08 January 2021: Review Articles
Trends in Workplace Violence Involving Health Care Professionals in China from 2000 to 2020: A Review
Xin Zhang12ABCDEF, Yizhi Li12C, Chunsheng Yang3D, Guan Jiang12D*DOI: 10.12659/MSM.928393
Med Sci Monit 2021; 27:e928393
Abstract
ABSTRACT: The safety of health care workers in China has received an increasing amount of attention owing to numerous incidents of hospital-based violence against medical professionals. When pictures and videos of violent injuries are posted on the internet with real-time data, such as gender or location, researchers can access the information to learn about the incident, its causes, and/or threats to survival. We examined the causes and risk factors for workplace violence by analyzing relevant data retrieved from reports by Chinese internet media for all incidents from 2000 to 2020. We present frequency data on hospital-based violence against medical professionals. A total of 345 incidents occurred in health care settings. The person who committed the violent act was a patient or sick person in the workplace or a co-worker in 95.4% of the incidents; 54 of the incidents resulted in the victim’s murder. We provide the characteristics and risk factors of violent criminals. We describe China’s past and current clinical practices and health care policies, and we discuss the challenges faced by medical professionals who are victims of hospital-based violence from the perspectives of patients, physicians, hospital leaders, and the government. We conclude by making recommendations for preventing violence in hospital settings. It is urgent for the public to understand that the occupational safety of health care workers must be protected, and treatment should be provided to patients in a harmonious and safe environment. This review aims to describe the trends in workplace violence involving health care professionals in China from 2000 to 2020 and to discuss possible strategies for improving working conditions in hospitals and other health care settings.
Keywords: Health Care Reform, Public Health, Workplace Violence, Health Personnel, Hospitals
Background
The World Health Organization (WHO) currently defines workplace violence as physical or psychological “incidents where staff are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, and involving an explicit or implicit challenge to their safety, well-being, or health” [1]. Whether intentionally or not, silence in response to workplace violence is an endorsement of violence and only serves to maintain and encourage it. When an Emergency Department doctor was fatally stabbed by a patient’s son at Beijing’s Civil Aviation General Hospital on December 24, 2019, doctor-patient relationships in China seemed to be at their worst [2]. This incident was a shocking, but not isolated event [3]. Within 1 month, tragedy again occurred when a chief physician of the Ophthalmology Department of Beijing Chaoyang Hospital was slashed with a knife. A survey [4] revealed that 66% of China’s physicians have experienced doctor-patient conflicts to a varying extent, and in 2018, 3308 people were prosecuted for intentionally harming medical personnel and causing disturbances in hospitals [5].
Similar to the United States, violence in the health care workplace is an underreported, widespread, and persistent problem that has been tolerated and largely ignored in China [6]. In recent years, increasing attacks on doctors and nurses by patients and their relatives have caused serious injuries and aroused deep concern [7]. Many studies, including those conducted in China, have noted that aggression against medical workers greatly exceeds aggression against other professional groups [8,9]. The combination of actual or feared physical attacks and verbal attacks troubles Chinese medical staff because they are obligated to fulfill vital and often busy roles [10]. Workplace violence in medical institutions could be an indicator of the general tension between doctors and patients, which could in turn compromise the accessibility and quality of the health care system [11].
China has implemented health care [12] and higher education reforms [13], as well as policies, to address this phenomenon. Given China’s diversity and unique history, solutions for this problem are worth pondering. In this review, we identified and analyzed the main causes of workplace violence in China, examined relevant clinical practices and health care policies, and recommended interventions to counter the frequent occurrence of violent incidents. Our intent was to respond to public dissatisfaction and to increase confidence in our ability to address this complex issue.
Research and Statistics on Hospital Workplace Violence in China 2000–2020
Chinese medical professionals are in crisis [14]. Daily insults and physical attacks in the workplace are increasing at an alarming pace [15]. The Bureau of Labor and Occupational Safety and Health Administration [6] in the United States, which specializes in collecting statistics on workplace violence, is an excellent resource. In China, the internet has become the authoritative source for coverage of such topics. However, some people doubt the comprehensiveness and fairness of the media in their reports on hospital-based violence [16], and most studies on workplace violence in other countries are based on voluntary retrospective surveys, which are prone to selection and recall bias [6]. In addition, data from the U.S. Bureau of Labor Statistics are likely to be inaccurate [17] because they do not include verbal abuse; therefore, they cannot provide a comprehensive assessment of workplace violence [18]. One study on the potential utility of nontraditional data sources for research showed that social media platforms could be useful as a supplemental data source [19]. In a 2017 survey, most of the respondents (Chinese doctors) did not agree with the following item: “The tension between doctors and patients is partially caused by the media’s inclination to influence public opinion” [4].
Based on the relationship between the violent offender and the workplace, experts have categorized workplace violence into 4 types [20]: (i) the person committing the act of violence or intimidation has nothing to do with the workplace or workers; (ii) the person committing the act of violence or intimidation is a patron or sick person in the workplace or a worker; (iii) the person committing the act of violence or intimidation is a present or former worker in the workplace; and (iv) the person committing the act of violence or intimidation has no relationship with the workplace, only with the workers. Information on hospital-based violence from 2000 to 2020 was searched on popular Chinese biomedical websites and on Chinese news portal sites, including Xinhuanet, People, Sin, Sohu, and Tencent. To ensure the authenticity of the retrieved reports of violent incidents, we conducted the search multiple times, and each incident was stringently verified. The analysis of the reports mainly involved deleting duplicate and false reports, and entering and processing the data using Excel 2016 and Access 2016. A total of 345 incidents occurred in health care settings from 2000 to 2020 (Figure 1). These incidents not only involved verbal insults and beatings of providers, but more seriously, 54 incidents ended with the victims being murdered. The second type of workplace violence was the most common (95.4%) among all incidents. In this type, the offenders had a legitimate relationship with the department and became violent during or after exercising their rights [6]. It was not surprising that there were no incidents of the third type of violence.
Characteristics of Violent Offenders and Risk Factors
The main characteristics of the perpetrators of hospital-based violence were altered mental state, poor behavior, psychological distortion, a confirmed diagnosis of malignant disease, and drunkenness (Figure 2). One study showed that most of the patients with malignant diseases had a low educational level and their families were relatively poor [21]. More than 70% of the perpetrators were unemployed, farmers, laid-off workers, or migrant workers; 40% were introverted, lonely, or paranoid; 30% had a history of mental illness; and for those with other diseases, incurability, difficulty paying medical expenses, and other stressors were present [21]. Patients, family members, and accompanying persons have been described as having specific emotional or behavioral tendencies before the violent incident occurred [22], and some patients had a mental illness and/or were easily irritated. No link was established between these perpetrators’ violent behaviors and the hospitals or medical staff members. Some patients and their families had very high or unrealistic expectations of treatments and believed the money they spent on medical care was their payment for excellent outcomes or complete recovery, even for incurable diseases in the advanced stage [9,22]. Other patients and their families lacked an understanding of medicine; therefore, the decisions and behaviors of health care workers caused them to have anxiety about their illness and to become frustrated with the workers’ response to them, to the point of losing emotional control.
From 2000 through 2020, 38.3% of violent crimes were committed using lethal weapons, such as knives. Most incidents of assault against medical staff (96.5%) occurred within hospitals, mainly in wards, outpatient clinics, and emergency departments [9,22–24]. Considering the perpetrator alone, the most common causes of violence were the death of the patient (18.8%); disapproval of a staff member’s skills or the diagnosis or recommendation of the health care staff (18.3%); and poor treatment outcomes or sequelae (15.9%) (Figure 3A). When the interaction between the perpetrator and the provider was considered, common causes leading to violence were poor communication (38.8%), the patient’s death (18.8%), and the level of service (16.5%) (Figure 3B).
The risk factors for violence included ones related to the provider, such as interpersonal communication skills, awareness of humanistic care, job burn-out, infrastructure, and low awareness about security [25–27]. Some health care workers thought they only needed to complete medical tasks, and others were weary because of work overload and job-related pressures. Hospitals may allow doctors to receive 100 outpatients every day, which is an overwhelming workload that deprives doctors and their patients of a humane relationship, leaving them no time to establish or develop a mutually beneficial doctor-patient relationship [28]. When health care workers ignore the anxiety of patients or their families, it increases and the individuals’ attempts to communicate with the staff decrease, leading to patient dissatisfaction. Doctors’ salaries were modest and depended on improper incentives (e.g., the numbers of patients seen and drugs prescribed), rather than on the quality of care provided [28]. High workload and low remuneration diminished the sense of accomplishment among the health care workers [27]. Some medical institutions have neglected the needs of their hospitals because administrators have failed to view them as a public place with a large number of personnel and a complex mission. The small number of security personnel and inadequate surveillance and protection led to the failure to prevent violence in the early stage of conflict.
How to Reduce Workplace Violence
HEALTH CARE REFORMS:
In 1984, China was transformed into a market economy, reducing the government’s role in economic and social sectors, including health care [29–31]. Local governments shifted primary care to hospital-centric specialist care [29]. By the end of the 1990s, this reform had led to the public’s dissatisfaction and protests over the lack of access to medical services, and even widespread personal attacks on doctors [30]. In 2003, the Chinese government reduced the public’s dissatisfaction with health care by introducing a plan for moderate medical insurance that covered part of rural residents’ hospitalization expenses, but it was not enough to improve deep-rooted problems in China’s health care system [30]. To alleviate serious inequalities in medical care between the eastern and western provinces and urban and rural areas, the government launched an initiative in 2004, with countless doctors supporting rural health projects. Through long-term exchange programs, large hospitals in the eastern provinces provided support for rural areas in the western provinces [32]. Since 2006, the central government has been developing a strong primary health care system through efforts to train family doctors [29].
In 2009, the government launched new reforms in the medical and health care systems [6,31,33]. The medical service system plan, which was formulated at the national level for the first time in 2015, was designed to promote the development of medical reforms, to solve the difficult problem of expensive medical treatment, and to build a healthy China [34]. In 2016, a report from the China Joint Study Partnership proposed 8 strategic reforms to improve health care, with each reform consisting of a set of recommended core actions and guidance for implementation at all governmental levels [35]: (i) shaping a tiered health care delivery system, in accordance with the people-centered integrated care model; (ii) improving the quality of care in support of people-centered integrated care; (iii) engaging citizens in support of people-centered integrated care; (iv) reforming public hospitals and improving their performance; (v) realigning incentives for purchasing and provider payment; (vi) strengthening the health care workforce to promote people-centered integrated care; (vii) strengthening private-sector engagement in the production and delivery of health care services; and (viii) modernizing health care service planning to guide investment.
In response to violence-related injuries, the central government adopted a zero-tolerance policy at the legal level. In a joint notice, the Ministry of Health and the Ministry of Public Security called for the protection of medical staff from violence as a response to the deadly violence at the First Affiliated Hospital of Harbin Medical University [36]. On April 24, 2014, the Supreme Court announced its decision to cooperate with 4 relevant departments to impose fines on those responsible for workplace violence in hospitals [37]. In November 2015, the Chinese People’s Congress revised the criminal law to include penalties for people who disrupt hospital care [38]. On December 28, 2019, China’s top legislators approved the first comprehensive law to protect health care workers, which took effect on June 1, 2020 [2].
EDUCATIONAL REFORMS:
China initiated major reforms in medical education in 2013 to integrate it with the international model of medical education. The mode of standardized training for residents is referred to as “5+3” [7]. In 2016, the National Health Planning Commission implemented standardized training reforms for specialists, requiring Chinese doctors to complete specialized training for 2–4 years after completing standardized training for 3 years in a hospital [7,39]. Inspired by the reforms in the US medical education system, Peking University Medical College took the lead in launching the new 4+4 medical education program in 2018 [33,40].
Challenge
DEMANDS FOR HIGH QUALITY:
Chinese society has shifted focus from “material and cultural needs” to “happy life needs.” The pursuit of a better life brings unprecedented high expectations for better health care services [31,41,42]. From 2000 to 2018, the ranking of 8 consumption expenditures of Chinese rural residents changed significantly (Figure 4B). Although food expenditures still rank the highest, the proportion has fallen rapidly (down 19.0%), and the proportion of health care expenditures has continued to increase, from 5.2% in 2000 to 10.2% (up 5 percentage points) in 2018. The proportion of urban residents’ per capita health expenditures varies little from year to year (Figure 4C). The latest data from the National Bureau of Statistics shows that in 2019 the total urban population was 1.5 times the total rural population. Rural health care expenditures, which have increased in tandem with changes in the structure of urban and rural areas, highlight the challenge of solving the “symptom” of violence against medical workers since socialism with Chinese characteristics entered a new era.
The rapid increase in medical and health care consumption reflects the fairness of financing health expenditures and the magnitude of the economic burden of disease [43]. From 2000 to 2018, the average annual growth rate of per capita expenditures for medical care consumption of rural residents reached 16.9%, exceeding the average annual growth rate of residents’ disposable incomes (11.5%) [44]. At the same time, the proportion of health care consumption expenditures of residents’ disposable incomes also increased from 3.8% to 8.5% (Figure 4B). The average annual growth rate of per capita expenditures for the medical care consumption of urban residents was only 0.2% higher than the average annual growth rate of their disposable incomes [44]. As a percentage of disposable income, health care consumption expenditures did not increase or decrease significantly (Figure 4C). Apparently, the current medical care consumption of rural households accounts for a large share of living consumption, and the growth rate of medical care consumption clearly exceeds the income growth rate. For households with lower disposable incomes, the increase in medical consumption expenditures offsets the increase in disposable income, which seriously affects quality of life and has led to an increase in medical consumption expenditures. These huge changes in the patterns and costs of medical and health care consumption could foster negative attitudes toward the work of medical personnel, thereby creating a vicious cycle.
INFORMATION ASYMMETRY:
Most patients and their families are “outsiders” in relation to the behaviors of those in the field of medicine, as manifested by their lack of knowledge about medical treatments and health [45]. Strong emotions are vented against health care workers based on ignorance about medical behaviors and anxiety about the patient’s condition [46]. When patients’ or families’ expectations are not met, they suspect wrongdoing by the doctor [28]. In 2018, the average life expectancy of residents was 77 years [47]. Aging and high-end service trends are prompting people to downplay their awareness of illness and eventual death.
ROLE DISSATISFACTION:
Medicine is no longer considered a noble or attractive profession in China [38,39,41,48]. Many graduates of medical schools choose not to enter the medical profession after graduation or obtain certification to practice [28,41]. In addition to the heavy clinical workload, doctors have pressure to publish articles [49] and manage households, including childcare, which can be especially stressful for female doctors [50]. In a survey of physicians’ attitudes toward practice [4], male and female respondents showed significant differences in attitudes. The women were more motivated than the men, and individuals with senior professional titles had a more positive attitude toward practice. In 2018, male occupational physicians accounted for 53.8% of doctors in China, and occupational doctors with professional and technical positions below the junior level accounted for 53.0% [51]. The professional attitude of more than half of the physicians was worrisome.
This survey [4] also showed that 33.2% of physicians had 1 disease and 5.9% had more than 1 disease; more than half of the physicians had various symptoms, and the causes were diverse (e.g., disease, psychological factors, and transient physical discomfort). The high prevalence of diseases and other conditions among physicians cannot be ruled out as the root cause of “illnesses in the health care system.” There is growing evidence that deaths by overwork (karoshi) among Chinese doctors are escalating [39,48,52]. Doctors with high levels of professional satisfaction and fulfillment improve clinical efficiency [53] and patient dissatisfaction, and they have the potential to reduce hospital-based violence.
FRAGMENTED GOVERNANCE:
China’s 1.4 billion people live in a variety of economic environments and geographic regions. The medical service system is fragmented [54], with gaps in reaching the goals for developing a new mechanism for maintaining public welfare, mobilizing enthusiasm, and ensuring sustainability. The most serious of these problems is the lack of medical resources and the presence of imperfect diagnostic and treatment systems. Patients tend to seek treatment in tier 3 hospitals, where they encounter long waiting times and short consultation times in large facilities. Most (56.66%) medical incidents occurred in tertiary hospitals [55].
Chinese health technicians vary widely in the quality and quantity of their education [29,40]. In 2018, 63.8% of health technicians, excluding those in village clinics, did not have a bachelor’s degree [51]. Compared with doctors in developed countries, doctors in China mature on average more than 10 years later [56]. General practitioners are the “gatekeepers” of the residents’ health. The state has supported the training of general practitioners. However, new problems have emerged and experienced general practitioners have left primary care facilities [29].
Discussion
A serious public health challenge is the high prevalence of workplace violence in China’s health care sector [57]. Tolerance of abuse in recent times has led to low morale and psychological trauma of the victims [58,59], and restoration of medical professionals’ confidence in their profession is urgently needed. Violence in the medical workplace is complex and cannot be solved by any one person or by simple strategies. It may take a long time to build a culture of respect for medical care and to protect society throughout China.
Violence against medical personnel in health care settings must be proactively addressed and prevented in a comprehensive manner. Much work is needed by patients, physicians, hospital leaders, and governments. The main tasks include attaching importance to the role of chronic diseases and conducting in-depth health education activities; providing psychological first aid to patients and/or family members who have experienced a medical crisis; and paying attention to patients with alcoholism and mental disorders and performing comprehensive assessments of their behavioral health. The main tasks required of professionals are to improve the quality of physicians’ education; increase doctors’ benefits and pay, with attention to the decoupling of salaries and medical income; increase the number of workplace security guards; hire trained observers and install panic buttons; conduct training on risk factors for violence; improve the reporting system for violence; create a more scientific and reasonable evaluation system for doctors; pay attention to the medical expenditures of low-income families; involve people in the transformation of China’s health care system; and reallocate medical resources. With collaborative efforts involving the entire society, we are committed to improving and expanding the health care system.
Conclusions
Hospital-based violence against medical professionals is a common problem in China. This study illustrates that violence against medical personnel in health care settings must be proactively addressed and prevented in a comprehensive manner. Given China’s current national conditions, the prevention and control of violence in the medical workplace need to be highly valued by relevant managers and all medical professionals in order to develop therapeutic doctor-patient relationships and a medical environment that is safe and harmonious. In addition, the new coronavirus pandemic will reshape the currently evolving health care reforms and doctor-patient relationships. In the unique social environment of 2020, addressing hospital-based violence is at a critical crossroads.
Figures
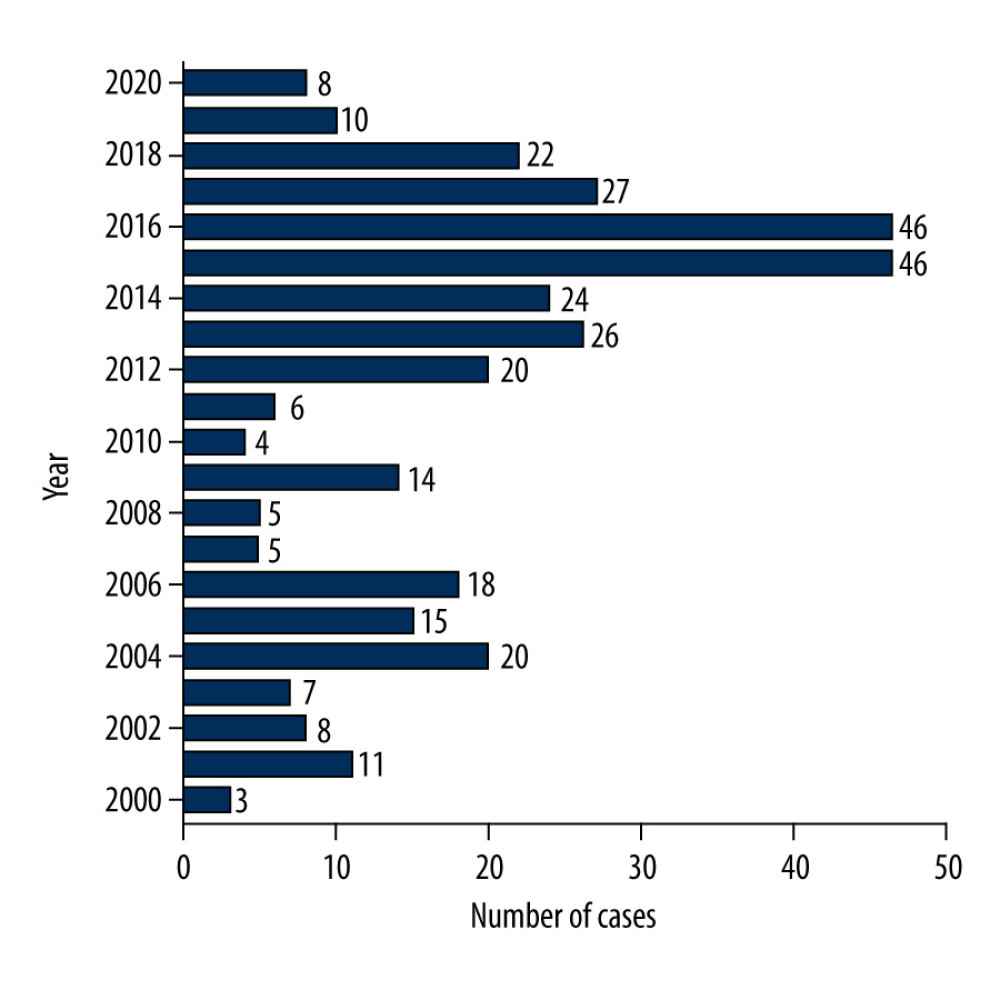 Figure 1. Violence-related injuries sustained by China’s health care workforce.
Figure 1. Violence-related injuries sustained by China’s health care workforce. 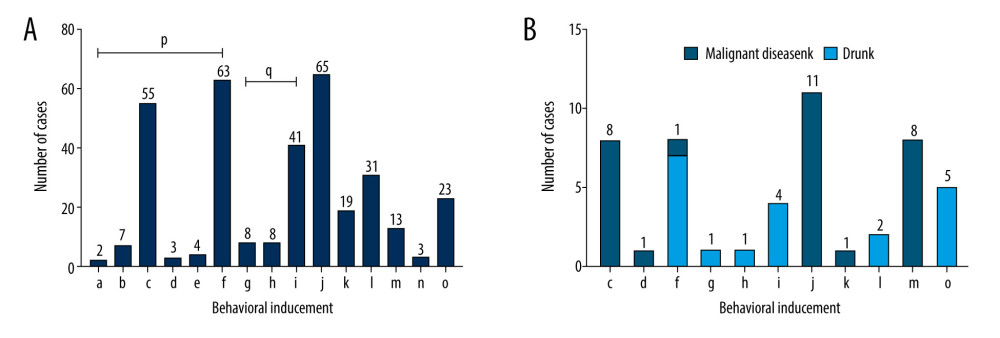 Figure 2. (A, B) Causes of hospital-based violence against medical personnel: a) overtesting of the patient by the hospital; b) misdiagnosis and delays; c) poor outcomes or sequelae; d) medical identification; e) sexual harassment; f) the health care worker’s choice of technology, diagnosis, or guidance; g) hospital charges; h) medical staff’s bearing; i) objective factors (such as provision, insufficient medical resources); j) death of the patient; k) mental state; l) absence of a valid diathesis; m) psychological distortion; n) other reasons (injury-related irritation, blackmail, or asking private questions); o) unknown reasons; p) a+b+c+d+e+f=communication; q) g+h+i=service.
Figure 2. (A, B) Causes of hospital-based violence against medical personnel: a) overtesting of the patient by the hospital; b) misdiagnosis and delays; c) poor outcomes or sequelae; d) medical identification; e) sexual harassment; f) the health care worker’s choice of technology, diagnosis, or guidance; g) hospital charges; h) medical staff’s bearing; i) objective factors (such as provision, insufficient medical resources); j) death of the patient; k) mental state; l) absence of a valid diathesis; m) psychological distortion; n) other reasons (injury-related irritation, blackmail, or asking private questions); o) unknown reasons; p) a+b+c+d+e+f=communication; q) g+h+i=service. 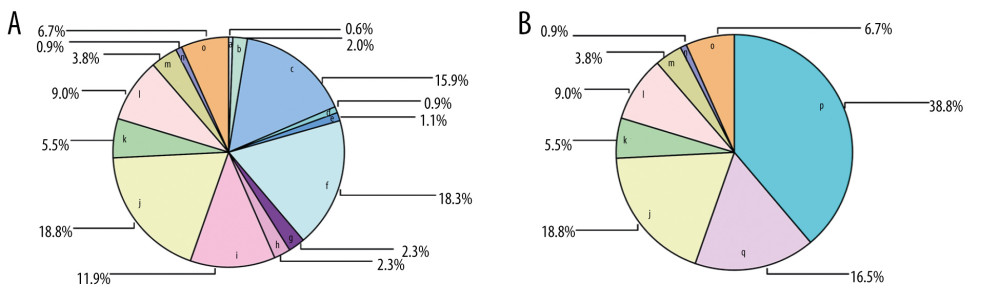 Figure 3. (A, B) The proportion of each cause of hospital-based violence. The causes of workplace violence and their representative letters (a–q) are the same as those reported in Figure 2.
Figure 3. (A, B) The proportion of each cause of hospital-based violence. The causes of workplace violence and their representative letters (a–q) are the same as those reported in Figure 2. ![China’s health expenditures (A) and per capita rural (B) and urban (C) distributions of consumption expenditures. Data are from the National Bureau of Statistics [44] and the National Health Commission [47].](https://jours.isi-science.com/imageXml.php?i=medscimonit-27-e928393-g004.jpg&idArt=928393&w=1000) Figure 4. China’s health expenditures (A) and per capita rural (B) and urban (C) distributions of consumption expenditures. Data are from the National Bureau of Statistics [44] and the National Health Commission [47].
Figure 4. China’s health expenditures (A) and per capita rural (B) and urban (C) distributions of consumption expenditures. Data are from the National Bureau of Statistics [44] and the National Health Commission [47]. References
1. World Health Organization (WHO): Framework guidelines for addressing workplace violence in the health sector, 2002, Geneva, WHO https://www.who.int/violence_injury_prevention/violence/interpersonal/en/WVguidelinesEN.pdf
2. , The Lancet: Protecting Chinese doctors: Lancet, 2020; 395; 90
3. Sibbald B, Workplace violence is not part of a doctor’s job: CMAJ, 2017; 189(5); E184
4. Chinese Medical Doctor Association [in Chinese]http://www.cmda.net/u/cms/www/201807/06181247ffex.pdf
5. The Supreme People’s Procuratorate [in Chinese]https://www.spp.gov.cn/spp/gzbg/201903/t20190319_412293.shtml
6. Phillips JP, Workplace violence against health care workers in the United States: N Engl J Med, 2016; 374; 1661-69
7. Lu L, Dong M, Wang SB, Prevalence of workplace violence against health-care professionals in China: A comprehensive meta-analysis of observational surveys: Trauma Violence Abuse, 2020; 21; 498-509
8. Hesketh T, Wu D, Mao L, Ma N, Violence against doctors in China: BMJ, 2012; 345; e5730
9. Geoffrion S, Hills DJ, Ross HM, Education and training for preventing and minimizing workplace aggression directed toward healthcare workers: Cochrane Database Syst Rev, 2020; 9; CD011860
10. Du Y, Wang W, Washburn DJ, Violence against healthcare workers and other serious responses to medical disputes in China: Surveys of patients at 12 public hospitals: BMC Health Serv Res, 2020; 20; 253
11. Cai R, Tang J, Deng C, Violence against health care workers in China, 2013–2016: Evidence from the national judgment documents: Hum Resour Health, 2019; 17; 103
12. Yip W, Fu H, Chen AT, 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage: Lancet, 2019; 394; 1192-204
13. Zhu J, Li W, Chen L, Doctors in China: Improving quality through modernisation of residency education: Lancet, 2016; 388; 1922-29
14. , Ending violence against doctors in China: Lancet, 2012; 379; 1764
15. Yao S, Zeng Q, Peng M, Stop violence against medical workers in China: J Thorac Dis, 2014; 6(6); E141-45
16. Yang Z, Liu Y, Fan D, Workplace violence against health care workers in the United States: N Engl J Med, 2016; 375(7); e14
17. Wuellner SE, Bonauto DK, Exploring the relationship between employer recordkeeping and underreporting in the BLS Survey of Occupational Injuries and Illnesses: Am J Ind Med, 2014; 57; 1133-43
18. Kowalenko T, Gates D, Gillespie GL, Prospective study of violence against ED workers: Am J Emerg Med, 2013; 31; 197-205
19. Sullivan M, Robinson S, Littnan C, Social media as a data resource for #monkseal conservation: PLoS One, 2019; 14(10); e0222627
20. Merchant J, Lundell J: Workplace violence: A report to the nation, Injury Prevention Research Center; University of Iowa https://iprc.public-health.uiowa.edu/wp-content/uploads/2015/09/workplace-violence-report-1.pdf
21. Jia X, Zhou H, Zhao Y, Investigation on hospital violence during 2003 to 2012 in China: Chinese Hospitals, 2014; 18; 1-3
22. Mei S, Li Z, Zhang X, Qualitative data analysis of 228 cases of workplace violence on medical staffs based on internet media: Chinese Health Service Management, 2019; 36; 439-41
23. Speroni KG, Fitch T, Dawson E, Incidence and cost of nurse workplace violence perpetrated by hospital patients or patient visitors: J Emerg Nurs, 2014; 40; 218-28
24. Ji JB, Xiao JC, Research on reported hospital violence from webpage news: Medicine & Philosophy (A), 2014; 15
25. Renzi C, Abeni D, Picardi A, Factors associated with patient satisfaction with care among dermatological outpatients: Br J Dermatol, 2001; 145; 617-23
26. Wyatt R, Anderson-Drevs K, Van Male LM, Workplace violence in health care: A critical issue with a promising solution: JAMA, 2016; 316; 1037-38
27. Liu Y, Song R, Hou PC, The poor health of paediatrics in China: BMJ, 2018; 361; k2567
28. , Violence against doctors: Why China? Why now? What next?: Lancet, 2014; 383(9922); 1013
29. Wu D, Lam TP, At a crossroads: Family medicine education in China: Acad Med, 2017; 92; 185-91
30. Blumenthal D, Hsiao W, Lessons from the East – China’s rapidly evolving health care system: N Engl J Med, 2015; 372; 1281-85
31. Yip W, Hsiao W, Harnessing the privatisation of China’s fragmented health-care delivery: Lancet, 2014; 384; 805-18
32. Wang T, Zeng R, Addressing inequalities in China’s health service: Lancet, 2015; 386; 1441
33. , China’s health-care reform: An independent evaluation: Lancet, 2019; 394(10204); 1113
34. The General Office of the State Council issued the “Outline of the National Medical and Health Service System Planning (2015–2020): Xinhua News Agency [in Chinese]http://www.gov.cn/xinwen/2015-03/30/content_2840331.htm
35. World Bank Group, World Health Organization, Ministry of Finance, National Health Family Planning Commission, Ministry of Human Resources and Social Security: Deepening health reform in China. Building high-quality and value-based service delivery, 2016 https://openknowledge.worldbank.org/bitstream/handle/10986/24720/HealthReformInChina.pdf
36. Zhao S, Liu H, Ma H, Coping with workplace violence in healthcare settings: social support and strategies: Int J Environ Res Public Health, 2015; 12; 14429-44
37. Guan J, Origin and prevention of workplace violence in health care in China: Legal and ethical considerations: Chin Med J (Engl), 2017; 130; 1731-36
38. Xiong P, Hu SX, Hall BJ, Violence against nurses in China undermines task-shifting implementation: Lancet Psychiatry, 2016; 3(6); 501
39. Wu LX, Qi L, Li Y, Challenges faced by young Chinese doctors: Lancet, 2016; 387; 1617
40. Wang C, Chen S, Zhu J, Li W, China’s new 4+4 medical education programme: Lancet, 2019; 394; 1121-23
41. , The doctors’ predicament: China’s health-care growing pains: Lancet, 2019; 393; 1569
42. Horton R, Offline: Health – the Chinese dream: Lancet, 2016; 387; 212
43. Zhang Y, Feng X, Health expenditure analysis for urban and rural residents in China: Chinese J Hosp Admin, 2010; 26; 185-88
44. National Bureau of Statistics of China [in Chinese]http://data.stats.gov.cn/easyquery.htm?cn=C01
45. Wang X, Huang Y, Birch S, People engagement in health-care system transition in China: Lancet Public Health, 2019; 4; e446
46. Chen S, Wang D, Fung H, Psychological aid following medical crises in China: Lancet, 2017; 389; 250
47. National Health Commission: Statistical bulletin on China’s health care development http://www.nhc.gov.cn
48. Song P, Jin C, Tang W, New medical education reform in China: Towards healthy China 2030: Biosci Trends, 2017; 11; 366-69
49. Yu P, Yang X, Qi Z, Evaluation of doctors in China: Imperative changes are required: Lancet, 2017; 390; 121
50. Li X, Zhang X, Female doctors in China: Challenges and hopes: Lancet, 2015; 386; 1441-42
51. National Health and Family Planning Commission: China health and family planning statistical yearbook, 2019, Beijing, Peking Union Medical College Press
52. Yang C, Chen Z, Chen L, Jiang J, Burnout in healthcare: A sign of death by overwork for doctors in China: BMJ, 2019; 366; l5582
53. National Academy of Medicine: Action collaborative on clinician wellbeing and resilience https://nam.edu/initiatives/clinician-resilience-and-well-being
54. , Health-care system transition in China: Lancet, 2018; 391; 1332
55. Ze-lin Y, Hao-yue Z, Si-jia L, Right-protection by Violence in Healthcare Service and Its Governance: Based on content analysis of news reports from 2002 to 2015: Soc Constr, 2017; 4; 49-63
56. The Central People’s Government of the People’s Republic of China [in Chinese]http://www.gov.cn/xinwen/2015-02/13/content_2818685.htm
57. Yang S, Wu D, Wang N, Workplace violence and its aftermath in China’s health sector: Implications from a cross-sectional survey across three tiers of the health system: BMJ Open, 2019; 9; e031513
58. Dubb SS, It doesn’t “come with the job”: Violence against doctors at work must stop: BMJ, 2015; 350
59. Merrill DG, Speak up: JAMA, 2017; 317; 2373-74
Figures
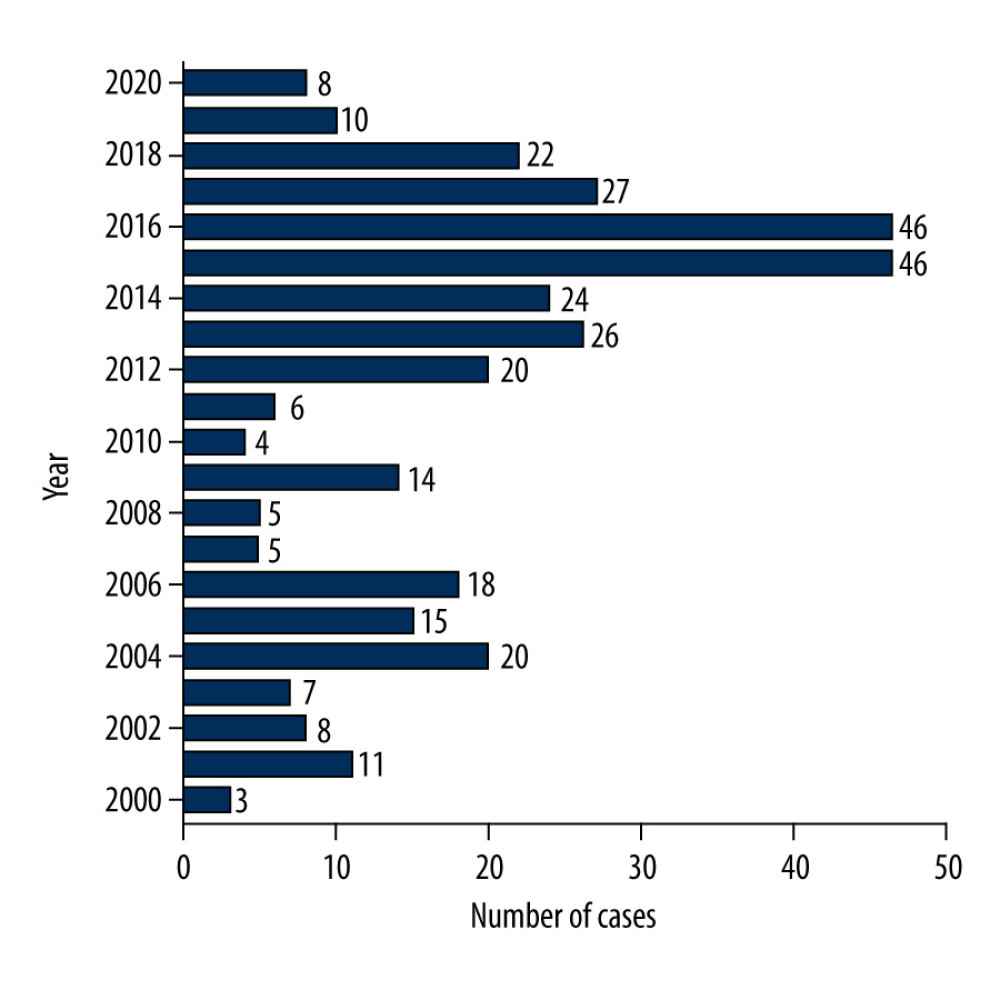 Figure 1. Violence-related injuries sustained by China’s health care workforce.
Figure 1. Violence-related injuries sustained by China’s health care workforce.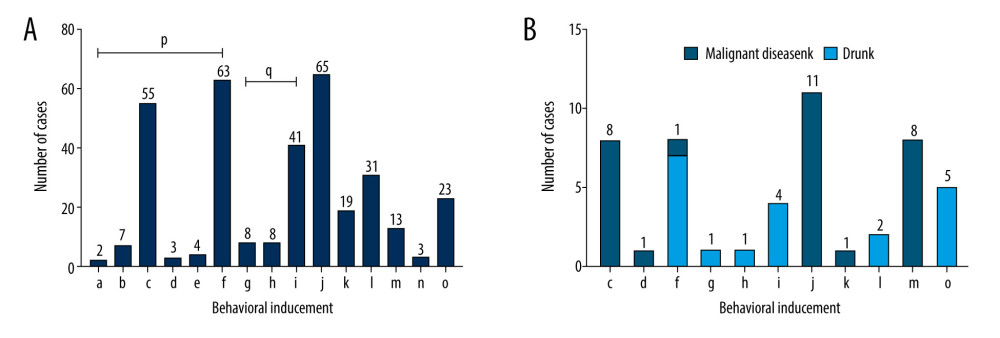 Figure 2. (A, B) Causes of hospital-based violence against medical personnel: a) overtesting of the patient by the hospital; b) misdiagnosis and delays; c) poor outcomes or sequelae; d) medical identification; e) sexual harassment; f) the health care worker’s choice of technology, diagnosis, or guidance; g) hospital charges; h) medical staff’s bearing; i) objective factors (such as provision, insufficient medical resources); j) death of the patient; k) mental state; l) absence of a valid diathesis; m) psychological distortion; n) other reasons (injury-related irritation, blackmail, or asking private questions); o) unknown reasons; p) a+b+c+d+e+f=communication; q) g+h+i=service.
Figure 2. (A, B) Causes of hospital-based violence against medical personnel: a) overtesting of the patient by the hospital; b) misdiagnosis and delays; c) poor outcomes or sequelae; d) medical identification; e) sexual harassment; f) the health care worker’s choice of technology, diagnosis, or guidance; g) hospital charges; h) medical staff’s bearing; i) objective factors (such as provision, insufficient medical resources); j) death of the patient; k) mental state; l) absence of a valid diathesis; m) psychological distortion; n) other reasons (injury-related irritation, blackmail, or asking private questions); o) unknown reasons; p) a+b+c+d+e+f=communication; q) g+h+i=service.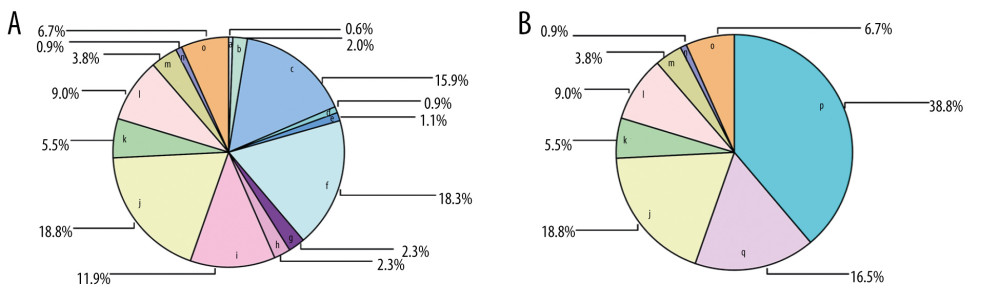 Figure 3. (A, B) The proportion of each cause of hospital-based violence. The causes of workplace violence and their representative letters (a–q) are the same as those reported in Figure 2.
Figure 3. (A, B) The proportion of each cause of hospital-based violence. The causes of workplace violence and their representative letters (a–q) are the same as those reported in Figure 2.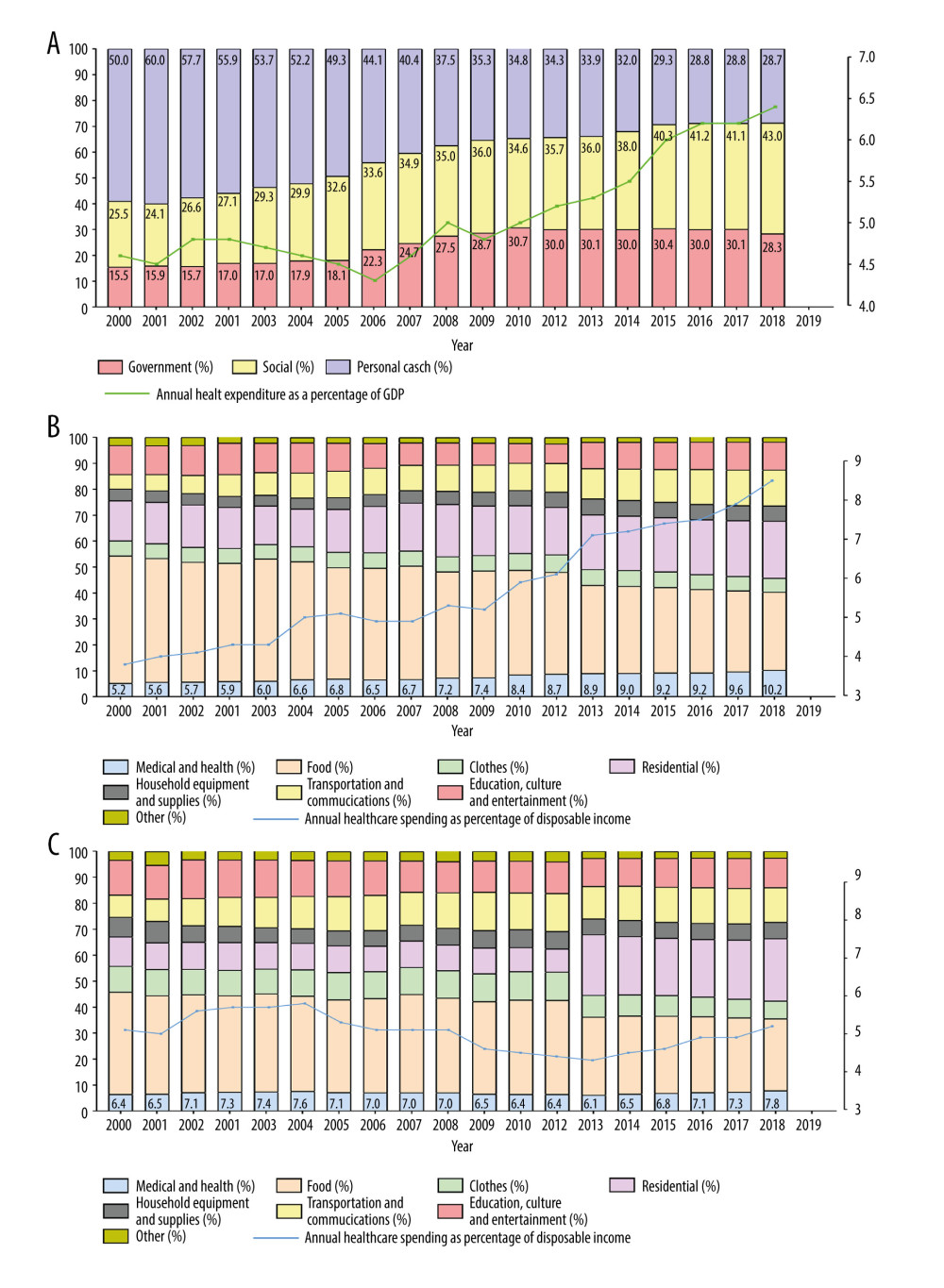 Figure 4. China’s health expenditures (A) and per capita rural (B) and urban (C) distributions of consumption expenditures. Data are from the National Bureau of Statistics [44] and the National Health Commission [47].
Figure 4. China’s health expenditures (A) and per capita rural (B) and urban (C) distributions of consumption expenditures. Data are from the National Bureau of Statistics [44] and the National Health Commission [47]. In Press
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








