01 March 2024: Clinical Research
A Study of 60 Patients with Low Back Pain to Compare Outcomes Following Magnetotherapy, Ultrasound, Laser, and Electrotherapy with and without Lumbosacral Kinesiotherapy
Marko KosićDOI: 10.12659/MSM.943732
Med Sci Monit 2024; 30:e943732
Abstract
BACKGROUND: This study of 60 patients with low back pain (LBP) aimed to compare outcomes following magnetotherapy, ultrasound therapy, laser therapy, and electrotherapy, with and without lumbosacral kinesiotherapy, and used the Roland-Morris Disability Questionnaire (RMDQ) and the Oswestry Low Back Pain Disability Questionnaire (OLBPDQ). This was a randomized actively controlled intervention trial of adding kinesiotherapy to a standard physiotherapy for LBP.
MATERIAL AND METHODS: The research included 60 participants with a diagnosis of chronic non-specific lumbar pain syndrome (CNSLPS) (mean±SD age 58.3±15.4 years, 37 women) LBP randomly assigned (1: 1) to 2 treatment groups. In Group 1, 30 patients were treated with magnetotherapy, ultrasound therapy, laser therapy, and electrotherapy. In Group 2, 30 patients received the same treatments as in Group 1, and also performed kinesiotherapy exercises affecting the lumbosacral spine and adjacent muscles. At baseline and at the end of the study, all participants completed the RMDQ and the OLBPDQ.
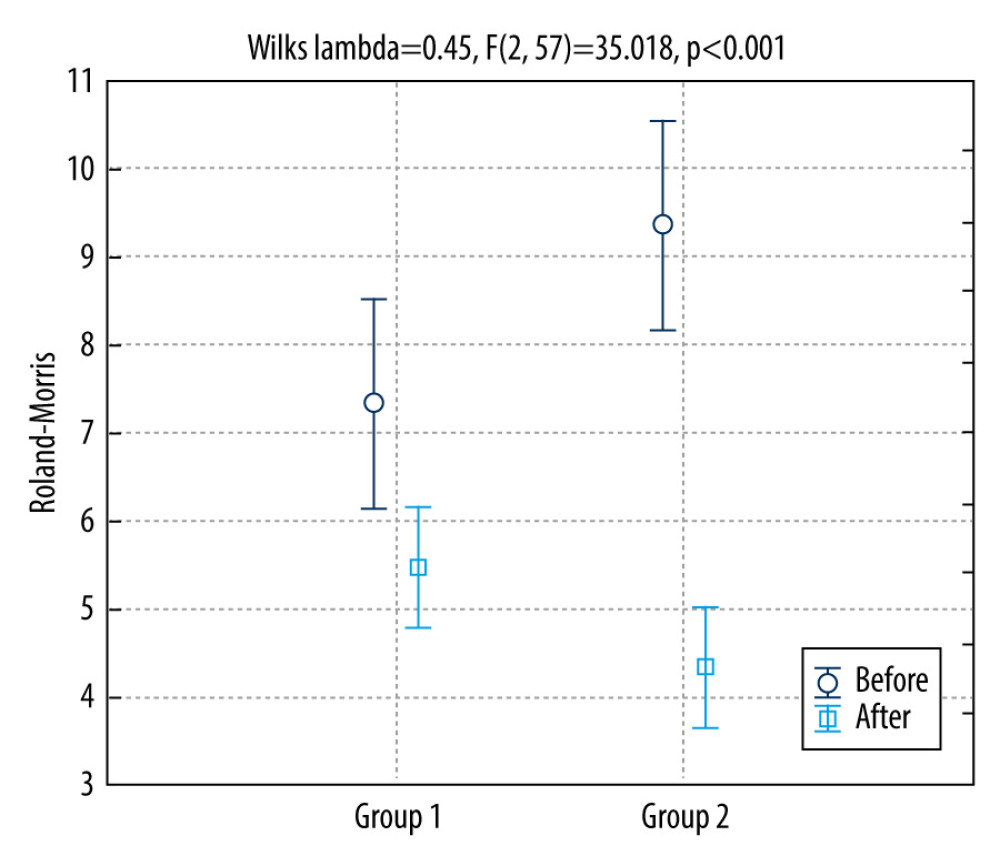
RESULTS: Both groups had significant improvement after therapy. Repeated-measures ANOVA indicated that at the end of treatment there was significantly greater progress and symptom reduction (P<0.001) in Group 2. Patients in Group 2 had a pain reduction of 52.5%, while Group 1 had 25.4% pain reduction (P=0.009).
CONCLUSIONS: For treatment of disability caused by CNSLPS, physical therapy combined with kinesiotherapy should be a treatment of choice.
Keywords: Low Back Pain, Physical Therapy Modalities, Rehabilitation, Spine
Introduction
DIAGNOSIS AND MANAGEMENT:
Differential diagnosis of back pain in adults is complicated [18] and it can have many causes: lumbosacral muscle strains and sprains, lumbar spondylosis, disk herniation, spondylolysis, spondylolisthesis, repetitive spinal stress [28], vertebral compression fracture, spinal stenosis, and tumors – 97% of spinal tumors are metastatic [29] and many patients have infections [30].
MANAGEMENT OF BACK PAIN IN ADULTS:
The first-line treatments are nonpharmacological and include [18] early return to normal routines, avoidance of activities that precipitate the pain, and patient education. Second-line options that may be offered to the patient include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, opioids, spinal manipulation, physical therapy, superficial heat application, and alternative treatments like acupuncture and massage. Patient education is crucial in preventing back pain aggravation or recurrence. The patient may be advised to follow up after 2 weeks [18]. If the cause is non-specific, advise the patient to remain active and avoid precipitating factors. Exercise therapy is also considered a first-line treatment [31,32].
CLINICAL PRACTICE GUIDELINES:
Exercise therapy is most effective, and most guidelines (10 of 14; 71%) recommend exercise therapy for patients with CNSLPS [25]. There are important differences in the type of exercise and the programs that are carried out, as well as the method of performance. Thus, we use a large selection of exercises such as water exercises, stretching, back schools, McKenzie approach to exercises, yoga, and tai-chi, then individually design supervised at-home exercise program and group exercises. Guidelines have been issued that make inconsistent recommendations about exercise therapy for acute LBP [25]. Most guidelines recommend the use of NSAIDs and antidepressants for the treatment of patients with CNSLPS, and prescribe exercise and psychosocial interventions. In case of more serious problems or no improvement after 4 weeks to 2 years, it is recommended that the patient consult a specialist [25]. The Oswestry Back Pain Disability Questionnaire (OLBPDQ) is considered the most important tool for use in research and assessment of permanent functional disability, and it is considered the criterion standard tool spondylolisthesis, repetitive [33]. The Roland-Morris Disability Questionnaire (RMDQ) is most sensitive for patients with mild to moderate disability caused by acute or chronic pain [34]. To assess patient health, 136 items are used, which cover all aspects of physical and mental functioning and serve as the basis for the RMDQ [34,35].
Our hypothesis in the present study was that physical therapy combined with kinesiotherapy would be more effective in treating chronic non-specific lumbar pain syndrome (CNSLPS) than physiotherapy alone in reducing pain [25]. Our primary objective was to determine which of these 2 therapeutic procedures provides better results in reducing pain in patients with LBP. Our secondary objective was to determine the effectiveness of these 2 therapeutic procedures. Therefore, this study of 60 patients with low back pain aimed to compare outcomes following magnetotherapy, ultrasound, laser, and electrotherapy with and without lumbosacral kinesiotherapy, and used the RMDQ and the OLBPDQ.
Material and Methods
ETHICS APPROVAL AND STUDY DESIGN:
The study was approved by a Local Ethics Committee, University of Rijeka, Faculty of Medicine (approval no. 2170-24-01-22-1/MJ). Patients were required to sign the informed consent form before any procedure was done. The study design and the informed consent were in accordance with the Nuremberg Code and the latest revision of the Declaration of Helsinki and national laws and bylaws.
This was a single-center, randomized, positive control intervention pilot study to assess the effectiveness of adding kinesitherapy to the usual physiotherapy care for LBP.
PARTICIPANTS AND GROUPS:
We recruited 60 participants referred to the polyclinic for physical therapy with a diagnosis of chronic non-specific lumbar pain syndrome (CNSLPS). The diagnosis was provided by the referring physician, who is a specialist in physical medicine and rehabilitation from another institution. The patients were assigned to a 1 of 2 treatment groups in a 1: 1 ratio using random assignment with numbers from a sealed envelope previously prepared by an independent statistician using an online randomizer program (
The groups are defined by the type of therapy performed: Group 1 received a combination of physiotherapy procedures: 1) ultrasound (MedicalDevice EV 904), power 0.8–2 W/cm2 with patient lying down on the table in prone position. Ultrasound was applied to the left and right lumbar area for 5 min (for a total for 10 min); 2) laser (ASV device), intensity 50%, frequencies 1500 Hz with the patient lying down on the table in prone position. Laser was applied to the left and right lumbar area for 3 min (for a total of 6 min). 3) IF current (MedicalDevice EV 904), maximal power 100 mA with the patient lying down in prone position. Electricity was applied to the area of the lumbar spine for 10 min. 4) Magnetotherapy (ASV device), frequencies 100 Hz, intensity 60%, with the patient lying down in supine position on the back. The coil of the magnet was placed on the lumbar part of the spine and activated for 20 min. The duration of a single-visit physiotherapy for group 1 was 46 min. Group 2 received a combination of the same physiotherapy procedures as in group 1 with the addition of kinesiotherapy of the lumbosacral spine. Kinesiotherapy was provided for 20 min. The exercises performed are presented in the supplemental material. Total treatment time for a single visit was 66 min.
Physical therapy for all patients was administered by a qualified physiotherapist with a Master of Physiotherapy degree.
QUESTIONNAIRES:
To assess the effectiveness of therapy in these 2 treatment groups, 2 questionnaires were used before and after treatment: the modified version of the Roland-Morris Disability Questionnaire (RMDQ) and the Oswestry Low Back Pain Disability Questionnaire (OLBPDQ).
The modified version of the RMDQ consists of 24 statements concerning different activities of everyday life. Each statement was assigned a score of 0 or 1, where the higher number of points indicates a higher degree of disability. The maximum number of points is 24 [34].
The OLBPDQ consists of 10 items – pain intensity, personal care (washing, dressing, etc.), lifting, walking, sitting, standing, sleeping, sex life, social life, travelling – for each of these items, there are 6 statements, with the score ranging from 0 to 5. The maximum number of points is 50 and a higher number of points indicates greater disability [33].
STATISTICAL METHODS:
For data processing, the software package Statistica, version 13.5.0.17, was used (TIBCO Software, Inc. USA). Statistical significance was assessed based on the level of statistical significance
The chi-square test was used to test the difference in the frequency of marked items in the RMDQ. Repeated-measures ANOVA was used to assess the difference in effectiveness between groups.
Results
DEMOGRAPHIC CHARACTERISTIC OF PARTICIPANTS:
The research included 60 participants – 37 women (62%) and 23 men (38%), with a mean age of 58.3 (standard deviation 15.4). The mean BMI of the patients was 22.6 with a standard deviation of 3.06 kg/m2. The groups did not significantly differ based on sex (
OSWESTRY LOW BACK PAIN DISABILITY QUESTIONNAIRE:
Results of the OLBPDQ showed that before treatment most participants had problems with everyday activities, such as in section 1, which concerns pain intensity, showing that analgesics provided moderate pain reduction in 31.7% of participants. Regarding personal care, 56.7% could look after themselves normally, but with pain; 43.3% had problems with lifting heavy objects; and 50% could not walk more than 1 km. Sitting was the greatest problem for the working-age participants – 40% experienced problems or felt pain when sitting. A third of the patients (33.3%) could stand as long as they wanted, but with pain. Many participants (51.7%) slept less than 6 h, regardless of the use of analgesics. Regarding physiological needs, sex life of the participants with LBP was very painful – 66.7% of them had painful or very painful sexual activity. Regarding social life, most participants (38.3%) had a normal social life, but social activities increased their degree of pain. Travel was possible for 41.7% of participants, but it caused increase pain.
Our participants could be divided into 2 categories of disability: 75% of them had minimal disability (0–10 points), while 25% had moderate disability (11–20 points). The total points in the questionnaire had an arithmetic mean of 15.83 and standard deviation of 6.19 points. Results for OLBPDQ compared between groups are presented in Table 1. We compared the points between our 2 groups, and the t test showed that there is no significant difference (P=0.592).
ROLAND-MORRIS DISABILITY QUESTIONNAIRE:
The 2 groups of respondents do not differ in the number of points they received on the RMDQ questionnaire (t=0.97, P=0.063) before treatment. Table 2 contains answers based on the items at the beginning and end of therapy.
Table 2 shows the data from RMDQ on the items marked by the respondents for both groups. After the therapy, there was a decrease in the scores of RMDQ, showing improvement in both groups. The chi-square test was used to compare the difference in the number of marked items in the questionnaire by group. Group 2 had significantly better results for questions 6, 7, 9, 10, 13, 14, 21, and 22, and there was no significant difference in the other questions (Table 2).
Group 1, which did not receive kinesiotherapy during rehabilitation, had equal or worse recovery results after treatment compared with before treatment. Group 2, which received kinesiotherapy, had significant progress and symptom reduction by end of treatment compared with the situation before treatment. Repeated-measures ANOVA was used to assess differences in improvement between groups (P<0.001) (Figure 1), showing significantly greater improvement in Group 2 after therapy (Figure 1).
Discussion
LIMITATIONS OF THE STUDY:
The limitations of our study are the small sample size, short duration of treatment, older age of the subjects (greater than 65 years), and lack of a follow-up period. The effect of physical therapy is different in older people; the therapeutic effect is achieved more slowly and pain reduction is more difficult to achieve. It would be interesting to call or contact patients who were in the study after 3 months so that the long-term effect of physical therapy could be assessed. The subjectivity of pain assessment is a limitation, but there are no objective measures of pain, so standardized pain questionnaires must be used so that the results can be comparable. Also, we used questionnaires that show the level of influence on everyday activities, which are important outcomes in pain syndromes. We did not use single-treatment procedures, so we do not know how a single procedure would work in providing benefit, because previous research shows both positive and negative effects on pain reduction in CNSLPS. For future studies, it would be interesting to investigate single procedures, which would need more patients, but also to compare the efficacy in the acute phase of lumbar pain syndrome and to compare it with CNSLPS.
Conclusions
Our study showed that adding kinesiotherapy to standard physiotherapy is superior to standard physiotherapy alone for CNSLPS. This is confirmed by the fact that the group with added kinesiotherapy experienced significantly greater improvement (52.5% vs 25.4%) after only 1 treatment cycle. Our results suggest that physical therapy combined with kinesiotherapy should be a treatment of choice for patients with disability due to CNSLPS. Further research is needed to assess duration of treatment and relapse of symptoms, and to answer questions about the associated individual characteristics important for success of treatment of CNSLPS.
Tables
Table 1. Results obtained using the Oswestry Low Back Pain Disability Questionnaire (N=60).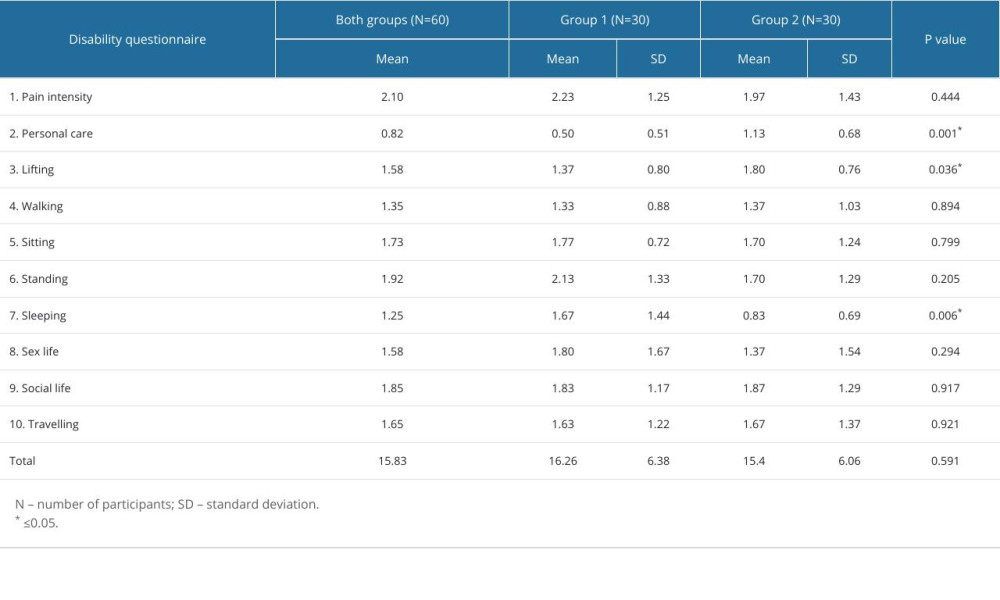 Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60).
Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60).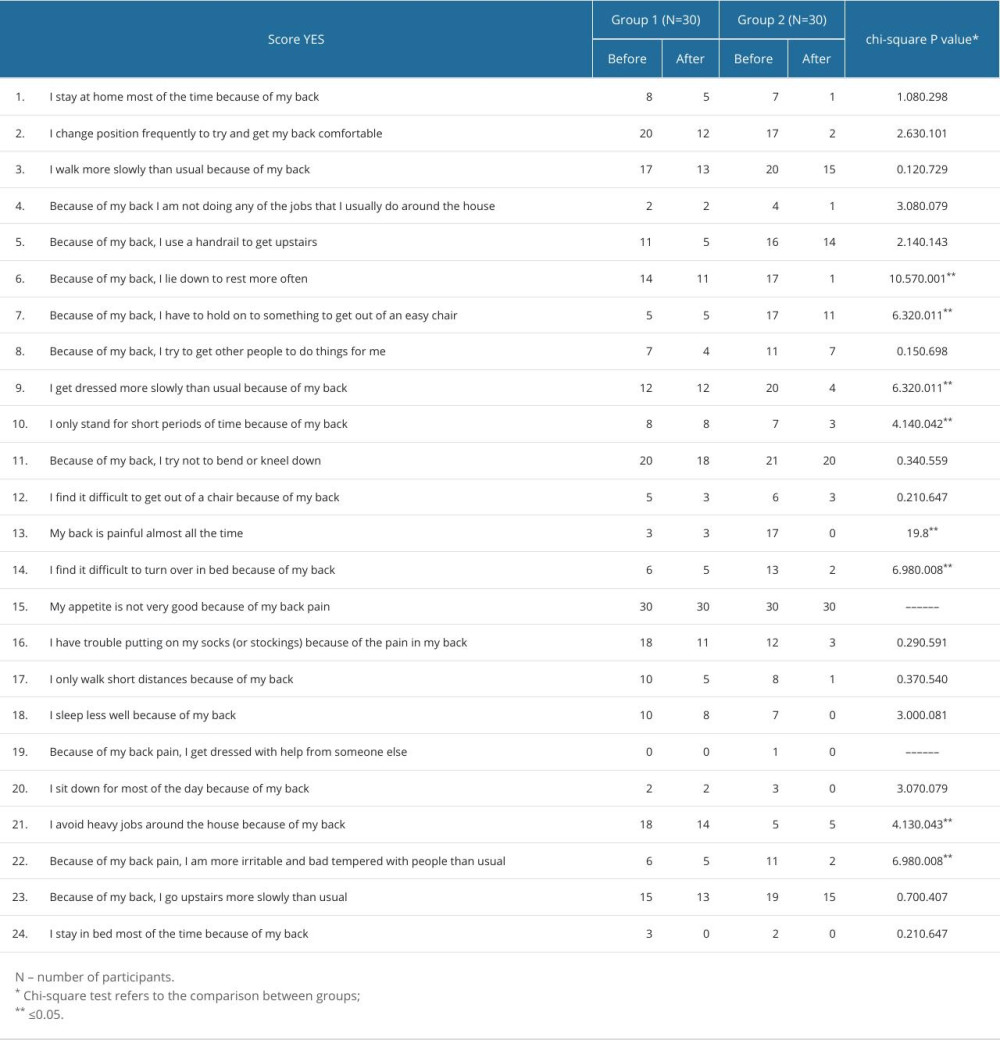
References
1. Akamatsu FE, Ayres BR, Saleh SO, Trigger points: An anatomical substratum: Biomed Res Int, 2015; 2015; 1-5
2. Kamper SJ, Henschke N, Hestbaek L, Musculoskeletal pain in children and adolescents: Braz J Phys Ther, 2016; 20(3); 275-84
3. Zhu S, Xiong J, Chen J, The effectiveness of moxibustion for treating of low back pain: A protocol for systematic review and meta-analysis: Medicine, 2020; 99(43); e22522
4. The Lancet Rheumatology, The global epidemic of low back pain: Lancet Rheumatol, 2023; 5(6); e305
5. Wallwork SB, Braithwaite FA, O’Keeffe M, The clinical course of acute, subacute and persistent low back pain: A systematic review and meta-analysis: CMAJ, 2024; 196(2); E29-E46
6. Common Causes of Back Pain: National Institute of Arthritis and Musculoskeletal and Skin Diseases Available on:https://www.niams.nih.gov/health-topics/back-pain
7. Abdel Shaheed C, Maher CG, Williams KA, Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: A systematic review and meta-analysis: JAMA Intern Med, 2016; 176(7); 958-68
8. Cohen SP, Chen Y, Neufeld NJ, Sacroiliac joint pain: A comprehensive review of epidemiology, diagnosis and treatment: Expert Rev Neurother, 2013; 13(1); 99-116
9. Will JS, Bury DC, Miller JA, Mechanical low back pain: Am Fam Physician, 2018; 98(7); 421-28
10. Patrick N, Emanski E, Knaub MA, Acute and chronic low back pain: Med Clin North Am, 2014; 98(4); 777-89
11. Frost B, Camarero-Espinosa S, Foster E, Materials for the spine: Anatomy, problems, and solutions: Materials, 2019; 12(2); 253
12. Grazio S, Ćurković B, Vlak TDiagnosis and conservative treatment of low back pain: Review and guidelines of the Croatian Vertebrologic Society: Acta Med Croatia, 2012; 66(4); 259-93 [in Croatian]
13. Conger A, Smuck M, Truumees E, Vertebrogenic pain: A paradigm shift in diagnosis and treatment of axial low back pain: Pain Medicine, 2022; 23(Suppl 2); S63-S71
14. Balagué F, Mannion AF, Pellisé F, Cedraschi C, Non-specific low back pain: Lancet, 2012; 379(9814); 482-91
15. Patel ND, Broderick DF, Burns J, ACR Appropriateness criteria low back pain: J Am Coll Radiol, 2016; 13(9); 1069-78
16. Remotti E, Nduaguba C, Woolley PA, Review: Discogenic back pain: Update on treatment: Orthop Rev (Pavia), 2023; 15; 84649
17. Downie A, Williams CM, Henschke N, Red flags to screen for malignancy and fracture in patients with low back pain: Systematic review: BMJ, 2013; 347; f7095
18. Chou R, Qaseem A, Owens DK, Shekelle PClinical Guidelines Committee of the American College of Physicians, Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians: Ann Intern Med, 2011; 154(3); 181-89
19. Peharec S, Jerković R, Funkcionalna procjena u pacijenata s nespecifičnom križoboljom: Medicina Fluminensis Mar 3, 2014; 50(1); 67-73 [in Croatian]
20. Casiano VE, Sarwan G, Dydyk AM, Varacallo M, Back pain: StatPearls [Internet], 2024, Treasure Island (FL), StatPearls Publishing
21. Haile G, Hailemariam TT, Haile TG, Effectiveness of ultrasound therapy on the management of chronic non-specific low back pain: A systematic review: J Pain Res, 2021; 14; 1251-57
22. Rahyussalim AJ, Zufar MLL, Kurniawati T, Significance of the association between disc degeneration changes on imaging and low back pain: A review article: Asian Spine J, 2020; 14(2); 245-57
23. Wang Z, Sato K, Nawrin SS, Low back pain exacerbation is predictable through motif identification in center of pressure time series recorded during dynamic sitting: Front Physiol, 2021; 12; 696077
24. Mattiuzzi C, Lippi G, Bovo C, Current epidemiology of low back pain: J Hosp Manag Health Policy, 2020; 4; 15
25. Hayden JA, Ellis J, Ogilvie R, Exercise therapy for chronic low back pain: Cochrane Database Syst Rev, 2021; 9(9); CD009790
26. Oliveira CB, Maher CG, Pinto RZ, Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview: Eur Spine J, 2018; 27(11); 2791-803
27. Associação Brasileira de Medicina Física e Reabilitação, Chronic nonspecific low back pain: rehabilitation: Rev Assoc Med Bras (1992), 2013; 59(6); 536-53
28. Krismer M, van Tulder M, Low back pain (non-specific): Best Pract Res Clin Rheumatol, 2007; 21(1); 77-91
29. Will JS, Bury DC, Miller JA, Mechanical low back pain: Am Fam Physician, 2018; 98(7); 421-28
30. Hartvigsen J, Hancock MJ, Kongsted A, What low back pain is and why we need to pay attention: Lancet, 2018; 391(10137); 2356-67
31. Trecarichi EM, Di Meco E, Mazzotta V, Fantoni M, Tuberculous spondylodiscitis: Epidemiology, clinical features, treatment, and outcome: Eur Rev Med Pharmacol Sci, 2012; 16(Suppl 2); 58-72
32. Rosedale R, Rastogi R, May S, Efficacy of exercise intervention as determined by the McKenzie System of Mechanical Diagnosis and Therapy for knee osteoarthritis: A randomized controlled trial: J Orthop Sports Phys Ther, 2014; 44(3); 173-81
33. Fairbank JC, Pynsent PB, The Oswestry Disability Index: Spine (Phila Pa 1976), 2000; 25(22); 2940-52 discussion 2952
34. Roland M, Fairbank J, The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire: Spine (Phila Pa 1976), 2000; 25(24); 3115-24
35. Davies CCNA, Psychometric properties of the Roland-Morris Disability Questionnaire compared to the Oswestry Disability Index: A systematic review: Physical Therapy Reviews, 2009; 14; 399-498
36. Hoy D, Brooks P, Blyth F, Buchbinder R, The Epidemiology of low back pain: Best Pract Res Clin Rheumatol, 2010; 24(6); 769-81
37. Hoy D, March L, Brooks P, The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study: Ann Rheum Dis, 2014; 73(6); 968-74
38. Urits I, Burshtein A, Sharma M, Low back pain, a comprehensive review: Pathophysiology, diagnosis, and treatment: Curr Pain Headache Rep, 2019; 23(3); 23
39. Járomi M, Kukla A, Szilágyi B, Back School programme for nurses has reduced low back pain levels: A randomised controlled trial: J Clin Nurs, 2018; 27(5–6); e895-e902
40. Kamali F, Panahi F, Ebrahimi S, Abbasi L, Comparison between massage and routine physical therapy in women with sub acute and chronic nonspecific low back pain: J Back Musculoskelet Rehabil, 2014; 27(4); 475-80
41. Waseem M, Karimi H, Gilani SA, Hassan D, Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population: J Back Musculoskelet Rehabil, 2019; 32(1); 149-54
42. Cimarras-Otal C, Marcen-Cinca N, Rabal-Pelay J, Adapted exercises versus general exercise recommendations on chronic low back pain in industrial workers: A randomized control pilot study: Work, 2020; 67(3); 733-40
43. Ozkaraoglu DK, Tarakci D, Algun ZC, Comparison of two different electrotherapy methods in low back pain treatment: J Back Musculoskelet Rehabil, 2020; 33(2); 193-99
44. Zdrodowska B, Leszczyńska-Filus M, Leszczyński R, Błaszczyk JComparison of the effect of laser and magnetic therapy for pain level and the range of motion of the spine of people with osteoarthritis lower back: Pol Merkur Lekarski, 2015; 38(223); 26-31 [in Polish]
45. Durmus D, Durmaz Y, Canturk F, Effects of therapeutic ultrasound and electrical stimulation program on pain, trunk muscle strength, disability, walking performance, quality of life, and depression in patients with low back pain: A randomized-controlled trial: Rheumatol Int, 2010; 30(7); 901-10
46. Hoy DG, Smith E, Cross M, Reflecting on the global burden of musculoskeletal conditions: Lessons learnt from the global burden of disease 2010 study and the next steps forward: Ann Rheum Dis, 2015; 74(1); 4-7
47. Henschke N, Maher CG, Refshauge KM, Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain: Arthritis Rheum, 2009; 60(10); 3072-80
48. Bergström C, Persson M, Mogren I, Pregnancy-related low back pain and pelvic girdle pain approximately 14 months after pregnancy – pain status, self-rated health and family situation: BMC Pregnancy Childbirth, 2014; 14; 48
49. Delitto A, George SZ, Van Dillen L, Low back pain: J Orthop Sports Phys Ther, 2012; 42(4); A1-57
50. Goldberg H, Firtch W, Tyburski M, Oral steroids for acute radiculopathy due to a herniated lumbar disk: A randomized clinical trial: JAMA, 2015; 313(19); 1915-23
51. Friedman BW, Dym AA, Davitt M, Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: A randomized clinical trial: JAMA, 2015; 314(15); 1572-80
52. Saragiotto BT, Machado GC, Ferreira ML, Paracetamol for low back pain: Cochrane Database Syst Rev, 2016; 2016(6); CD012230
53. Schousboe JT, Epidemiology of vertebral fractures: J Clin Densitom, 2016; 19(1); 8-22
Tables
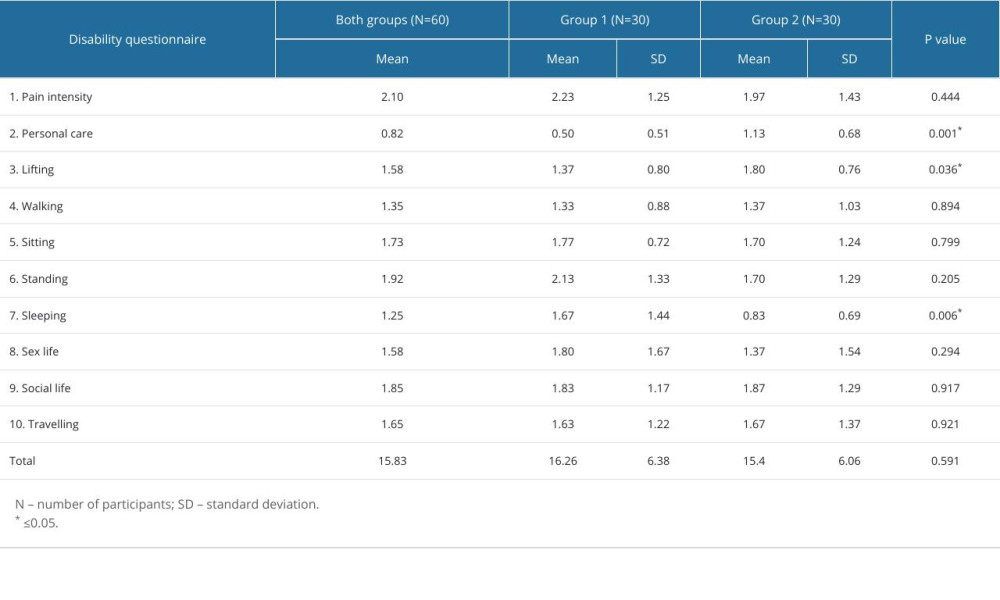 Table 1. Results obtained using the Oswestry Low Back Pain Disability Questionnaire (N=60).
Table 1. Results obtained using the Oswestry Low Back Pain Disability Questionnaire (N=60).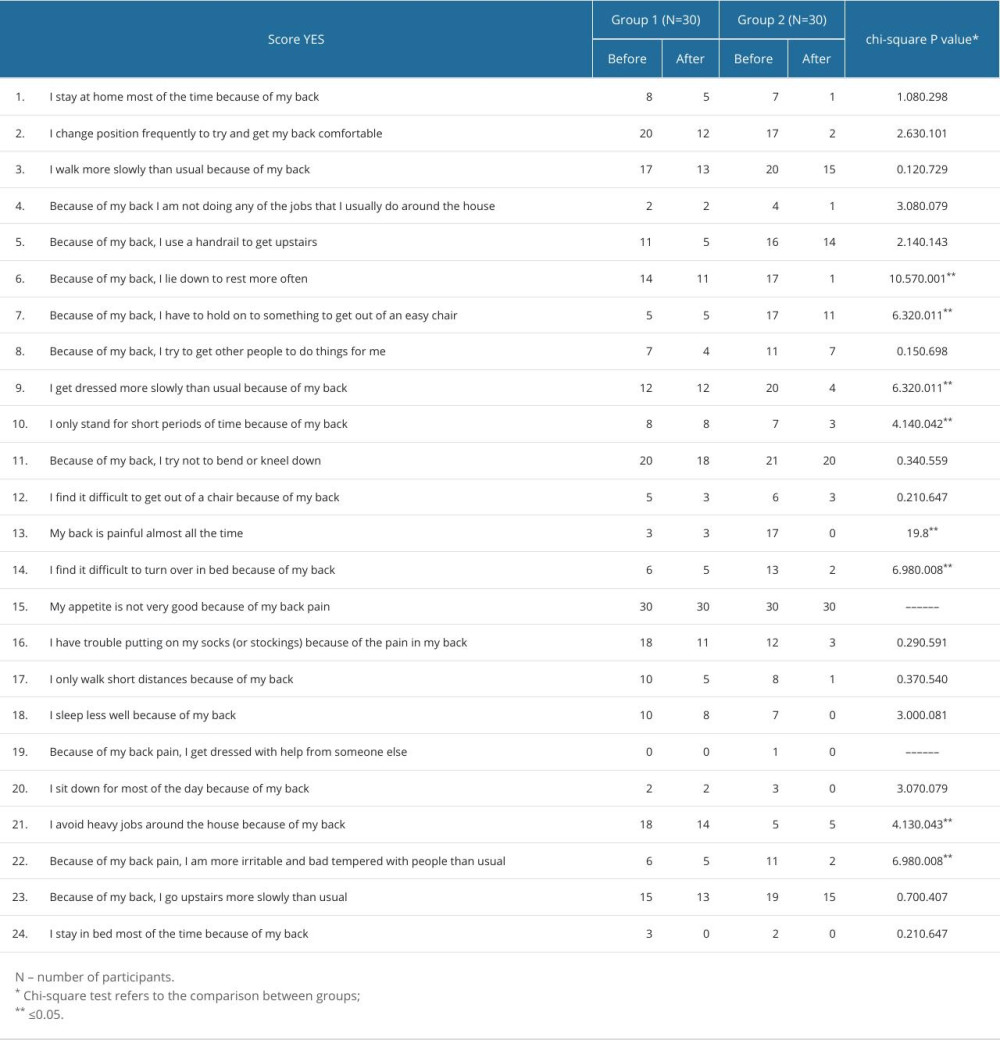 Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60).
Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60).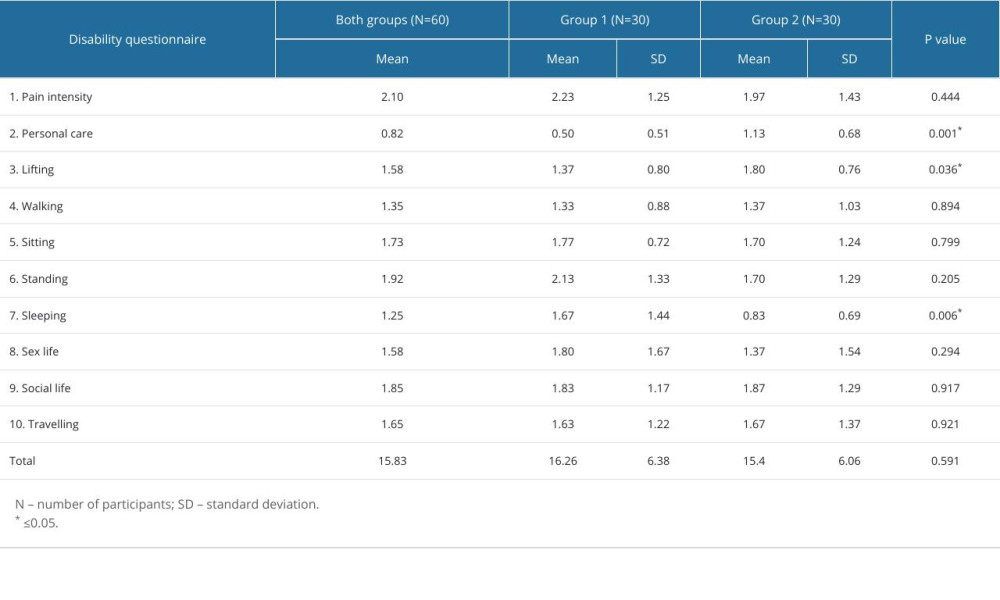 Table 1. Results obtained using the Oswestry Low Back Pain Disability Questionnaire (N=60).
Table 1. Results obtained using the Oswestry Low Back Pain Disability Questionnaire (N=60).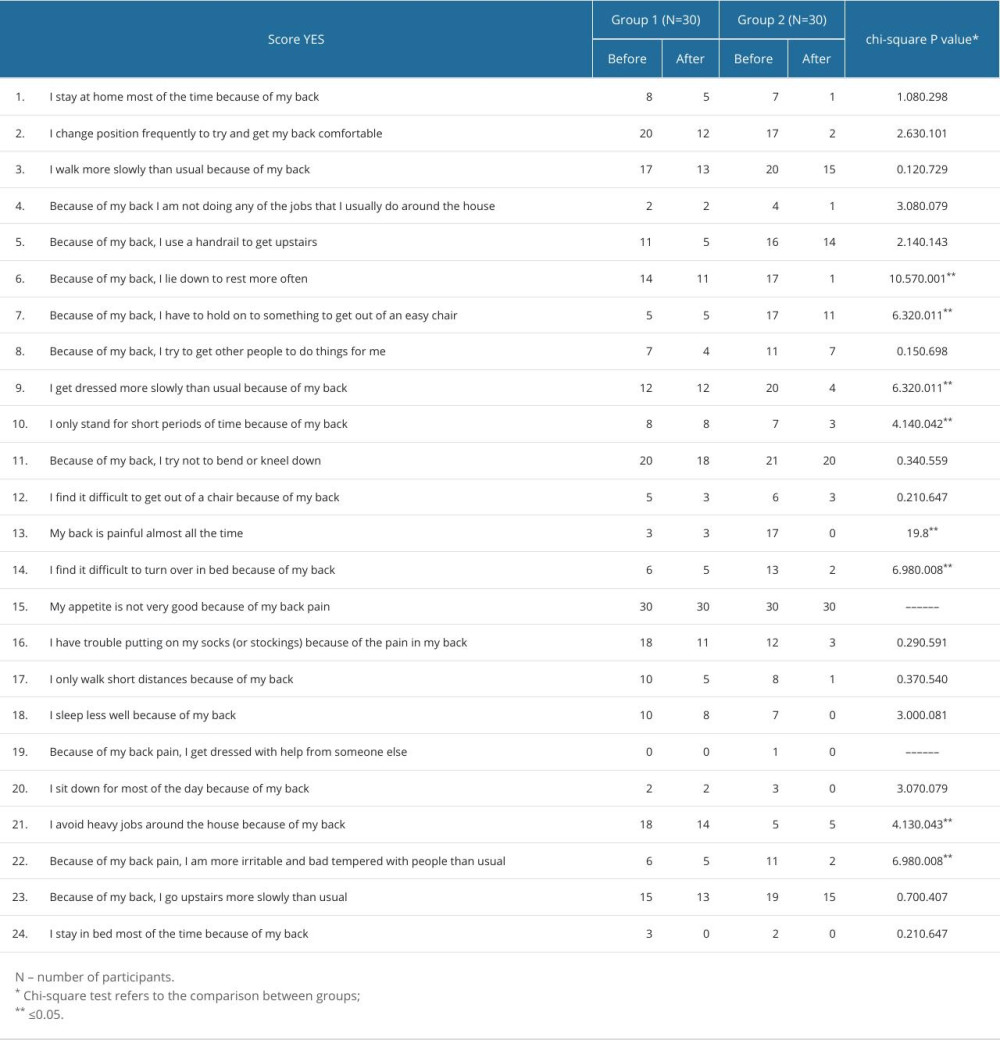 Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60).
Table 2. Results of the chi-square test on the Roland-Morris Disability Questionnaire before and after treatment. The frequency of marked answers was compared for each individual question between 2 group (N=60). In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952