07 April 2024: Clinical Research
Arthroscopic Treatment of Popliteal Cyst Through the Posterior Portal: A Comprehensive Clinical Study
Kanghua Yang1CE, Zhengnan Li1BD, Jinjie Gui1AF*DOI: 10.12659/MSM.943472
Med Sci Monit 2024; 30:e943472
Abstract
BACKGROUND: A popliteal cyst, often perceived as benign, poses potential harm and symptoms. This study focused on arthroscopic treatment through the posterior knee portal at our medical center, aiming to assess its efficacy, safety, and long-term outcomes compared to traditional methods.
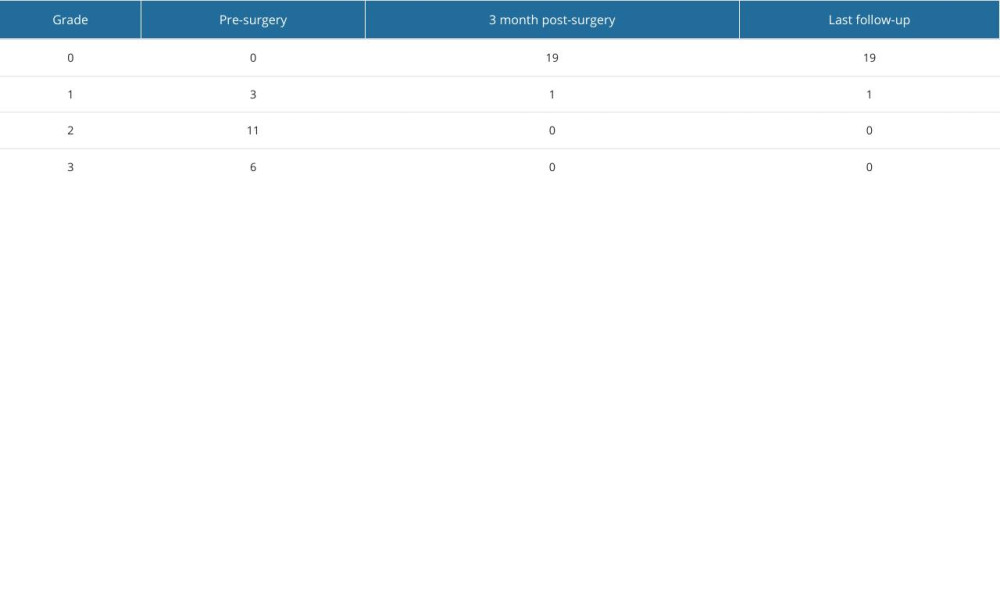
MATERIAL AND METHODS: A retrospective analysis of 20 patients (9 males and 11 females) with symptomatic popliteal cysts (January 2020 to December 2022) undergoing arthroscopic treatment via the posterior knee portal was conducted. Data on demographics, clinical presentation, preoperative imaging, surgical techniques, intraoperative findings, and postoperative Rauschning and Lindgren scores were collected and analyzed.
RESULTS: With a mean follow-up of 13.6 months (range: 12 to 36 months), all patients had associated intra-articular lesions and were treated. Degenerative cartilage damage was most common (65.0% of cases). The Rauschning and Lindgren score significantly improved after surgery (P<0.05), with no recurrence evident on MRI in any patients.
CONCLUSIONS: Arthroscopic treatment through the posterior knee portal has good potential for popliteal cyst management. This minimally invasive approach offers benefits such as direct visualization, precise cyst excision, and concurrent treatment of intra-articular pathologies.
Keywords: Arthroscopy, Popliteal Cyst, Posterior Portal, minimally invasive
Introduction
Popliteal cysts, commonly known as Baker’s cysts, are relatively common, particularly in adults aged 35 to 70 years, with a slightly higher prevalence in females. While many patients are asymptomatic, symptomatic presentations include visible swelling, pain, stiffness, and a feeling of tightness in the posterior knee [1,2]. These symptoms often worsen with activities involving knee flexion or extension. Joint effusion and restricted range of motion are also common features [3]. The diagnosis is frequently made through imaging studies, and Baker’s cysts can coexist with various other knee joint disorders. In managing these cysts, a range of approaches is employed based on symptom severity and underlying pathology [2]. Conservative measures involve rest, ice, compression, and analgesics, while more invasive options include cyst aspiration and corticosteroid injections [4]. Physical therapy aims to improve joint mobility and muscle strength. Surgical intervention, such as the arthroscopic treatment described here, is considered for persistent or symptomatic cases, offering benefits like direct visualization, precise cyst excision, and concurrent treatment of intra-articular pathologies. It is essential to address the underlying knee joint pathology to prevent recurrence. The management of Baker’s cysts is tailored to individual cases, emphasizing a combination of conservative and, when necessary, surgical interventions to alleviate symptoms, improve joint function, and enhance the overall quality of life for affected individuals [5].
Historically, open excision was considered for persistent symptomatic cases; however, the associated recurrence rate was quite high, reaching up to 63% [6]. One significant limitation of this approach was the difficulty in achieving a tight closure over the valvular opening, leading to the necessity of a large open wound [7]. Recognizing these challenges, in 1999, Sansone and De Ponti proposed arthroscopic treatment for popliteal cysts, presenting a novel approach that simultaneously addresses the valvular opening and the associated intra-articular pathology [8].
In this study, we investigated the evolving landscape of arthroscopic interventions for popliteal cysts by presenting a comprehensive clinical study focused on the outcomes of arthroscopic treatment through the posterior portal of the knee. Building upon previous studies, we assessed the efficacy and nuances of this technique, seeking to enhance our understanding of its clinical benefits, complications, and overall effectiveness in comparison to alternative approaches.
Through a review of results obtained from arthroscopic treatment at our center, we aim to provide valuable insights into the outcomes of this procedure, shedding light on its potential as a minimally invasive and effective alternative to traditional open excision. By critically analyzing the data, we seek to contribute to the ongoing discourse on optimal interventions for popliteal cysts, ultimately advancing the field towards improved patient outcomes and reduced recurrence rates. Therefore, this retrospective study included 20 patients with symptomatic popliteal cysts to evaluate arthroscopic treatment via the posterior transseptal portal between January 2020 and December 2022 at our medical center.
Material and Methods
PATIENT DEMOGRAPHICS:
The study obtained approval from the local ethics committee, and informed consent was obtained from all participating patients. The research focused on 20 patients with symptomatic popliteal cysts treated at the Department of Sports Medicine, Ganzhou People’s Hospital, between January 2020 and December 2022. The patient cohort comprised 9 males and 11 females, with an average age of 57.62 years (range: 21 to 76 years). Among these cases, 12 were observed in the left knee, while 8 were in the right knee. The main concerns reported by the patients were posterior knee pain, swelling, and restricted deep knee flexion. Each patient had undergone conservative treatments for a minimum of 6 months before considering surgical intervention. Preoperative magnetic resonance imaging (MRI) was conducted for all patients to assess the cyst and intra-articular pathology. The MRI procedures aimed to provide detailed visualization of the popliteal cyst, associated intra-articular lesions, and the overall condition of the knee joint. These imaging studies were crucial for preoperative planning and understanding the extent of pathology. The MRI evaluation followed standardized protocols to ensure consistency across the patient cohort. The imaging findings, including the size and characteristics of the cyst, were documented and utilized for preoperative assessment (Figure 1). Clinical evaluation followed the criteria proposed by Rauschning and Lindgren, and the surgical procedures were consistently performed by the same surgeon.
SURGICAL TECHNIQUE:
Following successful anesthesia, patients were placed in the supine position. A tourniquet was applied to the root of the affected-side thigh for hemostasis, and standard surgical draping was carried out in the conventional surgical field. The procedure was performed under tourniquet control.
A lateral incision was made on the anterior aspect of the affected knee. Arthroscopic exploration revealed synovial effusion, synovial hyperplasia, partial wear of the medial and lateral condyles of the femur, and the medial plateau of the tibia. No apparent abnormalities are observed in the anterior and posterior cruciate ligaments or the lateral meniscus. The medial meniscus showed degenerative changes. An additional medial incision was made on the anterior aspect of the knee. Using a curette and plasma radiofrequency knife, synovial hyperplasia was cleared, and the wound was carefully rendered hemostatic.
Two posterior medial incisions were established. Under arthroscopic surveillance, the light source entered through the lateral anterior aspect of the knee, passing through the gap between the posterior cruciate ligament and the medial condyle, and entering the posterior medial compartment. With the knee in a P-shaped position, a high-level posterior medial approach was established through skin-point localization. The curette was introduced through a high-level approach into the posterior medial compartment. The partial medial joint capsule was excised with the curette, exposing the popliteal cyst located behind the medial head of the gastrocnemius. Through the high-level approach, a probe was inserted into the popliteal cyst. The light source was withdrawn from the anterior lateral aspect, and the probe was inserted into the popliteal cyst from the posterior medial aspect. Under light-source surveillance, a low-level medial working approach was established from 3 cm below the high-level approach, through the gap between the semimembranosus and the gastrocnemius. A curette was inserted through this approach, thoroughly removing the cyst wall, enlarging the drainage opening, achieving effective hemostasis, and irrigating the joint cavity. After confirming the absence of instrument-related issues, each incision was sutured, and sterile dressings were applied.
FOLLOW-UP:
Each patient underwent a postoperative follow-up lasting a minimum of 1 year, with an average of 13.6 months (range: 12 to 36 months). At 3 months postoperatively and during the final follow-up, all patients underwent MRI examinations to identify any popliteal cyst recurrence. Additionally, the Rauschning and Lindgren score for clinical outcomes was assessed at 3 months after surgery and again at the last follow-up.
STATISTICAL ANALYSIS:
GraphPad Prism 8.0 (GraphPad Software, CA, USA) was used to perform the statistical analysis. The paired Student’s t test was applied to compare Rauschning and Lindgren scores before and after surgery.
Results
RAUSCHNING AND LINDGREN SCORE:
In all cases, we identified and addressed associated intra-articular lesions. The Rauschning and Lindgren scores recorded before surgery were grade 1 in 3 cases (15.0%), grade 2 in 11 cases (55.0%), and grade 3 in 6 cases (30.0%). Three months after surgery, there was a significant improvement in scores, with 19 cases (95.0%) achieving grade 0 and 1 case (5.0%) reaching grade 1 (P<0.05). These improvements were consistently observed until the last follow-up (Table 1).
MRI EVALUATION:
MRI evaluations were conducted for all patients at 3 months postoperatively and during the final follow-up (Figure 2). No signs of recurrence were identified in any patients, and there was no evidence of cysts after surgery through the last follow-up.
Throughout the follow-up period, we encountered no major complications, including neurovascular injury, deep vein thrombosis, or deep infection. We just found one case of superficial infection, which was cured after dressing changes.
Discussion
The findings of this comprehensive clinical study provide valuable insights into the efficacy and safety of arthroscopic treatment through the posterior portal of the knee for symptomatic popliteal cysts. The investigation, encompassing 20 patients over a mean follow-up period of 13.6 months, demonstrates promising outcomes in terms of both intra-articular pathology correction and prevention of recurrence, consistent with some previous studies [6,10].
Our results affirm the association between popliteal cysts and intra-articular pathology, with degenerative cartilage damage identified as the predominant pathology (65% of cases). This underscores the importance of addressing the underlying joint issues concurrently with cyst management. The use of the Rauschning and Lindgren score [9] as a clinical assessment tool reveals a significant improvement after surgery, indicating the positive impact of arthroscopic intervention on patients’ clinical outcomes.
In this study, the arthroscopic technique employed was a refined surgical method that included lateral incision, a medial incision, and 2 posterior medial incisions. This comprehensive approach allows for a thorough exploration of the joint, clearance of synovial hyperplasia, and, most importantly, direct observation and excision of the popliteal cyst. The use of arthroscopic surveillance, coupled with a figure-of-four positioning, further enhances the precision of the surgery. The application of arthroscopic technology reduces surgical trauma, accelerates recovery time, and minimizes the risk of postoperative infections. Additionally, it enables physicians to more accurately diagnose and treat knee joint diseases, thereby improving treatment outcomes. Kongmalai and Chernchujit [6] reported on intracystic debridement using a direct posterior portal, showcasing an alternative arthroscopic technique. Ahn et al [10], on the other hand, explore the posteromedial cystic portal for cystectomy. These studies contribute to the evolving landscape of arthroscopic interventions for popliteal cysts. In addition, a meta-analysis by Hao Li et al concluded that the posterior approach is undoubtedly more convenient and beneficial for patients requiring long-term knee rehabilitation [4].
In implementing this arthroscopic surgery, physicians should possess a high level of expertise and skills, while also utilizing various advanced medical devices. The arthroscopic surgery employed in this study is a delicate and complex procedure that requires a trained surgeon. Using advanced medical equipment and refined surgical instruments, physicians can more accurately diagnose and treat various knee joint diseases. This surgical approach not only reduces patient pain and recovery time but also enhances treatment effectiveness and patient satisfaction. For those who cannot tolerate traditional surgery, arthroscopic surgery can be an ideal choice [11].
Additionally, arthroscopic surgery can be employed to prevent the occurrence of knee joint diseases. Regular arthroscopic examinations can quickly detect and treat early knee joint injuries or diseases, thereby preventing worsening of the condition [12]. With the continuous development and refinement of this technology, we believe that it will play an increasingly important role in the future treatment of knee joint diseases. The absence of recurrence in any of our patients during the follow-up period, as confirmed by clinical evaluation and MRI examinations, is a noteworthy outcome. This suggests that arthroscopic treatment through the posterior portal effectively disrupts the unidirectional flow mechanism responsible for cyst persistence.
Arthroscopic treatment is a compelling alternative to the conventional open excision method, showing its potential as a minimally invasive and highly effective approach in management of popliteal cysts [13]. This innovative technique stands out not only for its efficacy but also for its favorable safety profile, as evidenced by the absence of major complications commonly associated with surgical procedures, including neurovascular injury, deep vein thrombosis, and infection. The meticulous examination of potential complications underscores the reliability and safety of arthroscopic treatment, reinforcing its status as a viable and secure option for patients.
A noteworthy aspect of this study is its dedicated exploration of long-term outcomes following arthroscopic intervention, providing a comprehensive perspective on the sustained effectiveness of this approach. Despite the relatively modest mean follow-up duration of 13.6 months, the findings contribute valuable insights into the durability and stability of the treatment outcomes. This emphasis on the extended postoperative period adds depth to our understanding of arthroscopic interventions, shedding light on their ability to deliver enduring benefits for patients with symptomatic popliteal cysts.
The study’s commitment to assessing complications beyond the immediate postoperative phase underscores a thorough evaluation of the procedure’s safety and durability. The absence of major complications not only attests to the proficiency of the surgical team but also reinforces the notion that arthroscopic treatment through the posterior knee portal is a reliable and secure method for treating popliteal cysts. This is particularly significant in the context of orthopedic interventions where patient safety and long-term well-being are paramount considerations.
The results of the study, indicating the successful identification and treatment of associated intra-articular lesions in all patients, further underscore the comprehensive nature of arthroscopic intervention. The prevalence of degenerative cartilage damage highlights the importance of addressing not only the cyst itself but also the concurrent pathologies within the joint. The improvement observed in the Rauschning and Lindgren scores after surgery aligns with the broader clinical goal of enhancing patients’ functional outcomes and quality of life.
Despite the promising results, it is essential to acknowledge certain limitations inherent in the study design and methodology. The relatively small sample size of 20 patients may limit the generalizability of the findings, and the short-to-moderate follow-up duration of 13.6 months raises questions about the long-term sustainability of the observed outcomes. Additionally, the absence of a control group and randomization in patient selection may have introduced bias, and the single-center nature of the study could have affected external validity. Furthermore, the reliance on self-reported patient symptoms and the retrospective nature of the analysis may have introduced recall bias. The study’s commitment to assessing complications beyond the immediate postoperative phase is commendable; however, a more extended follow-up period would provide a more comprehensive evaluation of the durability and stability of the treatment outcomes. These limitations should be considered when interpreting the study’s findings and formulating future research directions.
Conclusions
The outcomes of this study support arthroscopic treatment through the posterior portal of the knee as a promising and effective intervention for popliteal cysts. This minimally invasive approach offers benefits such as direct visualization, precise cyst excision, and concurrent treatment of intra-articular pathologies
Figures
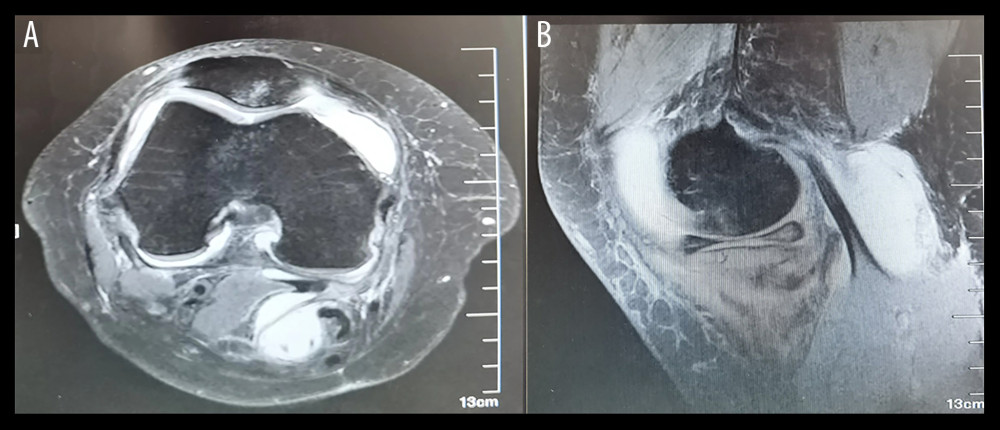 Figure 1. Case 1, Female, 53 years old, right popliteal cyst(A) Preoperative magnetic resonance imaging (MRI) transverse section showing: the popliteal cyst is located behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle; (B) Preoperative MRI sagittal section indicating: the popliteal cyst is situated behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle.
Figure 1. Case 1, Female, 53 years old, right popliteal cyst(A) Preoperative magnetic resonance imaging (MRI) transverse section showing: the popliteal cyst is located behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle; (B) Preoperative MRI sagittal section indicating: the popliteal cyst is situated behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle. 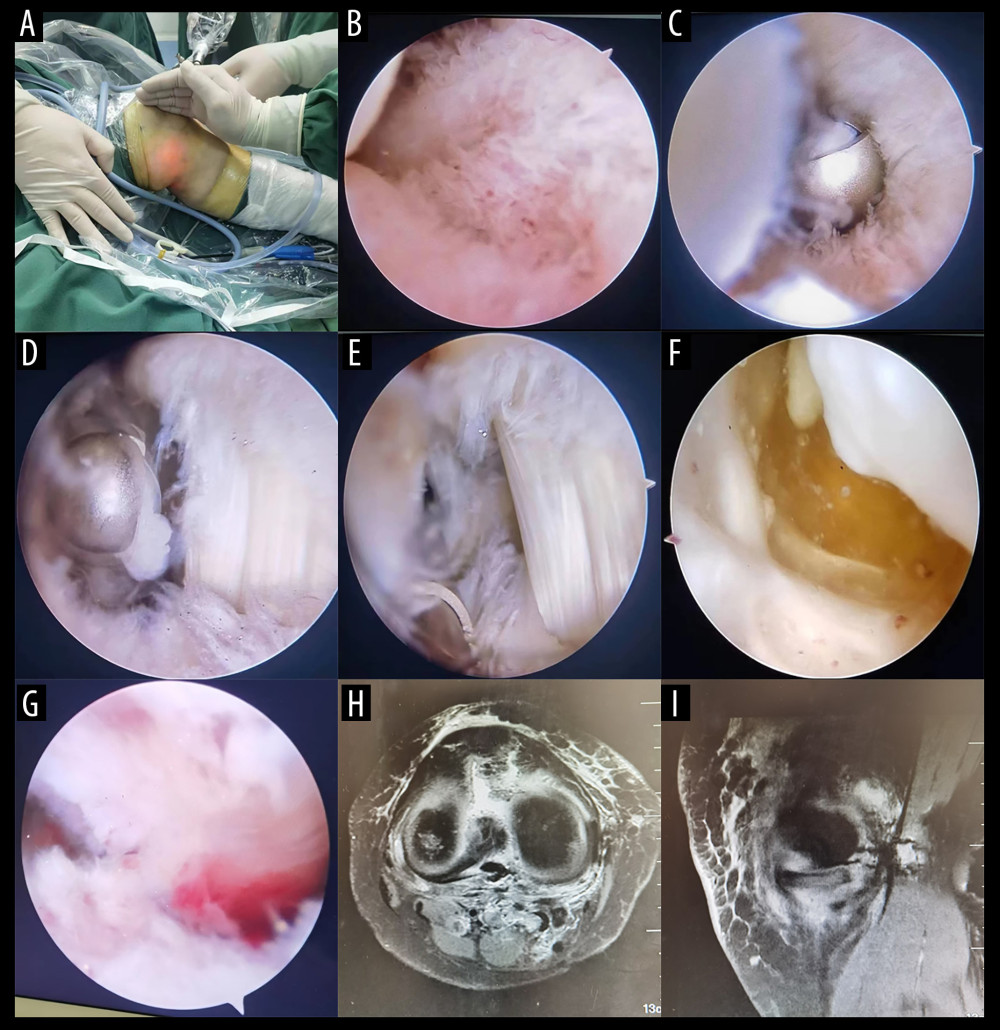 Figure 2. The surgical procedure and postoperative imaging data(A) Establishing the medial high-level channel through the light spot; (B) Expose the posterior medial compartment of the knee joint; (C) Use a gouge to excise the posterior medial portion of the joint capsule, exposing the inner head of the gastrocnemius muscle; (D) Expose the inner head of the gastrocnemius muscle; (E) Expose the drainage opening between the gastrocnemius and semimembranosus muscles; (F) Under the arthroscope, the cyst wall of the popliteal cyst and yellowish fluid within the cyst are observed; (G) The cyst wall is completely excised, and the drainage opening is enlarged postoperatively; (H, I) MRI cross-sectional and sagittal views: Postoperative review reveals excision of the cyst.
Figure 2. The surgical procedure and postoperative imaging data(A) Establishing the medial high-level channel through the light spot; (B) Expose the posterior medial compartment of the knee joint; (C) Use a gouge to excise the posterior medial portion of the joint capsule, exposing the inner head of the gastrocnemius muscle; (D) Expose the inner head of the gastrocnemius muscle; (E) Expose the drainage opening between the gastrocnemius and semimembranosus muscles; (F) Under the arthroscope, the cyst wall of the popliteal cyst and yellowish fluid within the cyst are observed; (G) The cyst wall is completely excised, and the drainage opening is enlarged postoperatively; (H, I) MRI cross-sectional and sagittal views: Postoperative review reveals excision of the cyst. References
1. Abate M, Di Carlo L, Di Iorio A, Salini V, Baker’s cyst with knee osteoarthritis: Clinical and therapeutic implications: Med Princ Pract, 2021; 30(6); 585-91
2. Frush TJ, Noyes FR, Baker’s cyst: Diagnostic and surgical considerations: Sports Health, 2015; 7(4); 359-65
3. Labropoulos N, Shifrin DA, Paxinos O, New insights into the development of popliteal cysts: Br J Surg, 2004; 91(10); 1313-18
4. Li H, Zhang M, Li Y, Wang H, Comparison of clinical outcomes associated with arthroscopic cyst wall preservation or resection in the treatment of popliteal cyst: A systematic review and meta-analysis: Arch Orthop Trauma Surg, 2021; 141(10); 1741-52
5. Ahn JH, Lee SH, Yoo JC, Arthroscopic treatment of popliteal cysts: Clinical and magnetic resonance imaging results: Arthroscopy, 2010; 26(10); 1340-47
6. Kongmalai P, Chernchujit B, Arthroscopic treatment of popliteal cyst: A direct posterior portal by inside-out technique for intracystic debridement: Arthrosc Tech, 2015; 4(2); e143-e48
7. Han JH, Bae JH, Nha KW, Arthroscopic treatment of popliteal cysts with and without cystectomy: A systematic review and meta-analysis: Knee Surg Relat Res, 2019; 31(2); 103-12
8. Sansone V, De Ponti A, Arthroscopic treatment of popliteal cyst and associated intra-articular knee disorders in adults: Arthroscopy, 1999; 15(4); 368-72
9. Rauschning W, Lindgren PG, Popliteal cysts (Baker’s cysts) in adults. I. Clinical and roentgenological results of operative excision: Acta Orthop Scand, 1979; 50(5); 583-91
10. Ahn JH, Yoo JC, Lee SH, Arthroscopic cystectomy for popliteal cysts through the posteromedial cystic portal: Arthroscopy, 2007; 23(5); 559e1-4
11. Zhang T, Xu S, Li H, Comparison of the clinical effects of arthroscopic surgery vs. open surgery for grade II gluteal muscle contracture in adults: Exp Ther Med, 2018; 16(1); 364-69
12. Madry H, Kon E, Condello V, Early osteoarthritis of the knee: Knee Surg Sports Traumatol Arthrosc, 2016; 24(6); 1753-62
13. Brazier BG, Sudekum SA, DeVito PM, Dodds JA, Arthroscopic treatment of popliteal cysts: Arthrosc Tech, 2018; 7(11); e1109-e14
Figures
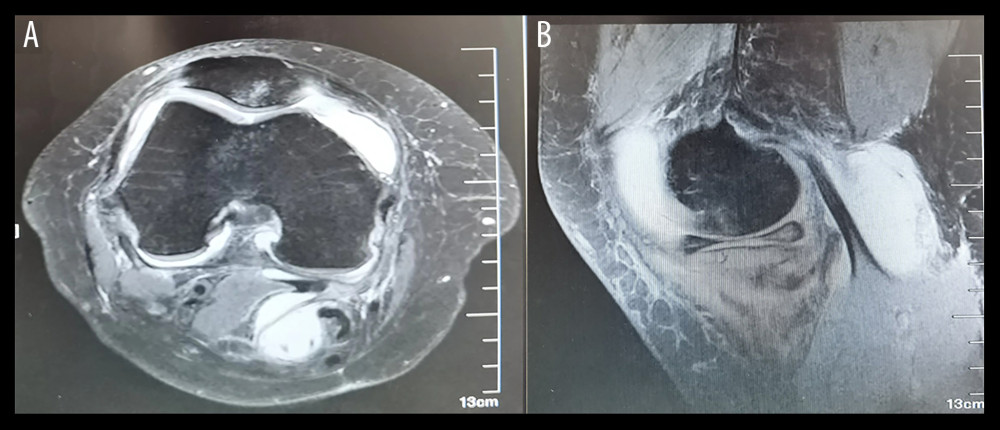 Figure 1. Case 1, Female, 53 years old, right popliteal cyst(A) Preoperative magnetic resonance imaging (MRI) transverse section showing: the popliteal cyst is located behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle; (B) Preoperative MRI sagittal section indicating: the popliteal cyst is situated behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle.
Figure 1. Case 1, Female, 53 years old, right popliteal cyst(A) Preoperative magnetic resonance imaging (MRI) transverse section showing: the popliteal cyst is located behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle; (B) Preoperative MRI sagittal section indicating: the popliteal cyst is situated behind the medial head of the gastrocnemius and the tendon of the semimembranosus muscle.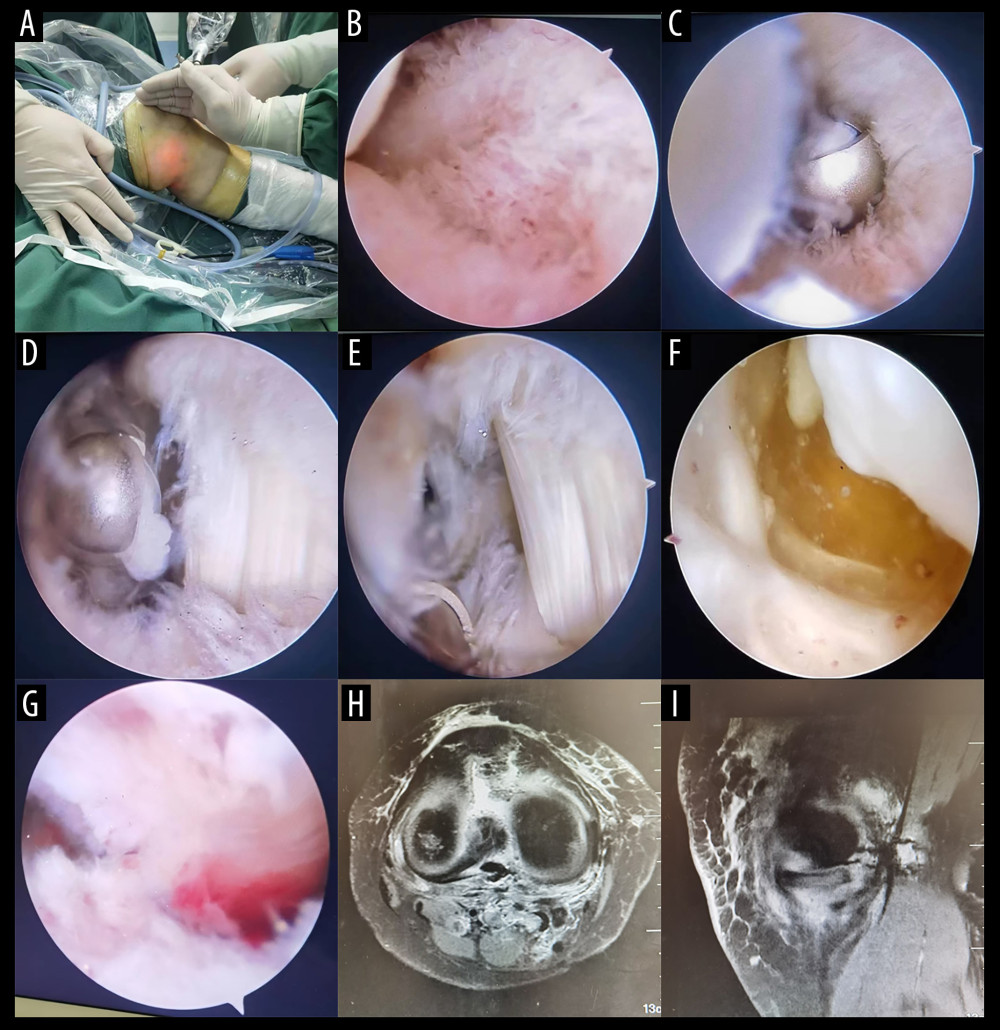 Figure 2. The surgical procedure and postoperative imaging data(A) Establishing the medial high-level channel through the light spot; (B) Expose the posterior medial compartment of the knee joint; (C) Use a gouge to excise the posterior medial portion of the joint capsule, exposing the inner head of the gastrocnemius muscle; (D) Expose the inner head of the gastrocnemius muscle; (E) Expose the drainage opening between the gastrocnemius and semimembranosus muscles; (F) Under the arthroscope, the cyst wall of the popliteal cyst and yellowish fluid within the cyst are observed; (G) The cyst wall is completely excised, and the drainage opening is enlarged postoperatively; (H, I) MRI cross-sectional and sagittal views: Postoperative review reveals excision of the cyst.
Figure 2. The surgical procedure and postoperative imaging data(A) Establishing the medial high-level channel through the light spot; (B) Expose the posterior medial compartment of the knee joint; (C) Use a gouge to excise the posterior medial portion of the joint capsule, exposing the inner head of the gastrocnemius muscle; (D) Expose the inner head of the gastrocnemius muscle; (E) Expose the drainage opening between the gastrocnemius and semimembranosus muscles; (F) Under the arthroscope, the cyst wall of the popliteal cyst and yellowish fluid within the cyst are observed; (G) The cyst wall is completely excised, and the drainage opening is enlarged postoperatively; (H, I) MRI cross-sectional and sagittal views: Postoperative review reveals excision of the cyst. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952