30 March 2022: Clinical Research
COVID-19 Pandemic Was Associated with Lower Activity but Not Higher Perioperative Mortality in a Large Eastern European Center
Stefan Andrei12ABCDEF, Sebastian Isac23ABDE, Diana Jelea2ABCDEF, Cristina Martac2ABCDEF, Mihai-Gabriel Stefan4DEF*, Mihail Cotorogea-Simion2BCD, Cristina Georgiana S. Buzatu2BDEFG, Daiana Ingustu2BDE, Imam Abdulkareem2BD, Catalin Vasilescu56DEF, Daniela Filipescu14DEF, Gabriela Droc12ABCDEFDOI: 10.12659/MSM.935809
Med Sci Monit 2022; 28:e935809
Abstract
BACKGROUND: Surges of critically ill patients can overwhelm hospitals during pandemic waves and disrupt essential surgical activity. This study aimed to determine whether hospital mortality increased during the COVID-19 pandemic and during pandemic waves.
MATERIAL AND METHODS: This was a retrospective analysis of a prospective, observational, epidemiological database. All patients who underwent surgery from January 1 to December 31, 2020, were included in the analysis. The setting was a large Eastern European Surgical Center referral center of liver transplant and liver surgery, a major center of abdominal surgery.
RESULTS: A total of 1078 patients were analyzed, and this number corresponded to a reduction of surgical activity by 30% during the year 2020 compared with 2019. Despite an increase in surgery complexity during the pandemic, perioperative mortality was not different, and this was maintained during the pandemic wave. The pandemic (OR 1.45 [0.65-3.22], P=0.365) and the wave period (OR 0.897 [0.4-2], P=0.79) were not associated with hospital mortality in univariate analysis. In the multivariate model analysis, only the American Society of Anesthesiology (ASA) score (OR 5.815 [2.9-11.67], P<0.0001), emergency surgery (OR 5.066 [2.24-11.48], P<0.0001), and need for surgical reintervention (OR 5.195 [1.78-15.16], P=0.003) were associated with hospital mortality.
CONCLUSIONS: Despite considerable challenges, in this large retrospective cohort, perioperative mortality was similar to that of pre-pandemic practice. Efforts should be made to optimize personnel issues, while maintaining COVID-19-free surgical pathways, to adequately address patients’ surgical needs during the following waves of the pandemic.
Keywords: Hospital Mortality, Pandemics, Perioperative Care, SARS-CoV-2, COVID-19, Humans, Prospective Studies
Background
Usual surgical activity was disrupted in the context of the new coronavirus (COVID-19) pandemic [1], particularly during the sudden surges in hospitalized patients associated with pandemic waves. These surges were expected to have a significant impact on adult elective surgeries in many countries, thus increasing perioperative mortality and the complication rate [2]. Each national health authority organized and made decisions according to local specificities, considering the COVID-19 pandemic evolution, healthcare characteristics, and other challenges [3–5]. Different recommendations concerning the postponing and cancelling of elective surgeries were proposed.
At a national level in Romania, owing to anticipated limitations in surge-response capacity, decisions were initially made to limit the number of non-urgent surgical interventions to free Intensive Care Unit (ICU) beds for patients with COVID-19 in need of ventilatory support or other specific therapies [6]. Later, hospitals were required to keep a dedicated ward and ICU beds for patients with COVID-19 as a back-up, while entire hospitals (mainly, but not limited to, those specializing in infectious diseases and pulmonology) were converted to COVID-19 facilities.
The impact of the pandemic on patient chronic pathologies and delayed surgeries has still not been very well evaluated, especially in the context of heterogenous measures and diversity of local conditions.
From the anesthesiologists’ perspective, the Romanian healthcare system has a history of chronic personnel deficits [7]; it was confronted with several challenges during the first year of the COVID-19 pandemic. The anesthesiologists are also intensive care medicine physicians and are responsible for ICU management and care, like those in various countries worldwide. Thus, the surges of critically ill patients in the successive waves of the pandemic posed challenges for staffing the operating rooms, particularly for non-urgent surgery, which were not fully addressed by emerging guidelines based on accumulating experience in other countries [8]. Medical staff volunteered or were temporarily transferred to other highly understaffed provincial hospitals due to new legislation allowing for relocation of physicians and nurses in areas under severe pressure caused by case overload [9]. Local personnel SARS-CoV-2 outbreaks required home-isolation or even hospitalization of staff members, creating further management difficulties [10]. Also, infrastructure particularities in the local ICUs caused another struggle, namely making patient isolation due to non-SARS-CoV-2 infections very difficult in a local environment with a high prevalence of antimicrobial resistance [11]. Dedicated personnel were hard to summon, which could have sometimes led to suboptimal bed use. This had an impact on surgical activity and, despite workload increase, owing to medical and administrative reasons, the chronic lack of medical staff was accentuated.
The main objective of this study was to evaluate the impact of the pandemic on perioperative mortality. The secondary objectives were (i) to evaluate the impact of wave periods on perioperative mortality; and (ii) to describe the patient profiles during the first pandemic year.
We hypothesized that diminished availability of medical personnel, restrictive surgical planning, and a lower number of available surgical ICU beds would be reflected in a higher incidence of perioperative mortality and surgical complications during the pandemic.
Material and Methods
DESIGN:
The study was a retrospective analysis of a prospective, observational, epidemiological database and was conducted in a single tertiary, university-affiliated national center, the main national center of liver transplant and liver surgery and a major center for abdominal surgery.
COVID-19 PANDEMIC IN ROMANIA:
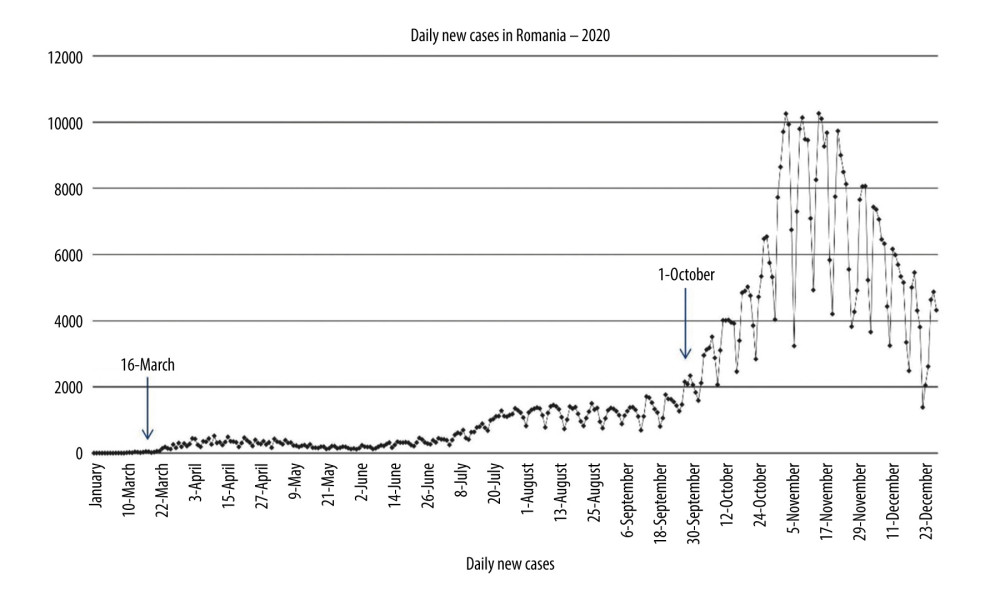
The timeline of the COVID-19 pandemic in Romania is illustrated in Figure 1. The pandemic was declared by the governmental authorities on March 16, 2020, when a state of emergency was issued with consequent restrictions, which had an impact on hospital activity [12]. This date was used to divide patients in our study into 2 groups by period: pandemic and non-pandemic. Furthermore, a surge in new cases with concomitant impact on ICU bed availability was registered from October 2020 until the end of 2020 (Figure 1). The patients undergoing surgery between October 1 and December 31, 2020, were treated in the context of the SARS-CoV-2 wave in data analysis. A comprehensive history of the epidemiology and legal framework of the pandemic in Romania is provided in Supplementary Table 1.
PATIENTS AND DATA COLLECTION:
All patients who underwent surgery from January 1, 2020, to December 31, 2020, in our department were included. The preoperative demographical characteristics (age, sex, American Society of Anesthesiology [ASA] score) and the intraoperative data (type and length of surgery, emergency status, cancer surgery, intraoperative packed red blood cell [PRBC] transfusion) for each patient were entered in an electronic database by the anesthetist at the end of surgery. Hospital mortality was recorded using electronic records.
STATISTICAL ANALYSIS:
Data were collected in a Microsoft Excel database and analyzed using SPSS (IBM SPSS Statistics for Windows, version 21.0; IBM Corp, Armonk, NY, USA). A 2-sided
We firstly determined the variables associated with 1-year mortality through univariate logistic regression analysis. Secondly, the statistically significant variables in univariate analysis were introduced in a multivariate logistic regression model to identify independent predictors of 1-year mortality. The rule of thumb of 5 to 10 events per variable in the multivariate logistic model was applied.
MANAGEMENT OF MISSING DATA:
There were no missing data in our final database. Therefore, no missing data strategy was required before the statistical analysis.
CLINICAL PATHWAY OF PATIENTS:
As previously proposed by experts [13], all patients were screened for SARS-CoV-2 prior to elective surgery and if they were positive, their surgeries were either postponed, if possible, or transferred to another center dedicated to managing COVID-19 in surgical patients. There was, however, a small number of patients (5 of 1078) that underwent surgery as emergencies having COVID-19; therefore, no general considerations can be made regarding increased mortality in COVID-19 patients as mentioned by other authors [14].
Results
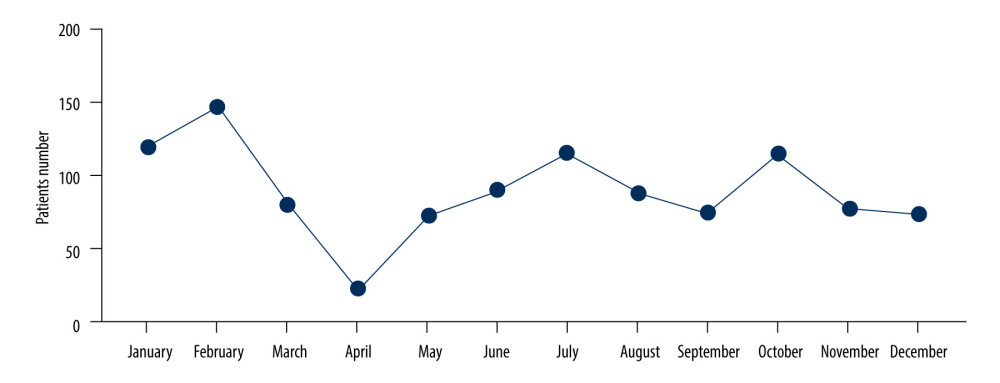
There were 1078 surgical patients in our department in 2020. The monthly distribution of surgeries is shown in Figure 2. When compared to the previous year (2019), the number of surgical patients corresponded to a reduction of 30% in surgical activity. The cohort demographic and surgical characteristics are shown in Table 1. The mean patient age was 59±14 years and 542 (50.28%) patients were female; 655 (60.76%) patients underwent a major surgical procedure; 663 (61.45%) interventions were performed in an oncological context; 216 (20.04%) were emergency surgeries; and 693 (64.3%) had an ASA score ≥III. The overall perioperative mortality was 3.25% (35 patients). The monthly variation of recorded mortality is shown in Supplementary Figure 1.
Patients’ characteristics are shown by the extra-pandemic, pandemic, and wave periods in Table 1. A total of 757 (70.2%) patients had surgery during the pandemic, and 267 (24.76%) patients underwent surgery during the COVID-19 wave. The comparative hospital mortality during the pandemic vs the extra-pandemic period was 3.57% vs 2.49% (
The univariate and multivariate logistic regression analyses results are shown in Table 2. In univariate analysis, major surgery, emergency intervention, reintervention, and ASA score were associated with hospital mortality. The pandemic (OR 1.45 [0.65–3.22],
Discussion
STUDY LIMITATIONS:
The first limitation of this study is its single-center and observational design. However, we already pointed out above that our center has a specific role in the local national healthcare system, with very specialized surgical activity.
Another limitation is the small number of variables considered in the data analysis. Other confounding factors could have had an impact on surgical mortality. Unfortunately, the database was not initially created with the purpose of exhaustively analyzing perioperative mortality. However, this limitation might generate an indiscriminative bias, affecting both pandemic and non-pandemic patients in data analysis, thus keeping the findings relevant in the current context. Also, the database was robust, without any missing data.
Ideally, the patients needed to be compared with those of the previous years, considering the same months of the year. This is another limitation of this study. However, we assumed that surgical activity is not mainly season- or month-dependent.
Conclusions
Despite considerable challenges regarding logistics and personnel, perioperative mortality was similar to pre-pandemic practices in our cohort, that of a tertiary care, academic hospital, the main center of liver transplant and a major center for abdominal surgery in an Eastern European country. This seems reassuring at a local level and should be regarded as a potential model for clinical practice. Special consideration should be given to pandemic waves, when surges of patients can lead to selection of less ill patients, with difficult to estimate consequences on mortality on a national level.
Efforts should be made to optimize personnel issues, while maintaining COVID-19-free surgical pathways to adequately address surgical needs during following waves of the pandemic.
References
1. Søreide K, Hallet J, Matthews JB, Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services: Br J Surg, 2020; 107(10); 1250-61
2. COVIDSurg Collaborative, Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans: Elective surgery during the SARS-CoV-2 pandemic: Br J Surg, 2020; 107; 1440-49
3. Chen YH, Fang CT, Mortality from COVID-19: A cross-country comparison of containment versus mitigation strategy: J Formos Med Assoc, 2020; 119(11); 1710-12
4. Ludvigsson JF, The first eight months of Sweden’s COVID-19 strategy and the key actions and actors that were involved: Acta Paediatr, 2020; 109(12); 2459-71
5. The Lancet, India under COVID-19 lockdown [editorial]: Lancet, 2020; 395(10233); 1315
6. : Ordinul nr. 555/2020 privind aprobarea Planului de măsuri pentru pregătirea spitalelor în contextul epidemiei de coronavirus COVID19, a Listei spitalelor care asigură asistenţa medicală pacienţilor testaţi pozitiv cu virusul SARS-CoV-2 în faza I şi în faza a II-a şi a Listei cu spitalele de suport pentru pacienţii testaţi pozitiv sau suspecţi cu virusul SARS-CoV-2. [serial online] Available from: [in Romanian]https://www.cnscbt.ro/index.php/lex/1753-ordinul-nr-555-2020-privind-aprobarea-planului-de-masuri-pentru-pregatirea-spitalelor-in-contextul-epidemiei-de-coronavirus-covid-19-a-listei-spitalelor-care-asigura-asistenta-medicala-pacientilor-tes/file
7. Mitre C, Breazu C, Mitre I, Filipescu D, Migration of skilled anaesthesiologists from low to high-income economies: Urgent action needed: Eur J Anaesthesiol, 2016; 33(3); 157-59
8. Aziz S, Arabi YM, Alhazzani W, Managing ICU surge during the COVID-19 crisis: Rapid guidelines: Intensive Care Med, 2020; 46(7); 1303-25
9. , LEGE nr. 55 din 15 mai 2020 privind unele măsuri pentru prevenirea şi combaterea efectelor pandemiei de COVID-19 Publicat în MONITORUL OFICIAL nr. 396 din 15 mai 2020 [serial online]. Available from: [in Romanian]https://www.mai.gov.ro/wp-content/uploads/2020/05/LEGE-nr.-55-din-15-mai-2020.pdf
10. Droc G, Brezeanu L, Martac C, The strategy management of a SARS-CoV-2 outbreak in an Eastern European hospital: J Crit Care Med, 2021; 7(1); 73-74
11. European Centre for Disease Prevention and Control: ECDC country visit to Romania to discuss antimicrobial issues: 26 10 March 2017. [serial online], 2018, LU: Publications Office [cited 2021 Aug 27]. Available from: https://data.europa.eu/doi/10.2900/052263
12.
13. Kibbe MR, Surgery and COVID-19: JAMA, 2020; 324(12); 1151-52
14. Doglietto F, Vezzoli M, Gheza F, Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy: JAMA Surg, 2020; 155(8); 691-702
15. Andrei S, Isac S, Cârstea M, Isolated liver trauma. A clinical perspective in a non-emergency center for liver surgery: Exp Ther Med, 2022; 23(1); 39
16. Filipescu D, Banateanu R, Beuran M, Perioperative Patient Blood Management Programme. Multidisciplinary recommendations from the Patient Blood Management Initiative Group: Romanian J Anaesth Intensive Care, 2017; 24(2); 139-57
17. COVIDSurg Collaborative, Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic: Colorectal Dis, 2021; 23(3); 732-49
18. Glasbey JC, Nepogodiev D, Simoes JFF, Elective cancer surgery in COVID-19 – free surgical pathways during the SARS-CoV-2 pandemic: An international, multicenter, comparative cohort study: J Clin Oncol, 2021; 39(1); 66-78
19. Sanmarchi F, Golinelli D, Lenzi J, Exploring the gap between excess mortality and COVID-19 deaths in 67 countries: JAMA Netw Open, 2021; 4(7); e2117359
Figures
Tables
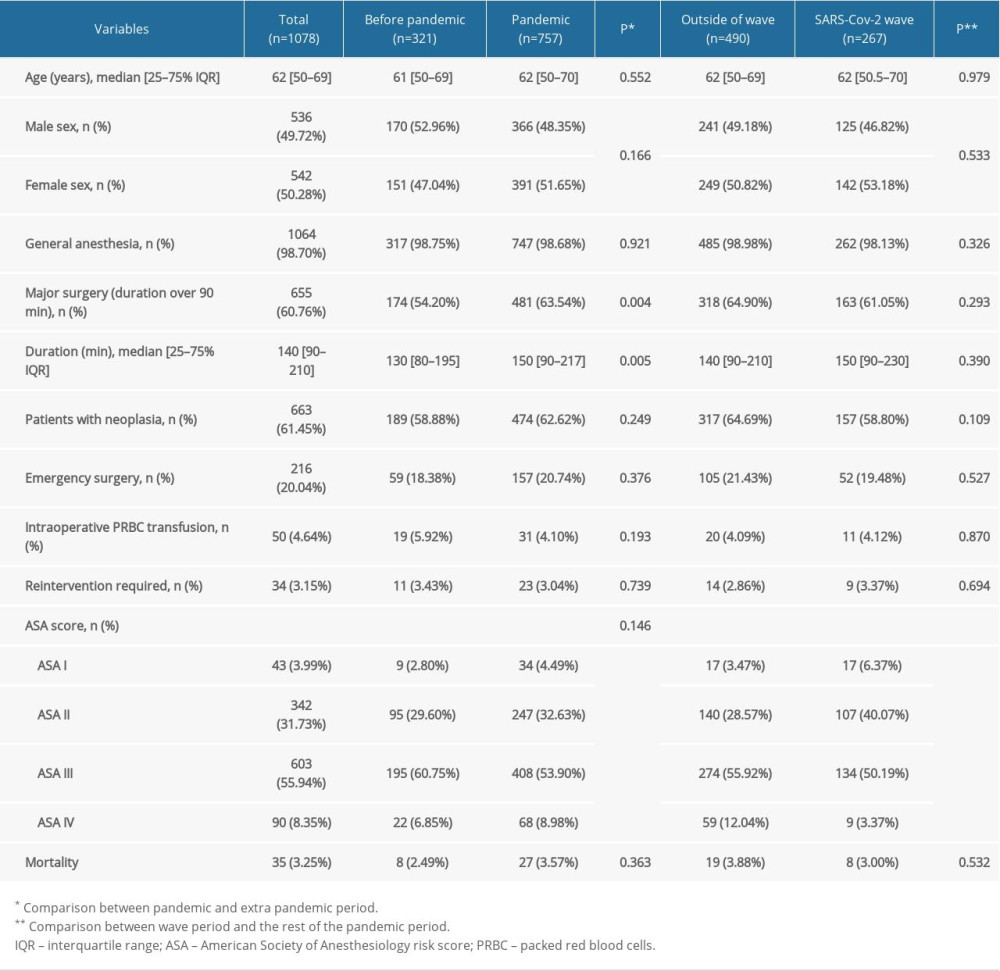 Table 1. Patient characteristics during 3 phases: pre-pandemic, pandemic, and during the wave.
Table 1. Patient characteristics during 3 phases: pre-pandemic, pandemic, and during the wave.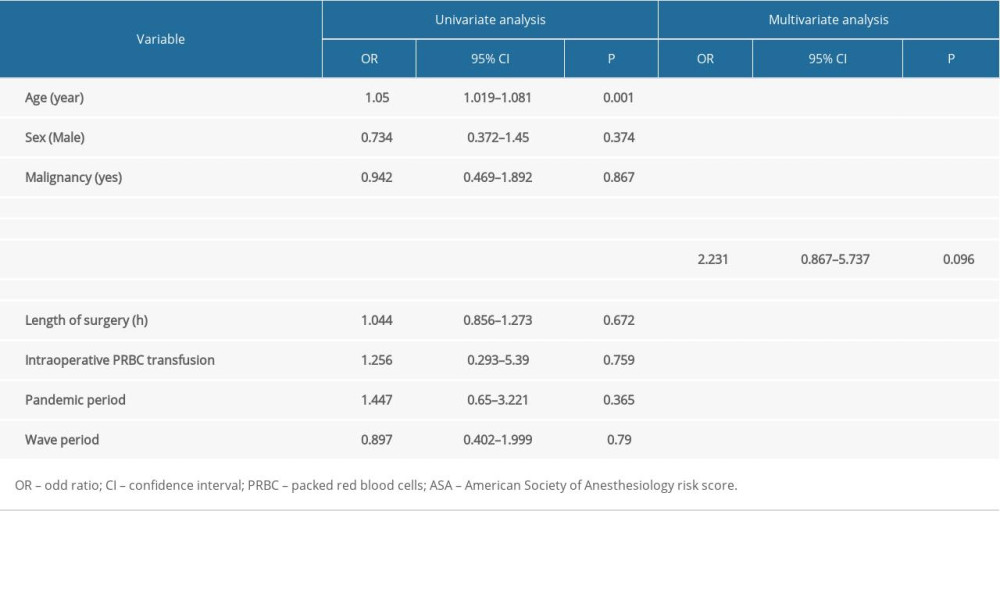 Table 2. Univariate and multivariate regression analysis of factors associated with mortality.
Table 2. Univariate and multivariate regression analysis of factors associated with mortality.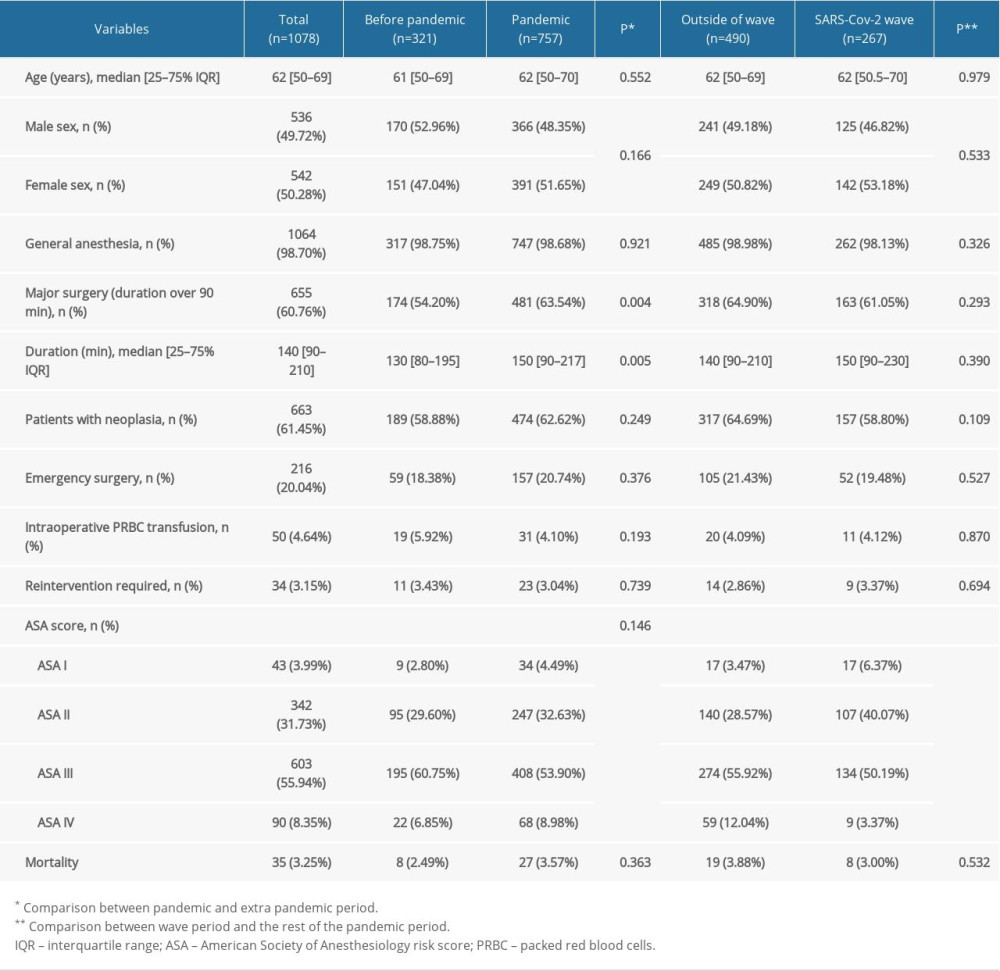 Table 1. Patient characteristics during 3 phases: pre-pandemic, pandemic, and during the wave.
Table 1. Patient characteristics during 3 phases: pre-pandemic, pandemic, and during the wave.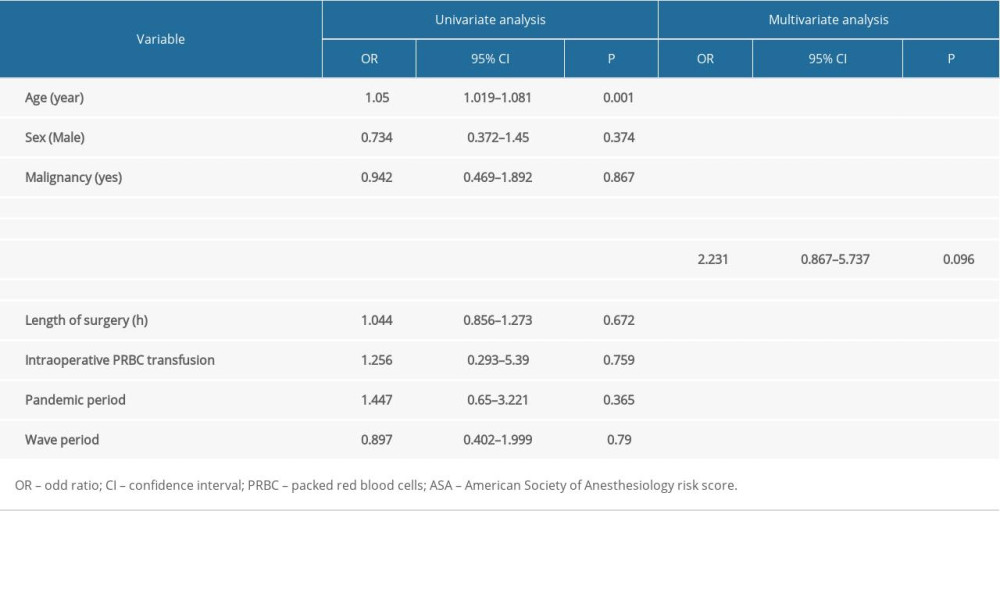 Table 2. Univariate and multivariate regression analysis of factors associated with mortality.
Table 2. Univariate and multivariate regression analysis of factors associated with mortality.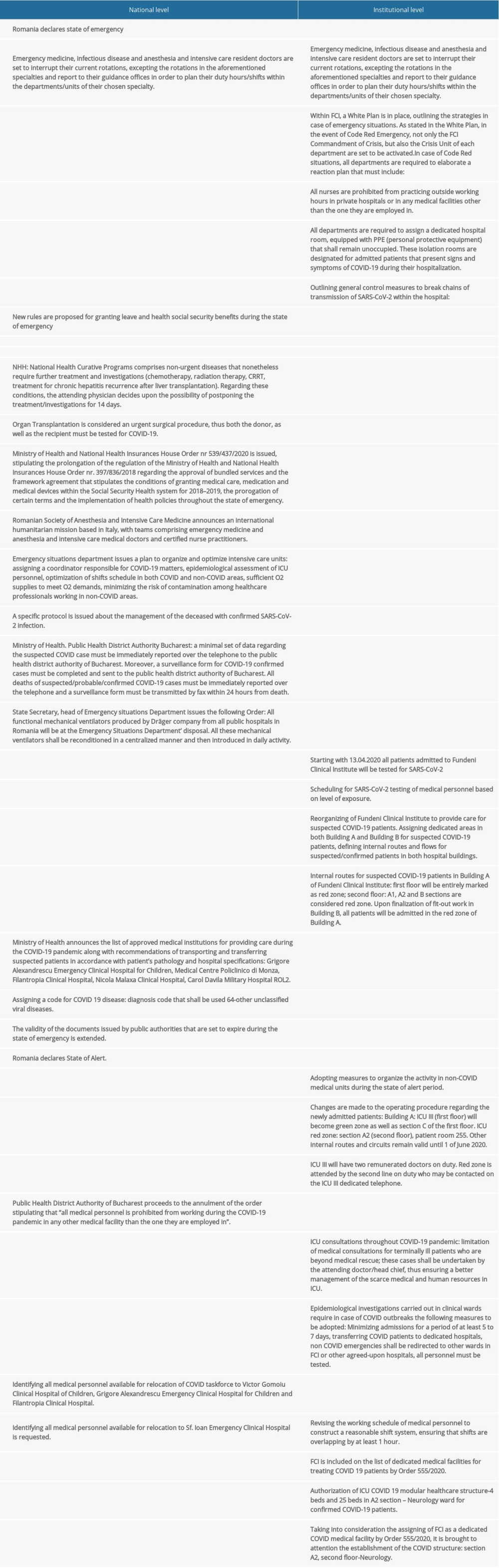 Supplementary Table 1. History of the epidemiology and legal framework of the pandemic in Romania.
Supplementary Table 1. History of the epidemiology and legal framework of the pandemic in Romania. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952