07 March 2024: Clinical Research
One-Year Clinical Outcomes in Acute ST-Segment Elevation Myocardial Infarction Patients Undergoing Optical Coherence Tomography-Guided Primary Percutaneous Coronary Intervention: A Comparative Study
Yen-Nan Fang1B, Wei-Chieh LeeDOI: 10.12659/MSM.943298
Med Sci Monit 2024; 30:e943298
Abstract
BACKGROUND: Percutaneous coronary intervention (PCI) with angiography guidance is a common procedure. Optical coherence tomography (OCT) is a non-invasive imaging method that uses light waves. This study from a single center aimed to compare 1-year outcomes in 75 patients with acute ST-segment elevation myocardial infarction (STEMI) who underwent OCT-guided primary PCI, with 163 patients with acute STEMI who underwent PCI without OCT guidance from February 2019 to July 2021.
MATERIAL AND METHODS: Patients with acute STEMI were enrolled from February 2019 to July 2021. Seventy-five patients underwent OCT-guided PCI (OCT group), while 163 underwent PCI without OCT (control group). Baseline characteristics, in-hospital mortality, target lesion revascularization, post-MI heart failure, and 1-year all-cause mortality were compared between groups.
RESULTS: The OCT group had lower diabetes mellitus and hyperlipidemia prevalence. Additionally, they experienced longer procedures (OCT: 50.45±21.75 min; control: 33.80±14.44 min; P<0.001). After PCI, the control group had lower left ventricular ejection fractions (OCT: 53.4%±10.5%; control: 47.8%±12.4%; P<0.001) and higher post-MI heart failure rates (OCT: 2.7%; control: 11.0%; P=0.030). Notably, the 1-year all-cause mortality rate was significantly lower in the OCT group (OCT: 1.3%; control: 8.0%; P=0.043).
CONCLUSIONS: During the 1-year follow-up, patients who received OCT-guided primary PCI experienced a notably lower rate of post-MI heart failure than did those who underwent primary PCI without OCT guidance. Importantly, the application of OCT in primary PCI procedures did not result in a higher incidence of distal embolism, even in cases with a significant thrombus burden.
Keywords: Myocardial Infarction, ST elevation myocardial infarction, percutaneous coronary intervention, Embolism, Heart Failure
Background
Acute myocardial infarction (MI) remains a leading cause of global morbidity and mortality [1]. MI disrupts the heart’s blood supply, exceeding a critical threshold and overwhelming the heart’s cellular repair mechanisms during ischemia [2]. Early effective reperfusion, achieved through thrombolytic therapy or primary percutaneous coronary intervention (PPCI), is essential to minimize ischemic damage and reduce the size of the MI [1,3]. Over the past two decades, advancements in early reperfusion therapies and pharmacotherapy have significantly improved outcomes for patients with ST-elevation myocardial infarction (STEMI) [4,5]. The timing of PPCI is critically linked to mortality risk, regardless of the time elapsed since symptom onset or the patient’s baseline mortality risk [6]. Optical coherence tomography (OCT) is a notable intracoronary diagnostic tool, providing highly detailed vascular images and superior structural detail, compared with intravascular ultrasound [7]. OCT, standing at the forefront of current intravascular imaging technology in clinical practice, excels in identifying calcified plaques and post-stent implantation, offering 3-dimensional reconstruction and real-time alignment with coronary angiographic images, thereby guiding PCI with its distinguished ability to provide high-resolution, exceptionally clear visualizations of vessel morphology [8–11]. Although OCT is gaining prominence in STEMI management during PPCI, its impact on clinical outcomes in this context is not fully established. Therefore, we aimed to compare outcomes in 75 patients from a single center with acute STEMI who underwent OCT-guided primary PCI with 163 patients with acute STEMI who underwent PCI without OCT guidance from February 2019 to July 2021.
Material and Methods
PATIENTS AND GROUPS:
Between February 2019 and July 2021, we enrolled 75 patients with acute STEMI who underwent OCT-guided PPCI, forming the OCT group. In addition, 163 patients with acute STEMI, who did not undergo OCT-guided PPCI, were selected as the control group. The exclusion criteria included patients with a critical status, those requiring supportive devices, such as extracorporeal membrane oxygenation or intra-aortic balloon pump support, and those in need of emergent coronary artery bypass graft surgery.
ETHICS STATEMENT:
This retrospective study received approval from the Institutional Review Committee of Kaohsiung Chang Gung Memorial Hospital, under approval number 201801078B0. It adhered to the ethics guidelines set forth in the 1975 Declaration of Helsinki.
OCT-GUIDED PCI PROCEDURAL STEPS:
OCT is an intravascular imaging modality that uses near-infrared light to provide high-definition, cross-sectional, and 3-dimensional images of the vessel microstructure during PCI (Figure 1). The OCT imaging system consists of 3 main components: the software, system, and catheter. The procedure’s steps are listed in Figure 2. In this study, the evaluation consisted of 6 steps, which included assessments of morphology, length, diameter, medial dissection, and expansion criteria. First, we performed an OCT pullback, in which an OCT catheter is inserted into the vessel and an infrared laser is used to scan the vessel wall in a spiral-like manner. The laser beam penetrates the tissue 2 to 3 mm deep, is reflected from there and returned to the OCT device via the catheter for evaluation. Second, we interpreted OCT images via the system, which can be done before PCI and is designed to help inform the treatment strategy, such as morphology, length, and diameter. Third, we detected the medial dissection, apposition, and expansion after PCI to optimize stent placement and outcome.
DEFINITIONS:
The definitions of MI in this study conformed to the most recent universal MI definition [12]. The Killip classes 1 to 4 were defined in 1967, when Killip and Kimball described the outcome of 250 patients with acute MI admitted to a coronary care unit, with 4 categories according to patient hemodynamic status [13]. Killip class 1 indicates without heart failure, Killip 2 indicates pulmonary rales less than half of lung field, Killip 3 indicates acute pulmonary edema, and Killip 4 indicates cardiogenic shock [14,15]. Cardiovascular mortality was defined specifically as death due to conditions including myocardial infarction, cardiac arrhythmia, and heart failure. Conversely, all-cause mortality included deaths from any cause. Target lesion revascularization was identified as any occurrence of PCI on a target lesion or coronary artery bypass graft surgery involving a target lesion.
STUDY ENDPOINTS:
This study was designed to evaluate a range of clinical endpoints over a 1-year follow-up period after treatment. Key among these endpoints was the incidence of MI, which signified a critical event in the cardiovascular health of the patients. Additionally, we closely monitored instances of target lesion revascularization, a significant indicator of the need for additional intervention at the site of the original cardiac event. The occurrence of heart failure was also a crucial endpoint, as it directly impacted patient quality of life and long-term health outcomes. Moreover, we assessed all-cause mortality rates within this period. This holistic approach allowed us to gain a thorough understanding of the treatment’s efficacy, encompassing both cardiac-specific and overall health outcomes in patients who underwent PPCI, with and without the guidance of OCT.
STATISTICAL ANALYSIS:
Data are presented in 2 forms: for continuous variables, we report means along with standard deviations to reflect the central tendency and variability of the data. Categorical variables are expressed as counts and percentages, providing a clear representation of their distribution across different categories. To rigorously compare continuous variables, we used 2 distinct statistical tests depending on the nature of the data distribution: the independent sample
Results
BASELINE CHARACTERISTICS:
Between the OCT and control groups, there was no significant difference in average age (OCT: 59±10.7 years; control: 60±12.2 years; P=0.208) or in the prevalence of male sex (OCT: 62.7%; control: 65.0%; P=0.331; Table 1). Both groups had a similar body mass index and systolic blood pressure at presentation. However, the control group had a higher prevalence of diabetes (OCT: 26.7%; control: 42.3%; P=0.020) and hyperlipidemia (OCT: 46.7%; control: 78.5%; P<0.001). Hemoglobin A1c levels were also notably higher in the control group (OCT: 6.5±1.4%; control: 6.9±1.8%; P=0.020). No significant differences were observed between the groups in terms of white blood cell count, creatinine levels, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, or peak troponin-I levels.
PROCEDURAL CHARACTERISTICS BETWEEN GROUPS:
The location of the infarction was similar in both groups, with most patients experiencing anterior wall STEMI (OCT: 57.3% vs control: 54.0%; P=0.872), as shown in Table 2. The severity of the condition, measured by Killip class, was also comparable, with most patients classified as Killip class 1 or 2 (OCT: 89.3% vs control: 91.4%; P=0.236). However, a notably higher percentage of patients in the control group were transferred from other hospitals (OCT: 26.7% vs control: 48.5%; P=0.002). While reperfusion times were similar between the groups, the procedure time was significantly longer in the OCT group (OCT: 50.45±21.75 min vs control: 33.80±14.44 min; P<0.001). The use of thrombectomy was similar in both groups (OCT: 74.7% vs control: 65.6%; P=0.164), but the OCT group had a higher usage of glycoprotein 2b/3a inhibitors than did the control group (OCT: 46.7% vs control: 27.6%; P=0.004). Furthermore, there were no significant differences in the incidence of slow flow and/or no reflow between the groups (OCT: 4.0% vs control: 5.5%; P=0.325).
FINDINGS OF OCT IMAGING:
The OCT findings are summarized in Table 3. In the OCT group, thrombus was present in 18.7% (14 out of 75) of patients, with 10.7% (8 out of 75) exhibiting white thrombus, and 8.0% (6 out of 75) showing red thrombus. Plaque rupture and erosion were observed in 32.0% (24 out of 75) of patients. A calcified nodule was noted in 2.7% (2 out of 75), and an intact fibrous cap (small protruding thrombus) was identified in 6.7% (5 out of 75) of cases.
POST-MI ECHOCARDIOGRAPHIC PARAMETERS AND 1-YEAR CLINICAL FOLLOW-UP CLINICAL OUTCOMES:
Table 4 shows the 1-year clinical follow-up results and echocardiography parameters. After PPCI, the control group exhibited a significantly lower left ventricular ejection fraction than the OCT group (OCT: 53.4±10.5% vs control: 47.8±12.4%; P<0.001). The prevalence of reduced and mildly reduced ejection fraction was comparable between the groups. Similarly, the incidence of mitral regurgitation grade exceeding 2 was not significantly different (OCT: 2.7% vs control: 7.2%; P=0.168). There were no significant differences in the rates of in-hospital mortality and 1-year target lesion revascularization. However, the OCT group demonstrated a lower incidence of post-myocardial infarction heart failure (OCT: 2.7% vs control: 11.0%; P=0.030). Importantly, the 1-year mortality rate was significantly lower in the OCT group than in the control group (OCT: 1.3% vs control: 8.0%; P=0.043).
Discussion
LIMITATIONS:
First, it is crucial to acknowledge that this study was conducted as a retrospective cohort study and did not incorporate randomization to reduce potential bias. The potential confounders influenced the study’s results and conclusions. Second, the study was limited by a relatively small number of enrolled patients and the exclusion of individuals requiring extracorporeal membrane oxygenation or intra-aortic balloon pump support. Third, our analysis could not establish a correlation between OCT findings and clinical outcomes, due to the limited number of clinical events observed in the OCT group. Fourth, it may be beneficial to include a group undergoing intravascular ultrasound-guided PCI to compare results. This could help in highlighting the differences and potential advantages of OCT-guidance PCI. Despite these limitations, our study, which was prospective and observational in nature, still provides valuable insights. Notably, OCT-guided PCI did not increase the incidence of distal embolism, especially in STEMI cases characterized by a high thrombus burden.
Conclusions
During the 1-year follow-up, patients who received OCT-guided PPCI experienced a notably lower rate of post-MI heart failure than did those who underwent PPCI without OCT guidance. Importantly, the application of OCT in PPCI procedures did not result in a higher incidence of distal embolism, even in cases with a significant thrombus burden.
Figures
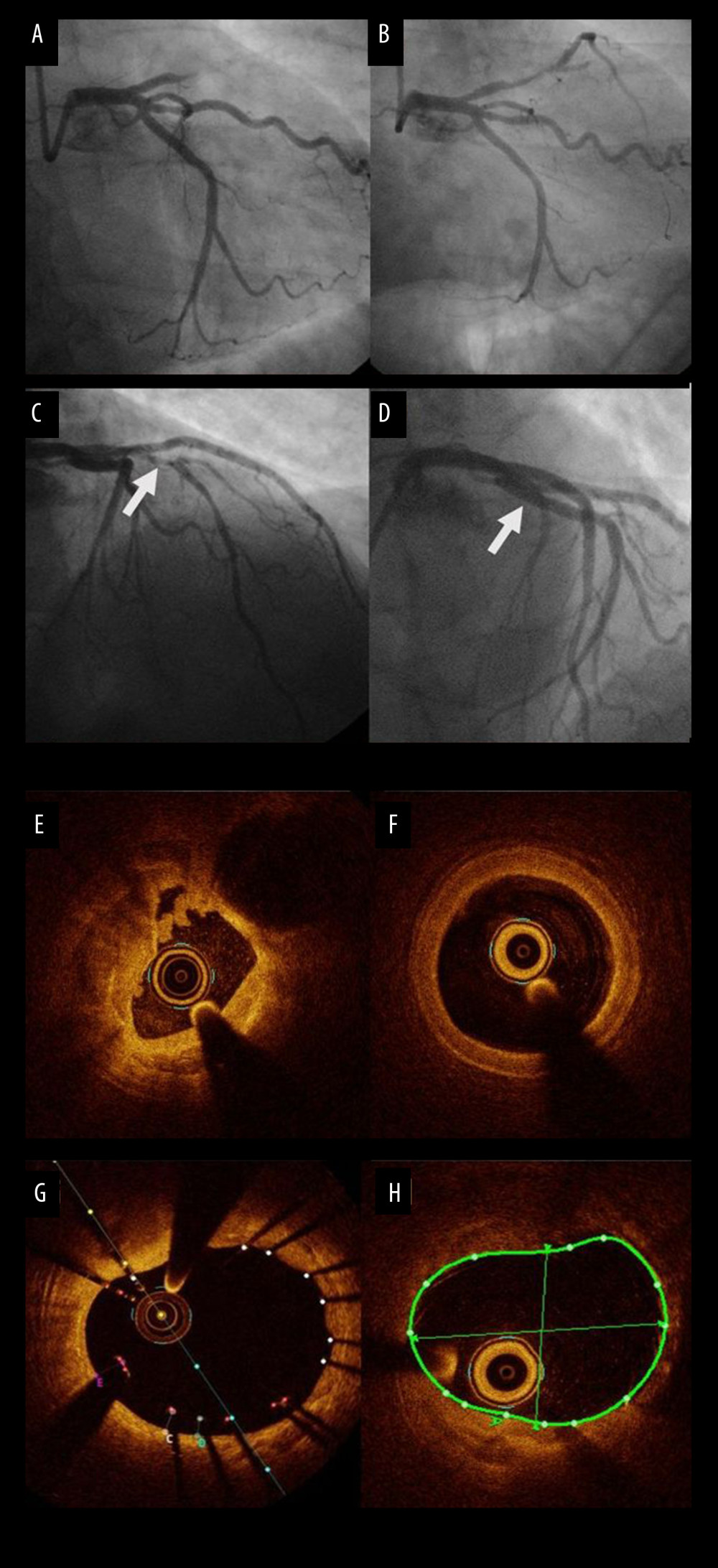 Figure 1. A 58-year-old woman presented with acute anterior wall ST elevation myocardial infarction. (A) the left coronary angiogram showed the culprit lesion thrombotic occlusion at proximal left anterior descending artery (LAD), with a right anterior oblique caudal view. (B) The left coronary angiogram after thrombus suction. (C) The arrow shows the culprit site after thrombus suction, with a right anterior oblique cranial view. (D) The arrow shows the result after drug-eluting stent (DES) and optical computed tomography (OCT)-guided percutaneous coronary intervention (PCI). (E) OCT finding at the culprit site, with much thrombus and minimal luminal area (MLA) only 1.9 mm2 after thrombus suction. (F) OCT finding at the LAD reference site, with MLA 4.7 mm2. (G) OCT finding at the culprit site after DES implantation. (H) OCT finding at the LAD reference site.
Figure 1. A 58-year-old woman presented with acute anterior wall ST elevation myocardial infarction. (A) the left coronary angiogram showed the culprit lesion thrombotic occlusion at proximal left anterior descending artery (LAD), with a right anterior oblique caudal view. (B) The left coronary angiogram after thrombus suction. (C) The arrow shows the culprit site after thrombus suction, with a right anterior oblique cranial view. (D) The arrow shows the result after drug-eluting stent (DES) and optical computed tomography (OCT)-guided percutaneous coronary intervention (PCI). (E) OCT finding at the culprit site, with much thrombus and minimal luminal area (MLA) only 1.9 mm2 after thrombus suction. (F) OCT finding at the LAD reference site, with MLA 4.7 mm2. (G) OCT finding at the culprit site after DES implantation. (H) OCT finding at the LAD reference site.  Figure 2. Stepwise explanation of the study procedures and decision-making process. The procedural guidelines for the study are delineated in a stepwise manner, encompassing several critical criteria. Morphological assessment involved identifying high calcium plaque characterized by an arc exceeding 180 degrees, thickness over 0.5 mm, and length of more than 5 mm. Landing zones for interventions were selected based on the visualization of healthy tissue and the external elastic lamina. Diameter criteria required measuring the dimensions of the vessel, stent, and balloon, with reference measurements taken distally to select stent and distal balloon sizes, and proximally for proximal balloons. Significant medial dissections, defined as those penetrating the medial layer and extending beyond 1 quadrant arc, were promptly addressed. Apposition criteria involved rectifying gross malposition, noted when the separation from the vessel wall exceeded 3 mm. Finally, expansion criteria verified stent deployment, with over 80% expansion considered acceptable and beyond 90% regarded as optimal, ensuring precision and efficacy in the intervention process.
Figure 2. Stepwise explanation of the study procedures and decision-making process. The procedural guidelines for the study are delineated in a stepwise manner, encompassing several critical criteria. Morphological assessment involved identifying high calcium plaque characterized by an arc exceeding 180 degrees, thickness over 0.5 mm, and length of more than 5 mm. Landing zones for interventions were selected based on the visualization of healthy tissue and the external elastic lamina. Diameter criteria required measuring the dimensions of the vessel, stent, and balloon, with reference measurements taken distally to select stent and distal balloon sizes, and proximally for proximal balloons. Significant medial dissections, defined as those penetrating the medial layer and extending beyond 1 quadrant arc, were promptly addressed. Apposition criteria involved rectifying gross malposition, noted when the separation from the vessel wall exceeded 3 mm. Finally, expansion criteria verified stent deployment, with over 80% expansion considered acceptable and beyond 90% regarded as optimal, ensuring precision and efficacy in the intervention process. References
1. O’Gara PT, Kushner FG, Ascheim DD, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: J Am Coll Cardiol, 2013; 61(4); 485-510
2. Ahmed M, Mehta P, Reddivari AKR, Percutaneous coronary intervention: Stat Pearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing
3. Ndrepepa G, Improving myocardial injury, infarct size, and myocardial salvage in the era of primary PCI for STEMI: Coron Artery Dis, 2015; 26(4); 341-55
4. Rasoul S, Ottervanger JP, de Boer MJ, Predictors of 30-day and 1-year mortality after primary percutaneous coronary intervention for ST-elevation myocardial infarction: Coron Artery Dis, 2009; 20(6); 415-21
5. Keeley EC, Boura JA, Grines CL, Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: A quantitative review of 23 randomised trials: Lancet, 2003; 361; 13-20
6. McNamara RL, Wang Y, Herrin J, Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction: J Am Coll Cardiol, 2006; 47(11); 2180-86
7. Kume T, Uemura S, Current clinical applications of coronary optical coherence tomography: Cardiovasc Interv Ther, 2018; 33(1); 1-10
8. Otake H, Optical coherence tomography-guided percutaneous coronary intervention: Evidence and clinical trials: Interv Cardiol Clin, 2023; 12(2); 225-36
9. Kume T, Akasaka T, Kawamoto T, Assessment of coronary arterial thrombus by optical coherence tomography: Am J Cardiol, 2006; 97(12); 1713-17
10. Bezerra HG, Attizzani GF, Sirbu V, Optical coherence tomography versus intravascular ultrasound to evaluate coronary artery disease and percutaneous coronary intervention: JACC Cardiovasc Interv, 2013; 6(3); 228-36
11. Bezerra HG, Attizzani GF, Costa MA, Three-dimensional imaging of fibrous cap by frequency-domain optical coherence tomography: Catheter Cardiovasc Interv, 2013; 81(3); 547-49
12. Thygesen K, Alpert JS, Jaffe AS, Fourth Universal Definition of Myocardial Infarction (2018): Circulation, 2018; 138(20); e618-e51
13. Killip T, Kimball JT, Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients: Am J Cardiol, 1967; 20; 457-64
14. Werns SW, Bates ER, The enduring value of Killip classification: Am Heart J, 1999; 137(2); 213-15
15. DeGeare VS, Boura JA, Grines LL, Predictive value of the Killip classification in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction: Am J Cardiol, 2001; 87(9); 1035-38
16. McLachlan C, Mossop P, Are elevations of N-terminal probrain natriuretic peptide in endurance athletes after prolonged strenuous exercise due to systemic inflammatory cytokines?: Am Heart J, 2006; 152(1); e1
17. Sawada T, Shite J, Garcia-Garcia HM, Feasibility of combined use of intravascular ultrasound radiofrequency data analysis and optical coherence tomography for detecting thin-cap fibroatheroma: Eur Heart J, 2008; 29(9); 1136-46
18. Stefano GT, Bezerra HG, Mehanna E, Unrestricted utilization of frequency domain optical coherence tomography in coronary interventions: Int J Cardiovasc Imaging, 2013; 29(4); 741-52
19. Prati F, Di Vito L, Biondi-Zoccai G, Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l’Infarto-Optimisation of Percutaneous Coronary Intervention (CLI-OPCI) study: EuroIntervention, 2012; 8(7); 823-29
20. Cervinka P, Spaček R, Bystroň M, Optical coherence tomography-guided primary percutaneous coronary intervention in ST-segment elevation myocardial infarction patients: A pilot study: Can J Cardiol, 2014; 30(4); 420-27
21. Higuma T, Soeda T, Yamada M, Coronary plaque characteristics associated with reduced TIMI (thrombolysis in myocardial infarction) flow grade in patients with ST-segment-elevation myocardial infarction: A combined optical coherence tomography and intravascular ultrasound study: Circ Cardiovasc Interv, 2016; 9(9); e003913
22. Ali ZA, Landmesser U, Maehara AILUMIEN IV Investigators, Optical coherence tomography-guided versus angiography-guided PCI: N Engl J Med, 2023; 389(16); 1466-76
23. Lawton JS, Tamis-Holland JE, Bangalore S, 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines: Circulation, 2022; 145(3); e4-17
24. Byrne RA, Rossello X, Coughlan JJESC Scientific Document Group, 2023 ESC Guidelines for the management of acute coronary syndromes: Eur Heart J, 2023 [Online ahead of print]
25. Lee WC, Chen HC, Fang HY, Comparison of different strategies for acute ST-segment elevation myocardial infarction with high thrombus burden in clinical practice: Symptom-free outcome at 1 year: Heart Lung, 2015; 44(6); 487-93
26. Lee WC, Fang CY, Chen HC, Aspiration thrombectomy and drug-eluting stent implantation decrease the occurrence of angina pectoris one year after acute myocardial infarction: Medicine (Baltimore), 2016; 95(17); e3426
Figures
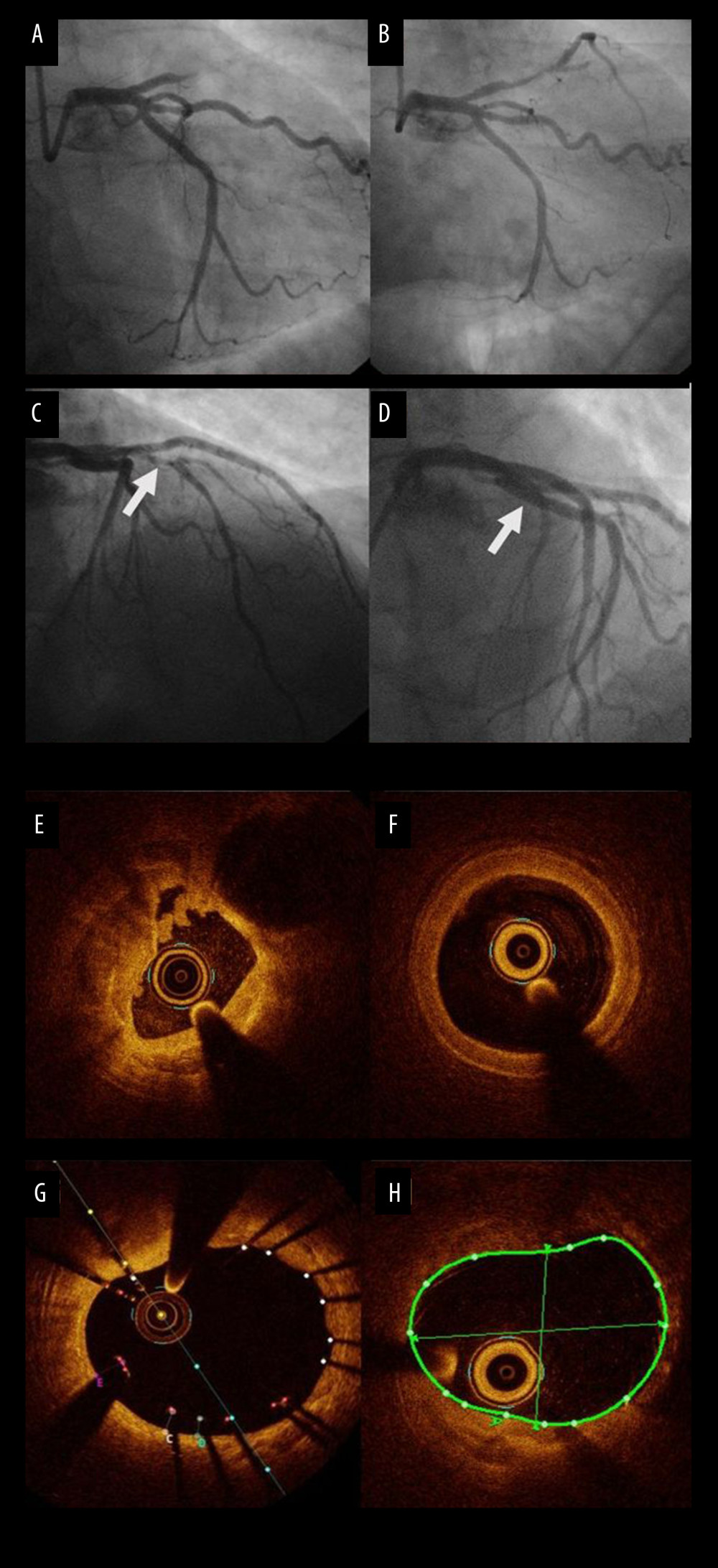 Figure 1. A 58-year-old woman presented with acute anterior wall ST elevation myocardial infarction. (A) the left coronary angiogram showed the culprit lesion thrombotic occlusion at proximal left anterior descending artery (LAD), with a right anterior oblique caudal view. (B) The left coronary angiogram after thrombus suction. (C) The arrow shows the culprit site after thrombus suction, with a right anterior oblique cranial view. (D) The arrow shows the result after drug-eluting stent (DES) and optical computed tomography (OCT)-guided percutaneous coronary intervention (PCI). (E) OCT finding at the culprit site, with much thrombus and minimal luminal area (MLA) only 1.9 mm2 after thrombus suction. (F) OCT finding at the LAD reference site, with MLA 4.7 mm2. (G) OCT finding at the culprit site after DES implantation. (H) OCT finding at the LAD reference site.
Figure 1. A 58-year-old woman presented with acute anterior wall ST elevation myocardial infarction. (A) the left coronary angiogram showed the culprit lesion thrombotic occlusion at proximal left anterior descending artery (LAD), with a right anterior oblique caudal view. (B) The left coronary angiogram after thrombus suction. (C) The arrow shows the culprit site after thrombus suction, with a right anterior oblique cranial view. (D) The arrow shows the result after drug-eluting stent (DES) and optical computed tomography (OCT)-guided percutaneous coronary intervention (PCI). (E) OCT finding at the culprit site, with much thrombus and minimal luminal area (MLA) only 1.9 mm2 after thrombus suction. (F) OCT finding at the LAD reference site, with MLA 4.7 mm2. (G) OCT finding at the culprit site after DES implantation. (H) OCT finding at the LAD reference site. Figure 2. Stepwise explanation of the study procedures and decision-making process. The procedural guidelines for the study are delineated in a stepwise manner, encompassing several critical criteria. Morphological assessment involved identifying high calcium plaque characterized by an arc exceeding 180 degrees, thickness over 0.5 mm, and length of more than 5 mm. Landing zones for interventions were selected based on the visualization of healthy tissue and the external elastic lamina. Diameter criteria required measuring the dimensions of the vessel, stent, and balloon, with reference measurements taken distally to select stent and distal balloon sizes, and proximally for proximal balloons. Significant medial dissections, defined as those penetrating the medial layer and extending beyond 1 quadrant arc, were promptly addressed. Apposition criteria involved rectifying gross malposition, noted when the separation from the vessel wall exceeded 3 mm. Finally, expansion criteria verified stent deployment, with over 80% expansion considered acceptable and beyond 90% regarded as optimal, ensuring precision and efficacy in the intervention process.
Figure 2. Stepwise explanation of the study procedures and decision-making process. The procedural guidelines for the study are delineated in a stepwise manner, encompassing several critical criteria. Morphological assessment involved identifying high calcium plaque characterized by an arc exceeding 180 degrees, thickness over 0.5 mm, and length of more than 5 mm. Landing zones for interventions were selected based on the visualization of healthy tissue and the external elastic lamina. Diameter criteria required measuring the dimensions of the vessel, stent, and balloon, with reference measurements taken distally to select stent and distal balloon sizes, and proximally for proximal balloons. Significant medial dissections, defined as those penetrating the medial layer and extending beyond 1 quadrant arc, were promptly addressed. Apposition criteria involved rectifying gross malposition, noted when the separation from the vessel wall exceeded 3 mm. Finally, expansion criteria verified stent deployment, with over 80% expansion considered acceptable and beyond 90% regarded as optimal, ensuring precision and efficacy in the intervention process. Tables
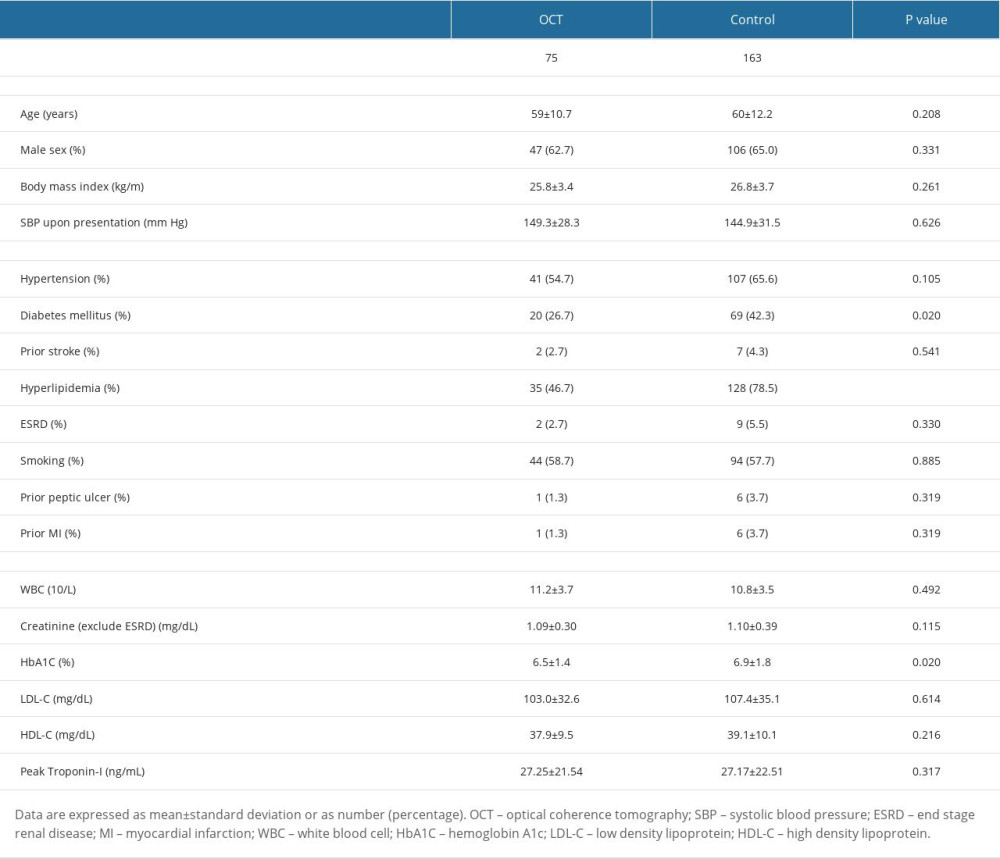 Table 1. Comparison of baseline characteristics between groups.
Table 1. Comparison of baseline characteristics between groups.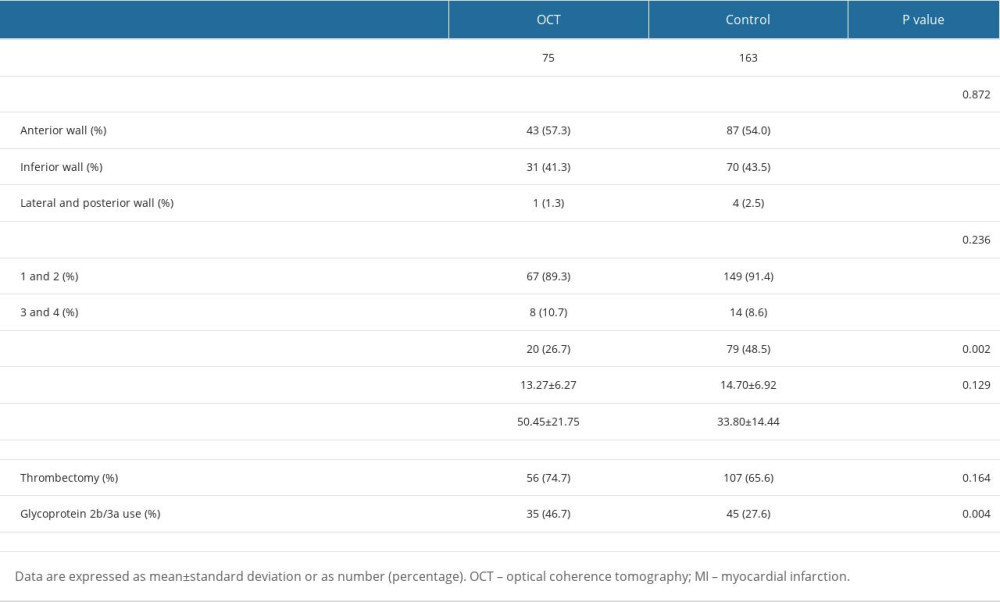 Table 2. Comparison of procedural characteristics between groups.
Table 2. Comparison of procedural characteristics between groups.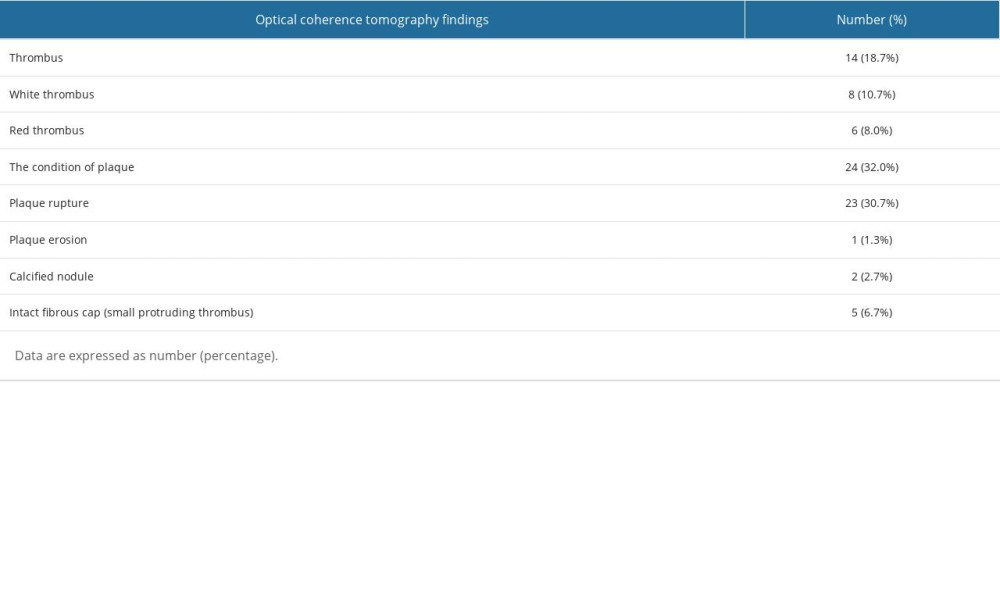 Table 3. The findings of optical coherence tomography.
Table 3. The findings of optical coherence tomography.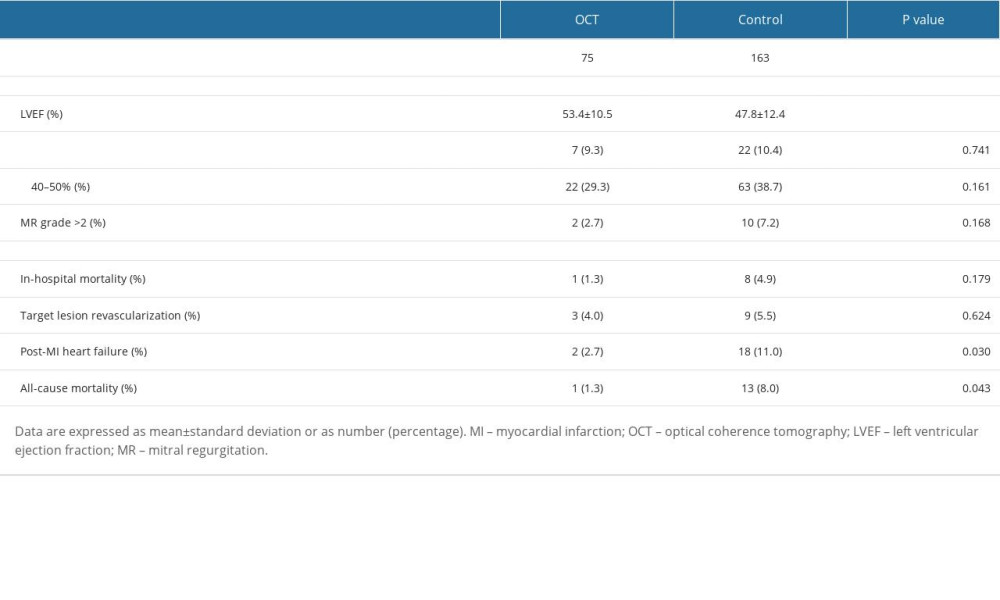 Table 4. Post-myocardial infarction echocardiographic parameters and 1-year follow-up clinical outcomes.
Table 4. Post-myocardial infarction echocardiographic parameters and 1-year follow-up clinical outcomes.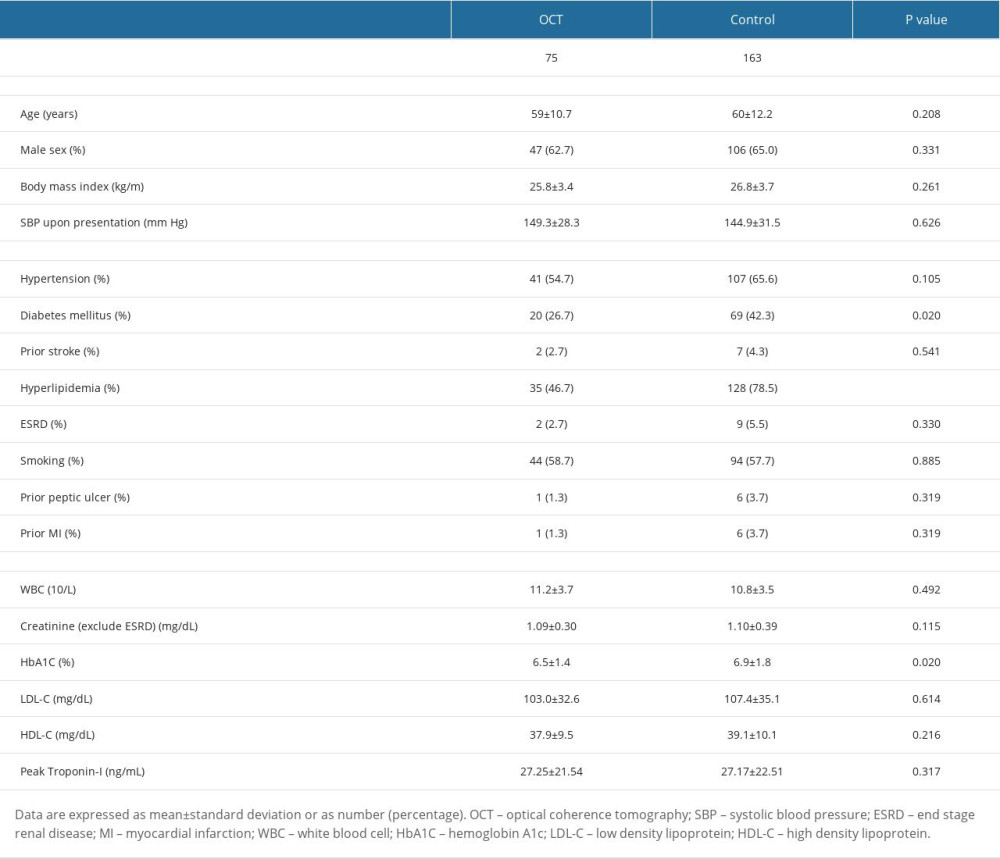 Table 1. Comparison of baseline characteristics between groups.
Table 1. Comparison of baseline characteristics between groups.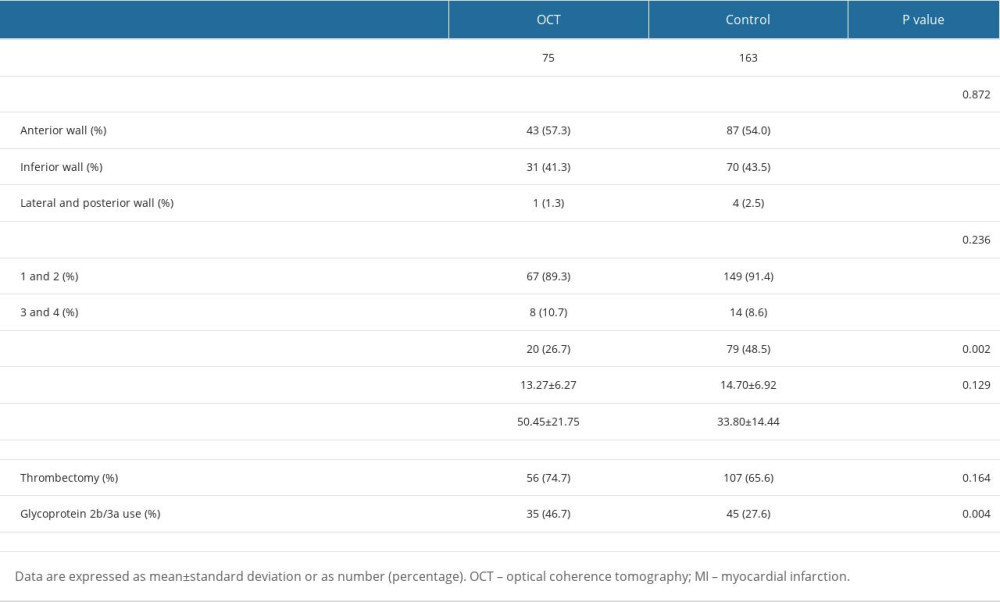 Table 2. Comparison of procedural characteristics between groups.
Table 2. Comparison of procedural characteristics between groups.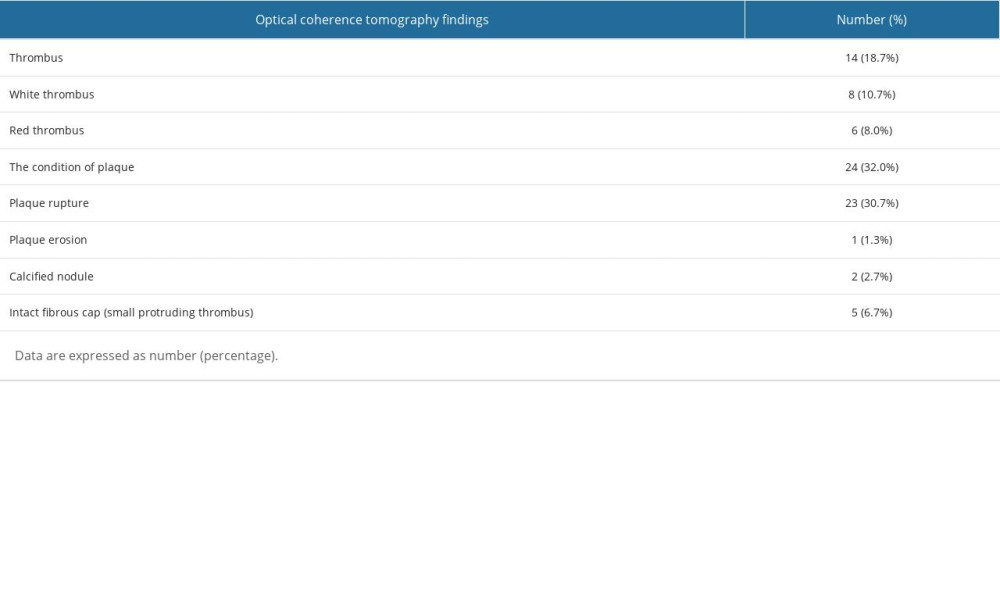 Table 3. The findings of optical coherence tomography.
Table 3. The findings of optical coherence tomography.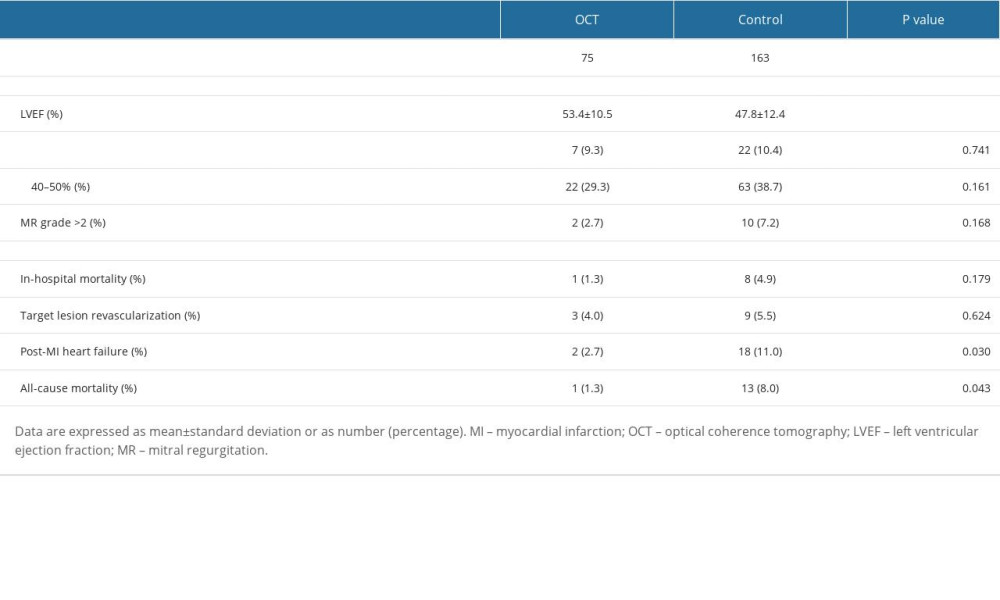 Table 4. Post-myocardial infarction echocardiographic parameters and 1-year follow-up clinical outcomes.
Table 4. Post-myocardial infarction echocardiographic parameters and 1-year follow-up clinical outcomes. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








