06 November 2020: Clinical Research
A Comparison of 2 Anterior Hybrid Techniques for 3-Level Cervical Degenerative Disc Disease
Han Wang1BCE, Yang Meng1DF, Hao Liu1A*, Xiaofei Wang1C, Chen Ding1FDOI: 10.12659/MSM.927972
Med Sci Monit 2020; 26:e927972
Abstract
BACKGROUND: Novel hybrid surgical techniques that incorporate anterior cervical discectomy and fusion with total disc replacement are widely used. Based on the number of implanted discs, 3-level hybrid surgery can be classified as single fusion combined with double replacement and single replacement combined with double fusion. Few studies to date have directly compared these hybrid techniques. The present study compared the clinical and radiological outcomes of these methods and assessed their characteristics and benefits.
MATERIAL AND METHODS: Clinical and radiological outcomes were retrospectively evaluated in 64 consecutive patients who underwent 3-level hybrid surgery by single fusion combined with double replacement or single replacement combined with double fusion.
RESULTS: Significant differences between the 2 groups were observed in postoperative range of motion of C2–C7. C2–C7 cervical lordosis assessed preoperatively and at final follow-up differed significantly in patients who underwent single replacement combined with double fusion. This group showed a higher incidence of heterotopic ossification than patients who underwent double replacement combined with single fusion.
CONCLUSIONS: Both types of hybrid surgery are safe and effective in treating 3-level cervical degenerative disc diseases. Single replacement combined with double fusion showed greater accuracy in correcting cervical lordosis, but was associated with a higher incidence of heterotopic ossification. In contrast, single fusion combined with double replacement was superior in maintaining cervical range of motion.
Keywords: intervertebral disc degeneration, Ossification, Heterotopic, Spinal Fusion, Total Disc Replacement, Cervical Vertebrae, Diskectomy, Neck Pain, Observer Variation, Postoperative Complications, Range of Motion, Articular, visual analog scale
Background
Cervical degenerative disc disease (CDDD) is a radiologically diagnosed condition characterized by the protrusion of intervertebral discs and osteophytes at the posterior borders of the vertebrae. This disease can lead to compression of the dural sac or spinal cord. Although non-surgical methods are generally preferred for patients with single-level disease or mild symptoms [1], surgical treatment is regarded as more effective for multilevel CDDD, which is associated with more complex characteristics and more severe symptoms [2,3]. A novel hybrid surgery (HS) technique, involving anterior cervical discectomy and fusion (ACDF) and total disc replacement (TDR), is thought to have the advantages of both, resulting in achievement of motion function and solid fusion. Patients are rigorously evaluated preoperatively to determine the degree of degeneration at each surgical level, followed by the performance of the most suitable surgical procedure for each surgical level. Based on the number of implanted discs, 3-level HS can be classified as single fusion combined with double replacement (1F2R) or single replacement combined with double fusion (1R2F).
HS has been reported similar to TDR and superior to ACDF for contiguous 2-level CDDD [4,5]. The fusion segment cephalic or caudal to the arthroplasty level was found to have no effect on the clinical outcomes of TDR in patients undergoing bi-level HS [6]. Questions have been raised, however, regarding 3-level HS, including whether patients who undergo 1R2F surgery experience postoperative hypermobility; whether the 1F2R operation can effectively preserve the range of motion (ROM) of the cervical spine; and whether arthrodesis can achieve solid fusion under the influence of the replacement level. Most previous studies have compared HS with ACDF or TDR, with few studies directly comparing clinical outcomes in patients who have undergone different hybrid techniques. The present study therefore compared clinical and radiological outcomes in patients who underwent 1F2R and 1R2F HS surgery and explored the characteristics and benefits of both operations.
Material and Methods
PATIENT DATA:
This retrospective case-control study enrolled 64 patients with 3-level CDDD who underwent continuous 3-level HS between July 2012 and July 2018. Patients were included if they: (1) had symptoms consistent with compression of the spinal cord or nerve roots; (2) had been clearly diagnosed with 3-level cervical myelopathy and/or radiculopathy by cervical X-ray examination, computed tomography (CT) scanning, magnetic resonance imaging (MRI), and physical examination; (3) were refractory to conservative treatment for more than 6 weeks; and (4) had undergone 3-level HS including TDR and ACDF. Patients were excluded if they: (1) had undergone previous cervical spine surgery; (2) had cervical trauma, infection, a tumor, or severe osteoporosis; (3) were followed up for less than 12 months; or (4) had insufficient X-ray, CT, or MRI data at any follow-up point. The study protocol was approved by the local medical ethics committee, which waived the requirement for informed consent because of the retrospective nature of this study.
SURGICAL DECISION:
The choice of 3-level hybrid technique was determined by comprehensively assessing the specific surgical indications and condition of each patient. TDR was preferred because it is closer to a physiological state. TDR was indicated for vertebral levels without sagittal plane translation >3 mm or sagittal plane angulation >11°; without a <2° absence of motion; without a disc height loss >50%; and without facet joint degeneration, bridge osteophytes, or instability. ACDF was performed at vertebral levels that did not fulfill these criteria.
SURGICAL PROCEDURES:
Following induction of general anesthesia, the patient was placed in a supine position with a cushion under the neck to maintain the normal lordosis of the cervical spine. A classical Robinson-Smith approach was adopted, and a transverse incision was made on the right side of the neck. The soft tissue was pulled to both sides and the targeted disc tissue and longitudinal ligament were removed. Surgery was performed initially on the most severely damaged level to avoid the potential risk of spinal cord injury due to the operation. The bilateral foramen and uncovertebral joints were also decompressed completely. The endplates were burred to expose the cortical endplate surface, followed by placement of a Prestige-LP artificial cervical disc (Medtronic Sofamor Danek, Memphis, TN) and use of the Zero-P system (Synthes, Oberdorf, Switzerland). The intervertebral space was filled with an appropriate provisional implant. TDR was performed before ACDF, whereas, for continuous 2-level TDR, the cephalic level underwent TDR first, because tapping during the implantation of a Prestige-LP may risk prosthesis migration and screw loosening [7]. Generally, surgery was performed so as not to increase the degree of spinal cord compression and not to affect the instability of the implanted discs.
OUTCOME EVALUATION:
Clinical characteristics of all involved patients were collected, including levels of surgery, intraoperative blood loss, hospital stay, hospitalization costs, and follow-up duration. Neurological status and pain intensity were assessed using the Japanese Orthopaedic Association (JOA) disability and visual analogue scale (VAS). The JOA recovery rate was calculated as: (postoperative score–preoperative score)/(17–preoperative score)×100% [8]. Scores of ≥75%, 50% to 74%, 25% to 49%, and <25% were graded as excellent, good, fair, and poor, respectively.
Radiological outcomes included cervical lordosis and ROM. Cervical lordosis was defined as the Cobb angle of C2–C7, which was determined by measuring the angle between the 2 lines drawn separately at the inferior endplate of C2 and C7 in the neutral X-ray view, with positive and negative angles regarded as lordosis and kyphosis, respectively. ROM was defined as the difference in Cobb angles at the extension and flexion positions on X-ray film. Segmental ROM was determined by measuring the line between the superior endplate of the cephalic vertebral body and the inferior endplate of the caudal vertebral body. Solid fusion was defined as a <3° ROM at the fusion level, with bridge osteophytes present at the posterior margin of the cage on CT scans. Heterotopic ossification (HO) was determined according to the McAfee classification, and dysphagia was quantified using the Bazaz scoring system. Also evaluated were reoperation rates and the frequencies of other complications [9,10].
STATISTICAL ANALYSIS:
All measurements were taken by 2 spine surgeons independently. Correlations were calculated using Spearman’s correlation coefficient. Quantitative data were presented as the mean±standard deviation, with differences between the 2 groups compared by independent sample
Results
PATIENT CHARACTERISTICS:
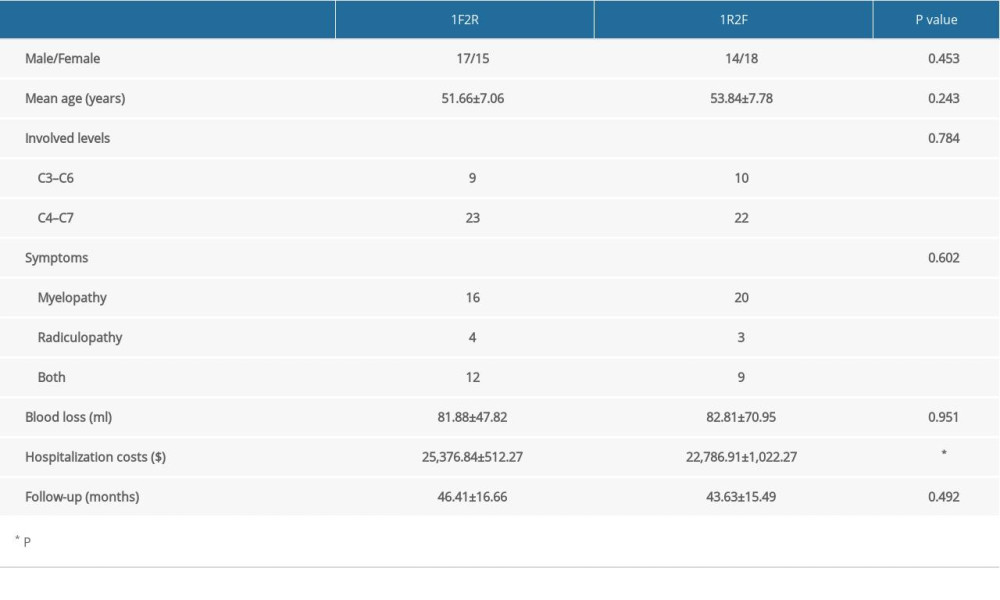
Of the 64 patients enrolled in this study, 32 underwent 1F2R and 32 underwent 1R2F HS (Figures 1, 2). Baseline characteristics in these 2 groups, including male-to-female ratio, average age, involved levels, clinical symptoms, blood loss, and follow-up period, did not differ significantly (Table 1), whereas hospitalization costs differed significantly in these 2 groups.
JOA SCORES AND RECOVERY RATE:
The JOA scores improved significantly in both groups, but the differences between the 2 groups was not statistically significant. The JOA recovery rates in the 1F2R and 1R2F groups were 76.47% and 76.09%, respectively, indicating excellent recovery.
VAS SCORES:
Pain VAS scores did not differ significantly in these 2 groups at any follow-up point. VAS scores over time decreased to satisfactory levels in both groups.
INTER-OBSERVER RELIABILITY:
Assessments of the inter-observer reliability based on radiological data showed that Spearman’s correlation coefficients for cervical lordosis and ROM of C2–C7 were 0.87 and 0.79, respectively, whereas Spearman’s correlation coefficients for replacement, fusion, and adjacent levels were 0.83, 0.88, and 0.86, respectively. Inter-observer reliability was deemed satisfactory, and the mean values determined by the 2 observers were used in the analysis.
C2–C7 CERVICAL LORDOSIS:
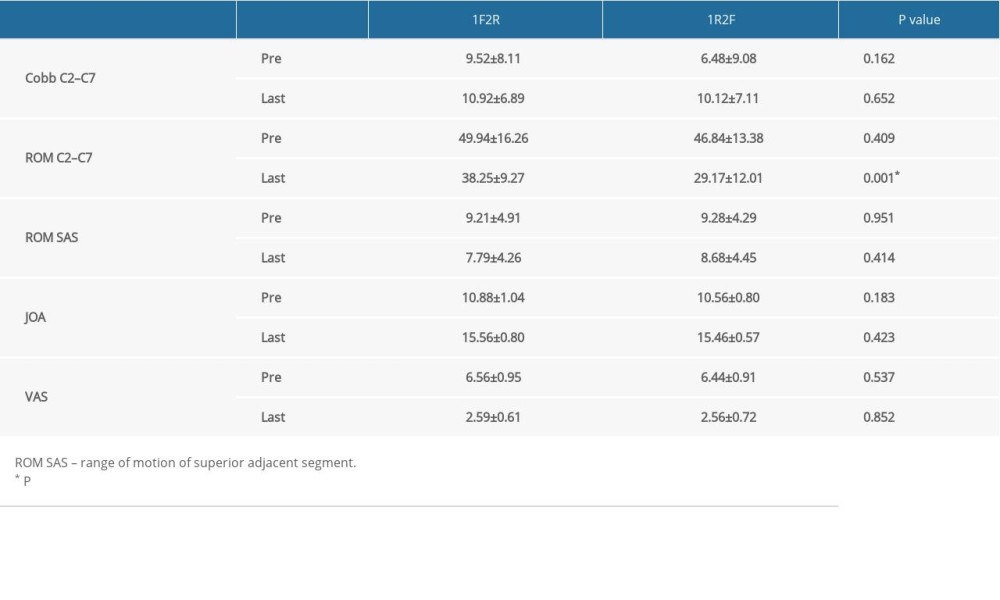
C2–C7 cervical lordosis was slightly higher in the 1F2R than in the 1R2F group. Postoperative and preoperative C2–C7 cervical lordosis differed significantly in the 1R2F group (
C2–C7 ROM:
Postoperative ROM of C2–C7 was significantly lower than preoperative ROM in both the 1F2R (
ROM OF REPLACEMENT LEVEL:
The ROM of replacement levels in both groups was lower than at baseline, but there were no significant differences between the 2 groups. Similar results were observed for the upper and lower levels in the 1F2R group.
FUSION RATE:
The ROM of fusion level in both groups was significantly lower at follow-up than at baseline. The fusion rates in the 1F2R and 1R2F groups were 93.75% and 89.06%, respectively. The 2 groups achieved completely solid fusion at the final follow-up, with no significant differences between them or between the superior and inferior fusion levels in the 1R2F group.
ROM OF SUPERIOR ADJACENT LEVEL: The ROM of the superior adjacent level was slightly lower at final follow-up than at baseline in both groups, with the difference in the 1F2R group being statistically significant (P=0.043). In contrast, there were no significant between-group differences at final follow-up. Clinical and radiological outcomes are summarized in Table 2.
COMPLICATIONS:
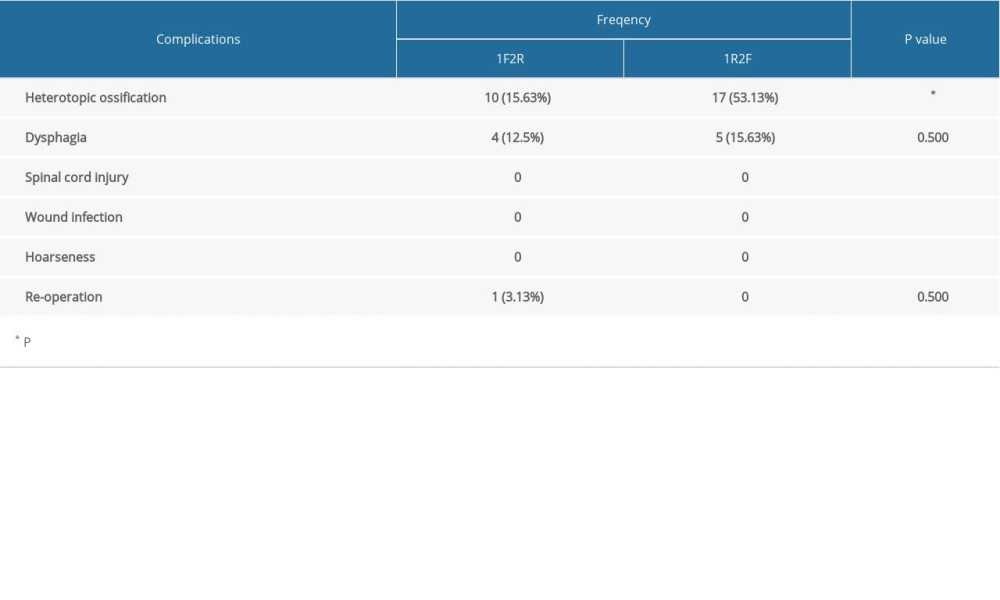
HO was observed in 10 segments in the 1F2R group, including severe HO at level III or IV in 2 segments based on the classical McAfee classification. Of 17 segments with HO in the 1R2F group, only 1 segment showed severe HO. Another patient underwent reoperation for CDDD at level IV 5 years after the first operation. Dysphagia was observed in 4 and 5 patients in the 1F2R and 1R2F groups, respectively; these symptoms gradually disappeared over the next 6 months. None of the patients in either group showed signs of spinal cord injury, wound infection, or hoarseness (Table 3).
Discussion
Based on the status of the target level, multilevel HS can provide the most appropriate surgical approach. Theoretically, appropriate arthroplasty and arthrodesis levels can be achieved through enhanced mobility and solid fusion, respectively. This can optimize postoperative ROM, improving patient quality of life. Satisfactory clinical outcomes after 5 years were first observed in 2004 in a patient who had undergone 4-level HS [11,12]. A case series in 2009 involving 7 patients with 3-level CDDD and 2 with 4-level CDDD described the surgical selection criteria and the suitability of a hybrid technique with fusion and non-fusion in the treatment of symptomatic multilevel CDDD [13]. Several subsequent studies have focused on multilevel HS with fusion and non-fusion. For example, postoperative ROM was higher and time to return to work was shorter following HS than ACDF, whereas functional outcomes did not differ in patients who underwent HS and TDR [14]. In addition, HS showed better outcomes than ACDF in the treatment of 3-level CDDD, as shown by NDI, cervical ROM, fusion rate, and rates of postoperative complications and ASD [15]. Similarly, multilevel HS improved operation time, blood loss, and cervical ROM compared with ACDF [16]. HS also resulted in less compromised ROM and a lower impact at adjacent levels than long-fusion surgery [17]. These findings suggested the need to compare the clinical and radiological outcome of 1F2R and 1R2F and to assess the characteristics and benefits of both.
This study showed that clinical outcomes were satisfactory in both groups of patients. In addition, JOA and VAS scores improved significantly in both groups at the final follow-up. ACDF has been shown to provide good alignment and TDR to improve cervical ROM [18]. However, few studies have shown that arthroplasty is superior in maintaining cervical alignment [19]. For example, TDR did not significantly improve sagittal profiles when compared with other cervical fusion techniques and is therefore not considered a lordosis-producing operation [20]. This study showed similar outcomes. In particular, because 1R2F involves fusion at more levels, it was superior to 1F2R in correcting global lordosis. Conversely, because 1F2R involves the implantation of more artificial cervical discs, it was superior to 1R2F in improving postoperative ROM. Additionally, Prestige-LP kinematic analysis showed that there was a loss of lordosis at the target level because the disc endplates have an almost parallel configuration [21], suggesting that 1R2F may be superior to 1F2R in correcting cervical lordosis. Furthermore, the ROM at the replacement level did not differ significantly in the 1R2F and 1F2R groups, despite implantation of an additional disc, suggesting that postoperative ROM would be greater in the 1F2R group. A previous study found that the overall success rate was 79.4%, based on success being defined as ROM >4° [22]. In the present study, the success rates were 78.13% in the 1R2F group and 79.69% in the 1F2R group, comparable to previous findings. Although several studies reported that 3-level TDR had satisfactory clinical outcomes, TDR was mostly performed at a single level. Because only Prestige-LP and Mobi-C have been approved for 2-level CDDD, assessment of the safety and efficacy of 3-level HS techniques requires more long-term data for validation [23–25].
TDR also plays an important role in slowing the degeneration of segments adjacent to the operated levels. However, several studies have demonstrated that non-fusion surgery cannot reduce the incidence of ASD [26–28]. The present study found that there was no compensatory increase in ROM in the superior adjacent level, which seemed to be an advantage of multilevel HS. The fusion rate achieved with different surgical procedures is clinically important. The Zero-P device was recommended due to a low dysphagia rate, but the fusion rate could not be determined due to the lack of a traditional anterior plate. Several studies have shown that the Zero-P system can achieve similar clinical and radiological improvements as a traditional plate and cage in single-level CDDD [29–31]. Although fusion rates have been reported to decline as the number of target levels increased, satisfactory fusion rates were also achieved for multilevel ACDF [32,33]. Reports using stand-alone devices showed fusion rates >90% [34–36]. In the present study, the 1-year fusion rates were 89.06% and 93.75% in the 1R2F and 1F2R groups, respectively. At last follow-up, bridge osteophytes were observed in all fusion segments, while the artificial cervical disc did not appear to affect fusion levels, in agreement with our previous findings [6].
The costs of these 2 types of operation are of key importance, both to patients and spinal surgeons. TDR is more cost-effective than ACDF in patients with double-level cervical disc disease [37], as well as being more cost-effective after 7 years of follow-up [38]. Two-level TDR and ACDF are both cost-effective strategies, particularly over the long term [39,40]. Although the present study found that outcomes differed significantly in the 2 groups, the gap between them seemed to be clinically insignificant. Although the Prestige-LP artificial disc is more expensive than the Zero-P device, 1F2R hybrid surgery costs only 11.37% more than 1R2F. Thus, for 3-level CDDD, the economic factor may not be a major obstacle to additional artificial discs. However, the rehabilitation costs after discharge from the hospital and the indirect costs associated with the treatment were not considered due to the absence of follow-up data. Long-term studies are needed to compare the cost-effectiveness of these hybrid procedures for 3-level surgery.
HO is one of the major obstacles to TDR. The present study showed that the incidence of HO was much higher in the 1R2F group than in the 1F2R group. Based on the statistical analysis, the higher incidence was associated with the number of cervical discs rather than with the number of patients. Because some patients were implanted with 1 artificial cervical disc while others were implanted with 2, it may not be accurate to classify a patient as HO-positive if only 1 disc is positive. The total number of artificial cervical discs in the 2 groups differed significantly, which may have led to potential bias. HO has been regarded as a type of postoperative degenerative process [41]. Because of the stringent surgical indications for TDR, patients with a higher degree of preoperative degeneration would be more likely to undergo fusion surgery. In the present study, the 1R2F group showed a greater potential for degeneration, which may have resulted in a higher incidence of HO. In addition, HO has been found to be a normal defense mechanism of the cervical spine in response to non-physiologic motion. ACDF can cause increased stress at adjacent levels, altering the biomechanical environment of the cervical spine, and may also explain the higher incidence of HO in the 1R2F group. Although the precise mechanism of HO is still unclear, multilevel disease, limited postoperative ROM, and surgical techniques are risk factors for HO [42,43]. Although we found that the incidence of HO was relatively high in 1R2F group, only 1 patient had McAfee III or IV degree HO. Long-term follow-up studies including larger numbers of patients are needed to confirm these findings.
The present study also had several limitations, including its retrospective design, which may have caused potential bias, and the small sample sizes and short follow-up periods. Large prospective, long-term, multicenter studies are therefore required.
Conclusions
This study found that the 2 types of HS incorporating fusion and non-fusion are safe and effective in the treatment of 3-level CDDD. The 1R2F operation was better in correcting the cervical lordosis, irrespective of the higher incidence of HO, whereas the 1F2R operation was superior in maintaining cervical ROM. However, the biomechanical characteristics of different types of HS are complex, suggesting the need for randomized controlled studies comparing types of HS.
Figures
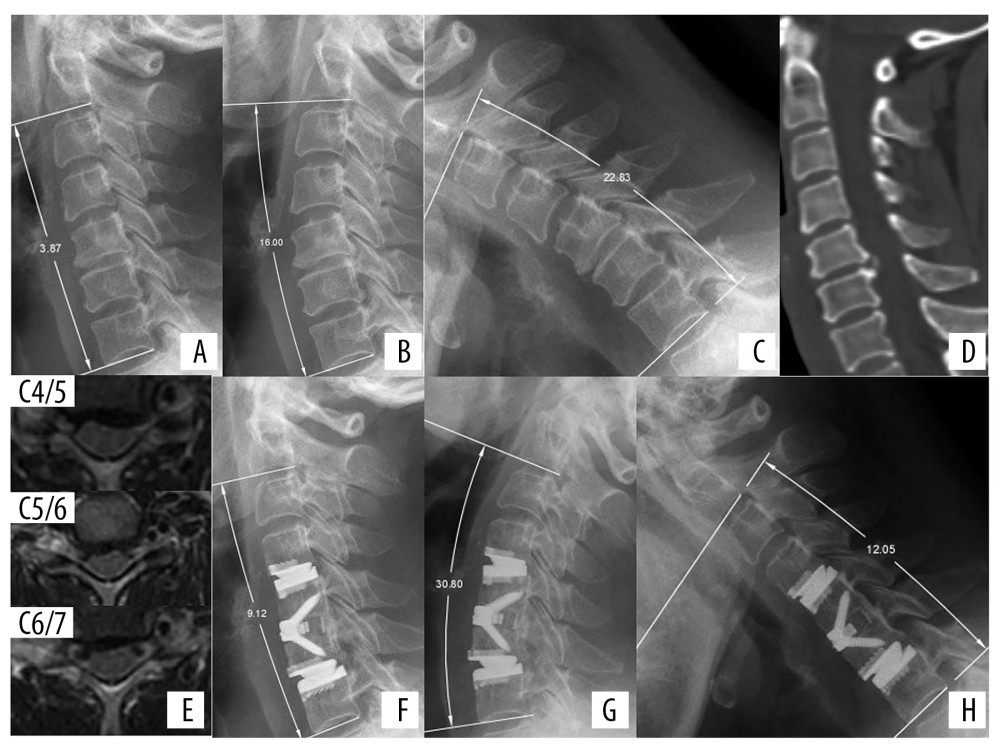 Figure 1. Radiologic examinations of a 55-year-old woman with neck pain for more than 2 years. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 3.87°. (B, C) Flexion-extension view, showing that ROM at C2–C7 was 38.83°. (D) CT scan, showing osteophytes at the posterior border of C4–C5. (E) MRI showing herniated cervical discs at C4/5, C5/6, and C6/7, causing pressure on the spinal cord. CDR was performed at C4/5 and C6/7 and ACDF at C5/6. (F) X-ray immediately after surgery, showing a cervical lordosis of 9.12°. (G, H) Flexion-extension view at 1 year, showing that ROM at C2–C7 was 42.85° (110.35% compared with preoperative ROM).
Figure 1. Radiologic examinations of a 55-year-old woman with neck pain for more than 2 years. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 3.87°. (B, C) Flexion-extension view, showing that ROM at C2–C7 was 38.83°. (D) CT scan, showing osteophytes at the posterior border of C4–C5. (E) MRI showing herniated cervical discs at C4/5, C5/6, and C6/7, causing pressure on the spinal cord. CDR was performed at C4/5 and C6/7 and ACDF at C5/6. (F) X-ray immediately after surgery, showing a cervical lordosis of 9.12°. (G, H) Flexion-extension view at 1 year, showing that ROM at C2–C7 was 42.85° (110.35% compared with preoperative ROM). 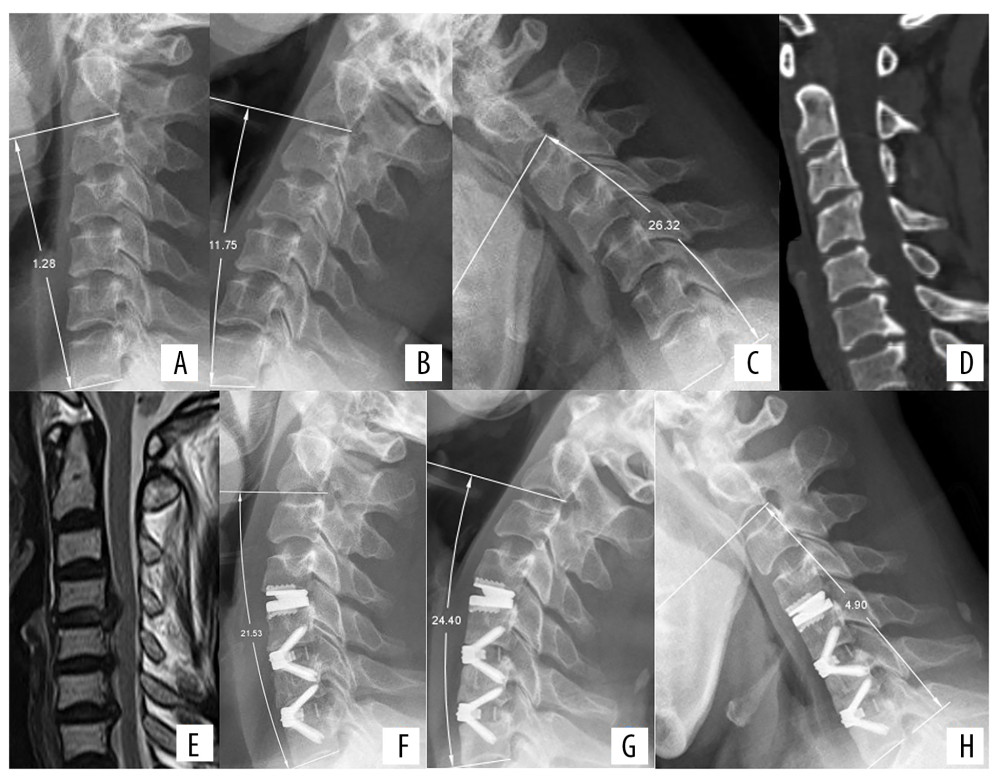 Figure 2. Radiologic examinations of a 52-year-old woman with neck pain for 2 months and numbness in both hands for 1 week. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 1.28°. (B, C) Extension-flexion view showing that ROM at C2–C7 was 38.07°. (D) CT scan showing osteophytes at the posterior borders of C5/6 and C6/7. (E) MRI showing protrusion of intervertebral discs at C4/5, C5/6, and C6/7. CDR was performed at C4/5 and ACDF at C5/6 and C6/7. (F) Lateral X-ray view immediately after surgery, showing cervical lordosis of 21.53°, a significant improvement compared with preoperative lordosis. (G, H) Extension-flexion X-ray at 1 year, showing that ROM of C2–C7 was 29.30°.
Figure 2. Radiologic examinations of a 52-year-old woman with neck pain for 2 months and numbness in both hands for 1 week. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 1.28°. (B, C) Extension-flexion view showing that ROM at C2–C7 was 38.07°. (D) CT scan showing osteophytes at the posterior borders of C5/6 and C6/7. (E) MRI showing protrusion of intervertebral discs at C4/5, C5/6, and C6/7. CDR was performed at C4/5 and ACDF at C5/6 and C6/7. (F) Lateral X-ray view immediately after surgery, showing cervical lordosis of 21.53°, a significant improvement compared with preoperative lordosis. (G, H) Extension-flexion X-ray at 1 year, showing that ROM of C2–C7 was 29.30°. References
1. Kadanka Z, Mares M, Bednaník J, Approaches to spondylotic cervical myelopathy: conservative versus surgical results in a 3-year follow-up study: Spine (Phila Pa 1976), 2002; 27(20); 2205-10 discussion 2210–11
2. Fehlings MG, Wilson JR, Kopjar B, Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: Results of the AOSpine North America prospective multi-center study: J Bone Joint Surg Am, 2013; 95(18); 1651-58
3. Fehlings MG, Ibrahim A, Tetreault L, A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: Results from the prospective multicenter AOSpine international study on 479 patients: Spine (Phila Pa 1976), 2015; 40(17); 1322-28
4. Xiong Y, Xu L, Yu X, Comparison of 6-year follow-up result of hybrid surgery and anterior cervical discectomy and fusion for the treatment of contiguous two-segment cervical degenerative disc diseases: Spine (Phila Pa 1976), 2018; 43(20); 1418-25
5. Wang KF, Duan S, Zhu ZQ, Clinical and radiologic features of 3 reconstructive procedures for the surgical management of patients with bilevel cervical degenerative disc disease at a minimum follow-up period of 5 years: A comparative study: World Neurosurg, 2018; 113; e70-76
6. Wu TK, Meng Y, Wang BY, Is the behavior of disc replacement adjacent to fusion affected by the location of the fused level in hybrid surgery?: Spine J, 2018; 18(12); 2171-80
7. Meng Y, Wang X, Zhao Z, Intraoperative anterior migration of the prestige-LP cervical disc owing to an inappropriate implantation sequence during continuous 2-level artificial cervical disc replacement: A case report with 8-year follow-up: World Neurosurg, 2018; 116; 194-200
8. Hirabayashi K, Miyakawa J, Satomi K, Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament: Spine (Phila Pa 1976), 1981; 6(4); 354-64
9. McAfee PC, Cunningham BW, Devine J, Classification of heterotopic ossification (HO) in artificial disk replacement: J Spinal Disord Tech, 2003; 16(4); 384-89
10. Bazaz R, Lee MJ, Yoo JU, Incidence of dysphagia after anterior cervical spine surgery: A prospective study: Spine (Phila Pa 1976), 2002; 27(22); 2453-58
11. Liu H, Liu X, Shi RTwo-level cervical artificial disc replacement combined with nearby segments fused for multi-level disc herniations: Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi, 2006; 20(4); 383-86 [in Chinese]
12. Ding C, Liu H, Hu T, Bi-level Bryan artificial disc replacement and nearby segment fusion in multi-level disc herniations: A 5-year follow-up study: J Spinal Surg, 2011; 9(5); 288-92
13. Barbagallo GMV, Assietti R, Corbino L, Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: Opposite or complementary techniques?: Eur Spine J, 2009; 18(Suppl 1); 29-39
14. Hollyer MA, Gill EC, Ayis S, Demetriades AK, The safety and efficacy of hybrid surgery for multilevel cervical degenerative disc disease versus anterior cervical discectomy and fusion or cervical disc arthroplasty: A systematic review and meta-analysis: Acta Neurochir (Wien), 2020; 162(2); 289-303
15. Jang SR, Lee SB, Cho KS, A comparison of anterior cervical discectomy and fusion versus fusion combined with artificial disc replacement for treating 3-level cervical spondylotic disease: J Korean Neurosurg Soc, 2017; 60(6); 676-83
16. Lu VM, Zhang L, Scherman DB, Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: A systematic review and meta-analysis: Eur Spine J, 2017; 26(2); 546-57
17. Ding F, Jia Z, Wu Y, Fusion-nonfusion hybrid construct versus anterior cervical hybrid decompression and fusion: A comparative study for 3-level cervical degenerative disc diseases: Spine (Phila Pa 1976), 2014; 39(23); 1934-42
18. Hung CW, Wu MF, Yu GF, Comparison of sagittal parameters for anterior cervical discectomy and fusion, hybrid surgery, and total disc replacement for three levels of cervical spondylosis: Clin Neurol Neurosurg, 2018; 168; 140-46
19. Yang X, Bartels RHMA, Donk R, The association of cervical sagittal alignment with adjacent segment degeneration: Eur Spine J, 2019 [Online ahead of print]
20. Katsuura Y, York PJ, Goto R, Sagittal reconstruction and clinical outcome using traditional ACDF, versus stand-alone ACDF versus TDR: A systematic review and quantitative analysis: Spine (Phila Pa 1976), 2019; 44(19); E1151-58
21. Kowalczyk I, Chaudhary N, Duggal N, Kinematic analysis following implantation of the PRESTIGE LP: Int J Spine Surg, 2013; 7; e118-22
22. Kang J, Shi C, Gu Y, Factors that may affect outcome in cervical artificial disc replacement: A systematic review: Eur Spine J, 2015; 24(9); 2023-32
23. Chang HK, Huang WC, Tu TH, Radiological and clinical outcomes of 3-level cervical disc arthroplasty: J Neurosurg Spine, 2019; 32(2); 174-81
24. Reinas R, Kitumba D, Pereira L, Multilevel cervical arthroplasty-clinical and radiological outcomes: J Spine Surg, 2020; 6(1); 233-42
25. Nunley PD, Coric D, Frank KA, Stone MB, Cervical disc arthroplasty: Current evidence and real-world application: Neurosurgery, 2018; 83(6); 1087-106
26. Pesce A, Wierzbicki V, Piccione E, Adjacent segment pathology: Natural history or effect of anterior cervical discectomy and fusion? A 10-year follow-up radiological multicenter study using an evaluation scale of the ageing spine: Eur J Orthop Surg Traumatol, 2017; 27(4); 503-11
27. Park JY, Kim KH, Kuh SU, What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT: Eur Spine J, 2013; 22(5); 1078-89
28. Chang UK, Kim DH, Lee MC, Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion: J Neurosurg Spine, 2007; 7(1); 33-39
29. Wang Z, Zhu R, Yang H, Zero-profile implant (Zero-p) versus plate cage benezech implant (PCB) in the treatment of single-level cervical spondylotic myelopathy: BMC Musculoskelet Disord, 2015; 16; 290
30. Li T, Yang JS, Wang XF, Can zero-profile cage maintain the cervical curvature similar to plate-cage construct for single-level anterior cervical diskectomy and fusion?: World Neurosurg, 2020; 135; e300-6
31. Lan T, Lin JZ, Hu SY, Comparison between zero-profile spacer and plate with cage in the treatment of single level cervical spondylosis: J Back Musculoskelet Rehabil, 2018; 31(2); 299-304
32. Albanese V, Certo F, Visocchi M, Barbagallo GMV, Multilevel anterior cervical diskectomy and fusion with zero-profile devices: Analysis of safety and feasibility, with focus on sagittal alignment and impact on clinical outcome: Single-institution experience and review of literature: World Neurosurg, 2017; 106; 724-35
33. Tong MJ, Xiang GH, He ZL, Zero-profile spacer versus cage-plate construct in anterior cervical diskectomy and fusion for multilevel cervical spondylotic myelopathy: Systematic review and meta-analysis: World Neurosurg, 2017; 104; 545-53
34. Xiong Y, Xu L, Bi LY, Dynamic fusion process in the anterior cervical discectomy and fusion with self-locking stand-alone cages: World Neurosurg, 2019; 125; e678-87
35. Bucci MN, Oh D, Cowan RS, The ROI-C zero-profile anchored spacer for anterior cervical discectomy and fusion: Biomechanical profile and clinical outcomes: Med Devices (Auckl), 2017; 10; 61-69
36. Kapetanakis S, Thomaidis T, Charitoudis G, Single anterior cervical discectomy and fusion (ACDF) using self- locking stand-alone polyetheretherketone (PEEK) cage: Evaluation of pain and health-related quality of life: J Spine Surg, 2017; 3(3); 312-22
37. Ament JD, Yang Z, Nunley P: JAMA Surg, 2014; 149(12); 1231-39
38. Kim JS, Dowdell J, Cheung ZB, The seven-year cost-effectiveness of anterior cervical discectomy and fusion versus cervical disc arthroplasty: A Markov analysis: Spine (Phila Pa 1976), 2018; 43(22); 1543-51
39. Merrill RK, McAnany SJ, Albert TJ, Qureshi SA, Is two-level cervical disc replacement more cost-effective than anterior cervical discectomy and fusion at 7 years?: Spine (Phila Pa 1976), 2018; 43(9); 610-16
40. Overley SC, McAnany SJ, Brochin RL, The 5-year cost-effectiveness of two-level anterior cervical discectomy and fusion or cervical disc replacement: A Markov analysis: Spine J, 2018; 18(1); 63-71
41. Li G, Wang Q, Liu H, Yang Y, Postoperative heterotopic ossification after cervical disc replacement is likely a reflection of the degeneration process: World Neurosurg, 2019; 125; e1063-68
42. Chang PY, Chang HK, Wu JC, Differences between C3–4 and other subaxial levels of cervical disc arthroplasty: More heterotopic ossification at the 5-year follow-up: J Neurosurg Spine, 2016; 24(5); 752-59
43. Wu JC, Huang WC, Tsai TY, Multilevel arthroplasty for cervical spondylosis: More heterotopic ossification at 3 years of follow-up: Spine (Phila Pa 1976), 2012; 37(20); E1251-59
Figures
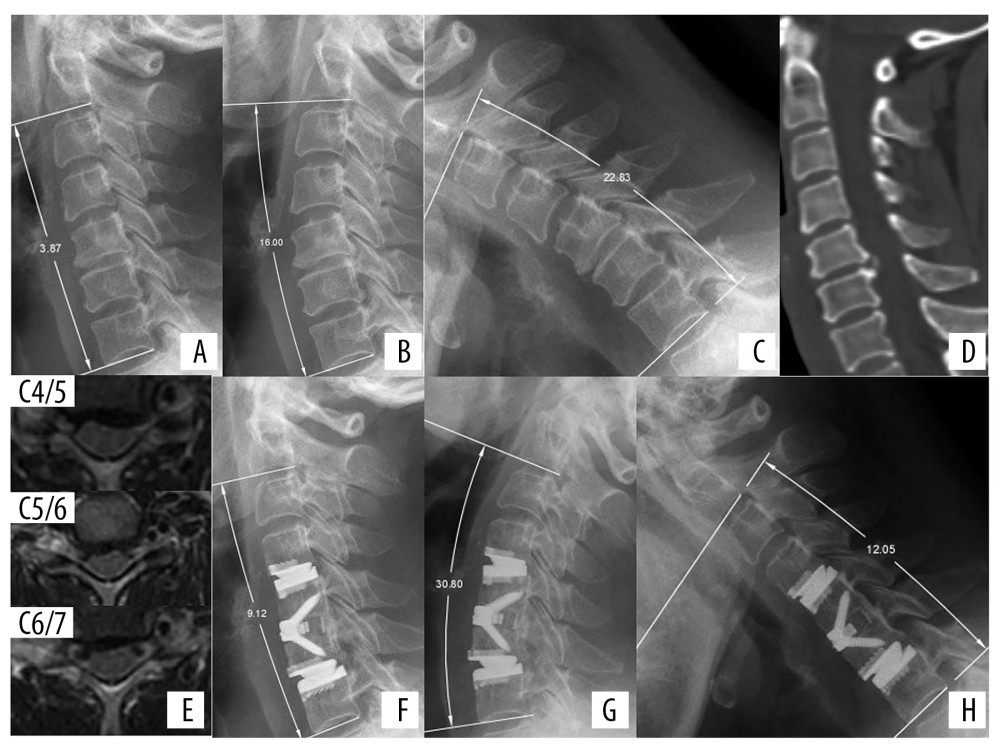 Figure 1. Radiologic examinations of a 55-year-old woman with neck pain for more than 2 years. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 3.87°. (B, C) Flexion-extension view, showing that ROM at C2–C7 was 38.83°. (D) CT scan, showing osteophytes at the posterior border of C4–C5. (E) MRI showing herniated cervical discs at C4/5, C5/6, and C6/7, causing pressure on the spinal cord. CDR was performed at C4/5 and C6/7 and ACDF at C5/6. (F) X-ray immediately after surgery, showing a cervical lordosis of 9.12°. (G, H) Flexion-extension view at 1 year, showing that ROM at C2–C7 was 42.85° (110.35% compared with preoperative ROM).
Figure 1. Radiologic examinations of a 55-year-old woman with neck pain for more than 2 years. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 3.87°. (B, C) Flexion-extension view, showing that ROM at C2–C7 was 38.83°. (D) CT scan, showing osteophytes at the posterior border of C4–C5. (E) MRI showing herniated cervical discs at C4/5, C5/6, and C6/7, causing pressure on the spinal cord. CDR was performed at C4/5 and C6/7 and ACDF at C5/6. (F) X-ray immediately after surgery, showing a cervical lordosis of 9.12°. (G, H) Flexion-extension view at 1 year, showing that ROM at C2–C7 was 42.85° (110.35% compared with preoperative ROM).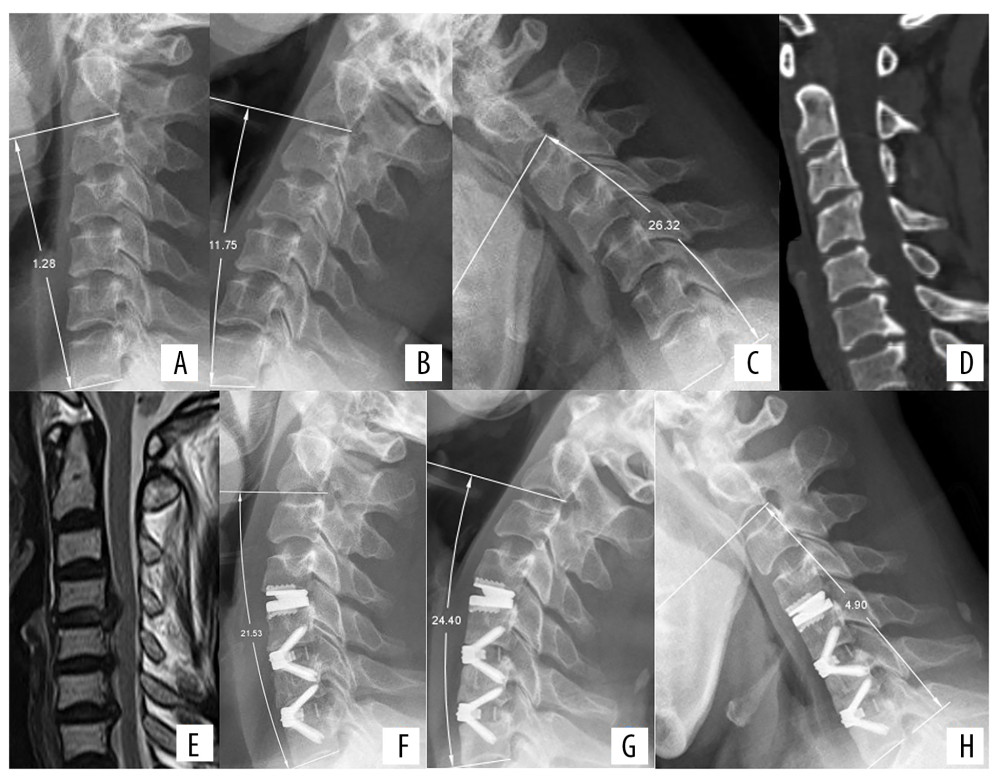 Figure 2. Radiologic examinations of a 52-year-old woman with neck pain for 2 months and numbness in both hands for 1 week. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 1.28°. (B, C) Extension-flexion view showing that ROM at C2–C7 was 38.07°. (D) CT scan showing osteophytes at the posterior borders of C5/6 and C6/7. (E) MRI showing protrusion of intervertebral discs at C4/5, C5/6, and C6/7. CDR was performed at C4/5 and ACDF at C5/6 and C6/7. (F) Lateral X-ray view immediately after surgery, showing cervical lordosis of 21.53°, a significant improvement compared with preoperative lordosis. (G, H) Extension-flexion X-ray at 1 year, showing that ROM of C2–C7 was 29.30°.
Figure 2. Radiologic examinations of a 52-year-old woman with neck pain for 2 months and numbness in both hands for 1 week. (A) Preoperative lateral X-ray showing cervical lordosis at C2–C7 of 1.28°. (B, C) Extension-flexion view showing that ROM at C2–C7 was 38.07°. (D) CT scan showing osteophytes at the posterior borders of C5/6 and C6/7. (E) MRI showing protrusion of intervertebral discs at C4/5, C5/6, and C6/7. CDR was performed at C4/5 and ACDF at C5/6 and C6/7. (F) Lateral X-ray view immediately after surgery, showing cervical lordosis of 21.53°, a significant improvement compared with preoperative lordosis. (G, H) Extension-flexion X-ray at 1 year, showing that ROM of C2–C7 was 29.30°. In Press
05 Mar 2024 : Clinical Research
Effects of Thermal Insulation on Recovery and Comfort of Patients Undergoing Holmium Laser LithotripsyMed Sci Monit In Press; DOI: 10.12659/MSM.942836
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952