21 December 2022: Clinical Research
Comparison of Bond Strength of Orthodontic Brackets Onto the Tooth Enamel of 120 Freshly Extracted Adult Bovine Medial Lower Incisors Using 4 Adhesives: A Resin-Modified Glass Ionomer Adhesive, a Composite Adhesive, a Liquid Composite Adhesive, and a One-Step Light-Cured Adhesive
Agata Prylińska-Czyżewska1ABCDE*, Zofia Maciejewska-Szaniec1BEF, Aneta Olszewska1DF, Marta Polichnowska2D, Beniamin Oskar Grabarek3F, Damian Dudek4F, Dawid Sobański3F, Agata Czajka-Jakubowska1DEDOI: 10.12659/MSM.938867
Med Sci Monit 2022; 28:e938867
Abstract
BACKGROUND: This study aimed to compare the bond strength of orthodontic brackets onto the tooth enamel of 120 freshly extracted adult bovine medial lower incisors using 4 adhesives: a resin-modified glass ionomer adhesive, a composite adhesive, a liquid composite adhesive, and a one-step light-cured adhesive.
MATERIAL AND METHODS: The study group (120 freshly extracted bovine medial lower incisors) was divided into equal subgroups depending on the type of adhesive used to fix the brackets to the tooth enamel (n=30), and then according to the observation time (n=10). Orthodontic brackets were fixed onto the tooth enamel for 24 hours (T1), 3 months (T2), and 6 months (T3) using 4 types of adhesives: resin-modified glass ionomer adhesive Fuji Ortho LC, composite adhesive Transbond Plus Light Cure Band, flowable composite adhesive Transbond Supreme Low Viscosity, and a one-step light-cured adhesive GC Ortho Connect. Shear tests and fracture plane analyses were performed.
RESULTS: Statistically significant differences at time T1 were noted in the comparison of shear stress values when brackets were fixed with GC Ortho Connect adhesive compared to other adhesives (P<0.05), except for the Transbond Plus adhesive (P>0.05). At time T3, significant statistical differences occurred between GC Fuji Ortho LC and the other 3 adhesives (P<0.05). The fracture analysis showed that, regardless of the time function, adhesive-cohesive fractures without damage to the enamel were the most common for all the assessed materials.
CONCLUSIONS: Of the adhesives evaluated, GC Ortho Connect appears to be the most appropriate choice for bonding orthodontic brackets to the enamel surface.
Keywords: Adhesives, Bayer 2000, Orthodontic Brackets, Cattle, Animals, Incisor, Glass Ionomer Cements, Resin Cements, Materials Testing, Dental Enamel, Dental Bonding, Shear Strength
Background
Orthodontic treatment is widely used in both children and adults. The number of adult orthodontic cases has increased dramatically over the past few years [1]. According to the American Association of Orthodontists, the number of adults opting for orthodontic treatment in the US and Canada increased by 16% between 2012 and 2014 [2].
The popularity of orthodontic treatment with fixed appliances [3] means that more and more dental adhesives for securing orthodontic devices are appearing on the market [4–6], and many types of appliances are available that differ in the construction of brackets and bands [7].
Orthodontic brackets are the most important elements of an orthodontic appliance, because their main function is to keep the orthodontic archwire (a metal wire running the entire length of the dental arch) in the correct position. The orthodontic archwire exerts the appropriate force needed to move or rotate the teeth. Without the brackets, it would be impossible to realign uneven teeth, which is why they are an extremely important element. They are glued to the surface of the teeth using an orthodontic adhesive. The brackets have a horizontal slot in which the archwire (ie, the wire connecting the brackets) is placed. The orthodontic archwire is attached to the brackets with metal ligatures or elastic bands [8].
An important element determining the choice of adhesive used to fix orthodontic appliances, as well as the type of appliance, including the type of brackets and bands, is the effect of the applied treatment on the roughness and color of the enamel after its completion. ElSherifa et al showed that the use of APC™ Flash-Free coated brackets had the least effect on enamel roughness and color compared to brackets using APCTM PLUS and Clarity™ Advanced [9].
Considering the long duration of orthodontic treatment [10,11], an important issue is the appropriate choice of the orthodontic appliance and dental adhesive for the treatment process to run smoothly [11]. Due to the influence of additional factors in the oral cavity, such as temperature changes, pH, and forces triggered during chewing or malocclusion, the dental adhesives used should have the appropriate bonding strength to ensure a good bond of the orthodontic bracket to the tooth enamel, as well as preventing any damage to the enamel during the removal of the fixed appliance [12–14]. Moreover, the detachment of orthodontic brackets prolongs the treatment process and causes uncontrolled plaque accumulation, thereby increasing the risk of caries [15].
A relatively common problem that can occur during orthodontic treatment is detachment of the brackets, resulting from, among other things, occlusal forces, mistakes made during bonding of brackets, and structure of the enamel that does not respond to etching [16]. Information on the strength of specific bonding materials is vital for choosing the right adhesive, especially because an adhesive bond that is too strong can cause detachment of enamel prisms during bracket removal [17].
Bovine teeth are a useful research model in dentistry and orthodontics for testing the bond strength of adhesive systems to enamel and dentin. The structure of bovine enamel and dentin is similar to that of human teeth; it is also possible to remove them at the same time and store them under identical conditions [18,19].
Therefore, this study aimed to compare the bond strength of orthodontic brackets onto tooth enamel of 120 freshly extracted adult bovine medial lower incisors using 4 adhesives: a resin-modified glass ionomer adhesive, a composite adhesive, a liquid composite adhesive, and a one-step light-cured adhesive.
Material and Methods
ETHICS:
Based on the decision issued by the Chairman of the Bioethics Committee at the Poznan University of Medical Sciences, this study does not have the characteristics of a medical experiment and thus does not require approval by the Bioethics Committee. Because the animals were raised for meat and not specifically for this study, the teeth, which are classified as waste material, were harvested after the animals had been slaughtered in accordance with the applicable standards [20]. In connection with the above, on 13 December 2018, the only statement issued was “The study does not have the characteristics of a medical experiment”.
STUDY DESIGN:
The study was performed on 120 freshly extracted bovine medial lower incisors from 3-year-old cattle. The study group was divided into equal subgroups depending on the type of adhesive used to fix the brackets onto the tooth enamel (n=30), and then according to the observation time (n=10).
Orthodontic brackets were fixed onto tooth enamel for 24 hours (T1), 3 months (T2), and 6 months (T3) using 4 types of orthodontic adhesives: resin-modified glass ionomer adhesive Fuji Ortho LC (GC Orthodontics Europe GmbH, Breckerfeld, Germany), composite adhesive Transbond Plus Light Cure Band (3M ESPE, Wrocław, Poland), flowable composite adhesive Transbond Supreme Low Viscosity (3M ESPE, Wrocław, Poland), and a one-step light-cured adhesive GC Ortho Connect (GC Orthodontics Europe GmbH, Breckerfeld, Germany).
The specimens were placed in distilled water and incubated at 37°C for 24 hours, 3 months, or 6 months. Shear tests and fracture plane analyses were performed.
THE ATTACHMENT OF ORTHODONTIC BRACKETS TO TOOTH ENAMEL USING VARIOUS ADHESIVES:
Having been cleaned of residual soft tissues, the teeth were kept in physiological saline solution (Sigma Aldrich, St Louis, MO, USA) at 4°C for 1 day, then they were examined for hidden demineralization lesions using the Diagnodent 2095 instrument (KaVo, Biberach, Germany). The teeth were embedded in Futura Self acrylate resin (Schütz-Dental, Rosbach vor der Höhe, Germany) using Teflon moulds (2.5×2.5×2.5 cm) so that the incisal edge was 2 cm above the resin surface and the long axis of the tooth was perpendicular to the base of the mould. The specimens were then placed in physiological saline solution in an incubator at 37°C for 24 hours. Before attaching the brackets, the labial surfaces of the teeth were polished with fluoride-free Kerrhawe Superpolish paste (Spofadental S.A., Warsaw, Poland), then rinsed with distilled water, dried, and etched for 30 seconds with 37% phosphoric acid. In the next stage, the acid was rinsed off, the tooth surfaces were dried, and the brackets were bonded to the enamel according to the manufacturers’ instructions.
Axcess stainless-steel brackets (GC Orthodontics Europe GmbH, Breckerfeld, Germany) with parameters assigned to lower central incisors and a factory-prepared surface for bonding with tooth enamel were used in the tests. The teeth with the attached brackets were stored in distilled water (Sigma Aldrich, St. Louis, MO, USA) in an incubator throughout the study.
The characteristics of the orthodontic adhesive materials used in the current study are presented in Table 1.
SHEAR TEST ANALYSIS:
Shear tests were performed using a Hounsfield H 5KS (UTM, Hounsfield, England) universal testing machine, with a 5000 Newton (N) load cell and a crosshead speed of 0.5 mm/min (Figure 1). The value of the sheer bond strength (SBS) was recorded in megapascals (MPa) by dividing the shear force by the area of the bracket base (3.0 mm2). After the tests, all the teeth were assessed under a Nikon 2T optical microscope (Nikon, Tokyo, Japan) to determine the fracture plane according to the following criteria: A1 – adhesive fracture at the adhesives-bracket border, A2 – adhesive fracture at the enamel-adhesives border, K1 – cohesive fracture within the adhesives, K2 – cohesive fracture within the enamel, AK1 – adhesive-cohesive fracture without enamel damage, and AK2 – adhesive-cohesive fracture with enamel damage.
STATISTICAL ANALYSIS:
In the first statistical analysis stage, the Shapiro-Wilk test was used, confirming the results’ consistency with Gaussian distribution. Then, for the variables that did not have a normal distribution, the Mann-Whitney U test and the
Results
FINDINGS OF THE SHEAR STRESS EXAMINATION:
In the first step of the current study, we evaluated shear stress examinations for 4 different adhesive materials bonding stainless-steel brackets to tooth enamel at 3 time periods. We observed that regardless of the time, the highest values were noted for samples in which orthodontic brackets were bonded to tooth enamel using the GC Ortho Connect adhesive. Statistically significant differences at time T1 were noted in terms of shear stress comparisons when the GC Ortho Connect adhesive was used to fix the brackets compared to other adhesives (
After 3 months of the specimens being stored in distilled water (T2), no statistically significant differences were found between the analysed samples. However, at time T3 (after 6 months), significant statistical differences occurred between GC Fuji Ortho LC and the other 3 adhesives (P<0.05). In all the tested samples, regardless of the type of adhesive material, the shear stress values decreased significantly over time (T1>T2>T3) (P<0.05). Detailed findings are presented in Table 2.
FINDINGS OF THE FRACTURE ANALYSIS:
The fracture analysis showed that, regardless of the time function, adhesive-cohesive fractures without damage to the enamel were the most common for all the assessed materials (AK1, 62.0–62.5%) and, to a lesser extent, adhesive fractures of the A1 (17.5–27 5%) and A2 (10.0–20.0%) types. In the case of the GC Ortho Connect adhesive at T3 (after 6 months), 1 adhesive-cohesive fracture with damage to the enamel (AK2) was recorded. Detailed findings are presented in Table 3 (P<0.05).
Discussion
The bond strength of the bracket to the tooth surface depends on many factors. The most important are study design [21,22], the material from which the bracket was made [23–25], the type of surface [26], the type of adhesive polymerization [27], and the etching procedure [28].
The bond strength between the bracket and tooth enamel is an extremely important issue in the context of the treatment of malocclusion. Re-fixing the brackets after they have become detached is a difficult and unpleasant task, involving mechanical trauma to the adjacent soft tissues of the oral cavity, as well as causing delay in obtaining the expected therapeutic effect [29–31].
The in vitro model of bovine teeth is successfully used in studies which aim to assess the bonding of the bracket onto the enamel surface using various adhesives [18,19].
Over a 21-day period, Godard et al assessed the shear bond strength of ceramic orthodontic brackets to bovine enamel (n=30) using the conventional LI Signature Clear® (RMO) adhesive and the FLI ceramic adhesive® (RMO), dedicated for ceramic brackets. In the group in which the conventional adhesive system was used, the shear bond strength was significantly lower than in the other group [32].
Strength tests assessing the bond between orthodontic brackets and the enamel of bovine teeth using 4 adhesive materials, which differed in terms of their physical and chemical properties, showed that regardless of the time functions, the highest average values of shear stress were obtained for the samples where the GC Ortho Connect material was used.
The use of self-etching materials (SEM) produces a classic etching pattern, and thus a satisfactory bond strength. SEMs are agents that create the possibility of simultaneous conditioning and priming, without the need to rinse with water, and mild airflow is sufficient. Because the monomers responsible for etching are also responsible for bonding, the depth of the demineralized zone corresponds to the penetration depth of the polymerized adhesive. As a consequence, there are no problems with insufficient penetration depth, which improves the quality of the bond and benefits the long-term treatment process [33,34].
Moreover, in the current study it was found that the shear stress values, regardless of the type of adhesive system, decreased significantly (T1>T2>T3) over time, which is consistent with the observations of Mitić et al [6]. The fact that the bond strength weakens over time reduces the risk of damage to the enamel when removing orthodontic brackets. According to Zieliński et al [7], the risk of enamel defects resulting from detachment depends also on the type of bracket used.
The literature indicates that the minimum value of the bond strength must be in the range of 6–8 MPa [35] and the maximum bond strength must be lower than the enamel fracture threshold, which is 14 MPa [36]. Thus, we have confirmed the existence of a chemical bond between the bracket and the enamel surface, regardless of the adhesive used.
In the case of the GC Fuji Ortho LC glass ionomer resin-modified material, the bond strength decreased from 29.06 MPa (T1) to 14.75 MPa (T3) (ie, by almost 50%). It seems that in this case one of the possible reasons for the deterioration in the bond strength could be the absorption of large quantities of water by glass ionomer adhesives, possibly causing the bonds to hydrolyze in the material [37,38].
Summers et al showed that brackets bonded with a resin-modified glass ionomer adhesive had a significantly lower shear bond strength compared to a conventional resin in an in vitro model. Light Bond had a significantly higher bond strength than Fuji Ortho LC after 30 minutes (16.19±2.04 MPa vs 6.93±1.93 MPa) and 24 hours (18.46±2.95 MPa vs 9.56±1.85 MPa). Therefore, we suggest that using the Fuji Ortho LC adhesive is a better solution than using Light Bond because the weaker chemical bond makes it easier to remove any adhesive residue from the enamel surface after removing the brackets [39].
Such advanced degradation processes could also have led to stresses in the tested samples over different time periods. In the case of the GC Fuji Ortho LC material, after 24 hours of keeping the samples in distilled water, the values recorded for this adhesive were much higher than those obtained in similar studies. Feizbakhsh et al evaluated the bond strength of the bracket onto etched and non-etched enamel under dry and wet conditions using the Fuji Ortho LC adhesive. In that in vitro study, 60 intact premolars were used and randomly assigned to 6 groups: 1) etched and dried, 2) etched and moistened with distilled water, 3) etched and moistened with saliva, 4) unetched and dried, 5) unetched and moistened with water, and 6) unetched and moistened with saliva. The average bond strength values in the mentioned groups were 21.86, 16.46, 10.49, 8.12, 9.15, and 9.52 MPa, respectively. Therefore, the bond strength is higher when the brackets are glued to an etched and dried enamel surface [40].
Also, Bucur et al used a group of 120 freshly extracted premolars, divided into 6 subgroups, to evaluate the bond strength of the bracket to dry, water-moistened, and saliva-moistened enamel using Transbond Plus Color Change with Transbond Plus Self-Etching Primer, and Fuji Ortho LC. They demonstrated the required bond strength regardless of the adhesive used and the manner of enamel preparation (12.31–15.86 MPa), and when the enamel was moistened with saliva, the Fuji Ortho LC adhesive was characterized by a higher bond strength compared to Transbond Plus Color Change with Transbond Plus Self-Etching Primer (13.11 MPa vs 13.04 MPa) [41].
The above differences may be due to the need for manual preparation of the material, as well as the use of different types of lamps and different lengths of polymerization time, as demonstrated in the study by Bayani et al. These authors showed that reducing the light-cure time from 40 seconds to 20 seconds had a significant effect on the strength of the bond between the bracket and the enamel when the Transbond Plus adhesive was used [23].
The obtained shear stress values for the Transbond Plus composite adhesives were 24.16 MPa (T1), 22.51 MPa (T2) and 18.40 MPa (T3), and these values were slightly higher than those for Transbond Supreme LV, namely 21.01 MPa (T1), 20.04 MPa (T2), and 16.29 MPa (T3). Similar values of bond strength were obtained by Yassaei et al after 24 hours of keeping the samples in an aqueous environment for metal (20.03 MPa) and ceramic (22.52 MPa) brackets bonded with tooth enamel using the Transbond XT primer paste [42]. However, the values of bond strength obtained in the same tests when using the GC Fuji Ortho LC material were 6.63 MPa (metal) and 8.69 MPa (ceramics), respectively. The lower bond strength of the resin-modified glass ionomer material compared to standard composite adhesives was also confirmed by some other authors.
Jurišć et al evaluated the bond strength of stainless-steel orthodontic brackets to enamel when resin-reinforced glass ionomer cement (GIC) (Fuji Ortho LC) and composite resin (Transbond XT) were used as the adhesive. These authors showed that the bond strength depends on the method of enamel preparation prior to bracket placement as well as on the type of adhesive. The composite resin showed a higher shear bond strength than GIC [43]. An interesting study was also conducted by Maurya et al, who compared the bond strength of 3 light-cured orthodontic adhesives – a glass ionomer (FujiOrthoLC, GC Orthodontics), a conventional composite resin (Transbond XT, 3M Unitek) and a color-changing composite resin (Transbond Plus, 3M Unitek) – with a conventional etching and self-etching primer (Transbond PlusSEP, 3M Unitek). The highest bond strength was recorded for the conventional light-cured composite resin, and the lowest for the glass ionomer resin adhesive. There was no statistically significant difference between the conventional composite used with a conventional etchant and the color-changing composite resin used with a conventional etchant or self-etching primer [44].
This is probably related to the fact that the adsorption of water in composite materials based on bisphenol A-glycidyl methacrylate (Bis-GMA) and triethylene glycol dimethacrylate (TEGMA) resins is much lower than in the case of materials based on Poly(2-hydroxyethyl methacrylate) (poly-HEMA), such as resin-modified glass ionomer adhesives.
Obviously, the present study has some limitations as well as some strengths. First, the study was performed in vitro, so it was not possible to take into account factors affecting the bond strength, such as the presence of saliva, the temperature inside the oral cavity, or occlusal forces. Therefore, in the next stage it would be reasonable and advisable to conduct further laboratory tests, for example with regard to enamel demineralization after removing the brackets, or cyclical changes in temperature in the 5–35°C range to reproduce the normal conditions in the oral cavity (so-called thermocycling). Second, it would also seem necessary to conduct in vivo studies, including clinical trials, to confirm the results. Third, typical orthodontic treatment lasts more than a year, so it is worth considering extending the observation period. Fourth, we evaluated the bond strength of only one type of bracket to tooth enamel. Therefore, at a later stage, the bond strength of not only stainless-steel brackets but also ceramic brackets should be assessed. However, our study also has a number of strengths. First, the total number of teeth involved, as well as the number of teeth in the individual groups, made it possible, with 1 exception, to use parametric methods in statistical analysis, which have more assumptions to be met, a higher test power, and a more accurate measurement [45]. Second, each of the subgroups was homogeneous, which facilitates the interpretation of the obtained results. Third, the same preparatory procedures were used for all the teeth prior to the placement of the brackets. Fourth, before the brackets were attached, the teeth had been checked for any demineralization of the enamel, which means that homogeneous test conditions were maintained. Finally, this study appears to be ethically neutral as it used bovine teeth obtained from animals routinely raised for meat and not specifically for scientific purposes.
Conclusions
The present study aimed to compare the bond strength of orthodontic brackets to the tooth enamel of 120 freshly extracted adult bovine medial lower incisors using 4 adhesives: a resin-modified glass ionomer adhesive, a composite adhesive, a liquid composite adhesive, and a one-step light-cured adhesive. We showed that the GC Ortho Connect adhesive provides the highest bond strength between metal orthodontic brackets and tooth enamel compared to the other tested adhesive systems, regardless of the observation period. Second, we confirmed that over time, the bond strength between steel orthodontic brackets and tooth enamel decreases for all the tested adhesives. Finally, it can also be concluded that the tested adhesives are safe for clinical use as no cracks or other damage to the enamel were observed on any of the tooth surfaces.
The GC Ortho Connect light-cured adhesive bonds orthodontic brackets to the tooth surface through light polymerization, which allows more time for accurate bracket placement. The observations made in this study and the clinical experience of using GC Ortho Connect indicate that the consistency of GC Ortho Connect prevents the adhesive from leaking and the brackets from sliding, which in turn reduces costs and saves material. The short curing time enables immediate archwire placement, thus reducing visit duration. The use of universal adhesive systems in orthodontic treatment may have a beneficial effect in terms of reducing the number of adhesive systems required in dental surgeries.
Tables
Table 1. Characteristics of the orthodontic adhesive materials used in the current study.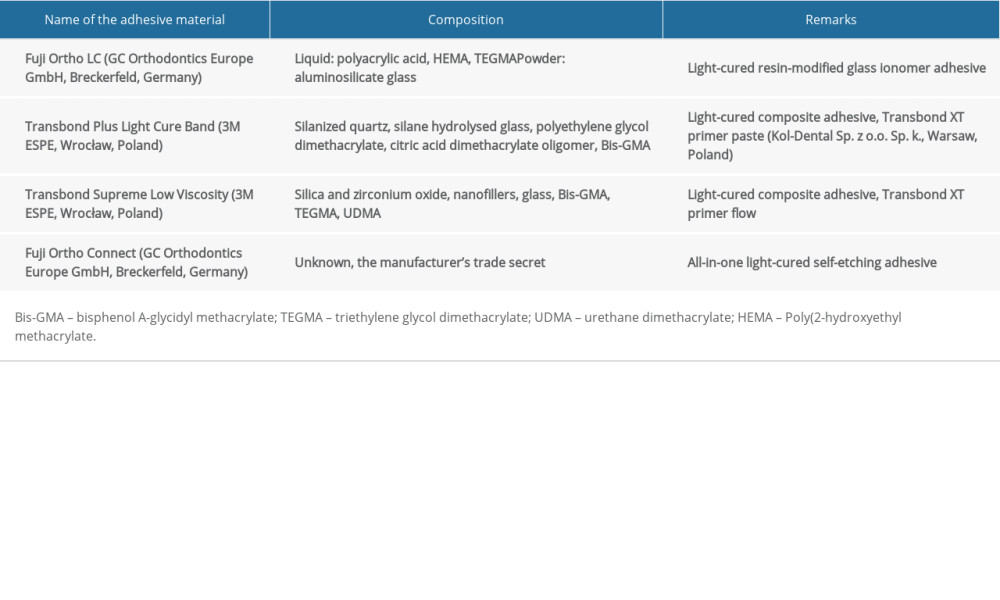 Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.
Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.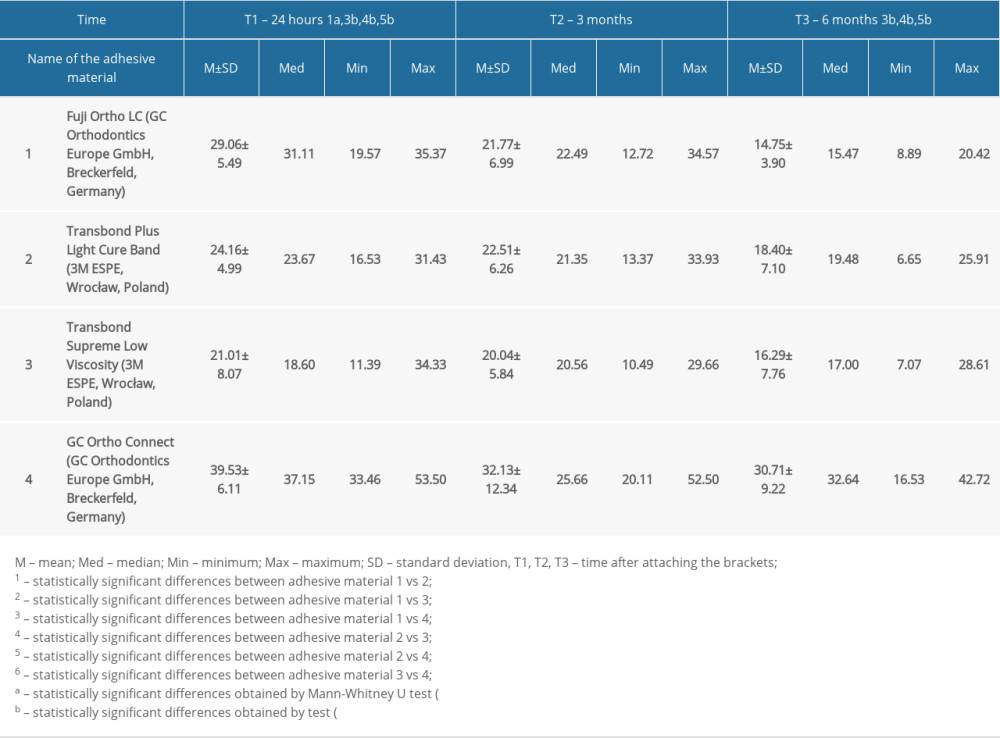 Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation.
Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation.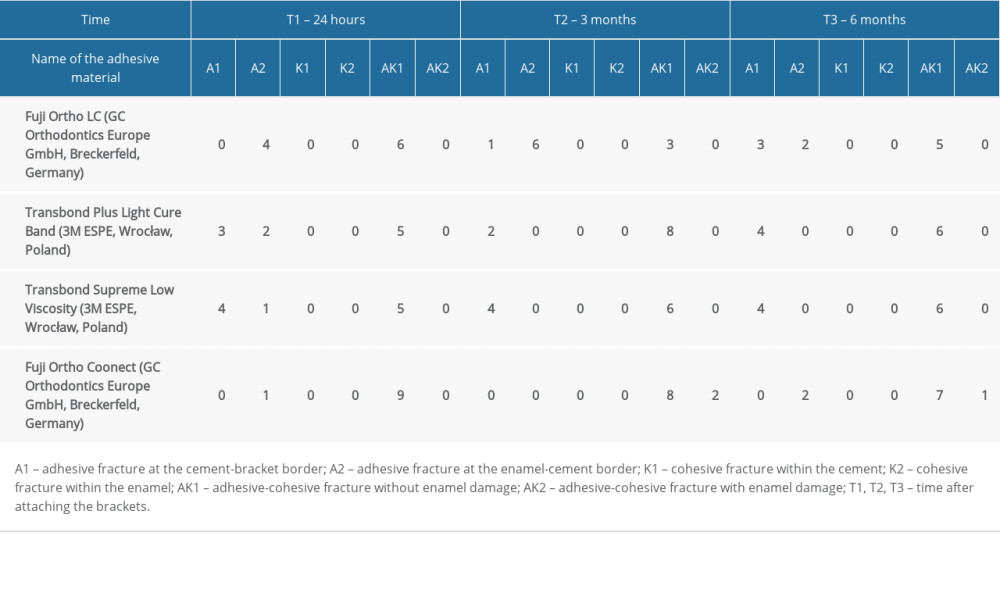
References
1. Chow L, Goonewardene MS, Cook R, Firth MJ, Adult orthodontic retreatment: A survey of patient profiles and original treatment failings: Am J Orthod Dentofac Orthop, 2020; 158(3); 371-82
2. USA DT: Adults are seeking orthodontic treatment in record... Dental Tribune USA Published April 29, 2016
3. Tamer İ, Öztaş E, Marşan G, Orthodontic treatment with clear aligners and the scientific reality behind their marketing: A literature review: Turk J Orthod, 2019; 32(4); 241-46
4. Alnatheer M, Alqerban A, Alhazmi H, Graphene oxide-modified dental adhesive for bonding orthodontic brackets: Int J Adhes Adhes, 2021; 110; 102928
5. Kuśmierczyk D, Małkiewicz K, Orthodontic adhesive systems – over half a century of research and experience: J Stomatol, 2019; 72(4); 179-83
6. Al Shehab A, Bakry AS, Hill R, Evaluation of bioactive glass and low viscosity resin as orthodontic enamel sealer: An in vitro study: J Funct Biomater, 2022; 13(4); 191
7. Soares FZM, Follak A, da Rosa LS, Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies: Dent Mater, 2016; 32(11); 1385-93
8. Bącela J, Łabowska MB, Detyna J, Functional coatings for orthodontic archwires – a review: Mater Basel Switz, 2020; 13(15); E3257
9. ElSherifa MT, Shamaa MS, Montasser MA, Enamel around orthodontic brackets coated with flash-free and conventional adhesives: J Orofac Orthop, 2020; 81(6); 419-26
10. Abbing A, Koretsi V, Eliades T, Papageorgiou SN, Duration of orthodontic treatment with fixed appliances in adolescents and adults: A systematic review with meta-analysis: Prog Orthod, 2020; 21(1); 37
11. Tsichlaki A, Chin SY, Pandis N, Fleming PS, How long does treatment with fixed orthodontic appliances last? A systematic review: Am J Orthod Dentofac, 2016; 149(3); 308-18
12. Groddeck AL, Schwestka-Polly R, Hecker H, Sostmann M, Temperatures in the pulpal cavity during orthodontic bonding using an LED light curing unit : An in vitro pilot study: J Orofac Orthop, 2020; 81(6); 396-406
13. Daneshkazemi P, Sadeghian S, Khodaei M, Shear bond strength of orthodontic brackets on intact and demineralized enamel after application of resin infiltrant, fluoride varnish and casein phosphopeptide-amorphous calcium phosphate remineralizing agents: In-vitro study: Int Orthod, 2021; 19(2); 259-68
14. Contreras ALC, López AM, Arriola-Guillén LE, Effect of different levels of salivary ph on the shear bond strength of two orthodontic adhesive systems for bracket placement: An in-vitro study: J Orofac Sci, 2020; 12(1); 47
15. Lanteri V, Poggi S, Blasi S: International Journal of Clinical Dentistry, 2020; 13(4); 419-47
16. Alzainal AH, Majud AS, Al-Ani AM, Mageet AO, Orthodontic bonding: Review of the literature: Int J Dent, 2020; 2020 8874909
17. Dalaie K, Fatemi SM, Behnaz M, Effect of different debonding techniques on shear bond strength and enamel cracks in simulated clinical set-ups: J World Fed Orthod, 2020; 9(1); 18-24
18. Wang C, Fang Y, Zhang L, Enamel microstructural features of bovine and human incisors: A comparative study: Ann Anat, 2021; 235; 151700
19. Fröhlich TT, Lenzi TL, Soares FZM, de Rocha RO, Bond strength of a universal adhesive system to bovine vs human primary teeth: Int J Adhes Adhes, 2021; 107; 102862
20. : [Uśmiercanie zwierząt w ubojni; ubój domowy] – Art. 34. – Ochrona zwierząt. – Dz.U.2022.572 t.j. – OpenLEX [in Polish]//sip.lex.pl/akty-prawne/dzu-dziennik-ustaw/ochrona-zwierzat-16798854/art-34
21. Kasraei S, Yarmohammadi E, Ghazizadeh MV, Microshear bond strength of OptiBond all-in-one self-adhesive agent to er: YAG laser treated enamel after thermocycling and water storage: J Lasers Med Sci, 2016; 7(3); 152-58
22. El Mourad AM, Assessment of bonding effectiveness of adhesive materials to tooth structure using bond strength test methods: A review of literature: Open Dent J, 2018; 12; 664-78
23. Bayani S, Ghassemi A, Manafi S, Delavarian M, Shear bond strength of orthodontic color-change adhesives with different light-curing times: Dent Res J Isfahan, 2015; 12(3); 265-70
24. Elsaka SE, Influence of surface treatments on bond strength of metal and ceramic brackets to a novel CAD/CAM hybrid ceramic material: Odontology, 2016; 104(1); 68-76
25. Chalipa J, Jalali YF, Gorjizadeh F, Comparison of bond strength of metal and ceramic brackets bonded with conventional and high-power LED light curing units: J Dent Tehran Iran, 2016; 13(6); 423-30
26. de Almeida JX, Deprá MB, Marquezan M, Effects of surface treatment of provisional crowns on the shear bond strength of brackets: Dent Press J Orthod, 2013; 18(4); 29-34
27. Hu B, Hu Y, Li X, Shear bond strength of different bonding agents to orthodontic metal bracket and zirconia: Dent Mater J, 2022; 41(5); 749-56
28. Hellak A, Ebeling J, Schauseil M, Shear bond strength of three orthodontic bonding systems on enamel and restorative materials: BioMed Res Int, 2016; 2016 6307107
29. Ribeiro GLU, Jacob HB, Understanding the basis of space closure in Orthodontics for a more efficient orthodontic treatment: Dent Press J Orthod, 2016; 21(2); 115-25
30. Almosa N, Zafar H, Incidence of orthodontic brackets detachment during orthodontic treatment: A systematic review: Pak J Med Sci, 2018; 34(3); 744-50
31. Mickenautsch S, Yengopal V, Banerjee A, Retention of orthodontic brackets bonded with resin-modified GIC versus composite resin adhesives – a quantitative systematic review of clinical trials: Clin Oral Investig, 2012; 16(1); 1-14
32. Godard M, Deuve B, Lopez I, Shear bond strength of two 2-step etch-and-rinse adhesives when bonding ceramic brackets to bovine enamel: Int Orthod, 2017; 15(3); 388-404
33. Fricker JP, Therapeutic properties of glass-ionomer cements: Their application to orthodontic treatment: Aust Dent J, 2022; 67(1); 12-20
34. Daou C, Akl R, Mati M, Effects of enamel deproteinization with different application times on the shear bond strength of a self-etching primer: An in vitro study: Int Orthod, 2021; 19(3); 505-11
35. Reynolds IR, A review of direct orthodontic bonding: Br J Orthod, 1975; 2(3); 171-78
36. Retief DH, Failure at the dental adhesive-etched enamel interface: J Oral Rehabil, 1974; 1(3); 265-84
37. Knight GM, The benefits and limitations of glass-ionomer cements and their use in contemporary dentistry: Glass-ionomers in dentistry, 2016; 57-79, Springer International Publishing
38. Sidhu SK, Nicholson JW, A review of glass-ionomer cements for clinical dentistry: J Funct Biomater, 2016; 7(3); 16
39. Summers A, Kao E, Gilmore J, Comparison of bond strength between a conventional resin adhesive and a resin-modified glass ionomer adhesive: An in vitro and in vivo study: Am J Orthod Dentofac Orthop, 2004; 126(2); 200-6 quiz 254–55
40. Feizbakhsh M, Aslani F, Gharizadeh N, Heidarizadeh M, Comparison of bracket bond strength to etched and unetched enamel under dry and wet conditions using Fuji Ortho LC glass-ionomer: J Dent Res Dent Clin Dent Prospects, 2017; 11(1); 30-35
41. Bucur SM, Bud A, Gligor A, Observational study regarding two bonding systems and the challenges of their use in orthodontics: An in vitro evaluation: Appl Sci, 2021; 11(15); 7091
42. Yassaei S, Davari A, Goldani Moghadam M, Kamaei A, Comparison of shear bond strength of RMGI and composite resin for orthodontic bracket bonding: J Dent Tehran Iran, 2014; 11(3); 282-89
43. Jurišić S, Jurišić G, Jurić H, Influence of adhesives and methods of enamel pretreatment on the shear bond strength of orthodontic brackets: Acta Stomatol Croat, 2015; 49(4); 269-74
44. Maurya R, Tripathi T, Rai P, New generation of color bonding: A comparative in vitro study: Indian J Dent Res, 2011; 22(5); 733-34
45. , Testy parametryczne a nieparametryczne – opis: Naukowiec.org [in Polish]https://www.naukowiec.org/wiedza/statystyka/testy-parametryczne-vs-nieparametryczne_753.html
Tables
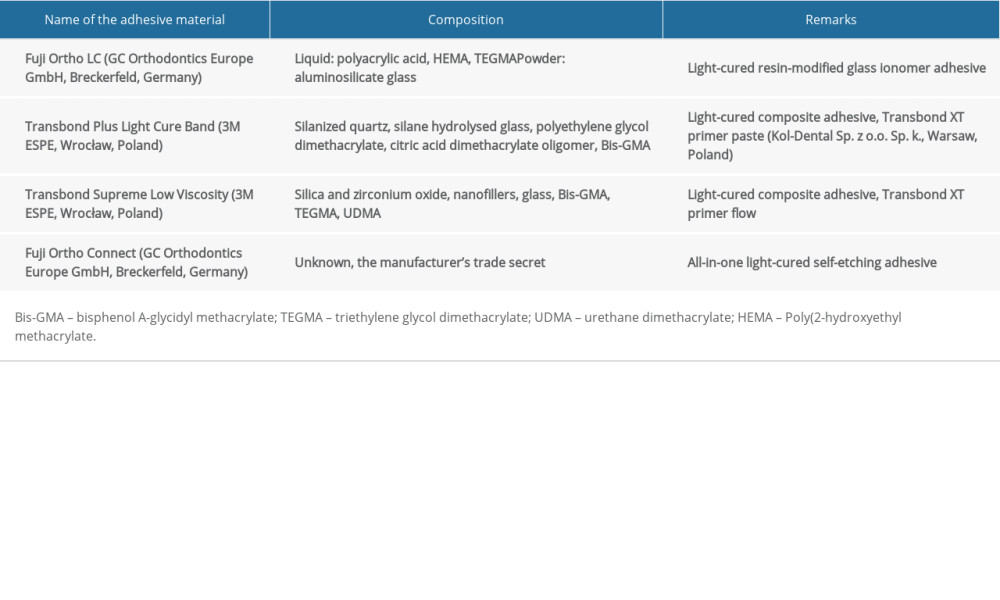 Table 1. Characteristics of the orthodontic adhesive materials used in the current study.
Table 1. Characteristics of the orthodontic adhesive materials used in the current study.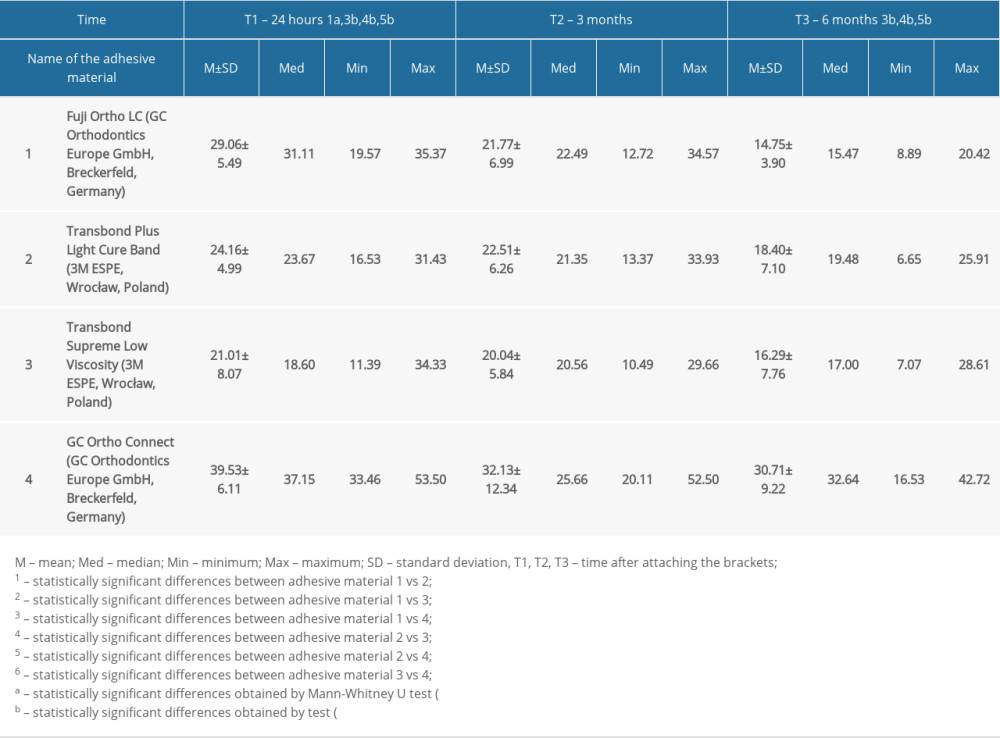 Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.
Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.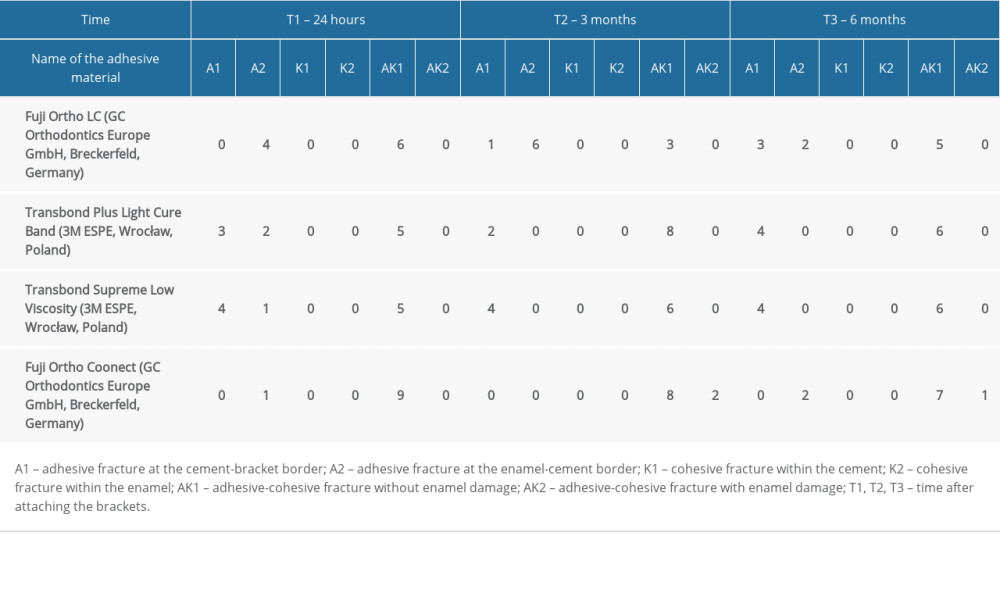 Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation.
Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation.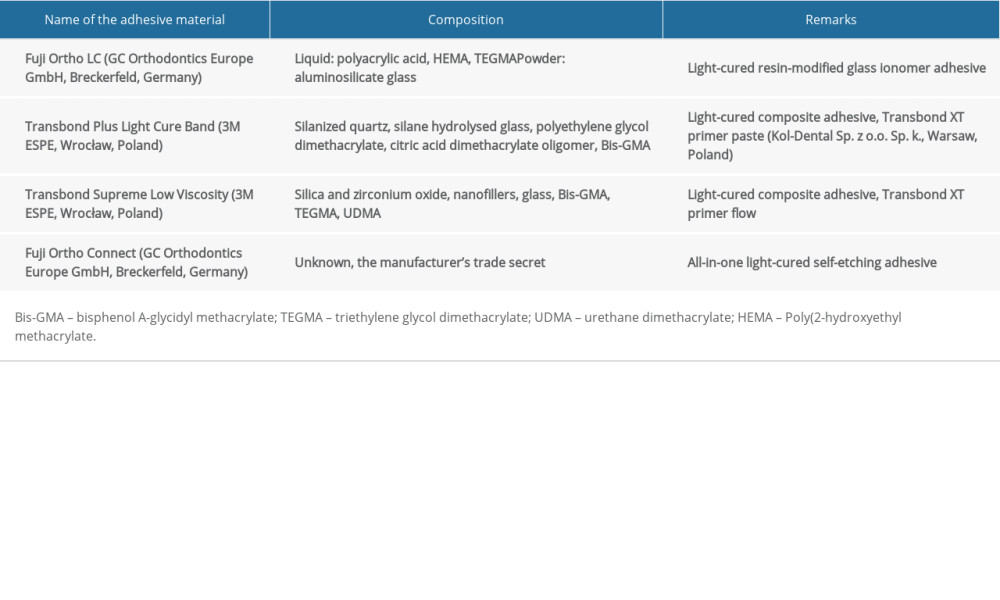 Table 1. Characteristics of the orthodontic adhesive materials used in the current study.
Table 1. Characteristics of the orthodontic adhesive materials used in the current study.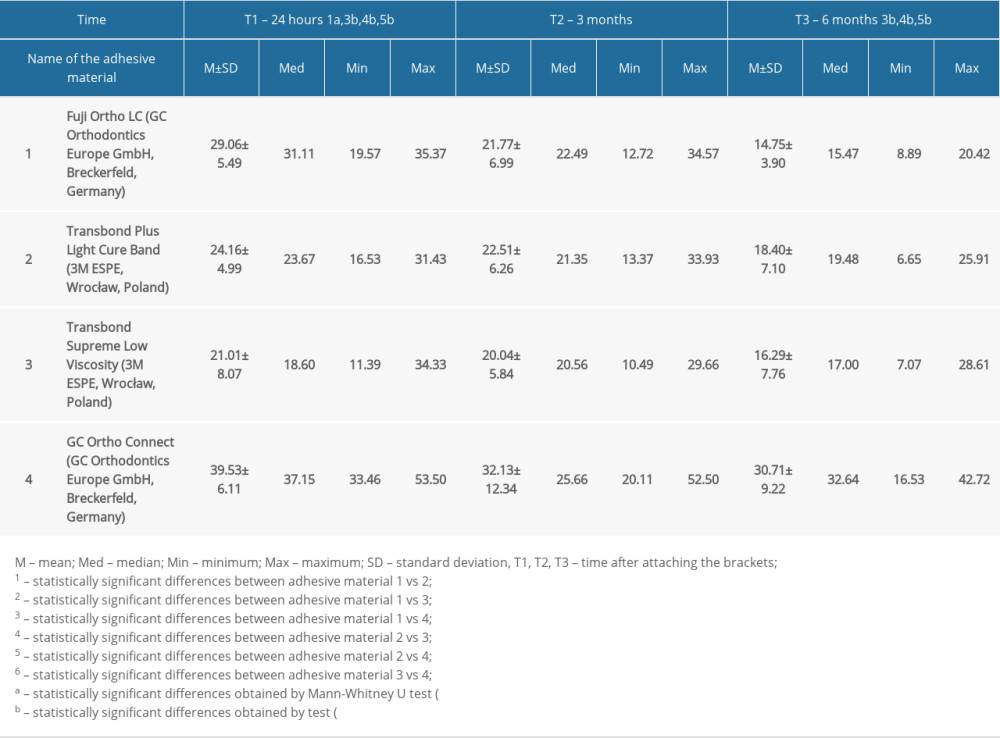 Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.
Table 2. The results of the shear stress examination using 4 different adhesive materials bonding stainless-steel brackets to tooth enamel during 6-month observation.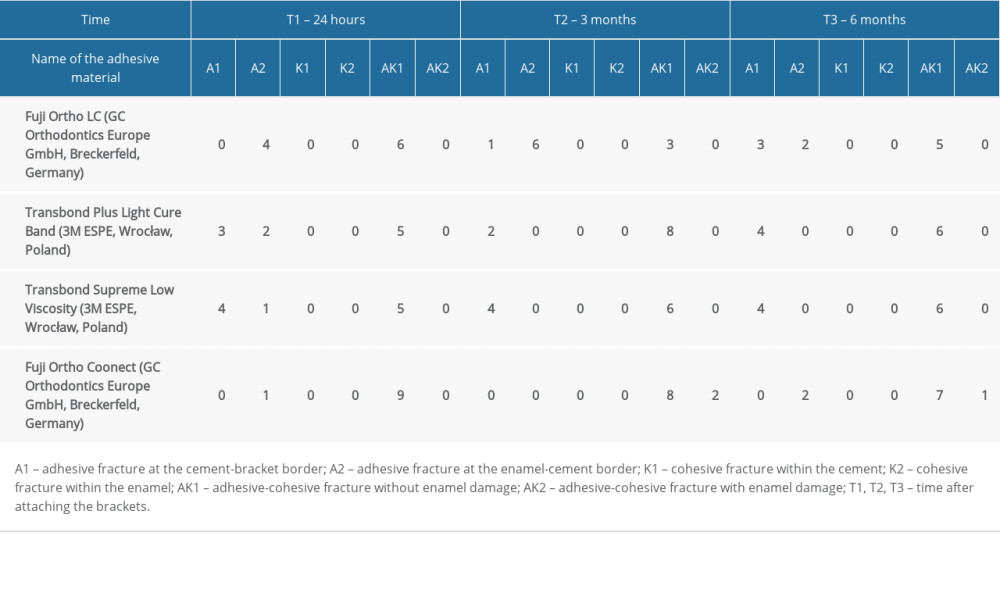 Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation.
Table 3. Characteristics of the types of fractures between steel orthodontic brackets and tooth enamel after a shear test during 6-month observation. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









![Specimen mounting in the testing machine – shear test [own source].](https://jours.isi-science.com/imageXml.php?i=medscimonit-28-e938867-g001.jpg&idArt=938867&w=1000)