18 June 2024: Clinical Research
Improving Function and Quality of Life in Patients with Chronic Neck Pain, Tension-Type Headache, and Forward Head Posture: The Role of Eyeball Exercise and Cervical Stabilization Programs
Sam-Ho ParkDOI: 10.12659/MSM.944315
Med Sci Monit 2024; 30:e944315
Abstract
BACKGROUND: The purpose of this study was to investigate the effects of eyeball exercise and cervical stabilization programs to patients with chronic neck pain, tension-type headache (TTH), and forward head posture (FHP).
MATERIAL AND METHODS: The design of this study was a randomized controlled trial. A total of 40 participants were randomly divided into 2 groups: the experimental group (n=20) and the control group (n=20). Both groups received cervical manual therapy and biofeedback-guided stabilization exercises (30 min/session, 3 sessions/week, 6 weeks). In addition to the regular treatments, the participants in the experimental group also performed eyeball exercises for 20 minutes per session, 3 sessions per week, for a total of 6 weeks. Changes in neck pain (numeric rating scale, NRS), neck disability index (NDI), quality of life (Short Form-12 Health Survey Questionnaire, SF-12), headache impact test-6 (HIT-6), craniovertebral angle (CVA), cranial rotation angle (CRA), and muscle tone were measured.
RESULTS: Both groups showed significant improvements in NRS, NDI, SF-12, HIT-6 scores, CVA, CRA, and muscle tone (p<0.05). The experimental group had significant differences in NDI, SF-12, HIT-6 scores, and suboccipital muscle tone compared to the control (p<0.05).
CONCLUSIONS: Combining the eyeball exercise program with commonly used manual therapy and stabilization exercises for patients with chronic neck pain can help reduce nerve compression and promote muscle relaxation in the eye and neck areas. The method is thus proposed as an effective intervention to enhance function and quality of life in patients with chronic neck pain patients, TTH, and FHP.
Keywords: Eye Movements, Muscle Tonus, Neck Pain, Tension-Type Headache
Introduction
In the International Classification of Headache Disorders 3rd edition, tension-type headache (TTH) is very common, with a lifetime prevalence in the general population ranging in different studies of between 30% and 78% [1]. The causes of TTH include excessive muscle activity due to stress, nerve root compression due to structural anomaly of the cervical vertebra(e), and muscle imbalance due to improper posture [2]. Additionally, TTH may be further aggravated by excessively increased activity of the neck, head, and periocular muscles, causing a sensation of pressure in the head and periocular muscles and persistent pain accompanied by neck discomfort [3].
The control of muscles in the cervical vertebral area requires integrated movements of the key sensory organs of visual, auditory, and balance functions and the stability of head and neck movements [4]. In neuroanatomical terms, muscle pain in the cervical region is caused by the first and second cervical nerves of the trigeminocervical complex (TCC). At such nerve endings, the fusion with the periocular nerve terminal leads to headache and pain in the periocular muscles [4]. To alleviate TTH, drugs or electrostimulation treatments are used in clinical practice. These treatments, however, only address the alleviation of pain, and it is difficult to suggest a fundamental solution [5]. The muscle activities in the cervical vertebral area affect eyeball movement and in the case of TTH, the muscle tone of the orbicularis oculi in the periocular region continuously increases. Therefore, a method to reduce TTH is to reduce the tonicity of the orbicularis oculi through eyeball movement in addition to reducing muscle tone in the cervical region via manual therapy, which has gained increasing attention [6–8].
Forward head posture (FHP), a muscle abnormality caused by poor posture and physical loading due to changes in cervical curvature, can result from abnormal control of muscles in the cervical region. Craniovertebral angle (CVA) is an objective indicator of FHP [9]. As the angle between the horizontal line and the line connecting the C7 vertebra and the tragus at the head, CVA decreases as the severity of FHP increases; CVA ≤53° is a criterion that classifies FHP [9]. Among the muscles associated with headache caused by FHP are suboccipital, upper trapezius, and longus colli muscles. The suboccipital and upper trapezius muscles are involved in cranial rotation, postural control, and head stability and shortening of these muscles is closely correlated with FHP. Hence, persistent FHP leads to headache as well as neck pain [10]. Additionally, the longus colli muscle is an intrinsic muscle with a role in stability and neutral position of the neck, which should be considered when employing strengthening exercises [10]. To alleviate TTH, the suboccipital and upper trapezius muscles as the main muscles affecting FHP should be relaxed, and the longus colli muscle should be strengthened, for which a stabilization exercise is required; thus, neck pain and headache as well as postural imbalance can be reduced [11].
Muscle fatigue results from excessive tension-type in the neck and shoulder muscles caused by improper posture such as FHP. As this leads to TTH with neck pain, a vicious cycle is created [12]. Among the muscles that are associated with TTH, the suboccipital muscle is where the laryngeal nerve and the TCC are found with potential effects on the periocular region. Thus, excessive muscle tension due to improper posture can lead to nerve compression, causing muscle pain in the periocular region [13]. Furthermore, abnormal function of the upper trapezius muscle can cause FHP and increase neck pain, which induces neurological symptoms and causes TTH [13].
TTH has been reported to be closely correlated with patients’ physical health conditions such as improper posture and mental health problems such as depression and anxiety [10]. Consequently, the estimation of a patient’s quality of life is an important factor that should be assessed via objective quantification. To assess the quality of life in patients with TTH, tests should be performed not only to assess pain but also to determine personal psychological issues, quality of life, social functions, and other various dimensions [14].
Several previous studies have actively investigated the effects of manual therapy and neck stabilization exercises in patients with headache [6,7,10]. However, few studies have focused on methods to control the muscle tone that influences postural stability as well as a sensation of pressure in the periocular muscles. Thus, this study aimed to determine the effects of an eyeball exercise program combined with a cervical stabilization program in patients with chronic neck pain, TTH, and FHP, with respect to pain and disability, quality of life, impact on headache, postural alignment, and suboccipital and upper trapezius muscle tonicity.
Material and Methods
PARTICIPANTS:
Using an advertisement posted in a hospital (P Hospital in D Metropolitan City, South Korea), 55 participants were recruited among admitted patients and outpatients with neck pain from June to August 2023. The inclusion criteria were individuals with the following: experience of headache in the past 6 weeks, average neck pain on the numeric rating scale (NRS) ≥3, neck disability index (NDI) ≥5 and ≤24, generalized persistent pressure based on the classification of the International Headache Society, bilateral pain in the head or neck, tightening pain in the occipital region at or below a moderate level satisfying 2 of the 4 conditions of lack of increased pain upon a physical activity [15], and an individual with a CVA ≤53. The exclusion criteria were individuals with an abnormality of the central nervous system, individuals who were administered an analgesic in the past month for headache, and those experiencing symptoms such as dizziness, nausea, or vomiting during eyeball exercises. All participants were provided adequate explanations on the study purpose and procedures, after which they voluntarily agreed to participate. This study received approval from the Bioethics Committee of D University in accordance with the Helsinki Declaration and was registered on the WHO International Clinical Trials Registry Platform (registration number: KCT0008636).
EXPERIMENTAL PROCEDURES AND METHODS:
This study was designed as a pretest-posttest, randomized controlled investigation. The G*power program was used to estimate the sample size. The main effect size (d) was set at 0.93, with significance level (α)=0.05 and power (1-β)=0 [16]. The estimated sample size at minimum was n=20 in each group, and considering a 10% drop-out rate, the minimum number of participants in each group was set at n=22.
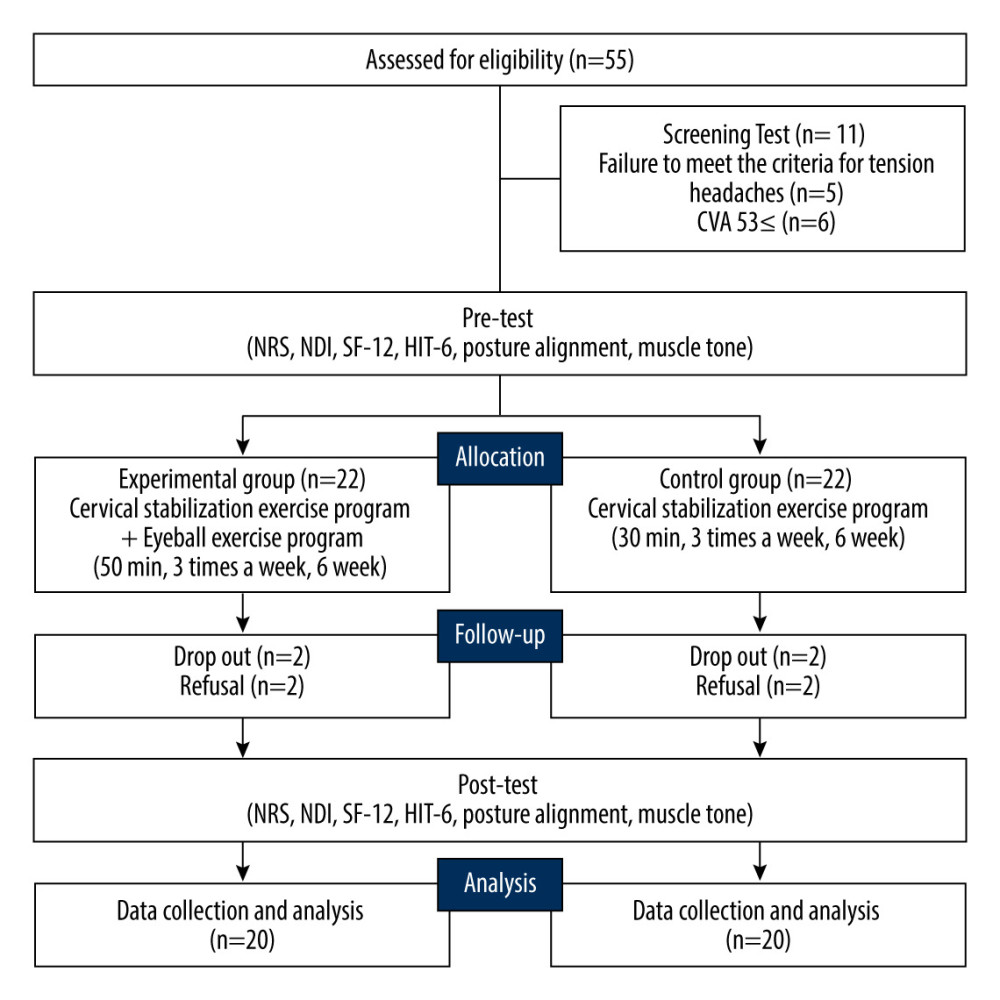
From the 55 recruited participants, those who did not satisfy the TTH criteria (n=5) and those with a CVA ≥53 (n=6) in the eligibility test were excluded. To compare the effects before and after the interventions, initial assessments were made before assigning them to experimental (n=22) and control (n=22) groups using the randomization program [17]. To analyze the pre- and post-intervention effects, neck pain (NRS), NDI, headache impact test-6 (HIT-6), Short Form-12 Health Survey Questionnaire (SF-12), postural alignment, and muscle tone were measured before and after the intervention. Both groups underwent cervical manual therapy and pressure biofeedback-guided stabilization exercise (30 min/session, 3 sessions per week, 6 weeks in total). Additionally, an eyeball exercise program (20 min/session, 3 sessions per week, 6 weeks in total) was applied in the experimental group. The experimental procedures are shown in Figure 1.
CERVICAL MANUAL THERAPY: Cervical manual therapy in this study was based on the method of Hyoung et al [18] in which rotation is applied to the atlanto-occipital joint in patients with neck pain. The rotation is applied as follows: One hand of the therapist is placed at the patient’s larynx and the other hand holds the patient’s chin. Next, the atlanto-occipital joint is rotated in a single direction to the anatomical limit, and a brief push is applied to the physiological space at a rapid rate and approximately 10 Hz frequency. This technique was performed on the joints bilaterally at approximately 10 min/session, 3 sessions per week, for 6 weeks in total.
CERVICAL STABILIZATION EXERCISE USING PRESSURE BIOFEEDBACK: Cervical stabilization exercise using pressure biofeedback (Chattanooga group Inc., Hixson, TN, USA) was based on the intervention method described by Abdel et al [19] with modifications. The pressure biofeedback used in this study provides quantitative indicators (Figure 2). The goal of the pressure biofeedback-guided cervical stabilization exercise is to improve the stability of the longus colli muscle through strengthening; it involves a chin-in exercise, whereby the chin is pulled downwards while the head is prevented from bending, such that the device is compressed during the exercise. The final target was set at 10 mm above the baseline (20 mm), and at the target level, the patient was instructed to hold for 10 s. The holding time of 10 s was repeated 10 times, with 10 s of resting time between each contraction. A break of 15 s was provided between each set. The exercise program consisted of 3 sets, repeated twice, at approximately 20 min/session, 3 sessions per week, for 6 weeks in total.
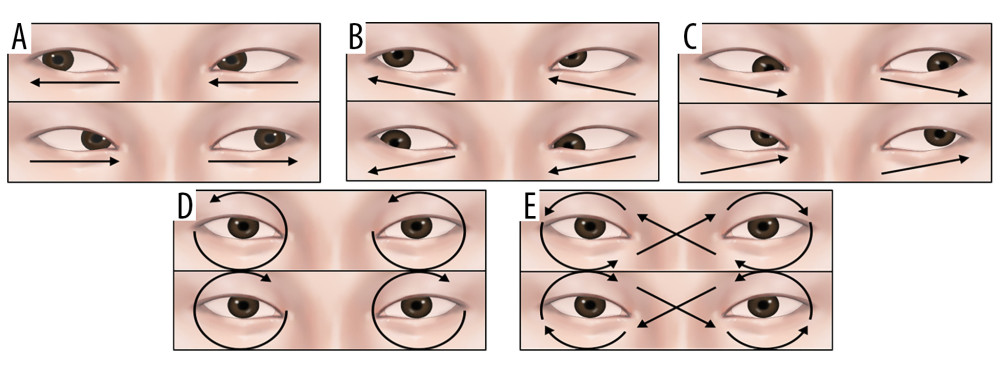
EYEBALL EXERCISE PROGRAM: The additional eyeball exercise program performed by the experimental group was based on the intervention method described by Sakshi & Kumar [20] with modifications. The method aims to use eyeball movements to relax the muscles in the periocular region. In this program, the physical therapist palpates the suboccipital muscle, after which the muscle is relaxed through the patient’s breathing, and then fixed by the physical therapist’s hand on the suboccipital muscle through gravity. The subsequent eyeball movements were performed: 1. leftward direction, 2. rightward direction (Figure 3A), 3. upper-left direction, 4. lower-left direction (Figure 3B), 5. upper-right direction, 6. lower-right direction (Figure 3C), 7. leftward circular motion, 8. rightward circular motion (Figure 3D), 9. leftward figure-eight motion, 10. rightward figure-eight motion (Figure 3E). In the eyeball exercise, the movements were performed to the maximum end range in the respective direction, with the holding time of 10 s, repeated 4 times. The resting time between each movement was 10 s. A break of 20 s was provided between each set, and the program consisted of 2 sets, performed at approximately 20 min/session, 3 sessions per week, for 6 weeks in total.
NUMERIC RATING SCALE (NRS): To examine the level of headache in patients, the NRS was used as a subjective verbal expression of the level of pain on a scale of 0–10, with higher scores indicating higher levels of pain. The reliability of NRS is high (intraclass correlation coefficient (ICC)=.61) [21].
NECK DISABILITY INDEX (NDI): The NDI was used to determine the level of neck disability in patients. The NDI is a questionnaire that rates the following 10 items on a scale of 0–5: pain intensity, personal care, lifting, reading, headache, concentration, work, driving, sleeping, and recreation. The NDI score is the sum of the score of each item. A score of 0–4 indicates “No disability”; a score of 5–14 indicates “Mild disability”; a score of 15–24 indicates “Moderate disability”; a score of 25–34 indicates “Severe disability”; and a score ≥35 indicates “Complete disability”. The intra-rater reliability of NDI is high at r=.85~.95 [22].
SHORT FORM-12 HEALTH SURVEY QUESTIONNAIRE (SF-12): To measure the quality of life in patients, the SF-12 was used as an instrument of health-related quality of life. The SF-12 is an abridged form of the Short Form-36 Health Survey Questionnaire (SF-36) developed by Ware and Shebourne [23]. The tool consists of 12 items in 8 subcategories of 2 main factors: physical health and mental health. Physical health comprises 4 domains: physical functioning, physical role limitations, bodily pain, and general health perceptions. Mental health comprises 4 domains: emotional role limitations, mental health, vitality, and social functioning. Each item is rated on a scale of 0–5; higher scores indicate greater health status. The total score as the sum of all scores of the 12 items ranges from 6 to 30 in both the physical component summary (PCS) and mental component summary (MCS). The reliability is high, at Cronbach’s alpha=0.88 [24].
HEADACHE IMPACT TEST-6 (HIT-6): The HIT-6 questions are designed to assess the following 6 parameters over the previous 4 weeks: pain, social functioning, role functioning, cognition, psychological pain, and vitality [25]. For each of the 6 HIT-6 questions, responses of “Never”, “Rarely”, “Sometimes”, “Often” and “Always” are assigned scores of 6, 8, 10, 11, and 13, respectively. The HIT-6 score is the sum of all scores for the 6 parameters, ranging from 36 to 78. Higher scores indicate greater levels of impact of headache on quality of life. The reliability of HIT-6 is high at Cronbach’s alpha=0.85 [25].
POSTURAL ALIGNMENT: To examine the changes in patient’s postural alignment according to the method of intervention, a tripod was placed at a distance of 1 m from the patient, and the patient was photographed in the straight stance position. Image J software (version1.46j, National Institutes of Health, USA) was used to measure the following angles: CVA, which is an angle formed by the line parallel to the 7th cervical vertebra and the line connecting to the tragus; the cranial rotation angle (CRA), which is an angle formed by the line connecting the 7th cervical vertebra and the tragus; and an angle formed by the line connecting the lateral side of the eye and the tragus. A single rater recorded the mean of triplicate measurements. The reliability of the instrument is high at r=0.86 [26].
MUSCLE TONE: To measure the tonicity of the upper trapezius and suboccipital muscles, MyotonPRO (Myoton AS, Tallinn, Estonia) was used to analyze the mechanical properties of the muscles. As a non-invasive device, MyotonPRO induces vibrational stimulation on the skin surface, and the device automatically takes measurements of the muscle tone. For the upper trapezius muscle, the muscle located at the center of the line connecting the acromion and the spinous process of the 7th cervical vertebra was palpated for measurements [27]. For the suboccipital muscle, the muscle located at the center of the line connecting the spinous process of the 2nd cervical vertebra and the occipital region was palpated for measurements [28]. During each measurement, the compressor of the MyotonPRO (3 mm in diameter) was vertically applied to the skin surface at a constant pressure (0.18N). The vibration at a lower tissue is induced by 10 short (15 ms) mechanical shocks applied at 1 Hz and low force (0.4 N). The tone was measured for both the upper trapezius and suboccipital muscles, and the mean of triplicate measurements was recorded. The ‘F’ parameter of the MyotonPRO indicates blood flow to the muscle and thus is reflective of muscle tone. It is defined as the effect arising from mechanical-elastic characteristics; higher values indicate greater muscle tone. The reliability of the tool is high (ICC=.85~.98) [28].
DATA ANALYSIS:
For data analysis, IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA) was used. Using descriptive statistics, the general characteristics of the participants are presented as means and standard deviations. The normality of data was tested using the Shapiro-Wilk test. The chi-square test was used to assess gender differences, while the t-test was used for comparisons of all other variables related to general characteristics and to test the homogeneity of pretest values. The between-group variations before and after the intervention was compared using the independent t-test, and the paired t-test was used to compare the within-group differences across dependent variables before and after the intervention. The level of significance was set at α=0.05.
Results
GENERAL CHARACTERISTICS:
Data of 20 participants in the experimental group and 20 participants in the control group among a total of 44 subjects were collected. Four subjects dropped out of the study for early discharge (n=2) and refusal to participate (n=2). The general characteristics of the participants are shown in Table 1.
COMPARISON OF PRE- AND POST-INTERVENTION NRS, NDI, SF-12, AND HIT-6:
Both the experimental and control groups were homogeneous for NRS, NDI, SF-12, and HIT-6 in the pretest. Both groups exhibited significantly reduced values after the intervention (p<.05). Variations of NDI, SF-12, and HIT-6 scores differed significantly between groups (p<.05) (Table 2).
COMPARISON OF PRE- AND POST-INTERVENTION CRA AND CVA:
Both the experimental and control groups were homogeneous for CVA and CRA in the pretest. Both groups exhibited significant changes after the intervention (p<.05), although variations in CVA and CRA did not differ significantly between the 2 groups (p>.05) (Table 3).
COMPARISON OF MUSCLE TONE PRE- AND POST-INTERVENTION FOR SUBOCCIPITAL AND UPPER TRAPEZIUS MUSCLES:
Both the experimental and control groups were homogeneous in tonicity for the suboccipital and upper trapezius muscles in the pretest. Both groups exhibited significant changes after the intervention (p<.05). Additionally, a significant difference was found between the 2 groups for variation in muscle tone of the suboccipital muscle (p<.05) (Table 3).
Discussion
This study aimed to determine the effects of an eyeball exercise program on patients with chronic neck pain, TTH, and FHP. The results demonstrated significant variations in NDI, SF-12, and HIT-6 scores, and suboccipital muscle tone in the experimental group, whose intervention included an additional eyeball exercise program.
The clinical practice guidelines (CPG) published in 2017 in the USA classify neck pain into the following 4 categories: neck pain with mobility deficits, neck pain with movement coordination impairments, neck pain with headache, and neck pain with radiating pain. TTH is included in the category of neck pain with headache, and the recommended intervention is self-stretching of C1/C2 for the acute phase, cervical manipulation and mobilization in addition to self-stretching for the subacute phase, and cervical and thoracic manipulation and combined manual therapy for the chronic phase [29]. The onset of neck pain with headaches in the participants of this study occurred approximately within the previous 11 months on average, indicating the chronic phase. According to the CPG recommendations, an exercise intervention including cervical manipulation was applied. In addition to cervical manual therapy, neck stabilization and eyeball exercises were applied for the purpose of relaxing the following pressure points in TTH: suboccipital, sternocleidomastoid, upper trapezius, and orbicularis oculi muscles. It is determined that increased neck stability and coordination effectively contributed to the alleviation of headache and neck pain.
Pachkhede and Singh [30] reported that symptoms of TTH, neck function, and quality of life could be improved through eyeball exercise. They also pointed out the need to systematically verify the effects of the exercise to reduce the pain intensity and frequency in treating TTH and for a randomized controlled study using rigorous methodological criteria. In TTH, complex effects of musculoskeletal and psychological factors caused by muscle tension-type affect the quality of life through such conditions as pain and reduced range of motion at the neck [31]. Accordingly, this study assessed the quality of life as well as neck function in all participants before and after the intervention, and the results showed significant improvements (p<.05). Furthermore, the experimental group whose intervention included an additional eyeball exercise program exhibited significant differences from the control group (p<.05). The percentage conversion of the total score demonstrated that NDI decreased from 33% to 14% (effect size, d=2.81) in the experimental group, and from 36% to 23% (effect size, d=2.24) in the control group. Among the PCS items of the SF-12, the scores of 1. General health, 5. Limited in kind of work, and 8. Pain-interference, increased by approximately 36% from 5.5 to 8.6 on average (effect size, d=−7.55) in the experimental group. Additionally, for the experimental group, among the MCS items of the SF-12, the scores of 7. Did work less careful and 12. Social limitations-time increased by approximately 39% from 5 to 8.3 on average (effect size, d=−5.29). This suggested that, the eyeball exercise program had equally positive effects on the quality of life as well as recovery of neck function via improvement in headache.
Rahimi et al. [32] reported that a 12-week intervention of eyeball exercise and diaphragm exercise had positive effects on the HIT-6 scores via improvement of sleep quality in 22 patients with TTH (p<.05). The HIT-6 is a tool to assess the impact of headache on normal daily activities [33]. In this study, post-intervention HIT-6 scores decreased significantly in all participants compared to pre-intervention HIT-6 scores (p<.05). Furthermore, the experimental group exhibited significant differences from the control group (p<.05). The percentage conversion of the total score demonstrated that HIT-6 scores decreased from ~79% to ~70% (effect size, d=2.06) in the experimental group and from ~78% to ~74% (effect size, d=1.36) in the control group. This suggested that the eyeball exercise program had positive effects on HIT-6 scores through changes in muscle length with increased movements of the muscles in the eye and neck regions. Thus, among the scales for assessment of headache, the HIT-6 and SF-12, which involve the assessment of pain and various emotional aspects, are likely to be closely associated with TTH.
Castien and Hertogh [13] reported that headache and periocular muscle pain could be induced by increased suboccipital muscle tone in the cervical region in TTH. They also reported that the cause was nerve root compression at the trigeminal and cervical nerves due to increased muscle tone. Olesiejuk et al [34] applied ischemic pressure on the neck and shoulder muscles in patients with TTH who had neck and shoulder pain and reported that the muscle tone in the neck and shoulder region decreased after 3 weeks of intervention (p<.05). Park and Park [35] applied a suboccipital muscle relaxation exercise combined with an ultrasound treatment in patients with TTH and reported that the suboccipital muscle tone decreased significantly after 4 weeks (p<.05). Similarly, in this study, a significant reduction in muscle tone after the intervention was observed in all participants (p<.05), although only the suboccipital muscle varied significantly between the control group and the experimental group (p<.05, effect size, Rt d=2.68, Lt d=4.65). The reduced muscle tone is attributed to the effects of the eyeball exercise to reduce nerve compression through muscle relaxation based on the physiological mechanisms at the trigeminal and cervical nerves. The eyeball exercise is also presumed to exert a simultaneous pain control effect, as the relaxation of the orbicularis oculi muscle contributes to the activation of beta-endorphin.
This study investigated the effects of an eyeball exercise program in patients with chronic neck pain, TTH, and FHP. There are several limitations in this study. First, as the mean age of the participants was approximately 35 years, it is difficult to generalize the results in other age groups or the elderly. Second, due to the lack of post-intervention follow-up, the long-term effects of the intervention remain unknown. Third, alternatives other than the eyeball exercise program implemented in this study should be discussed to provide a fundamental solution for TTH. Fourth, there are limitations in providing greater insight than objective methods by measuring the subjects’ psychological factors using subjective measurement methods. These limitations should be considered for future studies to offer more effective exercise methods for patients with chronic neck pain, TTH, and FHP.
Conclusions
This study was conducted to determine the effects of an eyeball exercise program on NRS, NDI, SF-12, and HIT-6 scores, postural alignment, muscle tone, and muscle thickness in patients with chronic neck pain, TTH, and FHP. The results revealed significant increases in NDI, SF-12, and HIT-6 scores, with significantly reduced suboccipital muscle tone in the experimental group. Based on the findings, the eyeball exercise program combined with manual therapy and stabilization exercise was shown to facilitate the relaxation of muscles in the eye and neck regions while reducing nerve compression. The method is thus suggested as an effective intervention to enhance function and quality of life in patients with chronic neck pain, TTH, and FHP.
References
1. Olesen J, International classification of headache disorders: Lancet Neurol, 2018; 17(5); 396-97
2. Thorud H-MS, Aurjord R, Falkenberg HK, Headache and musculoskeletal pain in school children are associated with uncorrected vision problems and need for glasses: A case-control study: Sci Rep, 2021; 11(1); 2093
3. Jespersen MS, Jaeger P, Ægidius KL, Sphenopalatine ganglion block for the treatment of postdural puncture headache: A randomised, blinded, clinical trial: Br J Anaesth, 2020; 124(6); 739-47
4. Madsen BK, Søgaard K, Andersen LL, Neck/shoulder function in tension-type headache patients and the effect of strength training: J Pain Res, 2018; 11; 445-54
5. Burch R, Migraine and tension-type headache: Diagnosis and treatment: Med Clin North Am, 2019; 103(2); 215-33
6. Bae S, Jung J, Moon D, Impact of movement control training using a laser device on the neck pain and movement of patients with cervicogenic headache: A pilot study: Healthcare, 2023; 11(10); 1439
7. Talbet JH, Elnahry AG, OnabotulinumtoxinA for the treatment of headache: An updated review: J Integr Neurosci, 2022; 21(1); 37
8. Kurt A, Turhan B, Physiotherapy management of migraine pain: Facial proprioceptive neuromuscular facilitation technique versus connective tissue massage: J Craniofac Surg, 2022; 33(8); 2328-32
9. Kawasaki T, Ohji S, Aizawa J, Correlation between the photographic cranial angles and radiographic cervical spine alignment: Int J Environ Res Public Health, 2022; 19(10); 6278
10. Park S-H, Lee M-M, Effect of lower trapezius strengthening exercise program on unstable support surface for neck pain patients with forward head posture: A randomized controlled trial: Physical Therapy Rehabilitation Science, 2022; 11(2); 189-97
11. Corum M, Aydin T, Ceylan CM, Kesiktas FN, The comparative effects of spinal manipulation, myofascial release and exercise in tension-type headache patients with neck pain: A randomized controlled trial: Complement Ther Clin Pract, 2021; 43; 101319
12. Runa A, Bao Q, Sai YC, Clinical observation of warming acupuncture and moxibustion at the temples combined with Deanxit in the treatment of tension headache with anxiety and depression: A retrospective study: Ann Palliat Med, 2021; 10(5); 5541-48
13. Castien R, De Hertogh W, A neuroscience perspective of physical treatment of headache and neck pain: Front Neurol, 2019; 10; 276
14. Ashina S, Buse DC, Bjorner JB, Health-related quality of life in tension-type headache: A population-based study: Scand J Pain, 2021; 21(4); 778-87
15. Arnold M, Headache classification committee of the international headache society (IHS) the international classification of headache disorders: Cephalalgia, 2018; 38(1); 1-211
16. Park S, Jung S, Effects of a complex exercise program using dynamic taping on patients with tension-type headache and chronic neck pain with forward head posture: KSIM, 2022; 10(4); 23-24
17. Saghaei M, Random allocation software for parallel group randomized trials: BMC Med Res Methodol, 2004; 4(1); 26
18. Hyong I-H, Kim H-S, Lee S-y, The effect of immediate pain and cervical ROM of cervical pain patients on stretching and manipulation: Journal of Korean Physical Therapy, 2009; 21(4); 1-7
19. Abdel-aziem AA, Draz AH, Efficacy of deep neck flexor exercise for neck pain: A randomized controlled study: Turkish Journal of Physical Medicine & Rehabilitation, 2016; 62(2); 107-15
20. Sharma S, MKS , Trataka Karma – a holistic approach for computer vision syndrome: International Ayurveda Publications, 2022; 7(2); 2034-39
21. Teyhen DS, Flynn TW, Bovik AC, Abraham LD, A new technique for digital fluoroscopic video assessment of sagittal plane lumbar spine motion: Spine, 2005; 30(14); E406-E13
22. Han S-Y, Nam J-M, Myoung S-M, Song K-J, A Comparison of sample size requirements for intraclass correlation coefficient (ICC): The Korean Journal of Applied Statistics, 2010; 23(3); 497-510
23. Framework IC, The MOS 36-item short-form health survey (SF-36): Med Care, 1992; 30(6); 473-83
24. Seo YA, Kim YA, Factors affecting acceptance of cosmetic surgery in adults in their 20s–30s: Aesthetic Plast Surg, 2020; 44; 1881-88
25. Kim E-J, Jung C-Y, Jang M-G, Review study of headache measurement tools-mainly on reliability and validity: Journal of Acupuncture Research, 2010; 27(1); 51-64
26. Choi Y-J, Hwang R, Effect of cervical and thoracic stretching and strengthening exercise program on forward head posture: The Journal of the Korea Contents Association, 2011; 11(10); 293-300
27. Kim J, Hyong I, Study on change of muscle tone and stiffness according to upper trapezius mild pain tf young adults: Indian Journal of Public Health Research & Development, 2018; 9(3); 605
28. Yeo SM, Kang H, An S, Cheong I, Mechanical properties of muscles around the shoulder in breast cancer patients: Intra-rater and inter-rater reliability of the MyotonPRO: PM&R, 2020; 12(4); 374-81
29. Ng JY, Hanna C, Headache and migraine clinical practice guidelines: A systematic review and assessment of complementary and alternative medicine recommendations: BMC Complement Med Ther, 2021; 21(1); 1-14
30. Pachkhede P, Singh R, Ocular exercises as a non conventional approach towards tension-type headache: A narrative review: Journal of Clinical & Diagnostic Research, 2023; 17(7); 6-10
31. Monzani L, Espí-López GV, Zurriaga R, Andersen LL, Manual therapy for tension-type headache related to quality of work life and work presenteeism: Secondary analysis of a randomized controlled trial: Complement Ther Med, 2016; 25; 86-91
32. Rahimi S, Soleymankhani A, Joyce L, Discriminating rapid eye movement sleep from wakefulness by analyzing high frequencies from single-channel EEG recordings in mice: Sci Rep, 2023; 13(1); 9608
33. Houts CR, Wirth R, McGinley JS, Content validity of HIT-6 as a measure of headache impact in people with migraine: A narrative review: Headache, 2020; 60(1); 28-39
34. Olesiejuk M, Marusiak J, Chalimoniuk M, Myofascial Trigger Points therapy decreases myotonometric tone and stiffness of trapezius muscle, benefits headaches and muscle pain in migraine: NeuroRehabilitation, 2023; 52(2); 299-310
35. Park S-K, Park S-H, The effect of combined suboccipitalis release exercise and therapeutic ultrasound on mechanical properties of cervical muscles and neck disability index, headache impact test in tension-type headache patients: Journal of The Korean Society of Integrative Medicine, 2021; 9(4); 271-81
Figures
Tables
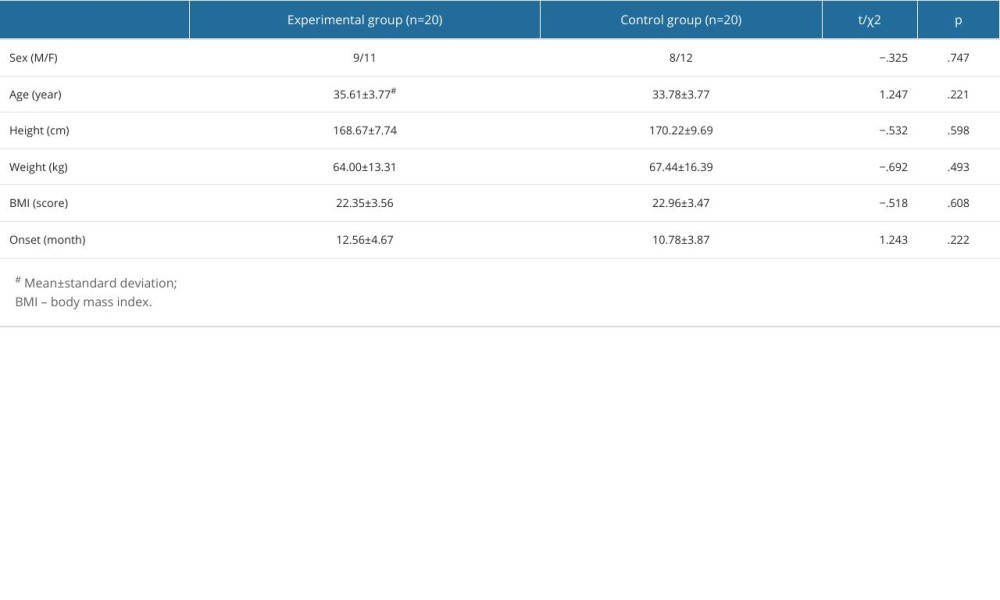 Table 1. General characteristics.
Table 1. General characteristics.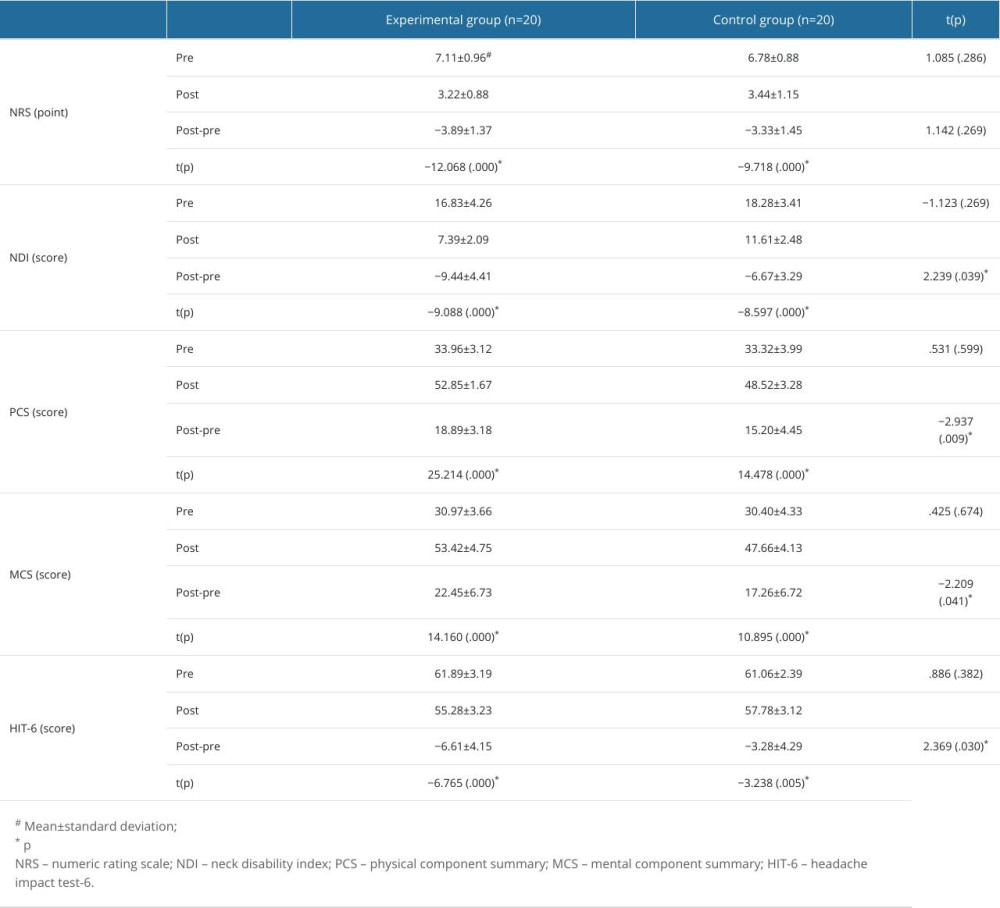 Table 2. Comparison of pre- and post-intervention scores between groups.
Table 2. Comparison of pre- and post-intervention scores between groups.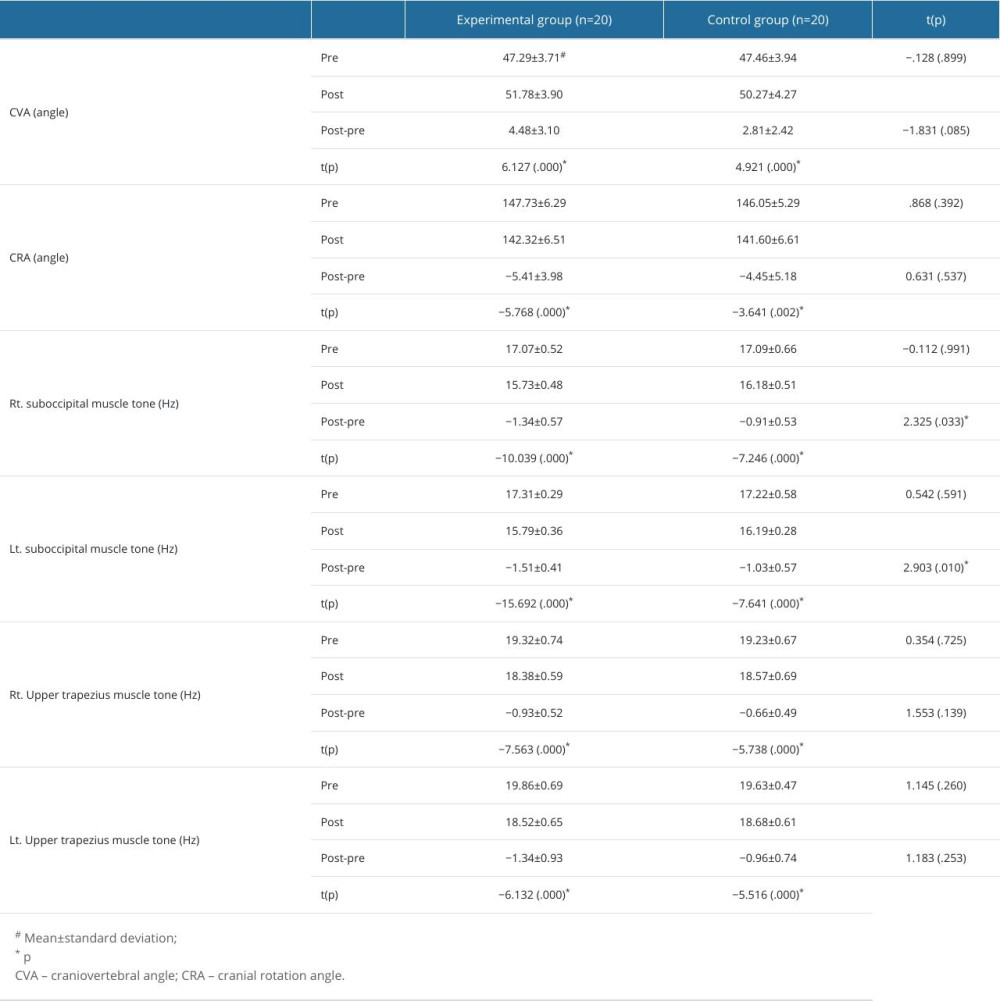 Table 3. Comparison of pre- and post-intervention variables between groups.
Table 3. Comparison of pre- and post-intervention variables between groups.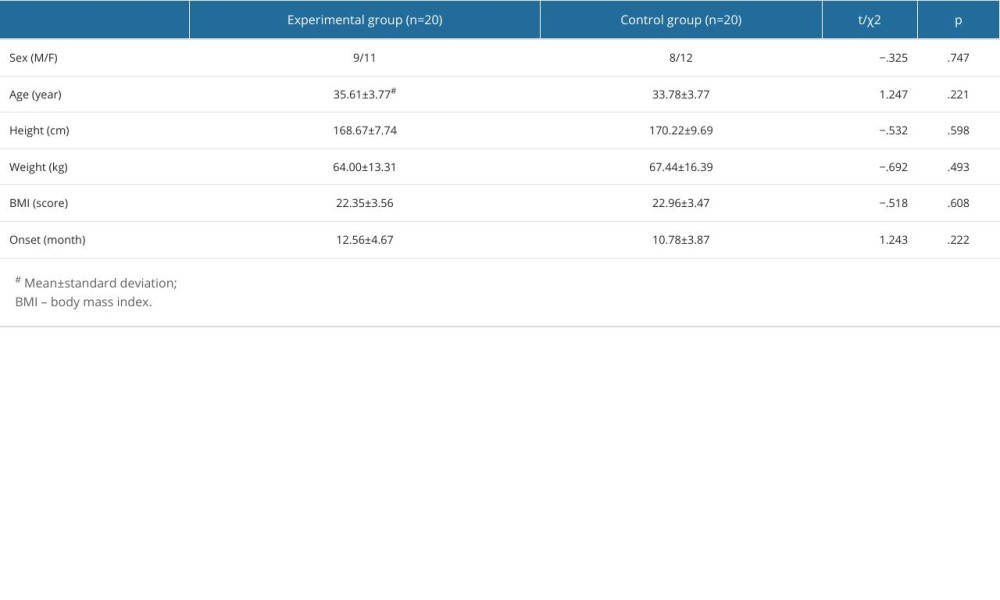 Table 1. General characteristics.
Table 1. General characteristics.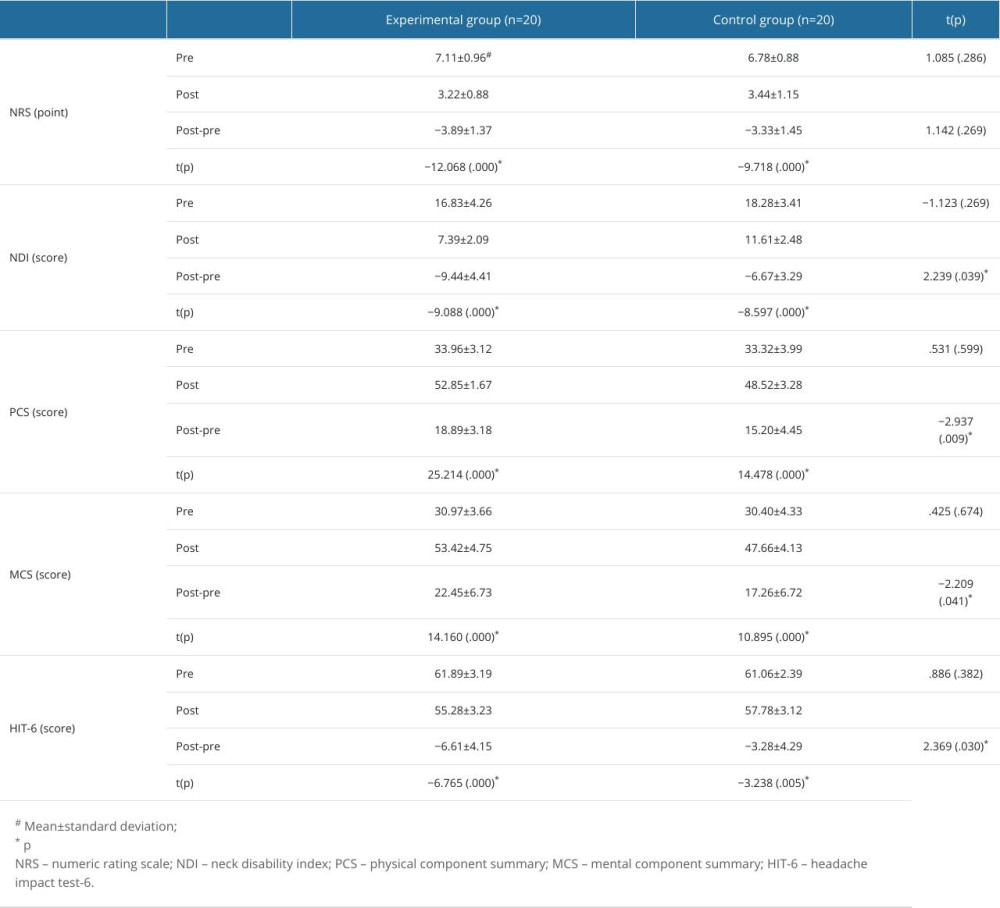 Table 2. Comparison of pre- and post-intervention scores between groups.
Table 2. Comparison of pre- and post-intervention scores between groups.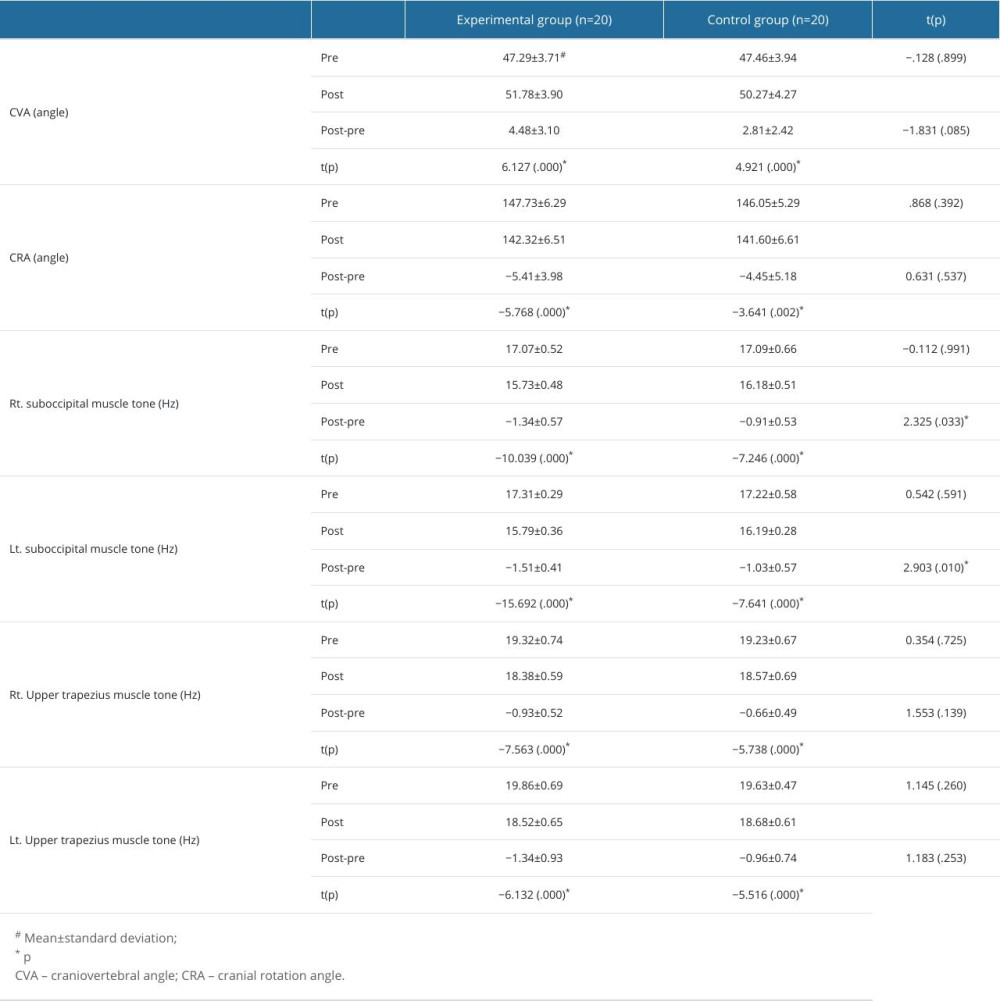 Table 3. Comparison of pre- and post-intervention variables between groups.
Table 3. Comparison of pre- and post-intervention variables between groups. In Press
Clinical Research
Surgical Reconstruction of Type IV Hypoplasia of the Thumb (Floating Thumb) in Infants: A Retrospective Ana...Med Sci Monit In Press; DOI: 10.12659/MSM.943686
Clinical Research
Effect of COVID-19 on Thrombosis Incidence and Patient Prognosis in Kidney Transplant RecipientsMed Sci Monit In Press; DOI: 10.12659/MSM.944285
Review article
The Influence of Acid-Base Balance on Anesthetic Muscle Relaxants: A Comprehensive Review on Clinical Appli...Med Sci Monit In Press; DOI: 10.12659/MSM.944510
Clinical Research
Enhancement of Pulmonary Function and Reduction of Complications Through EIT-Guided Yoga Breathing Exercis...Med Sci Monit In Press; DOI: 10.12659/MSM.942954
Most Viewed Current Articles
17 Jan 2024 : Review article 2,459,040
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research 1,560,914
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research 690,569
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial 50,460
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952