15 September 2023: Clinical Research
Helicopter Ambulance Transport to the Emergency Department: Demographic and Clinical Factors Impacting Outcomes in a Turkish Medical Center
Habibe Selmin ÖzensoyDOI: 10.12659/MSM.941464
Med Sci Monit 2023; 29:e941464
Abstract
BACKGROUND: Helicopter ambulances (HAs) are a significant component of pre-hospital emergency medical services. This study presents a report on the demographic and clinical factors associated with transport to the emergency department (ED) by HA of 161 patients to a single center in Turkey.
MATERIAL AND METHODS: Demographic data, diagnoses in arriving center’s ED, transferred distance, and outcomes of 161 patients transferred by HAs between March 01, 2019 and May 31, 2021 were retrospectively evaluated. Mortality rates of the cases were compared both with age and according to the distance traveled within the diagnostic groups.
RESULTS: There were 134 patients (83.2%) with internal diseases, and cardiovascular diseases were the leading cause (68 patients, 41.6%); 27 patients (16.7%) were transferred due to trauma. The mean distance traveled with HAs was 167.1 km (range, 47.0-1316.0) and the median transfer time was 50 min. The most common form of hospitalization after ED arrival was intensive care hospitalization (n=78, 48.4%). Mortality increased as the transfer distance increased in elderly patients, as well as those with a cardiac or trauma-related diagnosis (P=0.015, P=0.044, P=0.028, respectively).
CONCLUSIONS: Most patients transferred by HA had severe disease. ED physicians dealing with patient transfer by HAs should be prepared for severe cases, both in the HA and in the ED. HAs may be preferred when making the transfer decision for elderly patients, trauma patients, and those with cardiac disease.
Keywords: Air Ambulances, Emergency Medical Services, Emergency Service, Hospital, Patient Transfer, Emergency Medicine, Aged, Humans, Retrospective Studies, Turkey, Hospitals, Demography
Background
Ambulances play a crucial role in the provision of pre-hospital emergency medical services (EMS) [1]. In emergency conditions such as disasters, accidents, and acute illnesses; rapid response to the scene, initiation of treatment at the scene, stabilization of the patient, and prompt transfer to a healthcare center where definitive treatment can be provided contribute to increased patient survival and discharge without sequelae [2]. It has been reported that as the time spent at the scene and during transportation decreases in the pre-hospital period, patient outcomes improve, and survival rates increase [1]. In addition to ground ambulances, air ambulance (AAs) are also an important component of pre-hospital EMS [2]. In areas where transportation is challenging, distances are long, and delayed treatment is expected for trauma and acute illness, the use of AAs is the most suitable option [3,4]. AAs consist of rotorwings (helicopters) and fixed-wings (airplanes) [5]. Helicopters and airplane ambulances have different characteristics compared to ground ambulances. Speed and accessibility are at the forefront of these features. Of course, AAs are faster than ground ambulances and they can reach roadless areas [5]. HAs are suitable for the rapid transfer of critical patients at relatively shorter distances than aircraft ambulances and are used for this purpose. With this logic, helicopter ambulances (HAs) were used in wars for the transport of wounded soldiers over short distances [6]. AAs, on the other hand, are used for longer distances than ground ambulances and helicopters and have a critical role [5]. AAs are of course more affected by weather conditions than ground ambulances. In this context, helicopters are more disadvantageous than AAs. AAs work in stronger communication with central control mechanisms. In any case, AAs are a more risky transfer system than ground ambulances [5].
AAs are used as effectively as ground ambulances in terms of effective and difficult medical interventions [7,8]. For this reason, they are known to be more important in the transfer of critically ill patients. However, according to the literature, it is thought that long-term mortality does not increase in transfers by ground ambulances [9,10].
The cost of patient transfer by AA is higher than that of ground ambulance. However, when patient transfer by AA is used appropriately, it is highly beneficial and cost-effective [5,11]. Therefore, each country should establish criteria for the use of AAs based on its own conditions and strive to assess whether the current use of AAs complies with these criteria in order to improve patient health and cost-effectiveness [12].
The type of patients to be transported by AAs in Turkey and the rules for transportation are determined. The dispatch and management of (HAs) stationed in designated provinces are carried out by the 112 Command Control Center (CCC) of the respective province [13]. The dispatch and management of helicopters outside the region are performed by the Ministry’s Air Operations Center. When a request for AA service is received, the physician at the CCC evaluates whether the request requires AA service based on general and medical criteria and decides to dispatch an HA. The dispatch of the HA is carried out by the 112 Emergency CCC through the radio/telephone system, ensuring that the helicopter team is assigned as quickly as possible [14]. An HA crew consist of 4 personnel: a doctor, a paramedic, a responsible pilot complying with Civil Aviation regulations, and a co-pilot. After the patient is transferred from the scene to the HA, the CCC directs the helicopter to the appropriate heliport/landing area. Following the directions from the 112 Emergency CCC, the receiving hospital emergency department (ED) is informed about the incident. If there is a suitable heliport at the healthcare facility where the patient will receive treatment, the patient is transferred from the scene to the hospital. If there is no heliport available, the nearest landing and take-off area to the receiving hospital is determined, and the flight team is informed. The CCC ensures that the patient is picked up from that area and transferred to the hospital [15].
Evaluating patient transfers conducted by AAs in the pre-hospital period will contribute to the planning of future pre-hospital transfers and treatments, and it will enhance the effectiveness and cost-effectiveness of patient transfer by AAs. This study presents a report on the demographic and clinical factors associated with transport to the ED by HA of 161 patients to a single center in Turkey. According to the results obtained, current planning can be guided in patient transfer with HA and new measures can be taken in EDs with HA service.
Material and Methods
STUDY DESIGN AND ETHICS:
Approval for this study was obtained from the local clinical research ethics committee in Ankara (decision number E2-21-891). Informed consent was obtained from all participants. Patients brought to the ED of our tertiary hospital by HAs between 01.03.2019 and 31.05.2021 were retrospectively evaluated. This hospital is a 4-year-old hospital located in Ankara, the capital of Turkey, in the center of the country. It is also a regional hospital with a large number of beds. At the same time, it is designed and equipped accordingly, in such a way that all diagnostic and therapeutic procedures can be performed. Therefore, it has a helipad and the hospital has a critical role in patient traffic with HA.
DATA COLLECTION:
Data were scanned from the database of our hospital and demographic data, diagnoses at the receiving hospital, transfer distance, disposition, and patient outcomes were retrospectively evaluated. All of the patients were diagnosed by physical examination, imaging methods, and laboratory examinations in the EDs they were in before the transfer, but due to the lack of treatment opportunities, a transfer request was made from the EDs they were in. We planned to exclude patients who died during transfer as an exclusion criterion, but since there were no such patients, all patients during the study data collection period were included. Adult patients aged 18 and above were classified as adult patients, while patients under the age of 18 were classified as pediatric patients. Diseases were categorized as internal diseases (non-traumatic mechanisms and diagnoses) and trauma-related diagnoses.
The flight distances of the patients included in the study from the province or district where they left by HAs to our hospital was obtained from the team in charge of HA flights. The distances and durations of flight for each transferred patient are routinely recorded by these personel. Data on the outcomes of the patients and the types of disposition from the ED upon arrival were obtained through the electronic data accessed by the healthcare professionals in the hospital.
STATISTICAL ANALYSES:
The data were analyzed using the SPSS 24.0 (SPSS; IBM Corp, Armonk, NY, USA) program. For the level of significance,
Results
DESCRIPTIVE DATA:
A total of 161 patients were included in the study; 109 (67.7%) were male and 52 (32.3%) were female. The average age of the patients was 60.9±22.2 years (range, 0–98), and 5 patients were in the pediatric age group. The mean age of men was 57.5±22.3, while it was 68.3±20.2 for women (Table 1). All transfers performed by HA in the study were interhospital transfers. There were 144 patients (89.4%) transferred from districts in Ankara, 16 patients (10.6%) from other provinces, and 1 patient (0.6%) from abroad. The mean distance between the location of transfer and the hospital was 167.1±168.6 km (range, 47.0–1316.0, Table 2), and the median flight time of transfers was 50 min.
CLINICAL RESULTS:
Diagnoses made in the ED of a single center that accepted transfers that were not related to trauma were classified as internal diseases. Internal diseases were the most common reason for transfers (134 patients, 83.2%). The most common internal diseases leading to transfers were cardiovascular diseases (68 patients, 42.2%), neurological diseases (26 patients, 16.1%), and respiratory diseases (23 patients, 14.2%) (Table 3).
The diagnoses of patients who only had a trauma-related problem were also classified as trauma-related diseases. There were no patients who had both an internal and a trauma-related problem at the same time. There were 27 patients (16.7%) transferred due to trauma, and the most common traumatic conditions leading to transfers were traffic accidents (7 patients, 4.3%), femur fractures by fall from standing position (5 patients, 3.1%), and thermal burns (5 patients, 3.1% (Table 4). In pediatric cases, burns were the most common reason for transfers (2 out of 5 patients [40%]).
There were 75 patients (46.5%) transferred with oxygen, 78 patients (48.4%) without oxygen, and 6 patients (3.7%) were intubated during the transfer. Two patients (1.2%) in the pediatric age group were transported in an incubator.
The dispositions of the transferred patients in the ED were as follows: intensive care unit (ICU) admission (78 patients, 48.4%), hospital ward admission (40 patients, 24.8%), discharge from the ED (30 patients, 18.6%), death in the ED (7 patients, 4.3%), and transfer to another hospital by ground ambulance (6 patients, 3.7%). The electronic data of these 6 cases showed that 4 of them were admitted to the ICU and 2 of them were admitted to wards. Among the 118 patients admitted to the hospital, the outcomes were as follows: 20 patients (12.4%) died, 97 patients (60.2%) were discharged, and 1 patient (0.6%) was transferred to another hospital. Twenty-nine (18.1%) patients died within 1 month after transfer by HAs, and these patients were significantly older (66.3± 28.2, P=0.015). There was no significant difference in mortality according to transfer distances, sex, or whether they were transferred from within the province or from outside the province (Table 2). In 68 patients diagnosed with cardiac disease and in 27 patients diagnosed with a trauma-related injury upon arriving at our center’s ED, 1-month post-transfer mortality differed significantly according to the distance transferred by HAs. In these 2 diagnostic groups, mortality was significantly higher in patients transported long distances (P=0.028 and P=0.015, respectively) (Table 5).
Discussion
In this study, we retropsectively assessed data on 161 patients transferred by HAs from hospitals to our ED, and evaluated their clinical outcomes and transfer characteristics. Most of the patients were elderly and male; we also found that internal diseases were the most common diagnosis made in our ED. The median flight time was 50 min, and that almost half of them needed oxygen during transport. Most patients we examined were admitted to the ICU from the ED. The distance transferred by HAs was significantly associated with mortality rates within 1 month after transfer among patients with cardiac diseases and trauma-related injuries.
It has been reported that timely arrival of patients to an appropriate facility for the most suitable treatment has an impact on patient outcomes [4,16]. Two expressions are used for time-sensitive situations: “time is brain” and “time is muscle”, meaning that brain tissue in patients with ischemic strokes and the myocardium in patients with acute coronary syndromes can quickly become permanently damaged [17]. In the current study, coronary artery diseases were the most common type of internal disease among patients transferred by HAs. In addition, in these cardiac cases we also found that mortality was higher when transfer distances were longer. Our results support the importance of early and rapid intervention in patients with cardiac diseases, in accordance with the “time is muscle” phenomenon. The results of this study and the literature’s emphasis on ischemia sensitivity [17] for myocardium and brain show the great importance of rapid transfer of these patients with time-saving HAs.
The average age of the patients transferred by HA in the current study was 60.9 years, and the majority of them were males. Previous studies have also reported a wide age distribution among patients transferred by HA and a higher frequency of male patients compared to female patients [8,10,18]. Alstrup et al, in a Danish cohort of 10 618 patients, found more males than females were transferred by HAs [9]. The data of that large-cohort study, which included data from Northern Europe, and our study in Turkey that included much less data, from Turkey, are quite similar. While the median age was 60 years in the cohort of Alstrup et al, it was 60.9 in our study. In a smaller cohort in a different region, Tavakoli et al reported significantly more males than females were transported by HAs, and the median age was similar to that of our study. These higher proportions of male and elderly patients transported by HAs should be taken into account in planning transfer using HAs from EDs. Björkman et al reported that mortality was higher with increasing age in patients with trauma-related diagnoses who were transferred by HAs [19]. Both the literature and the results of the present study show that mortality increases with increasing age in patients transferred by HAs; therefore, clinicians need to quickly make transfer decisions and choose the correct transport method for elderly patients.
Patients with internal diseases and injuries were the most common group requiring transfer by HAs, which is consistent with previous studies [8,18]. Cardiac diseases and neurological diseases are the conditions that benefit most from time-sensitive and HAs transportation [1,3,10,16,18,20,21]. In the current study, among patients with internal diseases, patients with cardiac and neurological diseases were most frequently transferred by HA, accounting for more than 50% of the transferred patients. The high rate of referral for cardiovascular and neurological diseases is primarily due to our hospital being a center for invasive-interventional procedures in cardiac and neurological cases, as well as being a stroke center. It has been reported that patients requiring invasive-interventional procedures benefit the most from AA transportation, and we believe that the appropriate transfer of this patient group by HA is being achieved in our hospital [3,7,16]. Fouche et al showed that AAs perform as well as ground ambulances regarding successful endotracheal intubation. In this study, we detected that nearly half of the patients were transferred with oxygen support and 6 of them were intubated while in the air. Both the literature and this study revealed that invasive procedures such as intubation are possible in the air.
In previous studies, trauma patients were reported to be the second most frequently transferred group by AA, with traffic accidents being the most common cause, which is consistent with the results of the current study [21,22]. Rapid transfer of trauma patients by HA to trauma centers has been associated with a decrease in mortality [4,10,23,24]. Our study revealed that mortality was significantly higher as the transfer distance increased in trauma patients. Considering that time becomes more important in trauma cases, HAs can give critical support.
The importance of rapidly reaching definitive treatment for patients transferred by HA has been emphasized in previous studies [16,20,24]. In the current study, nearly half of the transferred patients were admitted to the ICU, while some died in the ED. Previous studies have also reported high rates of ICU admission and mortality for patients transferred by AA [8,10]. These results suggest that the transferred patients had high disease severity and highlight the importance of effective measures and personnel training to ensure stability during transport and rapid access to definitive treatment through HA transfers. Based on the fact that the hospital where this study was conducted is the main hospital of the region, it can be predicted that more severe patients are referred to this hospital, while patients who are in better condition are treated in small hospitals without being referred. This prediction is consistent with these data. On the other hand, as in the literature, transferring severe patients is a more beneficial action. All kinds of interhospital transfers are costly. It would be unwise to incur this cost for a patient who can be treated easily without referral. These inferences are consistent with both our study data and the literature.
The most common intervention applied to the transferred patients in the current study was the administration of supplemental oxygen, which is consistent with the literature [21]. The fact that approximately half of the patients received oxygen raises concerns about the severity of the transferred patients’ conditions. In the literature, it has been reported that patients with internal diseases receive supplemental oxygen at a higher rate compared to trauma patients [25]. We believe that further studies are needed to determine whether this result is related to the severity of the patients’ conditions and to explore other contributing factors.
Many of the transferred patients were discharged from an ED. Previous reports have also mentioned varying rates of discharge from a hospital’s ED for patients transferred by ambulance [6]. The main reasons for this could be either the patient not being transferred according to appropriate criteria or the inadequacy of evaluation capabilities at the receiving hospital. It is necessary to conduct more detailed studies on the reasons and outcomes of patients who are transferred by AA but are ultimately discharged from the receiving hospital in order to ensure proper selection and triage of patients to be transported by AA.
Wejnarski et al reported shorter flight distances with HAs in their comprehensive report. In general, flight distances in the literature aree shorter than in the present study [25,26]. The primary reason for this could be that the longer distance to be traveled along with the patient’s medical condition makes HA transport the primary choice. It has been reported that HA transport is suitable for long-distance patient transfers and is associated with decreased mortality and uncomplicated hospital discharges. Previous reports have indicated that the distance traveled by AA or ground ambulance does not significantly impact patient outcomes [16,26]. In HA transfers, we believe that consideration should be given to the patient’s distance from the hospital where definitive treatment will be provided, as well as the potential for faster access to treatment. Many of the patients in the current study were transferred from district hospitals, but the transfer duration was longer than reported in the literature [25,27]. This situation may also be related to the population distribution of the countries and regions where the studies were conducted. Our hospital is a very large regional hospital, so a plan may have been made for the transfer of patients to this hospital in the provision of health services. This increases the number of referrals from more distant hospitals to our hospital. The increase in distances may also explain the longer duration of referrals with HAs to our hospital compared to the literature.
This study contains some limitations. First, this was a single-center study. In a study with multicenter data, more valid comparisons could be made on subjects, such as flight times. The number of patients included was not large. Although our results agree with studies with large case numbers, the number of cases is a limitation. On the other hand, the study reports only descriptive data, and we did not perform cost analysis due to lack of data, which is an important factor to consider in air transfers. Multicenter and multinational studies with different methodologies may reach different conclusions.
Conclusions
Most of the patients transferred by HA were males and elderly people. Invasive procedures may also be required while aboard these HAs. Mortality increased as the transfer distance increased in elderly patients, as well as those with a cardiac- or trauma-related diagnoses. HAs may be preferred when making the transfer decision in elderly and trauma patients, or those with cardiac disease.
Tables
Table 1. Descriptive data of age and sex in patients transferred to a single center by HAs.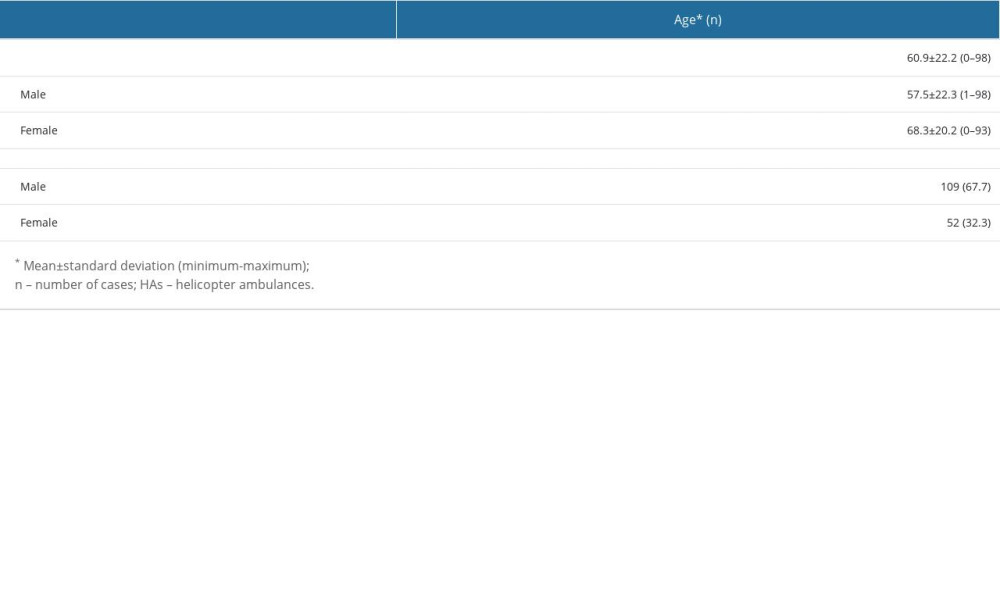 Table 2. Survival and mortality rates of patients transferred from another hospital by HAs to a single center according to sex, age, and distance transferred by HAs at 1 month after transfer.
Table 2. Survival and mortality rates of patients transferred from another hospital by HAs to a single center according to sex, age, and distance transferred by HAs at 1 month after transfer.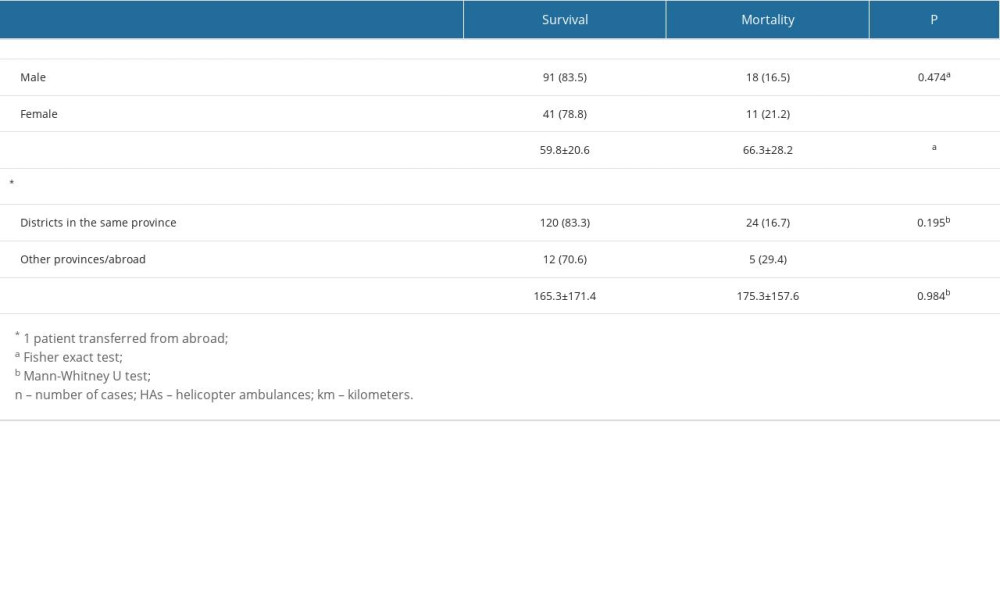 Table 3. Medical concerns of patients diagnosed with an internal disease, transferred by HA to a single center from other hospitals.
Table 3. Medical concerns of patients diagnosed with an internal disease, transferred by HA to a single center from other hospitals.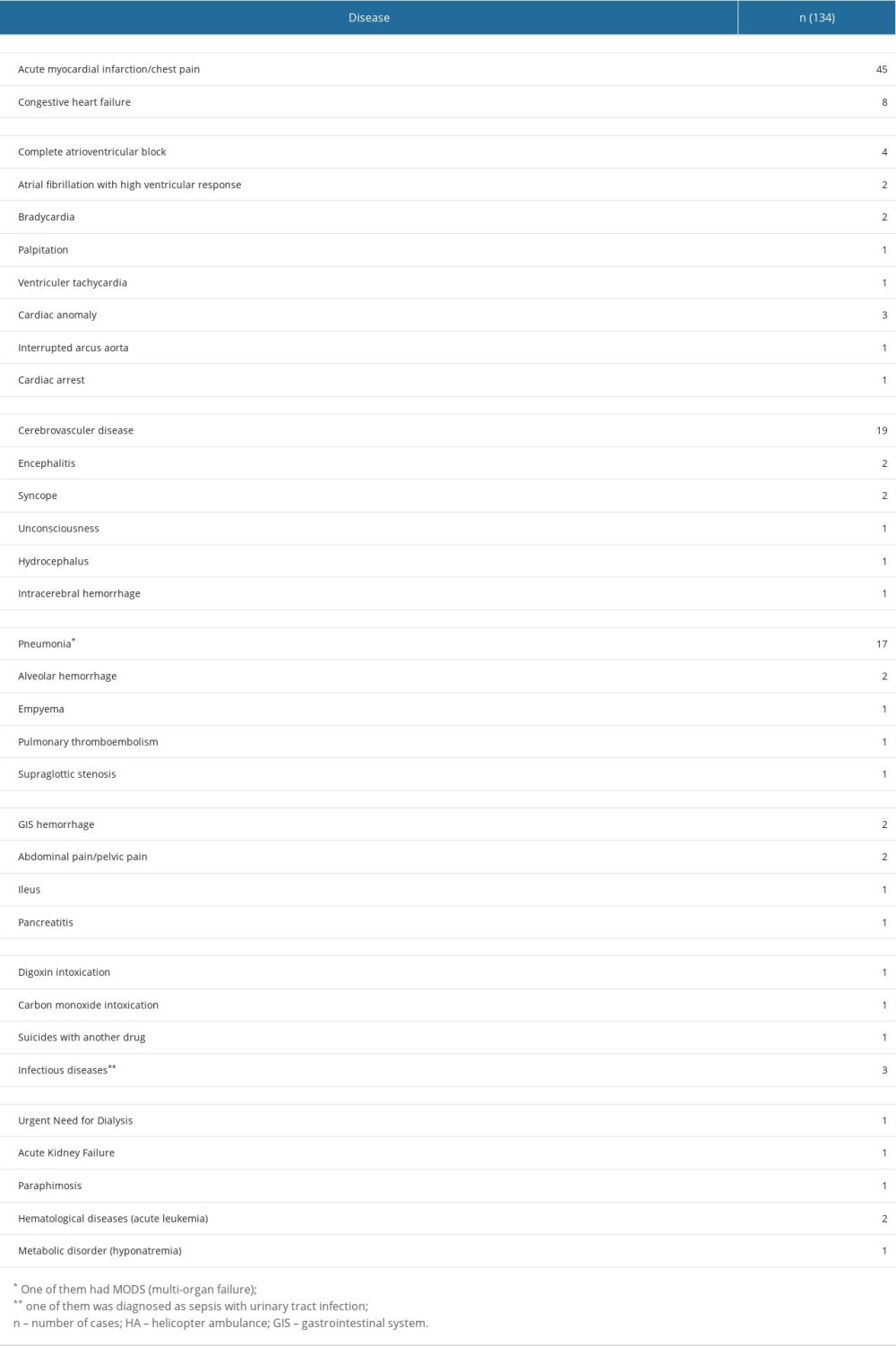 Table 4. Trauma mechanisms and trauma-related daignoses of injured patients transferred by HA to a single center from other hospitals.
Table 4. Trauma mechanisms and trauma-related daignoses of injured patients transferred by HA to a single center from other hospitals.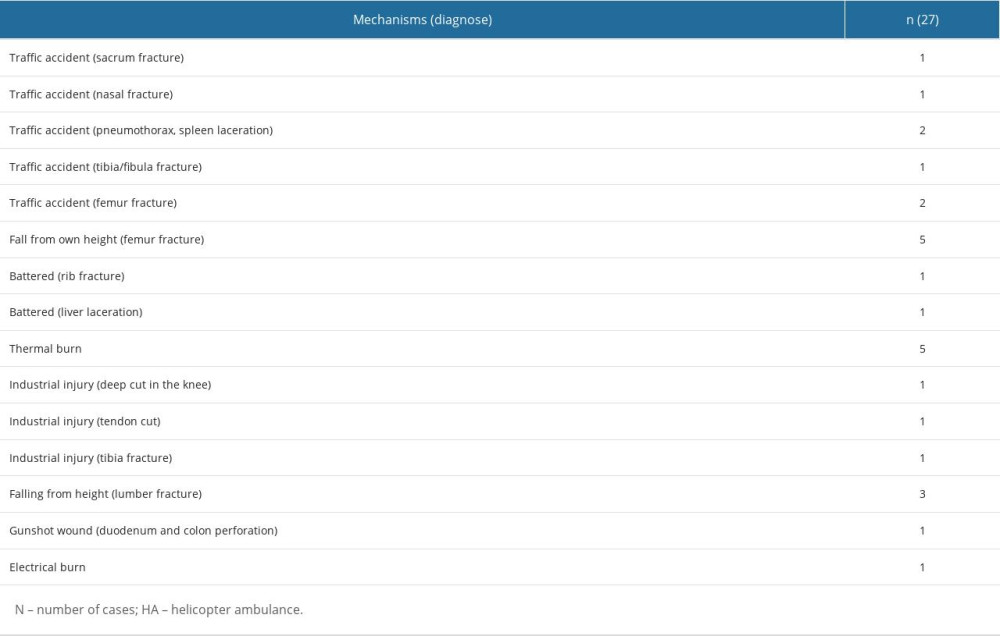 Table 5. Survival and mortality rates of patients transferred from another hospital by HAs to a single center diagnosed with a cardiac disease or a trauma-related injury upon ED arrival.
Table 5. Survival and mortality rates of patients transferred from another hospital by HAs to a single center diagnosed with a cardiac disease or a trauma-related injury upon ED arrival.
References
1. Sy E, Ross T, Air Aambulance transport: CMAJ, 2021; 193(37); E1462
2. Araiza A, Duran M, Surani S, Varon J, Aeromedical transport of critically ill patients: A literature review: Cureus, 2021; 13(5); e14889
3. Knudsen L, Stengaard C, Hansen TM, Earlier reperfusion in patients with ST-elevation myocardial infarction by use of helicopter: Scand J Trauma Resusc Emerg Med, 2012; 20; 70
4. Ageron FX, Debaty G, Savary D, Association of helicopter transportation and improved mortality for patients with major trauma in the northern French Alps trauma system: An observational study based on the TRENAU registry: Scand J Trauma Resusc Emerg Med, 2020; 28(1); 35
5. Loyd JW, Larsen T, Swanson D, Aeromedical transport: StatPearls, 2023, StatPearls Publishing. Copyright© 2023, StatPearls Publishing LLC Treasure Island (FL) ineligible companies. Disclosure: Timothy Larsen declares no relevant financial relationships with ineligible companies. Disclosure: Doug Swanson declares no relevant financial relationships with ineligible companies:
6. Melton JT, Jain S, Kendrick B, Deo SD, Helicopter Emergency Ambulance Service (HEAS) transfer: An analysis of trauma patient case-mix, injury severity and outcome: Ann R Coll Surg Engl, 2007; 89(5); 513-16
7. Fouche PF, Stein C, Simpson P, Flight versus ground out-of-hospital rapid sequence ıntubation success: A systematic review and meta-analysis: Prehosp Emerg Care, 2018; 22(5); 578-87
8. Alstrup K, Petersen JAK, Sollid S, Mortality and hospitalisation in the Danish Helicopter Emergency Medical Service (HEMS) population from 2014 to 2018: A national population-based study of HEMS triage: BMJ Open, 2020; 10(8); e038718
9. Alstrup K, Rognås L, Sollid S, Association of helicopter vs ground emergency medical transportation with 1-year mortality in Denmark: JAMA Netw Open, 2021; 4(1); e2033318
10. Alstrup K, Møller TP, Knudsen L, Characteristics of patients treated by the Danish Helicopter Emergency Medical Service from 2014–2018: A nationwide population-based study: Scand J Trauma Resusc Emerg Med, 2019; 27(1); 102
11. Tavakoli N, Saberian P, Bagheri Faradonbeh S, Cost-effectiveness analysis of air emergency versus ground emergency medical services regarding the patient’s transportation and treatment in selected hospital: Med J Islam Repub Iran, 2022; 36; 113
12. Hawilo H, Taneja R, Interfacility helicopter transfers for critically ill patients: Always the right choice?: Crit Care, 2020; 24(1); 153
13. Ünsal İ, Ekici-Ünsal D, Hava ambulans sisteminin Türkiye’ deki Gelişimi: Havacilik ve Uzay Çalişmalari Dergisi, 2021; 2(1); 47-69
14. Şimşek P, Gunaydin M, Gunduz A, Hastane öncesi acil sağlik hizmetleri: Türkiye örneği: Gümüşhane Üniversitesi Sağlik Bilimleri Dergisi, 2019; 8(1); 120-27
15. Yurt YC, Celal K, Metin O, Evaluation of the patients brought to the emergency service by helicopter ambulance by REMS and NACA score: Anatolian Journal of Emergency Medicine, 2021; 4(1); 17-22
16. Meuli L, Zimmermann A, Menges AL, Helicopter emergency medical service for time critical interfacility transfers of patients with cardiovascular emergencies: Scand J Trauma Resusc Emerg Med, 2021; 29(1); 168
17. Saver JL, Time is brain – quantified: Stroke, 2006; 37(1); 263-66
18. Kornhall D, Näslund R, Klingberg C, The mission characteristics of a newly implemented rural helicopter emergency medical service: BMC Emerg Med, 2018; 18(1); 28
19. Björkman J, Setälä P, Pulkkinen I, Effect of time intervals in critical care provided by helicopter emergency medical services on 30-day survival after trauma: Injury, 2022; 53(5); 1596-602
20. Pappinen J, Miettinen T, Laukkanen-Nevala P, The selection of an optimal transportation strategy in urgent stroke missions: A simulation study: Scand J Trauma Resusc Emerg Med, 2020; 28(1); 48
21. Wake K, Noguchi T, Hishinuma H, Characteristics of patients who received helicopter emergency medical services in Japan from 2012 to 2019: A retrospective analysis of data from Tochigi Prefecture: Scand J Trauma Resusc Emerg Med, 2022; 30(1); 25
22. Østerås Ø, Brattebø G, Heltne JK, Helicopter-based emergency medical services for a sparsely populated region: A study of 42,500 dispatches: Acta Anaesthesiol Scand, 2016; 60(5); 659-67
23. Andruszkow H, Lefering R, Frink M, Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients: Crit Care, 2013; 17(3); R124
24. Dowd B, Elkbuli A, In response to: Helicopter versus ground ambulance: Review of national database for outcomes in survival in transferred trauma patients in the USA Michaels D, Pham H, Puckett Y, et al Trauma Surg Acute Care Open 2019;4:e000211: Trauma Surg Acute Care Open, 2019; 4(1); e000404
25. Wejnarski A, Leszczyński P, Świeżewski S, Characteristics of aeromedical transport, both interhospital and directly from the scene of the incident, in patients with acute myocardial infarction or acute trauma between 2011–2016 in Poland: A case-control study: Adv Clin Exp Med, 2019; 28(11); 1495-505
26. Hoshiyama E, Noguchi T, Wake K, Characteristics of Emergency Neurological Patients Who Were Transported by Helicopter Emergency Medical Services in Tochigi, Japan: Tohoku J Exp Med, 2021; 255(1); 79-89
27. Imaizumi T, Hata N, Kobayashi N, Early access to patients with life-threatening cardiovascular disease by an AA service: J Nippon Med Sch, 2004; 71(5); 352-56
Tables
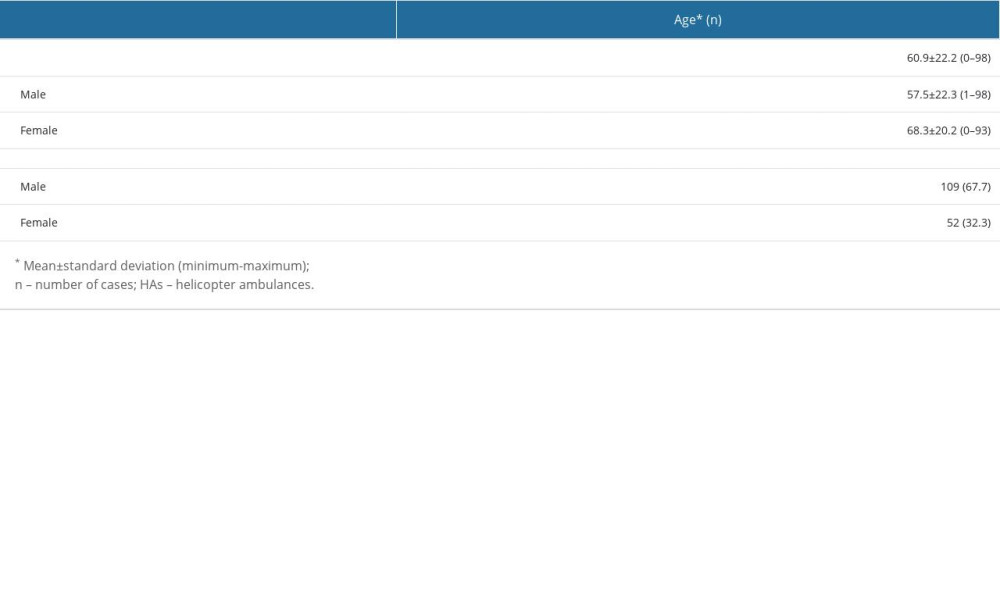 Table 1. Descriptive data of age and sex in patients transferred to a single center by HAs.
Table 1. Descriptive data of age and sex in patients transferred to a single center by HAs.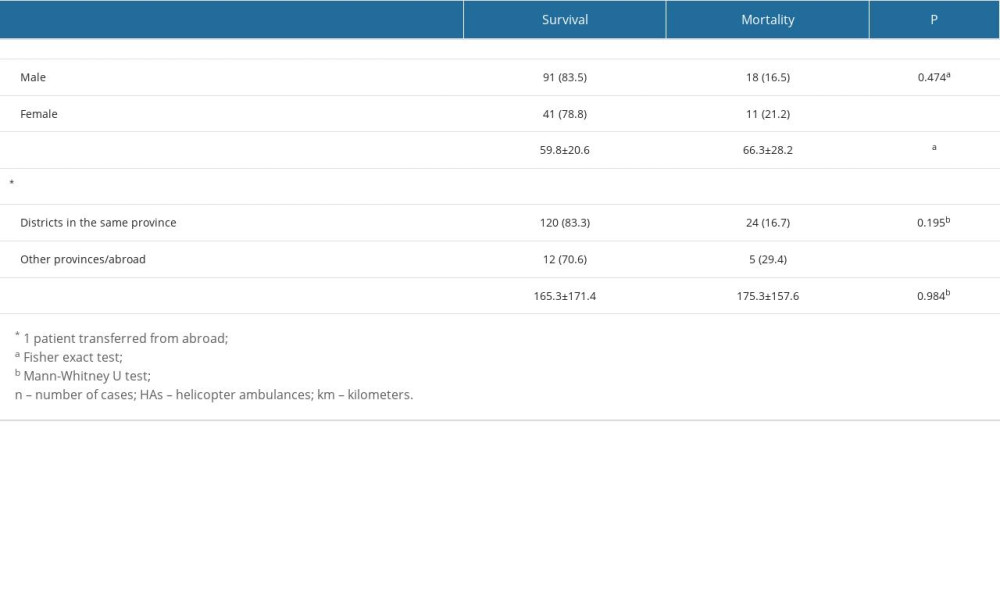 Table 2. Survival and mortality rates of patients transferred from another hospital by HAs to a single center according to sex, age, and distance transferred by HAs at 1 month after transfer.
Table 2. Survival and mortality rates of patients transferred from another hospital by HAs to a single center according to sex, age, and distance transferred by HAs at 1 month after transfer.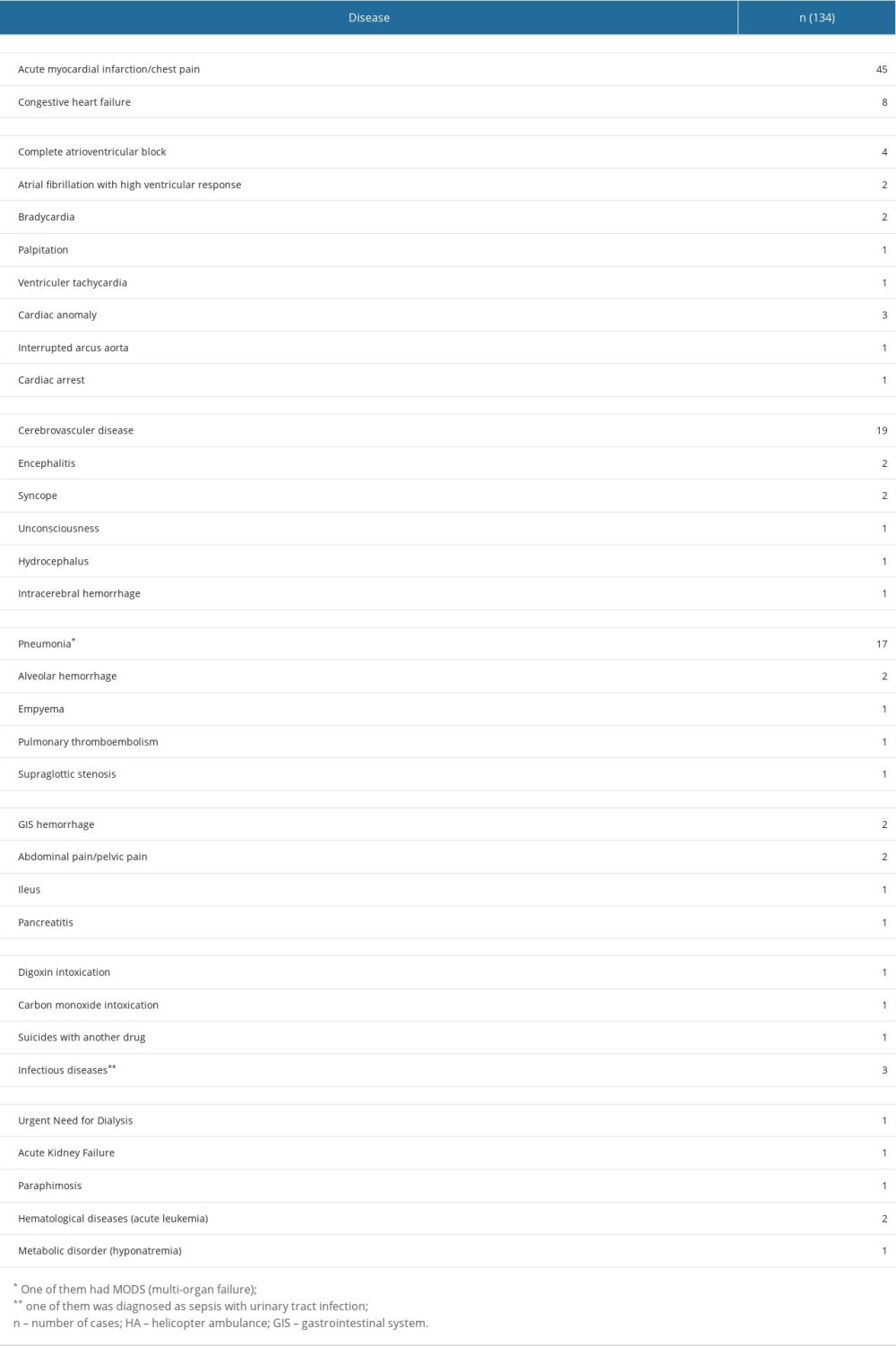 Table 3. Medical concerns of patients diagnosed with an internal disease, transferred by HA to a single center from other hospitals.
Table 3. Medical concerns of patients diagnosed with an internal disease, transferred by HA to a single center from other hospitals.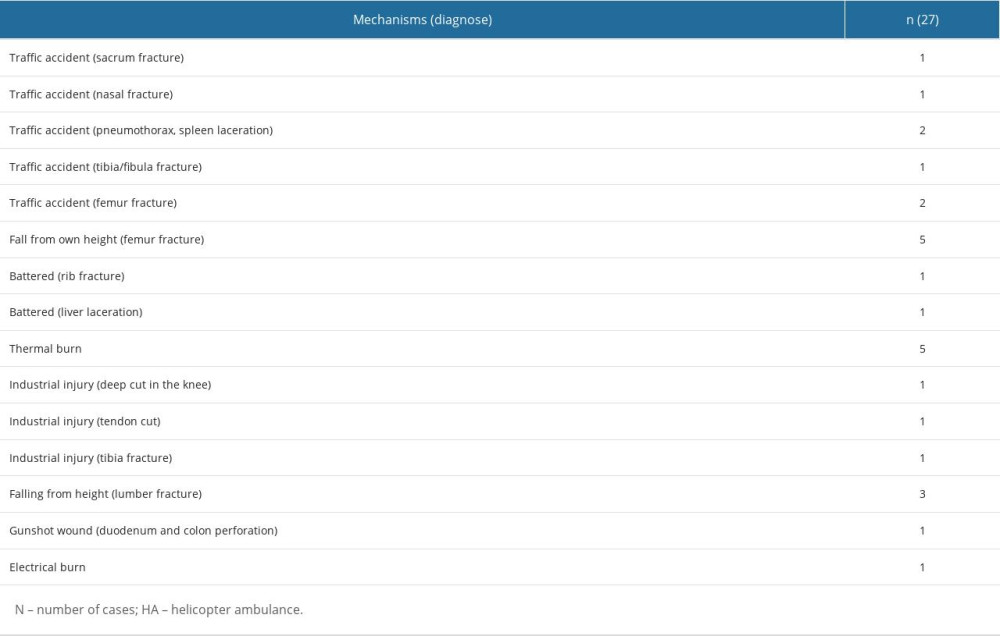 Table 4. Trauma mechanisms and trauma-related daignoses of injured patients transferred by HA to a single center from other hospitals.
Table 4. Trauma mechanisms and trauma-related daignoses of injured patients transferred by HA to a single center from other hospitals. Table 5. Survival and mortality rates of patients transferred from another hospital by HAs to a single center diagnosed with a cardiac disease or a trauma-related injury upon ED arrival.
Table 5. Survival and mortality rates of patients transferred from another hospital by HAs to a single center diagnosed with a cardiac disease or a trauma-related injury upon ED arrival. In Press
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








