11 January 2023: Clinical Research
Implementation of Ultrasound-Guided Infraclavicular Subclavian Venous Catheterization During Anesthesia and Elective Surgery: A Prospective Observational Study at a Single Center in Lithuania
Ainius Žarskus1A*, Dalia Zykutė1B, Darius Trepenaitis1D, Andrius Macas1DDOI: 10.12659/MSM.938851
Med Sci Monit 2023; 29:e938851
Abstract
BACKGROUND: Ultrasound-guided procedures have become more reliable and efficient in daily anesthesiology practice, with increased patient comfort, better antimicrobial pattern, and easer care, and can be used in routine central vein catheterization practice. The infraclavicular subclavian vein approach provides all these advandages and in some clinical scenarios ensures the only appropriate route to central vein access. Therefore, this study of 105 patients aimed to implement and evaluate the use of ultrasound-guided infraclavicular subclavian venous catheterization.
MATERIAL AND METHODS: We enrolled 108 patients who were scheduled for elective major abdominal surgery and had an indication for central venous access. Catheterization was done according to the developed protocol. Anesthesiologists with at least 1 year of experience in regional ultrasound-guided anesthesia participated in this study. Data were collected and compared with the existing literature.
RESULTS: Out of 108 patients enrolled, 3 were excluded due to unfulfilled protocol. The successful catheterization rate was 98.1%. A significant relationship with deeper and narrower vein and failure was noted. On average, the distance between the vein entry point and acoustic shadow of the clavicle was 10.45 mm, at this point the depth was 22.01 mm and the diameter of the vein was 10.74 mm. The length of catheter intratissue passage was 42.06 mm. The angle between the skin and catheter passage was 31.58°. The malposition rate was 8.7%, and no predictive factors were identified. Equations to predict vein diameter and depth were generated. Patient weight more than 119.5 kg predicted procedure failure. There were no complications.
CONCLUSIONS: Ultrasound-guided infraclavicular subclavian vein catheterization can be easily and safely integrated into daily clinical practice, with high success rates and low complication rates.
Keywords: Axillary Vein, Subclavian Vein, Humans, Anesthesiology, Lithuania, Catheterization, Central Venous, Anesthesia, Conduction
Background
Despite surgery improvements and less invasive approaches, central venous access remains crucial for advanced hemodynamic monitoring, administration of vasoactive drugs, temporary pacing, and even renal replacement therapy [1]. Even before the ultrasound era, 3 anatomical sites for central line placement were well described and evaluated. Large multicenter trails and meta-analyses showed an almost 3-fold better antimicrobial effect of using an infraclavicular site [2,3], but with a significant increase in catheter malposition and pneumothorax [3]. Use of a jugular site is characterized by high success rates and arterial puncture [2]. Use of a femoral site improves pleural safety but, due to possible vessel valves, guidewire introduction may be complicated. As ultrasound-guided procedures were implemented into clinical practice, some of the sites turned out to be better for ultrasound imaging. Consequently, the standard approach for central venous access during the last 3 decades has moved toward ultrasound-guided internal jugular vein catheterization. Factors such as proximity to the skin, low level of angulation, distance to the pleura, and absence of bony structures make this the easiest site with which to obtain good-quality ultrasound imaging, successful guidewire introduction, and fluent catheter placement. As anesthesiology-intensive care staff members become more familiar with ultrasound-guided procedures, a need emerges to introduce a method with a lower incidence of infection, better patient comfort, and easier nursing care, with a preserved high success rate and low level of procedure-related mechanical complications. The former anatomic landmark technique-based central vein access through the subclavian vein has provided these advantages [4]. However, a moderate success rate (92.5%) and an unacceptably high incidence of mechanical complications (11.9%) [5] make this technique inadequate for modern anesthesia. Even though real-time ultrasound-guided internal jugular vein catheterization has proven to be advantageous, the evidence base for ultrasound-guided infraclavicular approaches is sparse [1]. Initial evaluation of the ultrasound usage for subclavian vein puncture in 1994 failed to prove any advantage [6]. Although a meta-analysis showed clear reduction of mechanical complications, increase in success was found only in the 2D dynamic ultrasound subgroup [7]. Even authors who achieved 100% success describes this method as “technically difficult” [8] To date, only experienced practitioners have managed to achieve a high success rate and low complication incidence [9].Therefore, this study of 105 patients who underwent anesthesia and elective surgery at a single center in Lithuania aimed to implement and evaluate the use of ultrasound-guided infraclavicular subclavian venous catheterization.
Material and Methods
ETHICS STATEMENT:
This study is a part of the large “Alternative central vein access in bone marrow transplantation program” study. The study was approved by the Regional Ethical Review Board on 2020.03.02 (registration number BE-2-15) and conducted in accordance with the Declaration of Helsinki. Patients were informed and written consent was obtained on the day of surgery.
ENROLLMENT:
This prospective, observational, single-center study was conducted between October 1, 2020, and May 1, 2021, at the Lithuanian University of Health Sciences Hospital Kaunas Clinics. We included 108 patients who were scheduled for elective major abdominal surgery and had an indication for central venous access during the surgery. Exclusion criteria were incomplete adherence or breaches to the catheterization protocol. Six anesthesiologists with at least 1 year of post-training experience in ultrasound-guided regional anesthesia participated in this study.
STUDY PROTOCOL:
A protocol was developed with the goal of creating working conditions comparable to those for internal jugular vein catheterization, as this would ease implementation in routine practice. The aim was to adopt all current evidence-based techniques to facilitate the procedure. Catheterizations were performed under general endotracheal anesthesia.
PATIENT POSITIONING:
Patients were positioned in the 15-degree Trendelenburg position to increase subclavian [10] and likely axillary vein dilatation and achieve optimal conditions for puncture. A neutral right arm position near the body was used because it remains controversial whether arm abduction is advantageous [11], and most of our operating rooms did not facilitate such positioning. The anesthesiologist’s position was kept the same as when catheterizing the internal jugular vein (over the head of the patient).
VENTILATION:
Lung-protective ventilation was implemented (tidal volume of 7 ml/kg ideal body weight [12] and PEEP 6 cm H2O), and ventilation was maintained during the procedure, despite the possible benefit of apnea [13].
EQUIPMENT:
Identical equipment for all procedures was used: Philips Sparq ultrasound machines with L12–4 Linear Array Vascular probes. Arrow Two-Lumen Central Venous Catheterization Set ref: cv-15802 with blue FlexTip®Catheter Arrow, a nonechogenic introducer needle (18Ga x2-1) preloaded with a guide wire (“J” tip spring – wire guide 0.81 mm/60 cm) was selected for the study. Strict sterile technique was applied, and Pajunk SonoCover 6×80 and Parker Sterile Aquasonic 100 Ultrasound Transmission gel were used. All measurements were performed with MicroDICOM 3.1.4 software.
CATHETERIZATION TECHNIQUE:
The subclavian and axillary veins were visualized using a longitudinal approach because it lessens clavicle artifacts and allows the determination of needle-vein relationships in real time. In this way, posterior wall injury, as well as other mechanical complications, can be reduced [14]. The aim was to obtain an image with the medial edge of the transducer overlying the clavicular bone and to ensure that the maximum diameter of the vein was visualized in the longitudinal view (Figure 1). Due to the higher success rate, the most proximal point of the vessel was chosen as the primary puncture site [15]. Needle navigation or guiding techniques (electromagnetic-guided position system) were not used, as evidence for their effectiveness in humans is insufficient [16]. Venous puncture was performed using a syringe-free, in-plane technique. The introducer needle was advanced until the needle tip was clearly seen in the vein lumen; subsequently, the guidewire was introduced under direct ultrasound observation. The procedure was discontinued if puncture was unsuccessful after 3 needle redirection attempts or lasted more than 15 min. To reduce the incidence of cardiac arrhythmias, guidewire introduction was limited to 20 cm [17]. After confirmation that the posterior vein wall was not penetrated, a 9 Fr 10.2-cm tissue dilator was introduced. The catheter could be advanced up to 20 cm because the puncture site is placed 2–3 cm laterally compared to the anatomical landmark subclavian vein puncture site [18]. The catheter tip position was checked with postoperative chest X-ray and in cases of malposition it was corrected in the Post-Anesthesia Care Unit (PACU) (Figure 2). Catheterization was considered successful if blood from both lumens could be drawn freely. Catheter care was carried out as per the hospital protocol, and in case of dysfunction or premature fall-out, the anesthesiologist was informed.
STATISTICAL ANALYSIS:
Statistical analysis was carried out using SPSS v25.0 software. The normality of the data was determined with the Kolmogorov–Smirnov test. Normally distributed data are reported as the mean, and nonnormally distributed data are reported as the median. Binary logistic regression was used to determine factors affecting malposition and failure rate. Linear regression was used to determine factors affecting vein diameter and depth. Normally distributed data were compared with the
Results
SUCCESS RATE AND COMPLICATIONS:
In all cases our used probes produced satisfactory images; both ventral and dorsal vessel’s walls can be identified. We achieved a success rate of 98.1% (n=103). No pneumothorax, arterial puncture, or hematoma formation was observed. Catheter position was confirmed using postoperative chest X-rays. In 94 (91.3%) cases, correct placement was confirmed: 66 (64.1%) were positioned in the superior vena cava and 28 (27.2%) in right atrium. Malposition was observed in 9 (8.7%) patients: 5 (4.8%) in right jugular vein and 4 (3.9%) in left brachiocephalic vein. We were not able to distinguish any predicting factors (eg, age, weight, vein diameter, puncture angle, puncture proximity) for catheter tip malposition in any location (right internal jugular vein, contralateral brachiocephalic vein). One premature catheter fall-out was observed; however, it was due to an accidental infusion line pull.
PREDICTORS OF VEIN DIAMETER AND DEPTH AND SUCCESSFUL CATHETERIZATION:
Using linear regression analysis, an equation predicting vein diameter was generated. Age, weight, and sex were identified as independent contributing factors:
Vein diameter prediction equation [mm]=3.513+0.071×Age[years] +0.048×Weight[kg] −1.137 Female. R Square −0.240. Durbin-Watson – 1.850, Std Residual – 2.619; +2.166.
However, by predicting vein depth, these demographic parameters showed interdependancy, therefore only weight can be identified as reliable and significant predictor for vein depth.
Vein depth prediction equation [mm]=7.578+0.199×Weight[kg] R Square −0.328. Durbin-Watson – 2.287, Std Residual – 2.761; +2.656 (Table 2).
Binary logistic regression due to the low failure rate was not able to determine factors related to procedure failure (2 cases). However, an independent sample t test showed statistically significant smaller (4.46 mm) vein diameter and deeper (10.29 mm) vein location compared to the success group (Table 3).
With only 2 procedure failures, it is difficult to make strong conclusions, but ROC still identified a cut-off value of more than 119.5 kg as a predictor for unsuccessful catheterization, with AUC (area under the curve) – 0.995 (a sensitivity 99.1% and a specificity 100%) (Figure 3).
Discussion
LIMITATIONS:
All 6 anesthesiologists who participated in the study had completed residency and had at least 1 year of constant practice in ultrasound-guided regional anesthesia. Therefore, how the results of this study can be extrapolated to trainees or less experienced practitioners remains uncertain. We were not able to randomize who would perform the procedure. In addition, all catheterizations were performed in almost ideal conditions, which contributes to a higher success rate and might not be achievable in every clinical scenario of anesthesia practice. Another limitation is our sample size; it was clearly too small to detect mechanical complications, but still enough to update our own hospital protocols. A low possibility exists that late-onset pneumothorax could have been undetected; however, there were no patients with subsequent clinical signs of pneumothorax.
Conclusions
Ultrasound-guided infraclavicular subclavian venous access can be safely and effectively used into routine clinical practice without any additional changes in preparation protocols. Procedure failure is mainly associated with increasing vessel depth. Body weight above 120 kg could be a predictor of procedure failure. The incidence of catheter tip malposition in our study is similar to those reported when using the anatomical landmark technique. We could not find factors associated with malposition.
Figures
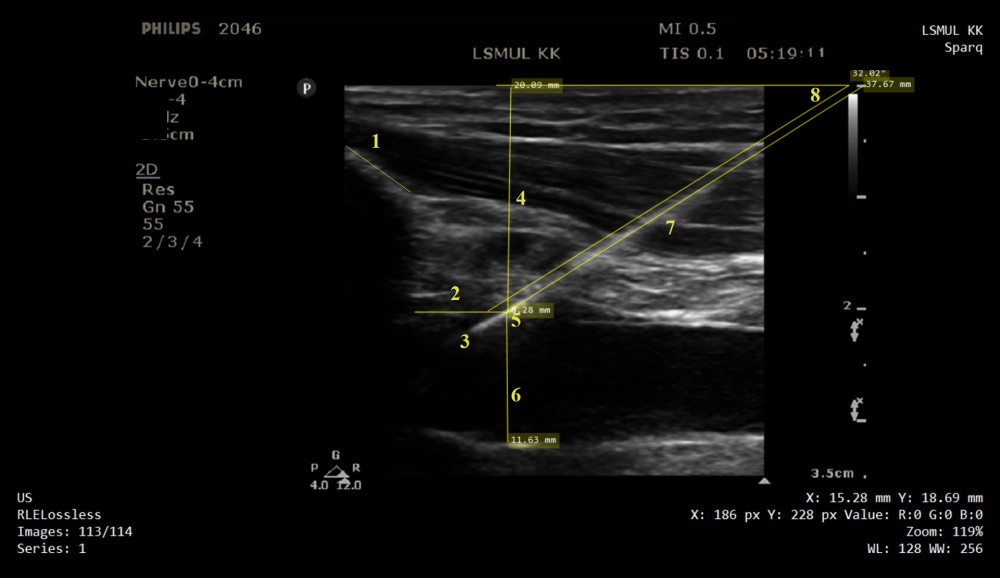 Figure 1. Ultrasound image of infraclavicular area, guidewire, subclavian and axillary veins are displayed in longitudinal view: 1 – clavicular bone; 2 – distance from the clavicle bone shadow and vein penetration point; 3 – guidewire placed in the vein lumen; 4 – vein depth; 5 – vein penetration point; 6 – vein diameter; 7 – intratissue passage; 8 – puncture angle.
Figure 1. Ultrasound image of infraclavicular area, guidewire, subclavian and axillary veins are displayed in longitudinal view: 1 – clavicular bone; 2 – distance from the clavicle bone shadow and vein penetration point; 3 – guidewire placed in the vein lumen; 4 – vein depth; 5 – vein penetration point; 6 – vein diameter; 7 – intratissue passage; 8 – puncture angle. 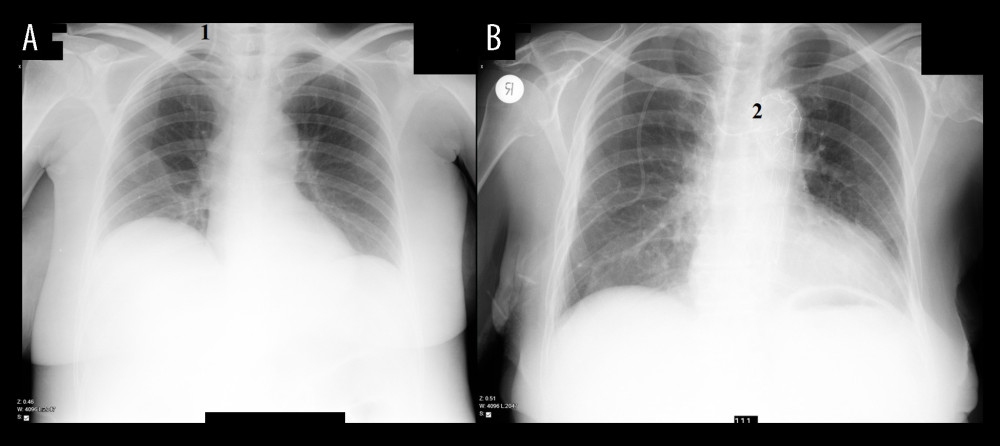 Figure 2. Catheter tip confirmation, chest X-ray obtained after catheterization. (A) Image 1, showing catheter’s tip is located in right jugular vein. (B) Image 2, showing catheter’s tip is located in a left brachiocephalic vein.
Figure 2. Catheter tip confirmation, chest X-ray obtained after catheterization. (A) Image 1, showing catheter’s tip is located in right jugular vein. (B) Image 2, showing catheter’s tip is located in a left brachiocephalic vein. 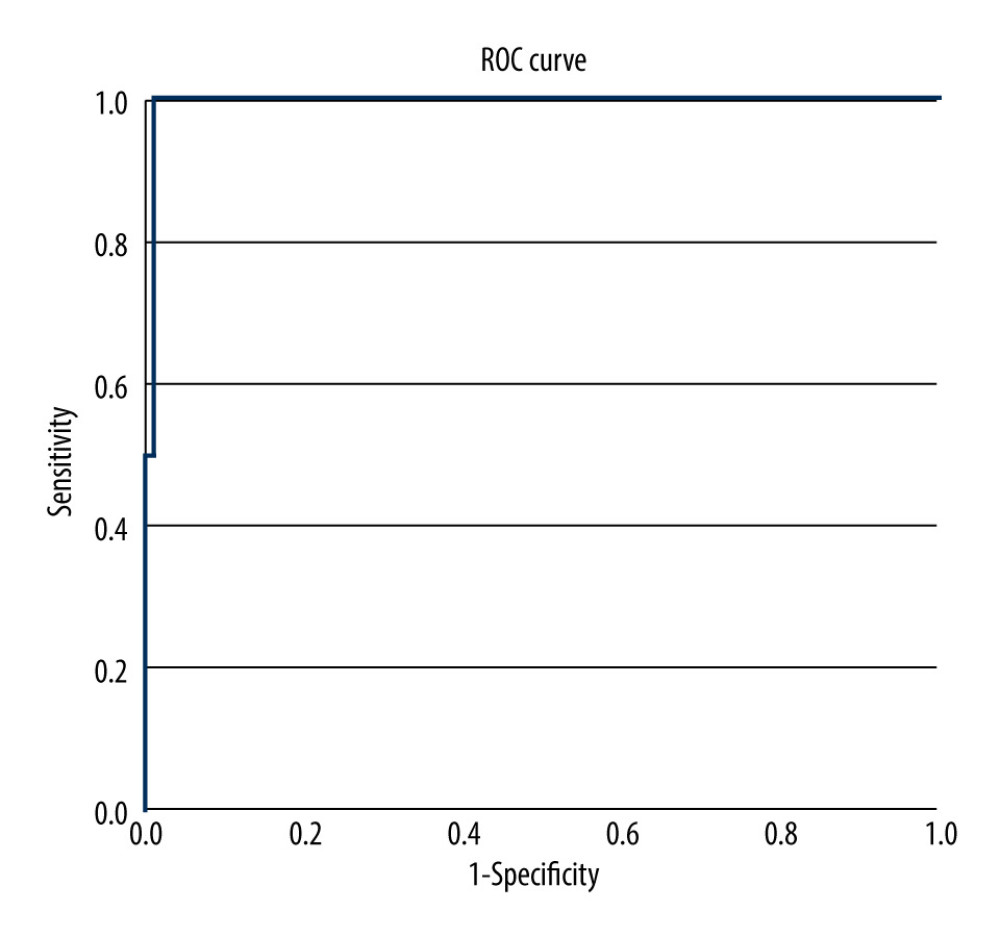 Figure 3. ROC with AUC of 0.995, predicting successful catheterization based on weight cut-off value 119.5 kg, with sensitivity 99.1% and specificity 100%. ROC – receiver operating characteristic; AUC – area under the curve.
Figure 3. ROC with AUC of 0.995, predicting successful catheterization based on weight cut-off value 119.5 kg, with sensitivity 99.1% and specificity 100%. ROC – receiver operating characteristic; AUC – area under the curve. Tables
Table 1. Demographic and anatomic parameters of patients enrolled into the research. Weight is expressed in kilograms, SAPS in points, distances in millimeters.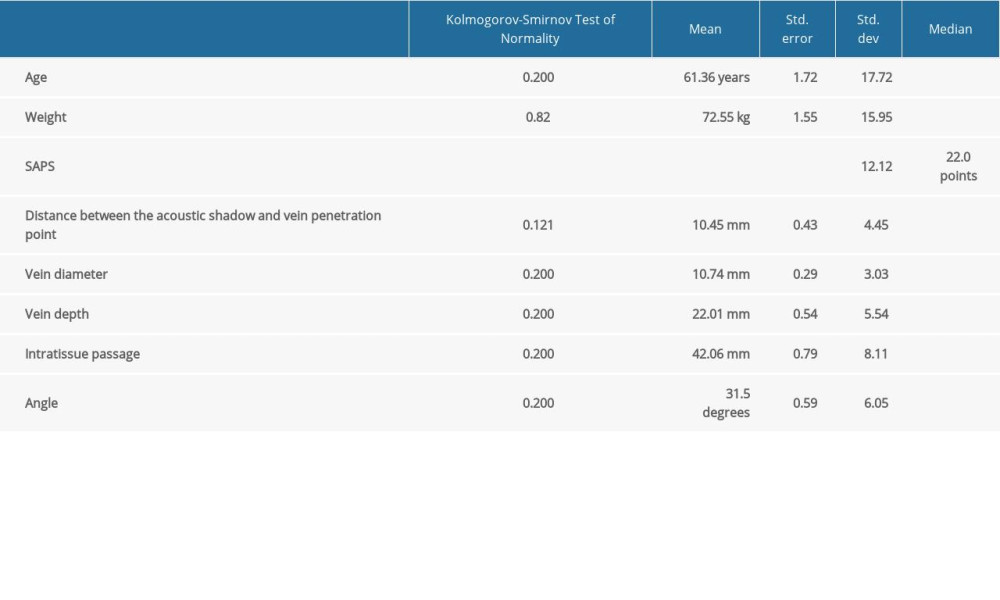 Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.
Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.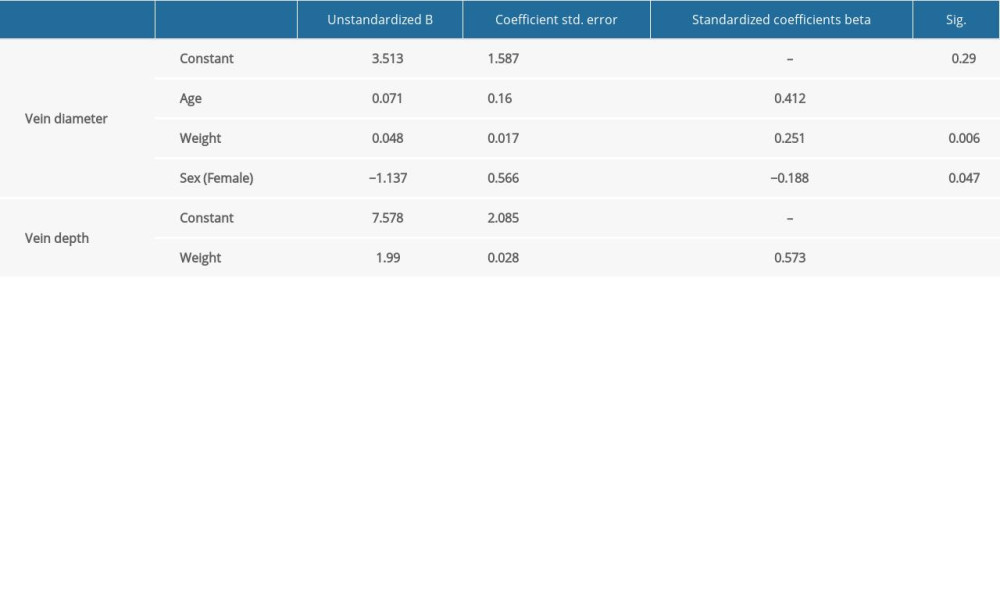 Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters.
Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters.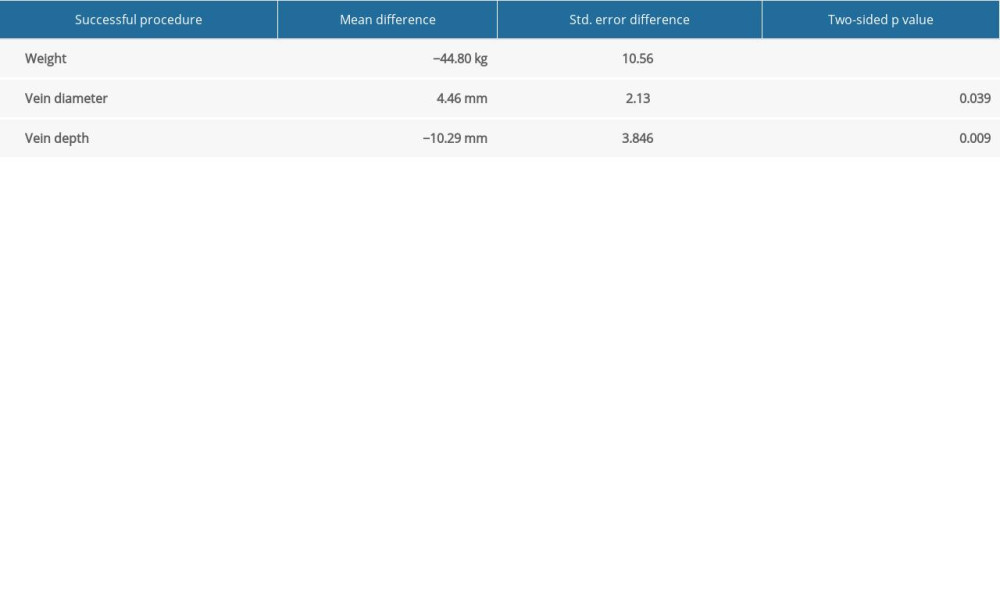
References
1. Practice Guidelines for Central Venous Access 2020, An updated report by the American Society of Anesthesiologists Task Force on Central Venous Access: Anesthesiology, 2020; 132(1); 8-43
2. Parienti JJ, Mongardon N, Mégarbane B, Intravascular complications of central venous catheterization by insertion site. 3SITES Study Group: N Engl J Med, 2015; 373; 1220
3. Ruesch S, Walder B, Tramèr MR, Complications of central venous catheters: Internal jugular versussubclavian access – a systematic review: Crit Care Med, 2002; 30; 2
4. Mcgee DC, Gould MK, Preventing complications of central venous catheterization: N Engl J Med, 2003; 348; 1123-33
5. Schulz J, Scholler A, Frank P, Complications and success rates of subclavian vein catheterization depending on experience: Anaesthesist, 2021; 70(4); 291-97
6. Mansfield PF, Hohn DC, Fornage BD, Complications and failures of subclavian-vein catheterization: N Engl J Med, 1994; 331(26); 1735-38
7. Lalu MM, Fayad A, Ahmed O, Ultrasound-guided subclavian vein catheterization: A systematic review and meta-analysis: Crit Care Med, 2015; 43(7); 1498-507
8. Fragou M, Gravvanis A, Dimitriou V, Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: A prospective randomized study: Crit Care Med, 2011; 39(7); 1607-12
9. Jiang L, Zhang M, Ma Y, Ultrasound-guided subclavian vein catheterization: A systematic review and meta-analysis: Several facts need to be noticed: Crit Care Med, 2015; 43(10); e474-75
10. Kawano M, Yoshimine K, Ultrasound observation of the subclavian vein: Changes in the diameter with the head tilted down: J Anesth, 2007; 21; 448
11. Lister RB, Welfare OWDA, Cheri T, Park MAJ, “Stop sign” position for subclavian ultrasound: A single-blinded observational study of subclavian vein dimensions: Eur J Emerg Med”, 2020; 27(5); 351-56
12. Serpa Neto A, Hemmes SNT, Barbas CS, Protective versus conventional ventilation for surgery: Anesthesiology, 2015; 123(1); 66-78
13. Palmaers T, Frank P, Eismann H, Catheterization of the subclavian vein and the risk of pneumothorax: Mechanical ventilation increases the risk of pneumothorax during infraclavicular landmark-guided subclavian vein puncture: A prospective randomized study: Anaesthesist, 2019; 68(5); 309-16
14. Lamperti M, Bodenham AR, Pittiruti M, International evidence-based recommendations on ultrasound-guided vascular access: Intensive Care Med, 2012; 38(7); 1105-17
15. Wang HY, Sheng RM, Gao YD, Ultrasound-guided proximal versus distal axillary vein puncture in elderly patients: A randomized controlled trial: J Vasc Access, 2020; 21(6); 854-60
16. Chew SC, Beh ZY, Hakumat Rai VR, Ultrasound-guided central venous vascular access – novel needle navigation technology compared with conventional method: A randomized study: J Vasc Access, 2020; 21(1); 26-32
17. Bodenham AR, Simcock L, Complications of central venous access: Central venous catheters, 2009; 175-205, Chichester, John Wiley & Sons, Inc
18. Morgan D, Ho K, Murray C, A randomized trial of catheters of different lengths to achieve right atrium versus superior vena cava placement for continuous renal replacement therapy: Am J Kidney Dis, 2012; 60(2); 272-79
19. Stachura MR, Socransky SJ, Wiss R, Betz M, A comparison of the supraclavicular and infraclavicular views for imaging the subclavian vein with ultrasound: Am J Emerg Med, 2014; 32(8); 905-8
20. Buetti N, Mimoz O, Mermel L, Ultrasound guidance and risk for central venous catheter-related infections in the ICU. A post hoc analysis of individual data of three multi-centric randomized trials: Clin Infect Dis, 2021; 73(5); e1054-61
21. Safety Committee of Japanese Society of Anesthesiologists, Practical guide for safe central venous catheterization and management 2017: J Anesth, 2020; 34(2); 167-86
22. O’Leary R, Ahmed SM, McLure H, Ultrasound-guided infraclavicular axillary vein cannulation: A useful alternative to the internal jugular vein: Br J Anaesth, 2012; 109(5); 762-68
23. Franco-Sadud R, Schnobrich D, Mathews BK, Recommendations on the use of ultrasound guidance for central and peripheral vascular access in adults: A position statement of the Society of Hospital Medicine: J Hosp Med, 2019; 14(9); E1-22
24. Farina A, Coppola G, Bassanelli G, Ultrasound-guided central venous catheter placement through the axillary vein in cardiac critical care patients: Safety and feasibility of a novel technique in a prospective observational study: Minerva Anestesiol, 2020; 86(2); 157-64
25. Sommerkamp SK, Romaniuk VM, Witting MD, A comparison of longitudinal and transverse approaches to ultrasound-guided axillary vein cannulation: Am J Emerg Med, 2013; 31(3); 478-81
26. Weber SU, Kim SC, The right supraclavicular ultrasound view for real-time ultrasound-guided definite placement of a central venous catheter with a microconvex transducer: Eur J Anaesthesiol, 2014; 31(3); 173-74
27. Tarbiat M, Davoudi M, Salimbahrami SA, Influence of arm position during infraclavicular subclavian vein catheterization in coronary artery bypass graft surgery: J Cardiovasc Thorac Res, 2018; 10(4); 192-96
28. Ahn JH, Kim IS, Shin KM, Influence of arm position on catheter placement during real-time ultrasound-guided right infraclavicular proximal axillary venous catheterization: Br J Anaesth, 2016; 116(3); 363-69
29. Rastogi A, Agarwal A, Goyal P, Ultrasound guided internal jugular vein cannulation in infants: Comparative evaluation of novel modified short axis out of plane approach with conventional short axis out of plane approach: Indian J Anaesth, 2018; 62(3); 208-13
30. Lal J, Bhardwaj M, Verma M, Bansal T, A prospective, randomised, comparative study to evaluate long axis, short axis and medial oblique axis approach for ultrasound-guided internal jugular vein cannulation: Indian J Anaesth, 2020; 64(3); 193-98
31. Shin HJ, Na HS, Koh WU, Complications in internal jugular vs subclavian ultrasound-guided central venous catheterization: A comparative randomized trial: Intensive Care Med, 2019; 45(7); 968-76
32. Roldan CJ, Paniagua L, Central venous catheter intravascular malpositioning: Causes, prevention, diagnosis, and correction: West J Emerg Med, 2015; 16(5); 658-64
33. Orihashi K, Imai K, Sato K, Extrathoracic subclavian venipuncture under ultrasound guidance: Circ J, 2005; 69; 1111-15
34. Polderman KH, Girbes AR, Central venous catheter use part 1: Mechanical complications: ntensive Care Med, 2002; 28(1); 1-17
35. Mageshwaran T, Singla D, Agarwal A, Kumar A, Comparative efficacy of supraclavicular versus infraclavicular approach of subclavian vein cannulation under ultrasound guidance: A randomised clinical trial: Indian J Anaesth, 2021; 65(Suppl 2); S69-72
36. Trabelsi B, Hajjej Z, Drira D, Comparison of ultrasound-guided internaljugular vein and supraclavicular subclavian vein catheterization in critically ill patients: A prospective, randomized clinical trial: Ann Intensive Care, 2022; 12; 91
Figures
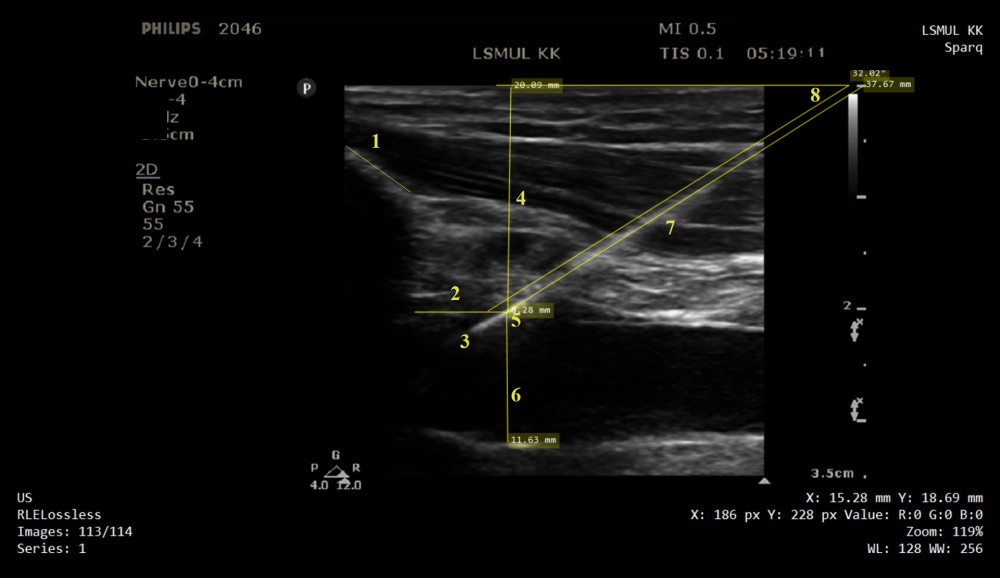 Figure 1. Ultrasound image of infraclavicular area, guidewire, subclavian and axillary veins are displayed in longitudinal view: 1 – clavicular bone; 2 – distance from the clavicle bone shadow and vein penetration point; 3 – guidewire placed in the vein lumen; 4 – vein depth; 5 – vein penetration point; 6 – vein diameter; 7 – intratissue passage; 8 – puncture angle.
Figure 1. Ultrasound image of infraclavicular area, guidewire, subclavian and axillary veins are displayed in longitudinal view: 1 – clavicular bone; 2 – distance from the clavicle bone shadow and vein penetration point; 3 – guidewire placed in the vein lumen; 4 – vein depth; 5 – vein penetration point; 6 – vein diameter; 7 – intratissue passage; 8 – puncture angle.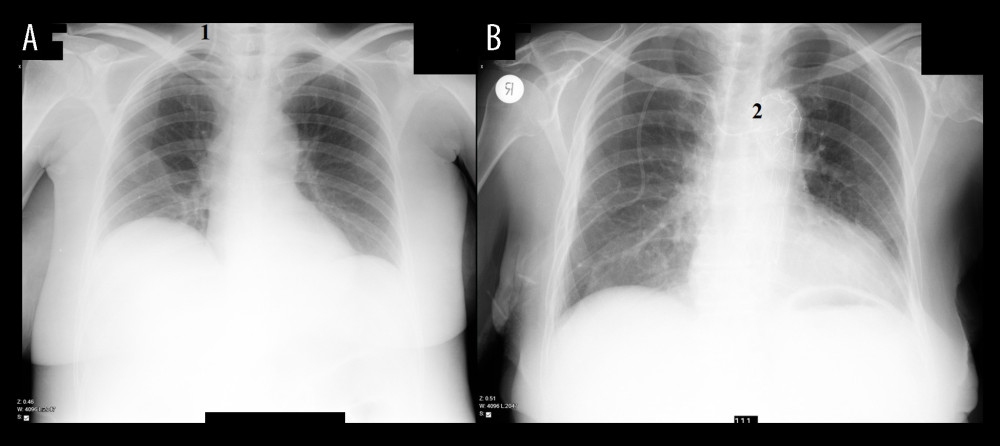 Figure 2. Catheter tip confirmation, chest X-ray obtained after catheterization. (A) Image 1, showing catheter’s tip is located in right jugular vein. (B) Image 2, showing catheter’s tip is located in a left brachiocephalic vein.
Figure 2. Catheter tip confirmation, chest X-ray obtained after catheterization. (A) Image 1, showing catheter’s tip is located in right jugular vein. (B) Image 2, showing catheter’s tip is located in a left brachiocephalic vein.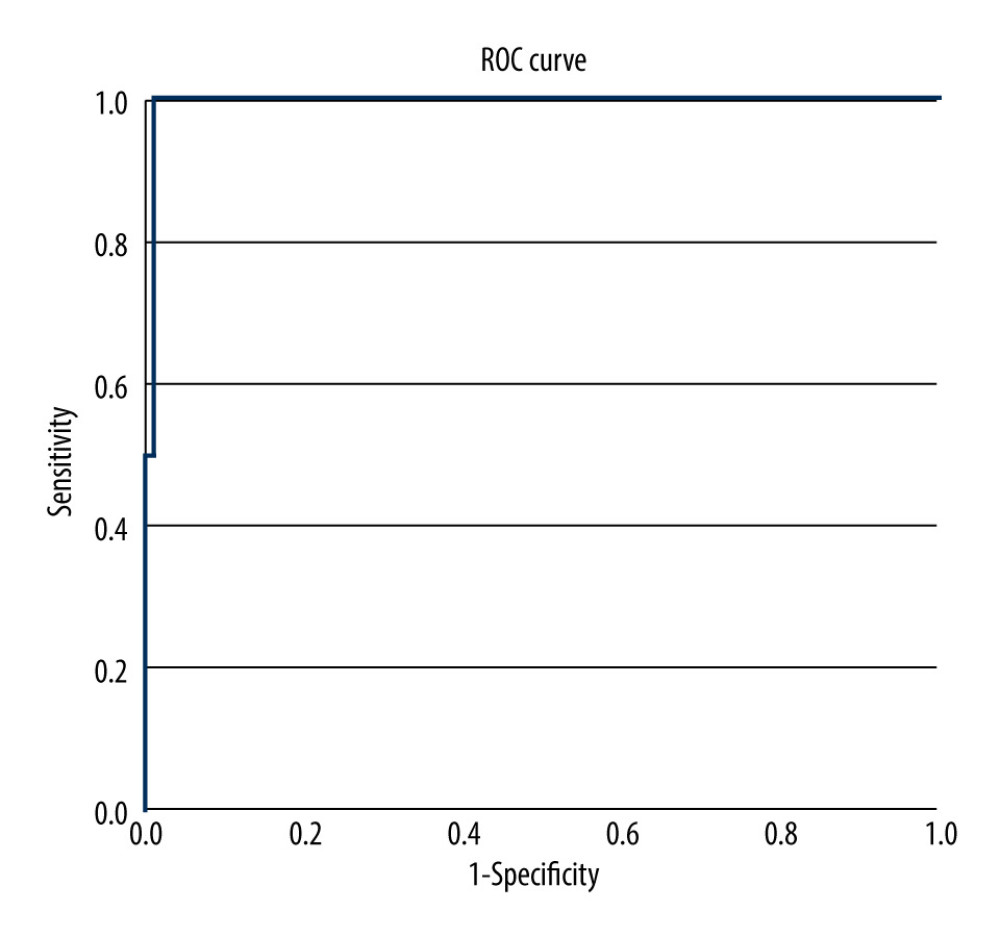 Figure 3. ROC with AUC of 0.995, predicting successful catheterization based on weight cut-off value 119.5 kg, with sensitivity 99.1% and specificity 100%. ROC – receiver operating characteristic; AUC – area under the curve.
Figure 3. ROC with AUC of 0.995, predicting successful catheterization based on weight cut-off value 119.5 kg, with sensitivity 99.1% and specificity 100%. ROC – receiver operating characteristic; AUC – area under the curve. Tables
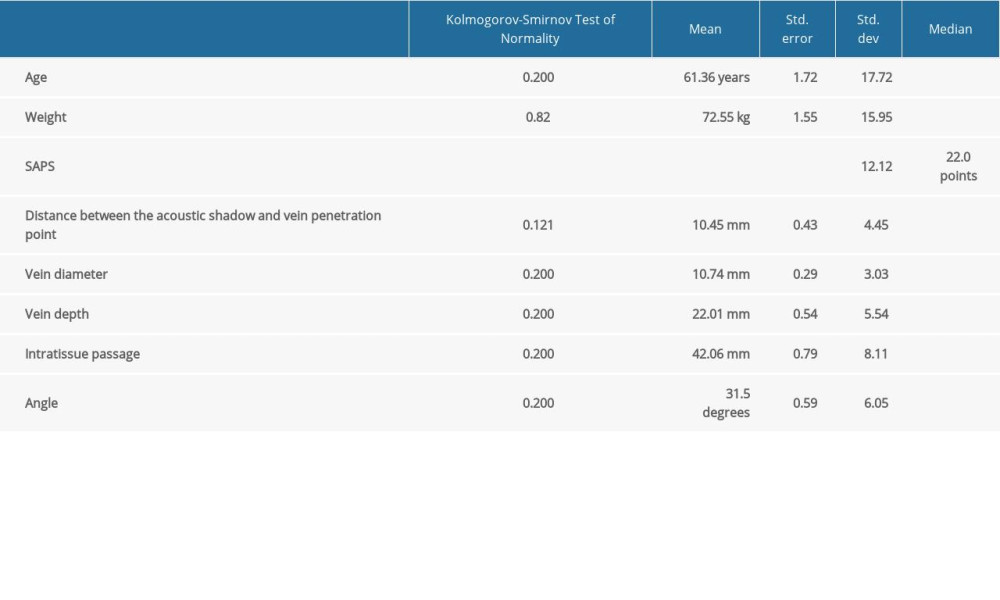 Table 1. Demographic and anatomic parameters of patients enrolled into the research. Weight is expressed in kilograms, SAPS in points, distances in millimeters.
Table 1. Demographic and anatomic parameters of patients enrolled into the research. Weight is expressed in kilograms, SAPS in points, distances in millimeters.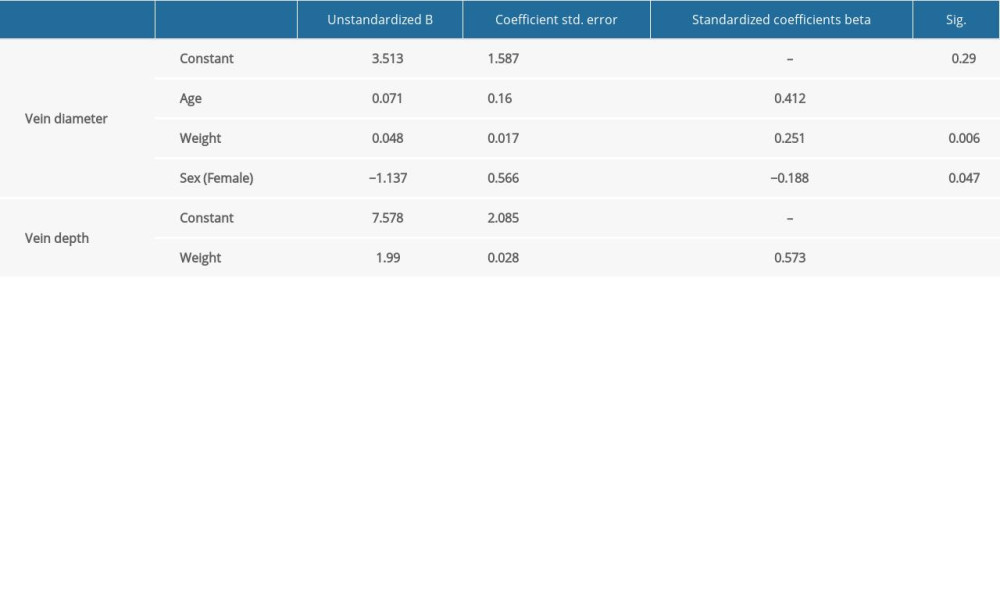 Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.
Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.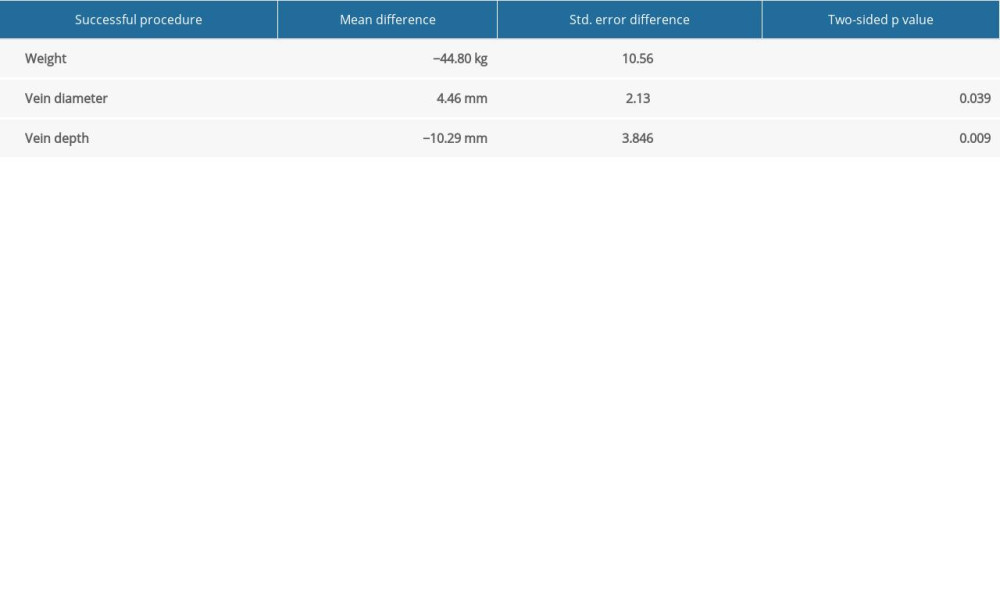 Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters.
Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters.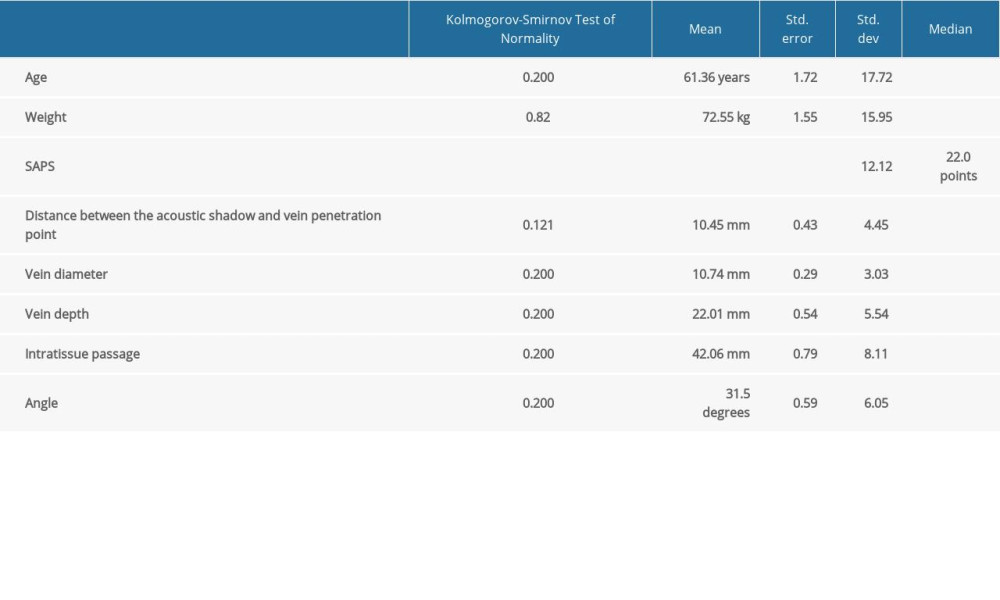 Table 1. Demographic and anatomic parameters of patients enrolled into the research. Weight is expressed in kilograms, SAPS in points, distances in millimeters.
Table 1. Demographic and anatomic parameters of patients enrolled into the research. Weight is expressed in kilograms, SAPS in points, distances in millimeters.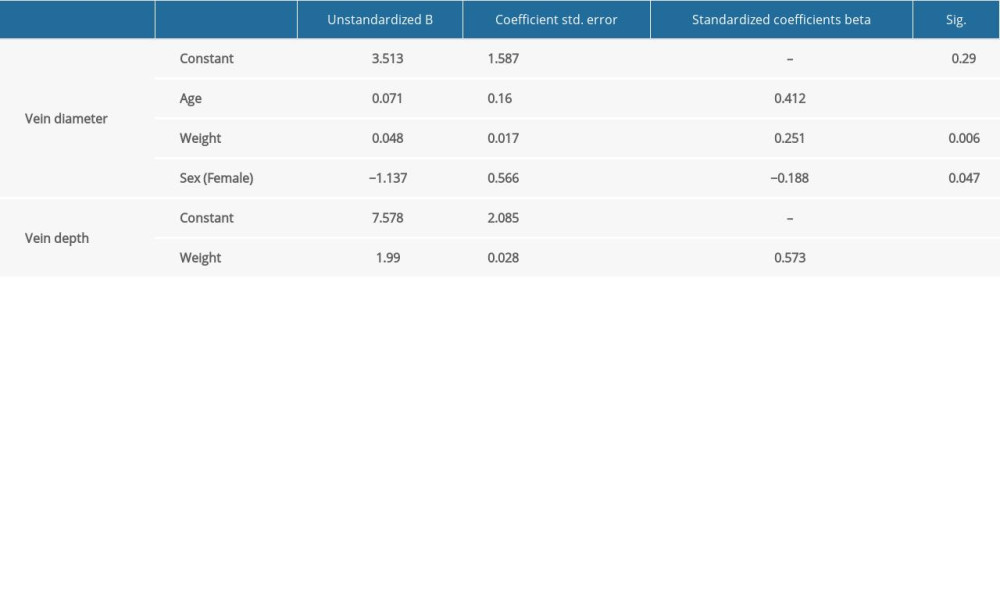 Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.
Table 2. Independent factors for prediction of vein diameter and depth. Age, weight, and male gender are significant independent prediction factors for large vein. Single independent contributor weight reliable predicts deeper vein location.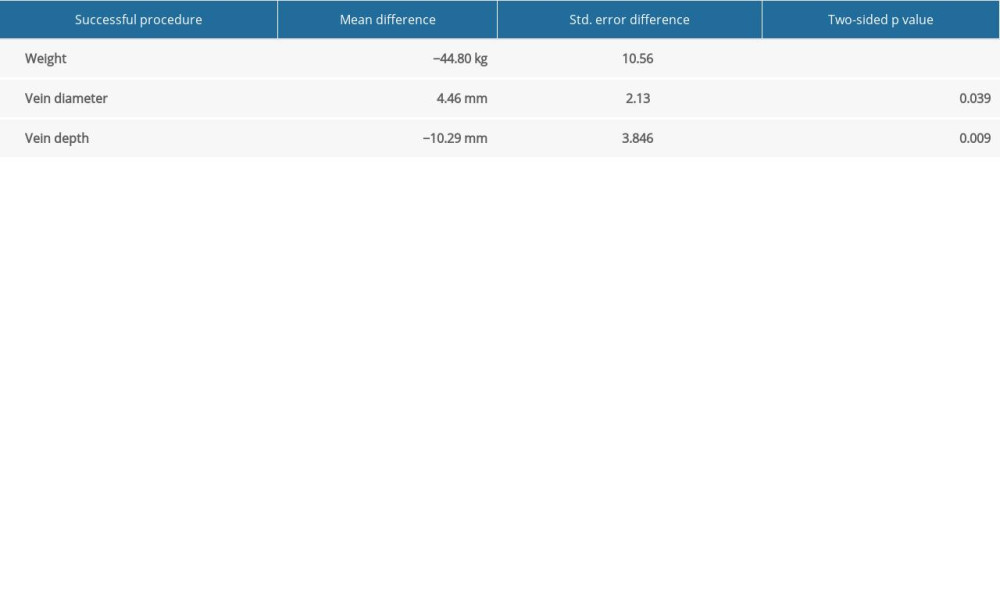 Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters.
Table 3. Relationship between procedure’s success and body weight, vein diameter, and depth. Weight is expressed in kilograms, distances in millimeters. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








