19 August 2023: Clinical Research
Concurrent Spinal Trauma in Patients with Traumatic Head Injury: A Seven-Year Retrospective Analysis
Wenye HeDOI: 10.12659/MSM.939215
Med Sci Monit 2023; 29:e939215
Abstract
BACKGROUND: Assessing spinal injuries in patients with traumatic head injuries is crucial due to their potential to alter functionality and increase mortality rates. This single-center retrospective study was conducted to understand the prevalence and characteristics of concurrent spinal injuries in adults with traumatic head injury from April 2015 to April 2022.
MATERIAL AND METHODS: The study incorporated demographic, clinical, traumatological, and hemodynamic data from 1,501 adult patients presenting with traumatic head injuries. Spinal injuries were identified through symptoms, physical signs, and radiological findings.
RESULTS: During the study period, 179 patients (12%) were reported with associated spinal injuries. These patients were predominantly male (p=0.0012), aged 65 years or above (p=0.0452), had thoracic injuries (p=0.0004), and arrived at the emergency department more than three hours post-trauma (p=0.0004). Most injuries were caused by motor vehicle accidents (p=0.0412) or falls from heights greater than 3 meters (p=0.0481). In addition, these patients had higher Abbreviated Injury Scale scores (≥2, p=0.0391), Eppendorf-Cologne Scale scores (≥2, p=0.0412), and lower systolic and diastolic blood pressure readings (p=0.0481, p=0.0412) along with lower heart rates (p=0.0482). However, no correlation was found between systolic and diastolic pressures and age among patients with spinal injuries.
CONCLUSIONS: This study reveals that the prevalence and severity of spinal injuries in patients with traumatic head injuries are influenced not only by demographic and clinical parameters, but also by the degree and extent of head trauma.
Keywords: Abbreviated Injury Scale, Blood Pressure, Craniocerebral Trauma, Emergency Medical Services, Spinal Injuries, Thoracic Injuries, Adult, Humans, Male, Female, Retrospective Studies, Accidents, Traffic
Background
An individual with traumatic head injuries has a high risk of associated spinal injuries [1]. It is necessary to maintain the cervical spinal cord in patients with traumatic head injuries to avoid secondary injuries [2]. According to available studies, 1–2% of individuals with head injuries also have spinal injuries [3]. Unlike other types of accidents, high rates of spinal injuries are reported in individuals involved in motor vehicle accidents [4,5]. Causes of injury may be associated with spinal injuries among individuals with traumatic head injuries [6]. Besides the type of accidents, other epidemiological characteristics like older age and degree of injuries are also associated with the prevalence of spinal injuries among individuals with traumatic head injuries [3]. Detection of spinal injuries among individuals with traumatic head injuries is necessary because spinal injuries lead to functional alterations [7]. Spinal injuries are a global health issue because of the high healthcare cost of treatment [8]. There is a rise in the mortality rate in the Chinese population from 2010 to 2019 among males, elderly people, rural residents, and western and central regions due to accidental injuries [9].
To understand the pattern of risk among traumatic head injury patients by any cause, it is necessary to understand the prevalence and association of several parameters that worsen the conditions [7]. There are several Chinese epidemiological studies [7,10–13] that stressed and discussed spinal injuries and mortality in traumatic brain injuries in the Chinese population. These epidemiological studies [7,10–13] discussed the biological burden of traumatic head injuries when stratified by the cause(s) of injuries (for example, self-harm, accidental injuries, and/or falls). However, the effects of the degree and extent of traumatic head injuries due to any cause of spinal injuries are not established yet. The problem of traumatic head injuries, including the degree and extent of traumatic head injuries and spinal injuries, is not yet addressed by policy-makers and medical researchers in China.
The objective of this retrospective study was to evaluate the prevalence of spinal injuries (based on signs, symptoms, and radiological findings) among patients with traumatic head injuries admitted at the Emergency Department of the institute. Evaluation of independent predictors (patients’ characteristics at the time of admission) for spinal injuries in the admitted patients at the Emergency Department with traumatic head injuries was the secondary objective of the study.
Material and Methods
ETHICS APPROVAL AND CONSENT TO PARTICIPATE:
The designed protocol of the established study (protocol number 14MSOU dated 15 December 2014) was approved by the Human Ethics Committee of the Soochow University. The study follows the law of China and the v2008 Declarations of Helsinki. Informed consent was signed by the legal guardian of the patients at the time of admission for treatment(s), pathology, and publication(s) of data in the form of an article(s) (routine protocol of the institutes).
INCLUSION CRITERIA:
Patients aged 18 years or more admitted at the Emergency Department of the institute with traumatic head injuries due to motor vehicle accident, fall, struck with an object(s), and/or other reason(s) were included in the study.
EXCLUSION CRITERIA:
Patients with incomplete data (key data points or 3 or more missing data points) were excluded from the study.
DEMOGRAPHIC AND CLINICAL PARAMETERS:
Demographic and clinical parameters of admitted patients were collected from patients’ records for analysis.
THE ABBREVIATED INJURY SCALE SCORE: This scale used for the assessment of severities of head injuries. Scores range from 0 to 6—0: no head injuries, 1: minor head injuries, 2: moderate head injuries, 3: severe head injuries but not life-threatening, 4: severe head injuries and life-threatening, 5: critical head injuries and uncertain survival, and 6: unsurvivable head injury [14]. The Abbreviated Injury Scale score was evaluated by traumatologist(s) following emergency treatment by a physician.
MOTOR FUNCTION ASSESSMENT: The Eppendorf-Cologne Scale score was used for the evaluation of motor function. According to pupil reactivity and size, motor function was assessed as 0: normal, 1: specific response, 2: nonspecific or diminished response, and 3: completely absent response [15]. The Eppendorf-Cologne Scale score was determined by traumatologist(s) following emergency treatment by a physician.
SPINAL INJURIES: Patients with spinal injuries have problems with walking, loss of posture control, loss of bladder control and/or bowels, inability to move the arms and/or legs, feelings of tingling in the extremities or spreading numbness, unconsciousness, headache, pain, pressure, and stiffness in the back and/or neck area, signs of shock, and/or unnatural positioning of the head [16]. Magnetic resonance imaging (MRI) and/or other forms of radiological imaging were performed to confirm spinal injuries. Computed tomography scans were used to provide evidence of bleeding in the brain (hemorrhage), blood clots (hematomas), bruised brain tissue (contusions), and brain tissue swelling. The detail view of brain was obtained by MRI.
HEMODYNAMIC PARAMETERS:
Systolic and diastolic blood pressures and heart rates of admitted patients at the time of admission were collected from patients’ records for analysis.
STATISTICAL ANALYSIS:
InStat 3.01 GraphPad Software (San Diego, CA, USA) was used for statistical analysis purposes. The Fisher exact test or chi-square test (χ2 test) was used for statistical analysis of categorical data. The Kolmogorov-Smirnov test was used to check the linearity of continuous and ordinal data. The unpaired t test was used to assess linear data and the Mann-Whitney test for non-linear data was used for continuous and ordinal data. Multivariable regression analysis following univariate analysis was performed to evaluate the association of spinal injuries with the demographic and clinical parameters of patients [17]. Spearman rank correlation was used to assess the association between the age and blood pressure of patients. All results were considered significant if the P value was less than 0.05.
Results
STUDY POPULATION:
From 15 April 2015 to 1 April 2022, a total of 1858 patients with traumatic head injuries were admitted to the Emergency Department of the First Affiliated Hospital of the Soochow University, Suzhou, Jiangsu, China, and the referring institute. Among them, 357 patients had incomplete data; therefore, data from these patients were excluded from the analysis. Demographic, clinical, traumatological, and hemodynamic parameters and the presence or absence of spinal injuries (as per signs, symptoms, and radiological findings) of a total of 1501 patients with traumatic head injuries were included in the analysis. The summary chart of the study is presented in Figure 1.
PREVALENCE OF SPINAL INJURIES:
As per signs, symptoms, and radiological findings in the followed-up period, a total of 179 (12%) patients were reported to have spinal injuries in the follow-up period.
DEMOGRAPHIC AND CLINICAL PARAMETERS:
Among 1501 patients, 639 (43%) males and 862 (57%) females were admitted to the Emergency Department of the institute. More males than females had spinal injuries in the follow-up period (P<0.0001, Fisher exact test). Admitted patients were 18–71 years of age. Patients with spinal injuries were more likely to be unconscious (P<0.0001, Fisher exact test) and older (P<0.0001, Mann-Whitney test, Figure 2) than patients without spinal injuries. Ethnicity and location were comparable among traumatically injured patients with and without spinal injuries. The details of the demographic and clinical parameters of the enrolled patients at the time of admission to the Emergency Department are reported in Table 1.
TRAUMATOLOGICAL PARAMETERS OF HEAD INJURIES:
Within 7 h of traumatic injuries, all patients were admitted to the Emergency Department. Patients who had longer time from traumatic injury to admission to the Emergency Department were more likely to have spinal injuries (P<0.0001, Mann-Whitney test, Figure 3). Patients with spinal injuries were more likely to have experienced a motor vehicle accident (P<0.0001, Fisher exact test) or falling >3 m (P<0.0001, Fisher exact test) than those who had no spinal injuries. Abbreviated Injury Scale score, Eppendorf-Cologne Scale score, and numbers of patients with thoracic injuries were higher among patients with spinal injuries than in those without spinal injuries. The details of the traumatological parameters of the enrolled patients at the time of admission to the Emergency Department are reported in Table 2.
HEMODYNAMIC PARAMETERS:
All patients without spinal injuries had systolic blood pressure 162 mmHg or less and diastolic blood pressure 120 mmHg or less. All patients with spinal injuries had 130 mmHg or less of systolic blood pressure and less than 90 mmHg of diastolic blood pressure at the time of hospital admission. Systolic blood pressure (Figure 4A), diastolic blood pressure (Figure 4B), and heart rate (Figure 5) were lower among patients with spinal injuries than those of patients without spinal injuries (P<0.05, Mann-Whitney test, for all). The details of the hemodynamic parameters of the enrolled patients at the time of admission to the Emergency Department are reported in Table 3.
ASSOCIATION OF SPINAL INJURIES WITH DEMOGRAPHIC AND CLINICAL PARAMETERS:
Patients with spinal injuries were more likely to be male (P=0.0012, multivariable regression analysis), ≥65 years of age (P=0.0452, multivariable regression analysis), had a thoracic injury (P=0.0004, multivariable regression analysis), time from traumatic injuries before admission in Emergency Department >3 h (P=0.0004, multivariable regression analysis), had motor vehicle accident (P=0.0412, multivariable regression analysis), falls from >3 m (P=0.0481, multivariable regression analysis), Abbreviated Injury Scale score ≥2 (P=0.0391, multivariable regression analysis), Eppendorf-Cologne Scale score ≥2 (P=0.0412, multivariable regression analysis), lower systolic blood pressure (P=0.0481, multivariable regression analysis), lower diastolic blood pressure (P=0.0412, multivariable regression analysis), and lower heart rate (P=0.0482, multivariable regression analysis). The details of the association of spinal injuries with demographic and clinical parameters are reported in Table 4.
CORRELATION BETWEEN AGE AND BLOOD PRESSURE:
Among patients without spinal injuries, systolic (
Discussion
The prevalence of spinal injuries was 12% among patients with head injuries. The results of the prevalence of spinal injuries in the current study are in line with that of a Hong Kong study [11] and a retrospective study [18]. However, the results of the prevalence of spinal injuries were not in line with that of a retrospective study [3] and an ecological study [7]. The reason for contradictory results is that the retrospective study [3] evaluated spinal injuries according to the Abbreviated Injury Scale, but the current study has evaluated spinal injuries according to signs, symptoms, and radiological parameters. The reason for contradictory results is that the ecological study [7] had a large sample size, leading to lower prevalence. Every 8th person admitted at the Emergency Department of the institute with head injuries also had spinal injuries.
Compared with females, males had a high risk of spinal injuries if they had head injuries. The results of gender variances among patients with head injuries in the current study are in line with an ecological study [7] and retrospective studies on the Chinese population [13,19–22] and the German population [3] but not in line with a retrospective study on the Taiwanese population [23]. Generally, in China males are more likely to be engaged in hazardous work than females [13]. The main labor force of mainland China is males [22]. Chinese males with traumatic head injuries may have a higher chance of spinal injuries.
Patients with traumatic head injuries and more than 65 years of age more likely to have spinal injuries. The results of age variances among patients with traumatic head injuries in the current study are in line with a retrospective study on the Chinese population [3,7,13,24]. Patients aged 65 years or more with head injuries have a higher chance of spinal injuries due to age-related osteoporosis [13]. Also, the population age 65 years or more is higher in China now [22], and injuries from falling are more common among people 65 years or more age [22] and those with traumatic head injuries are more likely to also have spinal injuries than are younger people.
Patients who had traumatic thoracic injuries are likely to also have spinal injuries. The results of the association of traumatic thoracic injuries and spinal injuries of the current study are in line with that of the available study on the Hong Kong population [11] and a retrospective study [23]. Patients with traumatic thoracic injuries may provide early signs of spinal injuries among patients who experienced trauma.
Spinal injuries were more common among people who arrived at the Emergency Department more than 3 h after the trauma event. Tranexamic acid treatment initiated within 3 h from traumatic injuries leads to positive outcomes, especially in those with mild-to-moderate head injuries [17]. Early admission of patients with traumatic head injuries is associated with better outcomes of traumatology interventions.
Patients with traumatic head injuries due to motor vehicle accidents and falls from more than 3 m are likely to also have spinal injuries. The reason(s) for traumatic injuries in the current study are in line with that of retrospective studies [3,7,13,19–21]. Motor vehicle accidents among younger people and falls from more than 3 m among older people are common causes of traumatic head injuries [7]. Careless driving, driving while impaired by alcohol [25], and driving motorcycles without helmets [7] are leading causes of spinal injuries in traumatic accidents. Patients with traumatic head injuries during motor vehicle accident and falls from more than 3 m are required to be checked for spinal injuries.
Abbreviated Injury Scale score and Eppendorf-Cologne Scale score 2 or more were associated with spinal injuries. Moderate and/or higher head injuries are always responsible for spinal injuries. The results of the association of the effects of the degree and extent of head injuries with spinal injuries of the current study are in line with retrospective studies [3,23]. The degree and extent of traumatic head injuries are required to evaluate spinal injuries in patients with head injuries.
All patients with spinal injuries had ≤89/130 mmHg blood pressure at the time of Emergency Department admission. The blood pressure results of the patients in the current study were in line with that of available studies on the Hong Kong population [11], retrospective studies [3,23], and a prospective observational study [26]. The traumatic head injury causes degeneration of the white matter of the spinal cord, leading to hypotension in cases of spinal injuries [27]. Hypotension is a general body response after traumatic head injuries in cases of spinal injuries. However, there is no information on the impact of any prehospital interventions on the variables taken at the time of Emergency Department admission and analyzed in this study. These include things like the effect of sedation and intubation on clinical scores, and the administration of fluids that can change hemodynamics.
Systolic and diastolic blood pressures of patients with traumatic head injuries with spinal injuries were not associated with the age of patients. Systolic and diastolic blood pressures of patients with traumatic head injuries without spinal injuries were associated with the age of patients. Systolic and diastolic blood pressures of individuals increase with age in normal condition(s) [28]. A decrease in blood pressure in patients with traumatic head injuries could be a sign of spinal injuries, but spinal injuries do not all present with hypotension. If there are no cervical or high thoracic spinal cord injuries, spinal shock is not usually presented, and mild compression fracture of the vertebral body does not usually lead to neurogenic or spinal shock.
Eppendorf-Cologne Scale score was used for the evaluation of motor function assessments. In addition, the Abbreviated Injury Scale score was used for the assessment of severities of head injuries. The Eppendorf-Cologne Scale is not well-known, as most neurologists use the Glasgow Coma Score. The Eppendorf-Cologne Scale is more simple and reliable than the Glasgow Coma Score [15]. The Abbreviated Injury Scale is an anatomically-based injury severity scoring system to classify each injury by body region using a 6-point scale. The Abbreviated Injury Scale is the system used to determine the Injury Severity Score in multiply injured patients.
Limitations of the present study include its retrospective design, and the fact that hypotension and hypoxia conditions of patients in follow-up were not evaluated. Unlike an ecological study [7], our study failed to show location-related variance among patients with traumatic head injuries, possibly because hospital emergency facilities are also available in rural and suburban areas of China. Another potential limitation is that the study only included admitted patients and did not include patients that died at the scene of the accident or en route to the hospital, which may have skewed the severity results. The population size was relatively small to analyze the characteristics of the study. Lumbar injury differs from cervical and thoracic spine injury in neurology and hemodynamics. Furthermore, it was unclear if patients had spinal cord injury or combined hypovolemic shock from the trunk (solid organs).
Conclusions
Every 8th person who was admitted to the Emergency Department of the institute with traumatic head injuries had spinal injuries. Male gender, age 65 years or more, thoracic injuries, prolonged time (>3 h) from traumatic injuries before admission in the Emergency Department, motor vehicle accident, falls from >3 m, Abbreviated Injury Scale score ≥2, Eppendorf-Cologne Scale score ≥2, and lower blood pressures were independent predictors for spinal injuries among patients with head injuries. The study provides meaningful data for early management when patients are admitted to the Emergency Department of the hospital in the Jiangsu area of China due to traumatic head injuries.
Figures
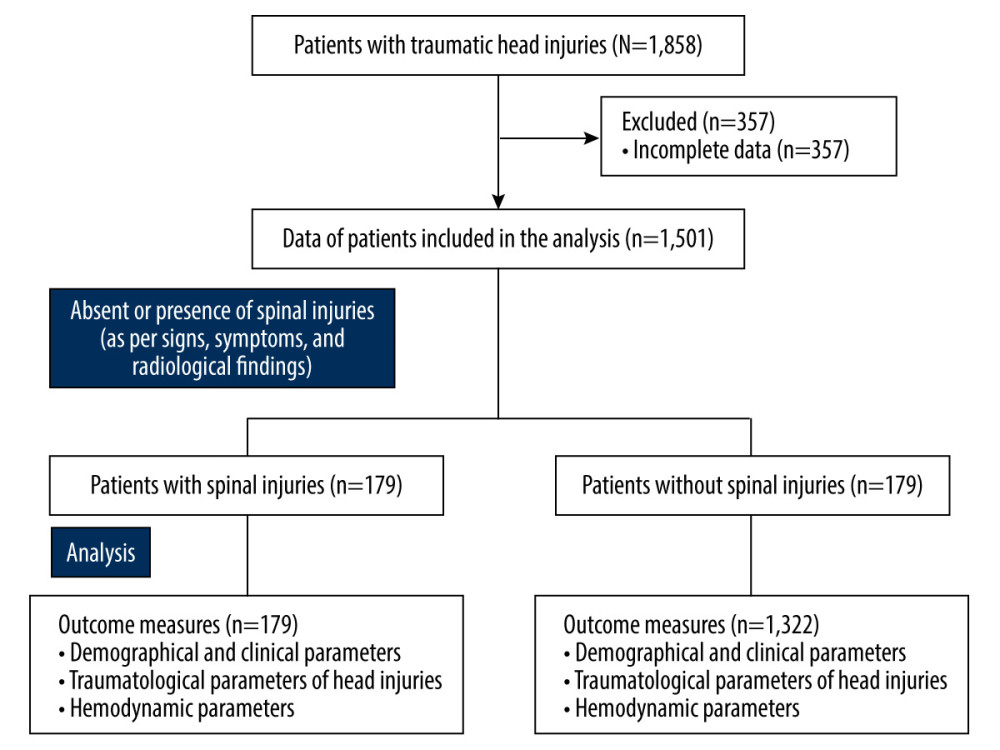 Figure 1. The summary chart of the study.
Figure 1. The summary chart of the study. 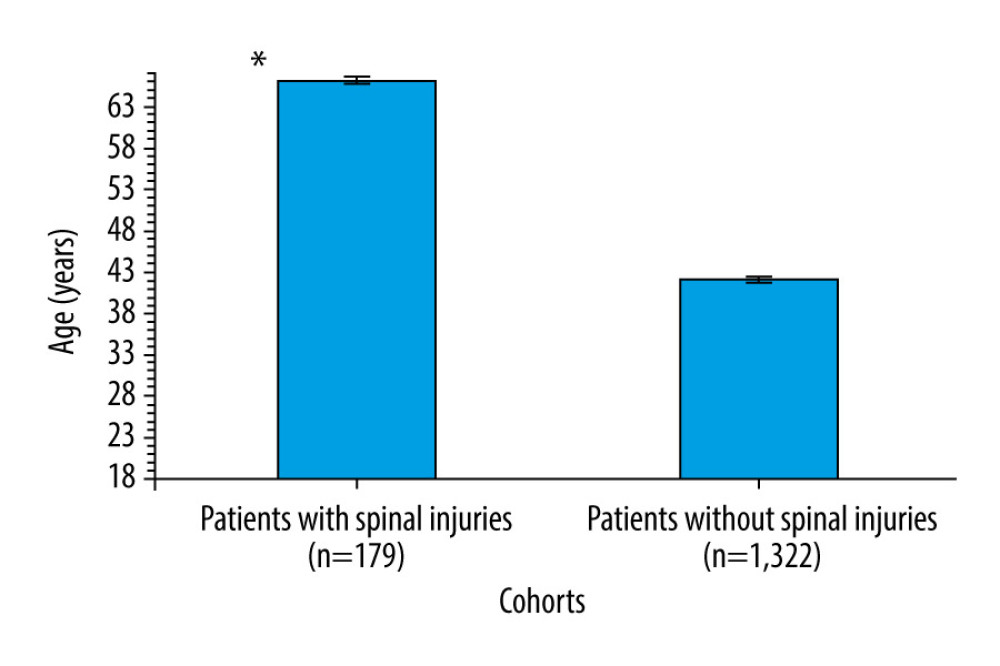 Figure 2. Distribution of age among patients with traumatic head injuries. Data presented as mean±standard error of the mean. * Higher age than those of patients without spinal injuries.
Figure 2. Distribution of age among patients with traumatic head injuries. Data presented as mean±standard error of the mean. * Higher age than those of patients without spinal injuries. 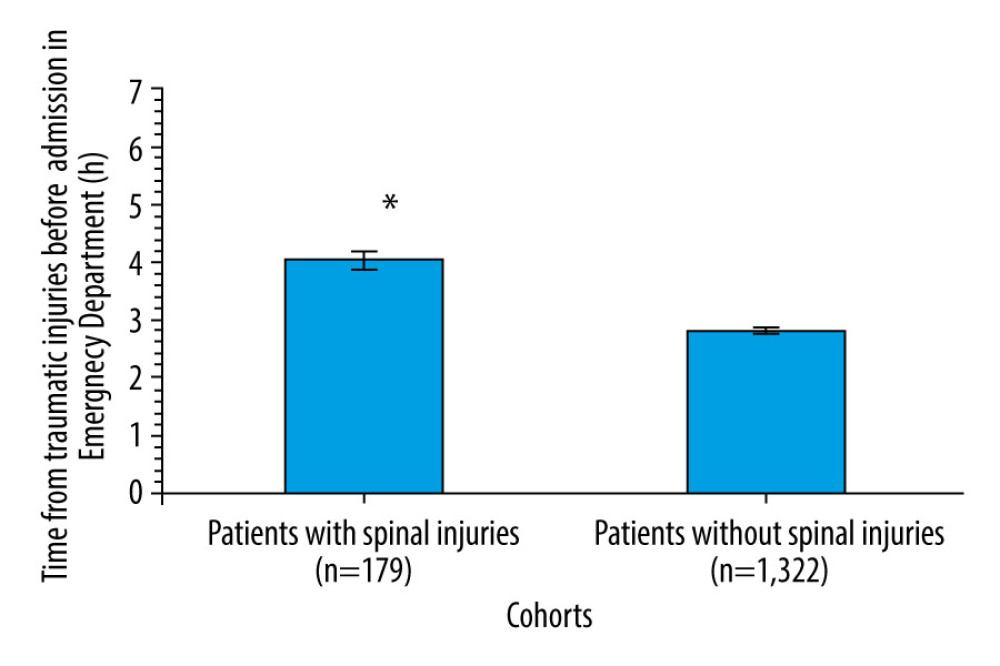 Figure 3. Time from traumatic injuries to admission to the Emergency Department among patients. Data presented as mean±standard error of the mean. * Higher time than those of patients without spinal injuries.
Figure 3. Time from traumatic injuries to admission to the Emergency Department among patients. Data presented as mean±standard error of the mean. * Higher time than those of patients without spinal injuries. 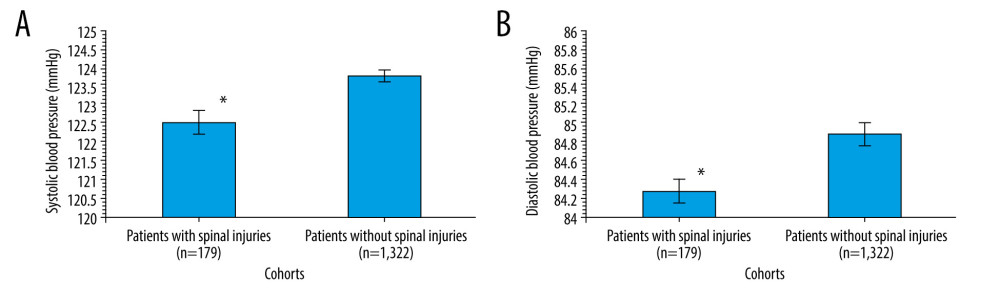 Figure 4. (A) Systolic blood pressure among patients. (B) Diastolic blood pressure among patients. Data presented as mean±standard error of the mean. * Lower blood pressure than those of patients without spinal injuries.
Figure 4. (A) Systolic blood pressure among patients. (B) Diastolic blood pressure among patients. Data presented as mean±standard error of the mean. * Lower blood pressure than those of patients without spinal injuries. 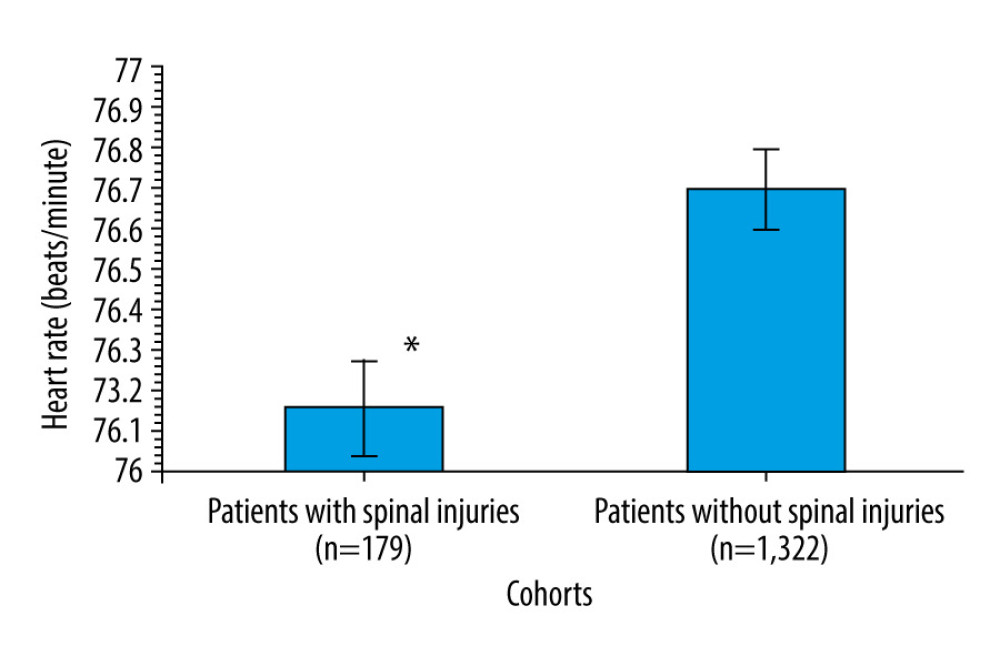 Figure 5. Distribution of heartbeats among patients. Data presented as mean±standard error of the mean. * Lower heartbeats than those of patients without spinal injuries.
Figure 5. Distribution of heartbeats among patients. Data presented as mean±standard error of the mean. * Lower heartbeats than those of patients without spinal injuries. Tables
Table 1. Demographical and clinical parameters of the enrolled patients at the time of admission in the Emergency Department.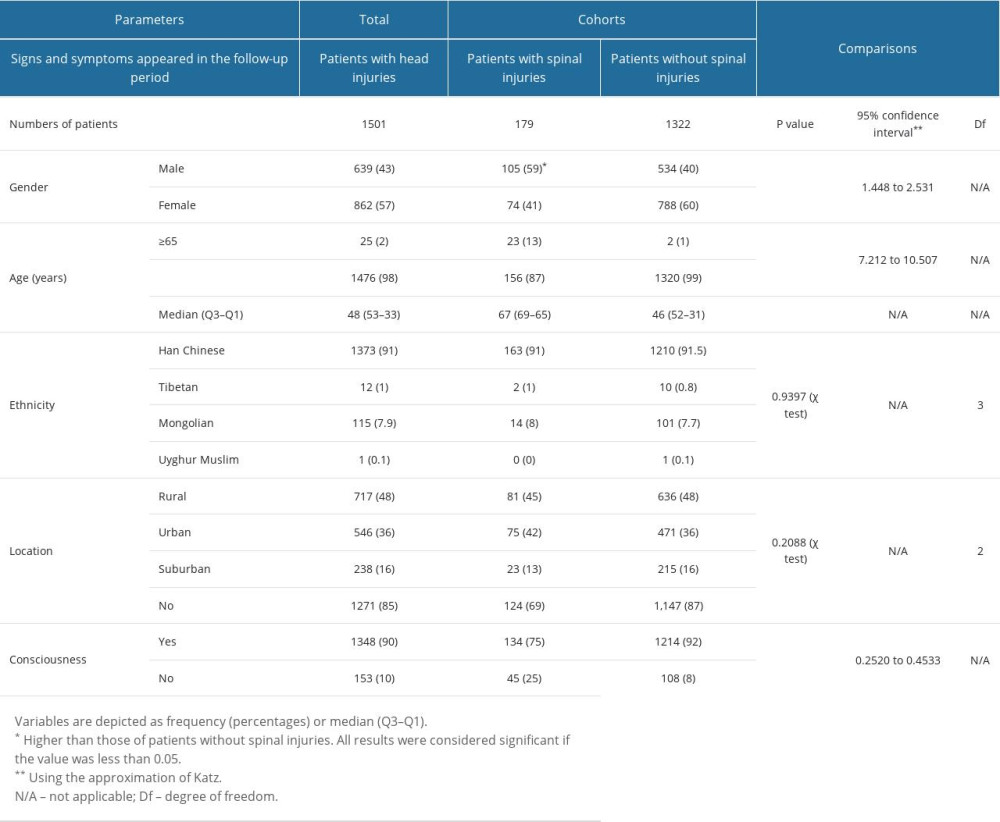 Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.
Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.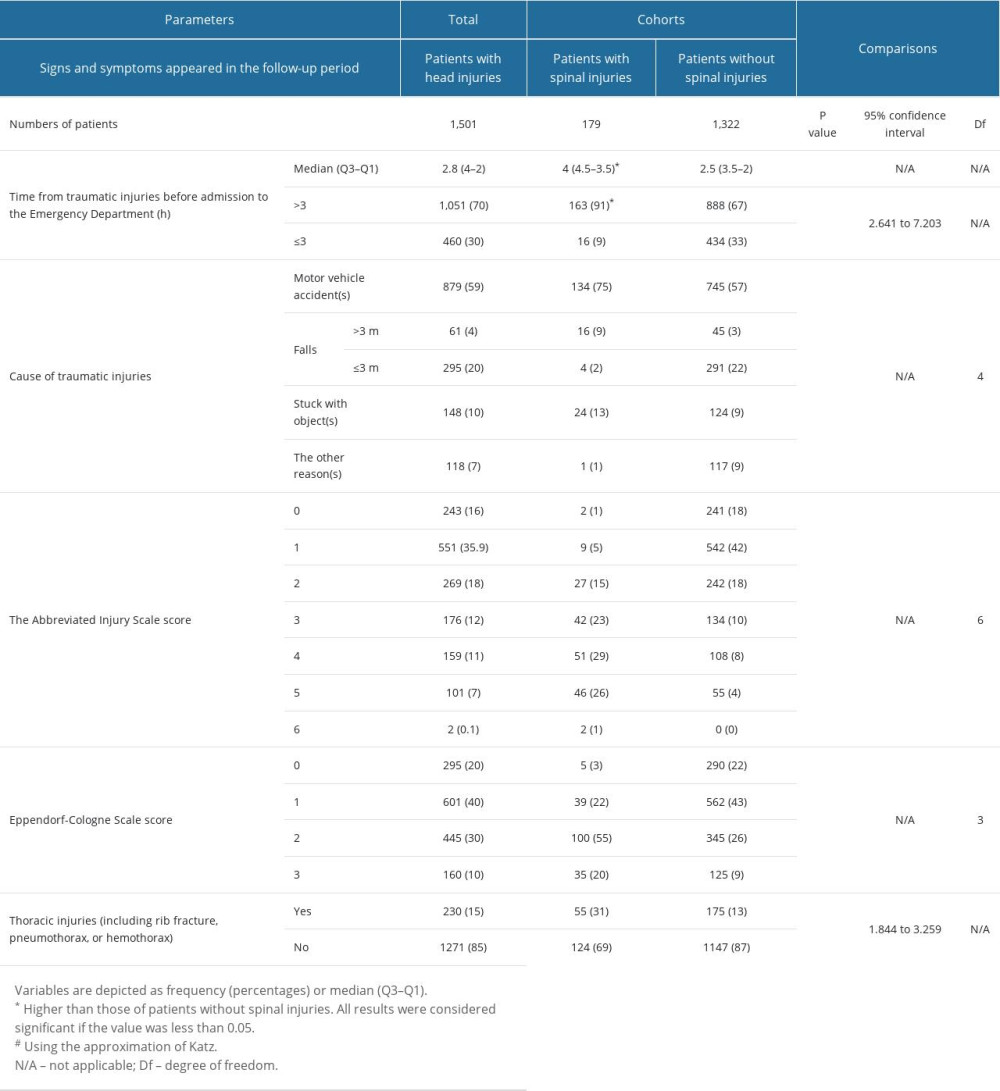 Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.
Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.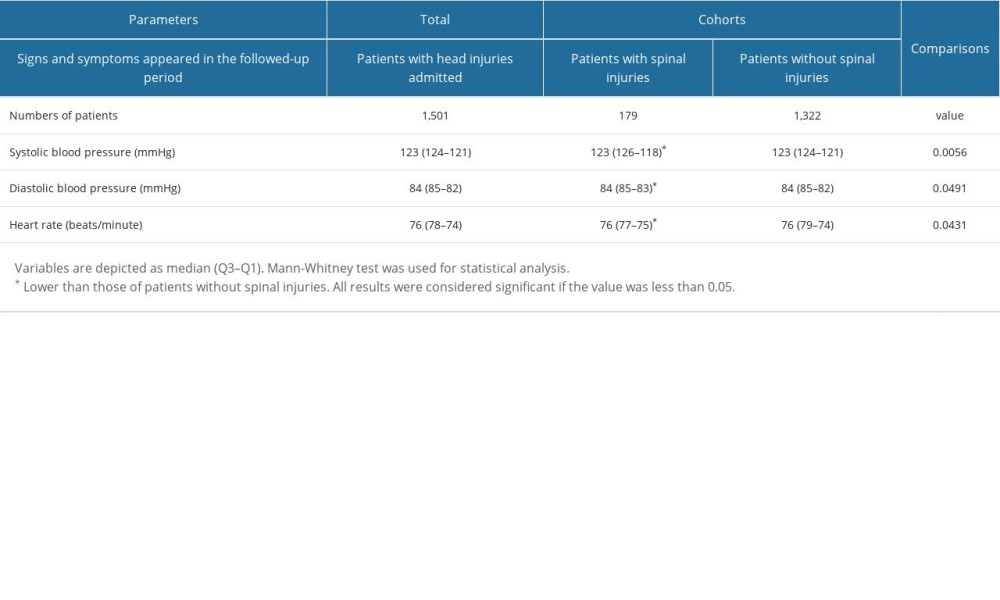 Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters.
Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters.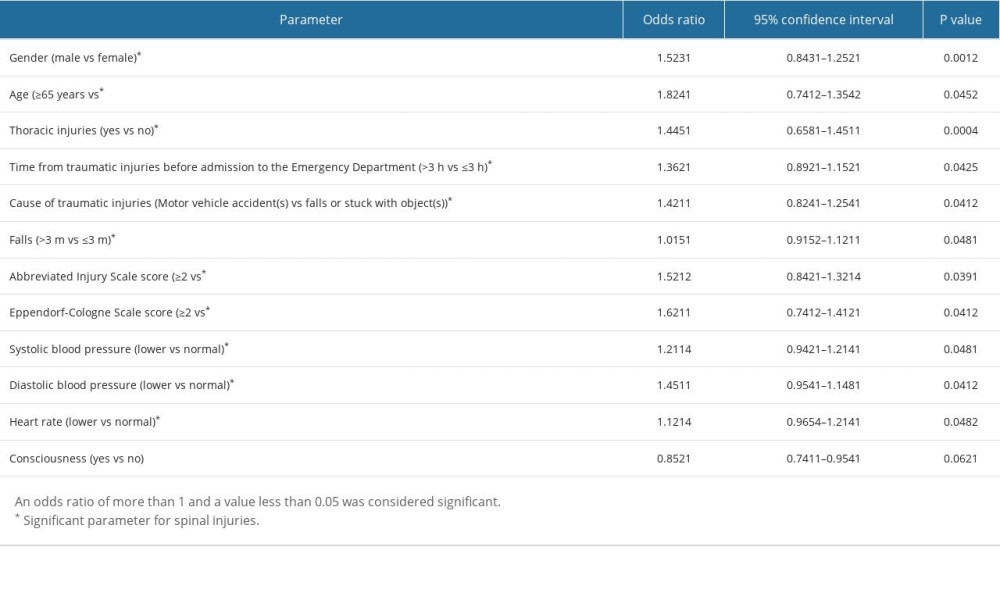
References
1. Eskesen TG, Baekgaard JS, Peponis T, Cervical spinal cord injury after blunt assault: Just a pain in the neck?: Am J Surg, 2019; 217(4); 648-52
2. Como JJ, Diaz JJ, Dunham CM, Practice management guidelines for identification of cervical spine injuries following trauma: Update from the Eastern Association for the Surgery of Trauma Practice Management Guidelines Committee: J Trauma, 2009; 67(3); 651-59
3. Häske D, Lefering R, Stock JP, Kreinest M, TraumaRegister DGU, Epidemiology and predictors of traumatic spine injury in severely injured patients: Implications for emergency procedures: Eur J Trauma Emerg Surg, 2022; 48(3); 1975-83
4. Derakhshanrad N, Yekaninejad MS, Vosoughi F, Epidemiological study of traumatic spinal cord injuries: Experience from a specialized spine center in Iran: Spinal Cord, 2016; 54(10); 901-7
5. Young AJ, Wolfe L, Tinkoff G, Duane TM, Assessing incidence and risk factors of cervical spine injury in blunt trauma patients using the national trauma data bank: Am Surg, 2015; 81(9); 879-83
6. Polytrauma Guideline Update Group, Level 3 guideline on the treatment of patients with severe/multiple injuries: AWMF Register-Nr. 012/019: Eur J Trauma Emerg Surg, 2018; 44(Suppl 1); 3-271
7. Zheng XY, Yi Q, Xu XJ, Trends and external causes of traumatic brain injury and spinal cord injury mortality in south China, 2014–2018: An ecological study: BMC Public Health, 2021; 21(1); 2225
8. Te Ao B, Brown P, Cost of traumatic brain injury in New Zealand: Evidence from a population-based study: Neurology, 2014; 83(18); 1645-52
9. Zhang MG, Zhou YB, Li CCLevels and trends of significant injury-caused deaths in the Chinese population, 2010–2019: Zhonghua Liu Xing Bing Xue Za Zhi, 2022; 43(6); 871-77 [in Chinese]
10. Kamal VK, Agrawal D, Pandey RM, Epidemiology, clinical characteristics and outcomes of traumatic brain injury: Evidences from integrated level 1 trauma center in India: J Neurosci Rural Pract, 2016; 7(4); 515-25
11. Chan DYC, He OY, Poon WS, Univariate and multivariable analyses on independent predictors for cervical spinal injury in patients with head injury: World Neurosurg, 2022; 166; e832-e40
12. Zhang Y, Qiu J, Zhou J, Epidemiological study of traffic accidents-related traumatic brain injury in 159,242 cases: Chin J Trauma, 2014; 30(12); 1215-18
13. Chen J, Chen Z, Zhang K, Epidemiological features of traumatic spinal cord injury in Guangdong Province, China: J Spinal Cord Med, 2021; 44(2); 276-81
14. Association for the Advancement of Automotive Medicine: Abbreviated Injury Scale (AIS) – overview, 2019 Available from: https://www.aaam.org/abbreviated-injury-scale-ais/
15. Hoffmann M, Lehmann W, Rueger JM, Lefering RTrauma Registry of the German Society for Trauma Surgery, Introduction of a novel trauma score: J Trauma Acute Care Surg, 2012; 73(6); 1607-13
16. Kuris EO, McDonald CL, Palumbo MA, Daniels AH, Evaluation and management of cauda equina syndrome: Am J Med, 2021; 134(12); 1483-89
17. Han F, Wang Y, Ling W, Sun Z, Effectiveness and safety of early tranexamic acid in patients with acute traumatic brain injuries: Int J Pharmacol, 2022; 18; 292-98
18. Vehviläinen J, Brinck T, Lindfors M, Occurrence and prognostic effect of cervical spine injuries and cervical artery injuries with concomitant severe head injury: Acta Neurochir, 2020; 162(6); 1445-53
19. Feng HY, Ning GZ, Feng SQ, Epidemiological profile of 239 traumatic spinal cord injury cases over a period of 12 years in Tianjin, China: J Spinal Cord Med, 2011; 34(4); 388-94
20. Yang R, Guo L, Huang L, Epidemiological characteristics of traumatic spinal cord injury in Guangdong, China: Spine, 2017; 42(9); E555-61
21. Zhou Y, Wang XB, Kan SL, Traumatic spinal cord injury in Tianjin, China: A single-center report of 354 cases: Spinal Cord, 2016; 54(9); 670-74
22. Liu J, Liu HW, Gao F, Li J, Li JJ, Epidemiological features of traumatic spinal cord injury in Beijing, China: J Spinal Cord Med, 2022; 45(2); 214-20
23. Kou HW, Liao CH, Huang JF, Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center: Eur J Trauma Emerg Surg, 2019; 45(6); 973-78
24. Liu P, Yao Y, Liu MY, Spinal trauma in mainland China from 2001 to 2007: An epidemiological study based on a nationwide database: Spine, 2012; 37(15); 1310-15
25. Kessaram T, McKenzie J, Girin N, Alcohol use in the Pacific region: Results from the STEPwise approach to surveillance, global school-based student health survey and youth risk behavior surveillance system: Drug Alcohol Rev, 2016; 35(4); 412-23
26. Sharwood LN, Joseph A, Guo C, Heterogeneous emergency department management of published recommendation defined hypotension in patients with acute traumatic spinal cord injury: A multi-centre overview: Emerg Med Australas, 2019; 31(6); 967-73
27. Biering-Sørensen F, Biering-Sørensen T, Liu N, Alterations in cardiac autonomic control in spinal cord injury: Auton Neurosci, 2018; 209; 4-18
28. Niss O, Quinn CT, Lane A, Cardiomyopathy with restrictive physiology in sickle cell disease: JACC Cardiovasc Imaging, 2016; 9(3); 243-52
Figures
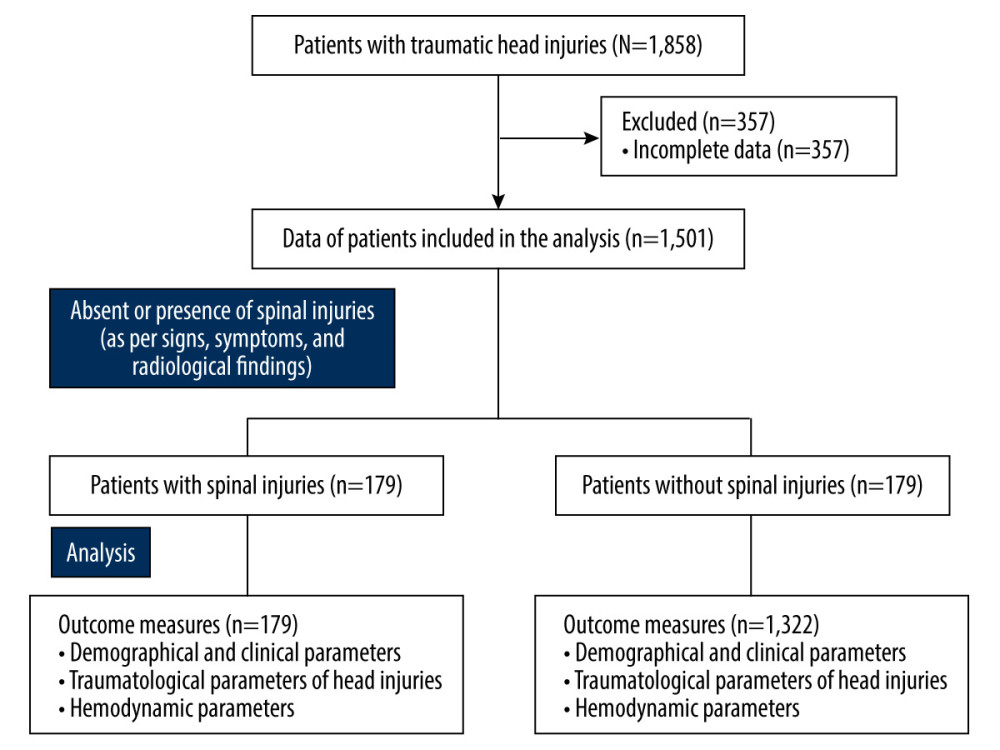 Figure 1. The summary chart of the study.
Figure 1. The summary chart of the study.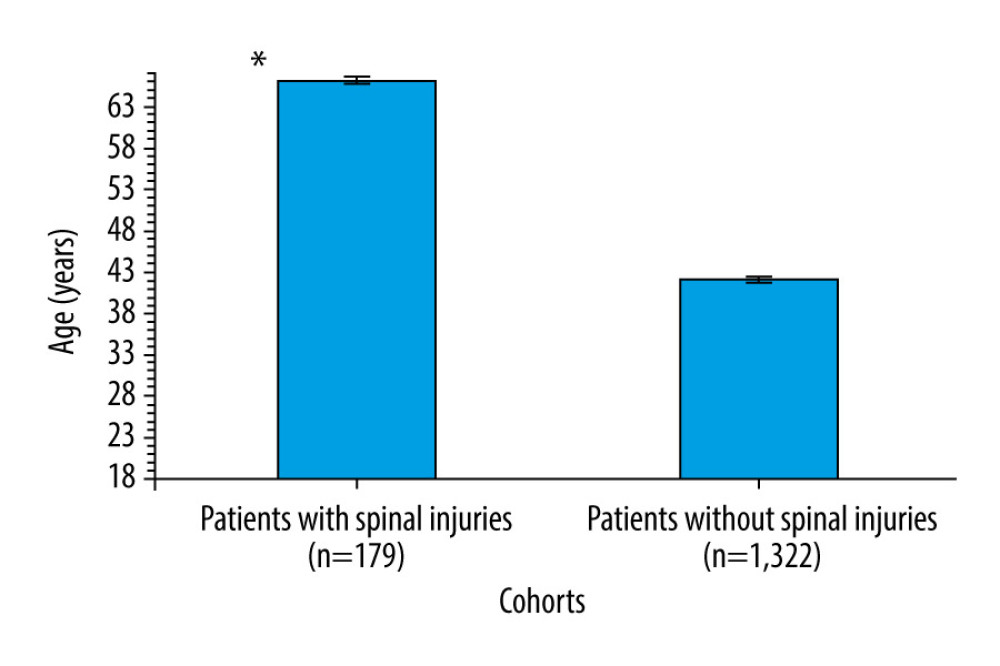 Figure 2. Distribution of age among patients with traumatic head injuries. Data presented as mean±standard error of the mean. * Higher age than those of patients without spinal injuries.
Figure 2. Distribution of age among patients with traumatic head injuries. Data presented as mean±standard error of the mean. * Higher age than those of patients without spinal injuries.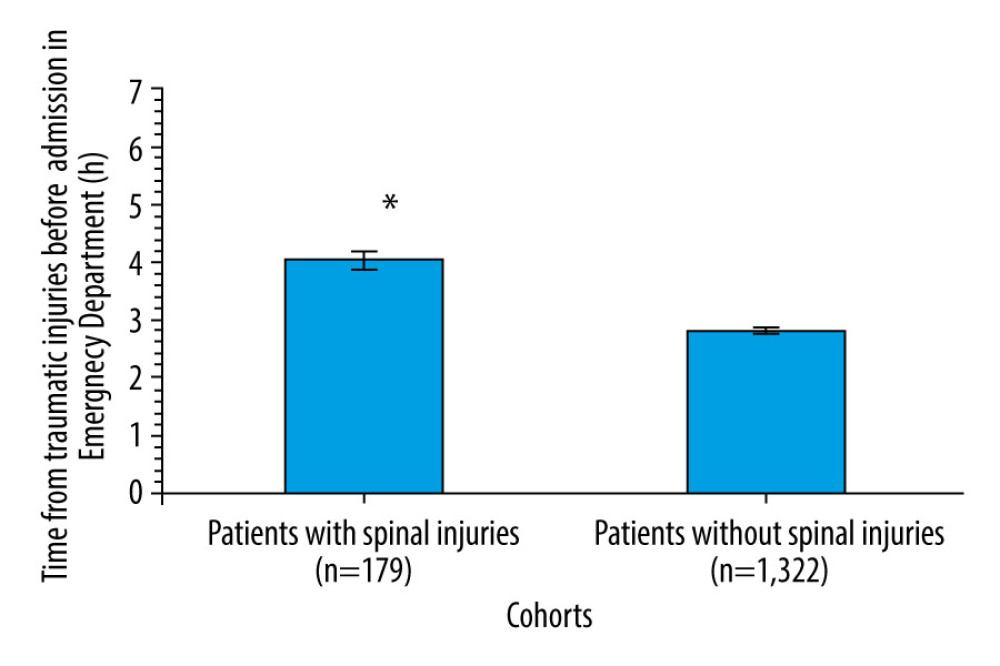 Figure 3. Time from traumatic injuries to admission to the Emergency Department among patients. Data presented as mean±standard error of the mean. * Higher time than those of patients without spinal injuries.
Figure 3. Time from traumatic injuries to admission to the Emergency Department among patients. Data presented as mean±standard error of the mean. * Higher time than those of patients without spinal injuries.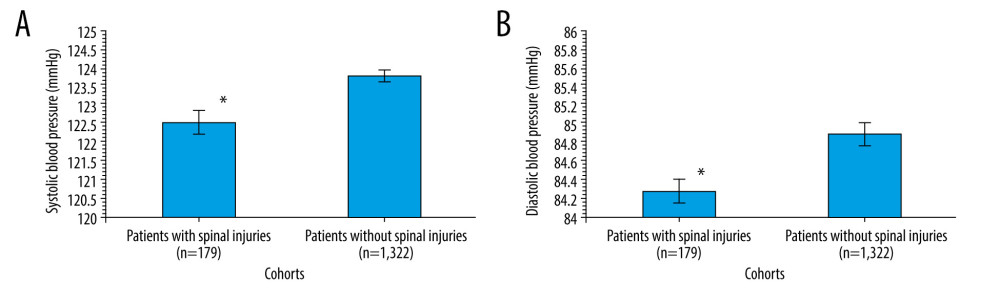 Figure 4. (A) Systolic blood pressure among patients. (B) Diastolic blood pressure among patients. Data presented as mean±standard error of the mean. * Lower blood pressure than those of patients without spinal injuries.
Figure 4. (A) Systolic blood pressure among patients. (B) Diastolic blood pressure among patients. Data presented as mean±standard error of the mean. * Lower blood pressure than those of patients without spinal injuries.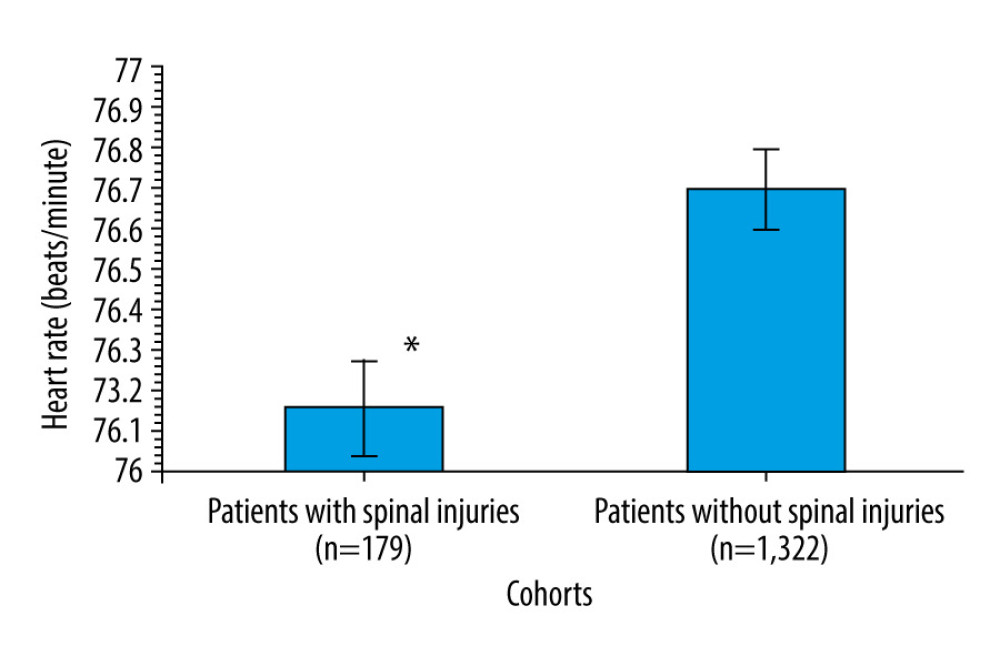 Figure 5. Distribution of heartbeats among patients. Data presented as mean±standard error of the mean. * Lower heartbeats than those of patients without spinal injuries.
Figure 5. Distribution of heartbeats among patients. Data presented as mean±standard error of the mean. * Lower heartbeats than those of patients without spinal injuries. Tables
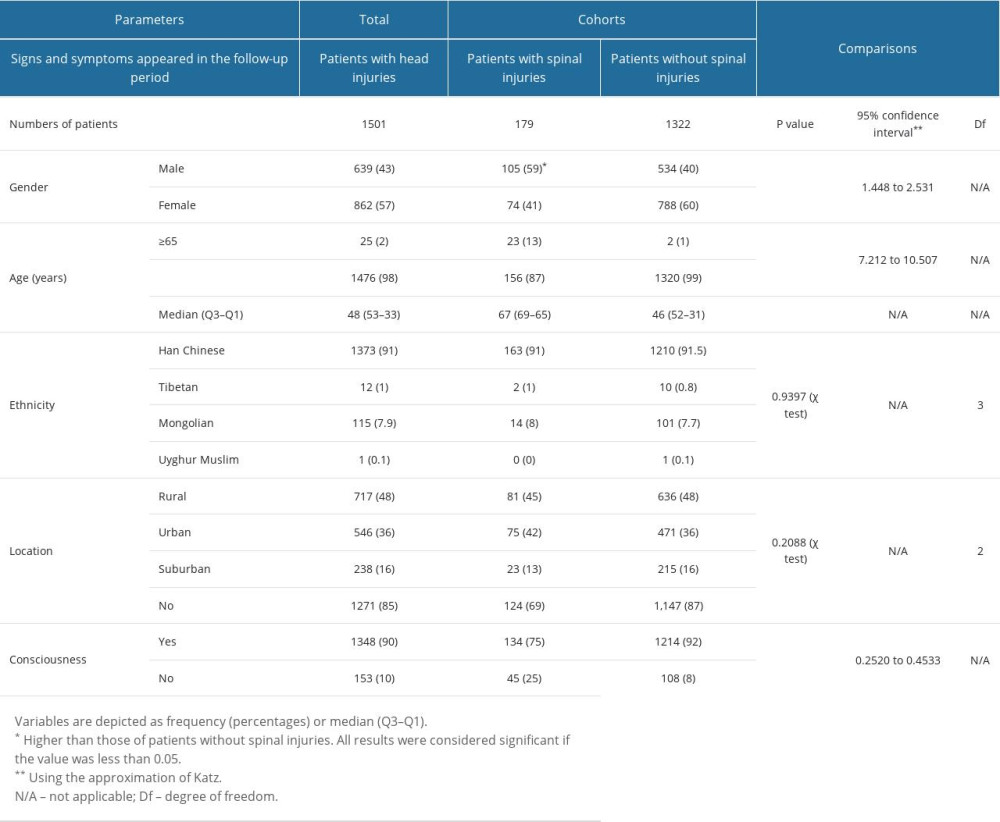 Table 1. Demographical and clinical parameters of the enrolled patients at the time of admission in the Emergency Department.
Table 1. Demographical and clinical parameters of the enrolled patients at the time of admission in the Emergency Department.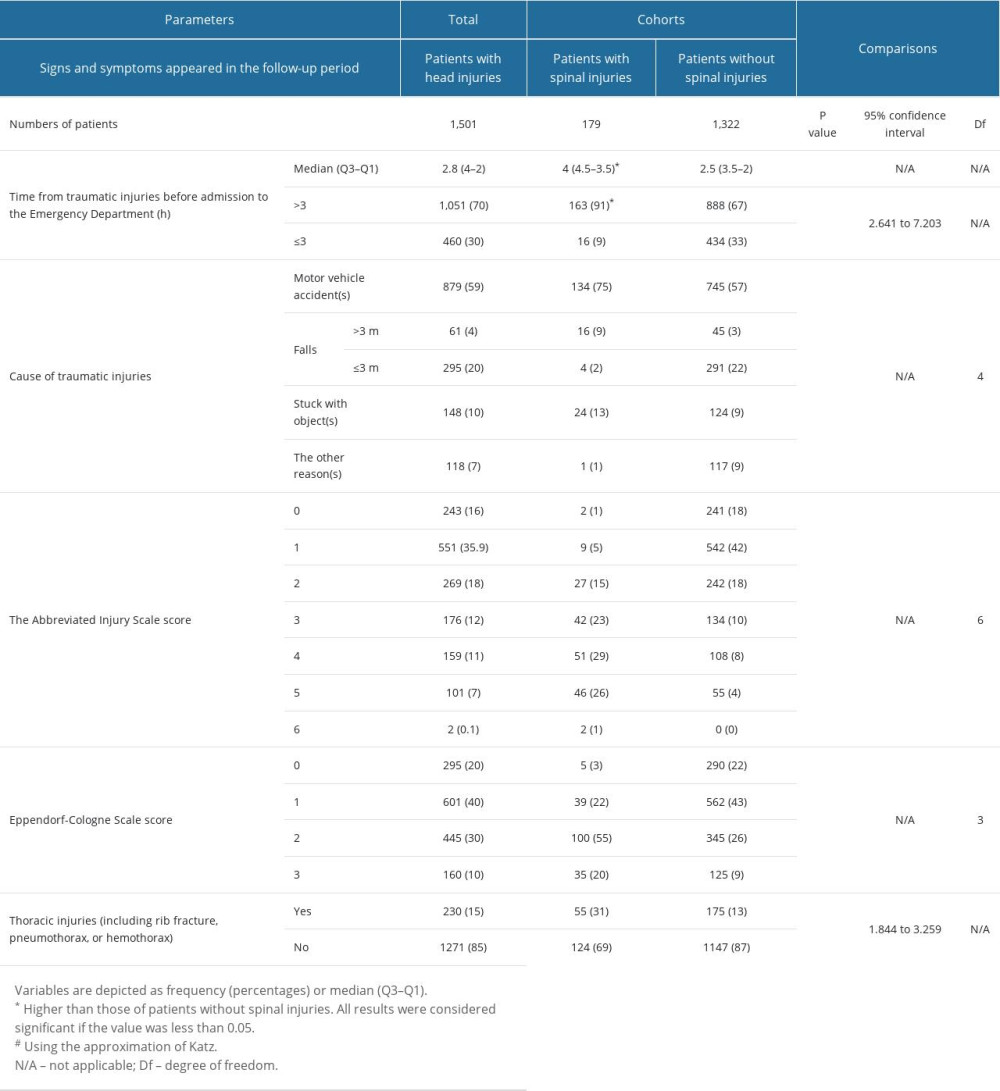 Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.
Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.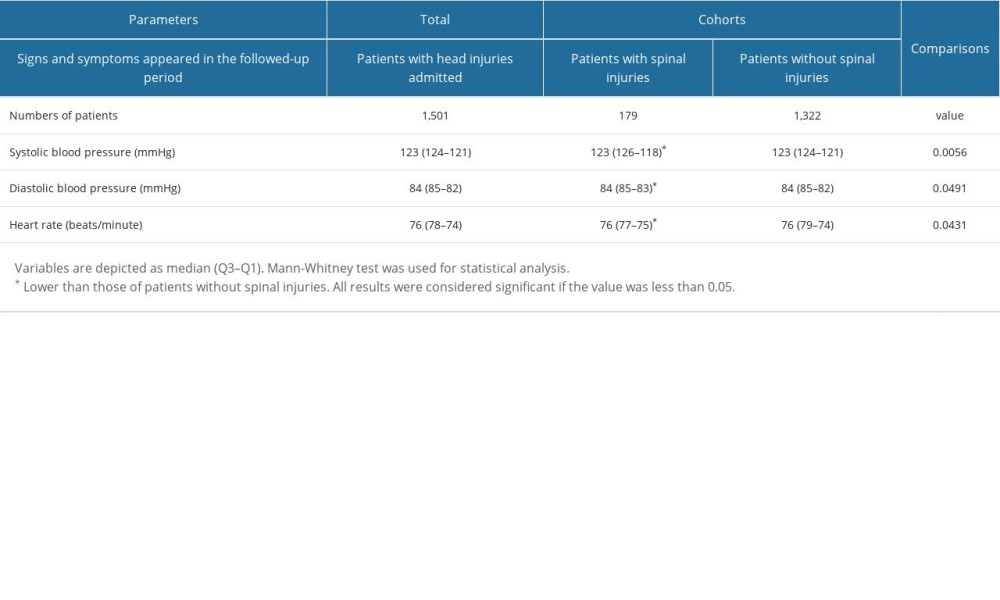 Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.
Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.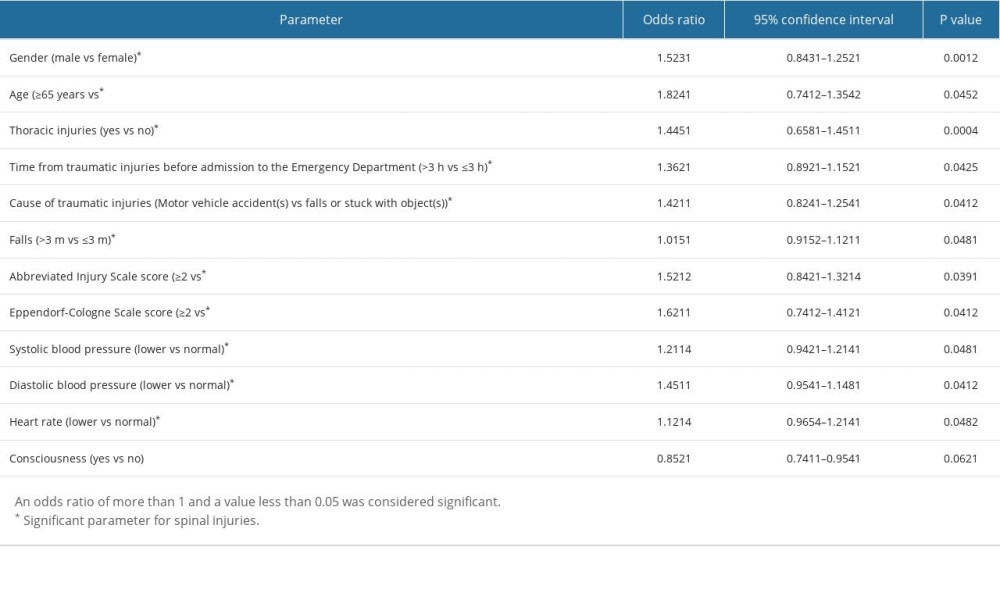 Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters.
Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters.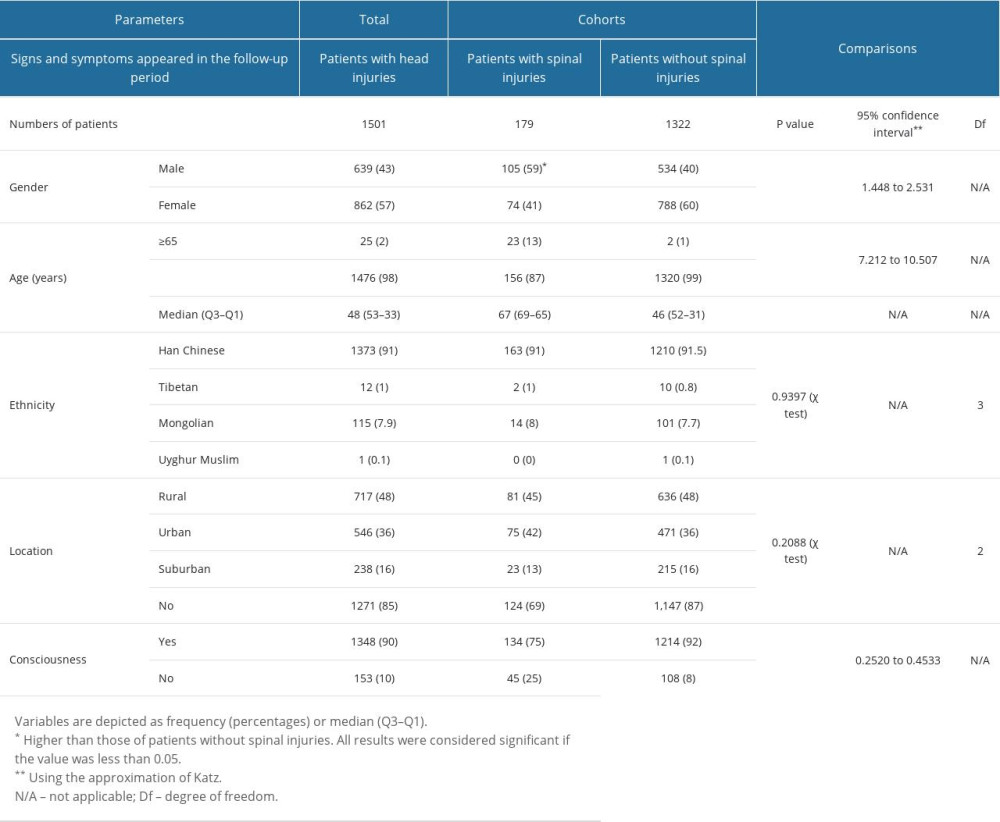 Table 1. Demographical and clinical parameters of the enrolled patients at the time of admission in the Emergency Department.
Table 1. Demographical and clinical parameters of the enrolled patients at the time of admission in the Emergency Department.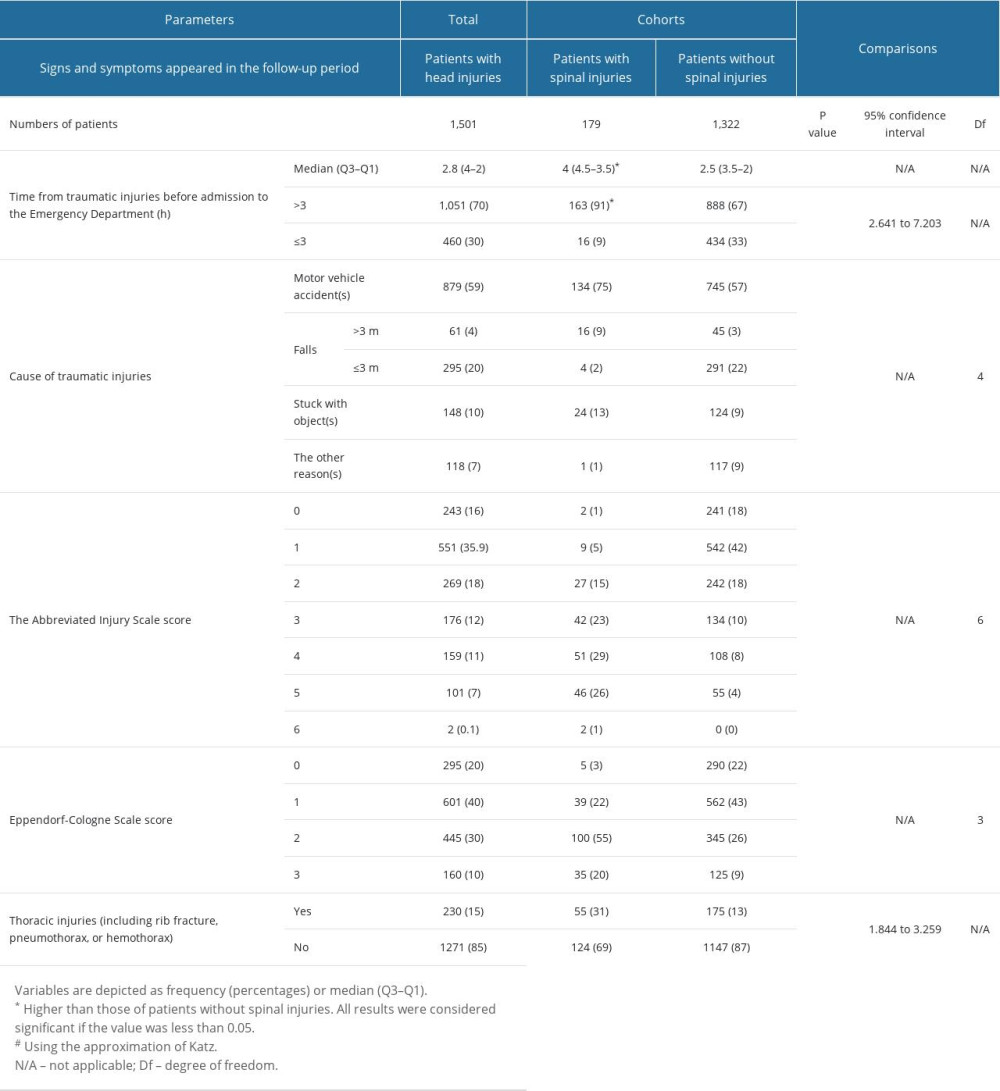 Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.
Table 2. Traumatological parameters of the enrolled patients at the time of admission in the Emergency Department.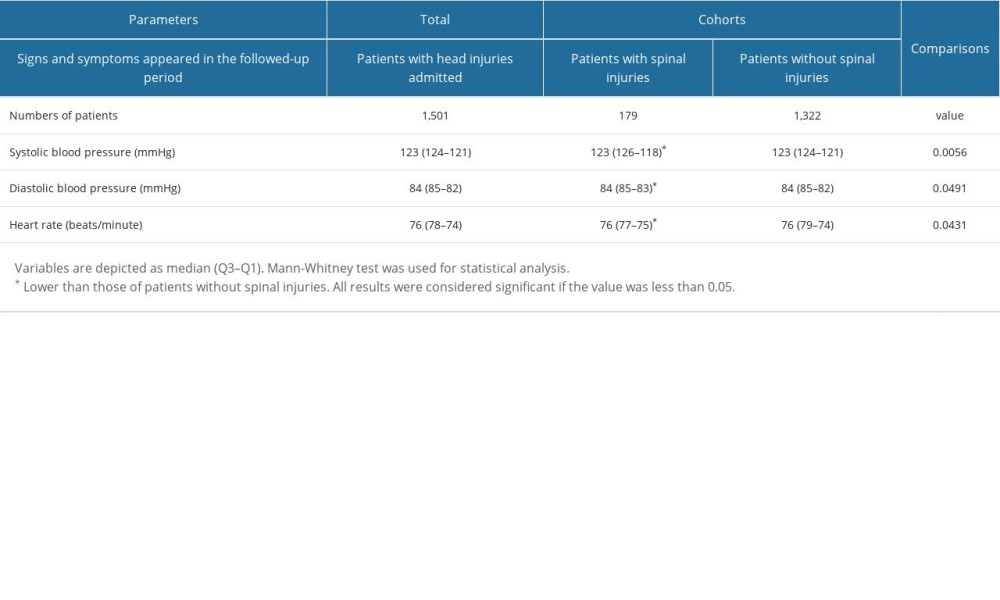 Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.
Table 3. Hemodynamic parameters of the enrolled patients at the time of admission in emergency.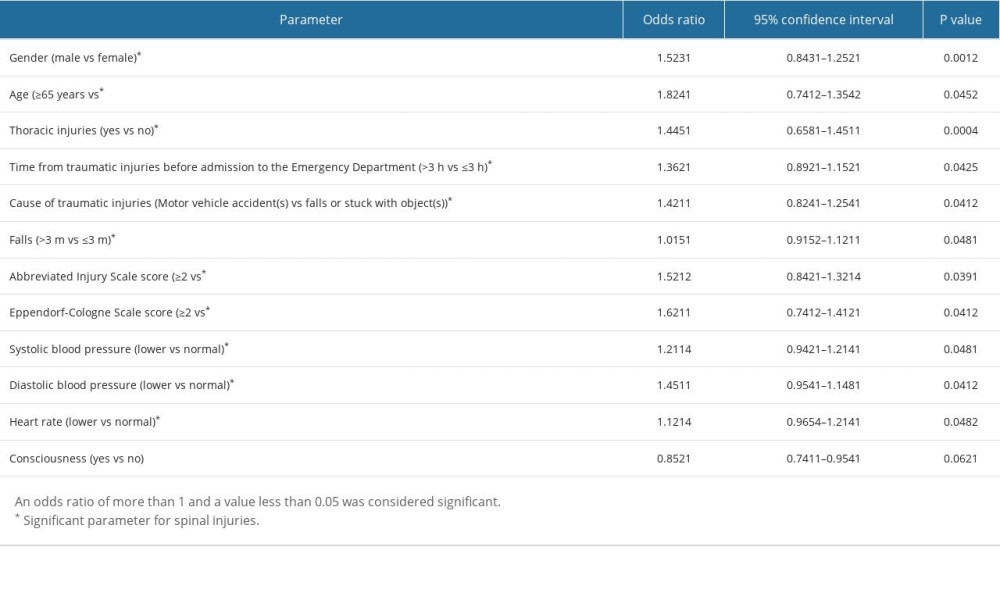 Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters.
Table 4. Multivariable regression analysis for association of spinal injuries with demographical and clinical parameters. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








