29 March 2024: Clinical Research
Sexual Dysfunction in Women After Tibial Fracture: A Retrospective Comparative Study
Müjdat Adaş1ABCDEF*, Murat Çakar1ABCD, Serhat Gürbüz2ABDF, Niyazi İğde2DEF, Ahmet KeskinDOI: 10.12659/MSM.944136
Med Sci Monit 2024; 30:e944136
Abstract
BACKGROUND: Tibial fractures, common in adults, are often treated with external or internal fixation methods. While effective, external fixation (EF) can lead to sexual dysfunction (SD), especially in young patients. This study aimed to assess SD in women undergoing EF versus internal fixation for tibial fractures.
MATERIAL AND METHODS: Sexual function and frequency of monthly sexual intercourse (SI) were evaluated using the Female Sexual Function Index (FSFI) before surgery, with the fixator, after at least 6 months following fixator removal in EF group, and after achieving bone union for at least 3 months in the IF group.
RESULTS: The EF group consisted of 107 (mean age 28.5 years; 19-40 years) and IF group consisted of 106 patients (mean age 32.1 years; 18-40 years). The duration of EF was an average of 4.7 months (range, 2.5-13 months). FSFI scores were significantly lower in the EF group compared to the IF group (9.33 versus 27.3, P<0.001). Also, there was no significant difference between the FSFI scores before EF and after EF was removed (34.22 versus 33.8, P=0.413). FSFI sub-group scores such as desire, arousal, lubrication, and orgasm were significantly lower in the EF group (P<0.001). The monthly average frequency of SI before surgery and after the removal of EF was 10.2 and 9.1, respectively, while this frequency was 2.56 when EF was present (P<0.001).
CONCLUSIONS: The quality and frequency of SI in women significantly deteriorate and decrease during the period of extremity fixation following tibial diaphyseal fractures treated with EF, but return to normal after removal.
Keywords: Fracture Fixation, Fracture Fixation, Internal, Sex, Sexual Dysfunction, Physiological, Tibia
Introduction
Tibial diaphyseal fractures are the most common long-bone fractures in adults (36.7%); they comprise 15% of all adult fractures and are often associated with high-energy injuries involving significant soft-tissue damage [1]. The subcutaneous structure of the tibia makes it more susceptible to open wounds. The current treatment option is operative, and intramedullary nailing (IMN) is often the preferred fixation method [2,3]. On the other hand, external fixation (EF) is beneficial in cases of significant swelling or extensive soft-tissue damage and is employed as a temporary surgical measure until it can be converted to internal fixation [4]. In these cases, either a monolateral external fixator (MEF) or a circular external fixator (CEF) is used [5]. External fixation (EF) can sometimes remain on the patient until the fracture has completely healed, either temporarily or permanently [6].
Although EFs can perform very well in managing fractures, they can have negative physical and psychological effects on patients and can significantly reduce the quality of life (QoL), especially in young patients. Among the functional disorders associated with EF, sexual dysfunction (SD) is a potential problem [7,8]. According to Marita P. McCabe, sexual dysfunction is defined as the impairment or unwanted alteration of an individual’s ability to successfully engage in sexual activity. This impairment or alteration can manifest in various forms, such as decreased sexual desire, arousal difficulties, orgasm problems, or painful sexual intercourse [9]. Given that tibial fractures are more common in young people as a result of traffic accidents, SDs can be a serious but overlooked complication of tibial fractures treated with EF. Sexual health, as defined by the World Health Organization, is a state of holistic well-being that encompasses the physical, emotional, mental, and social aspects of sexuality and is considered an important factor in maintaining the general QoL in adults [7,8]. SD refers to difficulties that cause distress and disruption in interpersonal relationships and prevent an individual from being satisfied with sexual activity [10]. Female sexual dysfunction (FSD) includes a number of overlapping sexual disorders with multiple causes within the biopsychosocial model and covers conditions related to desire/libido, arousal, pain/discomfort, and inhibition of orgasm [11,12]. Since the definition and diagnostic criteria for SD are still controversial and under development, estimating the prevalence of SD is relatively difficult. However, SD has been reported in 10–52% of men and 25–63% of women worldwide [13,14]. Even in sexually active young patients, post-traumatic SDs are often overlooked, leading to depression and a decrease in QoL [15]. In their study, Schulman et al demonstrated that although dyspareunia and anorgasmia are the main causes of sexual dysfunction in women after pelvic trauma, sexual dysfunction remains very high in the first weeks after fracture treatment following non-pelvic trauma [16]. They also reported that the energy of the injury mechanism is related to the severity of sexual dysfunction. Pain and soft-tissue injuries due to fractures impede mobility and restrict patients’ ability to assume positions necessary for sexual activity. In addition to these physiological limitations, they emphasized that psychological effects such as stress and anxiety after long-bone fractures may also reduce libido and performance. However, the effects of the method of fracture treatment and the implant used on an individual’s sexual life are often overlooked by orthopedists, who focus on fracture healing. This awareness is somewhat higher in surgeries close to the genital area, and studies have been published on the effects on the sexual functions of women and men after surgeries such as lumbar stenosis, pelvic fractures, and hip arthroplasties [17–22].
While changes in sexual life after EF treatment in men have been investigated, the effects in women are unknown [14]. Therefore, this retrospective study aimed to compare sexual dysfunction associated with external and internal fixation of traumatic diaphyseal tibial fracture in women using the 19-item Female Sexual Function Index (FSFI).
Material and Methods
STUDY SETTINGS AND DESIGN:
This retrospective comparative study was approved by the IRB. Ethics approval was obtained (EC approval no: 103-20/11/2023) and informed consent was obtained from the participants. A retrospective review of the digital patient database from the authors’ institution was conducted to identify adult female patients who had undergone EF or IF for tibial body fractures between July 2015 and December 2022.
This retrospective research used prospectively collected data of the patients. Retrospective information about the periods before and after surgery was obtained through face-to-face interviews with the patients at the very last follow-up. All interviews were conducted face-to-face in a hospital environment by the same interviewer (MA) to prevent observer bias.
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria were women aged 18–40 years who had tibial body fractures treated surgically who had undergone EF removal, and had at least 6 months passed afterwards or at least 3 months passed after bony union in the IF group, and who are sexually active with a regular sex life. The exclusion criteria were nonunion or prolonged healing, any additional organ or other bone fractures (except ipsilateral fibula fracture) at the time of injury, pregnancy or breastfeeding at the time of injury, malignancy, psychological disorders (depression, schizophrenia, and paranoid disorder based on medical diagnosis), any systemic diseases, did not want to participate, or with incomplete data.
INSTITUTIONAL DATABASE, DATA COLLECTION, AND PATIENTS’ SETTING:
Personal and demographic data, including age at the time of trauma, educational status (elementary, high, or university), and smoking, were collected from all patients participating in the study. Hospital records were reviewed to determine the cause of trauma, the presence of associated acute injuries, and the form of treatment.
EVALUATION OF SEXUAL DYSFUNCTION:
The Female Sexual Function Index (FSFI) questionnaire was used to evaluate FSD. FSFI is a 19-item self-report tool that analyzes 6 areas of sexual function in women, including desire, arousal, lubrication, orgasm, satisfaction, and pain [23]. The items in FSFI are calculated according to a 5-point Likert scale, and each question is scored from 0 or 1 to 5 [23]. A zero score indicates no sexual activity for 1 month. The total overall score ranges from 2 to 36, with a score below 26.55 considered as FSD, and the lower the score, the more severe the degree of SD [24]. The total FSFI scores and FSFI sub-group scores related to desire, arousal, lubrication, orgasm, satisfaction, and pain were evaluated in patients during the use of EF. The relationship between the development of SD with the use of EF and the type of fixator used with sexual functions was also examined. These scores were made for 2 separate periods: while EF was present and after EF was removed. Patients who developed SD were asked whether they sought help from a psychologist, gynecologist, or urologist during this period. Additionally, they were questioned about the characteristics, causes, and monthly number of episodes of sexual intercourses pertaining to the sexual problems they encountered during the presence of EF. The IF group was a control group for the study, and FSFI scores were calculated. The IF group consisted of patients treated with IF who met the same study inclusion criteria.
STATISTICAL ANALYSES:
Statistical analyses were performed using SPSS version 25.0 software. Descriptive statistics, including mean, standard deviation, median, and interquartile range (IQR), were used to present the data. Histogram graphs and the Kolmogorov-Smirnov test were used to check the normality of the data for quantitative variables. The independent group
Results
DEMOGRAPHIC DATA:
The demographic characteristics of the patients are shown in Table 1. File scanning revealed a total of 319 patients treated with EF (n=141) or IF (n=178) during this 7-year period. There were 141 female patients treated with EF, and 137 of them with timely bony union achieved completed the questionnaire. Of them, 7 patients could not be reached, 12 patients declined to participate in the study, 5 patients did not come to the interview, and 6 patients were excluded from the study due to systemic disease. Finally, a total of 213 patients were included in the study; 106 of them were treated by EF, with a mean age of 28.5 years (range, 19–40 years). Of these fractures, 71 (66%) were open, and 36 (34%) were closed. Conversely, 106 patients treated with IF during the same period were included as controls, with an average age of 32.1 years (range, 18–40 years). In the IF group, 11 could not be reached, 23 declined to participate, 9 did not come to the interview, 3 had incomplete data, 5 experienced union problems, and 21 patients were excluded from the study due to systemic disease. There was no significant difference in terms of age and smoking between patients with EF and those with IF (P=0.212 and P=0.134, respectively). The educational level of both groups was similar (P=0.427). There was no accompanying disease or other fracture in any patients.
The mean duration of EF retention was 4.7 months (range: 2.5–13 months), and sexual life assessment in this group of patients was performed at a mean of 7.5 months (range: 6–13 months) after fixator removal. Similarly, sexual life assessments of patients in the IF group were conducted at an average of 4.1 months (range: 2.2–7 months) after full bony consolidation
INJURY CHARACTERISTICS AND TREATMENT:
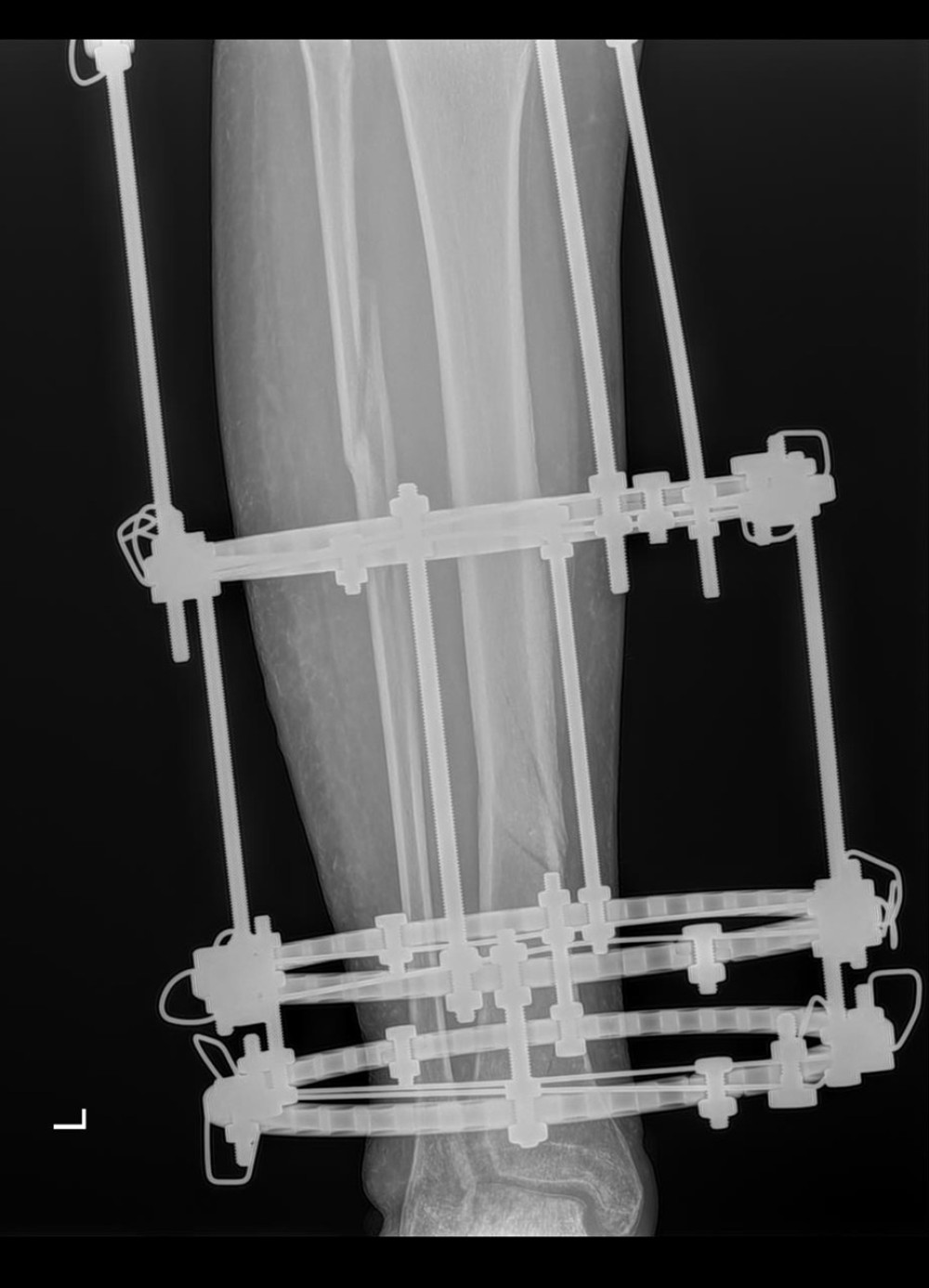
The causes of injury included 31 motorcycle accidents (29%), 28 automobile accidents (26%), 26 gunshot injuries (24%), 12 work accidents (11%), and 11 falls (10%). In 82 patients (77%), there was only a tibia fracture, while in 25 patients (23%) there was an accompanying fibula fracture. In contrast, 59 fractures (55%) were treated with CEF and 48 fractures (45%) were treated with MEF (Figures 1, 2). In the IF group, the causes of injury included 50 falls (47%), 24 (23%) traffic accidents, 13 (12%) gunshot injuries, 11 (10%) motorcycle accidents, and 8 (17%) work accidents. Of these patients, 75 patients were treated with IMN and 31 patients were treated with plate (Figures 3, 4).
RESULTS OF FSFI AND SD:
FSFI scores were significantly lower in the EF group compared to the IF group (9.33 versus 27.3, P<0.001). Also, there was no significant difference between the FSFI scores before EF and after EF was removed (34.,22 versus 33.8, P=0.413). FSFI sub-group scores regarding desire, arousal, lubrication, orgasm, satisfaction, and pain in the EF group were significantly lower than those in the IF group (P<0.001). The total average FSFI scores and FSFI sub-group scores are presented in Table 2. The FSFI scores in the CEF group were lower compared to the FSFI scores in the MEF group (9.22 versus 12.20, P<0.001) (Table 3). The decreases in FSFI scores were associated with the physical (77%) and psychological (23%) consequences of trauma.
There was also a noticeable decrease in the frequency of monthly sexual intercourse. The monthly average frequency of sexual intercourse before surgery and after the removal of EF was 10.2 and 9.1, respectively, while this frequency was 2.56 when EF was present (P<0.001). All patients who experienced sexual problems reported having multiple problems during sexual intercourse. The main problems were difficulty with whole-body bathing, difficulty in positioning, fear of harming the partner or the fracture, and discomfort with the possibility of EF tearing the sheet (Table 4). All patients who participated in the study answered all the questions in the survey. Some participants have indicated multiple reasons. No patient reported the need for support from any psychiatrist, psychologist, or urologist regarding SD. No permanent SD was detected in any patient who had problems with EF after the removal of EF.
Discussion
Sexual health, which is a crucial component of overall quality of life in adults and encompasses all aspects of sexuality, including physical, emotional, mental, and social dimensions, can be disrupted following long-bone fractures due to both the traumatic impact and the nature and duration of the treatment. This study is the first to establish a correlation between the high prevalence of sexual dysfunction (SD) in women with diaphyseal tibial fractures treated with EF by evaluating the FSFI. The most significant finding of this study is the presence of a statistically significant relationship between the frequency and severity of SDs and the decrease in quality of life in patients with diaphyseal tibial fractures treated with EF. FSFI sub-group scores such as desire, arousal, lubrication, and orgasm were significantly lower in the EF group. The monthly average frequency of sexual intercourse was significantly lower while EF was present.
Healthy sexual life and sexual satisfaction are important factors in improving the quality of life in adults [8]. It is well known that a healthy sexual life also improves women’s quality of life [25]. Biological, psychological, and sociocultural elements play a significant role in individuals maintaining a healthy sexual life. However, even in sexually active young patients, SDs are often overlooked, leading to depression and a decrease in quality of life [15].
The etiology of SD in patients who have experienced trauma is multifactorial. It is associated not only with the physical effects of the fracture but also with the form of surgical treatment and the psychological sequelae due to trauma. In recent years, various studies have been conducted on the effects, causes, and consequences of trauma and fracture formation on the sexual lives of female patients [17,18,26–28].
In the literature, SD has been reported in 43.6% of patients admitted to intensive care after general trauma and in 38–65% of women with pelvic fractures [17,29].
The EF used in the treatment of tibial fractures is a device that negatively physically, psychologically, and socially affects sexually active individuals. Functional disorders associated with EF include SD, a problem that arises with both physical and psychosocial factors. Because tibial fractures are more common in young people as a result of traffic accidents, SDs appear as short-term serious complications of tibial fractures treated with EF.
In this study, we investigated their sexual functions, which are unfortunately not given enough importance even though they significantly affect the quality of life of women during fracture treatment. In our study, all patients experienced varying degrees of SD, most of which were severe. The prevalence and severity of SD were strikingly high, especially the 92% decreased interest in intercourse. In those who had sexual intercourse, the rate of dyspareunia was 78%, while the rate of orgasmic dysfunction was 90%, and the rate of intercourse satisfaction was 10%. These results are consistent with the results of patients who developed SD after pelvic trauma. Based on this study, we believe that EF negatively affects sexual life and quality of life. Therefore, except for absolute indications, IF should be preferred instead of EF. If EF is necessary for absolute indications, it should be replaced with the IF method as soon as possible. This will help improve couples’ sexual and emotional relationships and increase quality of life.
This study inevitably had certain limitations. First, it had a retrospective design and SD evaluations were made with subjective self-reports, especially in a way that would provoke consideration of recall bias. A more accurate and reliable result could be achieved with objective criteria. Another important limitation of the study is that psychiatric examinations of the participants were not performed, although sexual life is highly affected by psychological state. However, none of the subjects had any psychiatric disorder and they were not receiving any psychiatric treatment. Finally, another limitation that needs to be addressed is the absence of age- and sex-matched analysis and the lack of adjusted statistical analysis for comorbidities that could cause sexual dysfunction. Due to the design of the study, these unavoidable limitations suggest that future prospective randomized studies may provide better results.
Conclusions
SD is a clinically significant and unnoticed problem in adult female patients treated with EF and we need to examine not only physical but also psychological and sexual problems during fracture treatment. Prospective randomized controlled studies will provide a more detailed understanding of these cases.
References
1. Mangukiya HJ, Mahajan NP, Pawar ED, Functional and radiological outcome in management of compound tibia diaphyseal fracture with AO monolateral fixator versus Limb reconstruction system: J Orthop, 2018; 15(1); 275-81
2. Bucholz RW, Heckman JD, Court-Brown CM: Rockwood and Green’s fractures in adults, 2006, Lippincott Williams & Wilkins http://catdir.loc.gov/catdir/toc/ecip061/2005028856.html
3. Adesina SA, Eyasan SU, Amole IO, Closed reduction and locked intramedullary nailing of diaphyseal long bone fractures without intra-operative imaging and fracture table: Int Orthop, 2022; 46(1); 51-59
4. Kazley J, Jahangir A, Tibia diaphyseal fracture: StatPearls, 2024, StatPearls Publishing http://www.ncbi.nlm.nih.gov/books/NBK537173/
5. Hao ZC, Xia Y, Xia DM, Treatment of open tibial diaphyseal fractures by external fixation combined with limited internal fixation versus simple external fixation: A retrospective cohort study: BMC Musculoskelet Disord, 2019; 20(1); 311
6. Tekin AÇ, Saygılı MS, Adaş M, Outcome of type 3 open tibial diaphyseal fractures managed with a limb reconstruction system: Analysis of a 49-patient cohort: Med Princ Pract, 2016; 25(3); 270-75
7. Edwards WM, Coleman E, Defining sexual health: A descriptive overview: Arch Sex Behav, 2004; 33(3); 189-95
8. Flynn KE, Lin L, Bruner DW, Sexual satisfaction and the importance of sexual health to quality of life throughout the life course of U.S. adults: J Sex Med, 2016; 13(11); 1642-50
9. McCabe MP, Sharlip ID, Atalla E, Definitions of sexual dysfunctions in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015: J Sex Med, 2016; 13(2); 135-43
10. Basson R, Berman J, Burnett A, Report of the international consensus development conference on female sexual dysfunction: Definitions and classifications: J Urol, 2000; 163(3); 888-93
11. Hatzimouratidis K, Hatzichristou D, Sexual dysfunctions: classifications and definitions: J Sex Med, 2007; 4(1); 241-50
12. Pluchino N, Carmignani A, Cubeddu A, Androgen therapy in women: For whom and when: Arch Gynecol Obstet, 2013; 288(4); 731-37
13. Laumann EO, Nicolosi A, Glasser DB, Sexual problems among women and men aged 40–80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors: Int J Impot Res, 2005; 17(1); 39-57
14. Adaş M, Tekin AÇ, Bayraktar MK, Effects of the lower extremity external fixators on the sexual life of males: Acta Orthop Traumatol Turc, 2016; 50(1); 76-81
15. Rovere G, Smakaj A, Perna A, Correlation between traumatic pelvic ring injuries and sexual dysfunctions: A multicentric retrospective study: Int Orthop, 2023; 47(6); 1407-14
16. Shulman BS, Taormina DP, Patsalos-Fox B, Sexual function is impaired after common orthopaedic nonpelvic trauma: J Orthop Trauma, 2015; 29(12); e487-92
17. Walton AB, Leinwand GZ, Raheem O, Female sexual dysfunction after pelvic fracture: A comprehensive review of the literature: J Sex Med, 2021; 18(3); 467-73
18. Gambrah HA, Hagedorn JC, Dmochowski RR, Johnsen NV, Sexual dysfunction in women after traumatic pelvic fracture negatively affects quality of life and mental health: J Sex Med, 2022; 19(12); 1759-65
19. Johnsen NV, Cohn E, Johnson T, Sexual dysfunction following traumatic pelvic fracture: J Trauma Acute Care Surg, 2021; 90(3); 550-56
20. Issa K, Pierce TP, Brothers A, Sexual activity after total hip arthroplasty: A systematic review of the outcomes: J Arthroplasty, 2017; 32(1); 336-40
21. Neonakis EM, Perna F, Traina F, Total hip arthroplasty and sexual activity: A systematic review: Musculoskelet Surg, 2020; 104(1); 17-24
22. Sobański D, Staszkiewicz R, Gadzieliński M, A study of 179 patients with degenerative stenosis of the lumbosacral spine to evaluate differences in quality of life and disability outcomes at 12 months, between conservative treatment and surgical decompression: Med Sci Monit, 2023; 29; e940213
23. Rosen R, Brown C, Heiman J, The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function: J Sex Marital Ther, 2000; 26(2); 191-208
24. Wiegel M, Meston C, Rosen R, The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores: J Sex Marital Ther, 2005; 31(1); 1-20
25. Dunn KM, Croft PR, Hackett GI, Association of sexual problems with social, psychological, and physical problems in men and women: A cross sectional population survey: J Epidemiol Community Health, 1999; 53(3); 144-48
26. Duramaz A, Ilter MH, Yıldız Ş, The relationship between injury mechanism and sexual dysfunction in surgically treated pelvic fractures: Eur J Trauma Emerg Surg, 2020; 46(4); 807-16
27. Li P, Zhou D, Fu B, Management and outcome of pelvic fracture associated with vaginal injuries: A retrospective study of 25 cases: BMC Musculoskelet Disord, 2019; 20(1); 466
28. Alexander MS, Aisen CM, Alexander SM, Aisen ML, Sexual concerns after Spinal Cord Injury: An update on management: NeuroRehabilitation, 2017; 41(2); 343-57
29. Ulvik A, Kvåle R, Wentzel-Larsen T, Flaatten H, Sexual function in ICU survivors more than 3 years after major trauma: Intensive Care Med, 2008; 34(3); 447-53
Figures
Tables
 Table 1. Demographic characteristics.
Table 1. Demographic characteristics.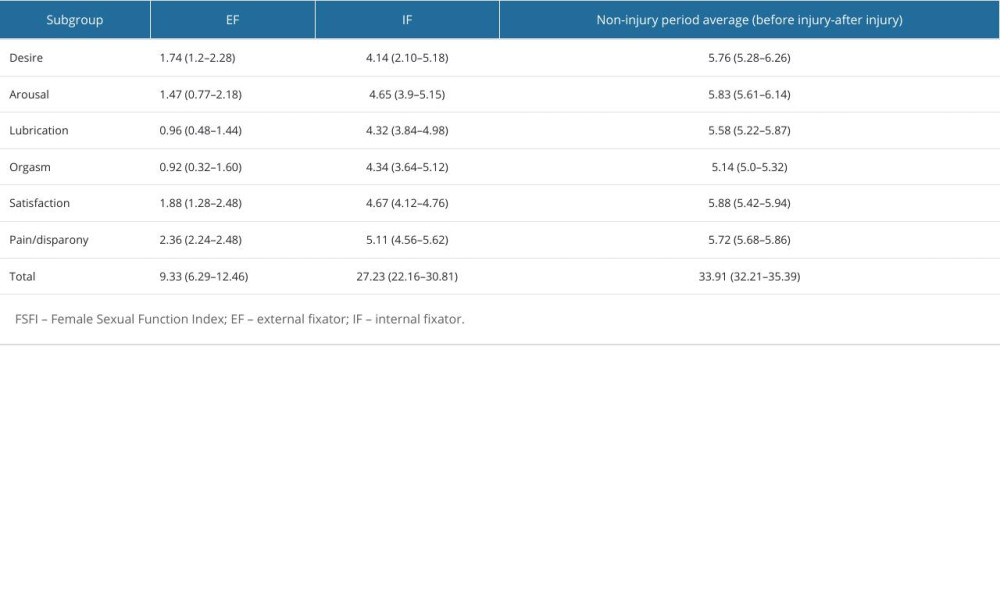 Table 2. Total average FSFI scores.
Table 2. Total average FSFI scores.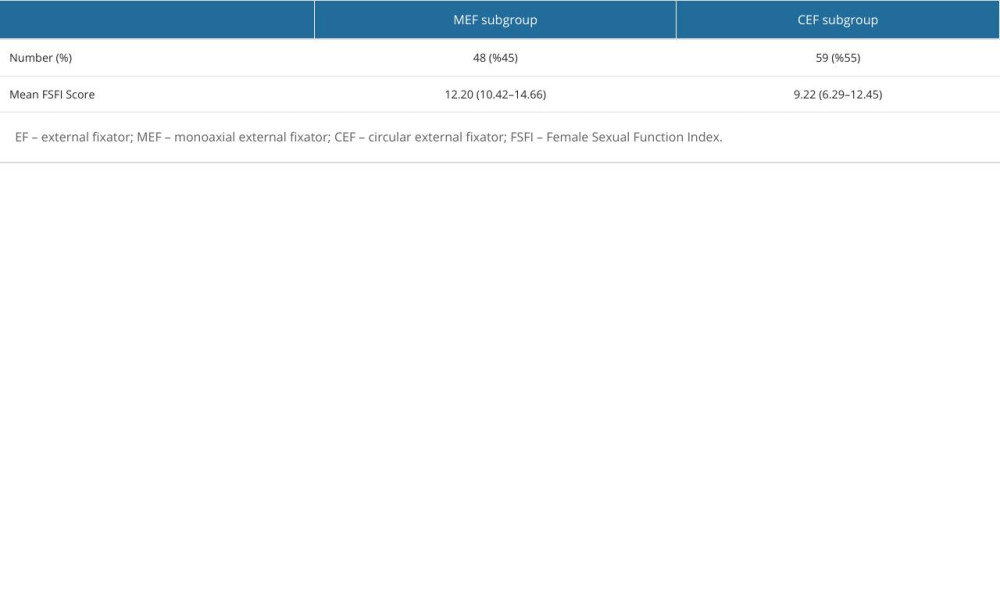 Table 3. EF subgroups and FSFI scores.
Table 3. EF subgroups and FSFI scores.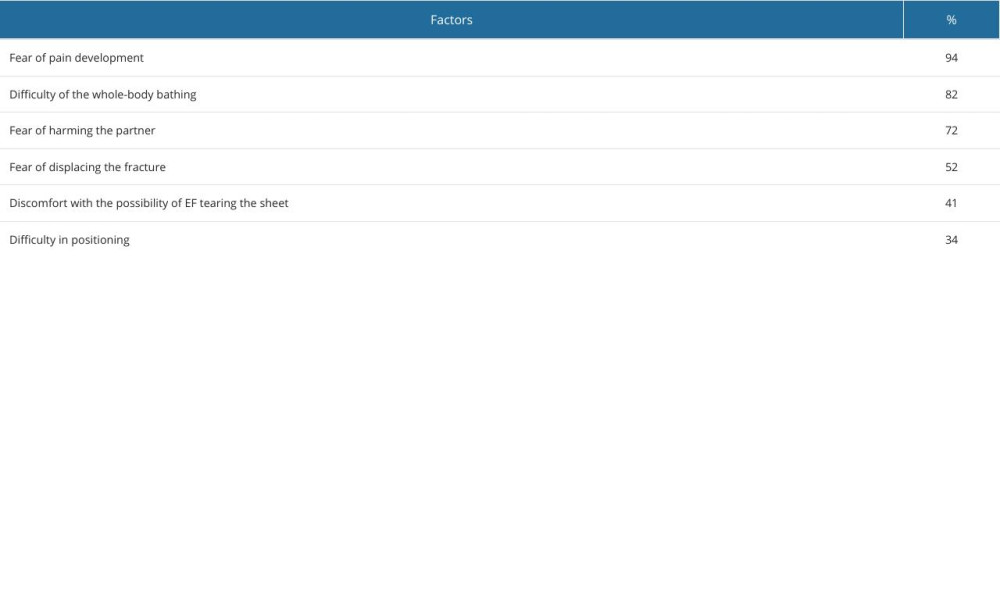 Table 4. Factors contributing to the decrease in monthly frequency of sexual intercourse (participants indicated multiple reasons).
Table 4. Factors contributing to the decrease in monthly frequency of sexual intercourse (participants indicated multiple reasons). Table 1. Demographic characteristics.
Table 1. Demographic characteristics.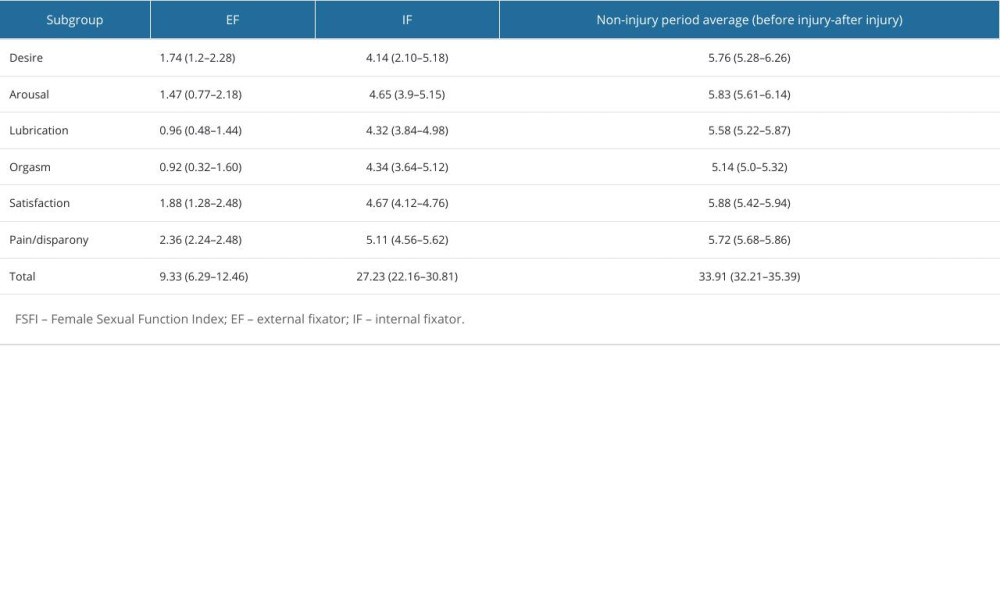 Table 2. Total average FSFI scores.
Table 2. Total average FSFI scores.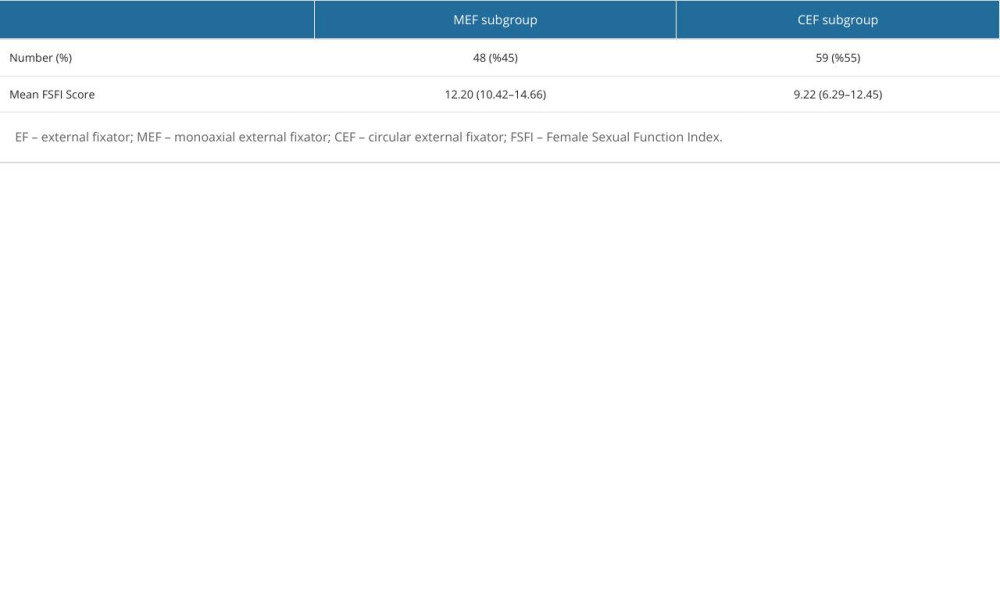 Table 3. EF subgroups and FSFI scores.
Table 3. EF subgroups and FSFI scores.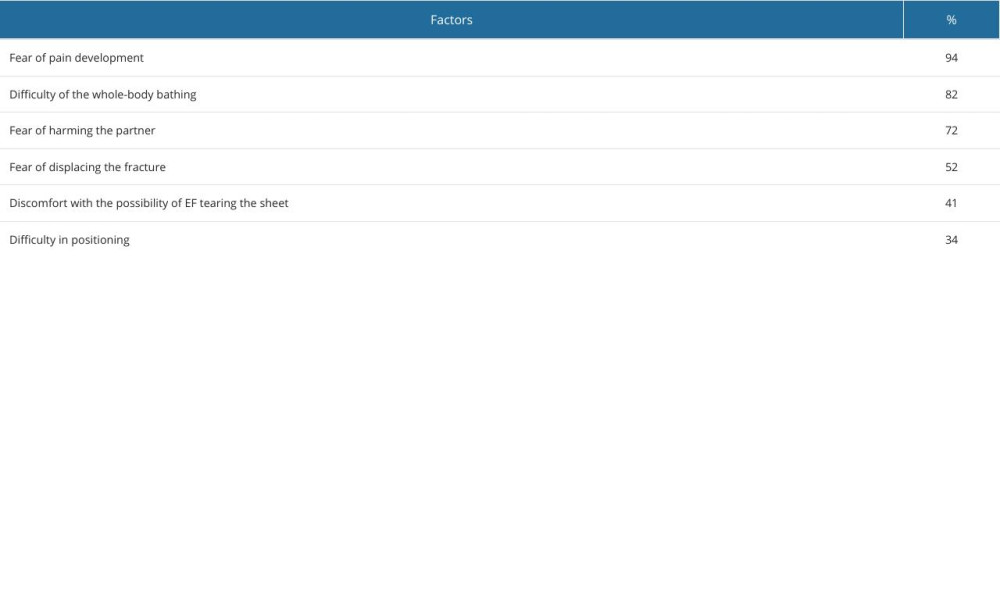 Table 4. Factors contributing to the decrease in monthly frequency of sexual intercourse (participants indicated multiple reasons).
Table 4. Factors contributing to the decrease in monthly frequency of sexual intercourse (participants indicated multiple reasons). In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952