and analysis of various research data in this study, patients with preoperative short-course intensive chemotherapy and traditional quadruple chemotherapy achieved satisfactory postoperative effects. There was no significant difference between groups in postoperative TB recurrence and delayed incision healing. Patients with progressive neurological deterioration should receive intensive anti-TB treatment before surgery, and when their general health improves, active surgical treatment should be performed to reduce the preoperative preparation time of patients. The recovery of neurological function creates favorable conditions and significantly shortens the perioperative time and hospitalization costs by about 1–3 weeks.
However, as this was a retrospective study with a small number of patients, it is necessary to expand the sample size and conduct a multicenter study.
Conclusions
Surgery is feasible for patients with thoracolumbar TB who present with progressive deterioration of neurological function after a short period of intensive preoperative antitubercular therapy (usually 1–7 days).
Data Availability
Available upon reasonable request from a bona fide researcher.
Figures
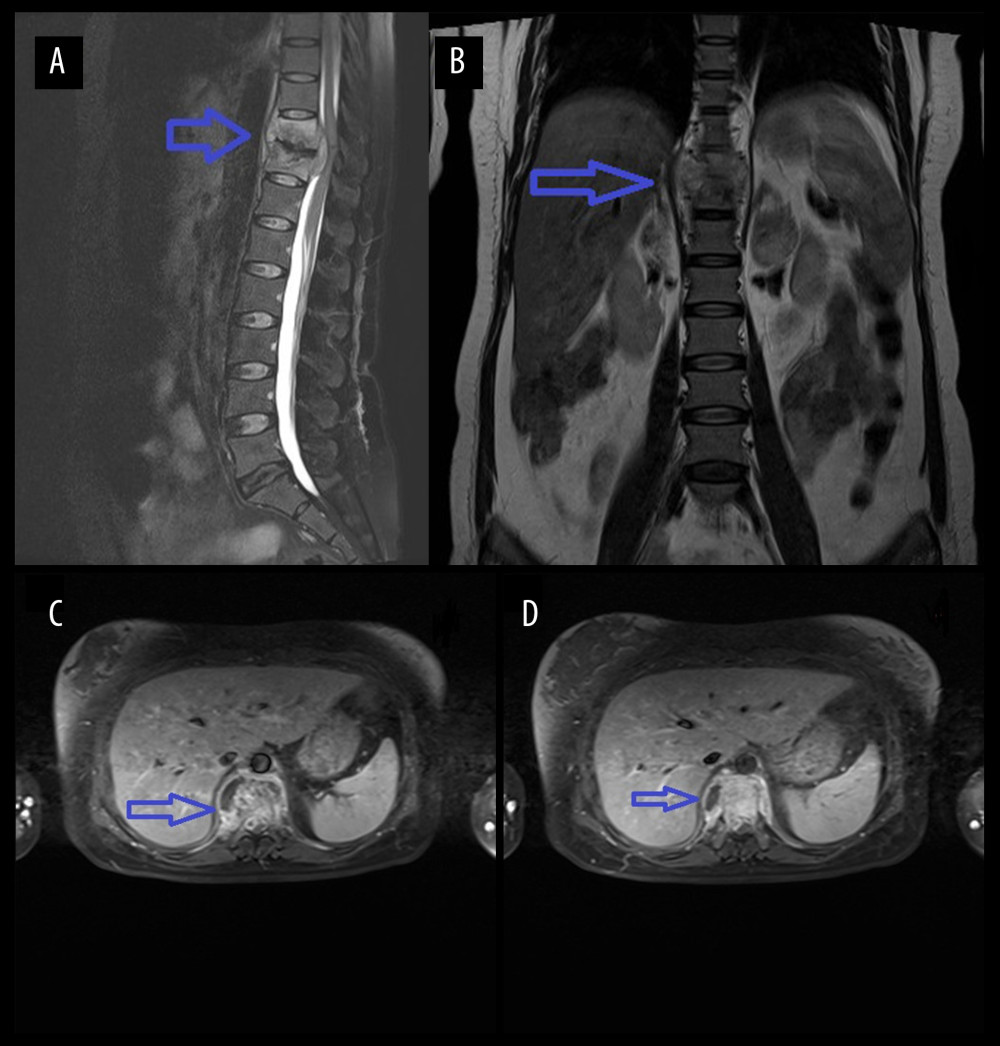 Figure 1. Figure A is the sagittal view of the preoperative thoracic spine MRI. Figure B is the coronal view. Figures C and D are the transverse views of the diseased vertebral body, showing high-signal intensity of the 10th and 11th thoracic vertebrae on T2WI, corresponding to the formation of abscesses in the spinal canal, compressing the spinal cord.
Figure 1. Figure A is the sagittal view of the preoperative thoracic spine MRI. Figure B is the coronal view. Figures C and D are the transverse views of the diseased vertebral body, showing high-signal intensity of the 10th and 11th thoracic vertebrae on T2WI, corresponding to the formation of abscesses in the spinal canal, compressing the spinal cord. 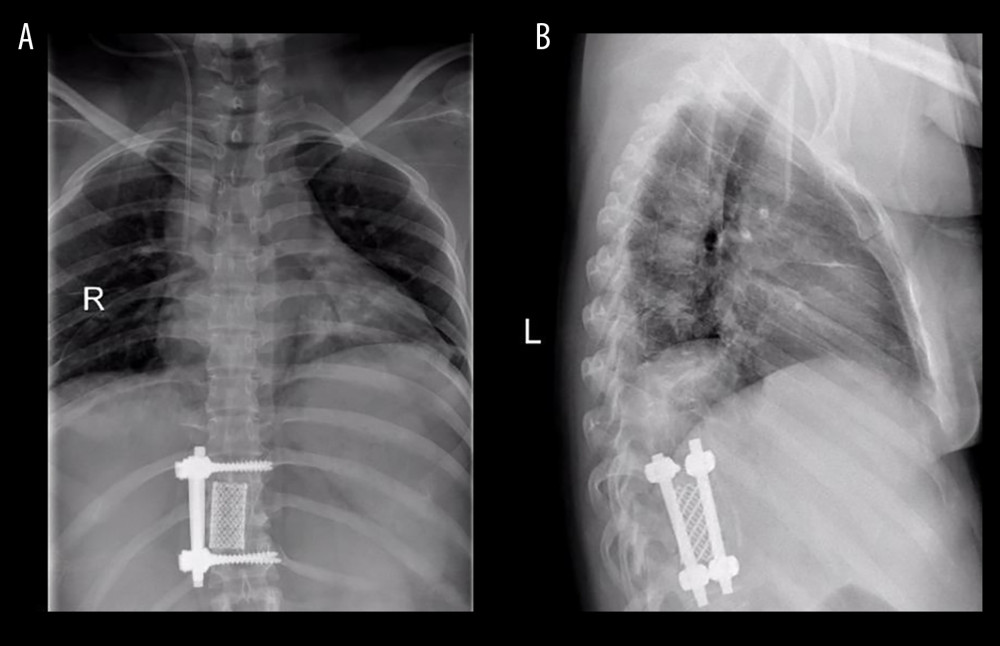 Figure 2. Figure A is the anteroposterior view of the thoracic vertebrae 1 month after operation. Figure B is the lateral view, showing that the titanium cage bone graft between the thoracic 10th and 11th vertebral bodies is well fused and the internal fixation position is good.
Figure 2. Figure A is the anteroposterior view of the thoracic vertebrae 1 month after operation. Figure B is the lateral view, showing that the titanium cage bone graft between the thoracic 10th and 11th vertebral bodies is well fused and the internal fixation position is good. Tables
Table 1. General information of patients.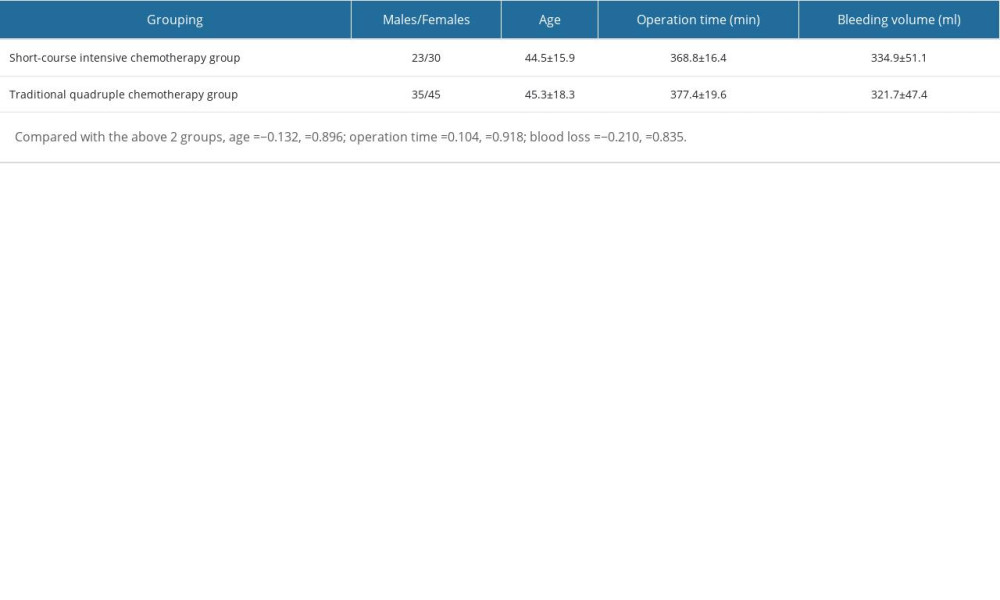 Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups.
Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups. Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.
Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.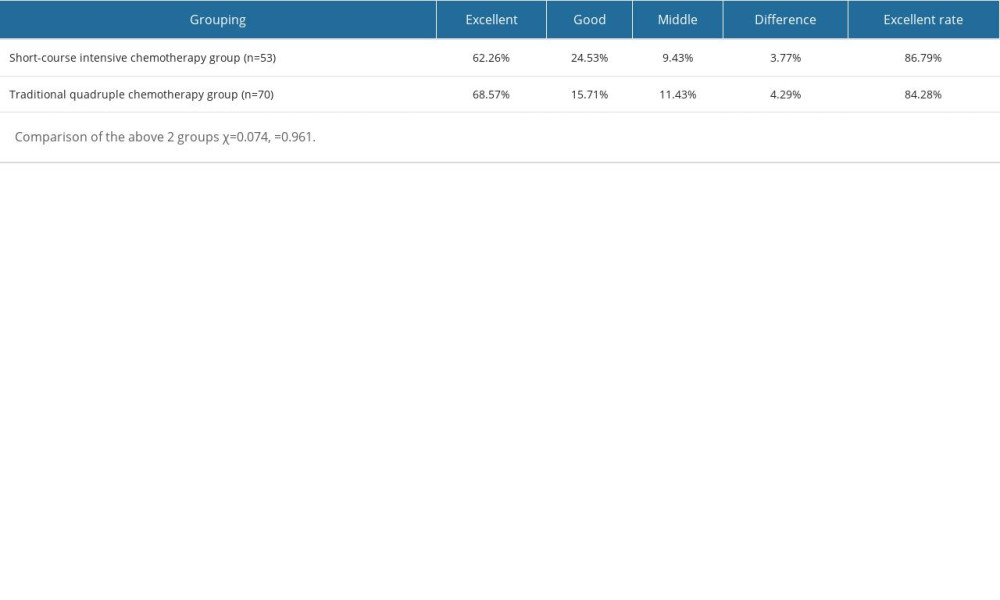 Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group.
Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group.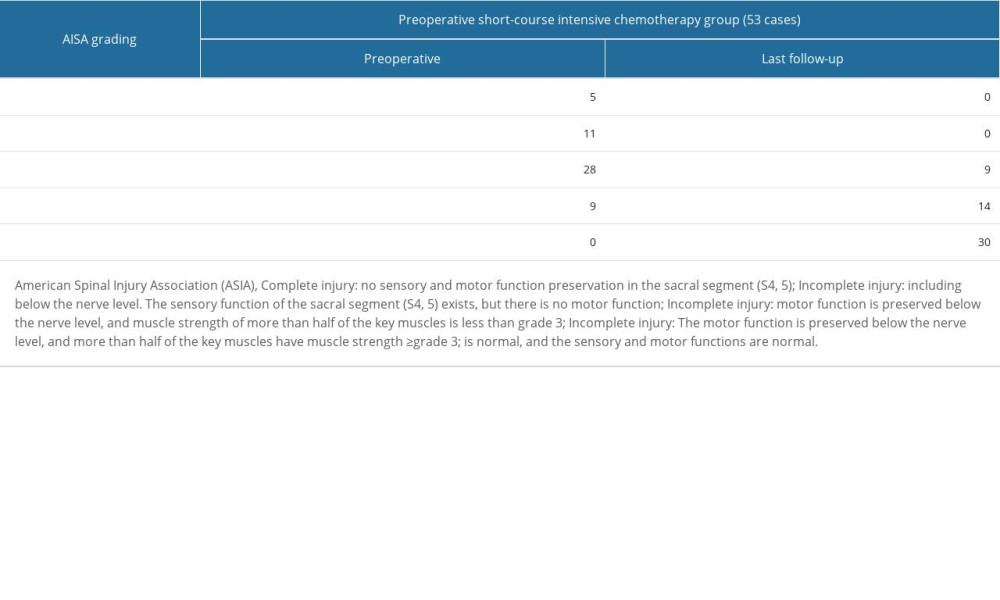 Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients.
Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients.
References
1. Heyde CE, Lübbert C, Wendt S, Spinal tuberculosis: Z Orthop Unfall, 2022; 160; 74-83
2. Chen CH, Chen YM, Lee CW, Early diagnosis of spinal tuberculosis: J Formos Med Assoc, 2016; 115(10); 825-36
3. Yuan B, Zhao Y, Zhou S, Treatment for tuberculosis of the subaxial cervical spine: A systematic review: Arch Orthop Trauma Surg, 2021; 141; 1863-76
4. Dunn RN, Ben HM, Spinal tuberculosis: Review of current management: Bone Joint J, 2018; 100B; 425-31
5. Gao Q, Han C, Romani MD, Posterior-only debridement, internal fixation, and interbody fusion using titanium mesh in the surgical treatment of thoracolumbar tuberculosis with spinal epidural abscess: A minimum 5-year follow-up: BMC Musculoskelet Disord, 2021; 22; 917
6. Wu W, Lyu J, Liu X, Surgical treatment of thoracic spinal tuberculosis: A multicenter retrospective study: World Neurosurg, 2018; 110; e842-e50
7. Heng Y, Xifeng Z, Lin Z, Clinical efficacy of spinal endoscopic treatment of thoracolumbar disc herniation: J Practical Orthoped, 2018(8); 733-36
8. Moon MS, Woo YK, Lee KS, Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines: Spine, 1995; 20; 1910-16
9. Basic Professional Committee of China Anti TB Association: Procedures for bacteriological examination of tuberculosis diagnosis [R], 2012, Beijing, Meeting of Basic Professional Committee of China Anti-TB Association
10. Pang XY, Shen X, Wu P, Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage: Arch Orthop Trauma Surg, 2013; 133; 765-72
11. Liu P, Zhu Q, Jiang J, Distribution of three antituberculous drugs and their metabolites in different parts of pathological vertebrae with spinal tuberculosis: Spine, 2011; 36(20); E1290-E95
12. Jia CG, Gao JG, Liu FS, Efficacy, safety and prognosis of treating neurological deficits caused by spinal tuberculosis within 4 weeks’ standard anti-tuberculosis treatment: A single medical center’s experience: Exp Ther Med, 2020; 19(1); 519-26
13. Shibing Q, Yanzheng S, Weijie D, Progress of clinical diagnosis and treatment of bone and joint tuberculosis and its standardization symposium summary: Chinese J Antituberculosis, 2013; 81-84
14. Benli IT, Acaroğlu E, Akalin S, Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis: Eur Spine J, 2003; 12; 224-34
15. Hongqi Z, Xungang X, Shaohua L: China Med Eng, 2007; 7; 548-51
16. Eminl A, Effect of preoperative chemotherapy on the outcome of surgical treatment of vertebral tuberculosis: Retrospective analysis of 434 cases: Arch Orthop Trauma Surg, 2001; 121; 65-66
17. Zhonglin X, Zhongxian C, Chaohua F, Preoperative short-term chemotherapy combined with anterior single screw rod system in the treatment of thoracolumbar tuberculosis: Chinese J Bone and Joint Surgery; 20135252-57
18. Ma YZ, Cui X, Li HW, Outcomes of anterior and posterior instrumentation under different surgical procedures for treating thoracic and lumbar spinal tuberculosis in adults: Int Orthop, 2012; 6; 299-305
19. Juan L, Jian D, Xilei L, Simple posterior approach and one-stage anterior approach in the treatment of thoracolumbar tuberculosis: Fudan J (Medical Science), 2013; 40(1); 38-43
20. Yin XH, Liu SH, Li JS, The role of costotransverse radical debridement, fusion and postural drainage in the surgical treatment of multisegmental thoracic spinal tuberculosis: A minimum 5-year follow-up: Eur Spine J, 2016; 25; 1047-55
21. Shibing Q, Pay attention to the diagnosis and treatment of tuberculosis and the selection of surgical opportunity for spinal tuberculosis: China Bone Trauma, 2013; 26(7); 533-35
22. Pang Y, Lu J, Huo F, Prevalence and treatment outcome of extensively drug-resistant tuberculosis plus additional drug resistance from the National Clinical Center for Tuberculosis in China: A five-year review: J Infect, 2017; 75(5); 433-40
23. World Health Organization: Treatment guidelines for drug resistant tuberculosis 2016 update, 2016, Geneva, World Health organization
Figures
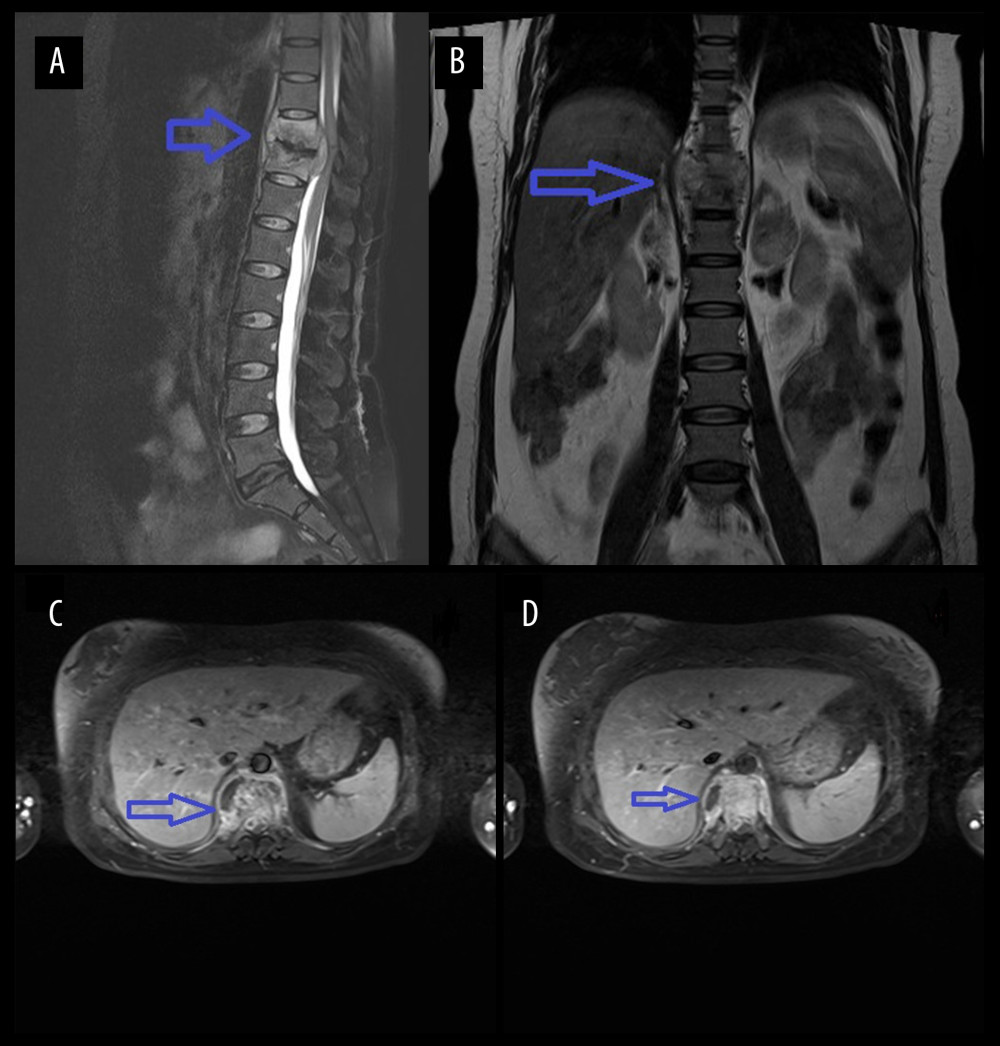 Figure 1. Figure A is the sagittal view of the preoperative thoracic spine MRI. Figure B is the coronal view. Figures C and D are the transverse views of the diseased vertebral body, showing high-signal intensity of the 10th and 11th thoracic vertebrae on T2WI, corresponding to the formation of abscesses in the spinal canal, compressing the spinal cord.
Figure 1. Figure A is the sagittal view of the preoperative thoracic spine MRI. Figure B is the coronal view. Figures C and D are the transverse views of the diseased vertebral body, showing high-signal intensity of the 10th and 11th thoracic vertebrae on T2WI, corresponding to the formation of abscesses in the spinal canal, compressing the spinal cord.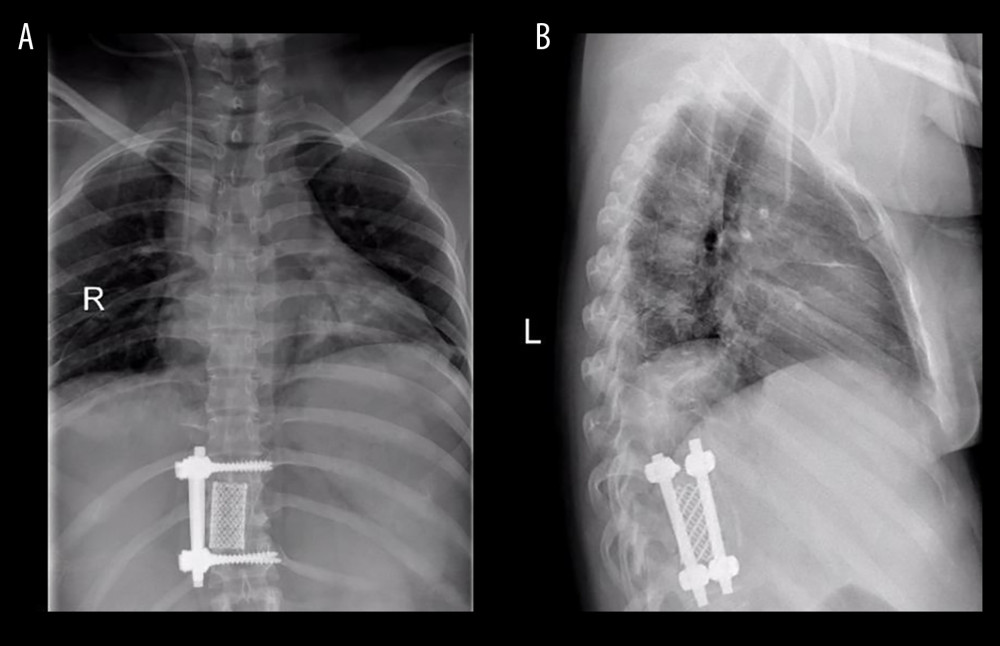 Figure 2. Figure A is the anteroposterior view of the thoracic vertebrae 1 month after operation. Figure B is the lateral view, showing that the titanium cage bone graft between the thoracic 10th and 11th vertebral bodies is well fused and the internal fixation position is good.
Figure 2. Figure A is the anteroposterior view of the thoracic vertebrae 1 month after operation. Figure B is the lateral view, showing that the titanium cage bone graft between the thoracic 10th and 11th vertebral bodies is well fused and the internal fixation position is good. Tables
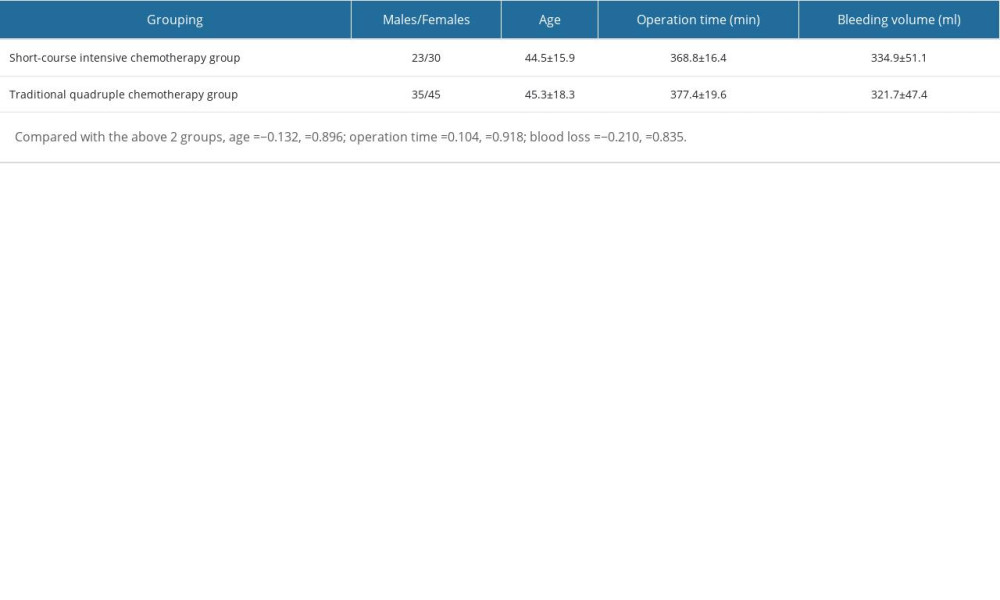 Table 1. General information of patients.
Table 1. General information of patients. Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups.
Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups.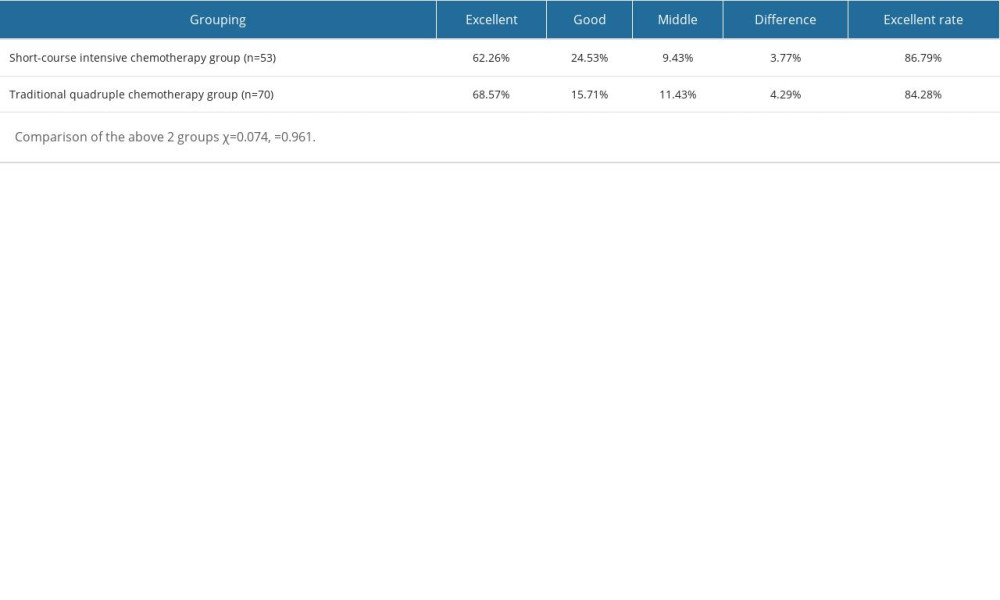 Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.
Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.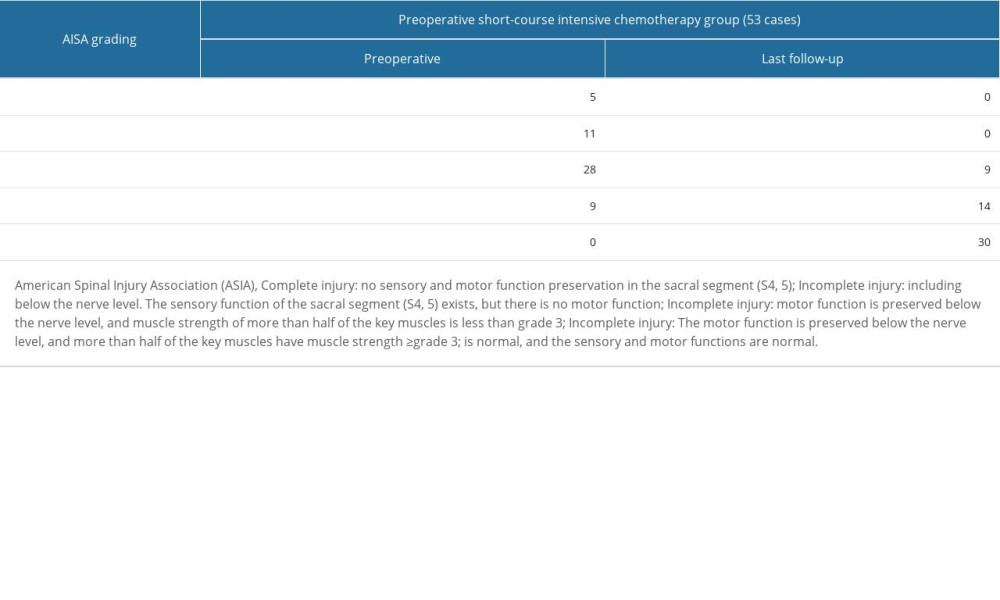 Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group.
Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group. Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients.
Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients.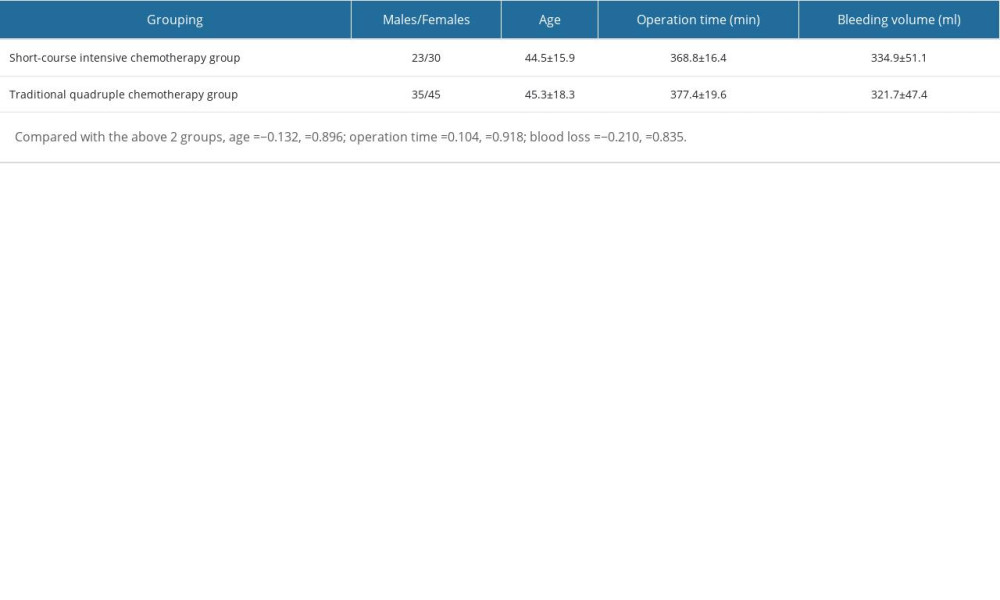 Table 1. General information of patients.
Table 1. General information of patients. Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups.
Table 2. Changes of pain VAS score after operation and last follow-up in 2 groups.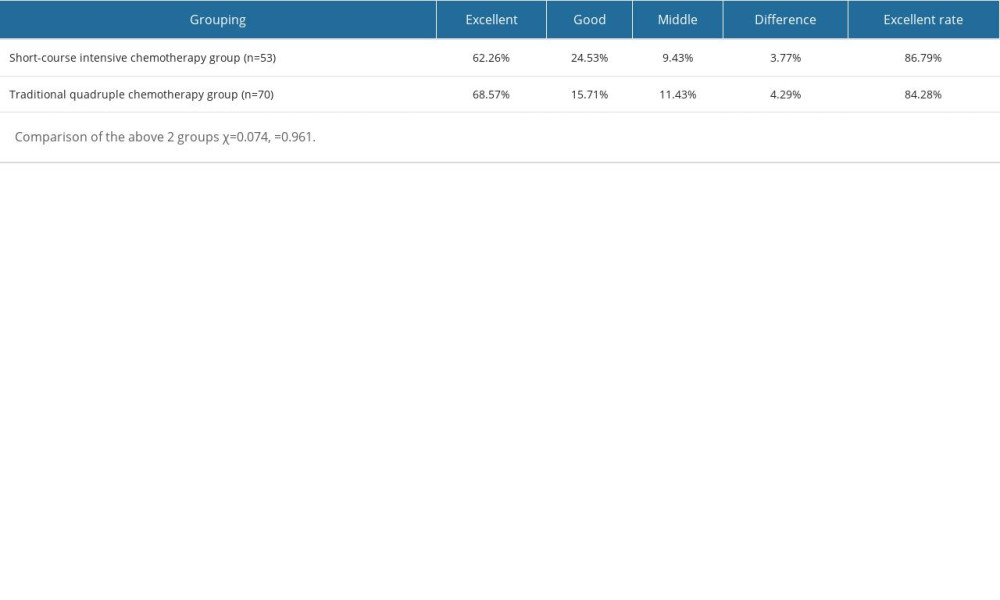 Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.
Table 3. Clinical efficacy evaluation of the 2 groups of patients at the last follow-up.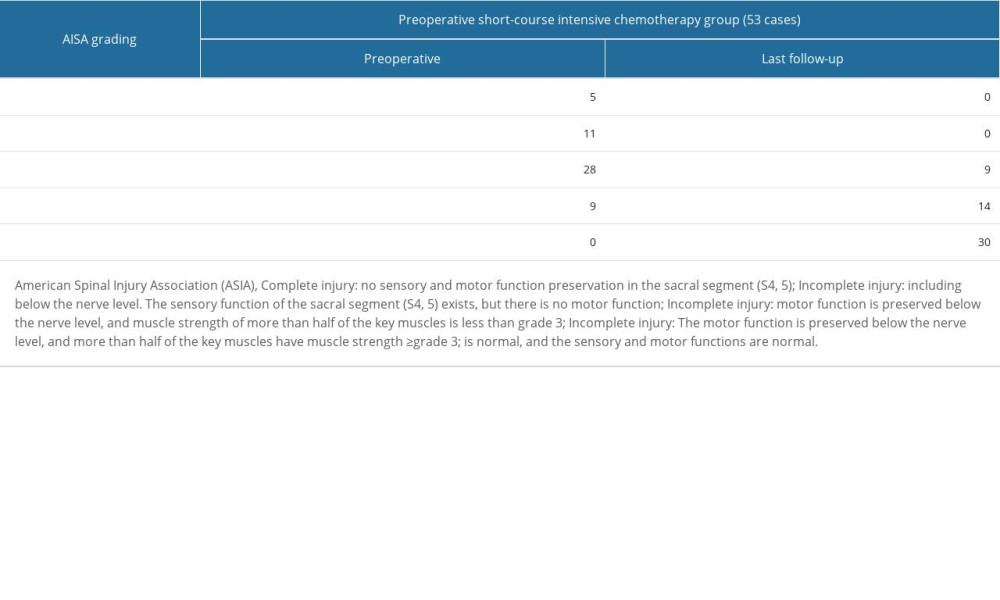 Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group.
Table 4. Changes of neurological function at the last follow-up in the short-course intensive chemotherapy group. Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients.
Table 5. Comparison of bone graft fusion time and tuberculosis recurrence rate between 2 groups of patients. In Press
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








