07 February 2022: Clinical Research
Comparison of Postoperative Pain in 70 Women with Breast Cancer Following General Anesthesia for Mastectomy with and without Serratus Anterior Plane Nerve Block
Binggao Chai12ACDEFG, Hongmei Yu3BCDF, Yafen Qian2B, Xiaoli Chen2B, Zhenqiang Zhu2BCD, Jianlong Du2BCD, Xianhui Kang1ADEF*, Shengmei Zhu1ADEFDOI: 10.12659/MSM.934064
Med Sci Monit 2022; 28:e934064
Abstract
BACKGROUND: [color=black]This study was conducted at a single center and aimed to compare postoperative pain in 70 women with breast cancer following general anesthesia for mastectomy with and without serratus anterior plane (SAP) block.[/color]
MATERIAL AND METHODS: [color=black]A total of 70 breast cancer patients who met the criteria were randomly divided into the general anesthesia combined with SAP block group (group S) and the general anesthesia only group (group G). Perioperative anesthetic drug dosage, the visual analog scale (VAS) score at different time points, and the patient’s satisfaction with analgesia 24 h after surgery, and incidence of postmastectomy pain syndrome (PMPS) were statistically analyzed in the 2 groups.[/color]
RESULTS: [color=black]Compared with group G, group S had lower intraoperative remifentanil dosages (P=0.003), a lower total amount of sufentanil via analgesia pump during the 24-h postoperative period (P<0.001), and lower VAS scores at 2 h, 4 h, and 8 h after surgery, and the differences were significant (P<0.05). Compared with group G, group S had a shorter first flatus time, got out of bed sooner, had a lower incidence of nausea and vomiting (P<0.05), and lower incidence of PMPS at 3 and 6 months after the operation (P<0.05).[/color]
CONCLUSIONS: [color=black]At a single center, preoperative SAP block can significantly reduce postoperative pain after modified radical mastectomy for breast cancer.[/color]
Keywords: Complex Regional Pain Syndromes, Analgesia, Mastectomy, Modified Radical, Adult, Anesthesia, General, Breast Neoplasms, China, Female, Humans, Mastectomy, Nerve Block, Pain, Postoperative
Background
Breast cancer is one of the most common malignant tumors in women [1,2], and surgery is the preferred treatment for early breast cancer [3]. Modified radical mastectomy for breast cancer can induce a surgical stress response, which is accompanied by moderate to severe postoperative pain [4,5]. In addition, approximately 25% to 60% of patients experience chronic pain due to poor postoperative acute pain control [6], and up to 50% of patients develop PMPS [7], which impairs rapid recovery. An important part of enhanced recovery after surgery is to reduce perioperative stress response and improve pain management [8]. Regional block technique is recognized as an effective technique to reduce perioperative stress and improve pain management [9].
At present, common clinical analgesia methods after breast cancer surgery include intravenous analgesia, epidural analgesia, regional block analgesia, and wound infiltration with local anesthetics [10]. Among these, intravenous analgesia has the shortcomings of high opioid dosages and a high incidence of nausea and vomiting. Epidural analgesia has the shortcomings of nerve injury and haemodynamic instability. The analgesic duration of wound infiltration with local anesthetics is short. Regional block analgesia includes thoracic paravertebral nerve block, intercostal nerve block, and SAP block. Among these, thoracic paravertebral nerve block has shortcomings such as a risk of pneumothorax, difficult administration, and a possibility of puncture failure. Intercostal nerve block often requires multiple injections and has a high risk of pneumothorax, and overlapping sensory innervation of the chest skin often results in incomplete analgesia [11,12].
SAP block is a new type of fascial plane block technique. Blocking the lateral cutaneous branch of the second to ninth intercostal nerves (T2–9) has a good analgesic effect on the anterior and the lateral chest walls [13]. Compared with other regional block techniques, SAP block is less difficult and has fewer serious complications. The reduction in the dosage of opioids, improvement in the analgesic effect [14], and reduction in the degree of stress response can benefit patients in many ways. SAP block has been initially used for postoperative analgesia after breast surgery, thoracotomy, and rib fracture fixation [15–18].
However, the impact of SAP block before radical mastectomy on the perioperative surgical stress response and rapid postoperative recovery has not been extensively studied, and its long-term efficacy relative to the incidence of PMPS has yet to be evaluated. Therefore, we conducted a single-center study to compare postoperative pain in 70 women with breast cancer following general anesthesia for mastectomy with and without SAP nerve block.
Material and Methods
STUDY DESIGN AND PARTICIPANTS:
Our study (approval number 2019-03) was approved by the Ethics Committee of Tongxiang First People’s Hospital, Zhejiang Province, China on 14 November 2019 and was registered on the Chinese Clinical Trial Registry website (registration number ChiCTR2000034508). The content of the study was thoroughly explained to the participants before written informed consent was obtained.
The inclusion criteria were: (1) diagnosed with unilateral breast cancer, (2) women aged 25 to 75 years, (3) American Society of Anesthesiologists (ASA) level I or II, and (4) body mass index (BMI) 18.5–28 kg/m2. The exclusion criteria were: (1) comorbid severe cardiovascular or cerebrovascular diseases; (2) skin damage or infection at the puncture site; (3) coagulation disorders; (4) history of allergies to local anesthetics; (5) history of long-term opioid or drug use; (6) abnormal liver or kidney function; (7) inability to cooperate with the study for various reasons; and (8) intraoperative surgical procedures were changed.
RANDOMIZATION AND BLINDING:
The participants were randomly divided into the general anesthesia combined with SAP block group (group S) and the general anesthesia only group (group G). Computer-based random grouping at a ratio of 1: 1 was conducted to generate random number lists, which were sealed in opaque envelopes. These sealed envelopes were marked with participant serial numbers and were maintained by the personnel responsible for screening. When a patient was recruited, the envelope corresponding to the patient’s serial number was sent to the anaesthesiologist. The anaesthesiologist opened the envelope and performed the intervention according to the anesthesia plan written on the card. The anesthesiologist who performed the blocks did not participate in intraoperative management of the patients.
ANESTHESIA AND MONITORING:
After entering the operating room, patients underwent routine electrocardiography (ECG), and noninvasive blood pressure, heart rate, oxygen saturation, and bispectral index (BIS) monitoring, and intravenous access was obtained. Our test method refers to the research of Swati Bhan et al [19]. In group S, the ultrasound-guided SAP block was performed prior to the induction of anesthesia. The patient was placed in a side-lying position, the opposite side was facing down, and the arm was raised. After disinfection and draping, the ultrasound probe was wrapped in a protective cover. The linear array probe (10–14 MHz) was placed inwardly and obliquely along the mid-axillary line. The 5th rib was located to distinguish the superficial latissimus dorsi, the deep serratus anterior muscle, and the ribs. After the application of 2 ml of 1% lidocaine for local anesthesia at the puncture site, a 20G needle for nerve block was inserted in a caudal-to-cephalic direction. When the needle tip reached the gap between the latissimus dorsi and the serratus anterior muscle, 2 ml of saline was slowly injected. The diffusion of saline into the gap between the latissimus dorsi and the serratus anterior was observed under ultrasound. If no blood or gas was observed when the plunger was withdrawn, 30 ml of 0.375% ropivacaine hydrochloride was then injected.
Anesthesia induction: Intravenous midazolam 0.05 mg/kg, sufentanil 0.4 μg/kg, propofol 2 mg/kg, and cisatracurium besilate 0.2 mg/kg were injected. After muscle relaxation, tracheal intubation and mechanical ventilation were performed. Respiration parameters were set as follows: tidal volume (TV) of 8–10 ml/kg, respiratory ratio of 1: 2, ventilation frequency of 12 times/min, and partial pressure of end-tidal CO2 (PetCO2) controlled between 35 and 45 mmHg (1 mmHg=0.133 kPa). Intraoperative maintenance was performed as follows: propofol 4–12 mg/kg/h, remifentanil 0.05–0.2 μg/kg/min, BIS maintained at between 45 and 60, and intermittent intravenous injection of cisatracurium besilate as needed. The maintenance dose of remifentanil and propofol was adjusted according to the BIS and hemo-fluctuations. If the patient developed hypertension (mean pressure >30% higher than the basal value), 5 mg urapidil was given, and if the patient developed hypotension (mean pressure >30% lower than the basal value), 6 mg ephedrine was administered intravenously. At the end of the surgery, remifentanil and propofol were discontinued. Intravenous infusion of 8 mg lornoxicam was administered for postoperative analgesia, intravenous injection of 0.25 mg palonosetron was administered to prevent postoperative nausea and vomiting, and the patient was sent to the postanesthesia care unit (PACU). All postoperative patients received patient-controlled intravenous analgesia (PCIA), and the disposable electronic analgesia pump formulation was as follows: 100 μg sufentanil diluted with saline to 100 ml, background dose 1 ml/h, single 1 ml dose, and a locking time 15 min. When VAS score was ≥4, PCA was pressed once for remedial analgesia.
ASSESSMENT AND EVALUATION:
SAP block was carried out in the anesthesia preparation room by an attending anesthesiologist who did not participate in the intraoperative management. Twenty minutes after the blocking, a bilateral thermal sensation comparison was performed using iodine swabs. Thermal sensation abnormalities in more than 3 thoracic vertebral segments indicated that the block was effective; otherwise, the patient was excluded from the experiments. Complications of SAP block were recorded. Postoperative follow-up was conducted by a member of the study group who was not involved in intraoperative management.
The perioperative dose of anesthetics and postoperative analgesia (the intraoperative dose of propofol and remifentanil, the dose of sufentanil during the 24-h postoperative period, the VAS score at different time points, and the patient’s satisfaction with analgesia 24 h after surgery), postoperative hemodynamic variables and stress indicators (average blood pressure and heart rate 5 min before and after skin incision, high-sensitivity C-reactive protein (hs-CRP), blood glucose level before and 3 h after operation), time of first postoperative flatus, time of first postoperative out-of-bed, and the length of postoperative hospital stay were recorded. Sleep quality was assessed by Pittsburgh Sleep Quality Index. Telephone follow-up was conducted 3, 6 and 9 months after surgery. Using the ID-Pain scale to screen for neuropathic pain, patients with a total score ≥2 points can be diagnosed as having PMPS.
STATISTICAL AANALYSIS:
G*Power 3.1.0 software was used for sample size calculation. The main observation indicator in this study was the dosage of sufentanil during the 24-h postoperative period. According to the results of our pre-experiment, the doses of sufentanil in the general anesthesia combined with SAP block group (group S) and the general anesthesia only group (group G) were 26.6±3.3 μg and 30.1±4.8 μg, respectively. The test level was set to 0.05, and the test power was 0.9. At least 27 patients in each group were required. Considering the loss to follow-up, 70 patients were selected.
SPSS22.0 software was used to process the data. Measurement data with a normal distribution are expressed as the mean±standard deviation. Intragroup comparisons were performed by analysis of variance (ANOVA) with repeated measurements, and intergroup comparisons were analyzed with
Results
Applying the inclusion and exclusion criteria, this study recruited 70 patients who underwent modified radical mastectomy between July 2020 and January 2021. These 70 patients were divided into 2 groups. Among them, in group S, 1 patient was judged to be ineligible for the block, 2 patients were lost to follow-up after discharge; in group G, 2 patients were lost to follow-up after discharge; all of these patients were excluded from the trial. In total, 65 patients completed this study, including 32 patients in group S and 33 patients in group G. The data of the 65 patients are as follows.
There were no block-related complications such as hematoma, pneumothorax, or infection in group S. Three patients in group S and 2 patients in group G received vasoactive drugs, and the difference was not significant (
There was no significant difference in the general information or intraoperative conditions between the 2 groups (
Compared with group G, group S had lower intraoperative dosages of propofol and remifentanil; a lower total amount of sufentanil via analgesia pump during the 24-h postoperative period; lower VAS scores 2 h, 4 h, and 8 h after the operation; and higher patient satisfaction with analgesia; the differences were significant (
Compared with group G, group S had significantly lower mean arterial pressure (MAP) and heart rate at 5 min after the skin incision and hs-CRP and blood glucose levels at 3 h after surgery (
Compared with group G, group S had a significantly earlier time to first passage of flatus, got out of bed sooner postoperatively, and had a significantly lower incidence of nausea and vomiting (
The incidence of postmastectomy pain syndrome in group S at 3 and 6 months after surgery was 15.63% (5/32) and 12.50% (4/33), respectively, which was significantly lower than the incidence of postmastectomy pain syndrome in group G, which was 39.39% (13/33) and 33.33% (11/33) (
Discussion
The results of this study show that preoperative SAP block can substantially minimize perioperative opioid consumption in modified radical mastectomy for breast cancer, reduce the perioperative surgical stress response, enhance patient satisfaction with postoperative pain management, and minimize the incidence of PMPS, all of which are conducive to surgery. Similar findings were observed by Swati Bhan et al [19], who evaluated 100 patients after surgery and found that administration of SAP block delays the need for first analgesic rescue. It improves postoperative pain scores and decreases intraoperative analgesic requirements without any added adverse events. Serratus anterior plan block as a regional block has been preliminarily applied for perioperative analgesia in breast, thoracic, and minimally invasive heart surgeries.
Due to the shallow position of the serratus anterior, the needle was inserted into the plane under ultrasound guidance to observe the position of the needle tip in real time. No nerve injury, pneumothorax, or other complications occurred in the general anesthesia combined with SAP block group. The SAP block was judged to be invalid in only 1 patient, indicating that ultrasound-guided SAP block is simple, safe, and effective and can largely meet clinical needs [20].
The ropivacaine hydrochloride used in this study is a long-acting amide-based local anesthetic with low cardiac and central nervous system toxicity that features separate motor and sensory blockade and provides satisfactory analgesia in the surgical region without affecting early movements of the arm on the treated side. The SAP block is a fascia block, and the volume and concentration of the local anesthetic determine the extent of analgesia and the duration of the SAP block. A relatively large volume of local anesthetics has been reported to be able to block more intercostal nerves and thus provide a better blocking effect [21]. A high volume and low concentration of anesthetic (0.375% ropivacaine hydrochloride, 30 ml) was used for the blockade to limit local anesthetic toxicity danger. The comparison of postoperative VAS scores and the dosage of analgesics showed that a single SAP block could provide effective postoperative analgesia for approximately 8 h. Postoperative pain is an important factor that hinders the rapid recovery of surgical patients and affects quality of life. The present results confirmed that the intraoperative remifentanil and 24 h postoperative sufentanil dosages and 2-h, 4-h, and 8-h VAS scores were extensively decreased in the general anesthesia combined with anterior serratus plane block group compared with the simple general anesthesia group, suggesting that SAP block can grant excellent postoperative analgesic outcomes for modified radical mastectomy. The reduction in the intraoperative propofol dosage in the SAP block group was related to the improvement in analgesia and consequent reduction in the need for sedation, and to the general effect of local anesthesia. On the other hand, the concentration of local anesthetics further affects the anesthetic concentration in systemic circulation, which in turn affects sodium channels in the central nervous system, resulting in sedation [12].
The components of rapid postoperative recovery include early recovery of gastrointestinal function, getting out of bed soon, improvement in sleep quality, and control of nausea and vomiting. Patients with breast cancer are at high risk of nausea and vomiting after surgery. SAP block can reduce the use of perioperative opioids, thereby reducing the incidence of nausea and vomiting and improving patient comfort. SAP block reduces the dosage of perioperative opioids and provides better perioperative analgesia, which explains the earlier first flatus time, the earlier time awakening, and the improvement in sleep quality.
The perioperative stress response is a nonspecific defense response when the body is subjected to strong stimuli such as surgery and anesthesia. The stress response disrupts the balance between oxygen free radicals and antioxidant systems, leading to oxidative stress injury, which is the pathological basis for a range of postoperative complications. hs-CRP is an acute-phase protein synthesized by the body when it is subjected to inflammatory stimuli such as tissue damage or microbial invasion [22]. The stress response can lead to insulin resistance and induce liver glycogenolysis and gluconeogenesis, leading to increased blood glucose. Therefore, hs-CRP, blood glucose and hemodynamic indicators before and after skin incision were used as indicators to reflect the body’s acute stress level. In this study, compared with the general anesthesia only group, the postoperative hs-CRP and blood glucose were lower, and the hemodynamic changes after skin incision were small in the general anesthesia combined with the SAP block group. Our results suggest that SAP block can reduce the stress response during radical mastectomy and effectively inhibit the release of inflammatory factors.
PMPS is a common chronic neuropathic pain syndrome that lasts for more than 3 months. Its pathogenesis is not yet completely clear. There are data showing that it is related to intraoperative nerve injury, changes in nerve plasticity, and continuous stimulation of peripheral receptors by inflammatory mediators that cause pain hypersensitivity [23] and is an important problem in clinical treatment. Preventive analgesia can inhibit the transmission of noxious stimuli to the central nervous system and reduce the possibility of central or peripheral sensitization to a certain extent. If acute postoperative pain is not well controlled, this pain can easily lead to peripheral sensitization, which, in turn, will lead to abnormal spinal cord regulation, resulting in central sensitization, hyperalgesia, and further chronic pain [24]. The results of this study showed that the incidence of PMPS in the anterior serratus muscle block group decreased after surgery. This reduction may be related to anterior serratus plane block before the operation, which is related to preventive analgesia and better perioperative analgesia. Postoperative pain syndrome of breast cancer is related to chemotherapy and radiotherapy. In this study, the difference between these 2 variables in the 2 groups was not statistically significant. Therefore, radiotherapy and chemotherapy did not interfere with the results of this study. This was a single-center study with a small sample size. The effect of SAP block on PMPS in breast cancer patients still needs to be demonstrated by multicenter research with large samples.
Our study has several limitations. First, this was a single-blind study. Considering that it would increase unnecessary harm to patients, we did not use placebo injections. Patients knew whether they had received serratus anterior block. We cannot minimize the placebo effect, which can increase bias error. Second, in this study, we only used sufentanil as the intravenous analgesic, which may be another limitation. In multimodal analgesia, intravenous analgesics with different mechanisms of action can better control pain. Finally, the use of a single center, small sample size, and subjective methods to assess pain may also have introduced bias.
Conclusions
In summary, at a single center, postoperative pain was significantly reduced in women with breast cancer following general anesthesia for mastectomy when combined with SAP nerve block, and perioperative opioid dosage was decreased. SAP block is simple and safe and is an effective choice for the control of acute and chronic pain after radical breast cancer surgery.
Tables
Table 1. Patient characteristics.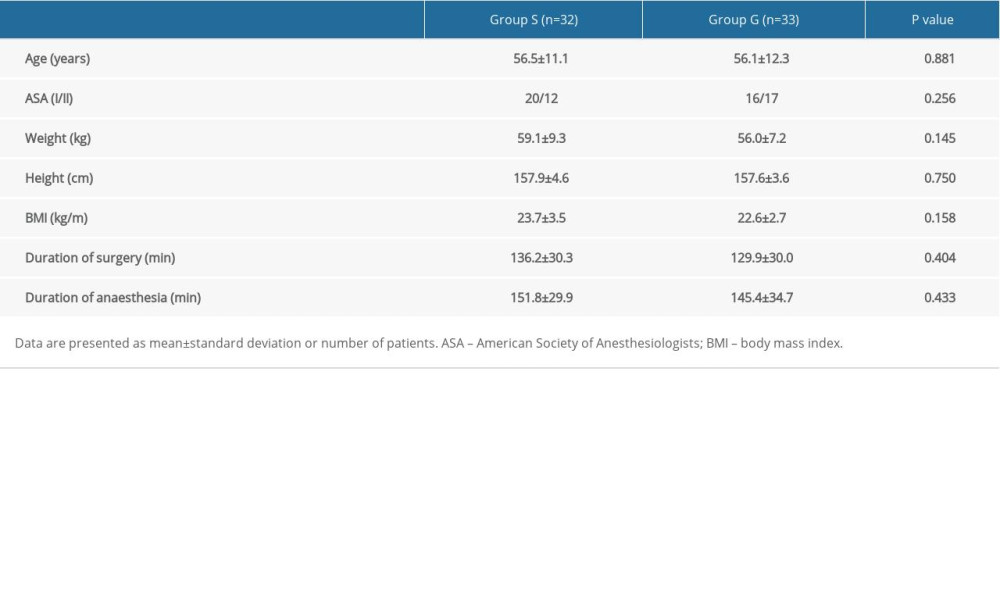 Table 2. Perioperative opioid consumption, postoperative VAS score and patient satisfaction with analgesia.
Table 2. Perioperative opioid consumption, postoperative VAS score and patient satisfaction with analgesia.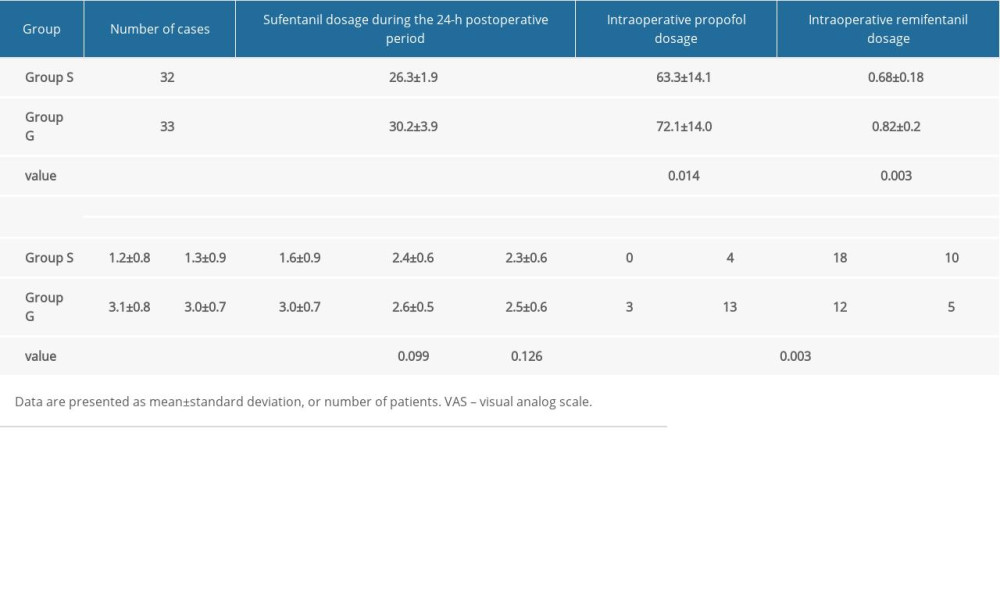 Table 3. Postoperative hemodynamic variables, hs-CRP and blood glucose.
Table 3. Postoperative hemodynamic variables, hs-CRP and blood glucose.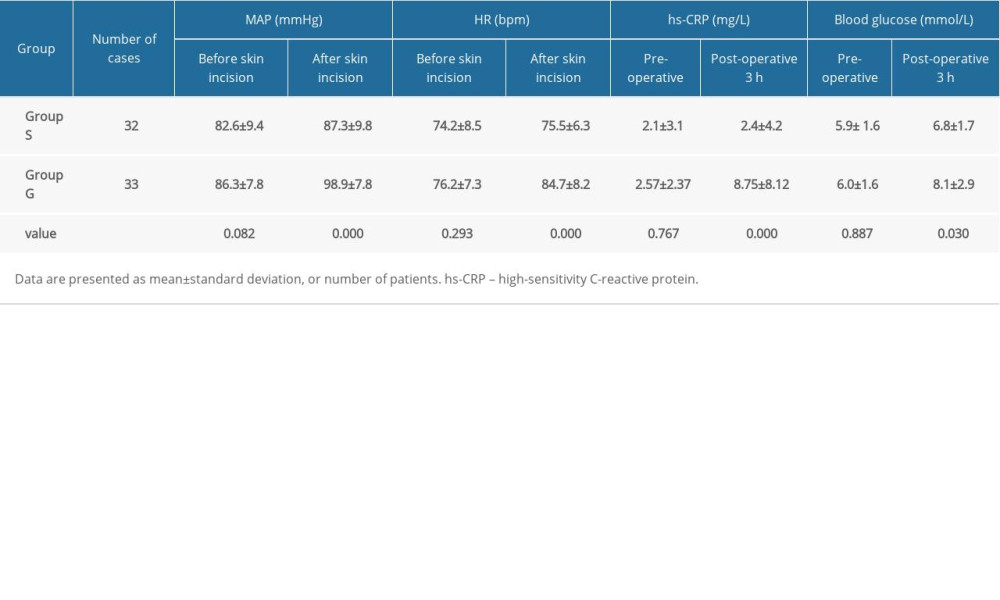 Table 4. Postoperative data.
Table 4. Postoperative data.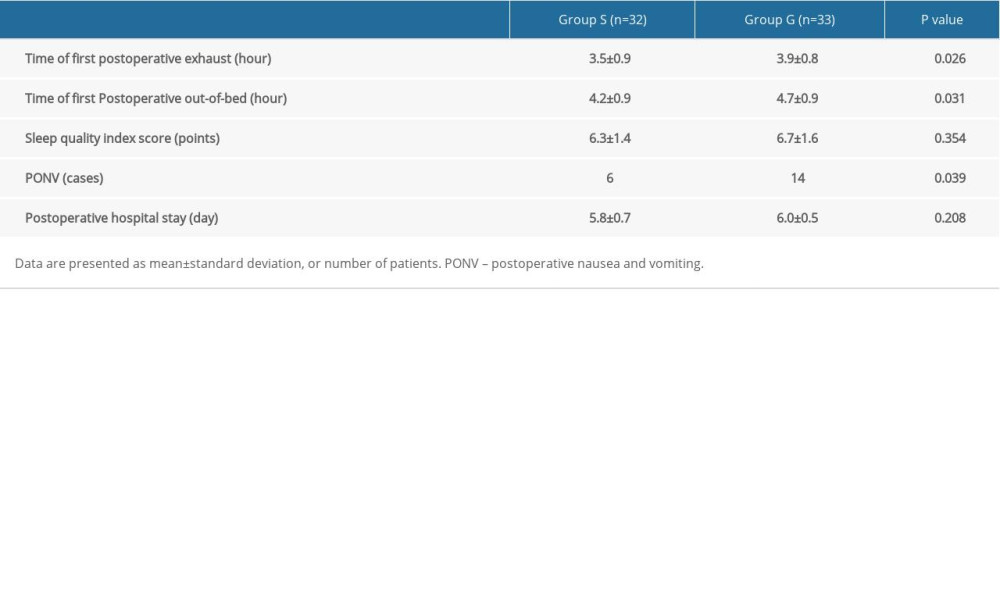 Table 5. Comparisons of incidence of postoperative chemoradiotherapy and PMPS between the 2 groups.
Table 5. Comparisons of incidence of postoperative chemoradiotherapy and PMPS between the 2 groups.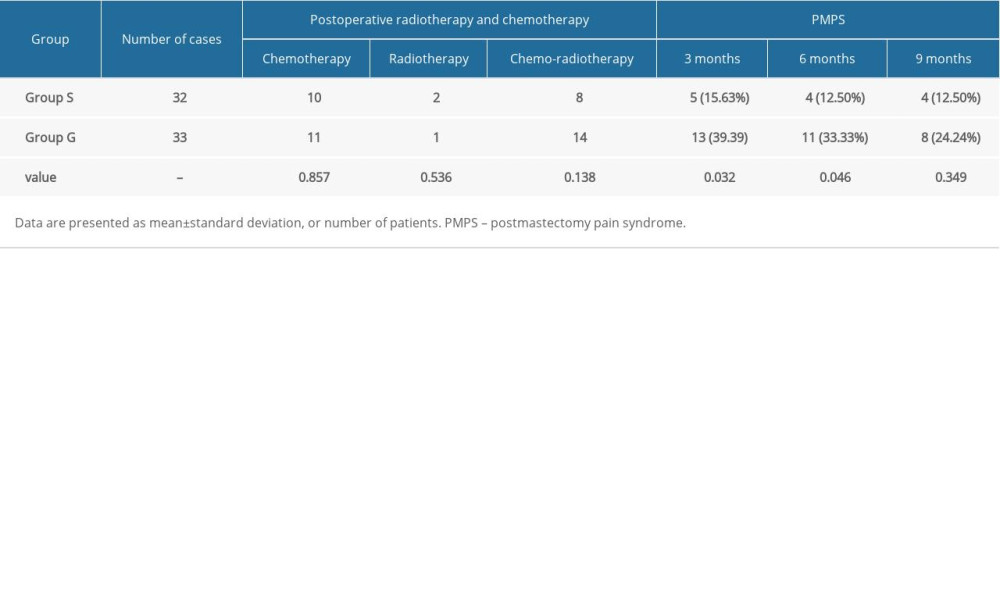
References
1. Allemani C, Matsuda T, Di Carlo V, Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of inspanidual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries: Lancet, 2018; 391(10125); 1023-75
2. Akram M, Iqbal M, Daniyal M, Khan AU, Awareness and current knowledge of breast cancer: Biol Res, 2017; 50(1); 33
3. Yao Y, Li J, Hu H, Xu T, Chen Y, Ultrasound-guided serratus plane block enhances pain relief and quality of recovery after breast cancer surgery: Eur J Anaesthesiol, 2019; 36(6); 436-41
4. Wang L, Guyatt GH, Kennedy SA, Predictors of persistent pain after breast cancer surgery: A systematic review and meta-analysis of observational studies: CMAJ, 2016; 188(14); E352-61
5. Fujii T, Shibata Y, Akane A, A randomised controlled trial of pectoral nerve-2(PECS 2) block vs. serratus plane block for chronic pain after mastectomy: Anaesthesia, 2019; 74(12); 1558-62
6. Chiu C, Aleshi P, Esserman LJ, Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy: BMC Anesthesiology, 2018; 18(1); 41
7. Macdonald L, Bruce J, Scott NW, Long-term follow-up of breast cancer survivors with post-mastectomy pain syndrome: Br J Cancer, 2005; 92(2); 225-30
8. Gonfiotti A, Viggiano D, Voltolini L, Enhanced recovery after surgery and video-assisted thoracic surgery lobectomy: The Italian VATS Group surgical protocol: J Thorac Dis, 2018; 10(S4); S564-70
9. Schnabel A, Reichl SU, Kranke P, Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials: Br J Anaesth, 2013; 111(3); 522
10. Arora S, Ovung R, Bharti N, Efficacy of serratus anterior plane block versus thoracic paravertebral block for postoperative analgesia after breast cancer surgery – a randomized trial: Braz J Anesthesiol, 2021 [Online ahead of print]
11. Kunigo T, Murouchi T, Yamamoto S, Yamakage M, Injection volume and anesthetic effect in serratus plane block: Reg Anesth Pain Med, 2017; 42(6); 737-40
12. Pace MM, Sharma B, Anderson-Dam J, Ultrasound-guided thoracic paravertebral blockade: Anesth Analg, 2016; 122(4); 1186-91
13. Kim D-H, Oh YJ, Lee JG, Efficacy of ultrasound-guided serratus plane block on postoperative quality of recovery and analgesia after video-assisted thoracic surgery: Anesth Analg, 2018; 126(4); 1353-61
14. Goswami S, Kundra P, Bhattacharyya J, Pectoral nerve block1 versus modified pectoral nerve block2 for postoperative pain relief in patients undergoing modified radical mastectomy: A randomized clinical trial: Br J Anaesth, 2017; 119(4); 830-35
15. Kamiya Y, Hasegawa M, Yoshida T, Impact of pectoral nerve block on postoperative pain and quality of recovery in patients undergoing breast cancer surgery: Eur J Anaesthesiol, 2018; 35(3); 215-23
16. Gao W, Yang X, Hu J, Continuous serratus anterior plane block improved early pulmonary function after lung cancer surgical procedure: Ann Thorac Surg, 2021 [Online ahead of print]
17. Khalil AE, Abdallah NM, Bashandy GM, Kaddah TA-H, Ultrasound-guided serratus anterior plane block versus thoracic epidural analgesia for thoracotomy pain: J Cardiothorac Vasc Anesth, 2017; 31(1); 152-58
18. Park MH, Kim JA, Ahn HJ, A randomised trial of serratus anterior plane block for analgesia after thoracoscopic surgery: Anaesthesia, 2018; 73(10); 1260-64
19. Bhan S, Mishra S, Gupta N, A Prospective randomised study to assess the analgesic efficacy of serratus anterior plane (SAP) block for modified radical mastectomy under general anaesthesia: Turk J Anaesthesiol Reanim, 2020; 49(2); 124-29
20. Gürkan Y, Aksu C, Kuş A, Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: A randomized controlled study: J Clin Anesth, 2018; 50; 65-68
21. Elsabeeny WY, Shehab NN, Wadod MA, Elkady MA, Perioperative analgesic modalities for breast cancer surgeries: A prospective randomized controlled trial: J Pain Res, 2020; 13; 2885-94
22. Kunigo T, Murouchi T, Yamamoto S, Yamakage M, Injection volume and anesthetic effect in serratus plane block: Reg Anesth Pain Med, 2017; 42(6); 737-40
23. Piracha MM, Thorp SL, Puttanniah V, Gulati A, A tale of two planes: Reg Anesth Pain Med, 2017; 42(2); 259-62
24. Pérez Herrero MA, López Álvarez S, Fadrique Fuentes A, Quality of postoperative recovery after breast surgery. General anaesthesia combined with paravertebral versus serratus-intercostal block: Rev Esp Anestesiol Reanim, 2016; 63(10); 564-71
Tables
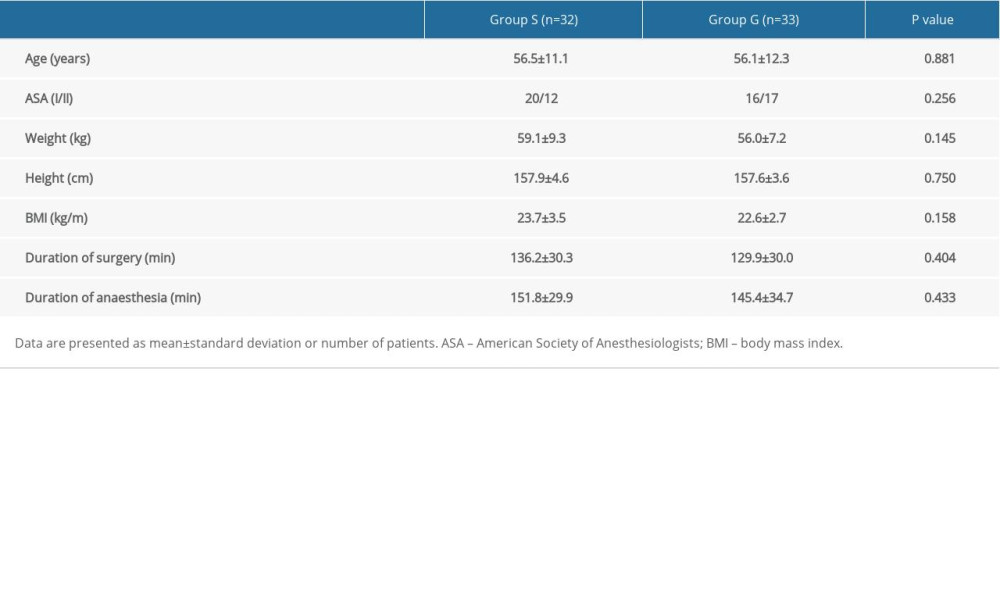 Table 1. Patient characteristics.
Table 1. Patient characteristics.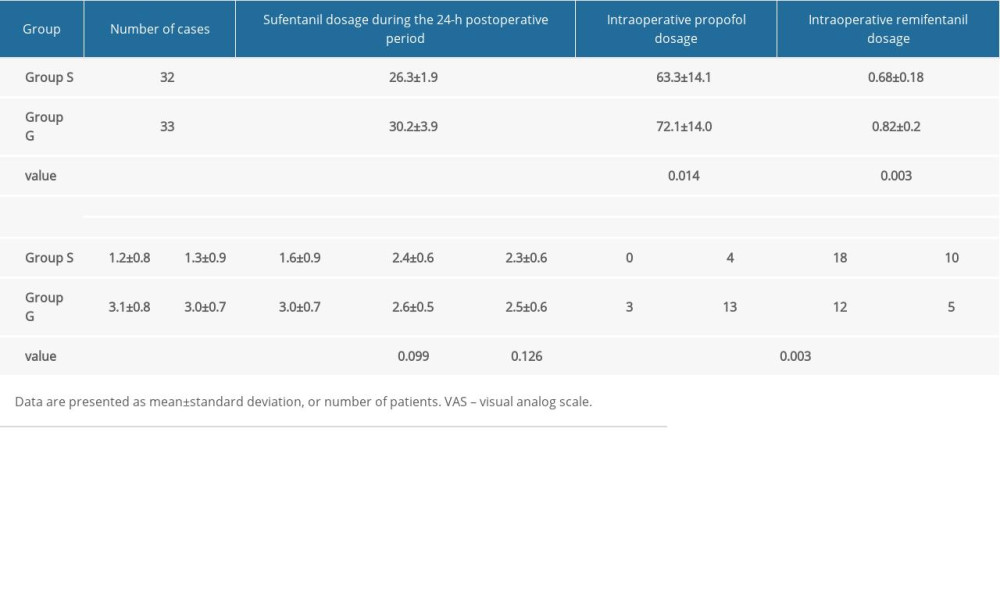 Table 2. Perioperative opioid consumption, postoperative VAS score and patient satisfaction with analgesia.
Table 2. Perioperative opioid consumption, postoperative VAS score and patient satisfaction with analgesia.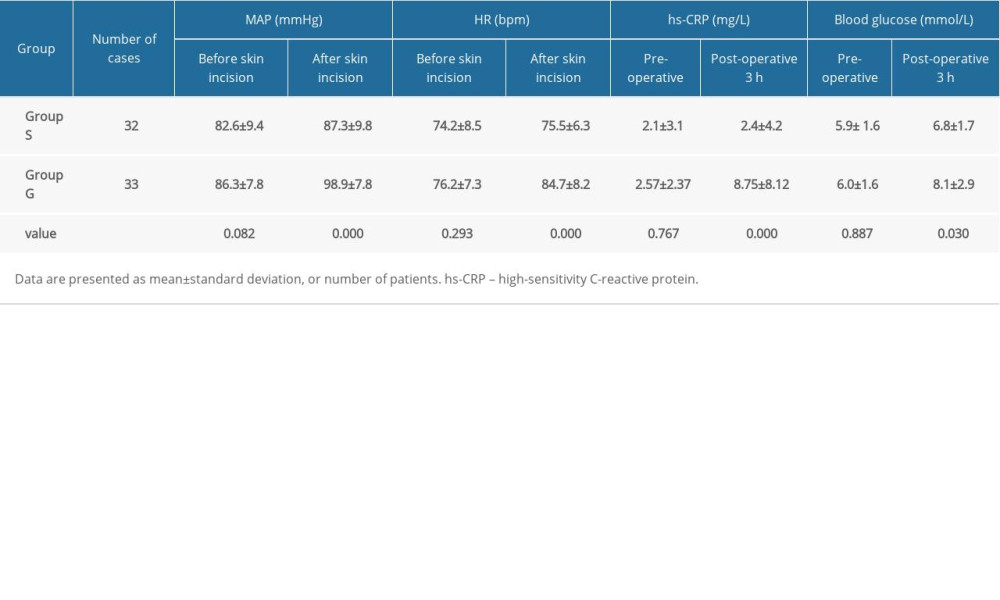 Table 3. Postoperative hemodynamic variables, hs-CRP and blood glucose.
Table 3. Postoperative hemodynamic variables, hs-CRP and blood glucose.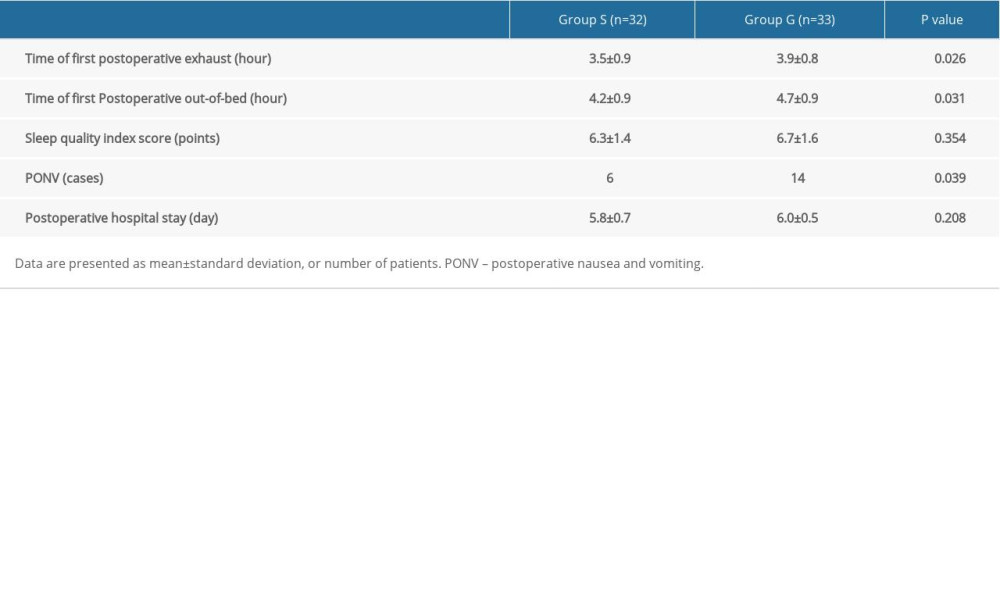 Table 4. Postoperative data.
Table 4. Postoperative data.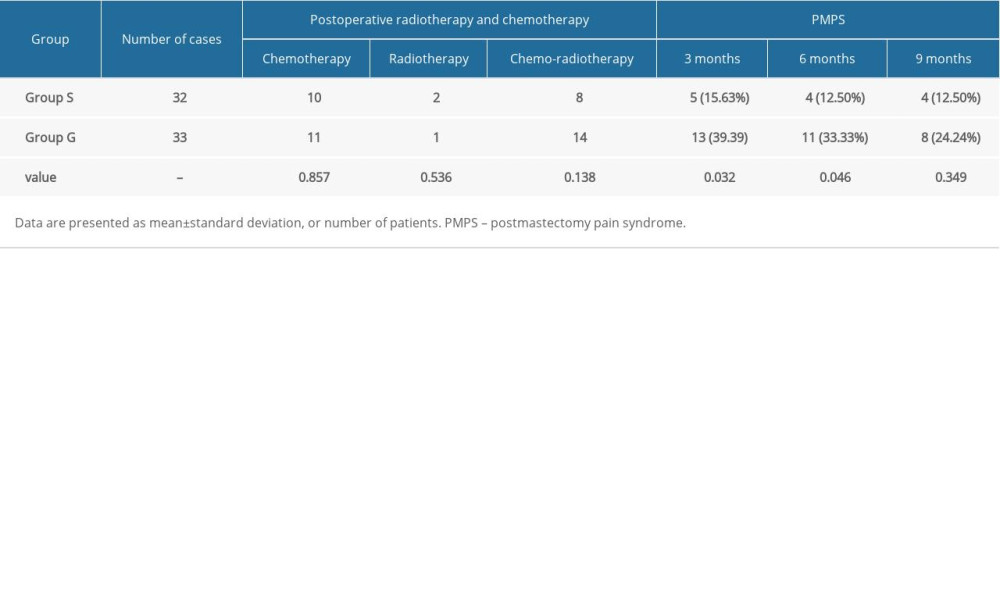 Table 5. Comparisons of incidence of postoperative chemoradiotherapy and PMPS between the 2 groups.
Table 5. Comparisons of incidence of postoperative chemoradiotherapy and PMPS between the 2 groups. In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








