05 May 2024: Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Patients
Heng Deng12ABCDG, Xiaoli Fang3EF, Hongchang Wang4D, Ming Li23AF*DOI: 10.12659/MSM.943126
Med Sci Monit 2024; 30:e943126
Abstract
BACKGROUND: Severe anemia caused by hemorrhoidal hematochezia is typically treated preoperatively with reference to severe anemia treatment strategies from other etiologies. This retrospective cohort study included 128 patients with hemorrhoidal severe anemia admitted to 3 hospitals from September 1, 2018, to August 1, 2023, and aimed to evaluate preoperative blood transfusion requirements.
MATERIAL AND METHODS: Of 5120 patients with hemorrhoids, 128 (2.25%; male/female: 72/56) experienced hemorrhoidal severe anemia, transfusion, and Milligan-Morgan surgery. Patients were categorized into 2 groups based on their preoperative hemoglobin (PHB) levels after transfusion: PHB ≥70 g/L as the liberal-transfusion group (LG), and PHB <70 as the restrictive-threshold group (RG). The general condition, bleeding duration, hemoglobin level on admission, transfusion volume, length of stay, immune transfusion reaction, surgical duration, and hospitalization cost were compared between the 2 groups.
RESULTS: Patients with severe anemia (age: 41.07±14.76) tended to be younger than those with common hemorrhoids (age: 49.431±15.59 years). The LG had a significantly higher transfusion volume (4.77±2.22 units), frequency of immune transfusion reactions (1.22±0.58), and hospitalization costs (16.69±3.31 thousand yuan) than the RG, which had a transfusion volume of 3.77±2.09 units, frequency of immune transfusion reactions of 0.44±0.51, and hospitalization costs of 15.00±3.06 thousand yuan. Surgical duration in the LG (25.69±14.71 min) was significantly lower than that of the RG (35.24±18.72 min).
CONCLUSIONS: Patients with hemorrhoids with severe anemia might require a lower preoperative transfusion threshold than the currently recognized threshold, with an undifferentiated treatment effect and additional benefits.
Keywords: Anemia, Blood Transfusion, Cohort Studies, hemorrhoids, Transfusion reaction
Introduction
Hemorrhoids are a common condition and account for nearly 80% of anorectal surgeries [1]. The most commonly reported symptoms of hemorrhoids are pain, bleeding during defecation, and prolapse [2]. While bleeding hemorrhoids are universal, life-threatening bleeding is rare, occurring in only 5 out of 1 million people, both in acute-onset and chronic cases [3,4]. Furthermore, some reported causes of lower gastrointestinal bleeding do not include hemorrhoidal bleeding [5]. Hemorrhoids are rarely mentioned as a cause of threatening lower gastrointestinal bleeding [6]. These findings suggest that hemorrhoidal bleeding may have a specific pathology. Numerous studies have shown that blood transfusion has benefits and risks. While it can improve a patient’s ability to withstand surgical trauma and recovery [7], it can also increase postoperative mortality and the risk of wound infection [8]. Reducing the frequency of blood transfusions while ensuring safety can lead to several benefits, including cost reduction, alleviating stress on the circulatory system and liver, minimizing disease transmission, and streamlining blood preservation, cold chain distribution, and other associated processes [9]. Therefore, it is necessary to explore an optimal preoperative transfusion cutoff value [10].
A recent study found that patients with hemorrhoidal anemia had an average preoperative hemoglobin (PHB) level of 75 g/L [11]. The European Society of Gastrointestinal Endoscopy Guideline recommends transfusing red blood cells in patients with a hemoglobin threshold of ≤70 g/L in cases of lower gastrointestinal bleeding [12]. However, considering that hemorrhoids are a rare cause of severe anemia, it raises the question of whether it is appropriate for hemorrhoids to share a common preoperative transfusion standard with the other causes of severe anemia.
To promote recognition, we aim to identify clinical features of severe anemia associated with hemorrhoids by comparing patients whose transfused hemoglobin did not meet the threshold of those whose transfused hemoglobin exceeded the threshold. Therefore, this retrospective cohort study included 128 patients with hemorrhoidal severe anemia admitted to 3 hospitals between September 1, 2018, and August 1, 2023, and aimed to evaluate preoperative blood transfusion requirements.
Material and Methods
PRINCIPLES OF THE STUDY:
The ethical approval (NO.2023SSSP07) from the Ethics Committee of the Second Affiliated Hospital of Anhui University of Chinese Medicine, and the patients’ informed consent was obtained. A 22-item checklist from the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies [13], was used for this study.
PATIENTS:
The study population consisted of 5120 patients with hemorrhoids who were retrospectively analyzed across 3 affiliated hospitals of a single academic institution. The data collection period spanned from September 1, 2018, to August 1, 2023. By applying the following criteria, 128 patients were included in the final analysis, using an electronic medical order calendar system. It is worth noting that all patients received standardized treatment due to the affiliation of the 3 hospitals to the same scientific research institution (Figure 1).
The inclusion criteria were as follows: (1) presence of bloody and bright red stool; (2) experience of dizziness and palpitation; (3) confirmation of hemorrhoids through anal digital examination and anoscopy [14]; (4) severe anemia defined as hemoglobin level on admission (AHB) <60 g/L; and (5) receipt of transfusion with concentrated erythrocyte suspension by the patients.
The exclusion criteria were as follows: (1) portal hypertension diagnosis based on portal vein ultrasound; (2) patients with a confirmed cause of anemia other than hemorrhoids; and (3) patients who had not undergone Milligan-Morgan surgery. Because intraoperative bleeding is more manageable with Milligan-Morgan surgery than in other procedures, all patients with anemia treated at the 3 hospitals had opted for this operation. The purpose of exclusion criterion 3 was to exclude patients who, after receiving a transfusion, voluntarily requested conservative treatment.
SCHEME OF THE STUDY:
The preoperative transfusion threshold for hemorrhoidal patients with severe anemia has always been a PHB value <70 g/L, as determined by peripheral blood routine examination. Patients with values that fell below this threshold and who were scheduled for surgery would receive blood transfusions in order to reach this value. However, due to limited availability of blood resources, particularly during the COVID-19 pandemic, the post-transfusion peripheral hemoglobin levels of certain patients did not meet the established standard. The availability of blood was beyond the control of the medical staff. Hence, the patients were divided into 2 groups based on their post-transfusion PHB values: the restrictive-threshold group (RG) consisted of 44 patients with PHB <70 g/L, and the liberal-transfusion group (LG) consisted of 84 patients with PHB ≥70 g/L. Apart from the amount of blood transfusions, there were no differences in perioperative management between the 2 groups. A total of 5120 patients with a diagnosis of hemorrhoids were included in the study. Among them, 205 patients with moderate or mild anemia and 11 patients with severe anemia were excluded from the analysis, as they did not undergo transfusion or surgery.
First, this study focused on comparing the general conditions of 128 patients who met the inclusion criteria with those of 4776 patients who underwent surgery for hemorrhoids but did not have anemia. Second, demographic information, duration of hemorrhoidal bleeding, hemoglobin levels at admission, blood transfusion volume, PHB, immune transfusion reaction, internal hemorrhoids stage (grade), surgical duration, length of stay, and hospitalization costs were compared between the RG and LG groups (Figure 2). To ensure safety, hospital discharge was approved only after confirming the absence of postoperative wound bleeding and pain. The immune transfusion reaction was calculated as the frequency of symptoms such as fever, respiratory distress, decreased blood pressure, pain, rash, changes in urine volume and color, and jaundice.
STATISTICAL ANALYSIS:
Statistical analysis was performed in R 4.2.1, using the ggplot2 package to visualize the data. Since the data did not follow a bivariate normal distribution or the overall distribution was unknown, the Spearman rank statistical method was used. The Wilcoxon rank-sum test was used to compare data between groups that did not meet the assumption of normality. This retrospective cohort study aimed to test the equivalence of restricted transfusion vs liberal transfusion. The mean value of PHB in the RG was 63.52 g/L, and the mean of PHB in the LG was 83.86 g/L, with corresponding standard deviations of 3.69 g/L and 10.06 g/L, respectively. A bilateral test with a significance level of P<0.05 was conducted, and a sample size of 40 was included for both groups [15]. To enhance the accuracy of the analysis, data from all patients over the past 5 years were included.
Results
CHARACTERISTICS AND PROPORTION OF PATIENTS WITH HEMORRHOIDAL SEVERE ANEMIA:
A retrospective analysis was conducted on the electronic medical records of 5120 patients with hemorrhoids over the previous 5 years. Among them, 128 (2.25%) patients experienced severe anemia, necessitating transfusions and Milligan-Morgan surgery. Of these patients, 72 were men and 56 were women. The age distribution revealed that most patients were between 27 and 42 years old (Figure 3). Upon hospitalization, the average AHB value was 48.85±7.93 g/L. The duration of hemorrhoidal bleeding was 33.07±24.28 days, indicating a chronic course. Interestingly, patients with severe anemia (age: 41.07±14.76 years) were significantly younger than those without anemia (age: 49.431±15.59 years); however, the opposite was true in terms of hospital costs. No significant differences were observed in other aspects (Table 1).
DIFFERENCE IN PHB BETWEEN LG AND RG GROUPS:
The average PHB value for the 84 patients in the LG group was 83.86±10.06 g/L, while the average PHB value for the 44 patients in the RG group was 63.52±3.69 g/L (P<0.001). It is worth noting that there was no significant difference observed in AHB between the 2 groups (Figure 4).
GENERAL INFORMATION, DURATION OF HEMORRHOIDAL BLEEDING, LENGTH OF STAY, AND INTERNAL HEMORRHOIDS STAGE (GRADE) COMPARISON BETWEEN LG AND RG GROUPS:
Statistical analysis was performed on various data variables for patients in the LG, including sex (46 men, 38 women), age (40.86±15.66 years), weight (64.76±12.24 kg), duration of hemorrhoidal bleeding (33.09±24.03 days), length of stay (19.51±12.42 days), and internal hemorrhoid stage (2.22±0.85). Similarly, data collected and calculated for patients in the RG group included sex (26 male, 18 female), age (41.47±13.11 years), weight (65.09±10.74 kg), duration of hemorrhoidal bleeding (33.02±25.02 days), length of stay (17.51±11.59 days), and internal hemorrhoid stage (2.38±0.86) (Table 2). No statistically significant differences were observed between the 2 groups in the aforementioned factors (Figure 5).
BLOOD TRANSFUSION VOLUME, FREQUENCY OF IMMUNE TRANSFUSION REACTIONS, SURGICAL DURATION, AND HOSPITALIZATION COST COMPARISON BETWEEN LG AND RG GROUPS:
The blood transfusion volume (4.77±2.22 units), frequency of immune transfusion reactions (1.22±0.58), and hospitalization cost (16.69±3.31 thousand yuan) in the LG were significantly higher than those in the RG. In the RG, the blood transfusion volume was 3.77±2.09 units, the frequency of immune transfusion reactions was 0.44±0.51, and hospitalization costs were 15.00±3.06 thousand yuan. Additionally, the surgical duration in LG (25.69±14.71 min) was significantly lower than that in the RG (35.24±18.72 min) (Figure 5).
Discussion
Our results have indicated that the preoperative transfusion threshold for patients with hemorrhoidal severe anemic may be lower than the currently accepted threshold. Patients with preoperative hemoglobin levels of less than 70 g/L after transfusion did not experience a reduction in efficacy throughout the perioperative period. Severe anemia is diagnosed when the hemoglobin level is less than 60 g/L and is accompanied by resting shortness of breath. Anemia can be divided into 3 categories based on its cause: hematopoietic dysplasia, hemorrhagic, and hemolytic. Alongside addressing the underlying cause of the disease, it is crucial to target severe anemia. Preoperative anemia is significantly associated with increased perioperative risk, mortality, and worse treatment outcomes, including cardiovascular surgery [16], abdominal surgery [17], and joint surgery [18]. The presence of preoperative anemia as an independent risk factor underscores the importance of carefully assessing and managing it to enhance the postoperative outcome. International consensus guidelines consistently recommend blood transfusion for patients undergoing abdominal surgery with PHB <70 g/L and no history of cardiovascular disease [19]. The PHB threshold for patients undergoing cardiovascular surgery is increased to mitigate perioperative risk. According to the 2018 Frankfurt Consensus Conference, the transfusion threshold for cardiac surgery patients is set at PHB <75 g/L [20]. Studies have also demonstrated that raising PHB to 100 g/L has the same efficacy as reducing sickle hemoglobin to less than 30% (more allogeneic blood transfusions) and reduces the immune transfusion reaction, due to reduced transfusion [21]. Older individuals have less tolerance for anemia and require higher hemoglobin levels to achieve peak oxygen capacity, comparable to younger individuals [22]. These studies highlight that the underlying cause of anemia, type of surgery, and patient age and overall health status all influence the threshold of preoperative transfusion.
Hemorrhoidal bleeding is a common condition and can cause anemia. Previous reports have primarily focused on surgical management strategies, such as hemorrhoid embolization [23] and polidocanol foam sclerotherapy [24,25]. It is worth noting that the proportion of patients with hemorrhoids with severe anemia is very low [3], and the existing reports mainly concentrate on emergency treatment or case reports [11,26]. Consequently, there is little research regarding transfusion thresholds specifically for severe anemia caused by hemorrhoids. Clinicians have traditionally managed hemorrhoidal severe anemia by applying transfusion thresholds established for severe anemia caused by other factors. However, the pathology of hemorrhoidal bleeding has its own specificity. These include chronic bleeding, long duration of bleeding, and self-limiting bleeding [27]. Milligan-Morgan surgery is considered the first choice and the most common indication [28]; it allows for the removal of bleeding hemorrhoids under direct vision [29], addresses the cause of anemia, and minimizes intraoperative bleeding. Moreover, our results indicate that patients with hemorrhoidal severe anemia are often young or in the prime of their lives, which can explain their ability to tolerate lower levels hemoglobin. As a result, the preoperative transfusion threshold for hemorrhoidal severe anemia can also have its own measure. This study showed a statistically significant difference in PHB between the RG and LG groups. This highlights the practical significance of this grouping to guide clinical practice. There were no significant differences observed in sex, age, weight, and duration of hemorrhoidal bleeding, indicating that the 2 groups were comparable prior to transfusion intervention. Moreover, no significant disparities were found in length of stay between the 2 groups, implying that a higher PHB level did not result in additional benefits during the perioperative period. Notably, the RG group exhibited lower blood transfusion volume, frequency of immune transfusion reactions, and hospitalization cost than did the LG, suggesting that a lower PHB level can provide these additional advantages. Furthermore, no significant correlation was discovered between the stage of internal hemorrhoids and the duration of surgery. It is possible that the higher surgical duration in the RG group than in the LG can be attributed to the surgeons’ increased focus on hemostasis during the procedure.
However, retrospective cohort studies are still inferior to randomized controlled trials, with a lack objective scores in terms of precise bleeding quantity or duration. This study did not adequately operationalize PHB level as a study variable, resulting in no specific preoperative transfusion threshold. Further research is required to address these limitations.
Conclusions
A lower preoperative transfusion threshold than the currently recognized threshold might exist in patients with hemorrhoidal severe anemia, and may have an undifferentiated treatment effect and additional benefits.
Data Availability Statement
Raw data extracted from all transfusion medical records can be obtained from: https://osf.io/h3k6a/?view_only=eeafa75fd9a240a8996f29035cf117cc.
Figures
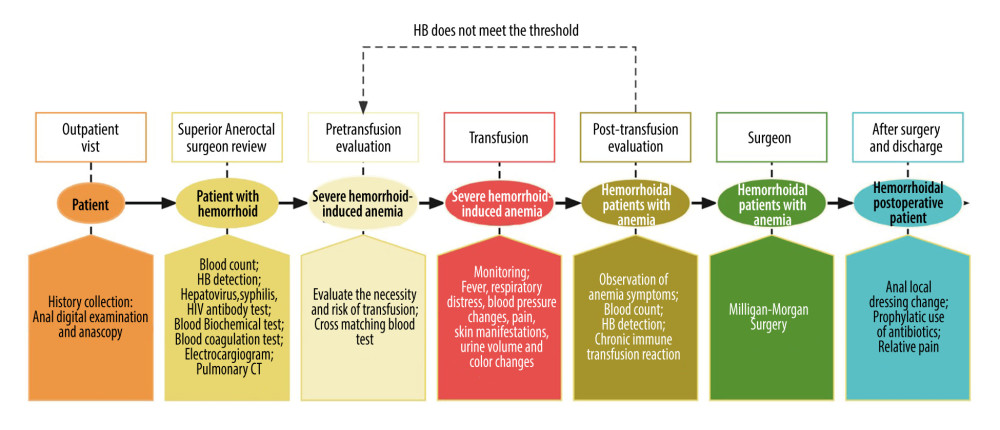 Figure 1. A uniform procedure for the treatment of patients with hemorrhoidal severe anemia. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.
Figure 1. A uniform procedure for the treatment of patients with hemorrhoidal severe anemia. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd. 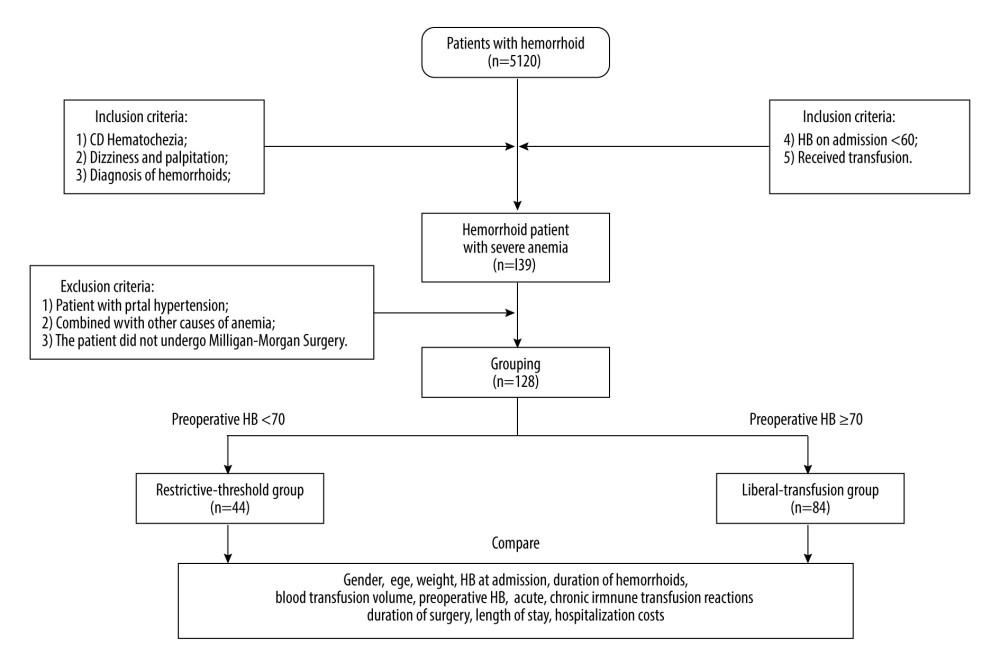 Figure 2. The process of the retrospective cohort study. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.
Figure 2. The process of the retrospective cohort study. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd. 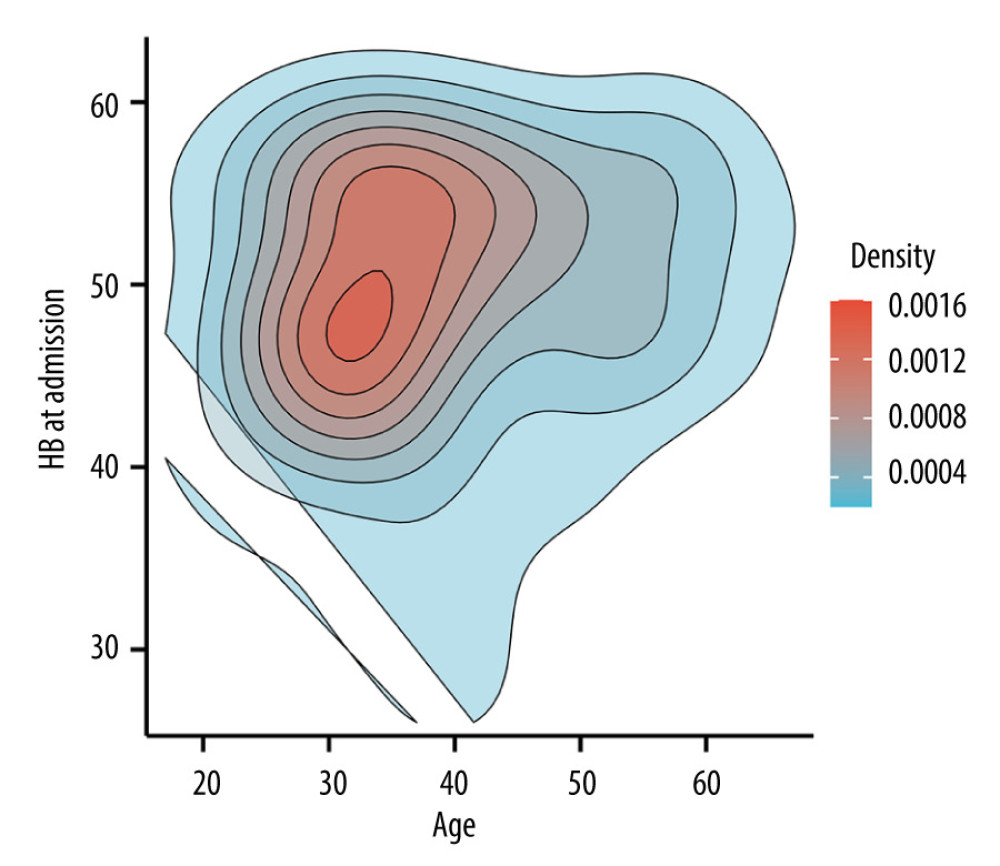 Figure 3. Two-dimensional density profile of patients with hemorrhoidal severe anemia illustrating the distribution of age and hemoglobin levels on admission (AHB). The intensity of the red color indicates the concentration of patients within each category. As shown in the figure, the largest number of patients falls within the age range of 27 to 42 years old, with AHB levels ranging from 43 to 57 g/L. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 3. Two-dimensional density profile of patients with hemorrhoidal severe anemia illustrating the distribution of age and hemoglobin levels on admission (AHB). The intensity of the red color indicates the concentration of patients within each category. As shown in the figure, the largest number of patients falls within the age range of 27 to 42 years old, with AHB levels ranging from 43 to 57 g/L. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd. 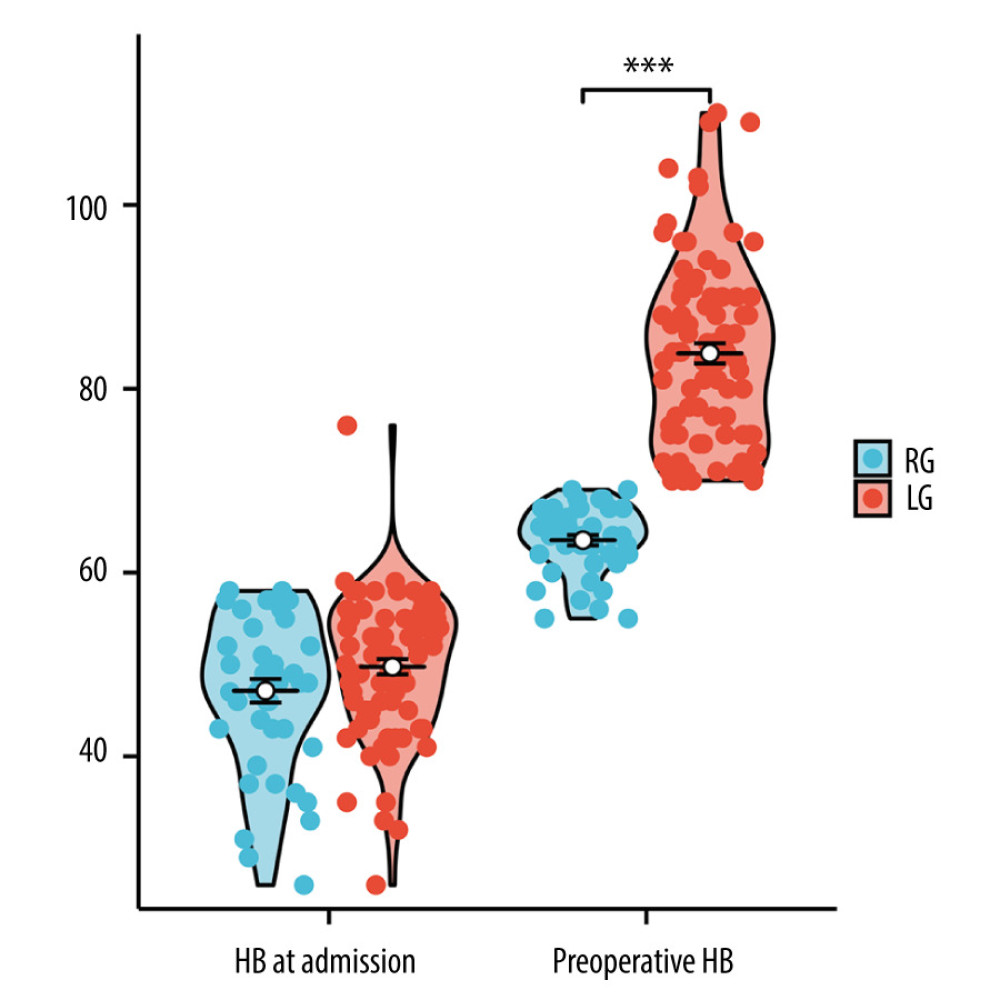 Figure 4. Group comparison chart showing the differences in preoperative hemoglobin levels (PHB) and hemoglobin levels on admission AHB between the 2 groups. *** P<0.001. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 4. Group comparison chart showing the differences in preoperative hemoglobin levels (PHB) and hemoglobin levels on admission AHB between the 2 groups. *** P<0.001. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd. 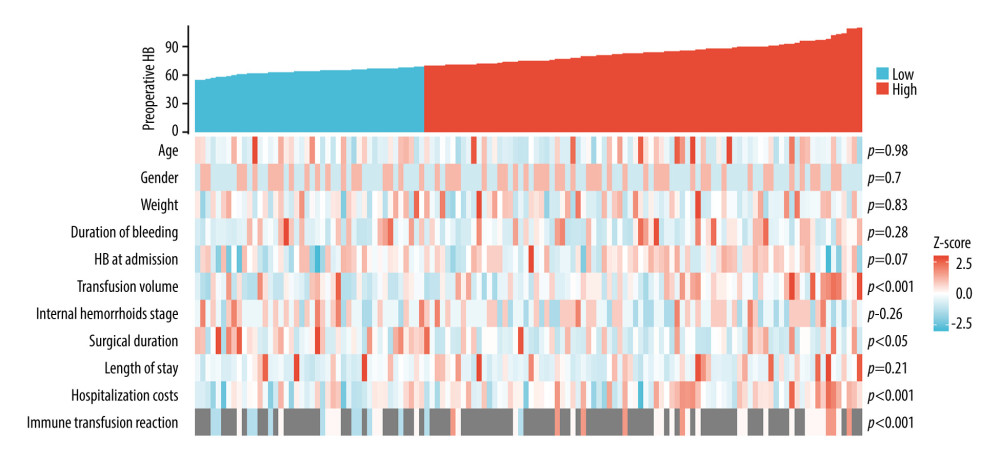 Figure 5. The co-expression heat map. The upper half shows the preoperative hemoglobin levels (PHB) in a column format, with a gradual increase from left to right. Blue indicates the PHB value in the restrictive-threshold group (RG), while red indicates that the PHB value in the liberal-transfusion group (LG). The lower half represents the values of other clinical entries for the same patient that correspond to the PHB of the upper half. In this section, red means high values, blue means low values in the heat map. These values are further divided into LG and RG for comparison, with the corresponding P values displayed on the right side. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 5. The co-expression heat map. The upper half shows the preoperative hemoglobin levels (PHB) in a column format, with a gradual increase from left to right. Blue indicates the PHB value in the restrictive-threshold group (RG), while red indicates that the PHB value in the liberal-transfusion group (LG). The lower half represents the values of other clinical entries for the same patient that correspond to the PHB of the upper half. In this section, red means high values, blue means low values in the heat map. These values are further divided into LG and RG for comparison, with the corresponding P values displayed on the right side. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd. References
1. Lawrence A, McLaren ER, External hemorrhoid. [Updated 2023 Aug 8]: StatPearls [Internet], 2024, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK500009/
2. Fontem RF, Eyvazzadeh D, Internal hemorrhoid. [Updated 2023 Jul 31[: StatPearls [Internet], 2024, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK537182/
3. Krebs ED, Zhang AY, Hassinger TE, Preoperative bleeding requiring transfusion: An under-reported indication for hemorrhoidectomy: Am J Surg, 2020; 220(2); 428-31
4. Davis BR, Lee-Kong SA, Migaly J, The American Society of Colon and rectal surgeons clinical practice guidelines for the management of hemorrhoids: Dis Colon Rectum, 2018; 61(3); 284-92
5. Kate V, Sureshkumar S, Gurushankari B, Kalayarasan R, Acute upper non-variceal and lower gastrointestinal bleeding: J Gastrointest Surg, 2022; 26(4); 932-49
6. Hawks MK, Svarverud JE, Acute lower gastrointestinal bleeding: Evaluation and management: Am Fam Physician, 2020; 101(4); 206-12
7. Nandhra S, Boylan L, Prentis J, Nesbitt CNorthern Vascular Centre, The influence of preoperative anemia on clinical outcomes after infrainguinal bypass surgery: Ann Vasc Surg, 2020; 66; 586-94
8. Kaserer A, Rössler J, Slankamenac K, Impact of allogeneic blood transfusions on clinical outcomes in severely burned patients: Burns, 2020; 46(5); 1083-90
9. Derzon JH, Clarke N, Alford A, Restrictive transfusion strategy and clinical decision support practices for reducing RBC transfusion overuse: Am J Clin Pathol, 2019; 152(5); 544-57
10. Tamini N, Deghi G, Gianotti L, Colon cancer surgery: Does preoperative blood transfusion influence short-term postoperative outcomes?: J Invest Surg, 2021; 34(9); 974-78
11. Güemes-Quinto A, Pichardo-Cruz DA, Luján-Mendoza KI, Jiménez-Bobadilla B, Villanueva-Herrero JA, Emergency surgical treatment for active bleeding and anemia in patients with hemorrhoidal disease: Cir, 2022; 90(S1); 77-83
12. Elimeleh Y, Gralnek IM, Diagnosis and management of acute lower gastrointestinal bleeding: Curr Opin Gastroenterol, 2024; 40(1); 34-42
13. Skrivankova VW, Richmond RC, Woolf BAR, Strengthening the reporting of observational studies in epidemiology using mendelian randomization: The STROBE-MR statement: JAMA, 2021; 326(16); 1614-21
14. van Tol RR, Kleijnen J, Watson AJM, European Society of ColoProctology: Guideline for haemorrhoidal disease: Colorectal Dis, 2020; 22(6); 650-62
15. Herrinton LJ, Liu L, Alexeeff S, Immediate sequential vs. delayed sequential bilateral cataract surgery: Retrospective comparison of postoperative visual outcomes: Ophthalmology, 2017; 124(8); 1126-35
16. Karkouti K, Wijeysundera DN, Beattie WSReducing Bleeding in Cardiac Surgery (RBC) Investigators, Risk associated with preoperative anemia in cardiac surgery: A multicenter cohort study: Circulation, 2008; 117(4); 478-84
17. Xu JY, Tian XD, Yang YM, Preoperative anemia is a predictor of worse postoperative outcomes following open pancreatoduodenectomy: A propensity score-based analysis: Front Med (Lausanne), 2022; 9; 818805
18. Cao G, Yang X, Xu H, Association between preoperative hemoglobin and postoperative moderate and severe anemia among patients undergoing primary total knee arthroplasty: A single-center retrospective study: J Orthop Surg Res, 2021; 16(1); 572
19. Shannon AB, Song Y, Davis Rivera LB, Preoperative transfusion for anemia in patients undergoing abdominal surgery for malignancy: J Gastrointest Surg, 2021; 25(6); 1534-44
20. Mueller MM, Van Remoortel H, Meybohm P, Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference: JAMA, 2019; 321(10); 983-97
21. Estcourt LJ, Kimber C, Trivella M, Preoperative blood transfusions for sickle cell disease: Cochrane Database Syst Rev, 2020; 7(7); CD003149
22. Simon GI, Craswell A, Thom O, Impacts of aging on anemia tolerance, transfusion thresholds, and patient blood management: Transfus Med Rev, 2019; 33(3); 154-61
23. Talaie R, Torkian P, Moghadam AD, Hemorrhoid embolization: A review of current evidences: Diagn Interv Imaging, 2022; 103(1); 3-11
24. Salgueiro P, Rei A, Garrido M, Polidocanol foam sclerotherapy in the treatment of hemorrhoidal disease in patients with bleeding disorders: A multicenter, prospective, cohort study: Tech Coloproctol, 2022; 26(8); 615-25
25. Gallo G, Pietroletti R, Novelli E, A multicentre, open-label, single-arm phase II trial of the efficacy and safety of sclerotherapy using 3% polidocanol foam to treat second-degree haemorrhoids (SCLEROFOAM): Tech Coloproctol, 2022; 26(8); 627-36
26. Kovács E, Palatka K, Németh ASevere anemia caused by haemorrhoids: The casae of a young man with toxic cirrhosis: Orv Hetil, 2013; 154(10); 382-86 [in Hungarian]
27. Wang H, Liang X, Li J, Qian X, Clinicopathological characteristics of a new type of hemorrhoids with anemia: Asian J Surg, 2023; 46(6); 2506-8
28. Gallo G, Martellucci J, Sturiale A, Consensus statement of the Italian society of colorectal surgery (SICCR): Management and treatment of hemorrhoidal disease: Tech Coloproctol, 2020; 24(2); 145-64
29. Song X, Sun W, Bao Y, Outcome of a modified Park’s submucosal hemorrhoidectomy versus Milligan-Morgan for grade III–IV circumferential prolapsed hemorrhoids: Asian J Surg, 2022; 45(11); 2208-13
Figures
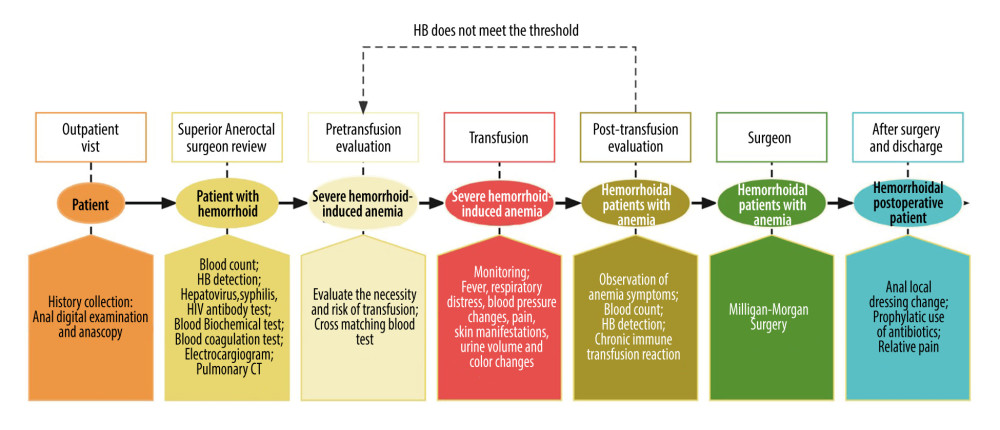 Figure 1. A uniform procedure for the treatment of patients with hemorrhoidal severe anemia. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.
Figure 1. A uniform procedure for the treatment of patients with hemorrhoidal severe anemia. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.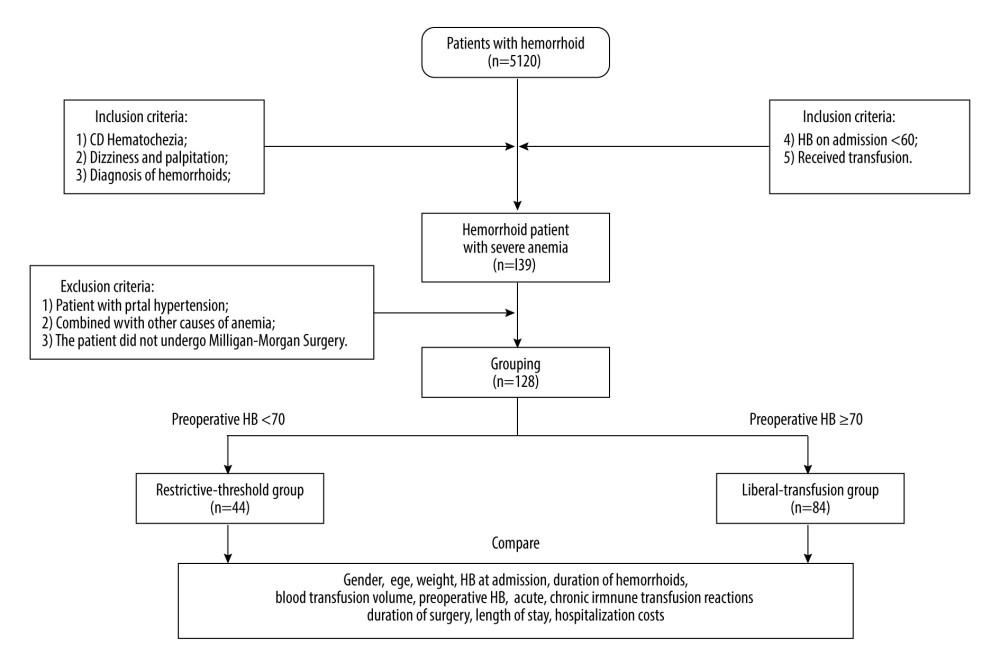 Figure 2. The process of the retrospective cohort study. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.
Figure 2. The process of the retrospective cohort study. Software: Process On online flowchart, 1st version, Beijing Damadi Information Technology Co, Ltd.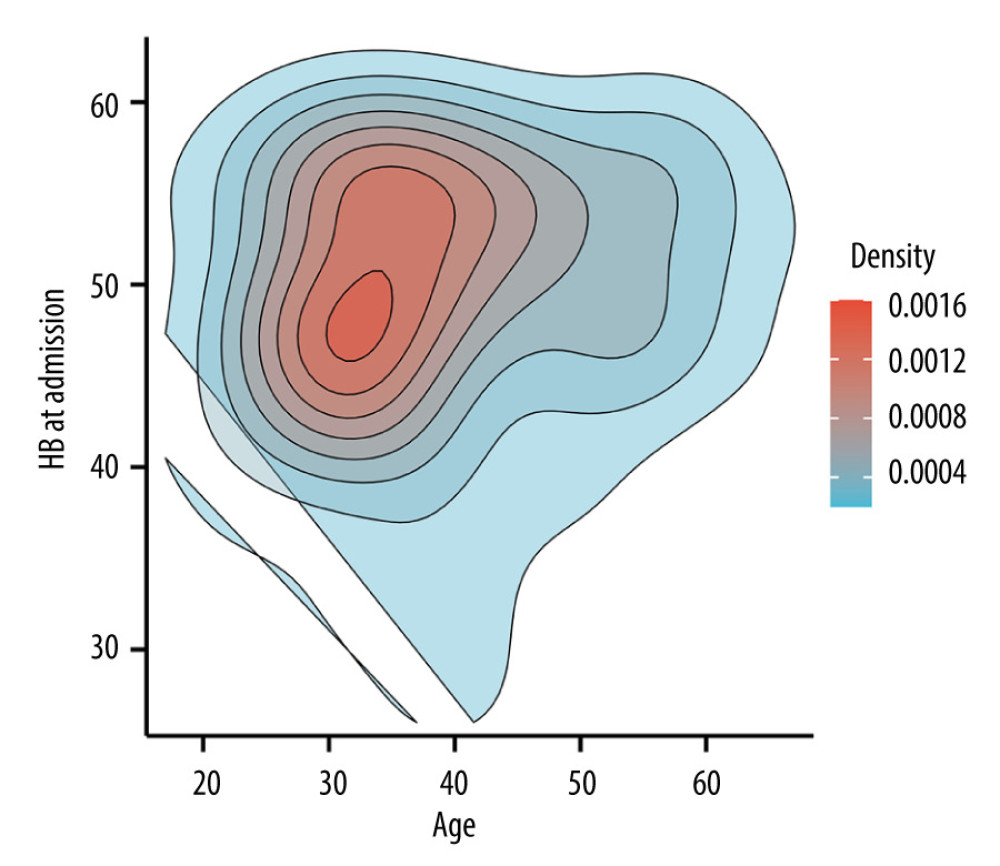 Figure 3. Two-dimensional density profile of patients with hemorrhoidal severe anemia illustrating the distribution of age and hemoglobin levels on admission (AHB). The intensity of the red color indicates the concentration of patients within each category. As shown in the figure, the largest number of patients falls within the age range of 27 to 42 years old, with AHB levels ranging from 43 to 57 g/L. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 3. Two-dimensional density profile of patients with hemorrhoidal severe anemia illustrating the distribution of age and hemoglobin levels on admission (AHB). The intensity of the red color indicates the concentration of patients within each category. As shown in the figure, the largest number of patients falls within the age range of 27 to 42 years old, with AHB levels ranging from 43 to 57 g/L. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.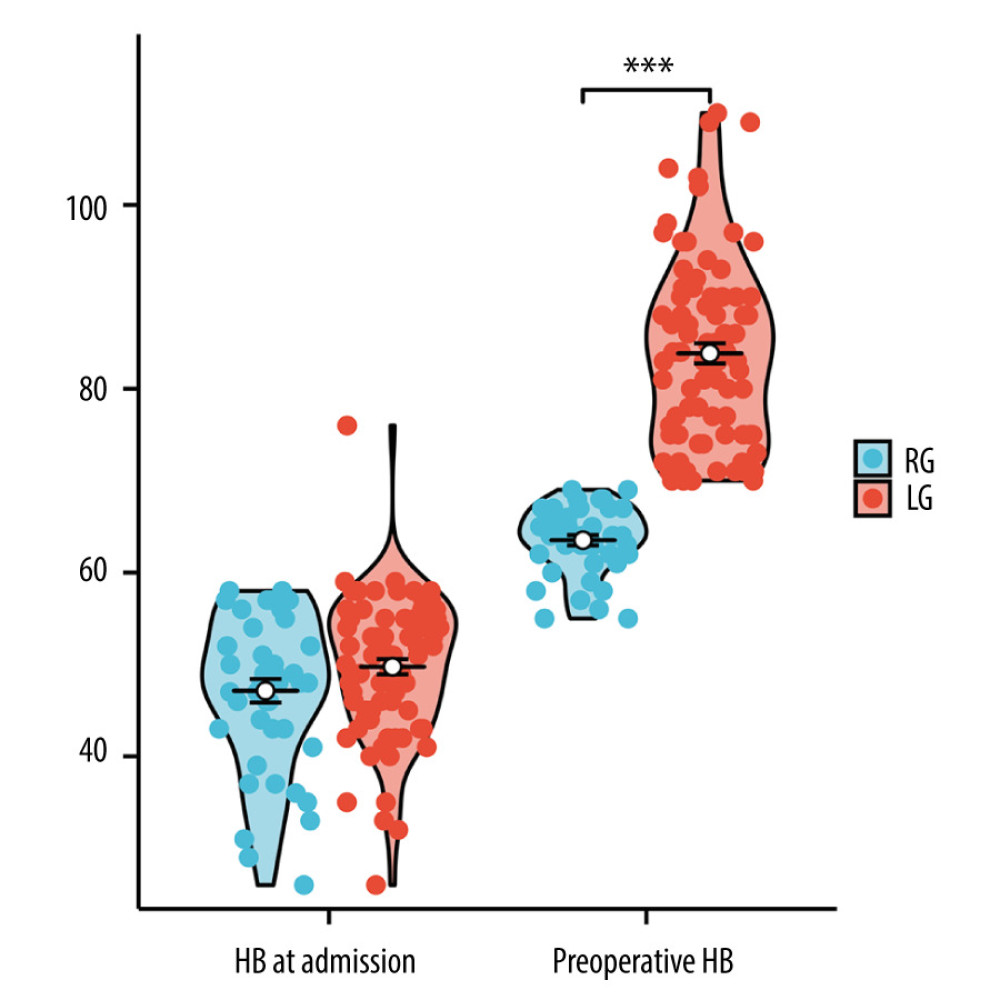 Figure 4. Group comparison chart showing the differences in preoperative hemoglobin levels (PHB) and hemoglobin levels on admission AHB between the 2 groups. *** P<0.001. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 4. Group comparison chart showing the differences in preoperative hemoglobin levels (PHB) and hemoglobin levels on admission AHB between the 2 groups. *** P<0.001. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.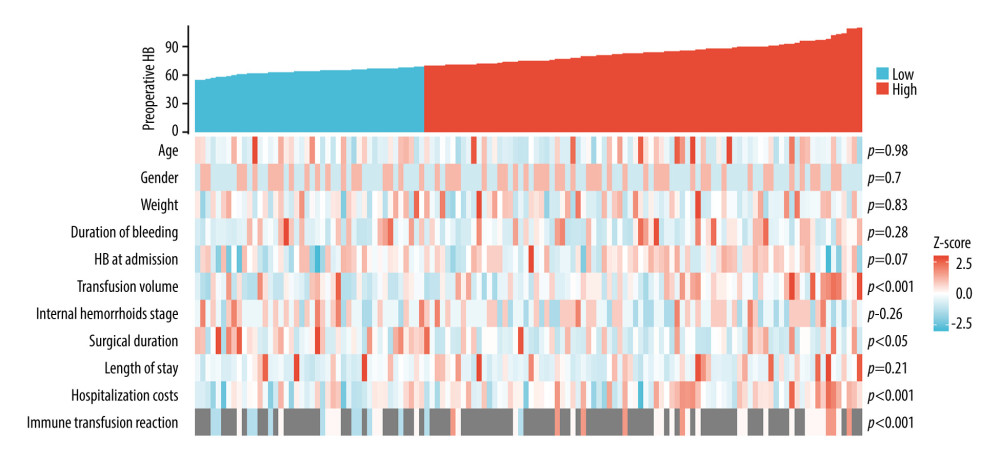 Figure 5. The co-expression heat map. The upper half shows the preoperative hemoglobin levels (PHB) in a column format, with a gradual increase from left to right. Blue indicates the PHB value in the restrictive-threshold group (RG), while red indicates that the PHB value in the liberal-transfusion group (LG). The lower half represents the values of other clinical entries for the same patient that correspond to the PHB of the upper half. In this section, red means high values, blue means low values in the heat map. These values are further divided into LG and RG for comparison, with the corresponding P values displayed on the right side. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd.
Figure 5. The co-expression heat map. The upper half shows the preoperative hemoglobin levels (PHB) in a column format, with a gradual increase from left to right. Blue indicates the PHB value in the restrictive-threshold group (RG), while red indicates that the PHB value in the liberal-transfusion group (LG). The lower half represents the values of other clinical entries for the same patient that correspond to the PHB of the upper half. In this section, red means high values, blue means low values in the heat map. These values are further divided into LG and RG for comparison, with the corresponding P values displayed on the right side. Software: Xiantao Academic, 2nd Edition, Shanghai Xiantao Data Technology Co, Ltd. Tables
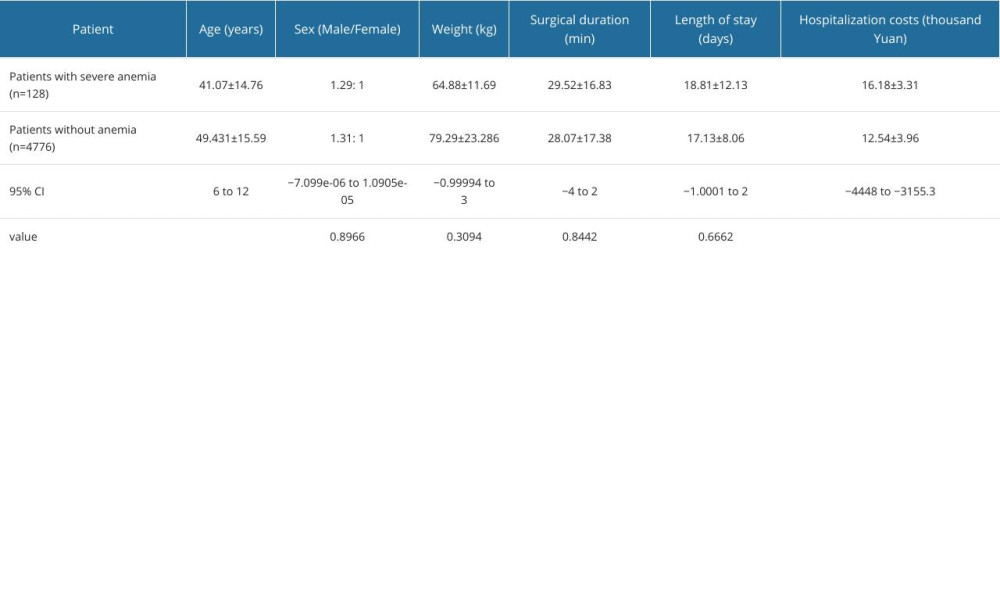 Table 1. Comparison of the general condition (mean±SD) of hemorrhoidal patients with severe anemia and that of hemorrhoidal patients without anemia.
Table 1. Comparison of the general condition (mean±SD) of hemorrhoidal patients with severe anemia and that of hemorrhoidal patients without anemia.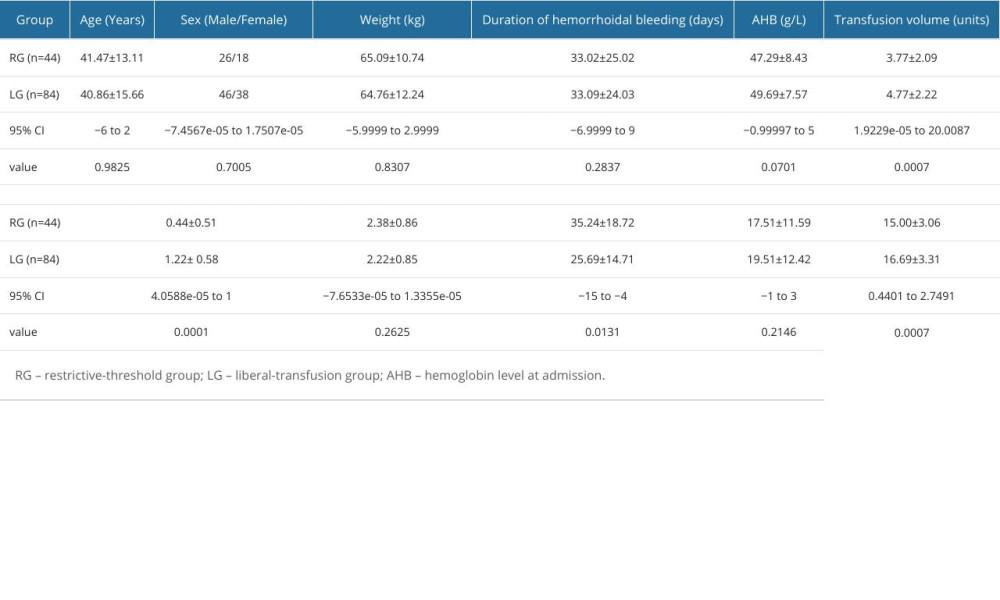 Table 2. Comparison of clinical terms (mean±SD) between the 2 groups.
Table 2. Comparison of clinical terms (mean±SD) between the 2 groups.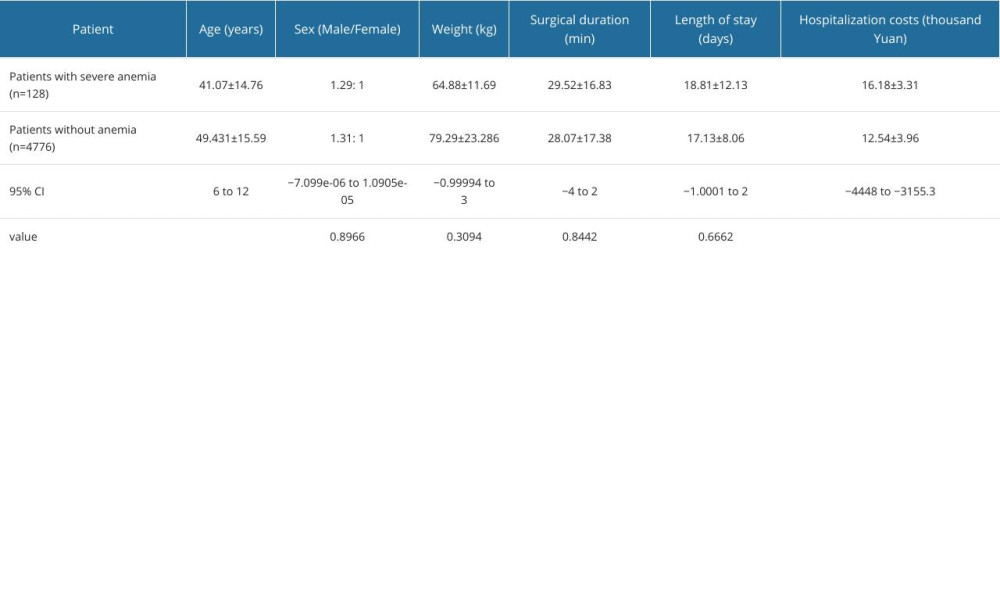 Table 1. Comparison of the general condition (mean±SD) of hemorrhoidal patients with severe anemia and that of hemorrhoidal patients without anemia.
Table 1. Comparison of the general condition (mean±SD) of hemorrhoidal patients with severe anemia and that of hemorrhoidal patients without anemia.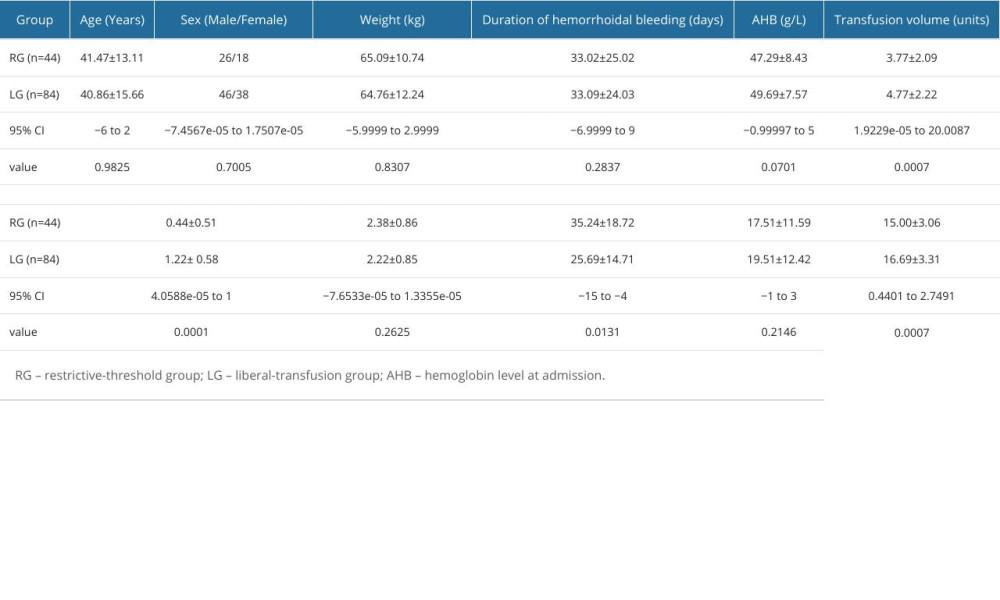 Table 2. Comparison of clinical terms (mean±SD) between the 2 groups.
Table 2. Comparison of clinical terms (mean±SD) between the 2 groups. In Press
08 May 2024 : Clinical Research
Effect of Individualized PEEP Guided by Driving Pressure on Diaphragm Function in Patients Undergoing Lapar...Med Sci Monit In Press; DOI: 10.12659/MSM.944022
21 Mar 2024 : Clinical Research
Impact of Serum Vitamin D, B6, and B12 and Cognitive Functions on Quality of Life in Peri- and Postmenopaus...Med Sci Monit In Press; DOI: 10.12659/MSM.943249
17 Mar 2024 : Clinical Research
Protective Role of TRPC3 Gene Polymorphism (rs10518289) in Obstructive Sleep Apnea Hypopnea Syndrome Among ...Med Sci Monit In Press; DOI: 10.12659/MSM.942667
27 Mar 2024 : Clinical Research
Impact of Patient Education Formats on Treatment Adherence and Denture Hygiene in Edentulous Patients: A Co...Med Sci Monit In Press; DOI: 10.12659/MSM.944175
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








