23 June 2020: Clinical Research
General Anesthesia Maintained with Sevoflurane versus Propofol in Pediatric Surgery Shorter Than 1 Hour: A Randomized Single-Blind Study
Guisheng Wu1ABCDE, Xia Xu1ABCD, Guanghua Fu1ABCD, Ping Zhang1AEF*DOI: 10.12659/MSM.923681
Med Sci Monit 2020; 26:e923681
Abstract
BACKGROUND: Sevoflurane was compared with propofol for general anesthesia maintenance in pediatric operations lasting less than 1 hour in terms of anesthetic effect and postoperative recovery.
MATERIAL AND METHODS: Children scheduled for inguinal hernia repair or hydrocele testis repair were randomly assigned to receive general anesthesia maintained with either sevoflurane (n=43) or propofol (n=43). The ilioinguinal nerve was blocked with 1% lidocaine (7 mg/kg) after intravenous administration of ketamine (2 mg/kg). At the end of the surgery in patients receiving sevoflurane, sevoflurane was stopped and a bolus of propofol of 1 mg/kg was administered.
RESULTS: Sevoflurane was associated with significantly less use of ketamine (35.1±10.6 mg) than was propofol (59.0±28.0 mg; P<0.001). In addition, sevoflurane was associated with a significantly shorter time in the post-anesthesia care unit (52.1±9.0 min) than was propofol (68.8±15.3 min; P<0.001). Propofol was associated with a significantly higher incidence of intraoperative body movement (33.3%) than was sevoflurane (13.5%; P=0.045). However, the 2 groups showed no important differences in other adverse events such as hypoxia, emergence agitation, and additional use of propofol.
CONCLUSIONS: In pediatric surgery lasting less than 1 hour, anesthesia maintained with sevoflurane was associated with significantly less use of ketamine, shorter postoperative recovery time, and less intraoperative body movement than was propofol.
Keywords: Anesthesia, general surgery, Hernia, Pediatrics, Propofol, Anesthesia Recovery Period, Anesthesia, General, Child, Child, Preschool, Hernia, Inguinal, Infant, Postoperative Period, sevoflurane, Single-Blind Method, Testicular Hydrocele
Background
Many pediatric operations, such as emergency appendectomy, high-level ligation of the inguinal sac, and ulnar fracture surgeries, are performed in a short time. These surgeries require fast and smooth anesthesia and relatively lower doses of muscle relaxants. Because of the young age of patients, these operations can be performed only with general anesthesia. However, general anesthesia often entails difficulties in establishing venous access, anesthesia induction, intraoperative airway management, and delay in postoperative awakening [1–4]. Therefore, selecting the proper anesthetic agent and anesthetic technique is critical for success in pediatric surgeries.
Propofol is a widely used intravenous anesthetic agent from which recovery is fast. It can be used for both induction and maintenance of anesthesia. However, it may cause hypotension and bradycardia if used at a high dose [5]. Propofol is often used with other anesthetic agents for general anesthesia in short pediatric operations. For example, intravenous anesthesia with remifentanil and propofol is used to do rigid bronchoscopy in children [6]. It has also been advised that the adjunctive use remifentanil can reduce the dose of propofol required during insertion of the laryngeal mask airway and laryngeal tube in pediatric patients [7, 8]. In addition, propofol has been proved to be associated with reduced risks of laryngospasm and apnea compared to sevoflurane [9].
Sevoflurane is the most often used inhalational agent for pediatric anesthesia. Its advantages are short induction, rapid postoperative recovery, and only mild irritation of the airway, and it is considered suitable for short pediatric operations. However, anesthesia with sevoflurane in children is associated with increased risk of postoperative emergence agitation, with an estimated incidence of approximately 10% [10]. Also known as emergence delirium, emergence agitation is a disturbance of consciousness during recovery time from general anesthesia and includes hallucinations, delusions, and confusion. It has been shown that use of propofol after sevoflurane anesthesia or anesthesia maintenance with propofol after sevoflurane induction can lessen the incidence of sevoflurane-associated adverse events, including emergence agitation [11,12].
The purpose of our study was to compare the anesthetic effect and postoperative recovery of sevoflurane with those of propofol for general anesthesia in short pediatric operations.
Material and Methods
PATIENTS:
This single-center, randomized, single-blind study was conducted from August 1, 2018, to August 31, 2018, at our hospital. Our study was approved by the ethics committee of our hospital (approval number: 2018032). Written informed consent was obtained from the parents of each patient. The study was registered at
The inclusion criteria were as follows: age between 6 months and 12 years; weight between 5 and 30 kg; American Society of Anesthesiologists physical status classification I; and being scheduled for inguinal hernia or hydrocele testis repair with an estimated surgical time of less than 60 min. Patients with the following conditions were excluded: allergy to sevoflurane or propofol; upper respiratory infection in the preceding 2 weeks; and use of sedatives or analgesics in the preceding 2 weeks.
ANESTHESIA PROTOCOL:
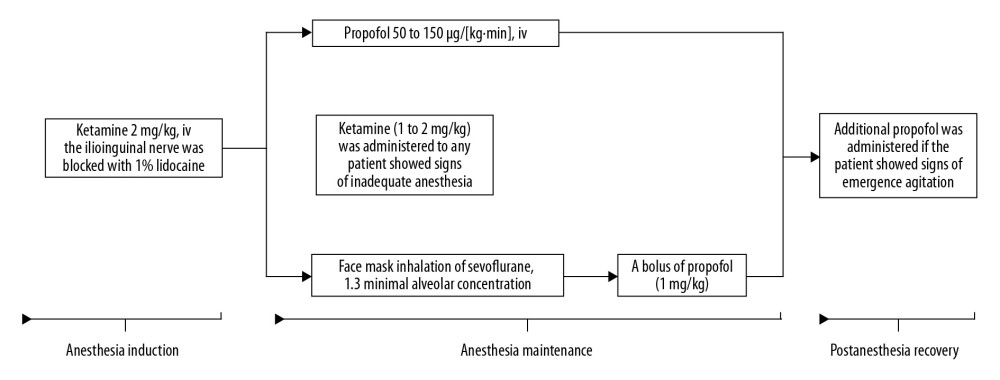
Preoperatively, food was not allowed for 6 to 8 hours, and fluid was not allowed for 2 hours. Atropine (0.02 mg/kg) and diazepam (0.1 mg/kg) were injected intramuscularly. The ilioinguinal nerve was blocked with 1% lidocaine (7 mg/kg) after intravenous administration of ketamine (2 mg/kg) for anesthesia induction. Patients were randomly assigned to receive general anesthesia maintained with intravenous propofol (propofol group) or facemask inhalation of sevoflurane (sevoflurane group) (Figure 1). The investigators alone were aware of which protocol the patients received. For anesthesia with sevoflurane, 3% sevoflurane (1.3 minimal alveolar concentration) was inhaled through a facemask without intubation. At the end of the surgery, sevoflurane was stopped, and a bolus of propofol (1 mg/kg) was administered. For anesthesia with propofol, propofol (50 to 150 μg/[kg·min]) was intravenously administered until the end of the surgery. Ketamine (1 to 2 mg/kg) was administered to any patient who showed signs of inadequate anesthesia, like body movement. During the recovery, additional propofol was administered if the patient showed signs of emergence agitation.
PATIENT ASSESSMENT:
Heart rate and blood pressure were constantly monitored. The doses of anesthetic agents were recorded. Intraoperative hypoxia (oxygen saturation <95%), intraoperative body movement, and postoperative emergence agitation were documented. Intraoperative body movement was defined as flexion movement in one or more limbs or head shaking immediately after skin incision, but did not include frowning, coughing, or swallowing. Emergence agitation was defined as manifestations such as crying, restlessness, irritability, and disorientation.
STATISTICAL ANALYSIS:
The mean recovery times of children after inguinal hernia or hydrocele testis repair at our hospital were 57±20 minutes for sevoflurane and 72±25.2 minutes for propofol. The ratio of sevoflurane anesthesia to propofol anesthesia was 1: 1, with α=0.05 and 1–β=90%. The minimal sample number required was 36 per group. Under the assumption that the dropout rate was 20%, the final sample size was 43 patients per group, and the total sample number was 86.
Normality of the continuous data assessed by the Kolmogorov-Smirnov test. Continuous data were calculated as means and standard deviations. Categorical data were calculated as frequencies or percentages. Comparisons were made with the independent-sample
Results
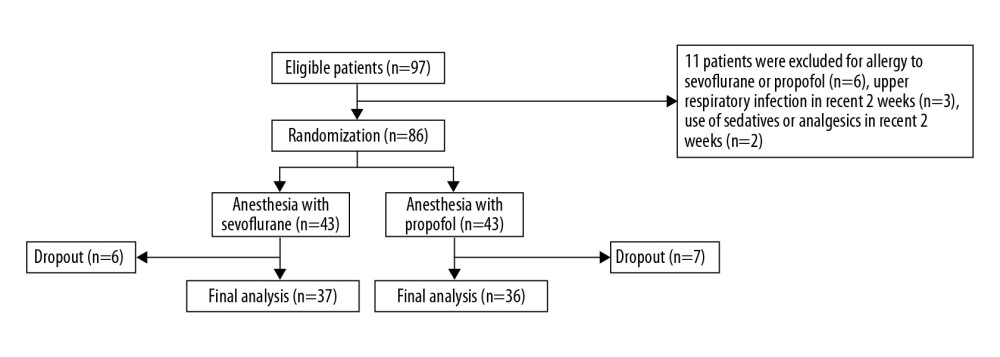
The patient inclusion process is illustrated in Figure 2. There was no obvious difference in the demographic and clinical characteristics between the sevoflurane recipients and the propofol recipients (Table 1). The propofol recipients had generally higher intraoperative and postoperative blood pressure and heart rate than did the sevoflurane recipients, but their values were still within the normal range and constitute no clinical concerns (Table 2). Sevoflurane was associated with significantly less use of ketamine (35.1±10.6 mg) than was propofol (59.0±28.0 mg;
Discussion
We found that in pediatric operations shorter than 1 hour, general anesthesia maintained with sevoflurane was associated with significantly less use of ketamine, shorter postoperative recovery time, and less intraoperative body movement than was propofol. Anesthesia with sevoflurane or propofol produced no significant difference in hypoxia, postoperative agitation, or the requirement for additional propofol.
It has been shown that transition to propofol at the end of anesthesia with sevoflurane may reduce the incidence, duration, and severity of emergence agitation [13]. A meta-analysis showed that a prophylactic bolus of propofol (1 mg/kg) after anesthesia with sevoflurane can prevent emergence agitation without a significant increase in adverse events [14]. In our study, a bolus of propofol (1 mg/kg) was also used prophylactically after anesthesia with sevoflurane. We discovered no obvious difference in the incidence of emergence agitation between patients anesthetized with sevoflurane and those anesthetized with propofol. In consideration of the reported risk of emergence agitation associated with sevoflurane, our findings suggest that prophylactic use of propofol is effective and safe for reducing the incidence of emergence agitation after anesthesia with sevoflurane.
In this study, the hemodynamic parameters were not obviously different between patients anesthetized with sevoflurane and those anesthetized with propofol. The incidence of hypoxia, emergence agitation, and need for additional postoperative propofol was not significantly different between the 2 groups. Significantly less ketamine was used with sevoflurane than with propofol. This finding might be due to the greater anesthetic effect of sevoflurane. Sevoflurane induces anesthesia rapidly, postoperative recovery is fast, the depth of anesthesia is adjustable, and the drug produces the same effects as a muscle relaxant [15]. All these features of sevoflurane resulted in less disturbance to hemodynamics and thus less body movement; therefore, the need for additional ketamine was reduced. With intravenous administration of ketamine (2 mg/kg), the effects can be maintained for 10 to 15 minutes. After ketamine use, it takes 15 to 30 minutes after the procedure for orientation to be restored and 0.5 to 1 hour for the patient to awaken completely. Therefore, the higher doses of ketamine used in the propofol recipients might explain the significantly longer time for postoperative recovery in this group.
Hypoxia may be caused by laryngospasms, which is associated with the use of anesthetic agents. It has been shown that propofol is associated with reduced risks of laryngospasm and apnea compared to sevoflurane [9]. In our study, propofol was used for anesthesia maintenance in the propofol group. In the sevoflurane group, propofol was used at the end of the surgery as a bolus injection, and during the recovery time for patients with signs of emergence agitation. The parallel use of propofol during the anesthesia recovery time might have reduced the difference in the incidence of postoperative hypoxia between the 2 groups.
This study has certain limitations. First, the investigators were aware of the anesthetic protocol and patient assignment, which may have introduced bias in patient evaluation. Second, the patients were not followed up postoperatively, and the long-term effect of the studied anesthetic agents on patient cognition and behavior was not evaluated.
Conclusions
General anesthesia maintained with sevoflurane is a reasonable alternative to propofol for short pediatric surgeries. It can reduce the dose of ketamine, postoperative recovery time, and the incidence of intraoperative body movement compared to propofol.
References
1. Davidson AJ, Morton NS, Arnup SJ, Apnea after awake regional and general anesthesia in infants: The general anesthesia compared to spinal anesthesia study – comparing apnea and neurodevelopmental outcomes, a randomized controlled trial: Anesthesiology, 2015; 123(1); 38-54
2. Lee HH, Milgrom P, Starks H, Burke W, Trends in death associated with pediatric dental sedation and general anesthesia: Paediatr Anaesth, 2013; 23(8); 741-46
3. Scheiermann P, Herzog F, Siebenhofer A, Intravenous versus inhalational anesthesia for pediatric inpatient surgery – A systematic review and meta-analysis: J Clin Anesth, 2018; 49; 19-25
4. Zhang Q, Peng Y, Wang Y, Long-duration general anesthesia influences the intelligence of school age children: BMC Anesthesiol, 2017; 17(1); 170
5. Erdman MJ, Doepker BA, Gerlach AT, A comparison of severe hemodynamic disturbances between dexmedetomidine and propofol for sedation in neurocritical care patients: Crit Care Med, 2014; 42(7); 1696-702
6. Bakan M, Topuz U, Umutoglu T, Remifentanil-based total intravenous anesthesia for pediatric rigid bronchoscopy: Comparison of adjuvant propofol and ketamine: Clinics (Sao Paulo), 2014; 69(6); 372-77
7. Park HJ, Lee JR, Kim CS, Remifentanil halves the EC50 of propofol for successful insertion of the laryngeal mask airway and laryngeal tube in pediatric patients: Anesth Analg, 2007; 105(1); 57-61
8. Kwak HJ, Kim JY, Kim YB, The optimum bolus dose of remifentanil to facilitate laryngeal mask airway insertion with a single standard dose of propofol at induction in children: Anaesthesia, 2008; 63(9); 954-58
9. Oberer C, von Ungern-Sternberg BS, Frei FJ, Erb TO, Respiratory reflex responses of the larynx differ between sevoflurane and propofol in pediatric patients: Anesthesiology, 2005; 103(6); 1142-48
10. Kotwani MB, Malde AD, Comparison of maintenance, emergence and recovery characteristics of sevoflurane and desflurane in pediatric ambulatory surgery: J Anaesthesiol Clin Pharmacol, 2017; 33(4); 503-8
11. Kim SH, Hong JY, Suk EH, Optimum bolus dose of propofol for tracheal intubation during sevoflurane induction without neuromuscular blockade in children: Anaesth Intensive Care, 2011; 39(5); 899-903
12. Siddik-Sayyid SM, Taha SK, Aouad MT, Propofol 2 mg/kg is superior to propofol 1 mg/kg for tracheal intubation in children during sevoflurane induction: Acta Anaesthesiol Scand, 2011; 55(5); 535-38
13. Costi D, Ellwood J, Wallace A, Transition to propofol after sevoflurane anesthesia to prevent emergence agitation: A randomized controlled trial: Paediatr Anaesth, 2015; 25(5); 517-23
14. van Hoff SL, O’Neill ES, Cohen LC, Collins BA, Does a prophylactic dose of propofol reduce emergence agitation in children receiving anesthesia? A systematic review and meta-analysis: Paediatr Anaesth, 2015; 25(7); 668-76
15. Rhondali O, Andre C, Pouyau A, Sevoflurane anesthesia and brain perfusion: Paediatr Anaesth, 2015; 25(2); 180-85
Figures
Tables
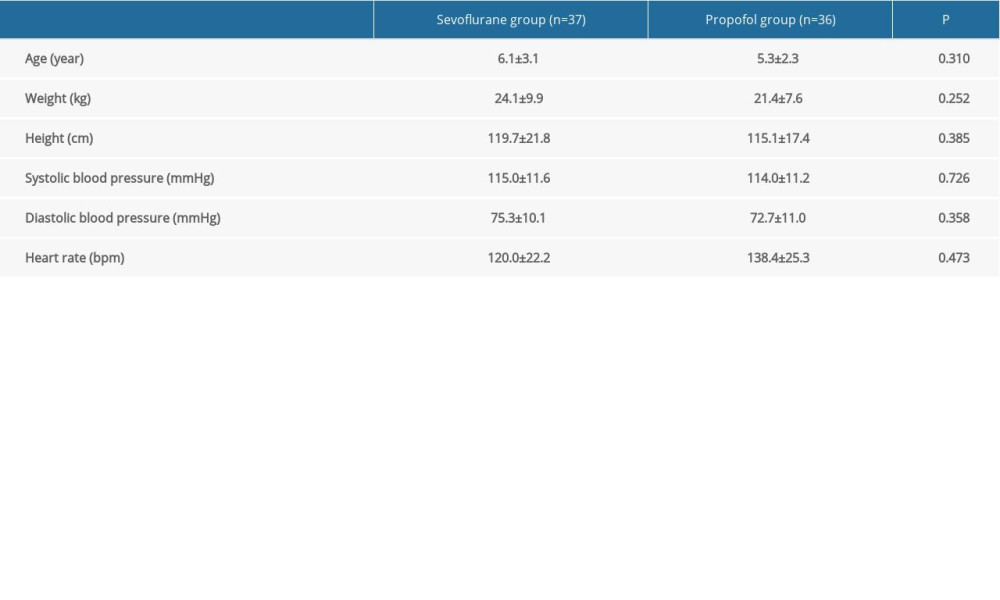 Table 1. Demographic and clinical characteristics of the patients at baseline.
Table 1. Demographic and clinical characteristics of the patients at baseline.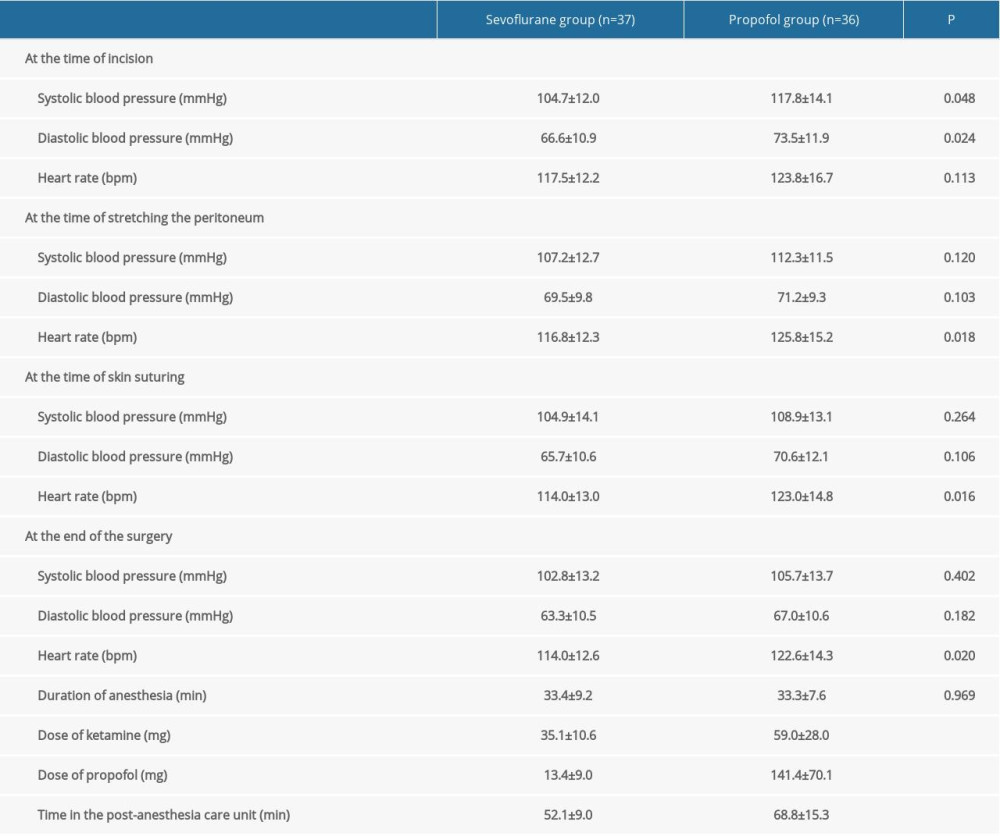 Table 2. Intraoperative and postoperative hemodynamics.
Table 2. Intraoperative and postoperative hemodynamics. Table 3. Intraoperative and postoperative adverse events.
Table 3. Intraoperative and postoperative adverse events.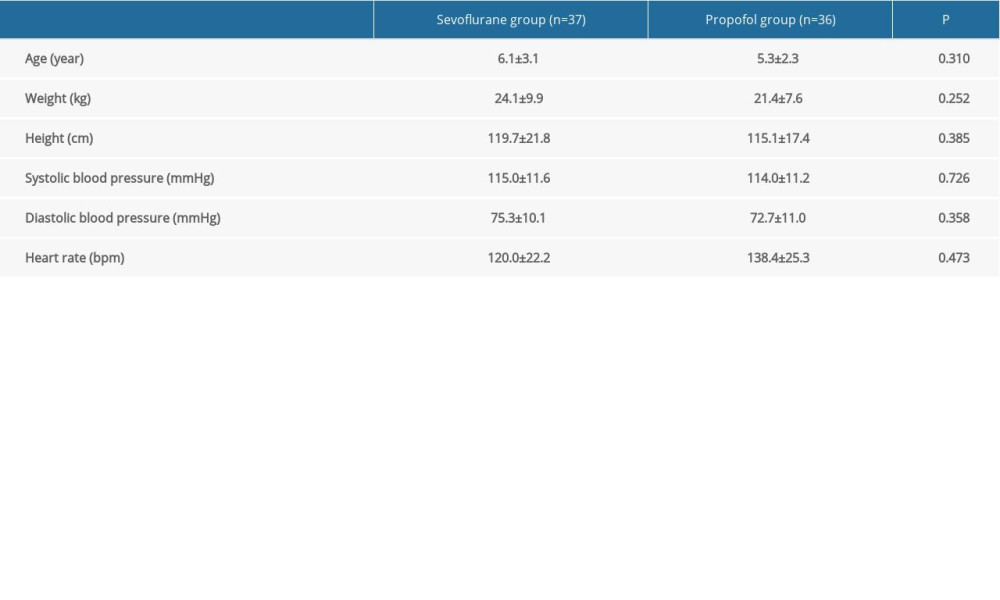 Table 1. Demographic and clinical characteristics of the patients at baseline.
Table 1. Demographic and clinical characteristics of the patients at baseline.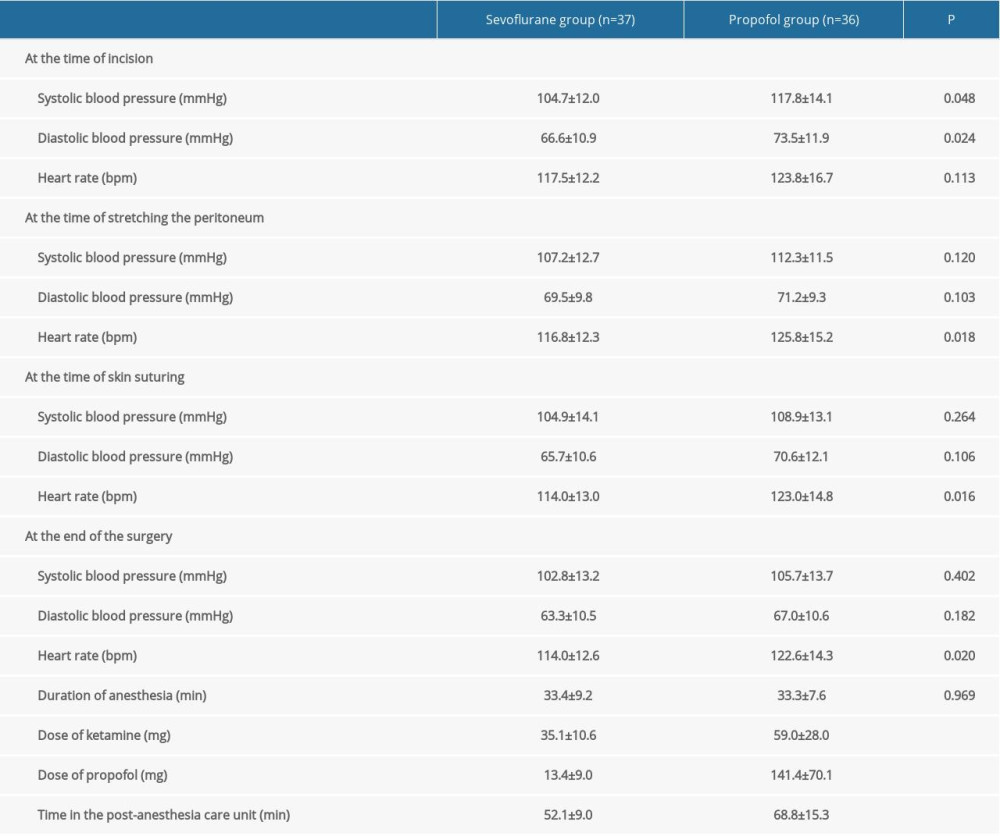 Table 2. Intraoperative and postoperative hemodynamics.
Table 2. Intraoperative and postoperative hemodynamics. Table 3. Intraoperative and postoperative adverse events.
Table 3. Intraoperative and postoperative adverse events. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952