23 November 2021: Clinical Research
Influence of Anterior-Posterior External Surface Perturbation on Trunk Stability During Abdominal Stabilization Strategies While Sitting
Sejun OhDOI: 10.12659/MSM.934022
Med Sci Monit 2021; 27:e934022
Abstract
BACKGROUND: Spinal and pelvic injuries during an unexpected perturbation are closely related to spinal stability, which is known to be controlled by abdominal stabilization maneuvers. This study aimed to evaluate the effects of unexpected perturbations on trunk stability and abdominal stabilization strategies in 42 sedentary adults while sitting.
MATERIAL AND METHODS: Abdominal stabilization strategies consisted of bracing and hollowing maneuvers. Abdominal bracing maneuvers (ABM) were focused on the abdominal wall muscles [inferior oblique (IO), exterior oblique (EO)], and abdominal hollowing maneuvers (AHM) were focused on deep muscle (TrA) activation. The subjects were instructed in abdominal stabilization maneuvers. Afterward, subjects were seated in a chair that could be moved forward or backward suddenly with the support surface.
RESULTS: Angular displacements of the upper thorax, lower thorax, and lumbopelvic during unexpected perturbation, with different abdominal stabilization maneuvers, were measured. During forward perturbation (d=0.71, F=10.324, P=0.001) and backward perturbation in high speed (d=0.62, F=9.265, P=0.011), there were significant differences in angular displacements of the upper thorax between hollowing and bracing maneuvers. Additionally, significant differences were found in the lumbopelvic angular displacement between the hollowing and bracing maneuvers (d=0.62, F=4.071, P=0.044).
CONCLUSIONS: Our findings indicate that the ABM is a better stabilizing technique for the upper thorax, and the AHM is a better stabilizing technique for the lumbopelvic region during unexpected perturbations at high speed in the seated position.
Keywords: Back Muscles, Pelvis, Sedentary Behavior, Sitting Position, Spine, Abdominal Muscles, Electromyography, Female, Humans, Male, Muscle Contraction, Torso
Background
Sedentary behavior involving prolonged sitting can lead to the development of various musculoskeletal disorders [1–4]. Specifically, continuous sitting increases the load on the spine by reducing lumbar lordosis and increasing posterior pelvic tilt and compression of the ischium [5]. Repeated loading of the lumbar segments leads to micro-trauma of musculoskeletal soft tissue and to spinal instability, eventually causing low back pain [6]. Furthermore, these injuries are frequently due to unexpected perturbations, which can occur not only during continuous static posture, but also during movement transfer, which is an important factor in falls [7,8]. Each of these situations can expose an individual to an unexpected moving surface while in a sitting position [1–4]. They may result in injuries to the musculoskeletal structure of the spine, which can in turn lead to a wide variety of clinical conditions that are grouped as whiplash-associated disorders [9,10]. In addition, unexpected perturbations in patients with back pain can cause muscle fatigue more easily than in healthy individuals, which may lead to injuries in the spine and pelvis [11–13].
Spinal and pelvic injuries caused by unexpected perturbations are associated with spinal instability [13–15]. Perturbations can be controlled by co-contraction of local muscles to the TrA, inferior oblique (IO), global muscles of the external oblique (EO), and surrounding tissues increases the stability of the upper and lower body balance by linking the surrounding tissues with the stabilization of the spine [16–19]. Therefore, various abdominal muscle co-contraction techniques have been developed to treat back pain in patients with spinal instability [19,20]. Among abdominal muscle co-contraction techniques, abdominal hollowing and bracing maneuvers are commonly used in clinical setting [20–23]. Abdominal hollowing maneuvers (AHM) is a technique for individually contracting local muscles such as the TrA with detailed movements as if halting urination [24]. Abdominal bracing maneuvers (ABM) is a technique that focuses on global muscles such as the EO and IO through overall contraction, induced by thinking of the abdomen like a jar [25–27]. These techniques of abdominal stabilization can be used consciously or activation patterns of abdominal muscles can be engaged automatically upon retraining of motor control [28–30]. Recently, the focus of rehabilitation programs for patients with low back pain has shifted to the technique called the hollowing maneuver, which restores motor control of key stabilization muscles, including the transversus abdominis [31–33].
However, the effectiveness of AHM and ABM on trunk stability has been debated for several years. Some studies have reported that the hollowing maneuver improves trunk stability during unexpected perturbation [21,34]. In contrast, other studies have found that ABM, but not AHM, improves trunk stability during unexpected perturbations [15,19]. Therefore, this study compared the differences between the AHM and ABM for trunk stability in the sitting position by motion analysis. An unexpected perturbation was created to prove momentary trunk stability by abdominal stabilization maneuvers.
This study aimed to evaluate the effects of unexpected perturbations on trunk stability and abdominal stabilization strategies in 42 adults in a sitting position. Therefore, we attempted to identify the factors associated with the different velocities in order to determine the relationship between the trunk segments and the stipulated maneuvers.
Material and Methods
PARTICIPANTS:
All subjects provided written informed consent prior to participation, and the study was approved by the Institutional Review Board of Korea University (IRB No: KU-IRB-13-20-A-2). Forty-two sedentary adults (21 men and 21 women; age: 25.45±3.22 years; height: 166.80±6.79 cm; weight: 62.45±11.72 kg) participated in this study. Participants were recruited for the study using advertisements in the Korea University and local community near the university. The sample size was calculated using G*power 3.1.7 (Franz Faul, Universitätkiel, Germany). Based on the method of calculation used in a previous study [35], we determined mean dispersion (502.445) and within-group dispersion (4294.34) of the trunk stability for AHM and ABM. The inclusion criteria were (1) sedentary behavior and absence of a history of physical or mental disorders or chronic non-specific low back pain within the last 3 months, and (2) absence of any history of neurological problems and vestibular deficiency in the past year. The exclusion criteria were (1) previous spinal surgery, (2) disc herniation within the last 3 months, and (3) spinal deformities such as scoliosis, kyphosis, or lordosis.
EQUIPMENT:
An ultrasound machine (Volusion I, GE Medical Systems, London, UK) with a 7.5 MHz linear head transducer (RSP6-RS, GE Medical Systems, London, UK) was used to measure thickness of the external oblique, internal oblique, and transversus abdominis muscles in real time and to teach abdominal stabilization maneuvers such as AHM and ABM.
Pre-defined perturbations were created using a custom-built moving platform (1.62 m long, 0.93 m wide, 0.35 m high), which was shifted forward or backward by 10 cm, with an initial period of acceleration (peak: 1.3 m/s2; high speed: 100 ms; medium speed: 300 ms; low speed: 500 ms) followed by a 2-s period of constant velocity (0.005 m/s) and a period of deceleration (peak: 1.7 m/s2; duration 200 ms) [36]. The perturbation movement was controlled using the commercial software PANATERM, version 5.0, (Panasonic, Gadomasi, Osaka, Japan).
Kinematics of subjects was measured using a motion capture system (Motion Analysis Corporation, Santa Rosa, CA, USA) with 6 cameras at a sampling rate of 200 Hz. A total of 11 reflective markers were positioned in the thoracic (6 markers) and lumbopelvic (5 markers) regions following a modified Helen-Hayes placement (Figure 1). A set of 3 reference markers was used during perturbation.
EXPERIMENTAL PROCEDURE:
The experimental system setup is depicted in Figure 2. The subject was seated in a chair supported by a platform that could be moved suddenly in the forward or backward direction. The subject was asked to sit with the arms crossed on the shoulders and the eyes open and was supported with a harness for safety [37]. The lower extremities were fixed to the chair to eliminate their role during perturbations.
An ultrasound transducer was transversely attached across the umbilicus and anterior axillary midline between the 12th rib and the iliac crest to obtain an accurate image [38]. The subject could see the ultrasound image in real time. Using these images, a physical therapist with 7 years of experience educated the subjects regarding natural maneuver and 2 abdominal stabilization maneuvers (AHM and ABM).
In the natural maneuver, the subject was instructed to breathe comfortably without moving the trunk, back, or pelvis. During the AHM, the subject was initially asked to inhale and exhale deeply and slowly 3 times for abdominal muscle relaxation. Immediately following this, the subject was instructed to draw the navel in slowly without moving the trunk, back, or pelvis [32,34,39]. During the ABM, the subject inhaled and exhaled deeply 3 times for abdominal muscle relaxation. Following the relaxation, the subject was instructed to push out all the abdominal muscles slowly without moving the trunk, back, or pelvis [32,33].
We confirmed that the subject was appropriately trained in all the abdominal stabilization maneuvers using the ultrasound machine by ensuring that the AHM induced isolated contraction of the transversus abdominis and the bracing maneuver induced co-contraction of the external and internal oblique muscles [18].
Thirty minutes later, the subject was tested using perturbation. Two types of unexpected perturbation (forward and backward) and 3 strategies (natural, AHM, and ABM) were used. During every perturbation, the subjects were encouraged to maintain balance and upright posture. After every perturbation with each of the 3 stabilization maneuvers, the subject was permitted to relax while the platform was moved slowly to the original position. Each subject underwent a total of 54 trials in a random order, with 3 abdominal stabilization maneuvers, 3 perturbation speeds, and 2 perturbation directions. Each perturbation was preceded by a random 10–30 s interval to reduce any confounding effects due to anticipation [40]. A short break was allowed after every 6 trials to minimize discomfort and fatigue.
KINEMATIC ANALYSIS:
The trunk was divided into 3 segments: the upper thorax (T1–T6), lower thorax (T7–T12), and lumbopelvis (L1–L5). The centers of mass of each trunk segment and the combined trunk segments in the sitting position were the kinematic variables of interest in this study. Marker position trajectories were sampled at 200 Hz and low-pass filtered to 6 Hz. The kinematic variables of interest were filtered again, with a cut-off frequency of 3.5 Hz, in order to retain at least 95% of the frequency power spectrum to obtain precise data [41].
DATA ANALYSIS:
Angular displacements of each trunk segment were analyzed using CORTEX software, version 1.0 (Motion Analysis Corporation, Santa Rosa, CA, USA). The absolute values of all angular displacements were calculated using the difference between the maximal and minimal values during the time interval from 100 ms before to 1.5 s after the onset of the perturbation with the help of MATLAB software (MathWorks Inc, Natick, MA, USA).
STATISTICAL ANALYSIS:
We performed 3×3×2×3 repeated-measures analysis of variance (ANOVA) with repeated measures to analyze the differences among the 3 trunk segments (the upper thorax, lower thorax, and lumbopelvis), speeds (low, medium, and high), abdominal stabilization maneuvers (natural, AHM, and ABM) and directions (forward and backward perturbation). Post hoc analyses were conducted using Tukey’s honest significant difference. Cohen’s d effect size index (
Results
FORWARD PERTURBATION:
During forward perturbation at the high speed, there were significant differences in the angular displacements of the upper thorax between the 3 maneuvers (natural and AHM: d=0.58, F=30.257, P=0.000; natural and ABM: d=0.52, F=9.345, P=0.005; AHM and ABM: d=0.71, F=10.324, P=0.001) (Figure 3, Table 1). For the lower thorax, there were significant differences between the natural and AHM (d=0.69; F=7.038; P=0.006) and the natural and ABM (d=0.73; F=5.936; P=0.01) but not between the AHM and ABM (d=0.56; P>0.05). For the lumbopelvis, a significant difference was observed only between the natural and ABM (d=0.61; F=10.629; P=0.001).
In contrast, at the low and medium speeds, we did not observe any significant differences in trunk stability in the upper thorax, lower thorax, and lumbopelvis regions.
BACKWARD PERTURBATION:
During backward perturbation at the high speed, there were significant differences in the angular displacements of the upper thorax between the natural and AHM (d=0.75; F=17.957; P=0.000), natural and ABM (d=0.72; F=8.750; P=0.001), and AHM and ABM (d=0.62; F=9.265; P=0.011) maneuvers (Figure 4, Table 2). There were also significant differences in the angular displacements of the lower thorax between the natural and AHM (d=0.45; F=8.750; P=0.049), natural and ABM (d=0.35; F=11.275; P=0.04), and ABM and AHM (d=0.67; F=6.648; P=0.07) maneuvers. In contrast, for the lumbopelvis, significant differences were present between the natural and AHM (d=0.55; F=4.923; P=0.048) and AHM and ABM (d=0.62; F=4.071; P=0.044) but not between the natural and ABM (d=0.10; P>0.05).
At the low and medium speeds, there were small differences for the upper thorax between the 3 maneuvers, but no significant differences were observed for the other spinal segments (
Discussion
We found that abdominal stabilization maneuvers may be specific to each segment. Specifically, the ABM was the most stabilizing technique for the upper thorax, whereas the AHM was the most stabilizing technique for the lumbopelvis.
In detail, in the fast forward perturbation, ABM had smaller angular displacement than AHM in the upper thorax, AHM was smaller than ABM in the lower thorax, and the lumbopelvis had a smaller angular displacement in AHM than in ABM. In the fast backward perturbation, ABM had smaller angular displacement than AHM in upper thorax, AHM had smaller angular displacement than ABM in lower thorax, and AHM was also smaller than ABM in the lumbopelvis. As for the front and rear perturbations, the upper thorax showed a tendency to be more stable than the ABM since the ABM had a smaller angular displacement. In both the lower thorax and the lumbopelvis, the AHM showed a tendency to be more stable than the ABM since the angular displacement was smaller than that of the ABM.
Generally, AHM and ABM are specialized methods used for trunk stabilization [17,18,21,32]. However, no previous study identified the different roles played in each segment of the trunk by the AHM and ABM. In this study, at high speed, segmental trunk stabilization focused on an abdominal strategy, with the application of the AHM and ABM according to increased body sway.
Although similar studies were performed in the past [12,33,40,42], we characterized these effects using more independent variables to obtain a clearer picture of trunk stabilization. A previous study compared only abdominal maneuver strategies, whereas we included 2 more variables, the trunk segment and perturbation speed. Additionally, the present study tested trunk stability under conditions that better approximate a sitting position compared to other studies, one of which [18,43] utilized a special semi-seated position. The current study was performed in a comfortable sitting position and focused on trunk stability in real life scenarios.
Previous studies that have investigated the stabilization maneuvers against unexpected perturbations in the standing position, highlighted the importance of core stability in relation to stabilization maneuvers [36,44]. In contrast, in the current study, there was no difference between detailed AHM and ABM. Furthermore, the previous study was focused on the abdominal part, but it was showed that the bracing maneuvers performed better than AHM in stabilizing the spine during fast perturbations in the sitting position. However, we investigated the specific abdominal stabilization maneuvers in the sitting position in the following 3 segments of the upper body: the upper thorax (T1–T6), lower thorax (T7–T12), and lumbopelvis (L1–L5).
Our study has several potential clinical implications. The ABM appears to be more efficient in preventing the whiplash syndrome during activities of daily living [9] since the upper thorax is anatomically connected to the head and cervical spine. On the other hand, the AHM decreases the moment arm of the abdominal muscles against the lumbar spine, which could affect trunk and pelvic stabilization. Therefore, the AHM should be more efficient in spine stabilization and other problems related to lumbopelvic coordination [45]. These results also suggest that the clinical outcomes of existing clinical interventions focus on transverse abdominis for AHM [41–45] and all the abdominal muscles for ABM [46], but also is an important consideration in the transition from abdominal maneuver to stabilization during the trunk segment. The limitation of our study was that because only sedentary adults were included, the results cannot be readily extended to individuals with low back pain. We did not measure the angular displacements of cervical part. Future studies should consider a more specific distinction based on participant’s whole-body system. In addition, due to our small sample size, it is difficult to generalize the results.
Conclusions
The present study compared the influence of unexpected perturbations on trunk stability during abdominal stabilization strategies while sitting. Our findings indicate that the ABM is a more appropriate stabilizing technique for the upper thorax than AHM, while AHM is a better technique for lumbopelvis compared to ABM at high perturbation speed. Therefore, for better trunk stability, we recommend focusing on the ABM for upper thorax and the AHM for lumbopelvis. Clinically, ABM is used for cervical spine stability, such as forward head posture (turtleneck syndrome), and AHM recommends interventions suitable for each situation to enhance the stability of the lumbar and pelvic regions.
Figures
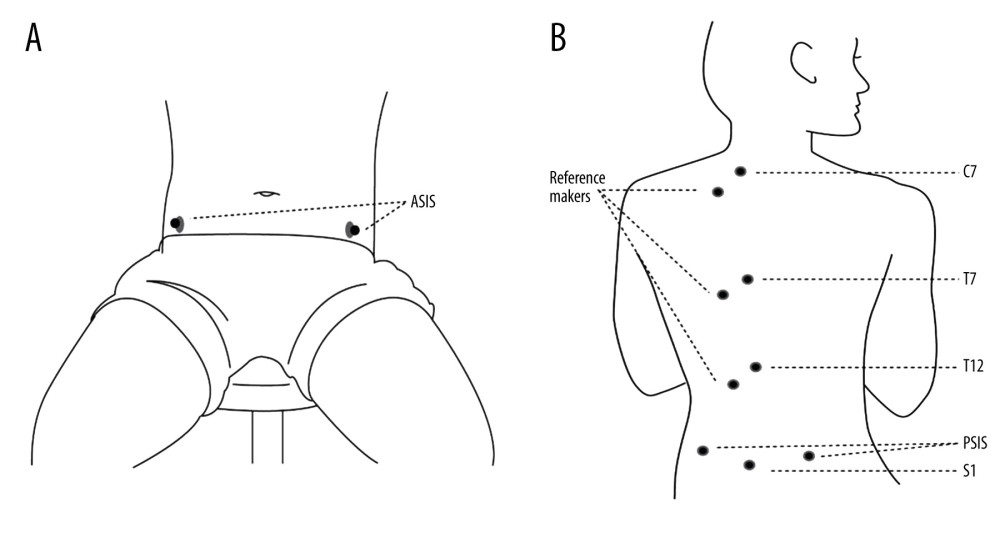 Figure 1. Skin-based marker placement: (A) anterior-superior iliac spine (ASIS); (B) cervical 7 (C7), thoracic 7 (T7), thoracic 12 (T12), and 3 reference makers at the posterior-superior iliac spine (PSIS) and sacrum (S1).
Figure 1. Skin-based marker placement: (A) anterior-superior iliac spine (ASIS); (B) cervical 7 (C7), thoracic 7 (T7), thoracic 12 (T12), and 3 reference makers at the posterior-superior iliac spine (PSIS) and sacrum (S1). 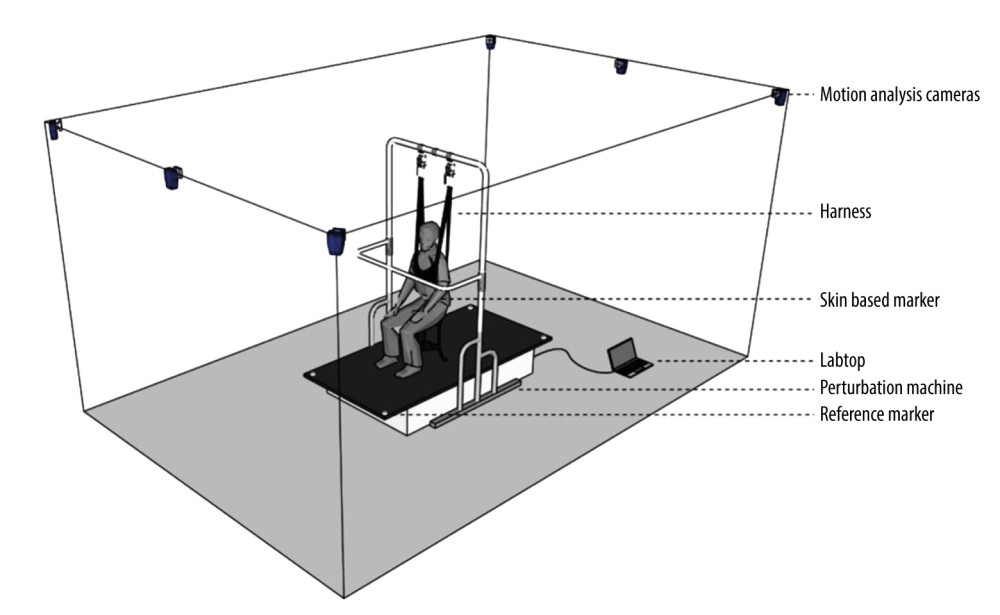 Figure 2. The experimental setup: subjects were asked to sit in a chair that was fixed on a supporting platform with the arms crossed on the shoulders and the eyes open. The moving platform (1.62 m long, 0.93 m wide, 0.35 m high) created unexpected perturbations in the forward and backward directions.
Figure 2. The experimental setup: subjects were asked to sit in a chair that was fixed on a supporting platform with the arms crossed on the shoulders and the eyes open. The moving platform (1.62 m long, 0.93 m wide, 0.35 m high) created unexpected perturbations in the forward and backward directions. 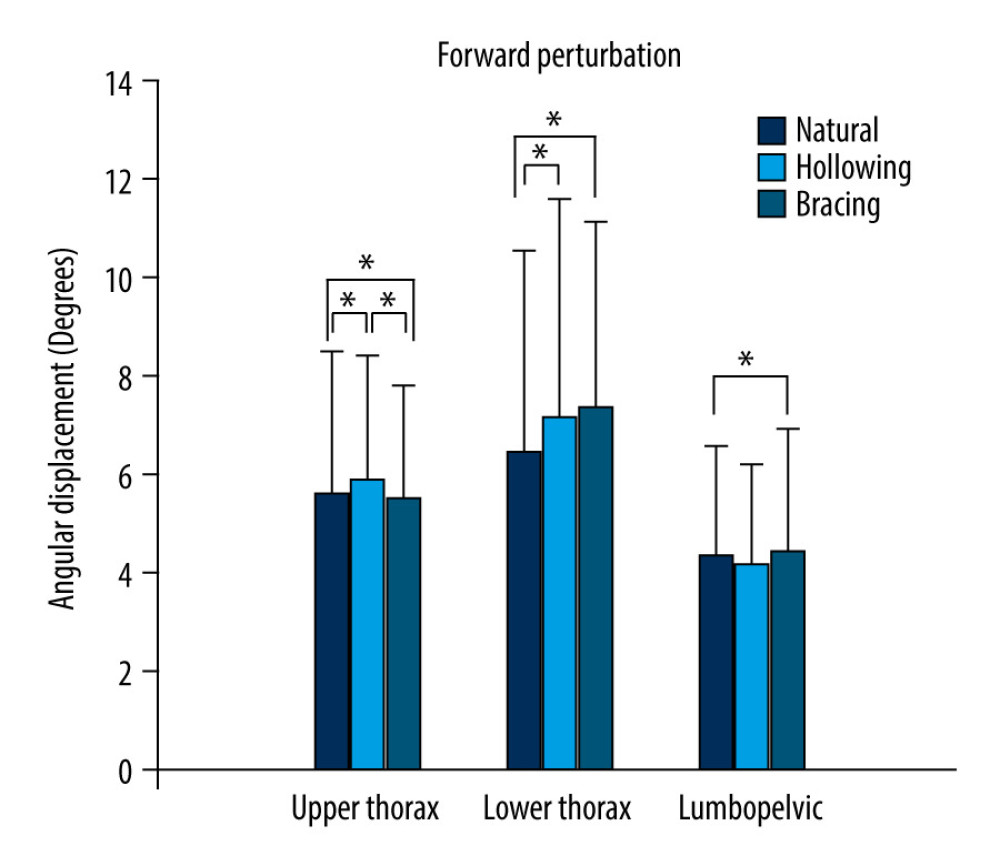 Figure 3. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during forward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05.
Figure 3. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during forward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05. 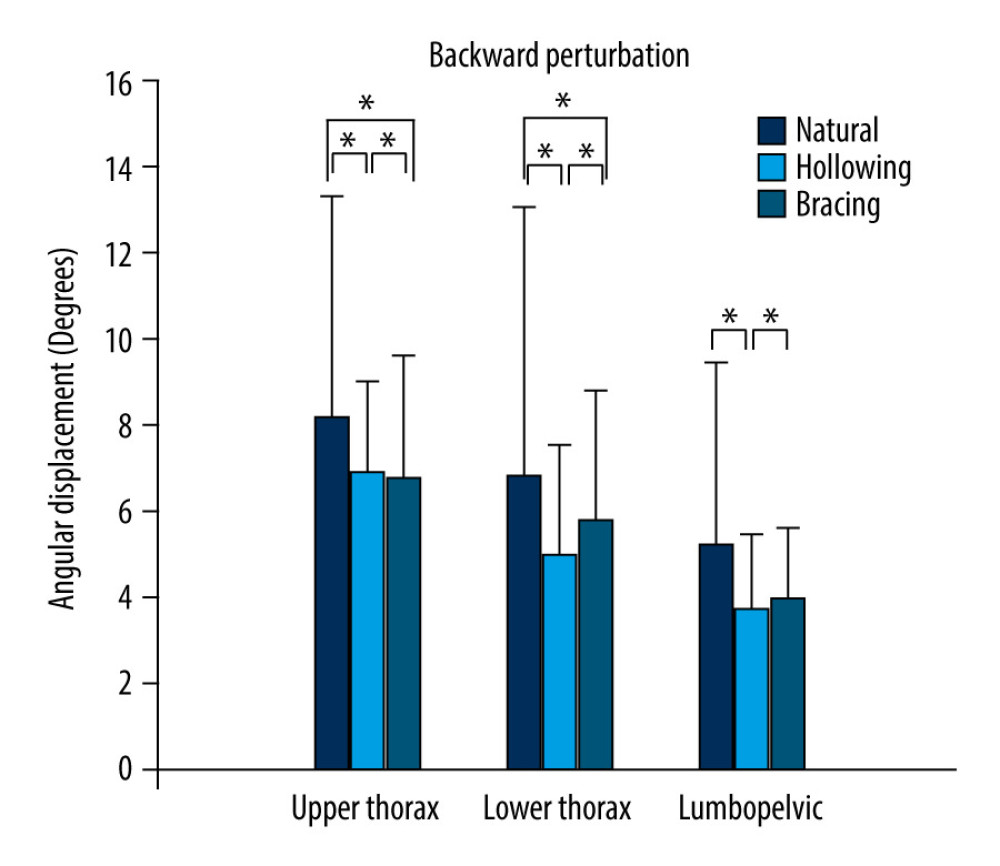 Figure 4. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during backward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05.
Figure 4. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during backward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05. References
1. Corlett E, Sitting as a hazard: Safety Science, 2008; 46(5); 815-21
2. del Pozo-Cruz B, Gusi N, Adsuar JC, Musculoskeletal fitness and health-related quality of life characteristics among sedentary office workers affected by sub-acute, non-specific low back pain: A cross-sectional study: Physiotherapy, 2013; 99; 194-200
3. Hootman JMMC, Ainsworth BE, Addy CL, Epidemiology of musculoskeletal injuries among sedentary and physically active adults: Med Sci Sports Exerc, 2002; 34; 838-44
4. Sitthipornvorakul E, Janwantanakul P, Lohsoonthorn V, The effect of daily walking steps on preventing neck and low back pain in sedentary workers: A 1-year prospective cohort study: Eur Spine J, 2015; 24; 417-24
5. Makhsous M, Lin F, Bankard J, Biomechanical effects of sitting with adjustable ischial and lumbar support on occupational low back pain: Evaluation of sitting load and back muscle activity: BMC Musculoskelet Disord, 2009; 10; 17
6. McGill SM, The biomechanics of low back injury: Implications on current practice in industry and the clinic: J Biomech, 1997; 30(5); 465-75
7. Jeon W, Whitall J, Griffin L, Westlake KP, Trunk kinematics and muscle activation patterns during stand-to-sit movement and the relationship with postural stability in aging: Gait Posture, 2021; 86; 292-98
8. Jeon W, Hsiao HY, Griffin L, Effects of different initial foot positions on kinematics, muscle activation patterns, and postural control during a sit-to-stand in younger and older adults: J Biomech, 2021; 117; 110251
9. Cote JN, Patenaude I, St-Onge N, Fung J, Whiplash-associated disorders affect postural reactions to antero-posterior support surface translations during sitting: Gait Posture, 2009; 29; 603-11
10. Panjabi MM, The stabilizing system of the spine, part I. Function, dysfunction, adaptation, and enhancement: J Spinal Disord, 1992; 5; 383-89
11. Jubany J, Danneels L, Angulo-Barrose R, The influence of fatigue and chronic low back pain on muscle recruitment patterns following an unexpected external perturbation: BMC Musculoskelet Disord, 2017; 18; 1-10
12. Manning DPMR, Blanchfield LP, Body movements and events contributing to accidental and nonaccidental back injuries: Spine, 1984; 9; 734-39
13. Marras WSRS, Lavender SA, Trunk loading and expectation: Ergonomics, 1987; 30; 551-62
14. Mok NW, Brauer SG, Hodges PW, Changes in lumbar movement in people with low back pain are related to compromised balance: Spine (Phila Pa 1976), 2011; 36; E45-52
15. Andersen TB, Essendrop M, Schibye B, Movement of the upper body and muscle activity patterns following a rapidly applied load: the influence of pre-load alterations: Eur J Appl Physiol, 2004; 91; 488-92
16. Essendrop MAT, Schibye B, Increase in spinal stability obtained at levels of intra-abdominal pressure and back muscle activity realistic to work situations: Appl Ergon, 2002; 33; 471-76
17. Stokes IA, Gardner-Morse MG, Henry SM, Abdominal muscle activation increases lumbar spinal stability: Analysis of contributions of different muscle groups: Clin Biomech (Bristol, Avon), 2011; 26; 797-803
18. Vera-Garcia FJ, Elvira JL, Brown SH, McGill SM, Effects of abdominal stabilization maneuvers on the control of spine motion and stability against sudden trunk perturbations: J Electromyogr Kinesiol, 2007; 17; 556-67
19. Macedo LGMC, Latimer J, McAuley JH, Motor control exercise for persistent, nonspecific low back pain: A systematic review: Physical Therapy, 2009; 89; 9-25
20. Richardson CAHP, Hides JA: Therapeutic exercise for spinal segmental stabilization in low back pain: Scientific basis and clinical approach, 1999, Churchill Livingstone
21. Beith ID, Synnott RE, Newman SA, Abdominal muscle activity during the abdominal hollowing manoeuvre in the four-point kneeling and prone positions: Man Ther, 2001; 6; 82-87
22. Oshikawa T, Adachi G, Akuzawa H, Electromyographic analysis of abdominal muscles during abdominal bracing and hollowing among six different positions. J: Phys Fit Sports Med, 2020; 9; 157-63
23. Vera-Garcia FJ, Elvira JL, Brown SH, McGill SM, Effects of abdominal stabilization maneuvers on the control of spine motion and stability against sudden trunk perturbations: J Electromyogr Kinesiol, 2007; 17(5); 556-67
24. Chanthapetch P, Kanlayanaphotporn R, Gaogasigam C, Chiradejnant A, Abdominal muscle activity during abdominal hollowing in four starting positions: Man Ther, 2009; 14(6); 642-46
25. Kim M, Kim Y, Oh S, Abdominal hollowing and bracing strategies increase joint stability in the trunk region during sudden support surface translation but not in the lower extremities: J Back Musculoskelet Rehabil, 2016; 27; 317-25
26. Hwang JH, Sung KS, Yi CH, Effects of abdominal hollowing and bracing maneuvers on hip extension strength in prone standing position: J Back Musculoskelet Rehabil, 2020; 28; 161-69
27. Maeo S, Takahashi T, Takai Y, Kanehisa H, Trunk muscle activities during abdominal bracing: comparison among muscles and exercises: J Sports Sci Med, 2013; 12(3); 467-74
28. Allison GTGP, Robinson G, EMG signal amplitude assessment during abdominal bracing and hollowing: J Electromyogr Kinesiol, 1998; 8; 51-57
29. Kavcic NGS, McGill SM, Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises: Spine, 2004; 29; 2319-29
30. O’Sullivan PBTL, Allison GT, Altered abdominal muscle recruitment in patients with chronic back pain following a specific exercise intervention: J Orthop Sports Phys Ther, 1998; 27; 114-24
31. Hides JWS, Stanton W, McMahon S, An MRI investigation into the function of the transversus abdominis muscle during “drawing-in” of the abdominal wall: Spine, 2006; 31; E175-78
32. Jull GARC, Motor control problems in patients with spinal pain: A new direction for therapeutic exercise: J Manipulative Physiol Ther, 2000; 23; 115-17
33. Urquhart DM, Hodges PW, Allen TJ, Story IH, Abdominal muscle recruitment during a range of voluntary exercises: Man Ther, 2005; 10; 144-53
34. Suehiro T, Mizutani M, Watanabe S, Comparison of spine motion and trunk muscle activity between abdominal hollowing and abdominal bracing maneuvers during prone hip extension: J Bodyw Mov Ther, 2014; 18; 482-88
35. Grenier SG, McGill SM, Quantification of lumbar stability by using 2 different abdominal activation strategies: Arch Phys Med Rehabil, 2007; 88; 54-62
36. Kim Y, Shim JK, Son J, A neuromuscular strategy to prevent spinal torsion: backward perturbation alters asymmetry of transversus abdominis muscle thickness into symmetry: Gait Posture, 2013; 38; 231-35
37. Bobet J, Masani K, Popovic MR, Vette AH, Kinematics-based prediction of trunk muscle activity in response to multi-directional perturbations during sitting: Med Eng Phys, 2018; 58; 56-63
38. Arab AM, Chehrehrazi M, Ultrasound measurement of abdominal muscles activity during abdominal hollowing and bracing in women with and without stress urinary incontinence: Man Ther, 2011; 16; 596-601
39. Monfort-Panego M, Vera-Garcia FJ, Sanchez-Zuriaga D, Sarti-Martinez MA, Electromyographic studies in abdominal exercises: A literature synthesis: J Manipulative Physiol Ther, 2009; 32; 232-44
40. Carpenter MG, Tokuno CD, Thorstensson A, Cresswell AG, Differential control of abdominal muscles during multi-directional support-surface translations in man: Exp Brain Res, 2008; 188; 445-55
41. Kim M, Kim Y, Oh S, Abdominal hollowing and bracing strategies increase joint stability in the trunk region during sudden support surface translation but not in the lower extremities: J Back Musculoskelet Rehabil, 2016; 29; 317-25
42. St-Onge N, Côté JN, Preuss RA, Direction-dependent neck and trunk postural reactions during sitting: J Electromyogr Kinesiol, 2011; 21; 904-12
43. Kasahara S, Miyamoto K, Takahashi M, Lumbar-pelvic coordination in the sitting position: Gait Posture, 2008; 28; 251-57
44. Cresswell AG, Oddsson L, Thorstensson A, The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure while standing: Exp Brain Res, 1994; 98(2); 336-41
45. Manshadi FD, Parnianpour M, Sarrafzadeh J, Abdominal hollowing and lateral abdominal wall muscles’ activity in both healthy men & women: An ultrasonic assessment in supine and standing positions: J Bodyw Mov Ther, 2011; 15; 108-13
46. Brown SHM, Vera-Garcia FJ, McGill SM, Effects of abdominal muscle coactivation on the externally preloaded trunk: Variations in motor control and its effect on spine stability: Spine, 2006; 31; E387-93
Figures
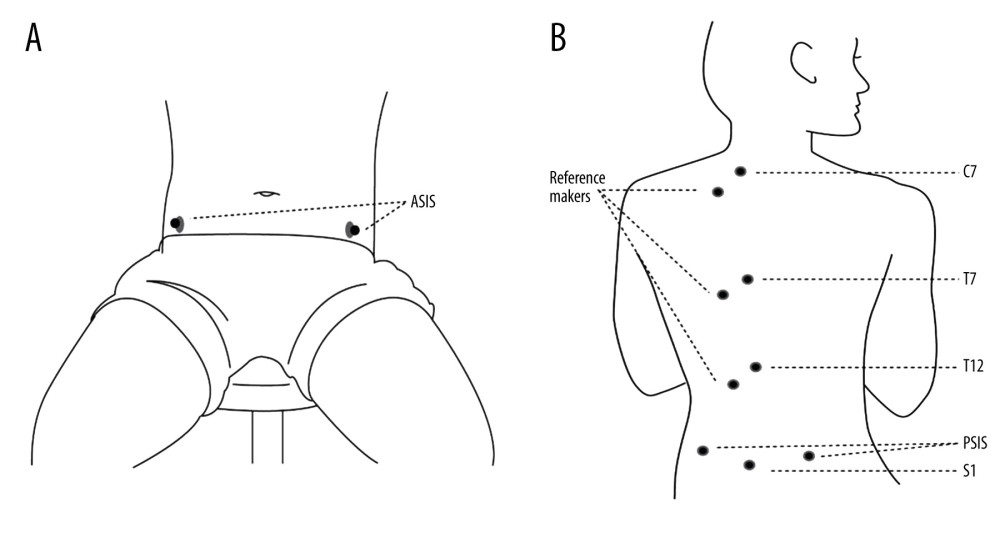 Figure 1. Skin-based marker placement: (A) anterior-superior iliac spine (ASIS); (B) cervical 7 (C7), thoracic 7 (T7), thoracic 12 (T12), and 3 reference makers at the posterior-superior iliac spine (PSIS) and sacrum (S1).
Figure 1. Skin-based marker placement: (A) anterior-superior iliac spine (ASIS); (B) cervical 7 (C7), thoracic 7 (T7), thoracic 12 (T12), and 3 reference makers at the posterior-superior iliac spine (PSIS) and sacrum (S1).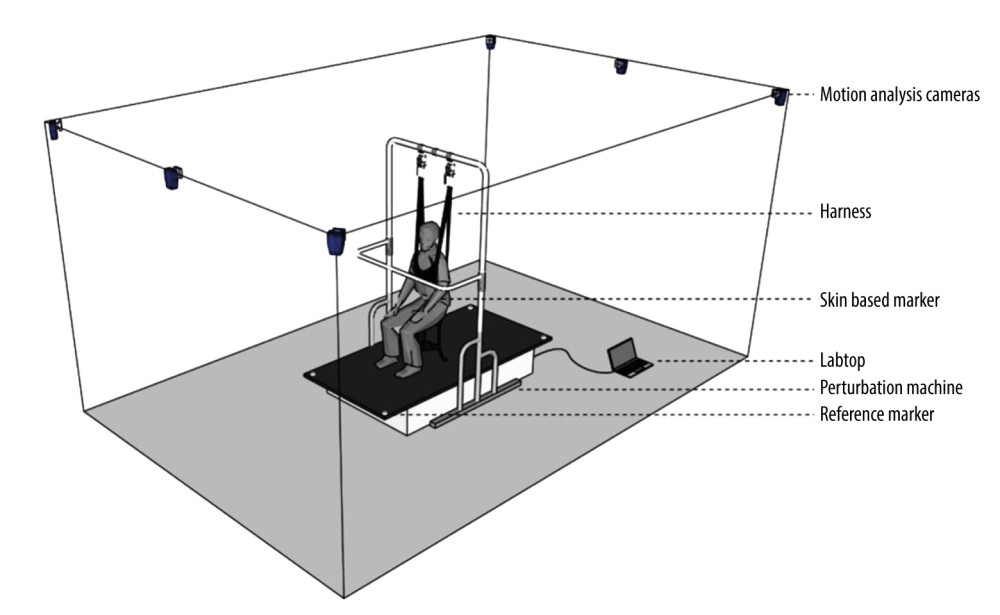 Figure 2. The experimental setup: subjects were asked to sit in a chair that was fixed on a supporting platform with the arms crossed on the shoulders and the eyes open. The moving platform (1.62 m long, 0.93 m wide, 0.35 m high) created unexpected perturbations in the forward and backward directions.
Figure 2. The experimental setup: subjects were asked to sit in a chair that was fixed on a supporting platform with the arms crossed on the shoulders and the eyes open. The moving platform (1.62 m long, 0.93 m wide, 0.35 m high) created unexpected perturbations in the forward and backward directions.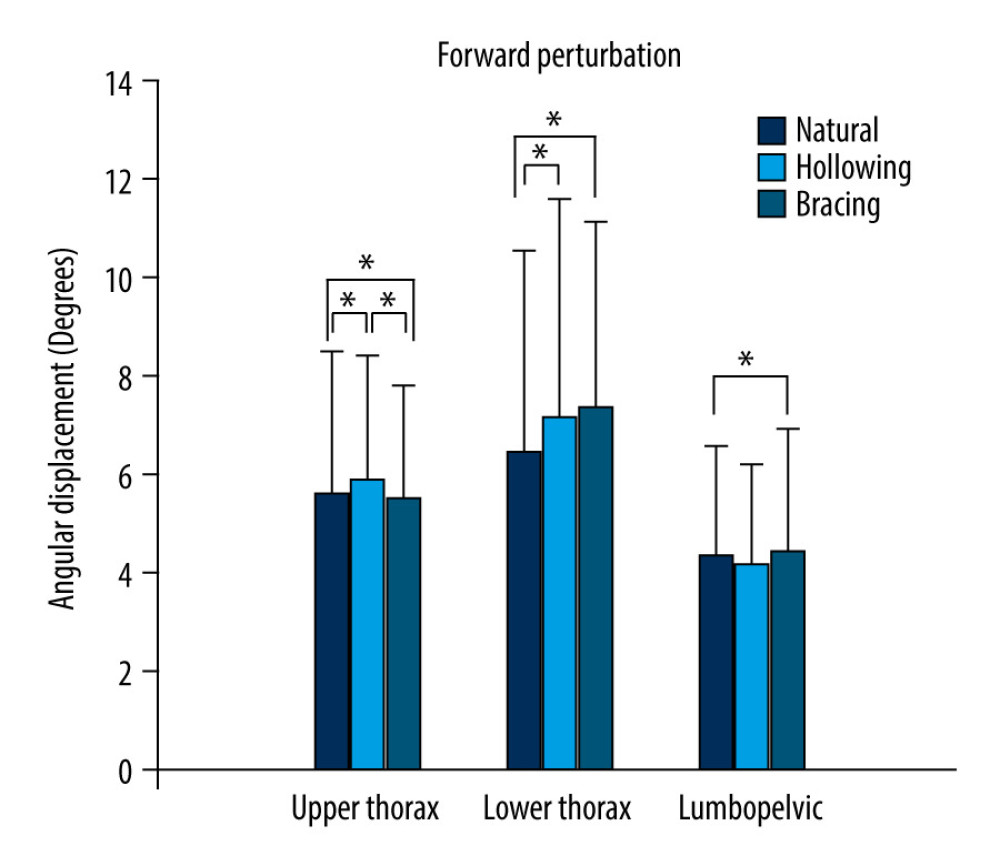 Figure 3. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during forward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05.
Figure 3. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during forward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05.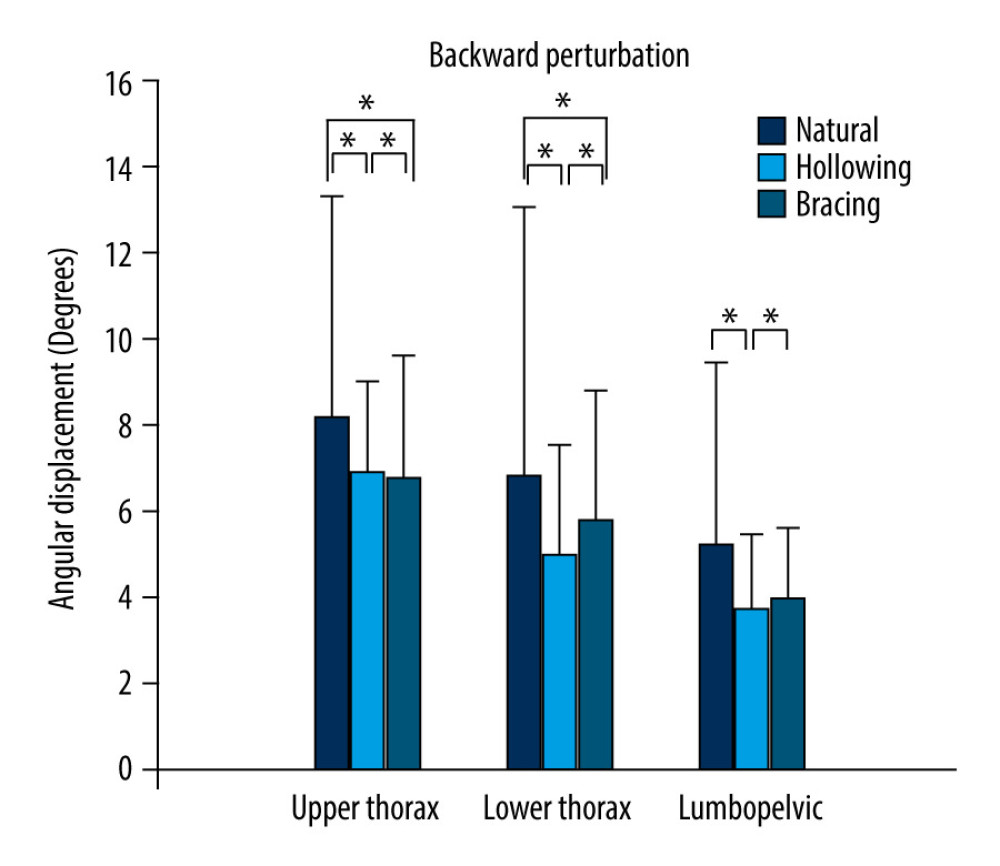 Figure 4. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during backward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05.
Figure 4. Angular displacements of the upper thorax, lower thorax, and lumbopelvis during backward perturbation in high speeds when using 3 different abdominal stabilization maneuvers. The data are presented as mean±SD. * P<0.05. Tables
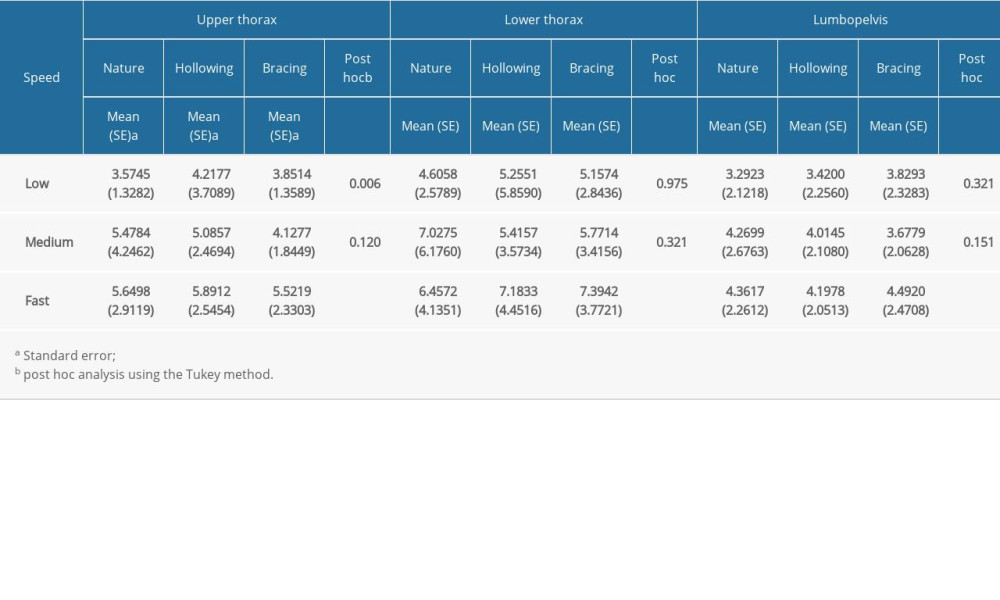 Table 1. Outcome of forward perturbation tests in upper thorax, lower thorax, and lumbopelvis.
Table 1. Outcome of forward perturbation tests in upper thorax, lower thorax, and lumbopelvis.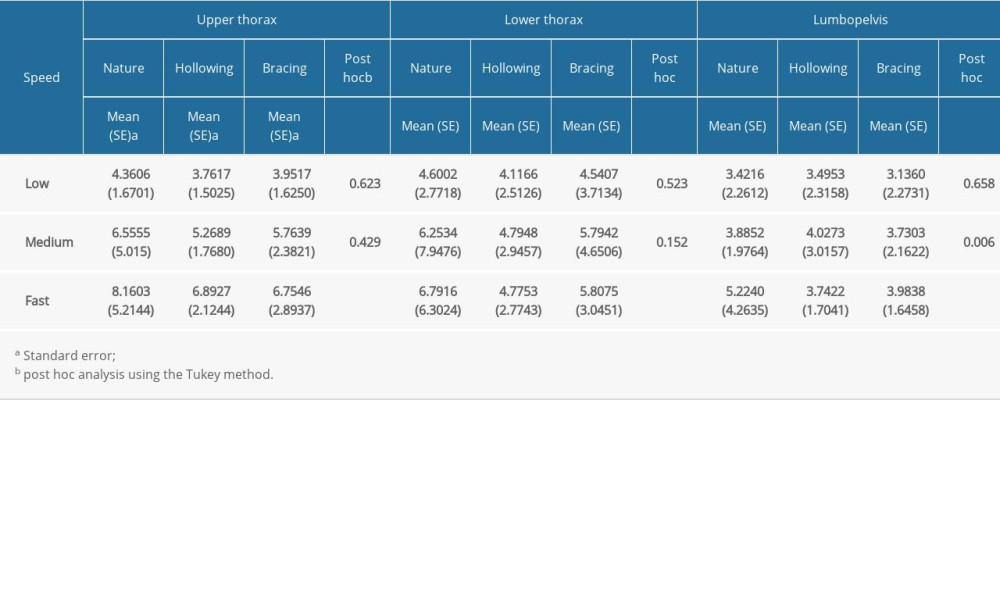 Table 2. Outcome of backward perturbation tests in upper thorax, lower thorax, and lumbopelvis.
Table 2. Outcome of backward perturbation tests in upper thorax, lower thorax, and lumbopelvis.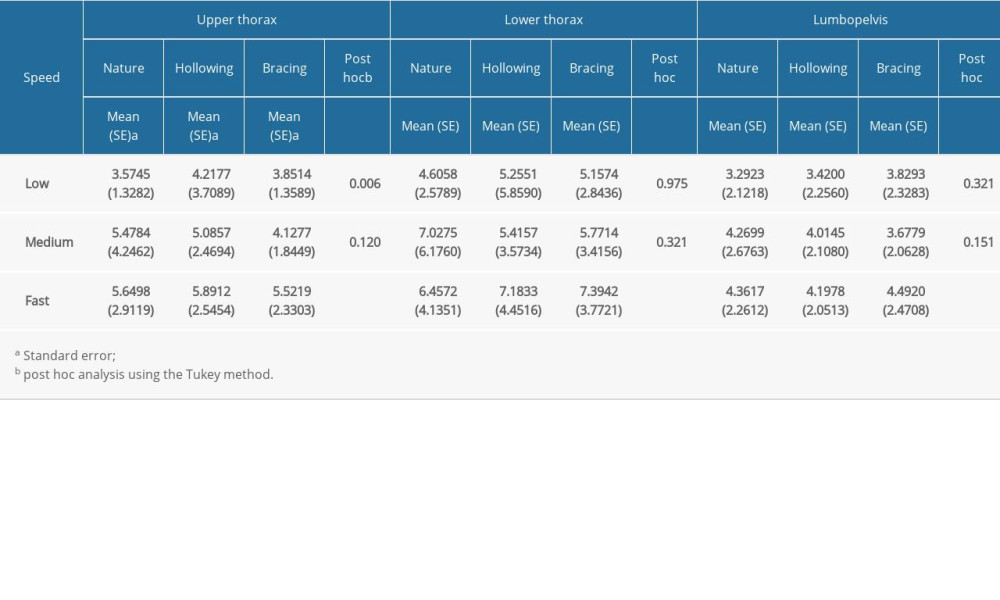 Table 1. Outcome of forward perturbation tests in upper thorax, lower thorax, and lumbopelvis.
Table 1. Outcome of forward perturbation tests in upper thorax, lower thorax, and lumbopelvis.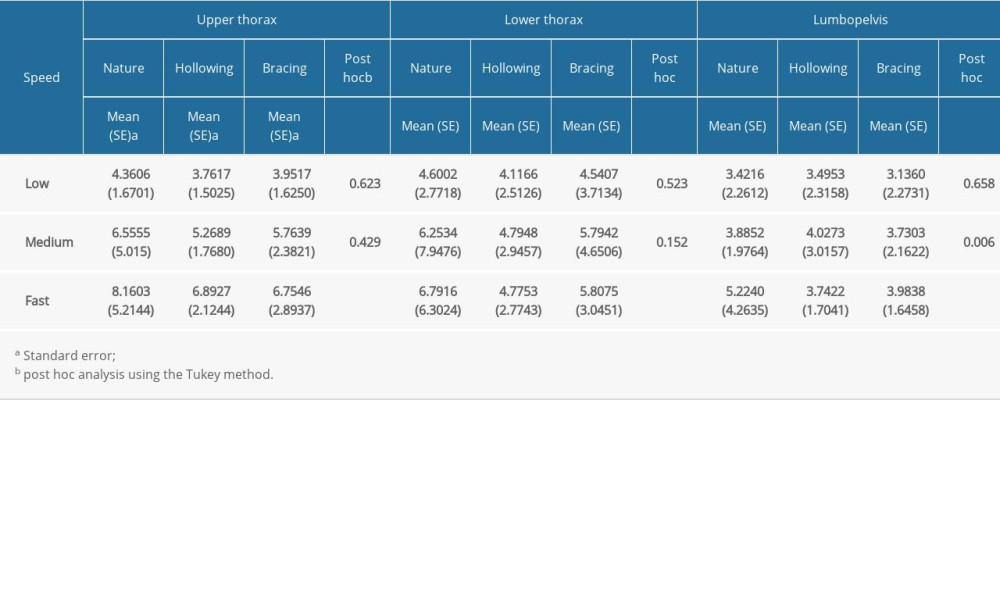 Table 2. Outcome of backward perturbation tests in upper thorax, lower thorax, and lumbopelvis.
Table 2. Outcome of backward perturbation tests in upper thorax, lower thorax, and lumbopelvis. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








