06 March 2022: Clinical Research
Children with Arteriovenous Malformations of the Central Nervous System: A Retrospective Study of 12 Pediatric Cases from a Single Tertiary Center in Slovenia
Ula Arkar1ABCDEF, Tina Vipotnik Vesnaver2BDE, Anja Troha Gergeli1BDE, Neli Bizjak1BD, Damjan OsredkarDOI: 10.12659/MSM.936240
Med Sci Monit 2022; 28:e936240
Abstract
BACKGROUND: Arteriovenous malformation (AVM) of the central nervous system (CNS) is a developmental condition that consists of a focal mass of interconnected veins and arteries. This retrospective study was conducted at the only tertiary center in Slovenia and included 12 pediatric cases of AVM of the CNS, diagnosed between 2000 and 2020.
MATERIAL AND METHODS: The patients were collected based on the ICD coding system. All available medical documentation was reviewed.
RESULTS: Our cohort included 6 boys and 6 girls. The mean age of patients was 9.1 years, range 1 month to 16.3 years. The estimated incidence of pediatric AVM of the CNS in Slovenia is 0.22/100 000 children per year. Ten patients had brain AVM and 2 patients had spinal AVM. At first presentation, 7 patients presented with intracerebral hemorrhage, 2 with focal neurological deficits, 1 with epilepsy, 1 with chronic headache, and 1 patient was asymptomatic. Two patients had their first hemorrhage after an already-established diagnosis of AVM. Endovascular embolization was performed in 50%, surgical resection in 33%, and conservative treatment in 17% of patients. Five patients had no residual neurological sequelae, 6 had some neurological deficits, and 1 patient died. Complete obliteration of AVM was achieved in 3 patients treated with surgery. They all had a favorable outcome, with no or mild deficit.
CONCLUSIONS: The study findings support that early diagnosis and management are required to prevent neurological deterioration and vessel rupture from AVM. Endovascular embolization was the most commonly used procedure. Complete obliteration was associated with good neurological outcome.
Keywords: Arteriovenous Malformations, Central Nervous System, Child, Headache, Hemorrhage, Adolescent, Child, Preschool, Embolization, Therapeutic, Female, Follow-Up Studies, Humans, Incidence, Infant, Infant, Newborn, Intracranial Arteriovenous Malformations, Male, Radiosurgery, Slovenia, Tertiary Care Centers
Background
Although arteriovenous malformations (AVM) are a rare vascular pathology of the central nervous system (CNS), they are the most common cause of spontaneous intracranial hemorrhage and hemorrhagic stroke in the pediatric population and thus represent an important cause of morbidity and mortality [1–5]. The lesions consist of feeding arteries, a dysplastic nidus, and draining veins, and are therefore a type of arteriovenous shunt with high blood flow and low resistance [1–5]. The reported incidence of brain AVM is 1.3 per 100 000 patient-years [2,3,5] and approximately 12–21% of all lesions are found in children [1,4,6,7].
Arteriovenous malformations were previously described as congenital lesions, but the increasing number of cases with de novo formation suggests that they are dynamic lesions that can arise postnatally and may spontaneously regress or enlarge over time [2,8]. They may present at any age, but most commonly between the second and the fourth decade of life [2,3,6]. They usually appear as solitary lesions [2,3,5,6]. However, multiple lesions can be observed in association with some syndromes, such as Osler-Weber-Rendu syndrome [2,3,5,6].
Arteriovenous malformations present with a variety of clinical symptoms and signs, most commonly with intracranial hemorrhage, seizures, chronic headache, and/or focal neurologic deficits [2–5]. Approximately 15% of lesions are incidental findings [2–5]. In children, hemorrhagic presentation is more common than in adults, accounting for approximately 75% of all cases [1,4,6]. Presentation in the neonatal period and infancy is rare [6]. In neonates, congestive heart failure (CHF) is the most common presentation of AVM [6]. Infants may present with macrocrania and hemorrhage, whereas CHF is less common in this age group, and is usually milder [6].
For previously unruptured lesions, the reported annual risk of hemorrhage is 2–4% in children and adults [1,4–6]. However, the cumulative risk is greater in children because they have more years to live with an AVM [1,4–6]. Factors that increase the risk of rupture include previous rupture, deep venous drainage, associated aneurysms, and deep-seated location [1–3,5]. Lesions can occur anywhere in the brain and spinal cord [3].
The morphology of AVM differs among age groups [2]. In neonates and infants, the lesions are fistulous, without a dysplastic vascular network, whereas older children have nidal lesions [2]. Computed tomography (CT) is usually the first examination performed when intracranial hemorrhage is suspected, but it often fails to identify the cause of the hemorrhage [2,3,6]. With CT angiography (CTA), feeding arteries, the intervening nidus, and draining veins are visualized after administration of contrast [2,3,6]. Magnetic resonance imaging (MRI) is used for screening and routine follow-ups and can help determine the location and size of the lesion [2,3,6]. Digital subtraction angiography (DSA) remains the criterion standard, as it can reveal the exact angioarchitecture and hemodynamic features of AVM and is necessary for surgical planning [2,3,6]. Various classification systems are used to guide treatment and predict outcome [4–6]. The most commonly used system for intracranial lesions is the Spetzer Martin grade, which classifies lesions into 5 classes based on size, location, and pattern of venous drainage [4–6].
Arteriovenous malformations can be treated conservatively or by endovascular embolization, microsurgical resection, and stereotactic radiosurgery [2,6]. Any combination of techniques can be used for a better outcome [2,6]. The goal of treatment is complete obliteration to prevent further bleeding [2,6]. Treatment of asymptomatic lesions remains controversial as treatment-related morbidity can be significant but should be considered in children because the lifetime risk of bleeding is high [1,2,6].
This retrospective study included 12 pediatric cases of arteriovenous malformations of the central nervous system, diagnosed between 2000 and 2020 at University Children’s Hospital in Ljubljana, which is the only tertiary center in Slovenia for treatment of pediatric patients with AVM of the CNS.
Material and Methods
ETHICS STATEMENT:
The study was approved by the National Medical Ethics Committee of the Republic of Slovenia (0120-18/2020/15). Due to the retrospective nature of the study, informed consent was not obtained from patients/parents.
PATIENT COLLECTION:
For this observational cohort study, we evaluated medical records of children aged 0–18 years diagnosed with AVM of the CNS and treated at University Children’s Hospital, Slovenia, between January 2000 and April 2020. Patient data were collected from an electronic medical record system and paper record archives, and radiological images were collected for all patients. Variables analyzed included sex, clinical presentation, age at first presentation, radiological characteristics, treatment, and outcome.
We relied on the disease coding system when recruiting patients. In Slovenia, we have used the International Classification of Diseases (ICD) version 10 from 2000 onward. In our cohort of patients, brain AVM were coded as Q28.2 (Arteriovenous malformation of cerebral vessels) and spinal AVM were coded as Q28.0 (Arteriovenous malformation of precerebral vessels). Some patients in our cohort were initially evaluated for the complication of AVM or as an unspecific finding on brain imaging, so they were not assigned an optimal code at first presentation. We observed this in 3 patients, who were coded as D43.1 (Neoplasm of uncertain or unknown behavior of brain, infratentorial), D33.0 (Benign neoplasm of brain, supratentorial), and I60.6 (Subarachnoid hemorrhage from other intracranial arteries). In those 3 patients, the code was corrected after it became clear that they had an AVM.
INCIDENCE ESTIMATION:
To estimate the incidence of AVM of the CNS in Slovenia, we used demographic data from the Statistical Office of the Republic of Slovenia. Since our hospital is the only tertiary center for pediatric neurology in the country, we believe that our data are representative of the entire pediatric population in Slovenia.
Results
BASIC PATIENT DATA AND DEMOGRAPHICS:
We identified 12 patients with AVM of the CNS during the 20-year period. The female-to-male ratio was 1: 1, and the mean age at presentation was 9.1 years (range 1 month to 16.3 years).
To estimate the incidence of AVM of the CNS in Slovenia, we used demographic data from the Statistical Office of the Republic of Slovenia. When analyzing the data, we noticed that new cases of children with AVM were unevenly distributed across years, with a large percentage of new cases identified after 2009. To avoid underreporting of incidence, we decided to calculate incidence based on data from 2009–2020 to make the incidence estimate more reliable. Prior to 2009, MRI imaging was less accessible, so it is possible that some patients with AVM who became symptomatic and perhaps died during this period remained undiagnosed with AVM. Therefore, the estimated incidence of pediatric AVM of the CNS in Slovenia is 0.22/100 000 children per year.
PRESENTATION AND MEDICAL HISTORY:
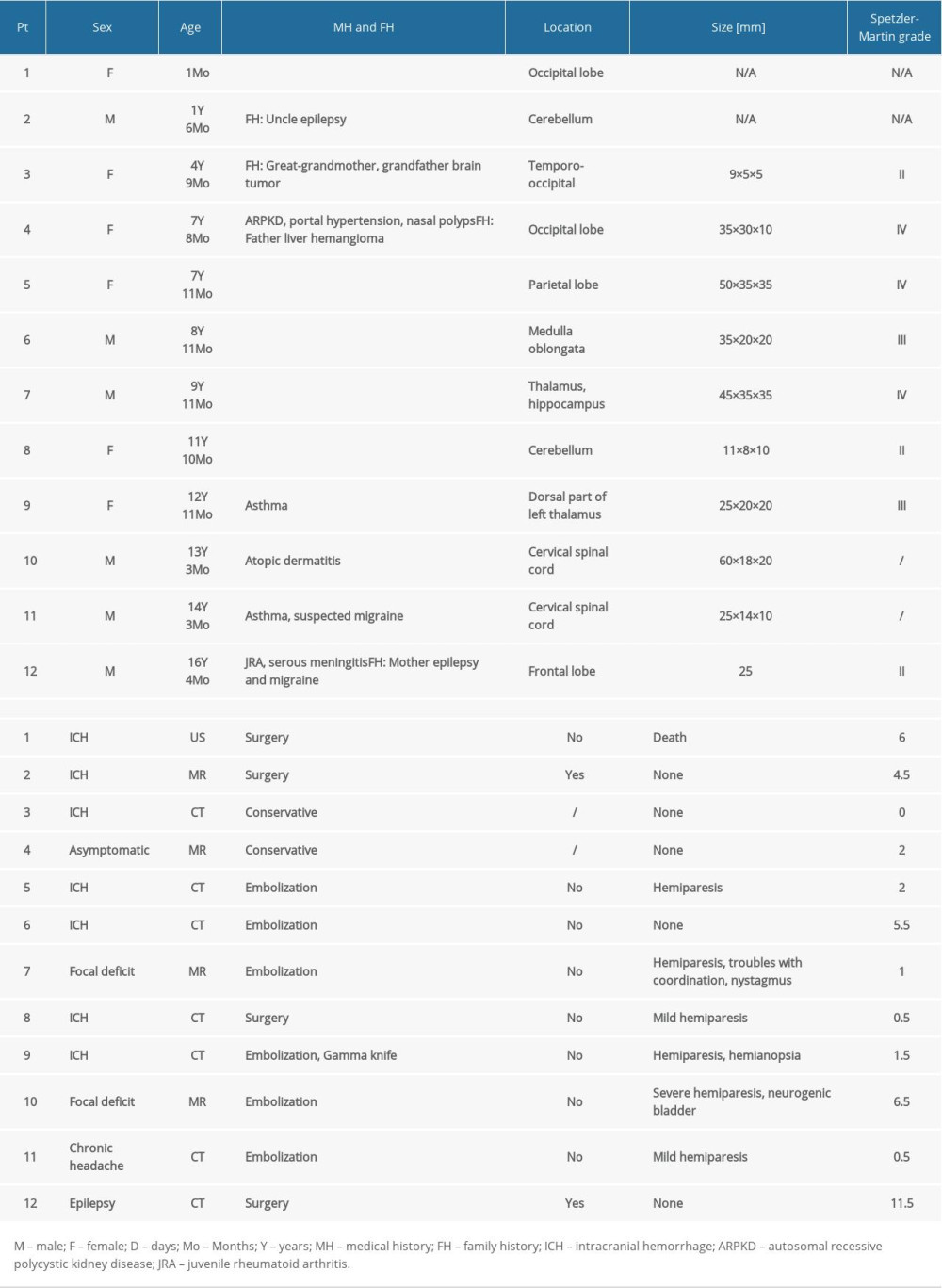
Of the 12 patients, 11 were symptomatic and 1 was asymptomatic. The former were discovered after an acute onset of neurological symptoms, and in the latter the presence of an AVM was an incidental finding. In our cohort, 7 patients presented with symptomatic intracerebral hemorrhage (ICH), 2 patients with focal neurological deficits (both with hemiparesis), 1 patient with epilepsy, and 1 patient with chronic headache. Of 12 patients, 9 had a hemorrhage: 7 as first presentation and 2 after a previously established diagnosis (Patients 7 and 11). Patient 7 first presented with hemiparesis and experienced his first ICH 6 months after being diagnosed. Before ICH, we underwent 1 procedure of endovascular embolization. Patient 11 presented with chronic headache that first appeared 2 years before his first ICH. He did not receive treatment before his first ICH. A case of acute parenchymal and intraventricular hemorrhage is shown in Figure 1. As for vision problems, Patient 2 had strabismus and Patient 8 reported a feeling of pain between the eyes. None of our patients reported visual field defects, which we could not detect even on examination. None of our patients had hearing problems at the time of diagnosis.
Some patients had a history of other diseases and a family history of neurological diseases. The specific data for each patient are shown in Table 1. Patient 4, the only asymptomatic patient in our cohort, had autosomal recessive polycystic kidney disease with portal hypertension and confirmed genetic mutation in the gene PKHD1. The arteriovenous malformation was detected on cranial MRI performed to evaluate nasal polyps.
RADIOLOGIC IMAGING AND FEATURES:
Location, size, morphology, and Spetzler-Martin grade of the AVM were evaluated. All patients had a single lesion. Of the 12 patients, 7 had supratentorial AVM, 2 patients had cerebellar AVM, 2 patients had spinal AVM, and 1 patient had brainstem AVM. More detailed localizations for each patient are listed in Table 1. Regarding the side, 3 lesions were located in the median plane, 5 on the right side, and 4 on the left side. Spetzler-Martin grade was assigned for intracranial lesions. Three lesions were classified as grade II, 2 as grade III, and 3 as grade IV. For Patient 1, we could not determine the size or Spetzler-Martin grade because radiological images were not available at the time of evaluation for this study. In Patient 2, the AVM was not seen on radiological images but was later confirmed histologically.
We were also interested in which imaging modalities were used at initial presentation, what additional imaging was performed for better morphologic characterization, and what modality was used for follow-up. At initial presentation, the youngest of our patients, at 1 month of age, underwent US, 4 patients underwent MRI, and 7 patients underwent a CT scan. Additional imaging was performed for better morphologic characterization. Overall, US was performed in 1, CT in 10, and MRI in 12 of 12 patients. We also utilized DSA in 11 patients. MRI was the modality of choice for follow-up, although US was used as long as possible in the youngest of our patients. During follow-up, none of the patients developed a new AVM.
TREATMENT STRATEGIES AND OUTCOME:
In our cohort, endovascular embolization was the most common treatment procedure and was performed in 6/12 patients. Of these 6 patients, 5 had more than 1 procedure and 1 of them had as many as 11 procedures. Surgical resection was performed in 4 patients, and 2 of them needed more than 1 procedure. Two patients were managed conservatively – Patient 4 was asymptomatic and had the lesion discovered incidentally. She was followed up regularly every 2 years and did not require surgical treatment. Patient 3 presented with a hemorrhage but had no residual neurologic deficits after the acute event. For lesions treated surgically, complete obliteration of the lesion was achieved in 75% of patients. In lesions treated with endovascular embolization, complete obliteration was not achieved in any of the 6 treated patients. Three endovascular procedures were performed in Patient 9, while the remaining portion of the AVM was treated with a gamma knife. Patient 9 had an AVM lesion in the dorsal part of the left thalamus. Because of the hemorrhagic history of the lesion and to avoid further possible bleeding, the surgeons suggested complete resolution of the lesion. However, they felt that the final step of resolution should be performed with the gamma knife to allow complete closure and avoid worsening of the neurologic deficits.
An example of complete obliteration of AVM after surgical treatment is shown in Figure 2. An example of partial occlusion after endovascular embolization is shown in Figure 3.
The mean follow-up time was 3.5 years (range, 0 years to 11.5 years). At the time of the study, 9 patients were still receiving regular follow-up, Patient 1 died, Patient 3 was lost to follow-up, and Patient 12 was referred to an adult neurologist for follow-up. Of the 12 patients, 5 had no residual neurologic deficits at follow-up, 2 patients had mild deficits (discrete hemiparesis and well-controlled epilepsy), 3 patients had moderate deficits (spastic hemiparesis), one patient had severe deficits (developmental delay with severe attention deficit), and 1 patient died. The specific deficits for each patient are listed in Table 1. Hemiparesis of varying degrees was the most common residual deficit. The only patient who died had dystonic cerebral palsy, epilepsy, severe intellectual disability, and hypertrophic cardiomyopathy (Patient 1), and she died at the age of 8.7 years; the cause of death remains unknown since she died outside the hospital and her parents refused autopsy. Of the 3 patients who achieved complete obliteration of the lesion, 2 patients had no deficits and 1 had a mild deficit (discrete hemiparesis).
Although only 1 patient initially presented with epilepsy (Patient 12), 3 other patients developed seizures after the initial hemorrhage or after surgery. Of the 12 patients, 5 received antiepileptic drugs (AED). The most frequently used AED was levetiracetam (3 patients).
Discussion
Arteriovenous malformations of the central nervous system are a rare vascular pathology but are prone to bleeding and can cause a life-threatening medical condition. We identified 12 children diagnosed with AVM in the past 20 years in Slovenia; thus, the estimated incidence of AVM in the pediatric population of Slovenia is 0.22/100 000 children per year. Endovascular embolization was found to be the most commonly used treatment procedure in our cohort of patients, and complete obliteration was associated with a good neurological outcome.
In our cohort, AVM manifested with different clinical findings. The most common presentation was ICH, which is consistent with other studies [1,4,6]; it was observed in 58% of patients. Some patients in our cohort experienced their first bleed after AVM had already been diagnosed, suggesting that early surgical or endovascular intervention should be considered to prevent further complications.
All 12 patients in our cohort had a solitary lesion. Only 1 patient had a known genetic comorbidity (an autosomal recessive polycystic kidney disease with mutation in the PKHD1 gene), but it is uncertain whether this contributed to the development of the AVM. This gene may be associated with Abernethy malformation, a rare congenital anomaly characterized by partial or complete absence of the portal vein and subsequent development of an extrahepatic portosystemic shunt [9]. AVM are usually associated with somatic mutations [10,11]. Genotyping of affected tissue can provide additional data on somatic mutations [10,11] and offer new approaches with genetically targeted treatment [12]. Published case reports of genetically targeted treatment with trametinib, a mitogen-activated protein kinase (MEK) inhibitor, in patients with extracranial AVM showed promising results, with decreased blood flow through AVM and significant improvement of clinical status [12,13].
In our cohort, a Spetzler-Martin grade could not be assigned for all lesions because radiological images were not available for some patients in our cohort and because it is not applicable for spinal lesions. The grading system did not prove to be a relevant clinical tool in our patient cohort as it did not guide decisions about therapeutic interventions or predict outcome, although this may be related to the relatively small number of patients in our study.
The optimal management for pediatric AVM remains controversial. A recent systematic review and meta-analysis of treatment strategies and related outcomes of brain AVM in children [14] found that patients treated only with surgery had a 79.4% obliteration rate, 22.5% complication rate, and 4.4% recurrent hemorrhage rate, while embolization alone had a 54.1% obliteration rate, 26.4% complication rate, and 9.7% recurrent hemorrhage rate. Complication and mortality rates were the lowest for multimodal treatments, while mortality rate was highest in conservatively managed patients. Recurrence after treatment of brain AVM has been shown to be more common in children than in adults [14,15]. Recurrence of AVM after treatment was also shown to be inversely associated with age [14]. In our cohort, different therapeutic approaches were used depending on lesion size, location, vascular anatomy, clinical presentation, and age of the patient. Management was led by a multidisciplinary team (pediatric neurologist, neuroradiologist, interventional radiologist, and neurosurgeon) with experience in treating infants and children with AVM. The best therapeutic approach was decided individually for each patient. In the only asymptomatic patient from our cohort, immediate treatment was not indicated. In symptomatic patients, we strived to use less-invasive methods, using endovascular embolization instead of surgery, whenever this would lead to resolution of patients’ problems and would likely result in a favorable outcome. We also collaborated with neurosurgeons from abroad and sometimes transferred patients for treatment abroad, where surgeons decided on optimal treatment in their local multidisciplinary teams. In our cohort, endovascular embolization was used in 50% of cases, with 83% of children requiring more than 1 procedure, and complete obliteration was not achieved in any case, which considerably differs from the findings in previously mentioned meta-analysis. Radiosurgery could be used to achieve complete obliteration in these patients to minimize the possibility of bleeding or rebleeding. In the subgroup of patients treated with surgery, complete obliteration was achieved in 75% of patients. Half of the surgically treated patients underwent more than 1 procedure. All patients with complete obliteration of the lesion had good neurologic outcomes, with mild or no neurologic deficit. Some studies suggest that achieving complete angiographic obliteration of the AVM is essential in children because of their longer life expectancy and higher risk of rupture compared with adults [16]. However, despite complete obliteration of the lesion, long-term radiologic follow-up is recommended to rule out the small possibility of AVM recurrence [17,18].
This study has several limitations, including its retrospective nature and a small sample size. Because our hospital is the only tertiary center for pediatric neurology in the country, we believe that we identified all children diagnosed with AVM of the CNS in Slovenia during the studied 20-year period. However, we may have missed some asymptomatic patients or patients who died because of an acute hemorrhage, which would cause the reported incidence to be underestimated. It is also possible that a patient with AVM was not referred to our tertiary center, but the likelihood of this happening is negligible. During the analysis of the data, we noticed that new cases of children with AVM were unevenly distributed over the years. We attribute this to the fact that MRI was much more readily available in the years after 2009. Another limitation of the study is the 20-year study duration, a period during which the availability of various diagnostic methods has changed. Because of the small sample size, we could not identify relevant clinical features of AVM, which would be related to a better outcome if certain treatment options would be utilized. Larger studies or pooled data could provide such relevant medical information.
Conclusions
Arteriovenous malformations of the central nervous system are a rare pathology in the pediatric population, with potentially serious consequences. The study findings support that early diagnosis and management are required to prevent neurological deterioration and vessel rupture from AVM. Clinical presentation is not uniform and outcome is often unpredictable, but early diagnosis and treatment can reduce mortality and morbidity in these patients. Endovascular embolization was the most commonly used treatment procedure in our cohort of patients. Complete obliteration was associated with good neurological outcome. Further research is needed to better understand the subtle relationships between pathology, treatment, and outcome in children with AVM and to develop optimal diagnostic and treatment protocols.
Figures
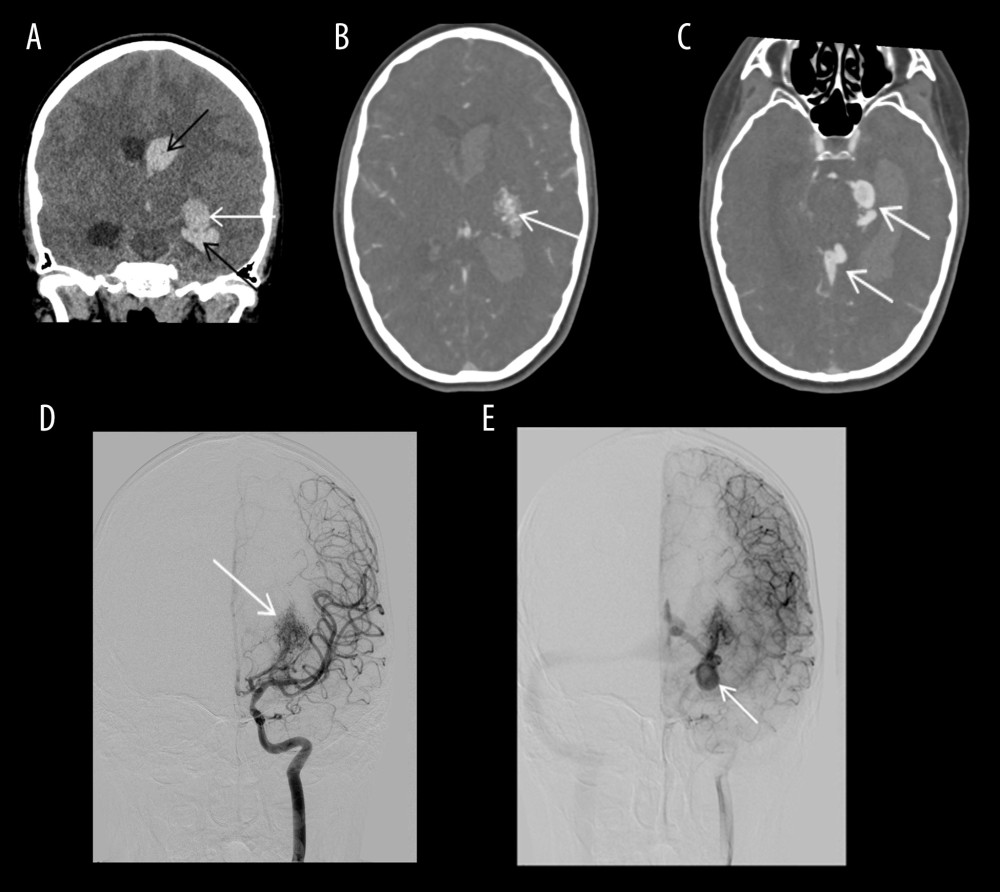 Figure 1. Acute parenchymal and intraventricular hemorrhage in a patient with arteriovenous malformation (Patient 9)(A) CT image in coronal plane: acute parenchymal (white arrow) and intraventricular hemorrhage (black arrows). (B) Intracranial CT angiography: Arteriovenous malformation (AVM) nidus (arrow). (C) Intracranial CT angiography: dilated draining veins (arrows). (D) DSA arterial phase: AVM nidus with feeding anterior choroidal artery. (E) DSA early venous phase: dilated veins draining to the deep venous system.
Figure 1. Acute parenchymal and intraventricular hemorrhage in a patient with arteriovenous malformation (Patient 9)(A) CT image in coronal plane: acute parenchymal (white arrow) and intraventricular hemorrhage (black arrows). (B) Intracranial CT angiography: Arteriovenous malformation (AVM) nidus (arrow). (C) Intracranial CT angiography: dilated draining veins (arrows). (D) DSA arterial phase: AVM nidus with feeding anterior choroidal artery. (E) DSA early venous phase: dilated veins draining to the deep venous system. 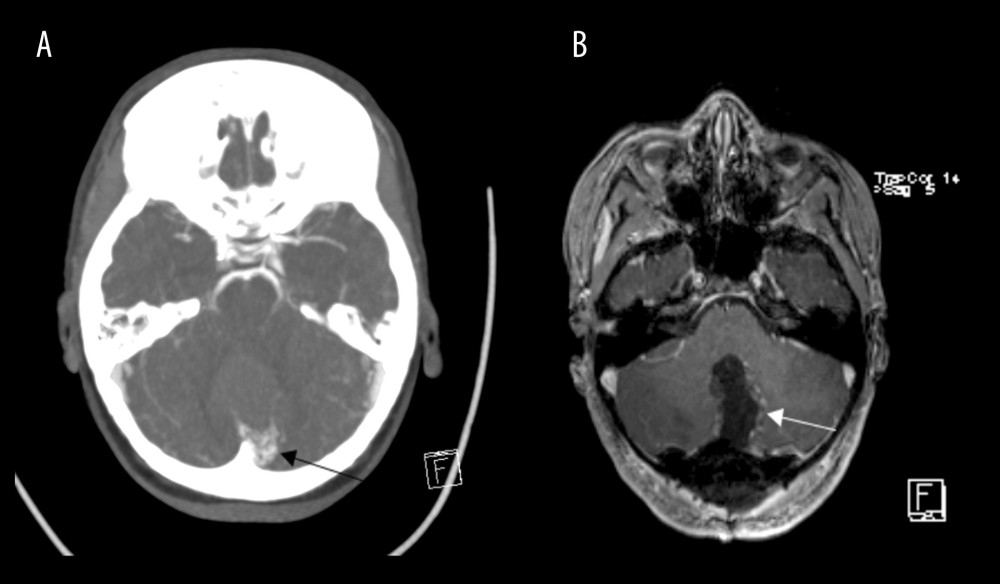 Figure 2. Complete obliteration of arteriovenous malformation after surgical treatment (Patient 8)(A) CT image in transverse plane; small arteriovenous malformation (AVM) in the left parasagittal infratentorial region (arrow). (B) MRI T1 CE sequence in transverse plane; complete surgical resection of the AVM (arrow).
Figure 2. Complete obliteration of arteriovenous malformation after surgical treatment (Patient 8)(A) CT image in transverse plane; small arteriovenous malformation (AVM) in the left parasagittal infratentorial region (arrow). (B) MRI T1 CE sequence in transverse plane; complete surgical resection of the AVM (arrow). 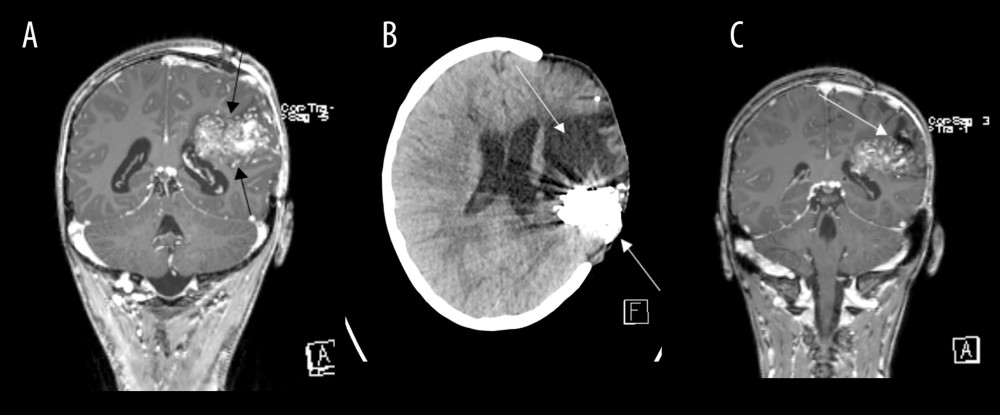 Figure 3. Partial occlusion of arteriovenous malformation after endovascular embolization (Patient 5)(A) MRI T1 CE sequence in coronal plane: Large arteriovenous malformation (AVM) in the left frontoparietal region (arrows). (B) CT in transverse plane; hyperdense embolization material (arrow) posterior to large area of encephalomalacia after parenchymal hematoma (arrow). (C) MRI T1 CE sequence in coronal plane; partially occluded AVM (arrow).
Figure 3. Partial occlusion of arteriovenous malformation after endovascular embolization (Patient 5)(A) MRI T1 CE sequence in coronal plane: Large arteriovenous malformation (AVM) in the left frontoparietal region (arrows). (B) CT in transverse plane; hyperdense embolization material (arrow) posterior to large area of encephalomalacia after parenchymal hematoma (arrow). (C) MRI T1 CE sequence in coronal plane; partially occluded AVM (arrow). References
1. Ding D, Starke RM, Kano H, International multicenter cohort study of pediatric brain arteriovenous malformations. Part 1: Predictors of hemorrhagic presentation: J Neurosurg Pediatr, 2017; 19; 127-35
2. Lawton MT, Rutledge WC, Kim H, Brain arteriovenous malformations: Nat Rev Dis Primers, 2015; 1; 1-21
3. Osbun JW, Reynolds MR, Barrow DL, Chapter 3 – Arteriovenous malformations: Epidemiology, clinical presentation, and diagnostic evaluation: Handbook of Clinical Neurology, 2017; 143; 25-29, Elsevier
4. Oulasvirta E, Koroknay-Pál P, Hafez A, Characteristics and long-term outcome of 127 children with cerebral arteriovenous malformations: Neurosurgery, 2019; 84; 151-59
5. Ozpinar A, Mendez G, Abla AA, Chapter 1 – Epidemiology, genetics, pathophysiology, and prognostic classifications of cerebral arteriovenous malformations: Handbook of Clinical Neurology, 2017; 143; 5-13, Elsevier
6. Toma AK, Davagnanam I, Ganesan V, Brew S, Cerebral arteriovenous shunts in children: Neuroimaging Clin N Am, 2013; 23; 757-70
7. Ma X, Tong X, Wu J, Seizure control following treatment of brain arteriovenous malformations in pediatric patients: Child’s Nervous System, 2016; 32; 2387-94
8. Dalton A, Dobson G, Prasad M, Mukerji N, De novo intracerebral arteriovenous malformations and a review of the theories of their formation: Br J Neurosurg, 2018; 32; 305-11
9. Mi X-X, Li X-G, Wang Z-R, Abernethy malformation associated with Caroli’s syndrome in a patient with a PKHD1 mutation: A case report: Diagn Pathol, 2017; 12; 61
10. Konczyk DJ, Goss JA, Smits PJ, Arteriovenous malformation associated with a HRAS mutation: Hum Genet, 2019; 138; 1419-21
11. Revencu N, Fastre E, Ravoet M, RASA1 mosaic mutations in patients with capillary malformation-arteriovenous malformation: J Med Genet, 2020; 57; 48-52
12. Edwards EA, Phelps AS, Cooke D, Monitoring arteriovenous malformation response to genotype-targeted therapy: Pediatrics, 2020; 146; e20193206
13. Lekwuttikarn R, Lim YH, Admani S, Genotype-guided medical treatment of an arteriovenous malformation in a child: JAMA Dermatology, 2019; 155; 256-57
14. Pezeshkpour P, Dmytriw AA, Phan K, Treatment strategies and related outcomes for brain arteriovenous malformations in children: A systematic review and meta-analysis: Am J Roentgenol, 2020; 215; 472-87
15. Morgenstern PF, Hoffman CE, Kocharian G, Postoperative imaging for detection of recurrent arteriovenous malformations in children: J Neurosurg Pediatr, 2016; 17; 134-40
16. El-Ghanem M, Kass-Hout T, Kass-Hout O, Arteriovenous malformations in the pediatric population: Review of the existing literature: Interv Neurol, 2016; 5; 218-25
17. Niazi TN, Klimo P, Anderson RCE, Raffel C, Diagnosis and management of arteriovenous malformations in children: Neurosurg Clin North Am, 2010; 21; 443-56
18. Copelan A, Drocton G, Caton MT, Brain arteriovenous malformation recurrence after apparent microsurgical cure: Increased risk in children who present with arteriovenous malformation rupture: Stroke, 2020; 51; 2990-96
Figures
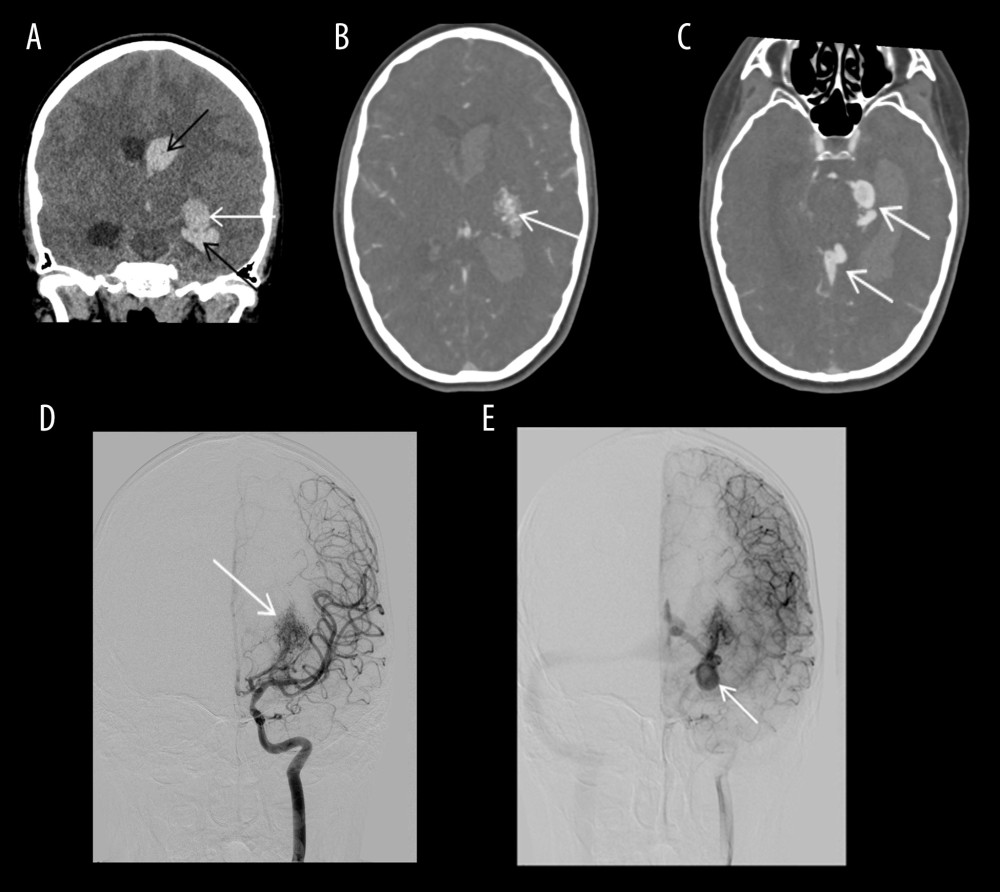 Figure 1. Acute parenchymal and intraventricular hemorrhage in a patient with arteriovenous malformation (Patient 9)(A) CT image in coronal plane: acute parenchymal (white arrow) and intraventricular hemorrhage (black arrows). (B) Intracranial CT angiography: Arteriovenous malformation (AVM) nidus (arrow). (C) Intracranial CT angiography: dilated draining veins (arrows). (D) DSA arterial phase: AVM nidus with feeding anterior choroidal artery. (E) DSA early venous phase: dilated veins draining to the deep venous system.
Figure 1. Acute parenchymal and intraventricular hemorrhage in a patient with arteriovenous malformation (Patient 9)(A) CT image in coronal plane: acute parenchymal (white arrow) and intraventricular hemorrhage (black arrows). (B) Intracranial CT angiography: Arteriovenous malformation (AVM) nidus (arrow). (C) Intracranial CT angiography: dilated draining veins (arrows). (D) DSA arterial phase: AVM nidus with feeding anterior choroidal artery. (E) DSA early venous phase: dilated veins draining to the deep venous system.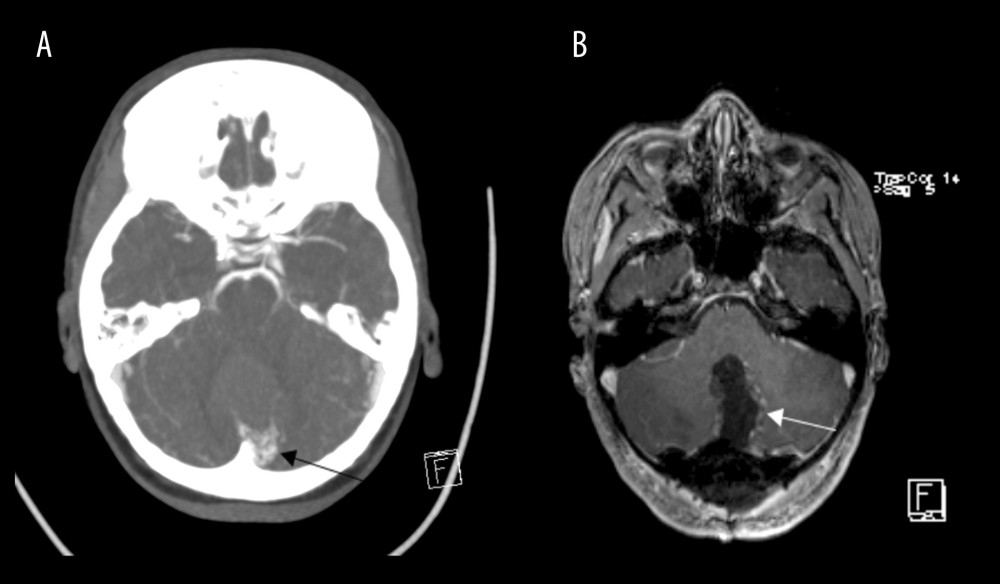 Figure 2. Complete obliteration of arteriovenous malformation after surgical treatment (Patient 8)(A) CT image in transverse plane; small arteriovenous malformation (AVM) in the left parasagittal infratentorial region (arrow). (B) MRI T1 CE sequence in transverse plane; complete surgical resection of the AVM (arrow).
Figure 2. Complete obliteration of arteriovenous malformation after surgical treatment (Patient 8)(A) CT image in transverse plane; small arteriovenous malformation (AVM) in the left parasagittal infratentorial region (arrow). (B) MRI T1 CE sequence in transverse plane; complete surgical resection of the AVM (arrow).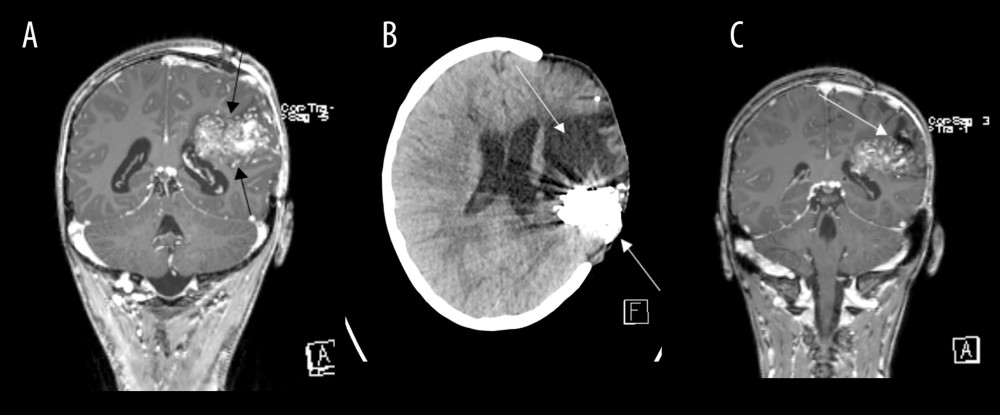 Figure 3. Partial occlusion of arteriovenous malformation after endovascular embolization (Patient 5)(A) MRI T1 CE sequence in coronal plane: Large arteriovenous malformation (AVM) in the left frontoparietal region (arrows). (B) CT in transverse plane; hyperdense embolization material (arrow) posterior to large area of encephalomalacia after parenchymal hematoma (arrow). (C) MRI T1 CE sequence in coronal plane; partially occluded AVM (arrow).
Figure 3. Partial occlusion of arteriovenous malformation after endovascular embolization (Patient 5)(A) MRI T1 CE sequence in coronal plane: Large arteriovenous malformation (AVM) in the left frontoparietal region (arrows). (B) CT in transverse plane; hyperdense embolization material (arrow) posterior to large area of encephalomalacia after parenchymal hematoma (arrow). (C) MRI T1 CE sequence in coronal plane; partially occluded AVM (arrow). In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952