23 November 2023: Clinical Research
Comparative Analysis of Super-Mini Percutaneous Nephrolithotomy Combined with Flexible Ureteroscopic Lithotripsy versus Flexible Ureteroscopic Lithotripsy Alone for Treating Complex Kidney Stones: A Retrospective Study of 205 Patients
Qi Ding1ABCDE, Hailiang Zhu1BCD, Zhijiang Fan1CD, Feng Li1DE, Wenjian Tu1BC, Xiaohua Jin1CD, Bo Fan1ABCDFG*DOI: 10.12659/MSM.941012
Med Sci Monit 2023; 29:e941012
Abstract
BACKGROUND: This retrospective study aimed to compare outcomes from super-mini percutaneous nephrolithotomy (SMP) combined with flexible ureteroscopic lithotripsy (FURL) and FURL alone in 205 patients with 2.5-4.2 cm diameter complex kidney stones.
MATERIAL AND METHODS: Between January 2018 and December 2022, 92 patients were treated with SMP combined with FURL (group A), and 113 patients were treated with FURL alone (group B). The stone-free rate (SFR), retreatment ratio, operation time, mean decline in hemoglobin level, postoperative pain visual analogue scale (VAS), and postoperative hospitalization time and complications were analyzed and compared between the 2 groups.
RESULTS: The SFR 3 days after the operation was 85.87% in group A, which was significantly higher than that in group B (72.57%) (P=0.021). The rate of retreatment in group A (3.26%) was significantly lower than that in group B (10.62%) (P=0.044). The SFR after 90 days was higher in group A (94.57%) than in group B (90.27%) (P=0.254). The mean decrease in hemoglobin, postoperative hospitalization duration, and VAS score 6 hours after the operation were all significantly higher in group A than in group B (P<0.05). However, there was no significant difference in operation time, VAS score at 12 and 24 hours after the operation, and complication rate.
CONCLUSIONS: In the treatment of complex renal stones, compared with FURL, SMP combined with FURL in the oblique supine lithotomy position has the advantages of a higher early SFR with no increased risk of complications.
Keywords: Endoscopes, nephrolithiasis, Nephrolithotomy, Percutaneous, Ureteroscopes
Background
Complex kidney stones generally refer to stones with a diameter of more than 2.5 cm, and include multiple kidney stones, staghorn stones, or stones with presentation complicated by renal anatomical abnormalities, such as solitary kidney stones, horseshoe kidney stones, or sponge kidney stones [1]. For kidney stones larger than 2 cm in diameter, percutaneous nephrolithotomy (PCNL) remains the preferred choice recommended by the European Association of Urology guidelines [2]. Flexible ureteroscopic lithotripsy (FURL) can be considered when there are contraindications for PCNL [2]. However, one meta-analysis found FURL to be comparable to PCNL, in terms of stone-free rate (SFR), for the treatment of kidney stones larger than 2 cm, without increasing the risk of complications [3]. FURL has become one of the safest and most effective treatment methods for multiple kidney stones in recent years [4]. Nevertheless, FURL also has some shortcomings, such as decreased removal efficiency for lower calyceal stones [5]. Super-mini percutaneous nephrolithotomy (SMP) was first reported by Zeng et al in 2016 [6]. The surgical system consists of a 7F nephroscope and a continuous negative pressure suction nephroscope sheath [6]. SMP is safe and effective for the treatment of kidney stones less than 2.5 cm, especially for lower calyceal stones and for those patients for whom FURL is not suitable [6]. Compared with standard-channel and microchannel PCNL, SMP causes less intraoperative trauma and has better safety [7]. For complex kidney stones, it is often necessary to establish 2 or more channels to improve the SFR [8]. The increase in the number of channels aggravates renal parenchyma injury and increases the incidence of complications such as bleeding [9]. To improve the SFR and reduce the complications of multi-tract PCNL, some surgeons have used PCNL combined with FURL to treat kidney stones in the prone position [10,11].
SMP combined with FURL in the treatment of complex kidney stones may make up for these deficiencies of FURL. This retrospective study aimed to compare outcomes from SMP combined with FURL vs FURL alone, in 205 patients with 2.5–4.2 cm diameter complex kidney stones.
Material and Methods
STUDY SUBJECTS:
The present study was reviewed and approved by the Institutional Ethics Committee of the Changshu Hospital Affiliated to Soochow University (Approval No. 2017–96). The clinical data for the 205 patients with 2.5–4.2 cm complex kidney stones admitted to the First People’s Hospital of Changshu between January 2018 and December 2022 were analyzed retrospectively. Ninety-two patients underwent SMP combined with FURL (group A) and 113 patients underwent FURL only (group B). Inclusion criteria were: (1) unilateral complex renal stones confirmed by Doppler ultrasound, kidney-ureter-bladder (KUB) film, and computer tomography (CT); (2) stone size exceeding 25 mm; (3) patient age range from 18 to 85; (4) for patients in group A, completion of the operation in the oblique supine lithotomy position. Exclusion criteria were: (1) complex renal calculi with severe urinary system infection that was difficult to control; (2) solitary kidney or serum creatinine >177 μmol/L; (3) body mass index (BMI) ≥35 kg/m2; (4) severe abnormal coagulation function; (5) severe spinal deformity or left kidney stone with splenomegaly.
Patients with a preoperative urinary tract infection were treated with antimicrobial drugs based on bacterial culture and drug sensitivity tests.
SURGICAL DEVICES AND MATERIALS:
The following surgical devices and materials were used in the study: F8.5/9.8 rigid ureteroscope (Storz, Germany), ureteral access sheath (UAS) with F12 inner diameter (Cook, USA), electronic flexible uretero-renoscope (Storz, Germany), 200/550 μm holmium laser fiber (Lumenis, USA), stone-collecting retrieval basket (Cook, USA), 60 W holmium laser (Lumenis, USA), and super-mini percutaneous nephroscope (HAWK, China).
SURGICAL PROCEDURE:
All procedures were performed by the same surgical team. The team leader was Fan Bo. Team members are Jin Xiaohua and Zhu Hailiang. All the key steps of the operation were performed by Fan Bo.
GROUP A SURGICAL PROCEDURE:
For group A, general anesthesia was used. First, the patient was supine with the lower edge of his or her buttocks against the lower third of the operation table. The patient was then turned to the healthy side, with his or her back as close as possible to the edge of the operation table. The arm on the healthy side was stretched, while that on the affected side was fixed on a hand frame, with the waist cushioned using a lumbar pad. The patient was tilted back 45° into an oblique supine position. The operation site in the lumber region was then exposed. The leg on the affected side was bent and placed on a leg plane. The leg on the healthy side was flexed, abducted, and placed on a horizontal board. At this point, the patient was in the oblique supine lithotomy position.
A Storz rigid ureteroscope was used to examine the ureter on the affected side. After inserting the guide wire, a Cook UAS with an F12 inner diameter was inserted along the guide wire, followed by insertion of the Storz electronic flexible ureteroscope. B mode ultrasound was used to observe the stones, hydronephrosis, and calyceal and perirenal organs of the kidney. Under real-time ultrasound guidance and direct vision from the ureteroscope, a vertical puncture was performed at the highest point of the fornix of the target calyceal below the 11th or 12th costal margin. The channel was expanded step by step to F14, then an F14 metal sheath was inserted. SMP was performed using a 550 μm holmium laser fiber. The energy of the holmium laser was set to 1.5~2.0 J, the frequency to 20~30 Hz, and power to 30~60 W. Stones detected in the visual field were cleared, then a flexible ureteroscope was retrograde inserted to examine the renal pelvis and calyces, followed by entry into the calyces which could not be reached by the percutaneous renal channel.
Some large stones were displaced into the renal pelvis through a stone basket and then removed using the percutaneous technique, while small stones were crushed by a 200 μm fiber holmium laser, with a lithotripsy energy of 0.8 J, frequency of 30 Hz, and power of 24 W. The stones were flushed out of the calyx through the PCNL channel by increasing the pressure of flushing. After all the stones had been cleared, an F6/7 ureteral stent was inserted.
GROUP B SURGICAL PROCEDURE:
For group B, after general anesthesia, patients were placed in the lithotomy position. A Storz rigid ureteroscope was used to examine the entire affected ureter up to the posterior renal pelvis, followed by insertion of a guide wire. A Cook UAS with F12 inner diameter was placed along the guide wire, followed by insertion of a Storz electronic flexible ureteroscope. After entering the pelvis, the calyces were examined successively to find the kidney stones. A 200 μm holmium laser fiber was used to fragment the stones. The lithotripsy energy was set at 0.8 J, frequency at 30 Hz, and power at 24 W. A stone basket was used to extract the large stone fragments after lithotripsy. All the calyces were examined to confirm that there were no large residual stones. An F6/7 double J tube was placed after the operation.
OUTCOME MEASURES:
The following data were recorded for statistical analysis: operation time, decline in hemoglobin level, postoperative hospitalization time, postoperative visual analogue scale (VAS) score, complications according to the Clavien complication grading system, SFR, retreatment ratio, and other perioperative data. KUB or CT was performed 3 days and 90 days after the operation to evaluate the SFR. KUB was used for postoperative examination of X-ray-positive stones. CT was used for X-ray-negative stones. Of the 205 patients included, 11 had X-ray-negative stones, including 6 in group A and 5 in group B. The absence of residual stones on the KUB or CT, or presence of only residual stones <4 mm in diameter, was classified as stone clearance. The efficiency quotient, combined with stone clearance and the proportion of additional treatment required after the initial surgical treatment, was calculated [12].
STATISTICAL ANALYSIS:
The measurement data were analyzed by STATA 14.0. Normally distributed continuous data were expressed as mean±standard deviation (χ̄±s) and analyzed by t-test. Non-normally distributed continuous data were expressed as the median (Q1–Q3) and analyzed by Wilcoxon rank-sum (Mann-Whitney) test. Categorical data were expressed as percentages and analyzed using the χ2 test or Fisher precise probability method. A
Results
CHARACTERISTICS OF STUDY SUBJECTS:
The mean age in group A was 55.71±11.64, similar to that in group B (55.92±12.06) (P=0.902). No difference was observed in terms of gender composition between the 2 groups (P=0.264). In addition, there were no significant differences in stone size, body side distribution, BMI, CT value of stones, comorbidities, degree of hydronephrosis, urine culture positivity rate, and surgical history of urinary stones, between the 2 groups (P>0.05) (Table 1).
EFFICACY AND SAFETY ANALYSIS FOR THE 2 GROUPS:
The SFR 3 days after the operation was 85.87% in group A, which was significantly higher than that in group B (72.57%) (P=0.021). In group B, 12 cases (10.62%) needed either a further FURL (3 cases), extracorporeal shock wave lithotripsy (ESWL) (7 cases), or SMP (2 cases) to treat residual stones. The retreatment rate in group B was higher than that in group A (3.26%). In addition, the SFR after 90 days in group A was 94.57%, which is higher than that of group B (90.27%) (Table 2).
In group B, the average postoperative hemoglobin reduction (11.5 g/L; range: 6.0–19.0 g/L), postoperative hospital stay (6.0 days; range: 4.0–8.0 days), and VAS score at 6 hours after the operation (2.20±0.74) were significantly higher than those in group A (7.0 g/L; range: 0–12.0 g/L; 3.0 days; range: 2.0–3.0 days; and 1.93±0.62, respectively) (P<0.05). As shown in Tables 2 and 3, the efficiency quotient of group A was 83.16%, which was higher than that in group B (65.61%). The operation time (83.59±8.36 min), VAS score at 12 hours after the operation (1.01±0.56), VAS score at 24 hours after the operation (0.16±0.37), and complication rate (30.43%) in group A did not differ significantly from the corresponding values in group B (81.42±8.38 min; 0.92±0.50; 0.12±0.32, and 29.20%, respectively).
Discussion
This study showed that, compared with FURL, SMP combined with FURL in the oblique supine lithotomy position has the advantage of higher early SFR without increasing the risk of complications in the treatment of complex renal stones.
At present, PCNL is the first choice for treating complex renal stones in clinical practice [13]. The guidelines of the American Society of Urology recommend that PCNL for complex kidney stones often requires more than 2 channels [14]. However, multi-channel PCNL increases the occurrence of many complications such as bleeding and infection during and after an operation [15,16]. In 2005, Marguet et al reported the simultaneous combined use of flexible ureteroscopy and PCNL in the management of complex renal calculi [17]. Some studies have reported the use of mini PCNL (mPCNL) or PCNL combined with anterograde FURL in the prone position for the treatment of renal calculi [18,19]. Leng et al performed mPCNL combined with retrograde FURL for 44 patents with staghorn calculi in the oblique supine lithotomy position [20]. Gao et al conducted a retrospective cohort analysis that included 45 patients with complex renal stones treated with SMP combined with retrograde FURL in the prone position [10]. However, to date, there is no relevant report on the treatment of complex renal calculi by SMP combined with flexible ureteroscopy in the oblique supine lithotomy position. Thus, we conducted this retrospective study.
This study showed that the SFR 3 days after the operation in group A was 85.87%, significantly higher than that in group B (72.57%). This result may be related to the large size of the renal stones and the long stone-drainage process after FURL. In group A, for kidney stones that were difficult to reach by SMP, SMP lithotripsy was performed after displacing the stone with a stone basket under flexible ureteroscope. Some stones could be taken out through the percutaneous renal channel during the operation, which improved the primary SFR. Gao et al reported that 45 patients with complex renal stones underwent combined SMP and FURL in the prone position. The SFR 3 days after the procedure was 97.8%, which was higher than that in our study, possibly related to the smaller stones in their group. This difference in SFR may also be related to a difference in stone hardness. The CT values of the stones were not specified in their paper [10].
In our study, the rate of retreatment in group B (10.62%) was significantly higher than that in group A (3.26%). The SFR 90 days after the operation was 94.57% in group A, higher than that measured in group B (90.27%). Hamamoto et al performed mPCNL combined with FURL for 60 patients with renal calculi of 34.6±2.3 mm in size. The initial SFR was 81.7%, and 11.67% of the patients needed ancillary treatments including PCNL, ESWL, and ureteroscopy. The final SFR increased to 86.7% [11]. The higher retreatment rate and lower SFR in their study may be related to larger sizes of stones in their patients. Our study showed that postoperative hospitalization time in group A was significantly longer than that in group B (
The decrease in hemoglobin levels after the operation in group A was significantly higher than that in group B, which is similar to the results reported by Gao et al [10]. This may be related to the percutaneous renal puncture, as bleeding caused by renal puncture is inevitable. Compared with standard-channel PCNL or microchannel PCNL, the puncture channel of SMP was smaller and the amount of bleeding was relatively lower. Furthermore, SMP combined with FURL avoids the increase in bleeding risk conferred by the establishment of a multi-channel or large-scale swinging of the nephroscope. In this study, only one patient in group A received blood transfusion after surgery, indicating that bleeding during and after SMP combined with FURL could be controlled.
The length of hospital stay for PCNL combined with FURL varies in the literature. Gao et al used SMP combined with FURL to treat patients with stones of 2.6±1.2 cm, resulting in a length of hospital stay of 7.36±1.77 days [10]. Hamamoto et al treated kidney stones larger than 2 cm with mPCNL combined with FURL, and the hospital stay was 7.0±0.6 days [11]. Our results showed a hospital stay of 6.0 (range, 4.0–8.0) days, similar to the studies mentioned above. However, Leng et al reported that mPCNL combined with FURL for kidney stones of 5.171±0.942 cm resulted in a hospital stay of 9.659±3.524 days [20]. Goktug et al showed that PCNL combined with FURL to treat kidney stones with a stone surface area of 1187.13±190.05 cm2 resulted in a hospital stay of 2.39±0.9 days [18]. Guo et al used ultra-mini PCNL combined with FURL to treat pediatric patients with multiple kidney stones. The average stone size was 2.0±1.0 cm, and the length of hospitalization was 4.85±1.39 days [21]. Differences in stone size, surgical method, surgical position, age, race, BMI, and other parameters are all possible reasons for the differences in hospital stay length.
The VAS pain score 6 hours after the operation in group A was higher (2.20±0.74) than that in group B (1.93±0.62). This was attributable to the invasive nature of SMP, although the pain gradually declined over time. Compared with standard PCNL, SMP has a significantly lower incidence of postoperative pain [22]. In addition, our results showed no significant difference between the 2 groups for VAS scores 12 and 24 hours after the operation, with the proportion of VAS scores ≥4 points suggesting that the degree of postoperative pain in group A was slight and controllable.
The complication rate in group A was 30.43%, which was similar to that in group B (29.2%). The incidence of complications of SMP combined with FURL in the study by Gao et al (57.8%) was significantly higher than that in our study [10]. The reason may be related to the fact that, in their study, 28.9% of the patients suffered from postoperative pain, a percentage that was significantly higher than ours (8.7%). However, their study did not provide a definition of pain, so it may not be comparable to our study. Our study showed that the incidence of fever exceeding 38.5 degrees after the combined technique operation was 6.52%, which is similar to the findings of Gao et al (8.9%) [10]. Notably, this was lower than that in the FURL group (11.50%). Although the difference was not statistically significant, a relevant factor may be the relatively low pressure in the renal pelvis during the treatment of complex renal stones using the combined technique. When SMP or FURL is performed, the other endoscope can be withdrawn, resulting in the perfusion fluid flowing out through the UAS or percutaneous nephroscope channel. This greatly lowers pressure in the renal pelvis during the operation, thereby reducing the absorption of perfusion fluid and risk of infection.
Our study showed that the operation time in the SMP combined with FURL group was 83.59±8.36 minutes, which was higher than that in the FURL group (81.42±8.38 minutes), and the difference was borderline significant. The reasons for the slight difference in operation time between the 2 groups may be as follows. First, SMP combined with FURL was performed in the oblique supine lithotomy position, without changing the position during the operation, which saved time to some extent. Second, the power of the SMP was 30–60 W, which is higher than the 24 W of FURL, and the crushing efficiency is higher, which can offset the added time caused by the SMP puncture. However, the sample size included in our study was small and more cases will be included in the future to obtain more realistic results.
Most of the published articles on this subject have reported that PCNL, mPCNL, or SMP combined with FURL were performed in the prone position [10,11,18,19]. The oblique supine lithotomy position has the following advantages. First, compared with the prone position, it has no influence on the respiratory and circulatory systems, and is convenient for airway management during general anesthesia. Second, SMP and FURL can be performed simultaneously without changing the position of the body during the operation, which saves operation time. Third, in the oblique supine position, the percutaneous renal channel is parallel to the horizontal plane, which is convenient for drainage of lavage fluid and stone fragments. This also reduces pressure in the renal pelvis and reduces the risk of infection.
Our study has the following limitations. First, due to the fact that this is a retrospective study, there may be selection bias involved. Second, the sample size was relatively small and this was a single-center study, so the results need to be interpreted with caution. Third, we did not perform the SMP combined with FURL in the prone position in this study, so no comparison could be made between surgery in the prone position and surgery in the oblique supine lithotomy position. Fourth, the postoperative examination was not standardized to a single examination method, which may lead to bias in the results. Fifth, lack of data on the treatment of complex kidney stones by SMP makes it impossible to compare SMP combined with FURL with SMP alone to further illustrate the benefits of the combined technique.
Conclusions
Compared with simple FURL, the combined technique of SMP and FURL in the oblique supine lithotomy position has a higher early SFR without increasing the risk of complications, and is safe and effective in the treatment of complex renal calculi. Multicenter studies with a larger number of cases are necessary in the future to verify our results.
Tables
Table 1. Comparison of clinical data for patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and clinical data for those who underwent FURL alone (Group B) (n=113).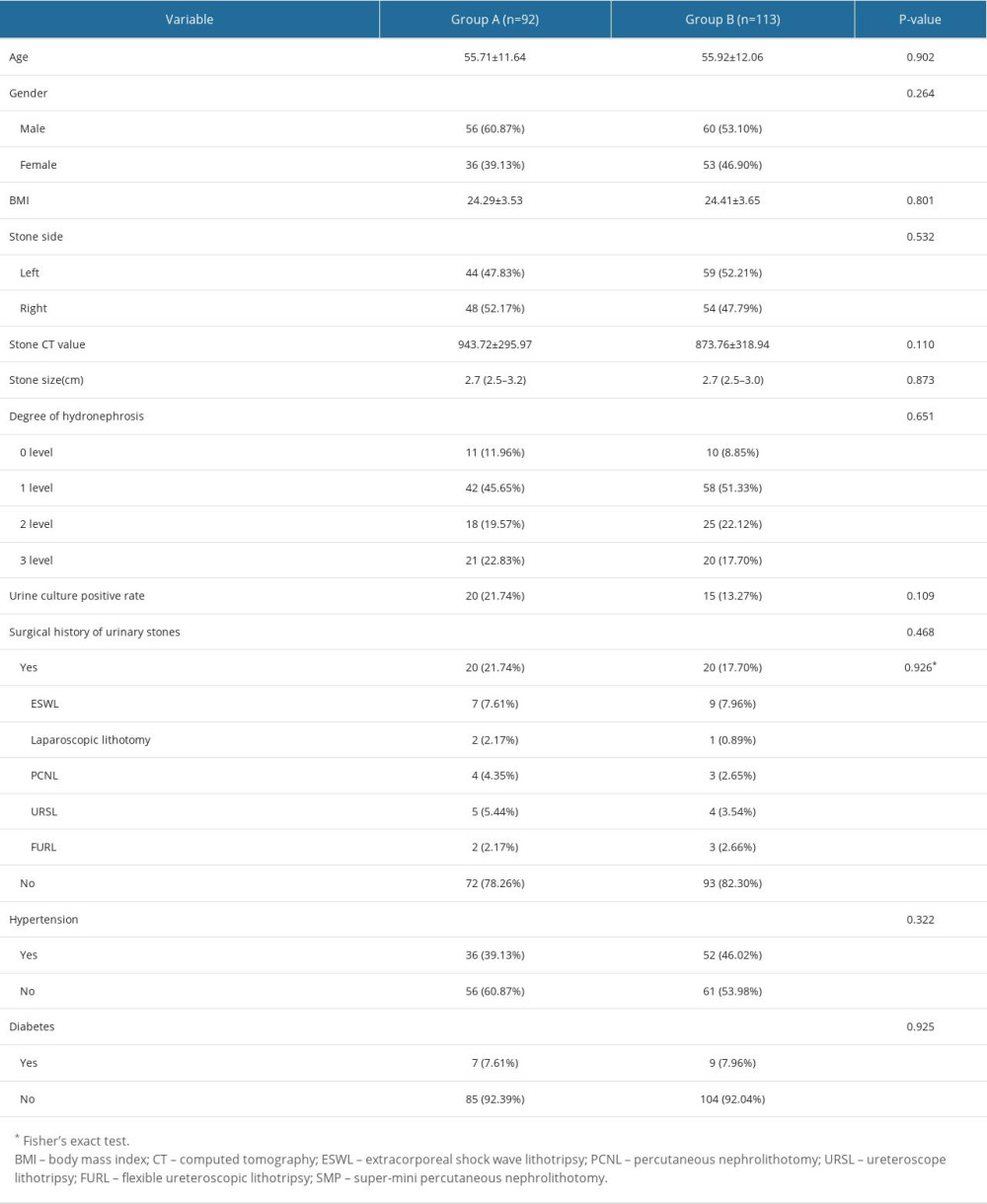 Table 2. Comparison of the peri-operative indices between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).
Table 2. Comparison of the peri-operative indices between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).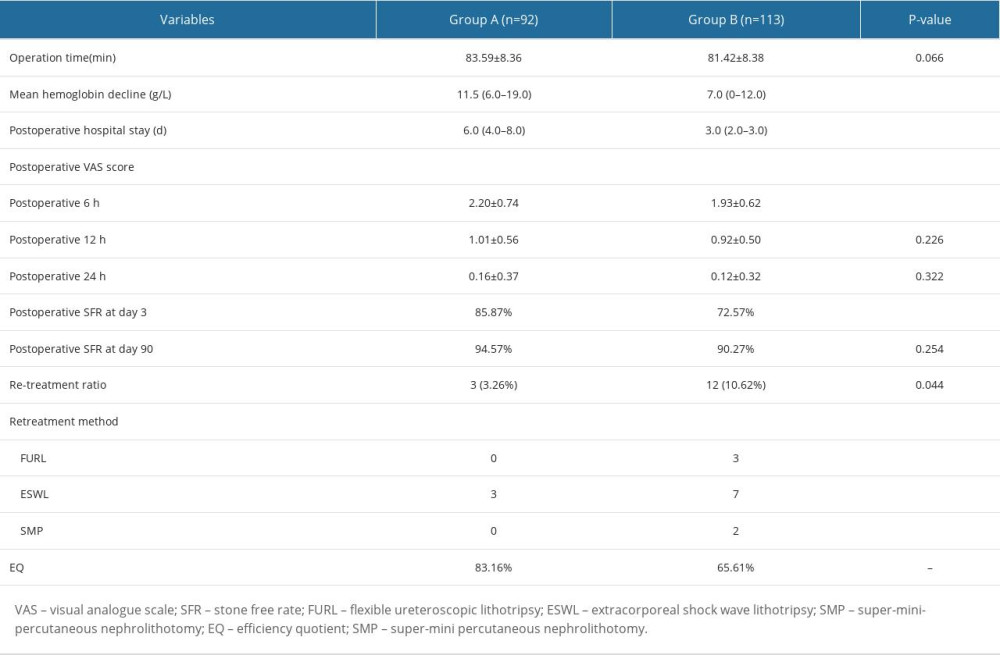 Table 3. Comparison of postoperative complications between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).
Table 3. Comparison of postoperative complications between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).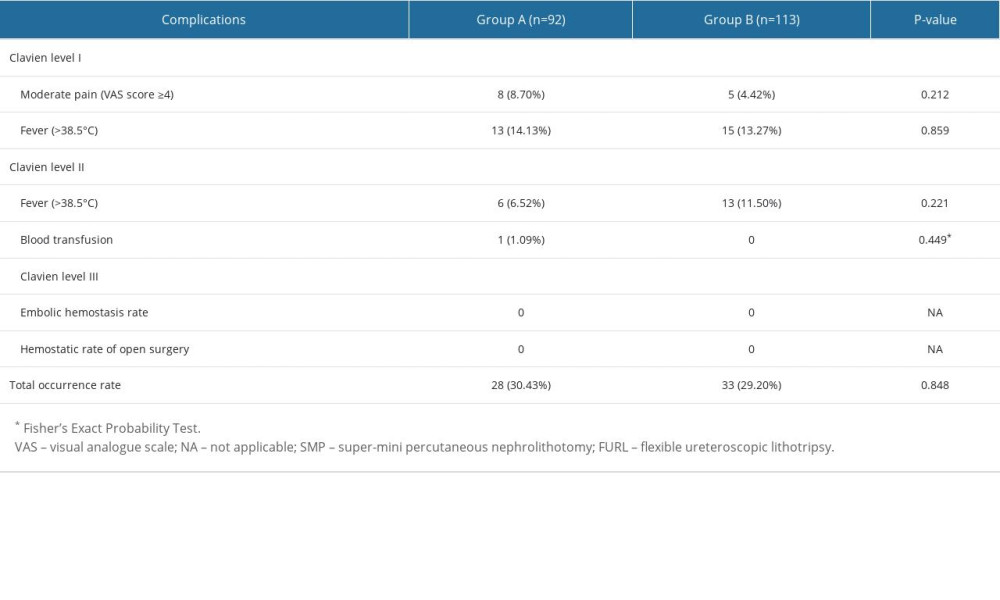
References
1. Wu JP: Wu Jieping Urology, 2004, Jinan, Shandong Science and Technology Press
2. Skolarikos A, Jung H, Neisius A, Arnhem, The Netherlands, EAU Guidelines Office Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Urolithiasis-2023.pdf
3. Fernández Alcalde ÁA, Ruiz Hernández M, Gómez Dos Santos V, Comparison between percutaneous nephrolithotomy and flexible ureteroscopy for the treatment of 2 and 3 cm renal lithiasis: Actas Urol Esp (Engl Ed), 2019; 43(3); 111-17
4. Doizi S, Traxer O, Flexible ureteroscopy: Technique, tips and tricks: Urolithiasis, 2018; 46(1); 47-58
5. Knoll T, Super-, perfect-, ultra-, micro-, mini-, …: does anybody benefit from miniaturized percutaneous nephrolithotomy?: World J Urol, 2018; 36(2); 319-20
6. Zeng G, Wan S, Zhao Z, Super-mini percutaneous nephrolithotomy (SMP): A new concept in technique and instrumentation: BJU Int, 2016; 117(4); 655-61
7. Zhao Z, Tuerxu A, Liu Y, Super-mini PCNL (SMP): Material, indications, technique, advantages and results: Arch Esp Urol, 2017; 70(1); 211-16
8. Wu J, He S, Wang H, Efficacy and economy of two-stage percutaneous nephrolithotomy for complex renal calculi: Arch Esp Urol, 2022; 75(10); 862-66
9. Wang Z, Feng D, Cao D, Zhang Y, Wei W, Comparison of safety and efficacy between single-tract and multiple-tract percutaneous nephrolithotomy treatment of complex renal calculi: A systematic review and meta-analysis: Minerva Urol Nephrol, 2021; 73(6); 731-38
10. Gao H, Zhang H, Wang Y, Treatment of complex renal calculi by digital flexible ureterorenoscopy combined with single-tract super-mini percutaneous nephrolithotomy in prone position: A retrospective cohort study: Med Sci Monit, 2019; 25; 5878-85
11. Hamamoto S, Yasui T, Okada A, Endoscopic combined intrarenal surgery for large calculi: simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy: J Endourol, 2014; 28(1); 28-33
12. Clayman R, McClennan B, Garvin T, Lithostar: An electromagnetic, acoustic shock wave unit for extracorporeal lithotripsy: J Endourol, 1989; 3; 307-13
13. Ghani KR, Andonian S, Bultitude M, Percutaneous nephrolithotomy: Update, trends, and future directions: Eur Urol, 2016; 70(2); 382-96
14. Pearle MS, Goldfarb DS, Assimos DG, Medical management of kidney stones: AUA guideline: J Urol, 2014; 192(2); 316-24
15. Liang T, Zhao C, Wu G, Multi-tract percutaneous nephrolithotomy combined with EMS lithotripsy for bilateral complex renal stones: Our experience: BMC Urol, 2017; 17(1); 15
16. Desai M, Ganpule A, Manohar T, “Multiperc” for complete staghorn calculus: J Endourol, 2008; 22(9); 1831-33 discussion 1841
17. Marguet CG, Springhart WP, Tan YH, Simultaneous combined use of flexible ureteroscopy and percutaneous nephrolithotomy to reduce the number of access tracts in the management of complex renal calculi: BJU Int, 2005; 96(7); 1097-100
18. Goktug G, Karakoyunlu N, Sener NC, Standard percutaneous nephrolithotomy alone versus in combination with intraoperative anterograde flexible nephroscopy for staghorn stones: A retrospective study: Kaohsiung J Med Sci, 2015; 31(11); 568-71
19. Mishra DK, Agrawal MS, Use of a novel flexible mini-nephroscope in minimally invasive percutaneous nephrolithotomy: Urology, 2017; 103; 59-62
20. Leng S, Xie D, Zhong Y, Huang M, Combined single-tract of minimally percutaneous nephrolithotomy and flexible ureteroscopy for staghorn calculi in oblique supine lithotomy position: Surg Innov, 2018; 25(1); 22-27
21. Guo J, Yang WZ, Zhang Y, Ultramini nephrostomy tract combined with flexible ureterorenoscopy for the treatment of multiple renal calculi in paediatric patients: Korean J Urol, 2015; 56(7); 519-24
22. Guddeti RS, Hegde P, Chawla A, Super-mini percutaneous nephrolithotomy (PCNL) vs standard PCNL for the management of renal calculi of <2 cm: A randomised controlled study: BJU Int, 2020; 126(2); 273-79
Tables
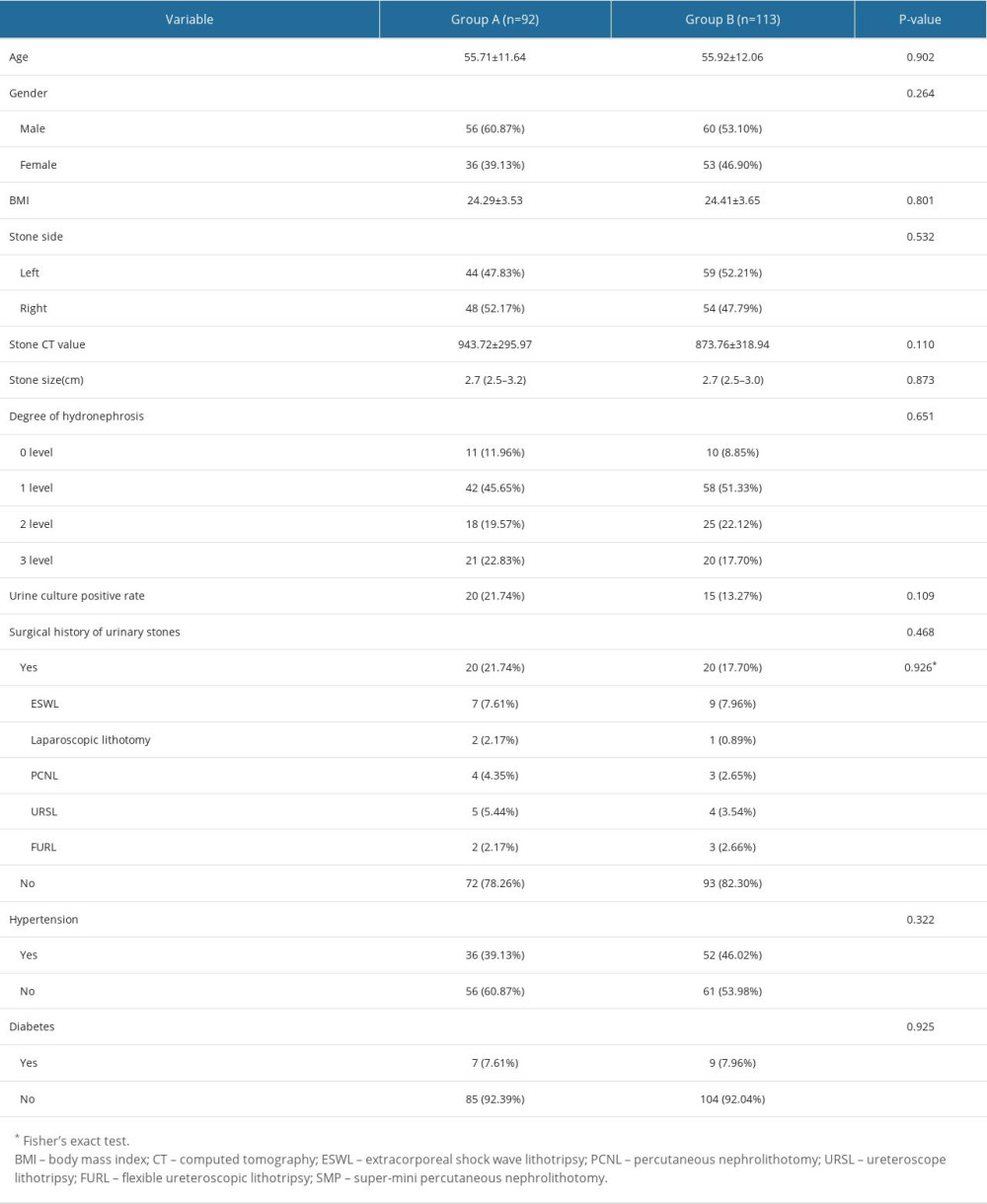 Table 1. Comparison of clinical data for patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and clinical data for those who underwent FURL alone (Group B) (n=113).
Table 1. Comparison of clinical data for patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and clinical data for those who underwent FURL alone (Group B) (n=113).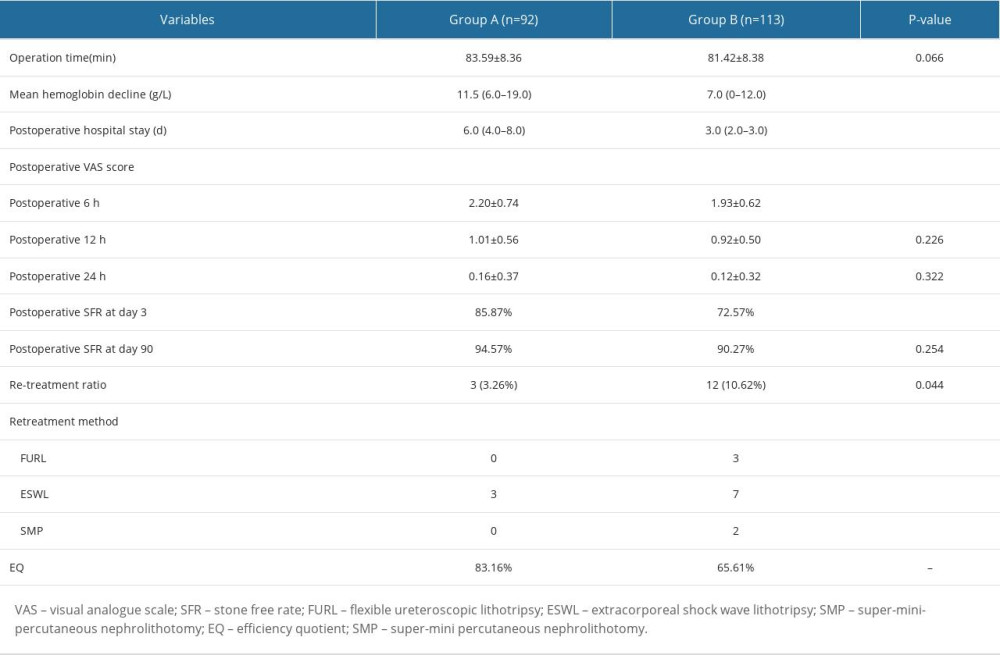 Table 2. Comparison of the peri-operative indices between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).
Table 2. Comparison of the peri-operative indices between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).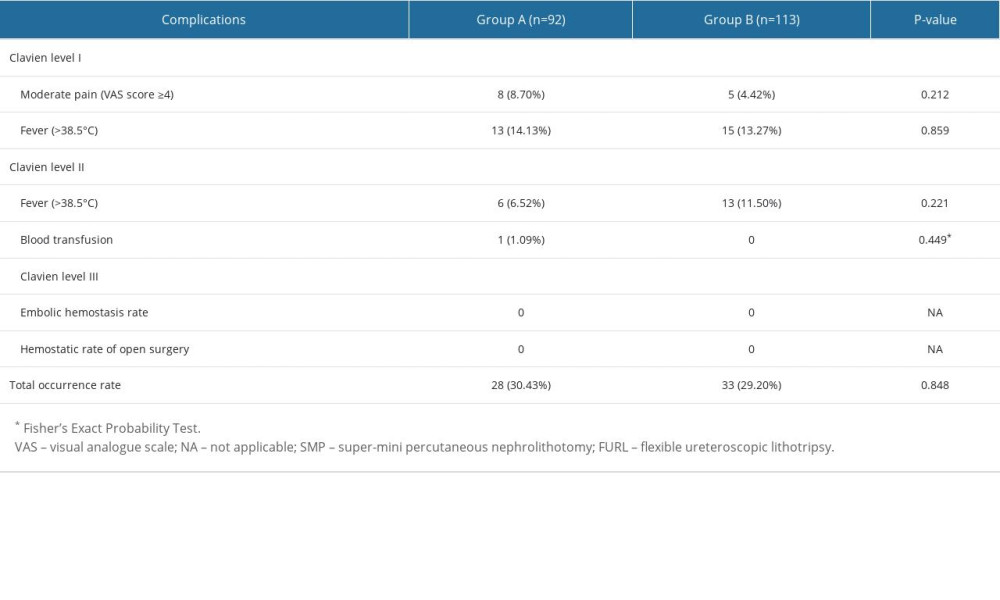 Table 3. Comparison of postoperative complications between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113).
Table 3. Comparison of postoperative complications between patients with complex kidney stones (n=205) who underwent SMP combined with FURL (Group A) (n=92) and those who underwent FURL alone (Group B) (n=113). In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








