18 February 2024: Clinical Research
Vertical Relationship Ratio (VRR): A High Reliability and Accuracy Radiographic Measurement for Basilar Invagination in Rheumatoid Arthritis
Monchai Ruangchainikom1ABDEF, Ekkapoj Korwutthikulrangsri1E, Apisit Rattanatanasarn1C, Ishthayapong Kanjanakeereewong1C, Win Boonsirikamchai2C, Panlop Tirawanish3C, Surin Thanapipatsiri1A, Werasak SutipornpalangkulDOI: 10.12659/MSM.943329
Med Sci Monit 2024; 30:e943329
Abstract
BACKGROUND: Previous radiographic measurements for diagnosis of a basilar invagination or impression (BI) in rheumatoid arthritis (RA) were used as reference values based on anatomical reference distances. Due to the obscured anatomical landmarks, our group proposed a new radiographic measurement based on anatomic ratios to identify BI.
MATERIAL AND METHODS: The vertical relationship ratio (VRR) was developed and evaluated. The VRR is the relationship between the distance obtained with the modified Ranawat method and the C3 vertebral body height. VRR was used to assess its ability to distinguish BI in 3 patient groups (28 RA with BI, 37 RA without BI, and 56 non-RA patients). The intra- and inter-observer reliability, the sensitivities, and specificities of all measurements were analyzed. The cutoff value of VRR measurement was calculated by using the receiver operating characteristic (ROC) curve.
RESULTS: The VRR measurement showed excellent intra- and inter-observer reliabilities. The VRR could significantly distinguish RA patients with BI from RA patients without BI. The mean VRR of RA patients with BI (1.82±0.20) was less than for the non-RA patients (2.26±0.19) and the RA patients without BI (2.24±0.19). The cutoff value of VRR from the ROC curve was below 2.025. Its sensitivity was 92.85%, specificity was 97.85%, positive predictive value was 92.86%, and negative predictive value was 97.84%.
CONCLUSIONS: VRR has excellent intra-/inter-observer reliability and can distinguished BI in RA patients. We recommend using VRR in preference to the other available methods for assessment and screening BI in rheumatoid arthritis.
Keywords: Arthritis, Rheumatoid, Basilar Impression, Primary, Radiographic Magnification
Background
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disease. It primarily affects the lining of the synovial joints and can cause progressive disability [1]. Although the joint involvement is mainly in the hands, wrists, elbows, shoulders, and knees, cervical spinal joints can also be affected. Erosive pannus formations at the atlantooccipital and atlantoaxial joints cause bony destruction and ligamentous laxity, thereby weakening and collapsing lateral masses. After these devastating consequences, basilar invagination or impression (BI) occurs [2]. The BI in RA patients has been referred to using several terms: cranial settling, atlantoaxial impaction, vertical settling, or superior migration of the odontoid process. Although these terms are defined slightly differently, BI is primarily considered to be projection of the tip of the odontoid process into the already limited space of the foramen magnum [3]. This BI affects brain stem function, leading to compromise of the autonomic center and increased morbidity [4,5]. Therefore, surgical intervention has been recommended to prevent these poor outcomes [3,6–8].
Normally, the diagnosis of BI is based on advanced imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI). However, the diagnosis of BI by using plain cervical spine radiographs remains valuable because of its cost-effectiveness and greater accessibility [9]. There are several available measurement methods based on plain radiographs of cervical spine to diagnose BI in RA patients. These measurements include the McRae line [10], McGregor line [11], Chamberlain line [12], Ranawat method [8], Redlund-Johnell method [13], and Clark station method [7]. However, most of these plain radiographic measurements for BI have common problems caused by the obscured anatomical landmarks and magnification [14,15], and lower sensitivity to detect the BI in each previous radiographic measurement techniques (61% in Redlund-Johnell, 71% in the Ranawat, and 83% in the Clark station criteria). In addition, Riew et al reported that the intraclass correlation coefficient scores (ICCS) with inter-observer and intra-observer of McRae line, Ranawat methods, and McGregor line had poor correlations. They suggested combining 3 radiographic measurement methods (Ranawat, Redlund-Johnell, and Clark station) to increase sensitivity and negative predictive values [15]. To the best of our knowledge, now there is no single method that is highly reliable and accurate in diagnosis of BI in RA patients. Therefore, the aim of this study was to develop a new radiographic measurement method and evaluate its reliability and accuracy in diagnosis of BI in RA patients. We also compared our new measurement methods with previously available measurement methods in terms of sensitivity, specificity, and cutoff value in diagnosis of BI.
Material and Methods
ETHICS APPROVAL:
The Ethics Committee of the Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand approved this study (COA no. Si 596/2018), and the guidelines and regulations of the Ethics Review Board were followed for all material and methods. Because this study was retrospective, the requirement for informed consent of each patient was waived.
PARTICIPANTS:
This study retrospectively enrolled 28 patients diagnosed with RA and BI between 2005 and 2020 (the “RA with BI” group). All had been diagnosed with RA by rheumatologists at the Faculty of Medicine Siriraj Hospital using the American College of Rheumatology criteria. BI was diagnosed if sagittal CT or MRI images showed the following: 1)The odontoid process tip passing through the foramen magnum, 2) The lack of ventral subarachnoid space, 3) The odontoid process indenting the medulla at the level of the foramen magnum [16]. Another 2 groups were recruited: “RA without BI” and “non-RA.” All patients had lateral cervical spine scans obtained through MRI or CT imaging. Individuals were excluded from the RA without BI and non-RA groups if they had: (1) congenital bony abnormalities of the craniovertebral junction; (2) fractures, tumors, or infections of the craniovertebral junction; or (3) prior craniovertebral junction surgery.
RADIOGRAPHIC MEASUREMENT AND DATA COLLECTION:
Two independent orthopedic surgeons were involved in evaluating plain lateral radiographs of the cervical spine. The observers independently measured and analyzed the radiographs without knowing the related diagnoses. Measurements were made with electronic calipers in the hospital’s picture archiving and communication system. Each radiograph was assessed twice by each surgeon, with at least a 1-month interval between the 2 measurements. To prevent recall bias, the order of the radiographs was randomly changed for the second set of measurements, with the 2 observers were blinded to the new sequence. Each surgeon used the following 5 methods to determine the presence of BI on the plain radiographs:
REDLUND-JOHNELL METHOD: The observer marked the midpoint of the base of C2 and then measured the minimum distance between that point and a line drawn from the posterior hard palate to the lowest point on the midline occipital curve. BI was indicated when the distance was less than 34 mm in males and 29 in females [13].
RANAWAT METHOD: The observer measured the perpendicular distance from the center of the pedicle of C2 to a line which crosses along to the transverse axis of C1. BI was indicated when the distance was less than 15 mm in males and 13 mm in females [8].
MODIFIED RANAWAT METHOD: The observer marked the midpoint of the base of C2 and drew a line from the center of the anterior arch of C1 to the center of the posterior arch. The distance between the 2 lines along the long axis of C2 was measured [17].
CLARK STATION METHOD: The observer identified the station of C1, determined by the level of the anterior ring of the atlas on the 3 parts of the odontoid process. BI was diagnosed if the anterior ring of the atlas was level at the middle third (station II) or caudal third (station III) of the odontoid process [7].
VRR METHOD: The ratio was calculated by dividing the distance obtained with the modified Ranawat method by the mean of the vertebral body height of C3 (Figure 1). The mean of the vertebral body height of C3 was derived by the formula (anterior vertebral height+posterior vertebral height)/2.
We compared the VRR with other present measuring methods by using the radiographic parameters in sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). In addition, we analyzed the ROC curve of the VRR to establish the cut off for the RA with BI group. The true positive (sensitivity) rate was plotted as a function of the false-positive (100-specificity) rate to obtain an optimal possible cut off value. The area under the ROC curve was used to identify the optimal cutoff for distinguishing cases of RA with BI from cases that did not have BI (the RA without BI and the non-RA groups).
STATISTICAL ANALYSIS:
The demographic data and radiographic measurements were analyzed and reported. Categorical data were compared using the chi-squared test. Continuous data were checked for normal distribution by using the Shapiro-wilk test. Normally distributed continuous data were compared using an independent
For the Clark station measurement method, there was calculated agreement with the Kappa value because of ordinal scale data. Moderate agreement was 0.41–0.60, substantial agreement was 0.61–0.80, and perfect agreement was 0.81–1.0. The sensitivity, specificity, PPV, and NPV of each radiographic parameter were calculated. ROC analysis was also used to determine the cutoff of the VRR. All these analyses were conducted using SPSS Statistics for Windows, version 18.0 (SPSS Inc, Chicago, IL, USA) and MedCalc, version 17.6 (MedCalc Statistical Software, Ostend, Belgium).
Results
CLINICAL, INTER-OBSERVER, INTRA-OBSERVER RESULTS:
This study enrolled 121 patients (28 in the RA with BI group, 37 in the RA without BI group, and 56 in the non-RA group). Most patients in the RA group with BI and without BI were female and older than non-RA patients (Table 1). The intra-observer reliabilities of the VRR, Redlund-Johnell, and modified Ranawat methods were excellent, with ICC values of more than 0.9. The Ranawat method had the lowest intra-observer reliability (ICC values of 0.880 and 0.894 for the 2 raters). The inter-observer reliabilities of all radiographic parameters were also excellent (ICC values, 0.919–0.962; Table 2). The Clark station method showed moderate to perfect agreement for intra-observer reliability (kappa, 0.695 and 0.915; P<0.001) and moderate to substantial agreement for inter-observer reliability (kappa, 0.590 and 0.739; P<0.001)
All parameter measurements for the Redlund-Johnell, Ranawat, modified Ranawat, Clark station, and VRR methods demonstrated statistically significant differences in distinguishing RA patients with BI from those patients in other groups. The mean VRR for the RA with BI group was 1.82±0.20, which was lower than the means of the other groups (2.24±0.19 in RA without BI, and 2.26±0.19 in non-RA). The other parameters (Redlund-Johnell, Ranawat, and modified Ranawat methods) were also lower for the patients in the RA with BI group than those patients without BI. In addition, there was a higher degree of Clark station in the RA with BI group than in the 2 other groups (Table 1).
ROC CURVE RESULTS:
The ROC curve of the VRR was analyzed. The optimal cutoff for the VRR was below 2.025 and the area under the ROC curve was 0.987 (P<0.001; Figure 2). The true-positive rate (sensitivity) was 96.43%, and the specificity was 97.85%. Moreover, the NPV for this cutoff in this population was 97.85%; this was excellent for interpreting a subject with a negative finding who does not have BI. The PPV that indicated the likelihood that a subject with a positive finding had BI was also excellent, at 92.85%. The sensitivity and NPV values of the VRR were greater than those for the other tests, even when the Redlund-Johnell, Ranawat, and Clark station methods were combined. Additionally, the VRR’s optimal cut off provided high sensitivity, specificity, PPV, and NPV for both sexes (88.89%, 100%, 100%, and 95.83% in males, 94.74%, 97.14%, 90.00%, and 98.56% in females, as shown in Table 3)
Discussion
STRENGTHS AND LIMITATIONS:
There are several strengths in our study. First, our study included all available measurement methods and demonstrated the effectiveness of each measurement method in diagnosis of BI. Second, we used 2 independent evaluators blinded in evaluation to prevent biased measurement of radiographic data.
Nevertheless, our study still has some limitations. First, it was a retrospective, case-control study that might have had a selection bias. Second, the BI in this study focused on RA, but other causes of BI were not included. Third, the study’s participants were mainly females, who are naturally predominant in the RA population. Moreover, the small population in this study was drawn from patients with BI, which is a rare disease.
Conclusions
VRR has the excellent intra-/inter-observer reliabilities and could distinguished BI in RA patient. We recommend using the VRR in preference to the other available methods for assessment and screening BI. In addition, the VRR cutoff value less than 2.025 in plain radiographs of the lateral cervical spine indicates the presence of BI with high sensitivity and specificity.
Figures
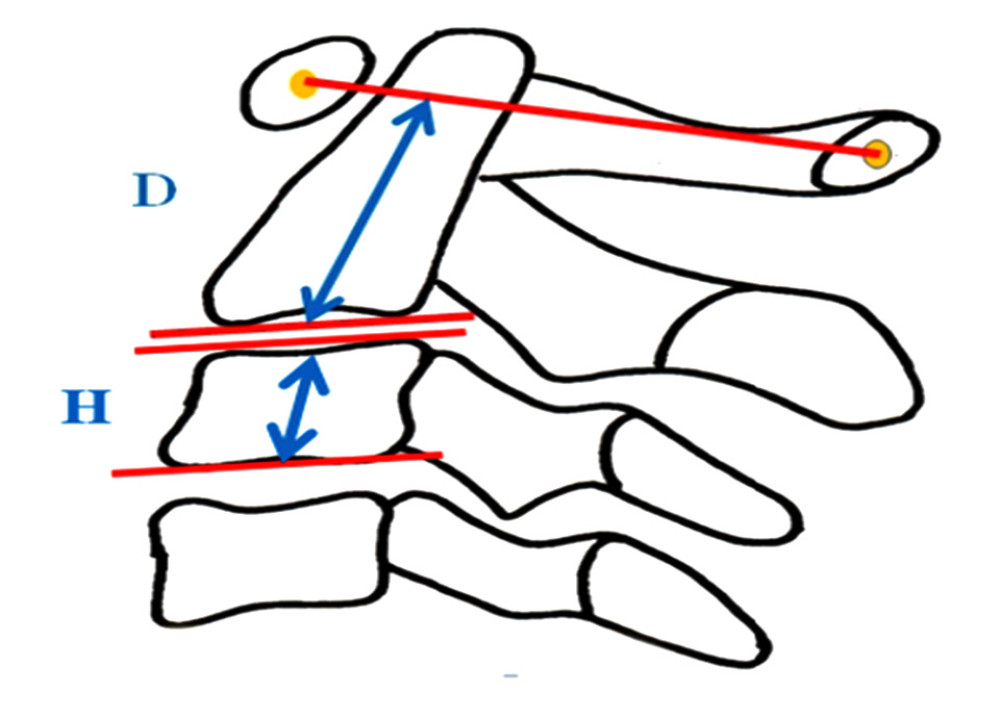 Figure 1. The measurement method of the Vertical Relationship Ratio (VRR): D/H, D: The distance between the midpoint of the base of C2 and a line from the center of the anterior and posterior arch of C1, H: mean of vertebral body height of C3 ((Anterior vertebral height+posterior vertebral height)/2). The figure was created using PowerPoint for Windows version 2311, Microsoft Corporation (Redmond, WA, USA).
Figure 1. The measurement method of the Vertical Relationship Ratio (VRR): D/H, D: The distance between the midpoint of the base of C2 and a line from the center of the anterior and posterior arch of C1, H: mean of vertebral body height of C3 ((Anterior vertebral height+posterior vertebral height)/2). The figure was created using PowerPoint for Windows version 2311, Microsoft Corporation (Redmond, WA, USA). 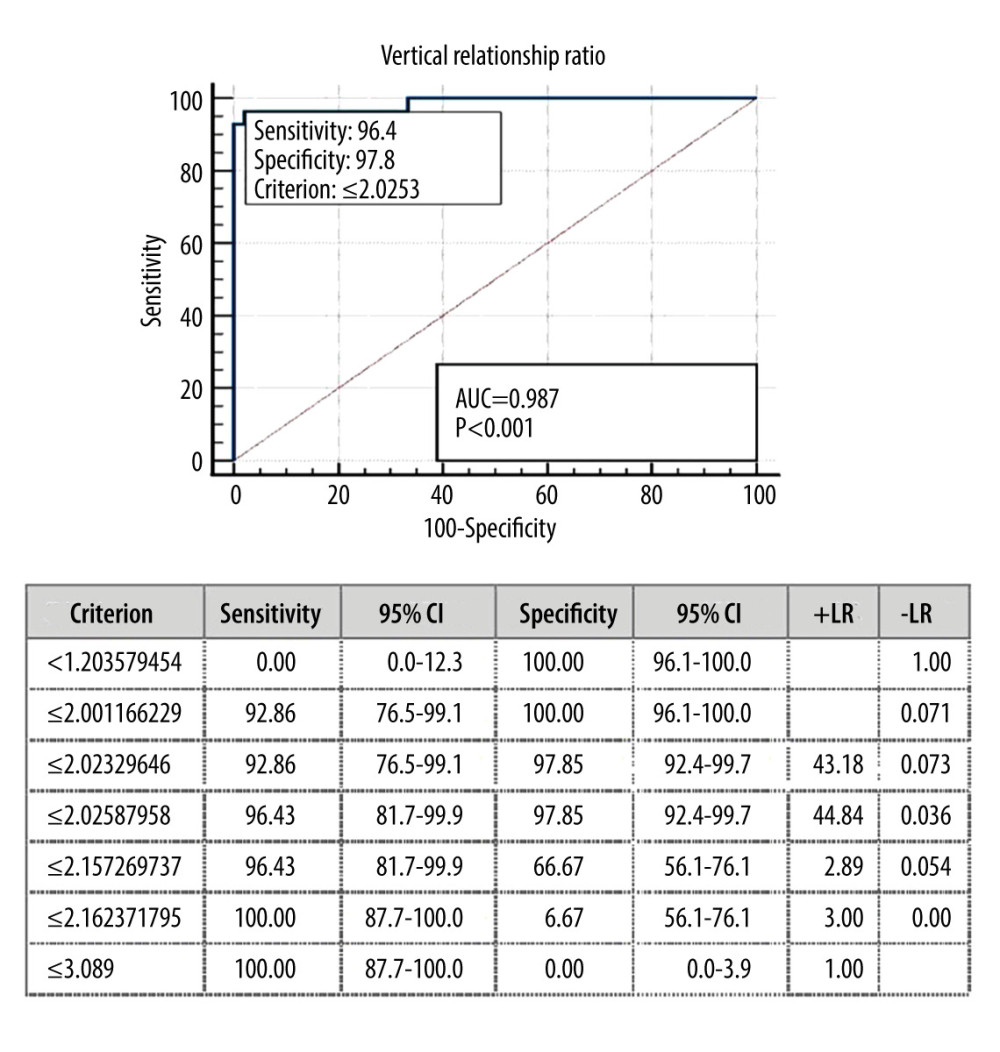 Figure 2. ROC curve, sensitivity, and specificity of the Vertical Relationship Ratio (VRR). The figure was created using MedCalc, version 17.6, MedCalc Statistical Software (Ostend, Belgium).
Figure 2. ROC curve, sensitivity, and specificity of the Vertical Relationship Ratio (VRR). The figure was created using MedCalc, version 17.6, MedCalc Statistical Software (Ostend, Belgium). References
1. Guo Q, Wang Y, Xu D, Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies: Bone Res, 2018; 6; 15
2. Kim DH, Hilibrand AS, Rheumatoid arthritis in the cervical spine: J Am Acad Orthop Surg, 2005; 13(7); 463-74
3. Donnally IC, Munakomi S, Varacallo M, Basilar invagination: StatPearls, 2023, Treasure Island (FL)
4. Mayer JW, Messner RP, Kaplan RJ, Brain stem compression in rheumatoid arthritis: JAMA, 1976; 236(18); 2094-95
5. Parish DC, Clark JA, Liebowitz SM, Hicks WC, Sudden death in rheumatoid arthritis from vertical subluxation of the odontoid process: J Natl Med Assoc, 1990; 82(4); 297-99
6. Conaty JP, Mongan ES, Cervical fusion in rheumatoid arthritis: J Bone Joint Surg Am, 1981; 63(8); 1218-27
7. Clark CR, Goetz DD, Menezes AH, Arthrodesis of the cervical spine in rheumatoid arthritis: J Bone Joint Surg Am, 1989; 71(3); 381-92
8. Ranawat CS, O’Leary P, Pellicci P, Cervical spine fusion in rheumatoid arthritis: J Bone Joint Surg Am, 1979; 61(7); 1003-10
9. Park JH, Kim JT, Kim IS, Hong JT, Are plain radiographic measurements still consistent with a diagnosis of basilar invagination in the era of cross-sectional images?: Medicine (Baltimore), 2022; 101(38); e30552
10. McRae DL, Barnum AS, Occipitalization of the atlas: Am J Roentgenol Radium Ther Nucl Med, 1953; 70(1); 23-46
11. McGreger M, The significance of certain measurements of the skull in the diagnosis of basilar impression: Br J Radiol, 1948; 21(244); 171-81
12. Chamberlain WE, Basilar impression (Platybasia): A bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations: Yale J Biol Med, 1939; 11(5); 487-96
13. Redlund-Johnell I, Pettersson H, Radiographic measurements of the cranio-vertebral region. Designed for evaluation of abnormalities in rheumatoid arthritis: Acta Radiol Diagn (Stockh), 1984; 25(1); 23-28
14. Lee HJ, Hong JT, Kim IS, Analysis of measurement accuracy for craniovertebral junction pathology: Most reliable method for cephalometric analysis: J Korean Neurosurg Soc, 2013; 54(4); 275-79
15. Riew KD, Hilibrand AS, Palumbo MA, Diagnosing basilar invagination in the rheumatoid patient. The reliability of radiographic criteria: J Bone Joint Surg Am, 2001; 83(2); 194-200
16. Kawaida H, Sakou T, Morizono Y, Vertical settling in rheumatoid arthritis. Diagnostic value of the Ranawat and Redlund-Johnell methods: Clin Orthop Relat Res, 1989(239); 128-35
17. Kwong Y, Rao N, Latief K, Craniometric measurements in the assessment of craniovertebral settling: Are they still relevant in the age of cross-sectional imaging?: Am J Roentgenol, 2011; 196(4); W421-25
18. Kauppi M, Sakaguchi M, Konttinen YT, Hamalainen M, A new method of screening for vertical atlantoaxial dislocation: J Rheumatol, 1990; 17(2); 167-72
19. Kulkarni AG, Goel AH, Vertical atlantoaxial index: A new craniovertebral radiographic index: J Spinal Disord Tech, 2008; 21(1); 4-10
20. Park JH, Hong JT, Lee JB, Kim IS, Clinical analysis of radiologic measurements in patients with basilar invagination: World Neurosurg, 2019; 131; e108-e15
Figures
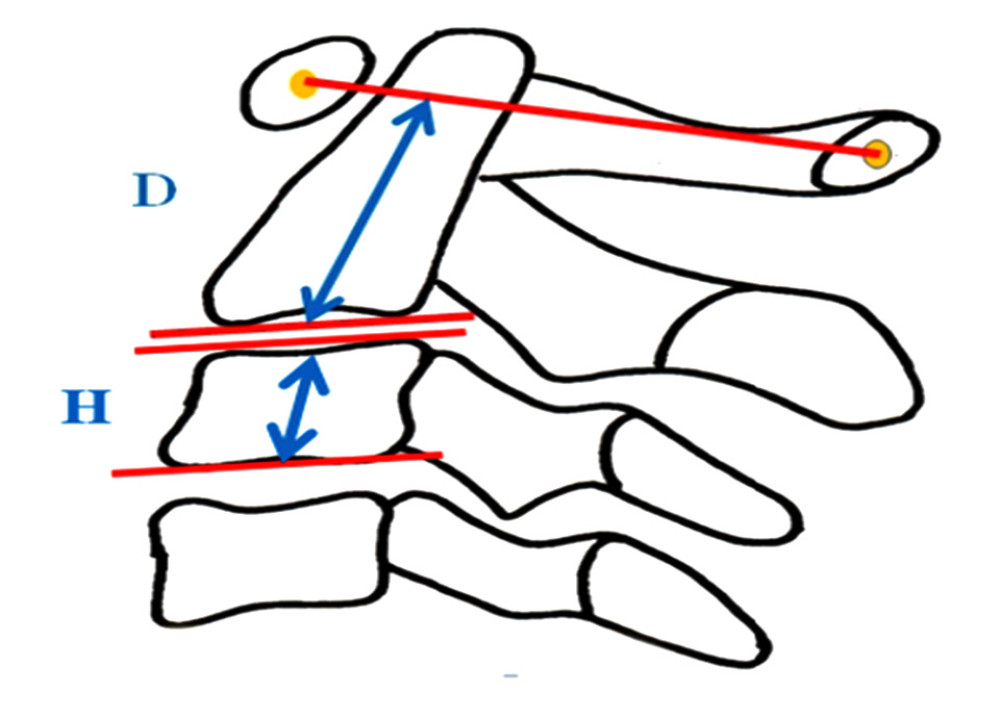 Figure 1. The measurement method of the Vertical Relationship Ratio (VRR): D/H, D: The distance between the midpoint of the base of C2 and a line from the center of the anterior and posterior arch of C1, H: mean of vertebral body height of C3 ((Anterior vertebral height+posterior vertebral height)/2). The figure was created using PowerPoint for Windows version 2311, Microsoft Corporation (Redmond, WA, USA).
Figure 1. The measurement method of the Vertical Relationship Ratio (VRR): D/H, D: The distance between the midpoint of the base of C2 and a line from the center of the anterior and posterior arch of C1, H: mean of vertebral body height of C3 ((Anterior vertebral height+posterior vertebral height)/2). The figure was created using PowerPoint for Windows version 2311, Microsoft Corporation (Redmond, WA, USA).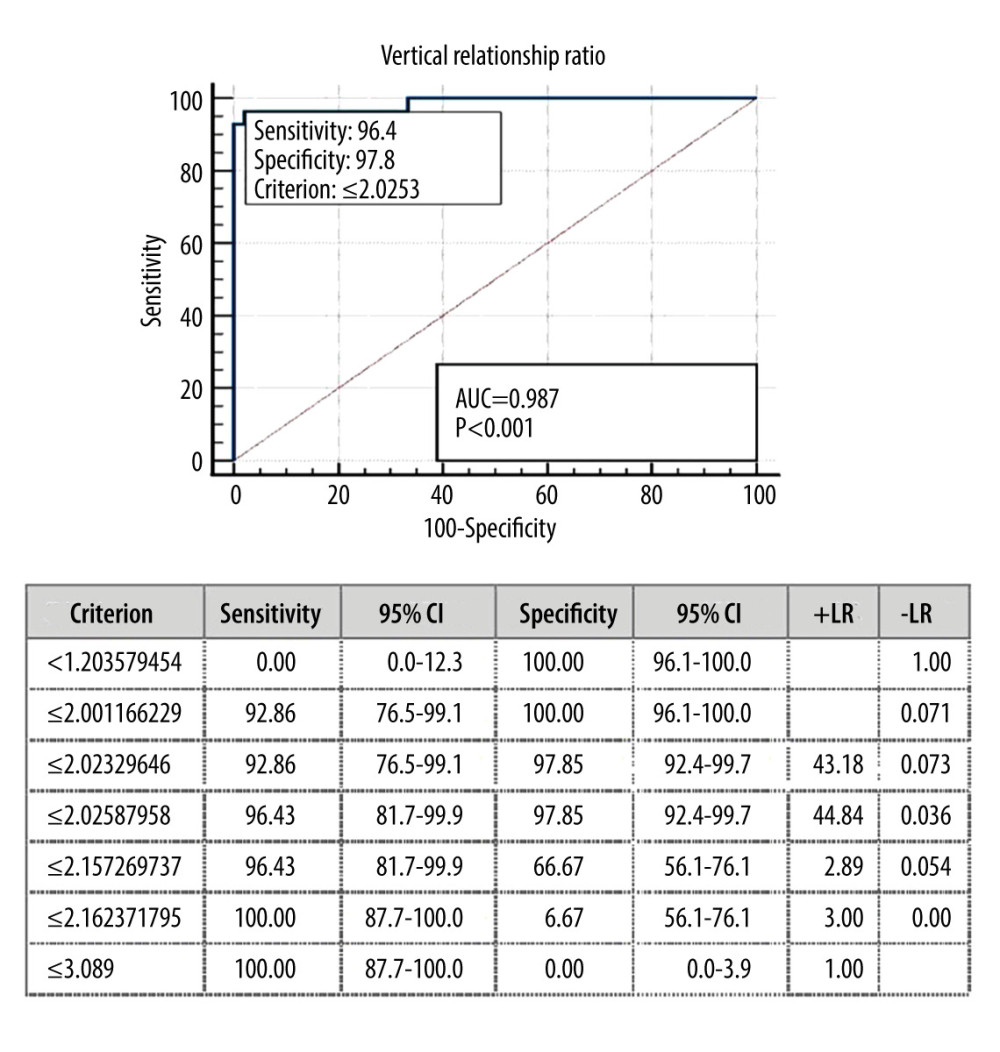 Figure 2. ROC curve, sensitivity, and specificity of the Vertical Relationship Ratio (VRR). The figure was created using MedCalc, version 17.6, MedCalc Statistical Software (Ostend, Belgium).
Figure 2. ROC curve, sensitivity, and specificity of the Vertical Relationship Ratio (VRR). The figure was created using MedCalc, version 17.6, MedCalc Statistical Software (Ostend, Belgium). Tables
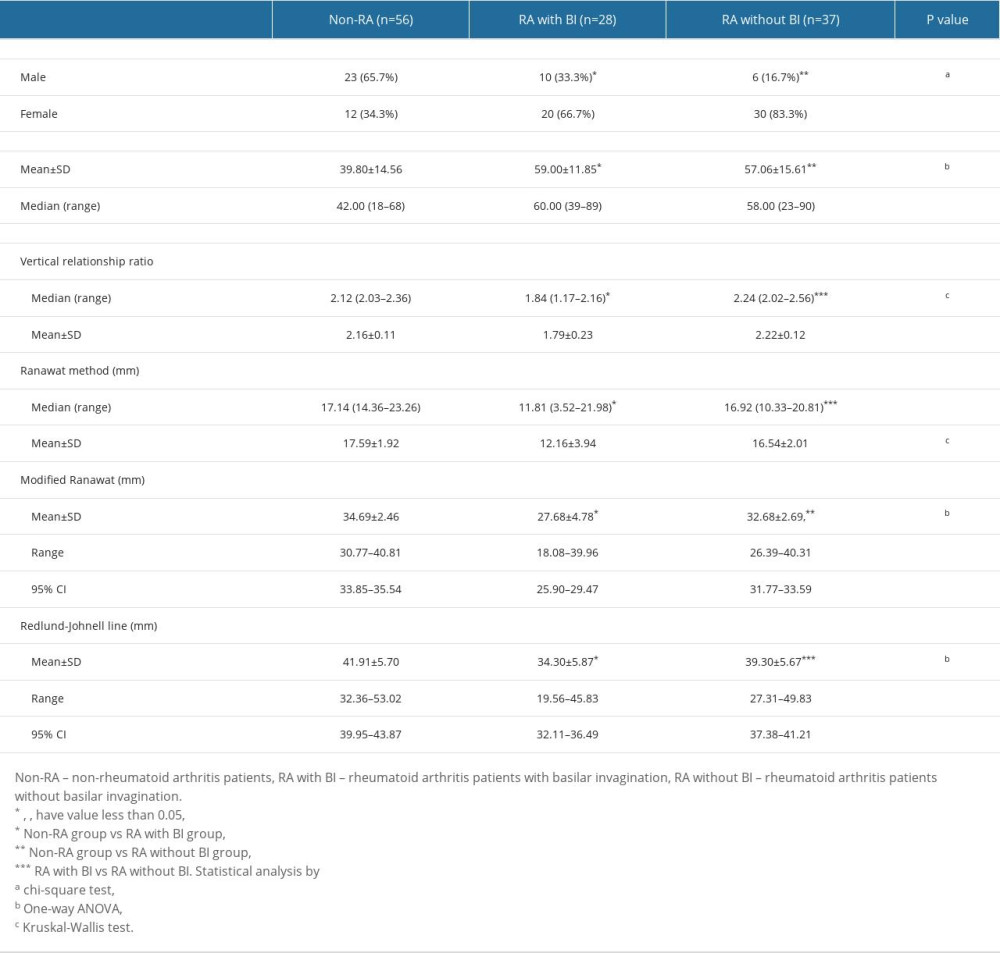 Table 1. Demographic data and different measurement parameters in each group of patients.
Table 1. Demographic data and different measurement parameters in each group of patients.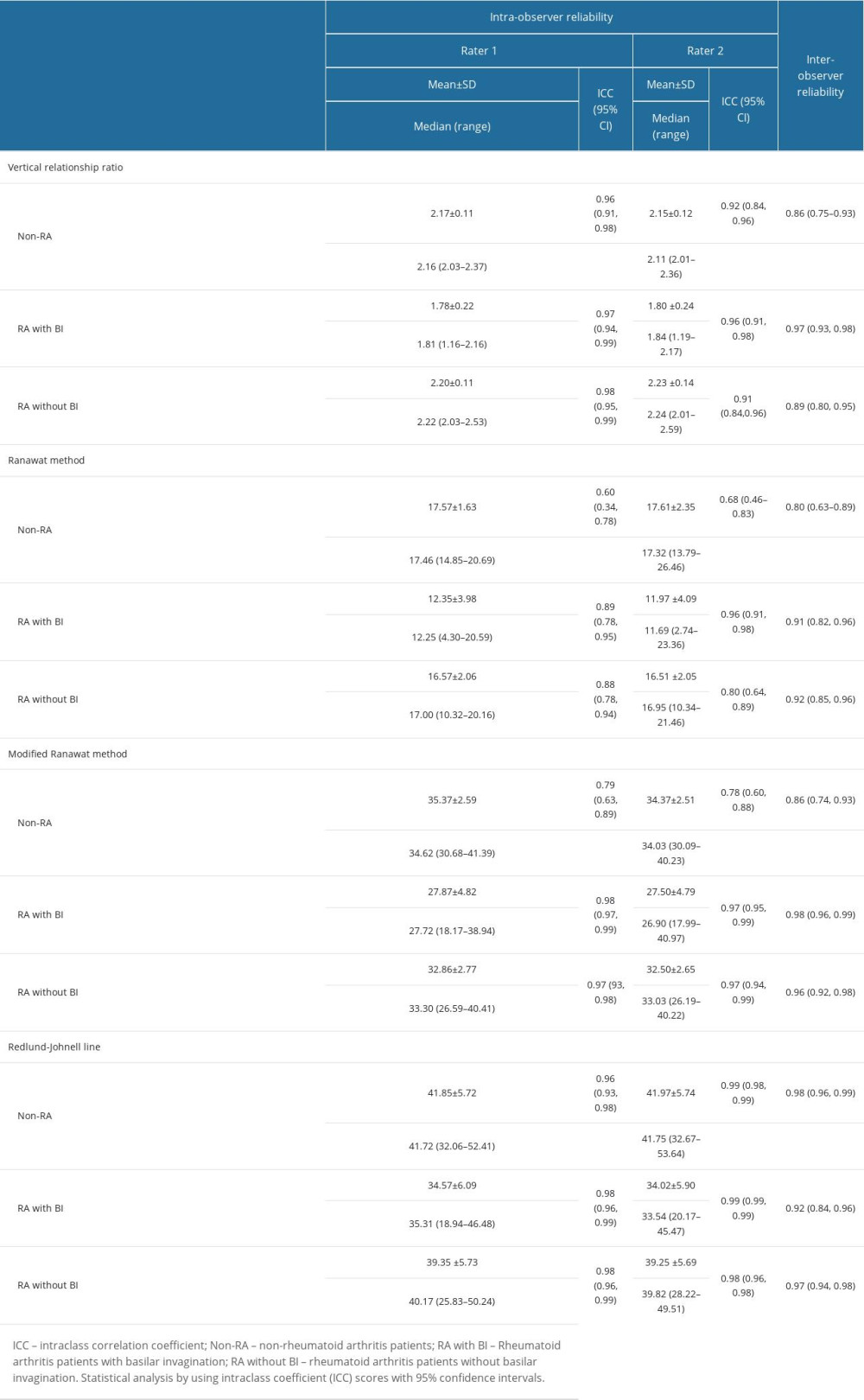 Table 2. Intra- and inter-observer reliability of different measurements in each group of patients.
Table 2. Intra- and inter-observer reliability of different measurements in each group of patients.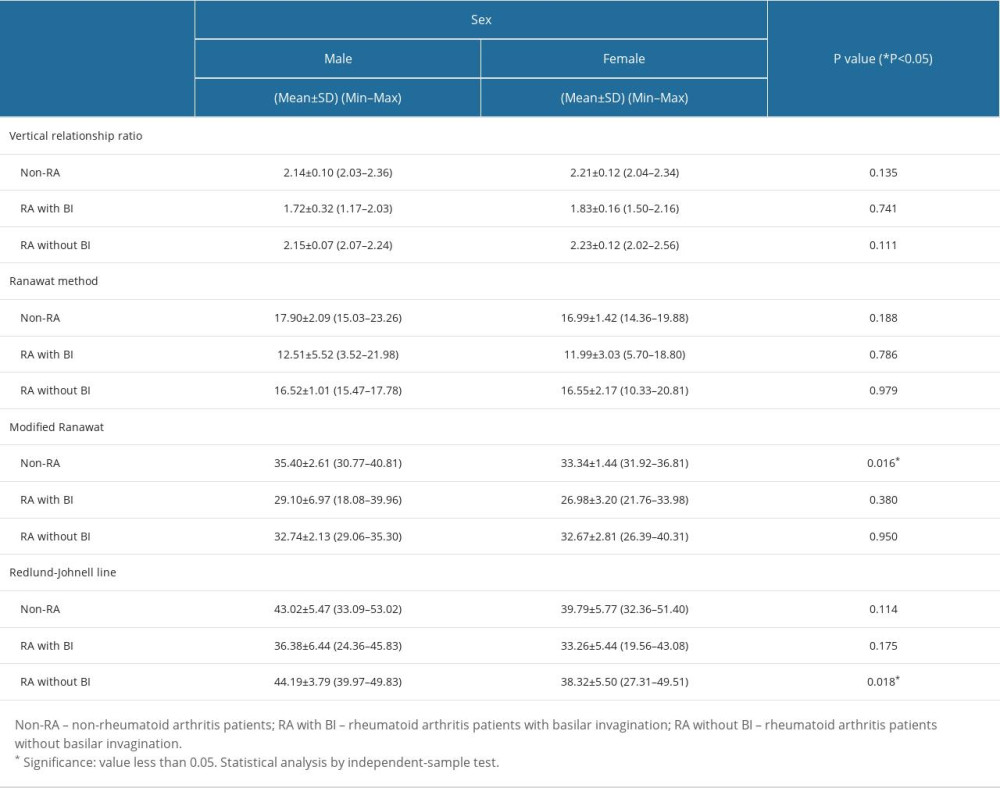 Table 3. Effect of sex on all different measurements in each group of patients.
Table 3. Effect of sex on all different measurements in each group of patients.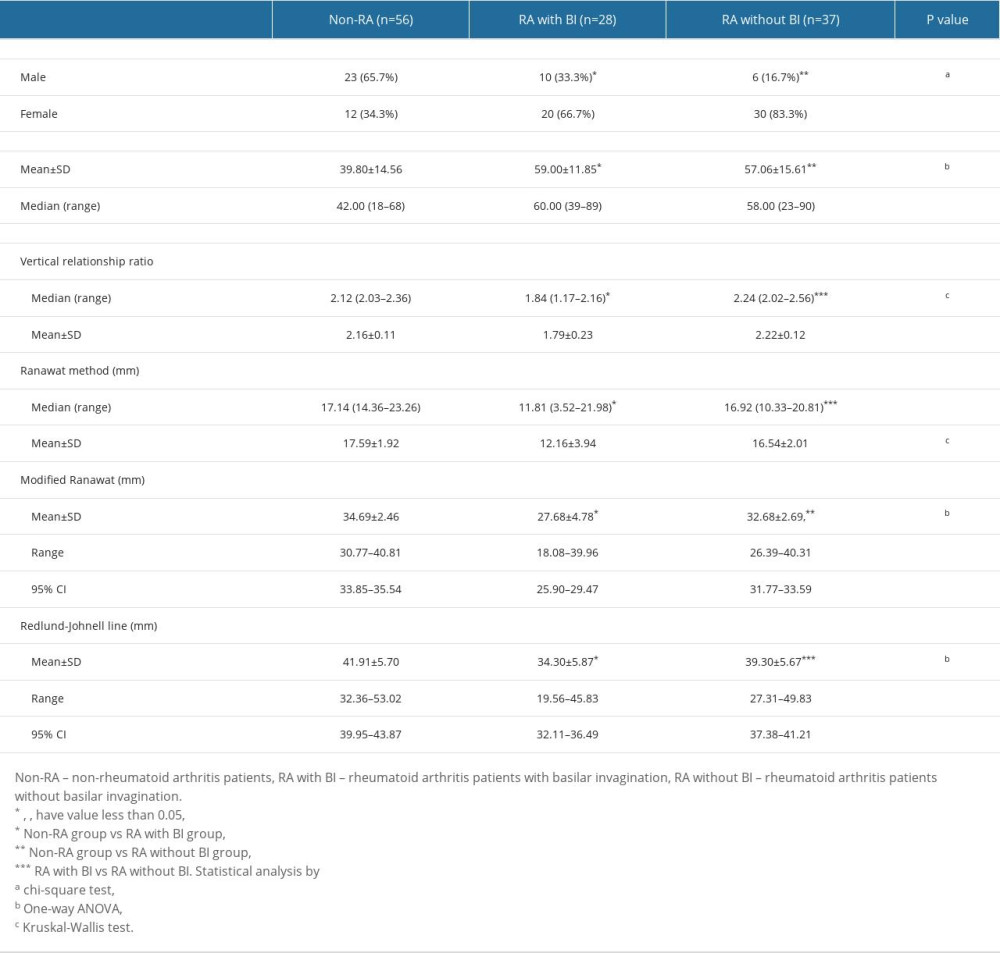 Table 1. Demographic data and different measurement parameters in each group of patients.
Table 1. Demographic data and different measurement parameters in each group of patients.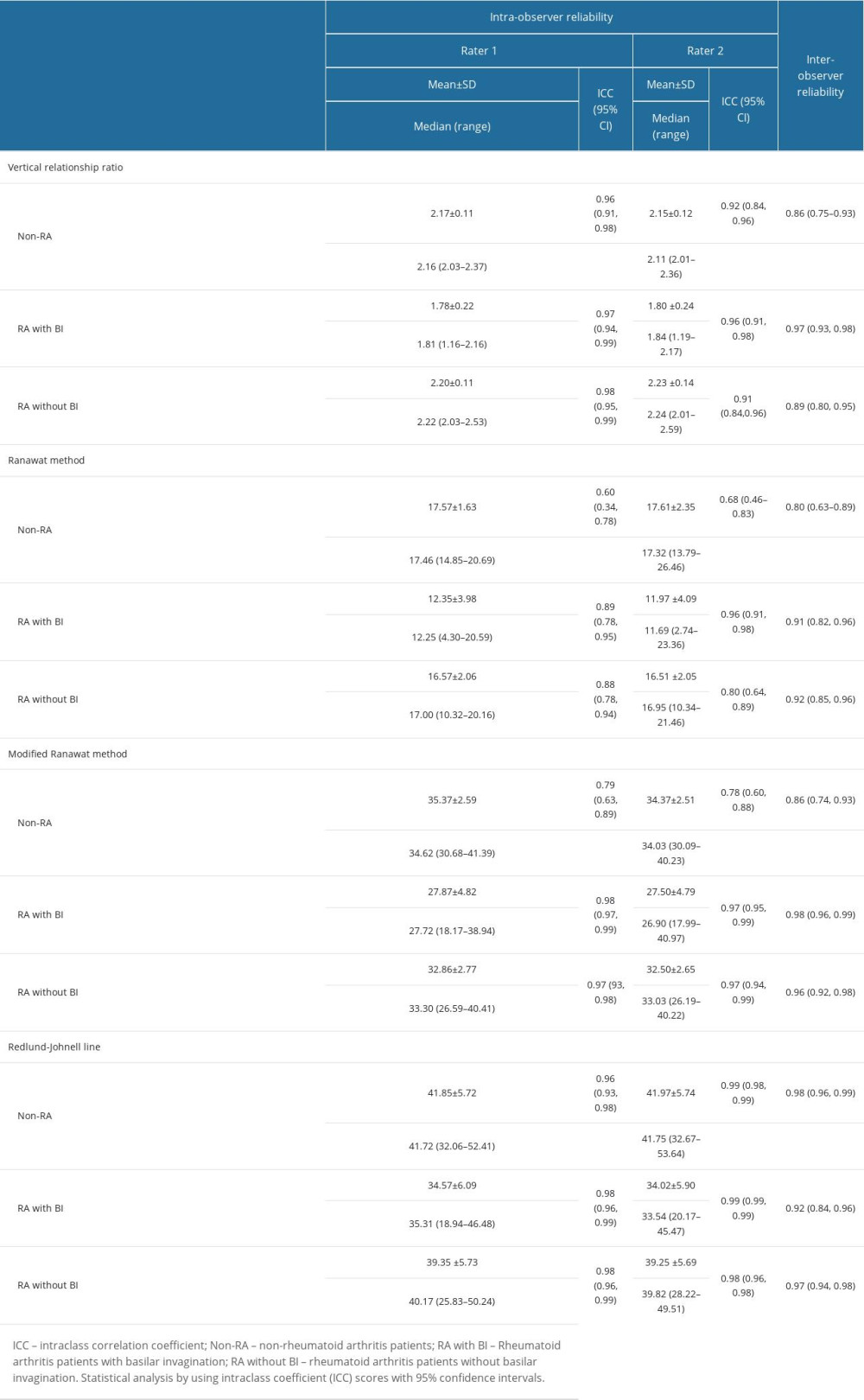 Table 2. Intra- and inter-observer reliability of different measurements in each group of patients.
Table 2. Intra- and inter-observer reliability of different measurements in each group of patients.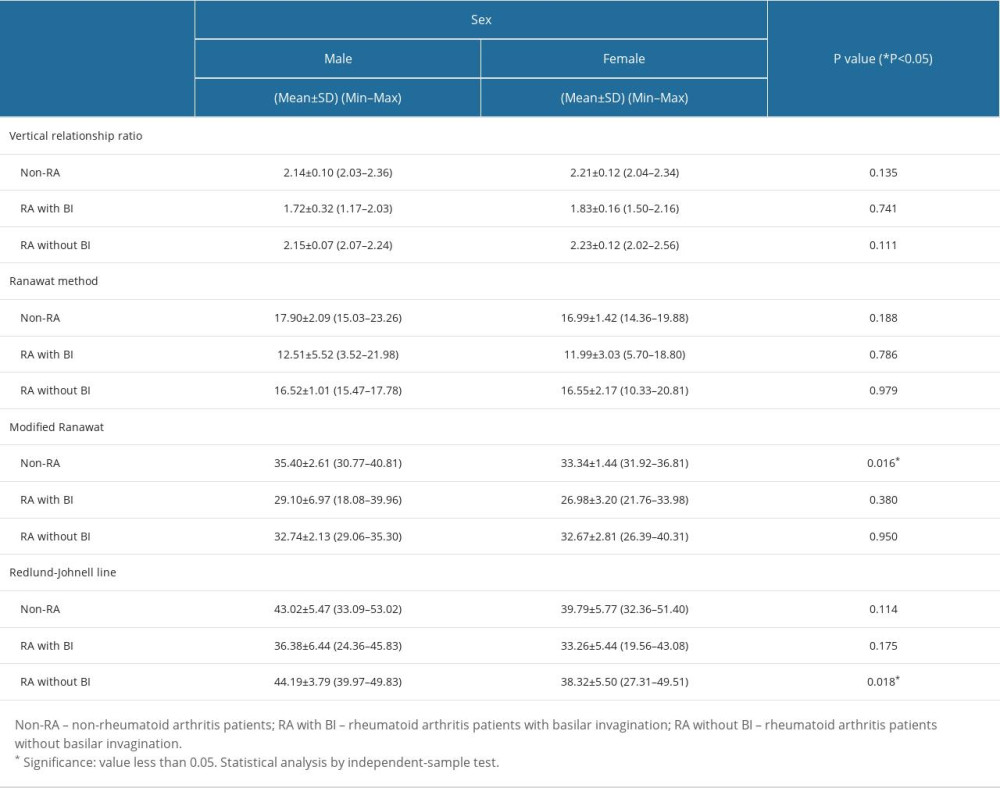 Table 3. Effect of sex on all different measurements in each group of patients.
Table 3. Effect of sex on all different measurements in each group of patients. In Press
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








