05 March 2024: Clinical Research
Clinical Outcomes of Arthroscopic Surgery in Patients with Gluteal Muscle Contracture: Single-Institution Results from a High-Volume Cohort
Jianhai Hu12ABCEF, Jiazhuang Zhu2BC, Zheng Zhou2CD, Xiaoxiang Yang3B, Min Zhu1A, Peng Wu2AFG*DOI: 10.12659/MSM.942945
Med Sci Monit 2024; 30:e942945
Abstract
BACKGROUND: The aim of this study was to assess clinical outcomes of arthroscopic surgery for gluteal muscle contracture (GMC) with at least 2 years of follow-up in a large sample.
MATERIAL AND METHODS: A total of 665 patients who underwent arthroscopic release procedure at our institution between March 2014 and December 2018 and met the inclusion criteria were included in this study. All the patients were operated on by the same surgeon and the surgeon released the contracture band from anterior to posterior starting from the anterior edge of the ITB, the contracture band of the gluteus maximus, and vastus medialis tensor. After exclusion, 544 patients (218 males and 326 females) were finally included. Clinical outcomes at 2 years of postoperative follow-up were evaluated by a combination of several methods, including a new criterion we proposed for postoperative assessment, which included the cross-leg test, difficulty in squatting with legs together, and abnormal gait, the visual analogue scale (VAS), the modified Harris hip score (mHHS), and the satisfaction of patients.
RESULTS: The average follow-up time was 48.2±14.9 months. Based on the new criteria, 513 (94.3%) patients were evaluated as good, 25 (4.6%) as fair, and 6 (1.1%) as poor. The mHHS increased from 72.1±6.0 (range, 56.0-81.3) to 97.3±2.2 (range, 92.3-100.0) (P<0.001). The VAS decreased from 3.3±1.1 (range, 0-5) to 0.062±0.13 (range, 0-1) (P<0.001). For subjective satisfaction, 526 (96.7%) patients were satisfied, 14 (2.6%) patients were neutral, and 4 (0.7%) patients were dissatisfied.
CONCLUSIONS: In a large sample, favorable and durable clinical outcomes were observed after the arthroscopic procedure. Clinical symptoms and mHHS showed significant improvement with a minimum 2-year follow-up.
Keywords: Arthroscopy, Disability Evaluation, Hip Contracture
Background
Gluteal muscle contracture (GMC), a condition commonly occurring in the young, mainly due to repeated intramuscular injections of penicillin into the hip, is the most common reason for external snapping hip (ESH) syndrome [1–5]. ESH is a type of snapping hip syndrome (SHS), which typically presents with an audible snapping or sensation during hip motion, and is usually associated with localized pain [6–9]. SHS generally consists of 2 types – extra-articular and intra-articular – with the extra-articular snapping hip being divided into the internal snapping hip and the ESH, the latter being more common [9–11]. According to previous reports, ESH commonly occurs when the hip is in flexion, extension, and external or internal rotation, and the iliotibial band (ITB) or anterior edge of the gluteus maximus slides over the greater trochanter (GT) [6,11–14]. Additionally, diagnosis of GMC is generally based on the patient’s history of multiple repeat penicillin gluteal injections, symptoms, signs, and radiographic findings. The symptoms and signs may include difficulty squatting with legs together, abnormal gait, positive cross-legged test, and positive Ober’s sign, among others (Figure 1A–1C) [15–18]. Radiographic findings may include a hyperdense line on the iliac bone approximately parallel to the sacroiliac joint (Figure 1D), which can aid in the diagnosis of GMC [19].
Typically, patients diagnosed with GMC will first begin conservative treatment, including rest, physical therapy, stretching, and non-steroidal anti-inflammatory drugs (NSAIDs), among others [5,11–13,20]. If conservative treatment fails to improve symptoms, surgery is recommended [12], which can be performed using open or arthroscopic techniques. Compared to open surgery, arthroscopic surgery has advantages such as shorter operation time, smaller scars, less postoperative pain, faster recovery time, and fewer complications. Hence, arthroscopic surgery is considered the criterion standard for treatment of GMC [21–23].
The purpose of this study was to analyze the clinical outcomes of arthroscopic surgery for GMC in a large sample. We hypothesized that patients who underwent this arthroscopic surgical approach would experience significant improvement in clinical symptoms and mHHS, with high levels of subjective satisfaction at a minimum 2-year follow-up.
Material and Methods
PATIENT DATA:
A total of 665 patients who underwent the arthroscopic release procedure for GMC at our institution between March 2014 and December 2018 were included in this study. And 554 patients (218 males and 326 females) completed follow-up and were included in the study. Among the patients, 523 patients had bilateral GMC and 21 patients had unilateral GMC. The inclusion criteria were: (1) diagnosed with GMC; (2) underwent an arthroscopic procedure; and (3) did not have other bone or joint diseases. The exclusion criteria were: (1) aged <18 years old at the time of the procedure; (2) underwent previous surgical treatment for GMC; (3) did not have a minimum 3-month conservative treatment; and (4) lost to follow-up (Figure 2).
The study was done in a single institution. All the patients were operated on by a single surgeon at our center.
SURGICAL TECHNIQUE:
Patients were positioned on a standard operating table in a lateral position and intravenous general anaesthesia was routinely used. The surgeon identified the area to be operated on by moving the hip in flexion, internal retraction, and internal rotation. The position of the GT and 2 portals – proximal and distal – were then marked, with both portals approximately 0.3 cm in length (Figure 3A). Once the markings were complete, disinfection and towel laying were performed. The endoscope was inserted through the proximal portal, and 30–50 ml of normal saline was used to improve visualization. The planer (Smith & Nephew) was inserted through the distal portal to remove fat and connective tissue that interfered with the surgical area, and exposed the contracted muscle tissue. Next, a radiofrequency knife (Smith & Nephew) was inserted through the distal portal, and the contracture band was incised from anterior to posterior starting from the anterior edge of the ITB. The remaining contracture band of the ITB was loosened after completion of exploration, followed by loosening the contracture bands of the gluteus maximus and vastus medialis tensor (Figure 3C). The decision to partially loosen the contracture bands of the gluteus medius and gluteus minimus was based on preoperative examination and intraoperative exploration. During the procedure, the assistant moved the patient’s hip joint to expose all contracted muscle tissue (Figure 3B). Finally, the hip joint was repeatedly moved to assess the degree of loosening, and if there was no snapping and a negative Ober’s sign, the procedure was deemed complete. Both portals were then sutured (Figure 3D). If the patient had bilateral GMC, the same procedure was performed on the other side after completing the first side. Care was taken not to damage the sciatic nerve and to stop any bleeding promptly. The operation time for each side was 10–15 min.
POSTOPERATIVE TREATMENT:
After the surgery, patients received ice application to relieve pain. If necessary, NSAIDs could be used to manage pain for 1 day postoperatively. Patients were encouraged to begin exercising their hip and knee function as early as possible and bear full weight on the second day after surgery, with the help of others. During sleep, the 2 legs were bound with a restraint strap for at least 1 week. The patients were allowed to flex the hip and knee and cross the legs side by side. Embracing the legs with the knees together as close to the chest as possible (passively or positively) was also repeated 3–5 times a day. Postoperative rehabilitation was standardized for each patient and included training in cross-leg, squatting with legs together, and gait. This rehabilitation program lasted for 6 months. After this period, patients could decide whether to continue with rehabilitation training at their discretion.
POSTOPERATIVE FOLLOW-UP:
We developed a new assessment criterion for postoperative evaluation of GMC, which included the cross-leg test, difficulty in squatting with legs together, and abnormal gait. Each criterion was scored as 1 or 0, and the scores were summed to obtain an overall score for each patient. A score of 3 indicated good recovery, 2 indicated fair recovery, and 1 or 0 indicated poor recovery (Table 1). In addition to this, we assessed the postoperative recovery of hip function using the mHHS and recorded the subjective satisfaction level of each patient. The subjective satisfaction level was categorized as satisfied, neutral, or dissatisfied. Furthermore, we stratified all patients into 2 groups by sex.
STATISTICAL ANALYSIS:
We performed all data analyses using SPSS 25.0 software (IBM). We used a chi-square test to compare the proportions of symptom improvement and good recovery rates between preoperative and postoperative periods, as well as between different subgroups. We used a paired
Results
PATIENT DATA:
A total of 544 patients (218 male and 326 female) who fulfilled the inclusion criteria were included in this study. The mean age of patients who underwent surgery was 28.2±5.2 years (range, 18–48 years). The mean length of hospitalization was 4.8±1.2 days (range, 3–9 days), and the mean postoperative follow-up was 48.2±14.9 months (range, 24–81 months). The symptoms and radiographic findings of GMC patients before surgery are summarized in Table 2. Among the patients, 523 patients had bilateral GMC and 21 patients had unilateral GMC.
CLINICAL OUTCOMES:
After surgery, all patients experienced a disappearance of hip snapping and a negative Ober’s sign. Micro-hematomas occurred postoperatively in 23 patients, but all were absorbed spontaneously. No patients experienced sciatic nerve injury, wound dehiscence, or infection, and no patients showed a positive Trendelenburg sign during the follow-up period.
Table 3 presents the results of our study, which included 544 patients. The number of patients with a positive cross-leg test decreased significantly from 538 (98.9%) to 15 (2.8%) (P<0.001) (Figure 4A, 4B). Likewise, the number of patients with difficulty in squatting with legs together decreased significantly from 543 (99.8%) to 12 (2.2%) (P<0.001) (Figure 4C). Furthermore, the number of patients with abnormal gait decreased from 543 (99.8%) to 10 (1.8%) (P<0.001). According to the criteria we developed, 513 (94.3%) patients were evaluated as good, 25 (4.6%) as fair, and 6 (1.1%) as poor. The mean mHHS improved from 72.1±6.0 (range, 56.0–81.3) to 97.3±2.2 (range, 92.3–100.0) (P<0.001). The mean VAS decreased from 3.3±1.1 (range, 0–5) to 0.062±0.13 (range, 0–1).
Subjective satisfaction was also assessed, with 526 (96.7%) patients being satisfied, 14 (2.6%) patients being neutral, and 4 (0.7%) patients being dissatisfied.
We also conducted an analysis based on sex, dividing all GMC patients into male (n=218) and female (n=326) groups. However, we found no significant correlation between sex and the improvement in symptoms, mHHS, or good rates (P>0.05) (Table 4).
Discussion
The most notable finding of this study is that using only 2 portals in arthroscopic surgical procedures on GMC patients resulted in favorable outcomes. In a large sample of patients, we observed significant improvements in typical symptoms and the modified Harris hip score (mHHS) during a minimum 2-year follow-up, and a high subjective patient satisfaction rate of 96.7%. Furthermore, we found no significant correlation between sex and surgical outcomes.
Since Ilizaliturri et al [24] first described the arthroscopic treatment of GMC internationally, several approaches to the arthroscopic procedure have been successively reported. For instance, Liu et al [25] treated 108 patients with arthroscopic GMC release through 3 portals (inferior, anterior, and posterior), with a minimum follow-up of 7 months. Fu et al [21] treated 52 patients through 2–3 portals with a minimum follow-up of 12 months. Rai et al [26] treated 75 patients using F and C arthroscopic GMC release through 2–3 portals with a minimum follow-up of 18 months. However, these approaches had some limitations, including more portals, smaller sample sizes, or shorter follow-up periods. Additionally, another center reported using needle knife surgery, a minimally invasive technique for GMC treatment, in 1059 patients through 4 portals determined by hip local tension position [27]. However, compared to arthroscopic surgery, in their study this method had the disadvantage of not providing a direct view and tended to damage the sciatic nerve, as well as failing to stop bleeding effectively, which resulted in 3 patients developing hematomas requiring emergency surgery. Therefore, we developed a novel arthroscopic surgical approach requiring only 2 portals for GMC patients, and we evaluated the clinical outcomes with a minimum follow-up of 2 years in 544 cases in this study.
Compared to the arthroscopic approaches proposed in previous studies, our approach achieved nearly the same clinical outcomes using fewer portals, which were less invasive and more beneficial for patients. Fu et al [21] performed arthroscopic surgery on 52 patients and obtained a good rate of 88.46% with a minimum follow-up of 12 months. Rai et al [26] used the F and C arthroscopic GMC release method in 75 patients and obtained a superior rate of 94.7% with a minimum follow-up of 18 months. Zhang et al [23] performed arthroscopic surgery on 41 patients and obtained a good rate of 92.68% with a minimum follow-up of 12 months. Gao et al [28] followed up 118 patients with a subjective patient satisfaction rate of 95.8% and a negative postoperative cross-leg test of 96.6%. In the present study, we evaluated the outcomes of our novel arthroscopic surgical approach based on our newly developed postoperative assessment criteria for GMC, mHHS, and subjective patient satisfaction. Our results showed that the postoperative patient good rate was 94.5%, the mHHS improved from 72.1±6.0 pre-operatively to 97.3±2.2 postoperatively, and the subjective satisfaction rate was 96.7%, indicating that our novel arthroscopic release procedure had favorable outcomes for GMC patients.
However, our study also revealed that some patients still experienced persistent clinical symptoms despite undergoing our novel arthroscopic surgical approach. Although these symptoms improved compared to the preoperative period and no longer significantly affected most patients’ lives, it suggests that further improvements are required to make our proposed approach more precise.
Previous studies have employed various assessment criteria to evaluate the symptoms and functional recovery of GMC patients after surgery. For instance, Ye et al [27] developed assessment criteria that included symptoms such as squatting with legs together, crossed legs, gait, and sliding of the contracture band. Tang et al [29] developed a more informative hip muscle contracture disability scale (GDS) that consisted of 15 criteria, including Trendelenburg gait, cross-leg, squat with legs together, snapping, hip morphology, and movement limitations, among others.
In this study, we developed a new assessment criterion that combined the 3 most common symptoms of GMC patients, which could be applied during telephone and video follow-ups: cross-leg test, difficulty in squatting with legs together, and abnormal gait. To make the follow-up more comprehensive, we also used the commonly used assessment criterion for hip patients, mHHS, to assess the recovery of postoperative hip function [30]. The mHHS comprised 8 aspects of pain, limp, support, distance walked, stairs, socks/shoes, sitting, and public transportation, and its total score was 100. In comparison to the Harris hip score (HHS), the mHHS excluded 2 components (range of motion and deformities) that needed physical examination[31]. Edwards et al [30] found no clinical differences between the mHHS and HHS. Additionally, subjective patient satisfaction was also assessed.
However, developing consistent and quantitative assessment criteria is crucial for evaluating the outcomes of surgical approaches for GMC patients. Compared with the assessment criteria used in previous studies, the assessment criteria used in this study was simple but comprehensive and especially suitable for telephone and video follow-up of large samples. Moreover, we anticipate the emergence of consistent and quantitative criteria for GMC assessment in the future, which would enable physicians and researchers to better evaluate and compare the outcomes of various surgical approaches for GMC patients.
In addition, it is important to note that postoperative rehabilitation plays a crucial role in achieving favorable outcomes for GMC patients [32]. Our follow-up findings revealed that most patients obtained favorable clinical outcomes after 6 months of postoperative rehabilitation. However, a few patients required continuous postoperative rehabilitation for about 2 years before their symptoms disappeared. Based on these observations, we recommend that GMC patients who still experience clinical symptoms after 6 months of postoperative rehabilitation should be considered for continued rehabilitation until their symptoms disappear, and should be reviewed within a specified time frame. Nevertheless, further research is needed to determine the optimal duration of rehabilitation therapy to maximize patient benefit.
This study has several limitations that should be acknowledged. Firstly, retrospective analyses are prone to inherent biases that can affect the validity of results. Secondly, the fact that our study subjects were from 1 institution may lead to regional and institutional bias, which limits the generalizability of our findings to other populations. Lastly, since we did not have a control group, and there are no standardized quantitative criteria for GMC, it was difficult to validly compare the results of our study with those of other studies.
Conclusions
The clinical outcomes of arthroscopic surgical approach for GMC patients in this study were favorable and durable. On the one hand, this approach is less invasive as it involves fewer portals, which is more beneficial for patients. On the other hand, our results showed a significant improvement in symptoms and mHHS with a minimum 2-year follow-up in a large sample.
Figures
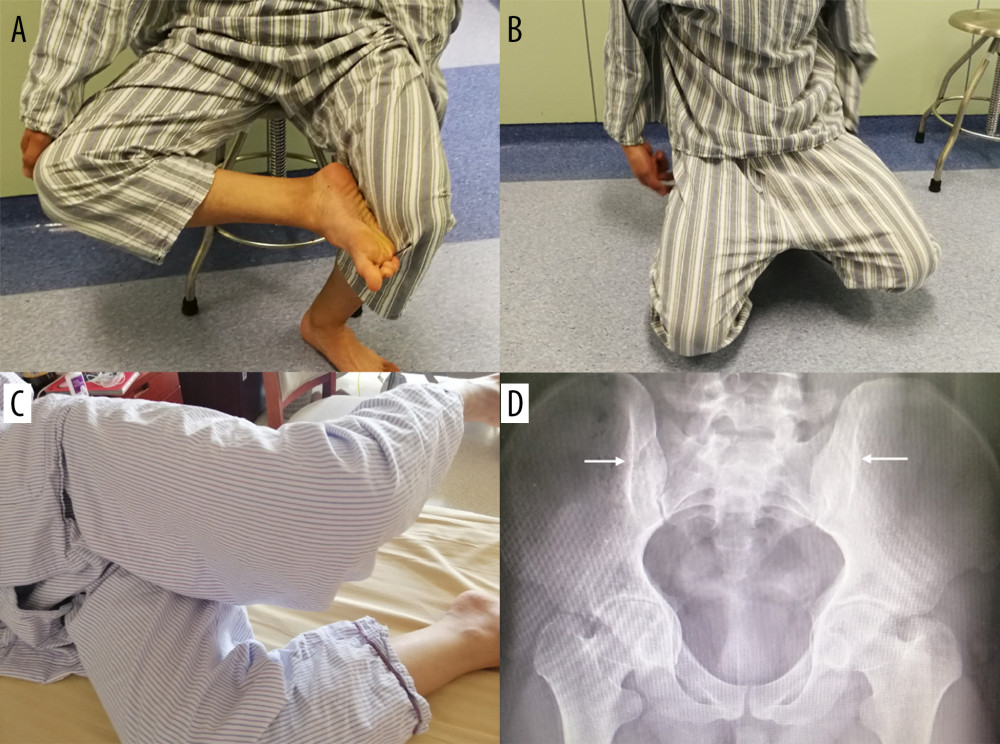 Figure 1. Symptoms, signs, and radiographic findings of a patient with GMC. (A) The patient could not cross his leg while sitting down. (B) The hip joint is fixed in abduction and external rotation when the patient squats and cannot squat with the legs together. (C) The doctor fixed the patient’s pelvis and ankle with the knee flexed at 90°, and then the doctor released the patient, and the patient maintained an upward and abducted position of the affected limb, which was a positive Ober’s sign. (D) Iliac hyperdense line sign (arrow).
Figure 1. Symptoms, signs, and radiographic findings of a patient with GMC. (A) The patient could not cross his leg while sitting down. (B) The hip joint is fixed in abduction and external rotation when the patient squats and cannot squat with the legs together. (C) The doctor fixed the patient’s pelvis and ankle with the knee flexed at 90°, and then the doctor released the patient, and the patient maintained an upward and abducted position of the affected limb, which was a positive Ober’s sign. (D) Iliac hyperdense line sign (arrow). 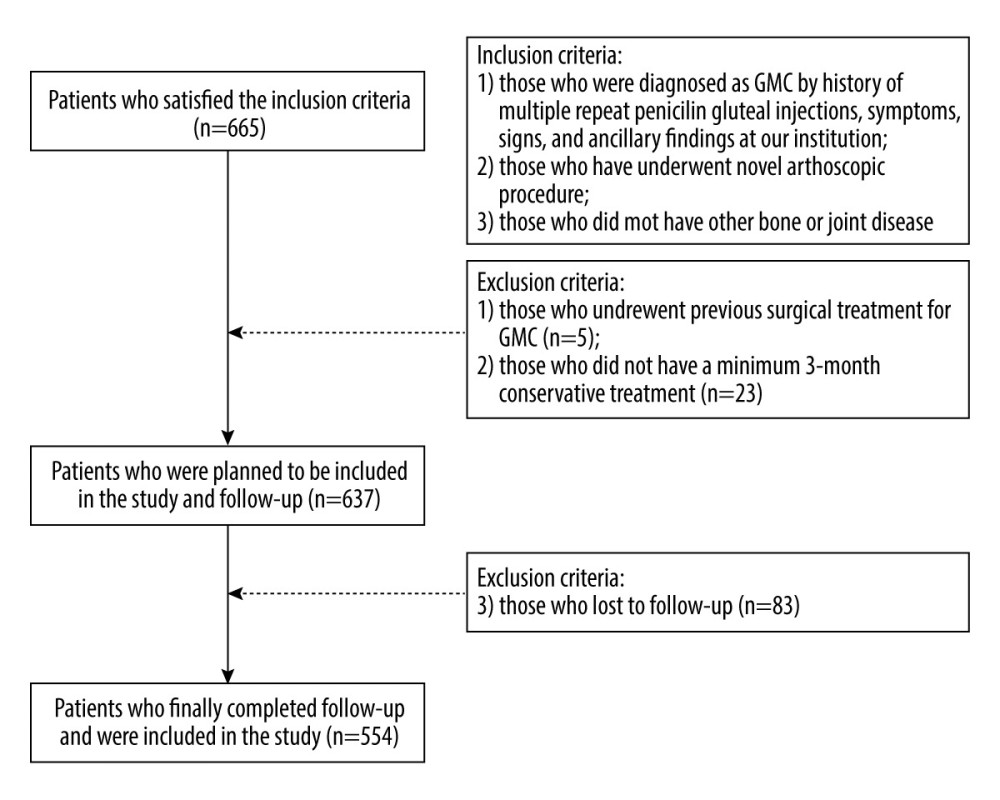 Figure 2. Patient selection in this study. Figure were created by Word Processing System, version: 12.1.0.16120, manufacturer: Kingsoft Corporation Limited.
Figure 2. Patient selection in this study. Figure were created by Word Processing System, version: 12.1.0.16120, manufacturer: Kingsoft Corporation Limited. 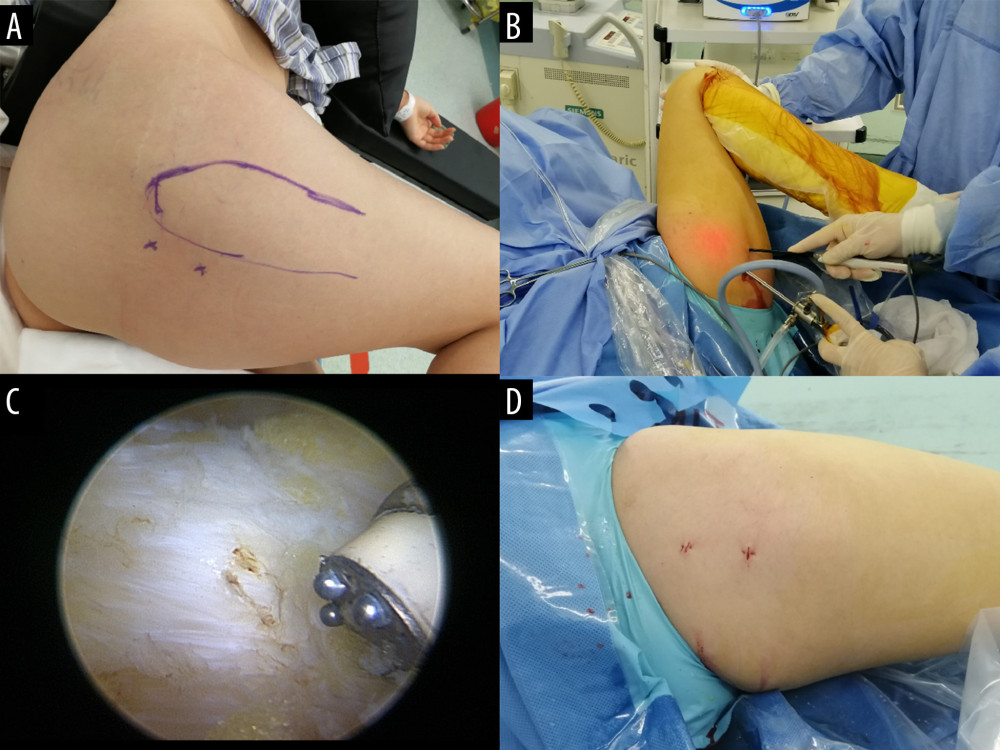 Figure 3. Procedure of the novel arthroscopic surgical approach for GMC patients. (A) Marking the surgical position and portal Including GT, the proximal portal (approximately 1 cm behind the apex of the GT), and the distal portal (4 cm away from the proximal portal). (B) The endoscope was inserted by the proximal portal and the planer or radiofrequency knife was inserted by the distal portal, and the assistant moved the patient’s hip sufficiently to completely expose all contracted muscle tissue. (C) The contracture band was visible under the microscope and released by the radiofrequency knife. (D) Both portals were sutured.
Figure 3. Procedure of the novel arthroscopic surgical approach for GMC patients. (A) Marking the surgical position and portal Including GT, the proximal portal (approximately 1 cm behind the apex of the GT), and the distal portal (4 cm away from the proximal portal). (B) The endoscope was inserted by the proximal portal and the planer or radiofrequency knife was inserted by the distal portal, and the assistant moved the patient’s hip sufficiently to completely expose all contracted muscle tissue. (C) The contracture band was visible under the microscope and released by the radiofrequency knife. (D) Both portals were sutured.  Figure 4. Recovery of symptoms for the patient in Figure 1 (A) and (B) at the follow-up. (A, B) The patient could cross his legs while sitting down. (C) The patient could squat with his legs together.
Figure 4. Recovery of symptoms for the patient in Figure 1 (A) and (B) at the follow-up. (A, B) The patient could cross his legs while sitting down. (C) The patient could squat with his legs together. Tables
Table 1. Assessment criteria for symptoms for patients with GMC.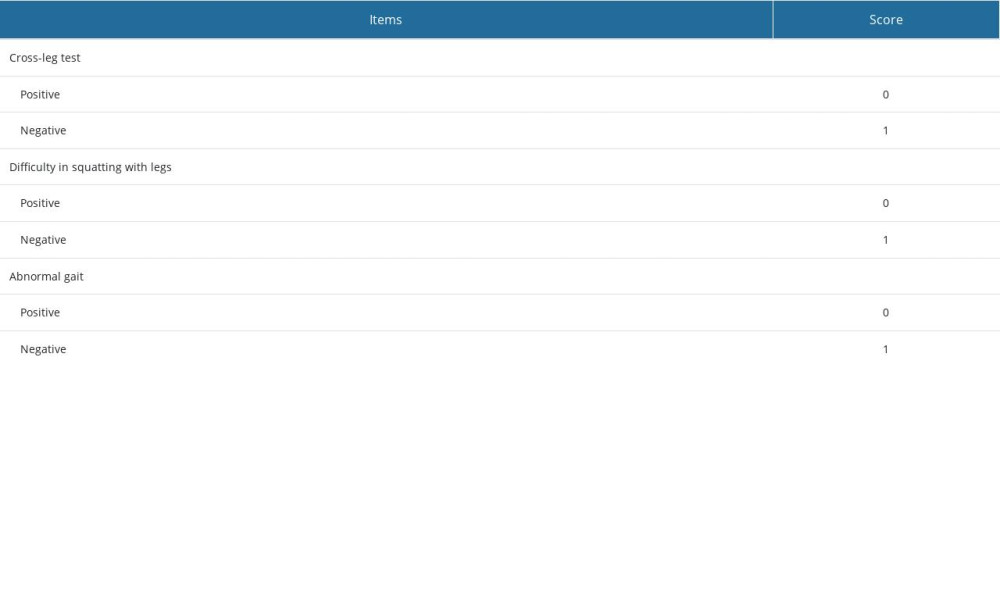 Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.
Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.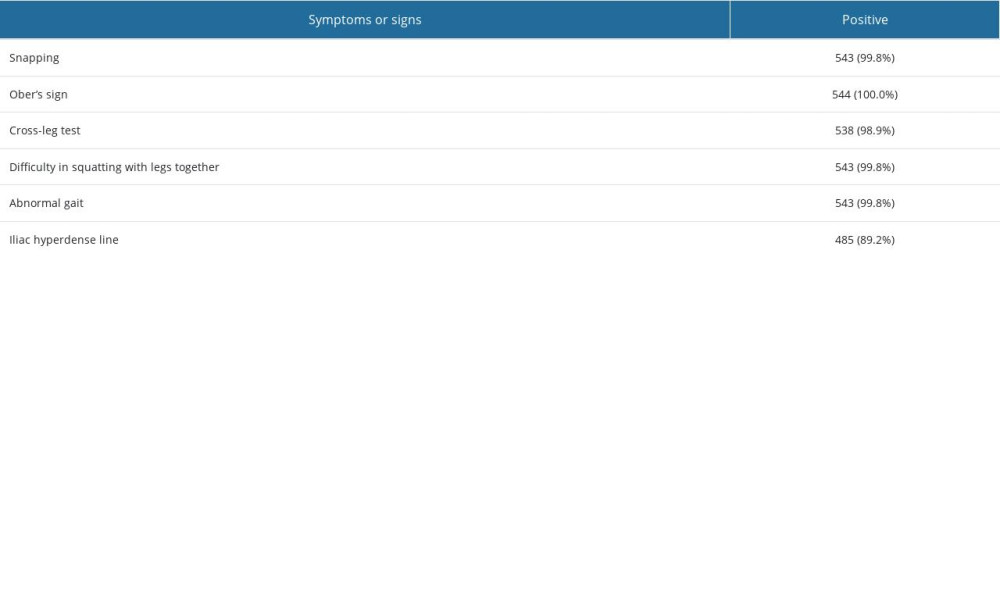 Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.
Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.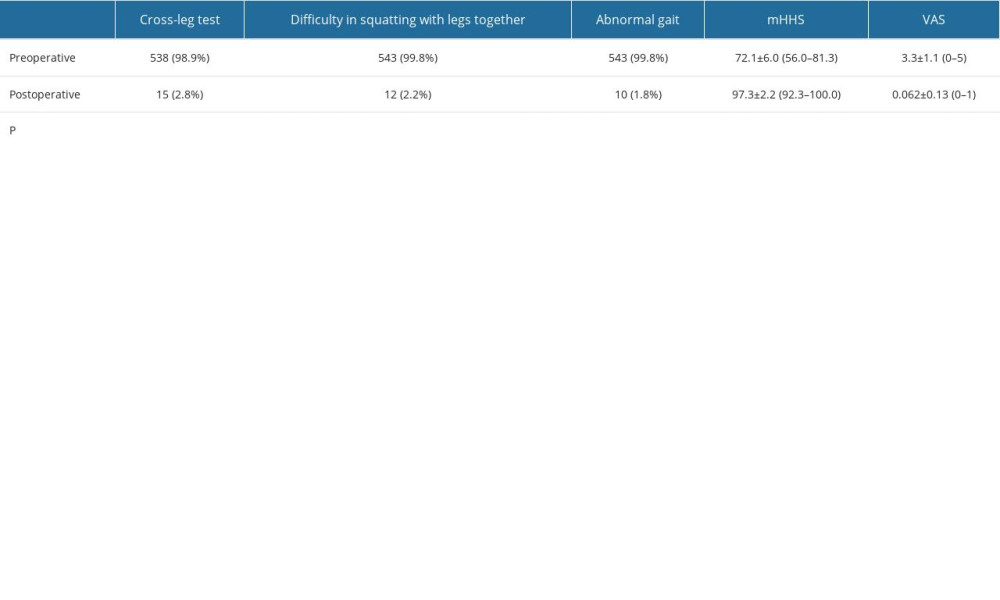 Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex.
Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex.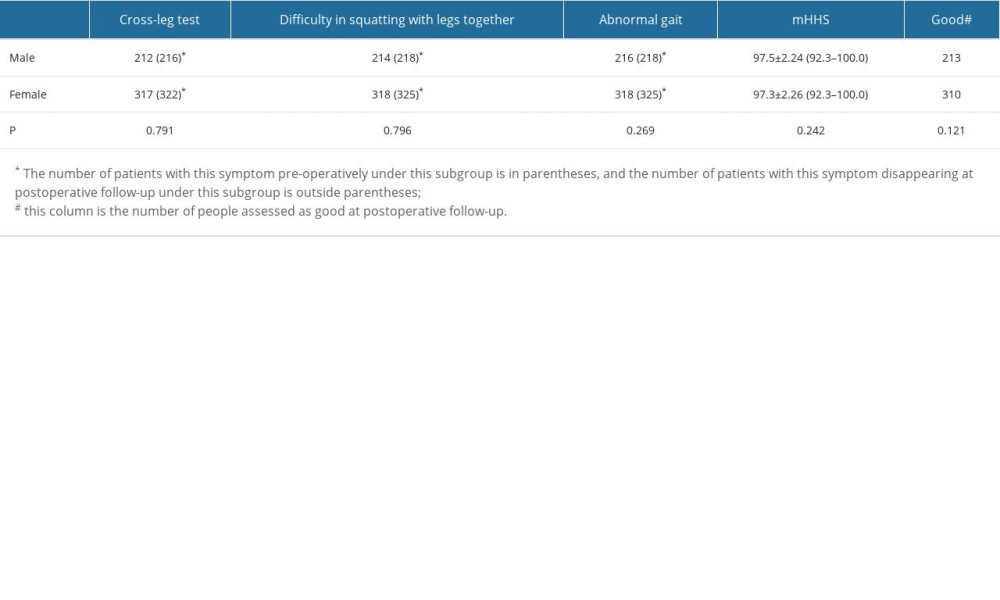
References
1. Peiro A, Fernandez CI, Gomar F, Gluteal fibrosis: J Bone Joint Surg Am, 1975; 57; 987-90
2. Hang YS, Contracture of the hip secondary to fibrosis of the gluteus maximus muscle: J Bone Joint Surg Am, 1979; 61; 52-55
3. Rai S, Meng C, Wang X, Gluteal muscle contracture: Diagnosis and management options: SICOT J, 2017; 3; 1
4. Yuan BT, Qu F, Wang SX, Histology and molecular pathology of iliotibial tract contracture in patients with gluteal muscle contracture: Biosci Rep, 2019; 3(9); BSR20181351
5. Zhao FY, Dong HM, Huang HJ, The application of arthroscopic techniques in the diagnosis and treatment of hip-related conditions in China: Orthop Surg, 2021; 13; 1697-706
6. Schaberg JE, Harper MC, Allen WC, The snapping hip syndrome: Am J Sports Med, 1984; 12; 361-65
7. Choi YS, Lee SM, Song BY, Dynamic sonography of external snapping hip syndrome: J Ultrasound Med, 2002; 21; 753-58
8. Polesello GC, Queiroz MC, Domb BG, Surgical technique: Endoscopic gluteus maximus tendon release for external snapping hip syndrome: Clin Orthop Relat Res, 2013; 471; 2471-76
9. Musick SRM, Varacallo, snapping hip syndrome: StatPearls, 2022, Treasure Island (FL), StatPearls Publishing LLC StatPearls Publishing Copyright 2022
10. Shrestha A, Wu P, Ge H, Clinical outcomes of arthroscopic surgery for external snapping hip: J Orthop Surg Res, 2017; 12; 81
11. White RA, Hughes MS, Burd T, A new operative approach in the correction of external coxa saltans: The snapping hip: Am J Sports Med, 2004; 32; 1504-8
12. Provencher MT, Hofmeister EP, Muldoon MP, The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band: Am J Sports Med, 2004; 32; 470-76
13. Lewis CL, Extra-articular snapping hip: A literature review: Sports Health, 2010; 2; 186-90
14. Jacobsen JS, Thorborg K, Søballe K, Eccentric hip abductor weakness in patients with symptomatic external snapping hip: Scand J Med Sci Sports, 2012; 12; e140-46
15. Yoon JY, Kwak HS, Yoon KS, Arthroscopic treatment for external snapping hip: Hip Pelvis, 2014; 26; 173-77
16. Reich MS, Shannon C, Tsai E, Hip arthroscopy for extra-articular hip disease: Curr Rev Musculoskelet Med, 2013; 6; 250-57
17. Ilizaliturri VM, Camacho-Galindo J, Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon: Sports Med Arthrosc Rev, 2010; 18; 120-27
18. Huang JB, Ge H, Zhang YL, The role of arthroscopic release of gluteal muscle contracture in improving patellofemoral instability: J Orthop Surg Res, 2019; 14; 159
19. Cai JH, Gan LF, Zheng HL, Iliac hyperdense line: A new radiographic sign of gluteal muscle contracture: Pediatr Radiol, 2005; 35; 995-97
20. Spina AA, External coxa saltans (snapping hip) treated with Active Release Techniques: A case report: J Can Chiropr Assoc, 2007; 51; 23-29
21. Fu D, Yang S, Xiao B, Comparison of endoscopic surgery and open surgery for gluteal muscle contracture: J Pediatr Orthop, 2011; 31; e38-43
22. Dai Z, Chen Z, Liao Y, Comparison of arthroscopic versus open surgery on external snapping hip caused by gluteal muscle contracture: Hip Int, 2018; 28; 173-77
23. Zhang T, Xu S, Li H, Comparison of the clinical effects of arthroscopic surgery vs open surgery for grade II gluteal muscle contracture in adults: Exp Ther Med, 2018; 16; 364-69
24. Ilizaliturri VM, Martinez-Escalante FA, Chaidez PA, Endoscopic iliotibial band release for external snapping hip syndrome: Arthroscopy, 2006; 22; 505-10
25. Liu YJ, Wang Y, Xue J, Arthroscopic gluteal muscle contracture release with radiofrequency energy: Clin Orthop Relat Res, 2009; 467; 799-804
26. Rai S, Jin S, Meng C, Arthroscopic release using F and C method versus conventional open release method in the treatment of gluteal muscle contracture: A comparative study: BMC Musculoskelet Disord, 2017; 18; 113
27. Ye B, Zhou P, Xia Y, New minimally invasive option for the treatment of gluteal muscle contracture: Orthopedics, 2012; 35; e1692-8
28. Gao SG, Liu WJ, Yang M, Clinical results of arthroscopic tight fibrous band release for adult moderate-to-severe gluteal fibrosis using anterior and posterior portals: A retrospective analysis of 118 consecutive cases: BMC Musculoskelet Disord, 2021; 22; 28
29. Tang X, Qi W, Liu Y, Arthroscopic C-shaped release around the greater trochanter for gluteal muscle contracture: Orthop Surg, 2021; 13; 1765-72
30. Edwards PK, Queen RM, Butler RJ, Are range of motion measurements needed when calculating the harris hip score?: J Arthroplasty, 2016; 31; 815-19
31. Byrd JWK, Jones S, Prospective analysis of hip arthroscopy with 2-year follow-up: Arthroscopy, 2000; 16; 578-87
32. Liu GH, Cao FQ, Yang SH, Factors influencing the treatment of severe gluteal muscle contracture in children: J Pediatr Orthop B, 2011; 20; 67-69
Figures
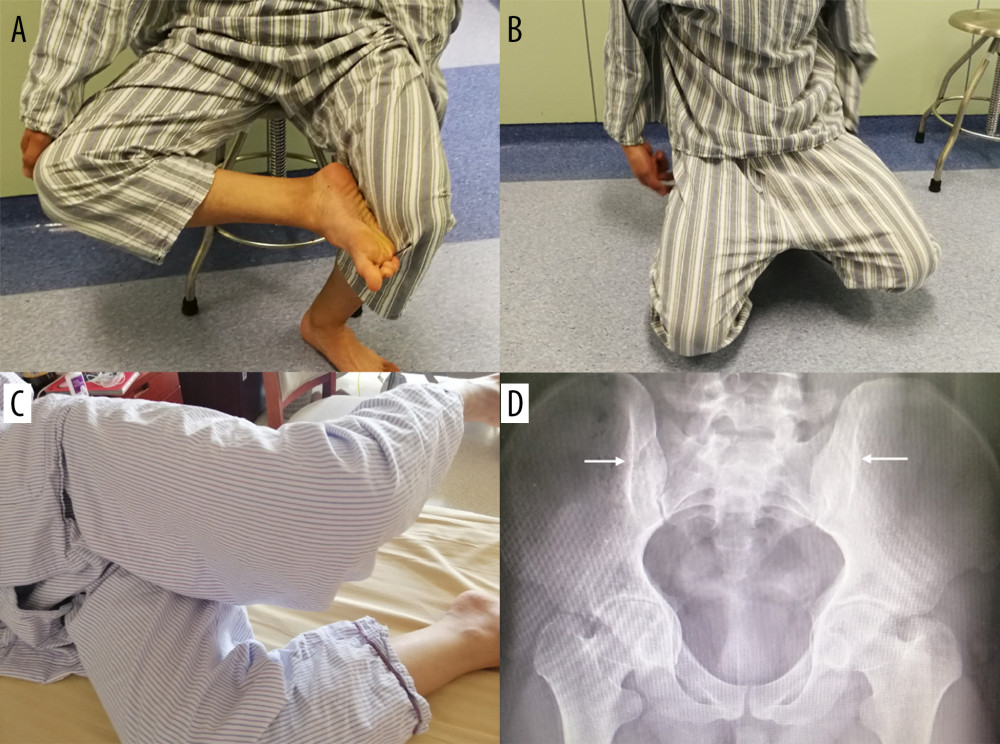 Figure 1. Symptoms, signs, and radiographic findings of a patient with GMC. (A) The patient could not cross his leg while sitting down. (B) The hip joint is fixed in abduction and external rotation when the patient squats and cannot squat with the legs together. (C) The doctor fixed the patient’s pelvis and ankle with the knee flexed at 90°, and then the doctor released the patient, and the patient maintained an upward and abducted position of the affected limb, which was a positive Ober’s sign. (D) Iliac hyperdense line sign (arrow).
Figure 1. Symptoms, signs, and radiographic findings of a patient with GMC. (A) The patient could not cross his leg while sitting down. (B) The hip joint is fixed in abduction and external rotation when the patient squats and cannot squat with the legs together. (C) The doctor fixed the patient’s pelvis and ankle with the knee flexed at 90°, and then the doctor released the patient, and the patient maintained an upward and abducted position of the affected limb, which was a positive Ober’s sign. (D) Iliac hyperdense line sign (arrow).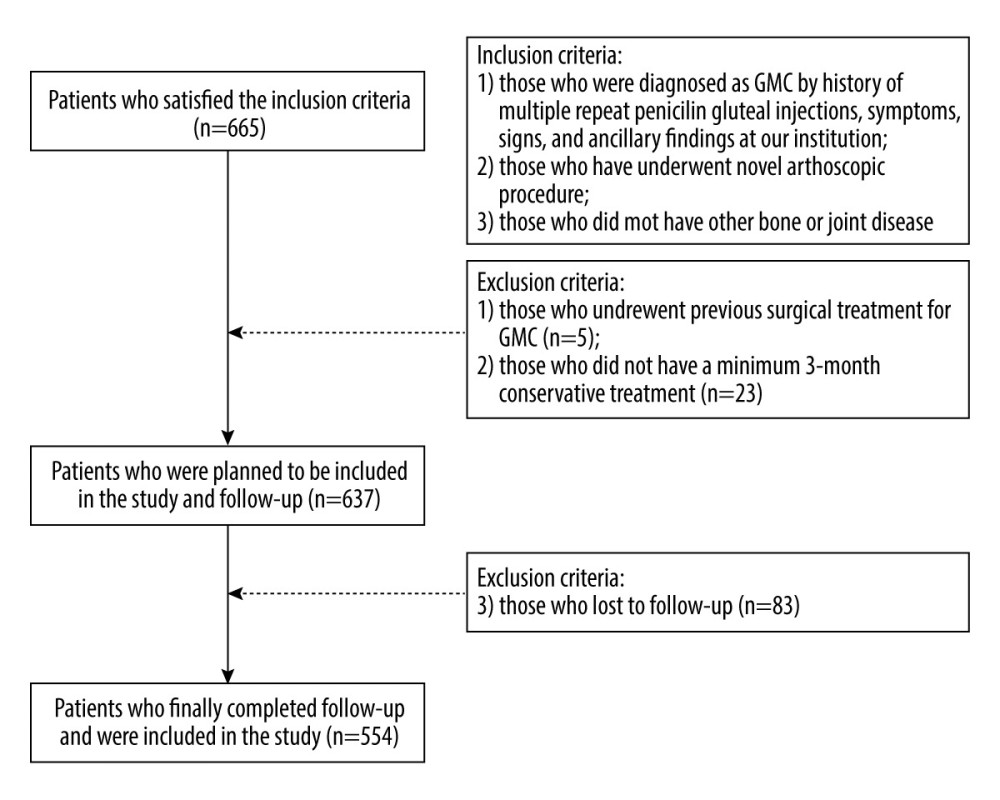 Figure 2. Patient selection in this study. Figure were created by Word Processing System, version: 12.1.0.16120, manufacturer: Kingsoft Corporation Limited.
Figure 2. Patient selection in this study. Figure were created by Word Processing System, version: 12.1.0.16120, manufacturer: Kingsoft Corporation Limited.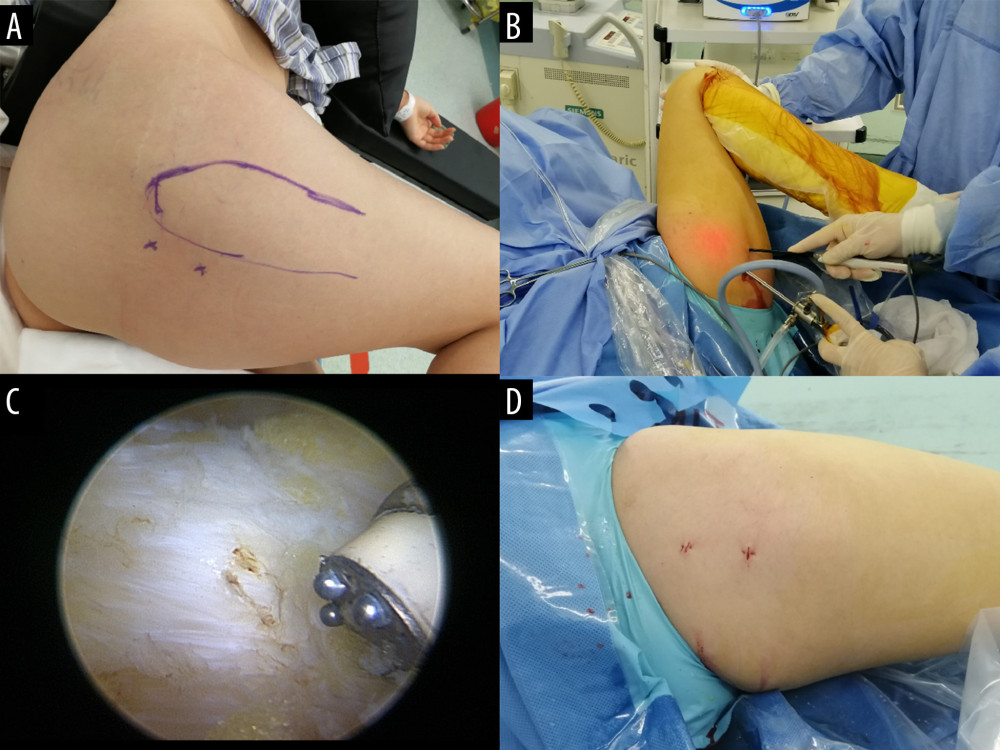 Figure 3. Procedure of the novel arthroscopic surgical approach for GMC patients. (A) Marking the surgical position and portal Including GT, the proximal portal (approximately 1 cm behind the apex of the GT), and the distal portal (4 cm away from the proximal portal). (B) The endoscope was inserted by the proximal portal and the planer or radiofrequency knife was inserted by the distal portal, and the assistant moved the patient’s hip sufficiently to completely expose all contracted muscle tissue. (C) The contracture band was visible under the microscope and released by the radiofrequency knife. (D) Both portals were sutured.
Figure 3. Procedure of the novel arthroscopic surgical approach for GMC patients. (A) Marking the surgical position and portal Including GT, the proximal portal (approximately 1 cm behind the apex of the GT), and the distal portal (4 cm away from the proximal portal). (B) The endoscope was inserted by the proximal portal and the planer or radiofrequency knife was inserted by the distal portal, and the assistant moved the patient’s hip sufficiently to completely expose all contracted muscle tissue. (C) The contracture band was visible under the microscope and released by the radiofrequency knife. (D) Both portals were sutured. Figure 4. Recovery of symptoms for the patient in Figure 1 (A) and (B) at the follow-up. (A, B) The patient could cross his legs while sitting down. (C) The patient could squat with his legs together.
Figure 4. Recovery of symptoms for the patient in Figure 1 (A) and (B) at the follow-up. (A, B) The patient could cross his legs while sitting down. (C) The patient could squat with his legs together. Tables
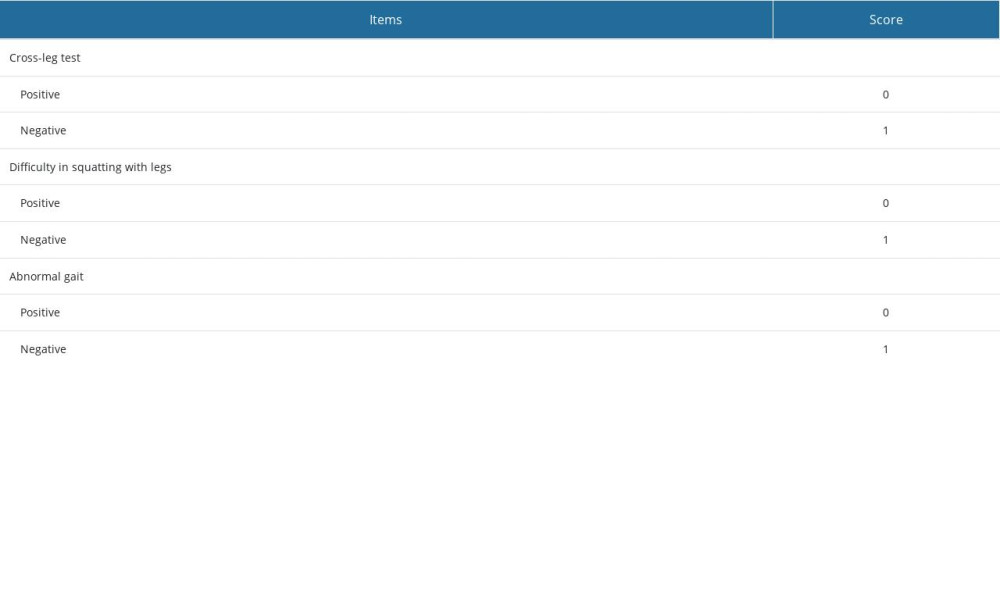 Table 1. Assessment criteria for symptoms for patients with GMC.
Table 1. Assessment criteria for symptoms for patients with GMC.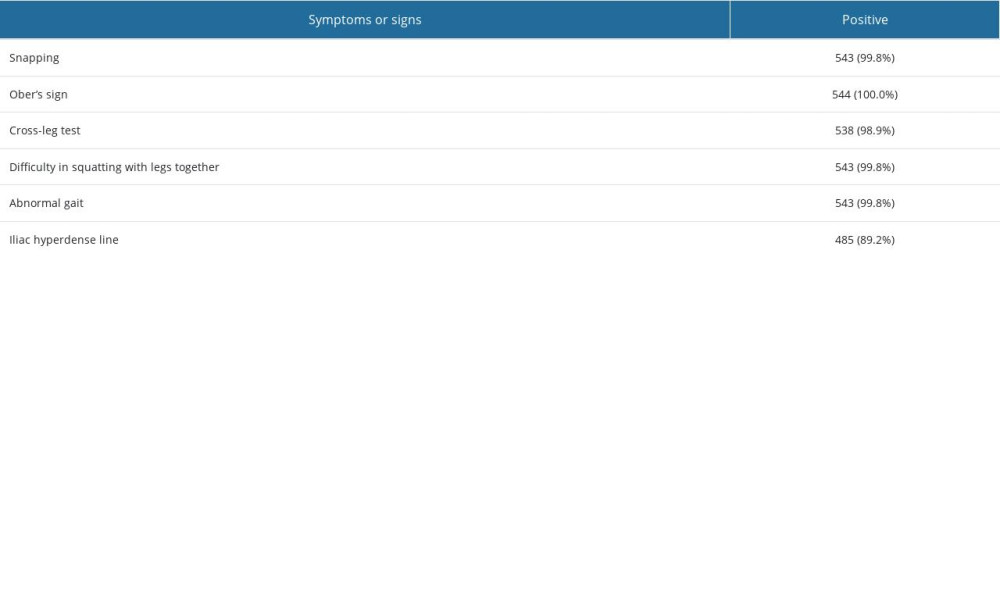 Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.
Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.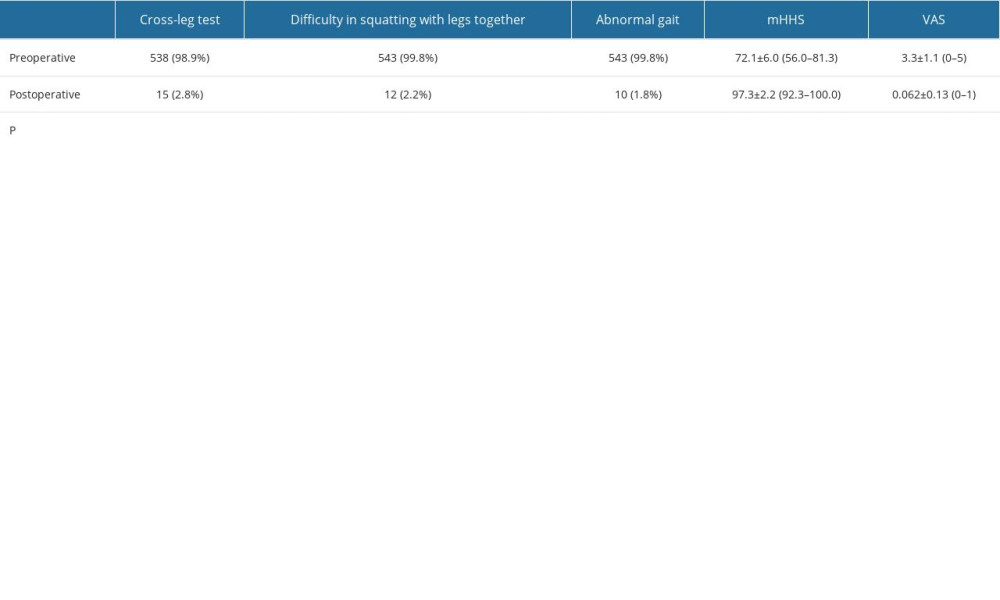 Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.
Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.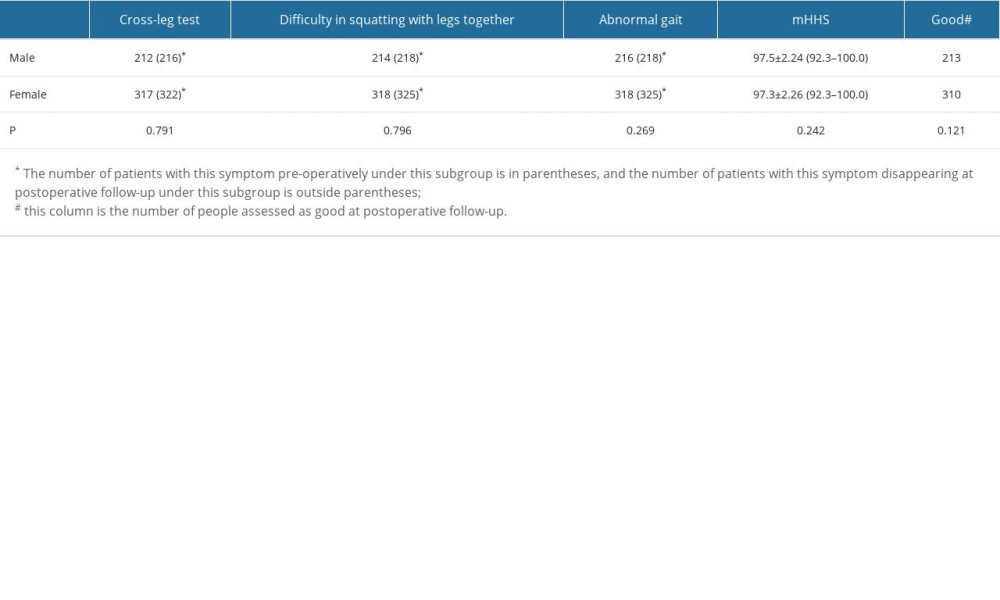 Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex.
Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex.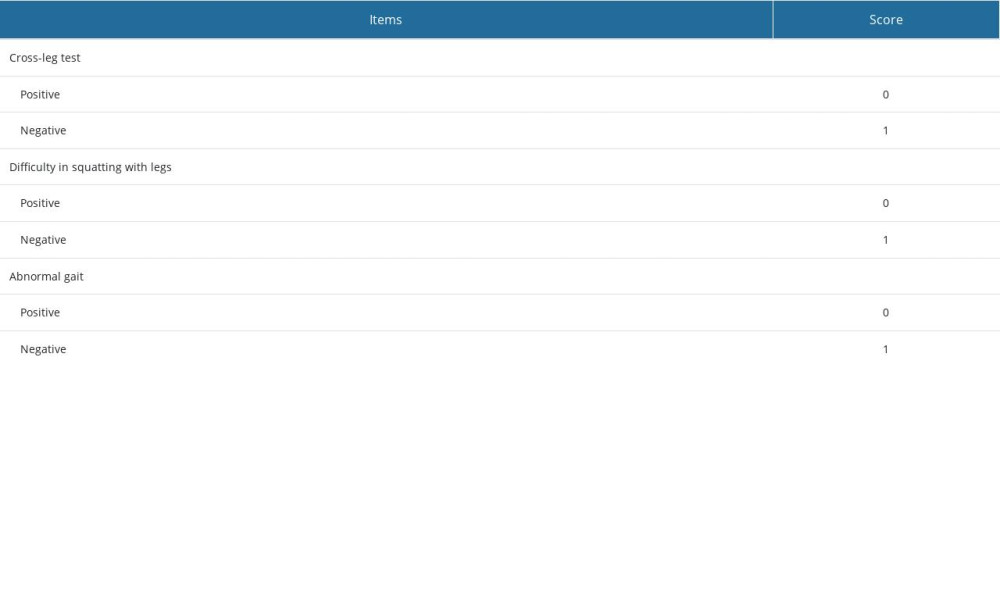 Table 1. Assessment criteria for symptoms for patients with GMC.
Table 1. Assessment criteria for symptoms for patients with GMC.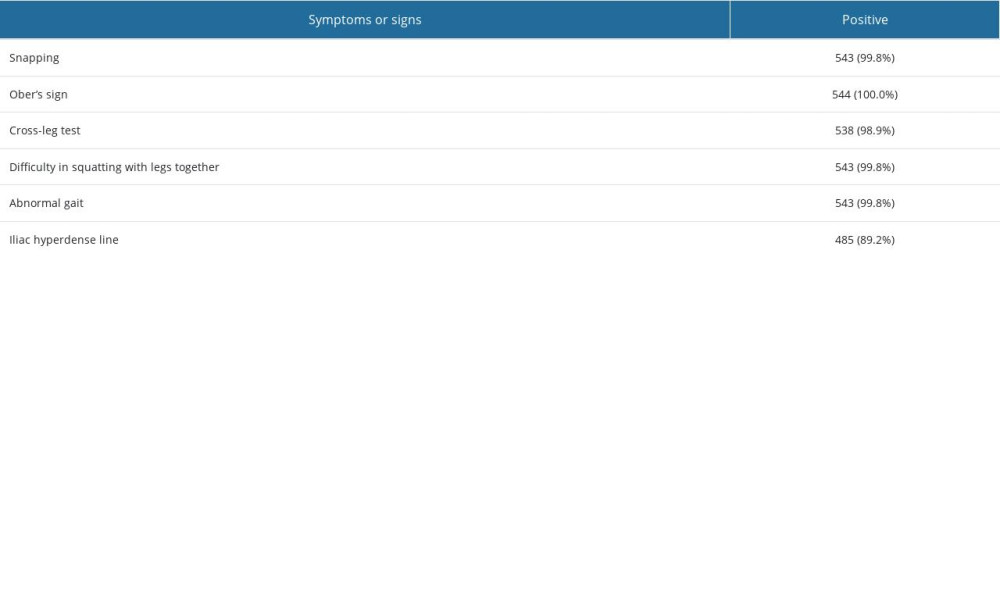 Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.
Table 2. Percentage of positive preoperative symptoms, signs, and radiographic finding.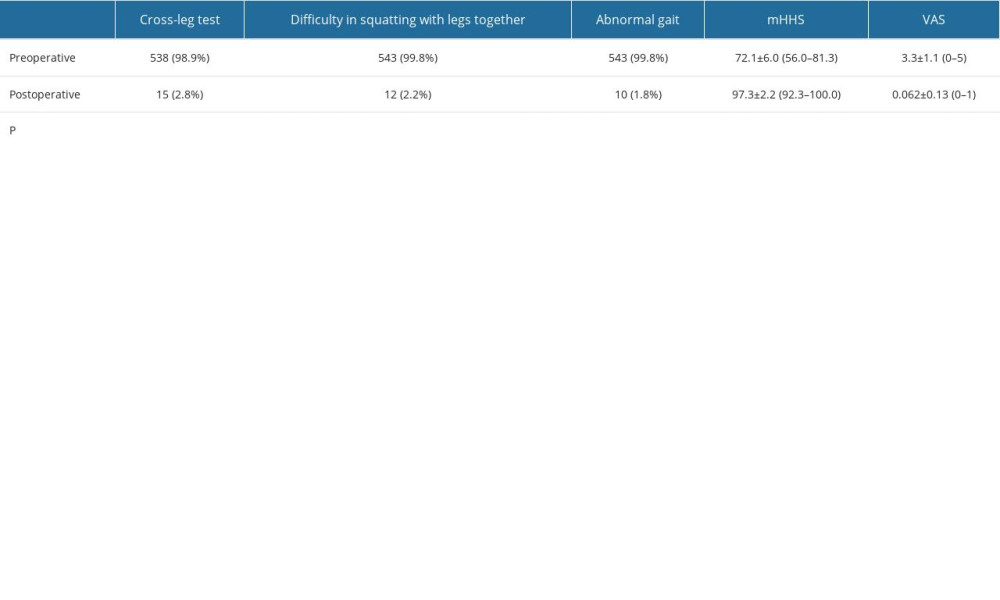 Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.
Table 3. Symptoms mHHS and VAS of all patients between preoperative and postoperative follow-up.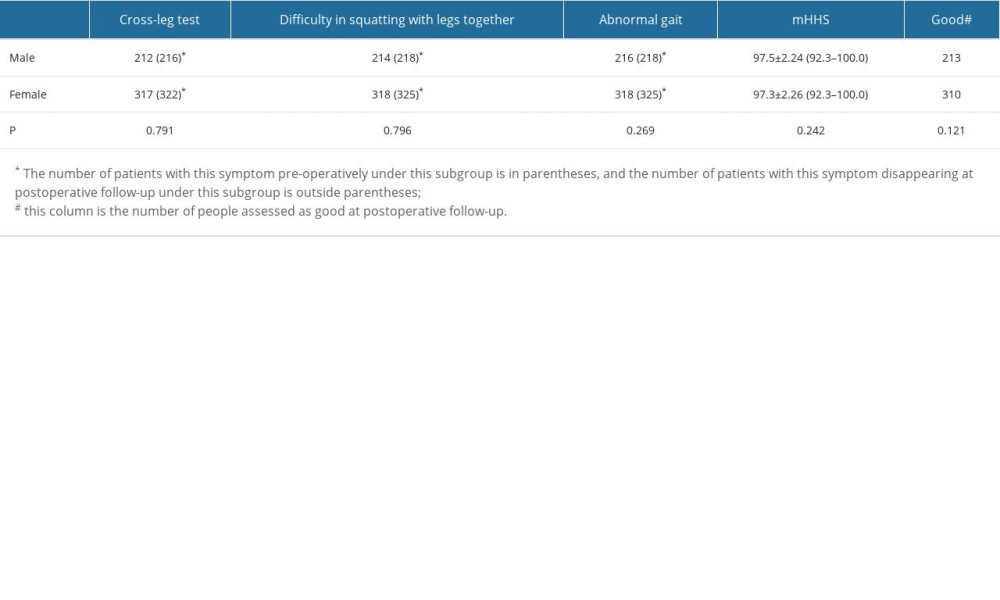 Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex.
Table 4. Comparison of the improvement in symptoms, mHHS, and good rates in patients of different sex. In Press
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








