27 June 2023: Clinical Research
Effects of Conventional Speech Therapy with Liuzijue Qigong, a Traditional Chinese Method of Breath Training, in 70 Patients with Post-Stroke Spastic Dysarthria
Jiayi Xia1AEFG*, Song Pei23BCDE, Zhu Chen1DE, Lin Wang1FG, Jun Hu1AEG, Jian Wang2AEGDOI: 10.12659/MSM.939623
Med Sci Monit 2023; 29:e939623
Abstract
BACKGROUND: Post-stroke spastic dysarthria (PSSD) is a motor speech impairment that impacts patient communication and quality of life. Liuzijue Qigong (LQG), a traditional Chinese method of breath training, could serve as an effective treatment for PSSD. This study compared the effects of conventional speech therapy and conventional speech therapy combined with LQG in patients with PSSD.
MATERIAL AND METHODS: Seventy patients with PSSD were randomly divided into a control group (conventional speech therapy, n=35, 77.14% cerebral infarction, 22.86% cerebral hemorrhage) and experimental group (LQG combined with conventional speech therapy, n=35, 85.71% cerebral infarction, 14.29% cerebral hemorrhage). Conventional speech therapy included relaxation, breath control, organ articulation, and pronunciation training. LQG involved producing 6 different sounds (Xu, He, Hu, Si, Chui, and Xi) accompanied by breathing and body movements. Patients were treated once a day, 5 times a week, for 4 weeks. The Frenchay Dysarthria Assessment scale (FDA), speech articulation, maximum phonation time (MPT), loudness, and Montreal Cognitive Assessment scale (MoCA) were evaluated.
RESULTS: At 4 weeks, the experimental group showed significant improvements compared with the control group in the change of FDA (13.26±6.84 vs 18.03±5.32, P=0.028), speech articulation (63.17±22.40 vs 76.51±15.28, P=0.024), MPT (1.34±1.30 vs 3.89±3.98, P<0.001), loudness (3.46±2.74 vs 7.14±2.56, P=0.009), MoCA (19.40±3.72 vs 22.20±5.30, P=0.020), total effective rate (68.57% vs 88.57%, P=0.041).
CONCLUSIONS: LQG, when combined with conventional speech therapy, enhanced the comprehensive speech ability of patients with PSSD compared with conventional treatment alone.
Keywords: Stroke, dysarthria, qigong, Speech Therapy, Humans, Cerebral Hemorrhage, cerebral infarction, Quality of Life, Speech, Breathing Exercises
Background
In recent years, stroke, characterized by high prevalence, incidence, and mortality, has emerged as a primary cause of disability and death [1]. A significant number of stroke survivors, approximately 25% to 42%, experience concurrent dysarthria [2], with spastic dysarthria being common in cases involving upper motor neuron lesions [3]. Post-stroke spastic dysarthria (PSSD) is an acquired speech disorder that arises from neurological injury and impairs speech intelligibility due to tense, imprecise, slow, or uncoordinated muscle control [4]. PSSD results in abnormalities in breathing, vocalization, resonance, and rhythm, manifesting as slow and laborious speech, unclear pronunciation, and hypernasality, thereby causing issues in linguistic function, social participation, and psychological and emotional dimensions [5]. Various treatment methods, including relaxation, breath control, organ articulation, and pronunciation training, are employed in the clinical treatment of PSSD to improve fluency and pronunciation clarity [6].
Liuzijue Qigong (LQG), a 6-word breathing exercise, integrates coordinated body-posture and movement, breathing, and meditation for health, spirituality, and martial-arts training purposes [7]. It is a slow and gentle exercise that combines breathing with lip and tongue movement and is performed simultaneously with a whole-body exercise [8]. LQG has been used in the rehabilitation of respiratory disorders, cognitive impairments, stroke, and other diseases, offering advantages such as being time-saving and labor-saving and having clinical efficacy [8–10]. Although patients with spastic dysarthria process a normal cortical language center, their difficulties in controlling breathing, vocalization, rhythm, and resonance lead to speech impairment. As nondrug therapy is recommended for integration into post-stroke dysarthria rehabilitation by clinical practice guidelines, LQG could serve as an effective and clinically significant treatment for the PSDD population [11]. However, no studies have yet investigated the effect of LQG in this population.
The purpose of this study was to compare the effects of conventional speech therapy and conventional speech therapy combined with LQG in patients with PSSD. The hypothesis of this study is that LQG combined with conventional speech therapy has better clinical outcome measures than conventional speech therapy alone.
Material and Methods
ETHICAL STATEMENT:
This study protocol was reviewed and approved by the Ethics Committee of the Second Rehabilitation Hospital of Shanghai (approval number 2020-01-03). The registration number for the clinical trial was ChiCTR2000038726. All patients provided written informed consent to participate in the study, and all research carried out in participants was in compliance with the Helsinki Declaration.
CONTROL GROUP:
Treatments were administered once a day, 5 times a week, for a period of 4 weeks. Patients in the control group received 20-min of conventional speech therapy, including relaxation training, breath control training, organ articulation training, and single vowels, diphthongs, syllables, and sentence repetition training [13].
EXPERIMENTAL GROUP:
Treatments were administered once a day, 5 times a week, for a period of 4 weeks. In addition to the 20-min conventional speech therapy session, patients in the experimental group also received a 20-min LQG session, as detailed by the 2003 LQG standards of the General Administration of Sport [10].
LQG adopts rhythmic abdominal breathing. The method involves inhaling slowly through the nose and exhaling through the mouth while producing 6 different sounds (Xu, He, Hu, Si, Chui, and Xi), supplemented by corresponding synchronous body movements [8]. In this study, patients were required to pay attention to the movements of the limbs and the torso in coordination with breathing, and to master the pronunciation with the correct tongue and mouth positions. Table 2 describes and compares conventional speech therapy and LQG.
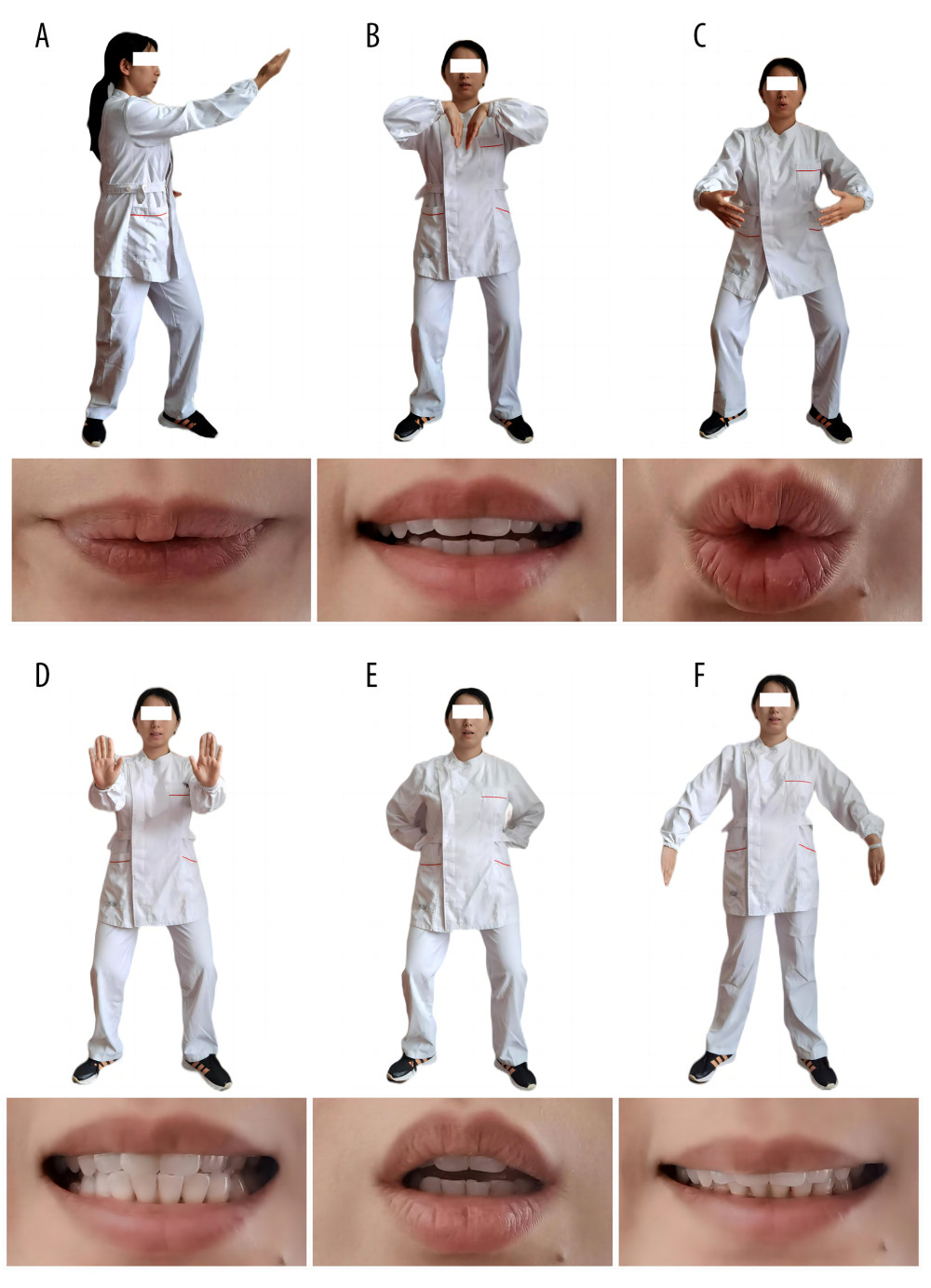
The 6 words and their pronunciation were as follows (Figure 1):
The experimental participants were trained in the proper technique for performing LQG by an experienced therapist, as follows. The body should remain relaxed, quiet, and maintain a relaxed mood while training. LQG started from a slight squat with a bent knees position. Before the treatment, the tongue and mouth positions were taught to each patient while they performed the breathing and pronunciation exercises. The patients were required to gradually feel the tongue and mouth positions of corresponding pronunciations to improve the accuracy of the pronunciation and breathing, rather than only forcing the pronunciation. Different pronunciations were completed with different body movements. In the training process, patients who failed to complete the tasks independently were assisted by the therapist or asked to change the body position appropriately.
Each pronunciation lasted for 5 to 8 s, including an inhalation and an exhalation. After 6 pronunciations of each sound, the breathing of each patient was adjusted twice before the pronunciation training for the next sound. All breathing, pronunciation, and actions were carried out in order and recorded as a complete cycle of LQG. In addition, the patients were asked to maintain mild exertion or mild fatigue, namely, reaching a score of 11 or 12 on the Borg Rating of Perceived Exertion Scale [14].
EVALUATION INDEX:
The current literature does not report any guidelines for clinical assessment of patients with post-stroke dysarthria [12]. Therefore, according to the recent systematic reviews, we selected the following scales and assessments, which are simple to use in clinical operation and have good patient compliance, for the diagnosis and quantification of dysarthria.
FRENCHAY DYSARTHRIA ASSESSMENT: The Frenchay Dysarthria Assessment scale (FDA), an objective test for assessing vocal organs and the severity of speech disorders, was used [15]. The test comprises 8 major items and 28 subitems. Each subitem is divided into 5 levels according to the degree of damage (from level A to level E), in which level A represents the norm, B mild severity, C moderate severity, D considerable severity, and E very high severity. Level A serves as the normal baseline to quantify recovery from dysarthria. Each item of level A was collectively recorded as 1 score, with the total score ranging from 0 to 28. The test evaluates functions such as swallowing, breathing, and performance of the tongue, lips, soft palate, and jaw, as well as reflexes, voicing, and intelligibility, among others. The test scores the degree of dysarthria as normal (27–28), mild (18–26), moderate (14–17), severe (7–13), or extremely severe (0–6).
PERCEPTUAL SUBJECTIVE VOICE ASSESSMENT: The grade-roughness-breathiness-asthenia-strain (GRBAS) scale is a perceptual subjective voice assessment to evaluate pathological voice quality [16]. We used the GRBAS of the Japan Society of Logopedics and Phoniatrics to evaluate the vocal disorders in the 2 groups, including grade, roughness, breathiness, asthenia, and strain. Each item was divided into 4 levels: level 0 (normal); level 1 (mild); level 2 (moderate); and level 3 (severe). Evaluators asked participants the same content and manner in a quiet environment and required them to answer in a natural tone and volume, followed by a recording of the score. Results of strain and roughness related to the patients with spastic dysarthria were used as evaluative indicators for the effective rate in this study.
If the severity of dysarthria was improved by one or more grades and either strain and roughness reduced by one or more levels, the intervention was considered effective. No change was considered ineffective. Total effective rate=effective number of people/total number of people in each group×100%.
ASSESSMENT OF SPEECH ARTICULATION: We used 2 word tables for the Chinese phonetic articulation test [17] to evaluate speech articulation, including Word Table I, designed according to the abnormal phonetics that patients are likely to encounter in clinical practice, and Word Table II, designed according to the initial consonant and vowels of the phonological rules of Mandarin Chinese. Each table contains 100 high-frequency Chinese characters. During the test, patients were asked to read the list of words one by one, and their pronunciations were recorded. A therapist not involved in the treatment, an untrained volunteer, and a patient’s family member performed dictation comparisons. The calculation of the percentage of independently correctly pronounced words were then taken from the average of the 3 measurements to record the result. Each patient was assessed by the same volunteer, speech therapist, and family member.
MAXIMUM PHONATION TIME: Maximum phonation time (MPT) has been identified as a reliable measurement in voice assessment [12]. Each patient was instructed to sit normally and continuously pronounce the vowel /a/ at maximum loudness until the end of expiration after a deep inhalation. A stopwatch was used to record the duration of the sound, with the maximum value obtained after 3 measurements. MPT measurements required: (1) the longest possible procuration duration, (2) uniform breathing flow, and (3) consistent loudness and tone.
LOUDNESS: Loudness is an indicator of acoustic characteristics [18]. A Xima AR824 decibel meter recorded patients’ pronunciations loudness during quiet conversation, positioned 1 cm away from the lips.
MONTREAL COGNITIVE ASSESSMENT SCALE: The Montreal Cognitive Assessment (MoCA) scale assesses 8 cognitive domains: visual-spatial and executive functions; naming; short-term memory; attention; language fluency; abstraction, delayed memory; and orientation [19]. The total MoCA scale score is 30, with patients scoring below 26 points considered to have cognitive dysfunction. Patients with 12 or fewer years of education received an additional point.
All results were evaluated and recorded at baseline and at the 4-week study completion. The primary observation indicator was the FDA, followed by the GRBAS, speech articulation, MPT, loudness, MoCA, and effective rate.
STATISTICAL ANALYSIS:
Data processing and statistical analysis were conducted using SPSS 22.0 software (IBM, Armonk, NY, USA). General statistical descriptions, such as the number of cases (%) or mean±standard deviation, were used for demographic and clinical characteristics. The FDA, speech articulation, MPT, loudness, and MoCA were expressed as mean±standard deviation. Difference between sexes, paralysis sides, stroke types, National Institutes of Health Stroke Scale scores, comorbidities, and effective rates were performed using the chi-square test. The evaluation data conformed to the normality test. Intergroup comparisons were performed using an independent sample
Results
BASELINE COMPARISON:
No significant differences were found between the 2 groups at baseline for FDA (10.54±7.02 vs 10.54±7.02, P=0.299), speech articulation (44.09±23.71 vs 46.26±20.09, P=0.460), MPT (9.60±4.51 vs 8.63±5.13, P=0.176), loudness (38.23±9.13 vs 36.71±8.44, P=0.951), and MoCA (17.91±4.14 vs 18.20±5.48, P=0.240; Tables 3–6).
INTRAGROUP COMPARISONS AFTER THE INTERVENTIONS:
After 4 weeks of intervention, statistically significant differences were observed within the control group before and after intervention in FDA (10.54±7.02 vs 13.26±6.84,
Similarly, significant differences were found within the experimental group before and after the interventions in the FDA (10.54±7.02 vs 18.03±5.32, P<0.001), speech articulation (46.26±20.09 vs 76.51±15.28, P<0.001), MPT (8.63±5.13 vs 12.51±5.04, P<0.001), loudness (36.71±8.44 vs 43.86±7.80, P<0.001), and MoCA (18.20±5.48 vs 22.20±5.30, P<0.001; Tables 3–6).
INTERGROUP COMPARISONS AFTER THE INTERVENTIONS:
After intervention, significant differences between the control and experimental groups were found in the FDA (13.26±6.84 vs 18.03±5.32, P=0.028), speech articulation (63.17±22.40 vs 76.51±15.28, P=0.024), and MoCA (19.40±3.72 vs 22.20±5.30, P=0.020), indicating improvements in articulator movements, speech articulation, and MoCA scores in the experimental group were more pronounced than in the control group (Tables 3, 6).
No significant differences were found between the 2 groups in MPT (10.94±4.54 vs 12.51±5.04, P=0.334) and loudness (41.69±8.58 vs 43.86±7.80, P=0.606) after the interventions. However, the increase in MPT (1.34±1.30 vs 3.89±3.98, P<0.001) and loudness (3.46±2.74 vs 7.14±2.56, P=0.009) showed a significant difference between the 2 groups, with the experimental group exhibiting greater increases in MPT and loudness than the control group (Tables 4, 5).
The combined evaluation of strained and rough sounds after the interventions demonstrated that the total effective rates for the experimental and control groups were 88.57% and 68.57%, respectively. This result indicated a significant difference between the 2 groups (
Discussion
LQG EFFECTS ON BREATHING REGULATION IN PSSD:
Speech output requires stable and effective breathing support to improve stability and airflow utilization efficiency. Establishment of a normal breathing pattern is fundamental to breathing regulation in LQG when treating PSSD [22]. Howard et al [23] found that patients with post-stroke dysarthria often exhibit abnormal breathing regulation. Restoring a proper and effective coordination pattern between breathing and speech facilitates normal speech recovery in these patients, as sound production relies on the volume and control of the breathing airflow [12]. Tang et al [24] demonstrated that the moderate strength of LQG positively impacts cardiopulmonary function and respiratory muscles. Exercises involving the 2 sounds “Hu” and “Si” increase lung volume. Traditional articulation training, such as blowing paper, blowing out a candle, and playing the flute, do not address the simultaneous pronunciation and breathing treatment and focus on muscle strengthening. LQG coordinates various body movements and lip shape changes during inhalation and exhalation. It improves aerobic metabolism and respiratory resistance in the thoracic and abdominal cavities, as well as improving peripheral blood circulation, respiratory muscle strength, endurance, and coordination [25]. Combined with the evaluation of MPT duration, the LQG breathing-regulation effect significantly improved respiratory function in patients with PSSD after intervention (Table 3).
LQG EFFECTS ON BODY REGULATION IN PSSD:
The effects of LQG on pronunciation, resonance, and articulation in speech output constitute the body regulation process of LQG in PSSD treatment. Practicing lip syncing with 6 sounds, “Xu,” “He,” “Hu,” “Si,” “Chui,” and “Xi,” results in varying strain on the larynx, tongue, teeth, and lips, and the qi, blood, and meridian movement in the involved organs also differ, based on traditional Chinese medicine theory [26]. In the human body, pronunciation primarily relates to throughput breath, vocal cord vibration, and body part resonance, meaning different sounds require the involvement of various body parts [21]. LQG, a health preservation method developed by ancient practitioners, is based on vocal system principles. Sound production relies on vibration, implying that health-preserving LQG principles are founded on the resonance of the human body.
Pronouncing the 6 sounds involves guttural sounds, dental consonants, lingual sounds, labial sounds, and breathy voices, improving articulator movements. Generally, the consonants of the 6 sounds belong to the unvoiced consonants category. Natural vocalization requires low muscle energy consumption, reducing muscle tension in patients with PSSD. Pronouncing these soft pitches reduces laryngeal muscles tension and achieves more complete glottal closure [27]. Combined with FDA, GRBAS, speech articulation, and calm loudness communication evaluations, LQG body regulation significantly improved pronunciation resonance, articulator movement, strained sounds, rough sounds, and speech articulation in patients with PSSD in the experimental group after the intervention (Tables 2, 4). Wang et al [10] showed that LQG, combined with basic articulation training, could improve the respiratory control ability of stroke patients with dysarthria. However, no significant difference was found in the loudness level between the groups, which might be due to the selection of 5 volume levels (whisper, soft, conversation, loud, and shouting) to evaluate loudness. Thus, the decibel value was used to quantify the loudness level, which might be a more objective evaluation method.
LQG EFFECTS ON MIND REGULATION IN PSSD:
Cognitive processing affects the entirety of speech production in the body. Some researchers believe that cognitive processing, including concepts and language, interacts with the sensory-motor systems of the body [28,29]. The cognitive-motor-language system of patients with PSSD is activated in the LQG process. The cognitive component involves the visual, tactile, proprioceptive, and cognitive processing module. The motor component involves the torso, mouth, and facial movement, and the language component involves speech production. With long-term enhancement, this training engages patients in movement feedback and cognition, whereby cognition enhances speech and leads to improvements in movement [30]. For middle-aged and older post-stroke patients, aerobic exercises, especially moderate-intensity aerobic exercises, promote the production of neurotrophic factors, the formation of blood vessels in brain tissues, nerve maturation development, and neuroplasticity occurrence, thereby promoting cognitive function and improving speech performance. Combined with the MoCA scale, cognitive function in patients with PSSD after intervention was significantly improved through the effects of LQG in mind regulation (Table 5).
Although this study demonstrated that LQG is an effective treatment for post-stroke patients with PSSD, there are some limitations. The study compared LQG with conventional therapy over only a 4-week period in post-stroke patients with PSSD, leaving the long-term effects unclear. The sample population primarily included patients with mild and moderate stroke, which means caution is needed when applying the outcomes to patients with severe stroke. Additionally, the mechanism of LQG’s effects on this population remains unclear. The study did not investigate the impact of LQG on variables related to neural pathways and brain function.
Conclusions
LQG, when combined with conventional speech therapy, could enhance the comprehensive speech ability of patients with PSSD, as the findings demonstrated improvements in breathing control ability, speech articulation, articulator function, and cognitive ability, compared with conventional treatment alone. LQG, a low-to-medium-intensity holistic exercise that combines the regulation of mind, breathing, and body, is not limited by time, space, venue, or equipment. Therefore, it can be used as an independent supplementary training for patients with PSSD following conventional speech therapy.
Tables
Table 1. Participant characteristics at baseline (n=35).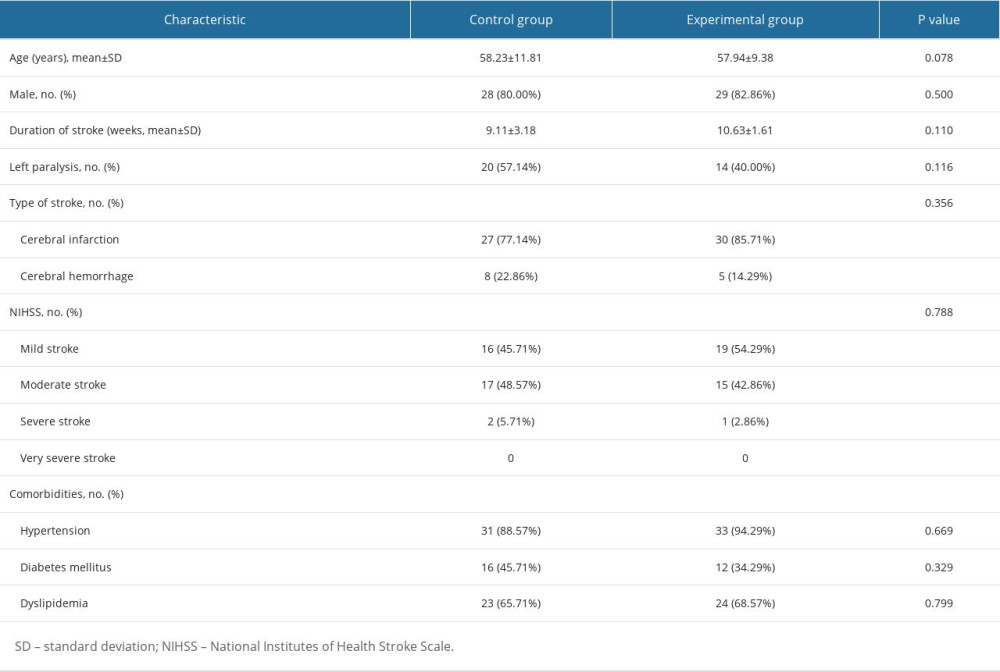 Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.
Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.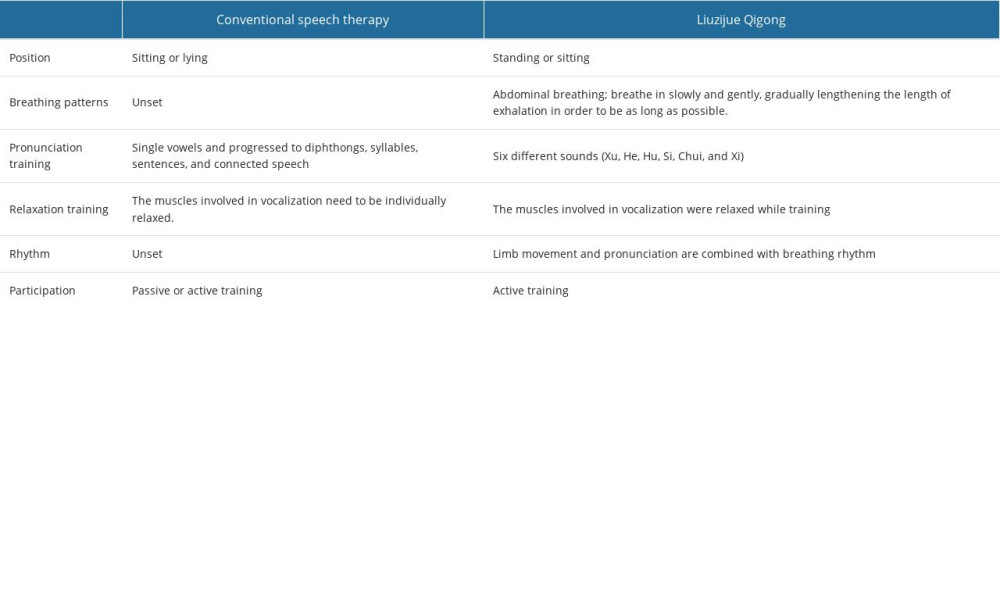 Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).
Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).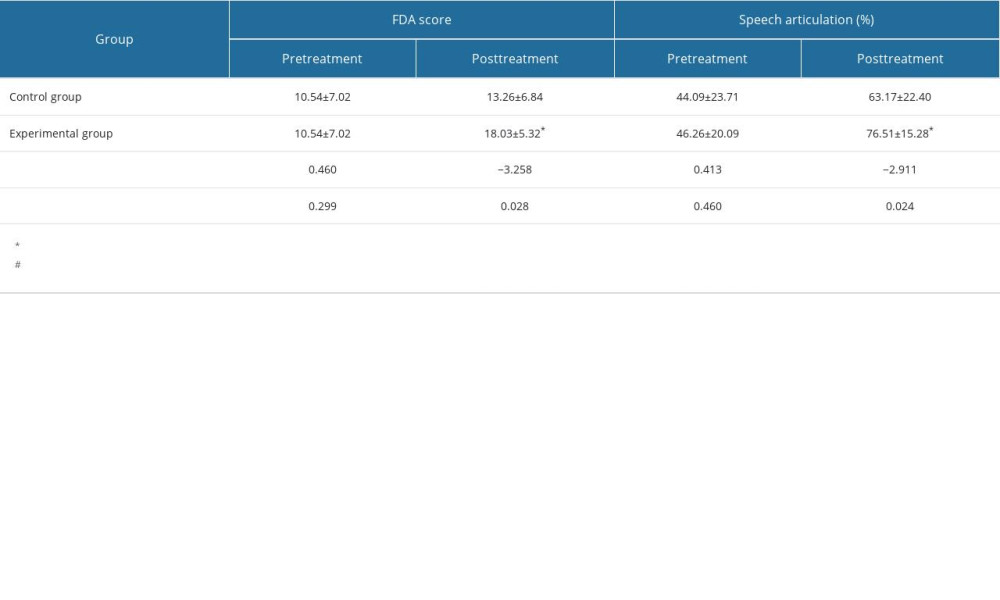 Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35).
Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35).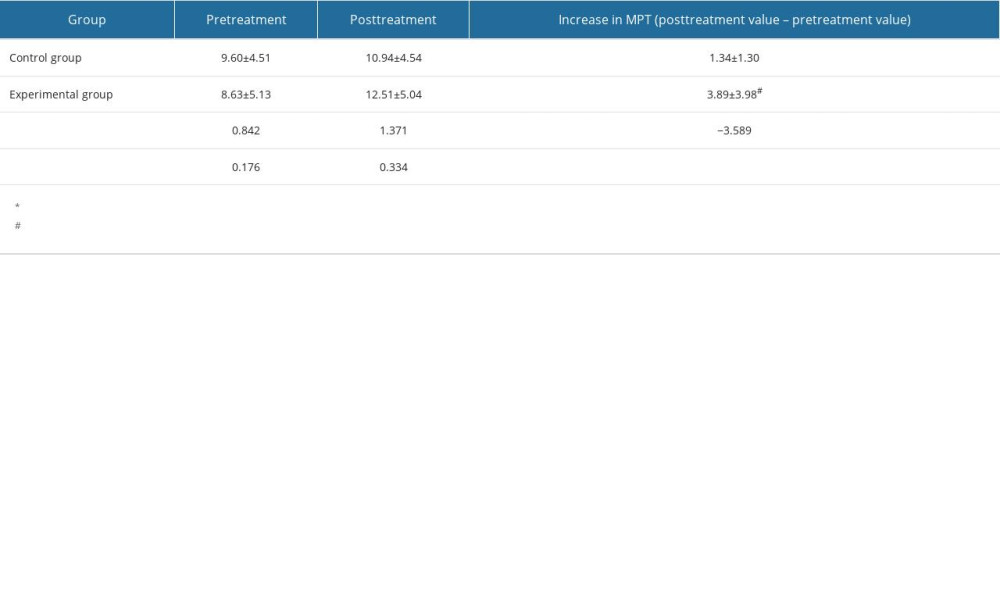 Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups.
Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups. Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35).
Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35).
References
1. Feigin VL, Krishnamurthi RV, Parmar P, Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: The GBD 2013 Study: Neuroepidemiology, 2015; 45; 161-76
2. Flowers HL, Silver FL, Fang J, The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke: J Commun Disord, 2013; 46; 238-48
3. Ge S, Wan Q, Yin M, Quantitative acoustic metrics of vowel production in mandarin-speakers with post-stroke spastic dysarthria: Clin Linguist Phon, 2021; 35; 779-92
4. Mitchell C, Bowen A, Tyson S, Interventions for dysarthria due to stroke and other adult-acquired, non-progressive brain injury: Cochrane Database Syst Rev, 2017; 1; CD002088
5. Comrie P, MacKenzie C, McCall J, The influence of acquired dysarthria on conversational turn-taking: Clin Linguist Phon, 2001; 15; 383-98
6. Gittler M, Davis AM, Guidelines for adult stroke rehabilitation and recovery: JAMA, 2018; 319; 820-21
7. Li L, Huang H, Song J, Network meta-analysis of the effects of different types of traditional Chinese exercises on pulmonary function, endurance capacity and quality of life in patients with COPD: Front Med (Lausanne), 2022; 9; 806025
8. Xu S, Zhang D, He Q, Efficacy of Liuzijue Qigong in patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis: Complement Ther Med, 2022; 65; 102809
9. Zheng Y, Zhang Y, Li H, Comparative effect of Liuzijue Qigong and conventional respiratory training on trunk control ability and respiratory muscle function in patients at an early recovery stage from stroke: A randomized controlled trial: Arch Phys Med Rehabil, 2021; 102; 423-30
10. Wang J, Li G, Ding SY, Liuzijue Qigong versus traditional breathing training for patients with post-stroke dysarthria complicated by abnormal respiratory control: Results of a single-center randomized controlled trial: Clin Rehabil, 2021; 35; 999-1010
11. Mackenzie C, Dysarthria in stroke: A narrative review of its description and the outcome of intervention: Int J Speech Lang Pathol, 2011; 13; 125-36
12. Chiaramonte R, Vecchio M, Dysarthria and stroke. The effectiveness of speech rehabilitation. A systematic review and meta-analysis of the studies: Eur J Phys Rehabil Med, 2021; 57; 24-43
13. Chiaramonte R, Pavone P, Vecchio M, Speech rehabilitation in dysarthria after stroke: A systematic review of the studies: Eur J Phys Rehabil Med, 2020; 56; 547-62
14. Arney BE, Glover R, Fusco A, Comparison of RPE (rating of perceived exertion) scales for session RPE: Int J Sports Physiol Perform, 2019; 14; 994-96
15. Chiaramonte R, Vecchio M, A systematic review of measures of dysarthria severity in stroke patients: PM R, 2021; 13; 314-24
16. Hidaka S, Lee Y, Nakanishi M, Automatic GRBAS scoring of pathological voices using deep learning and a small set of labeled voice data: J Voice; 2022 [Online ahead of print]
17. Pang Z-j, Liu H-x, Gao L-q, Advance in assessment of speech intelligibility in adults with dysarthria: Chinese Journal of Rehabilitation Theory and Practice, 2019(12); 140-45
18. Mahler LA, Ramig LO, Intensive treatment of dysarthria secondary to stroke: Clin Linguist Phon, 2012; 26; 681-94
19. Tsuboi T, Watanabe H, Tanaka Y, Clinical correlates of repetitive speech disorders in Parkinson’s disease: J Neurol Sci, 2019; 401; 67-71
20. Mou Z, Chen Z, Yang J, Xu L, Acoustic properties of vowel production in Mandarin-speaking patients with post-stroke dysarthria: Sci Rep, 2018; 8; 14188
21. Gong T, Lu T, Zhang Y, Effects of Liuzijue Qigong posture on aerodynamics of phonation in healthy volunteers: J Voice, 2022 [Online ahead of print]
22. Li H, Li G, Liu G, Zhang Y, Liuzijue Qigong vs traditional breathing training for patients with post-stroke dysarthria complicated with abnormal respiratory control: Study protocol of a single center randomized controlled trial: Trials, 2018; 19; 335
23. Howard RS, Rudd AG, Wolfe CD, Williams AJ, Pathophysiological and clinical aspects of breathing after stroke: Postgrad Med J, 2001; 77; 700-2
24. Tang Y, Jiang J, Shen P, Liuzijue is a promising exercise option for rehabilitating discharged COVID-19 patients: Medicine (Baltimore), 2021; 100; e24564
25. Gao P, Tang F, Liu W, Effect of liuzijue qigong on patients with stable chronic obstructive pulmonary disease: A systematic review and meta-analysis: Medicine (Baltimore), 2021; 100; e27344
26. Wang C, Yu L, Yang J, Effectiveness of LiuZiJue Qigong versus traditional core stability training for poststroke patients complicated with abnormal trunk postural control: Study protocol for a single-center randomized controlled trial: Trials, 2020; 21; 254
27. Tang J, Huang W, Chen X, Liuzijue Qigong: A voice training method for unilateral vocal fold paralysis patients: Ann Otol Rhinol Laryngol, 2019; 128; 654-61
28. Hugues N, Pellegrino C, Rivera C, Is high-intensity interval training suitable to promote neuroplasticity and cognitive functions after stroke?: Int J Mol Sci, 2021; 22(6); 3003
29. Estrada-Rojas K, Cedeno Ortiz NP, Increased improvement in speech-language skills after transcranial photobiomodulation plus speech-language therapy, compared to speech-language therapy alone: Case report with aphasia: Photobiomodul Photomed Laser Surg, 2023; 41(5); 234-40
30. Zhang S, JI X, Wang Q, Action verb processing for exciting the motor cortex and promoting the recovery of upper limb function after stroke: Chinese Journal of Physical Medicine and Rehabilitation, 2017(12); 412-17
Tables
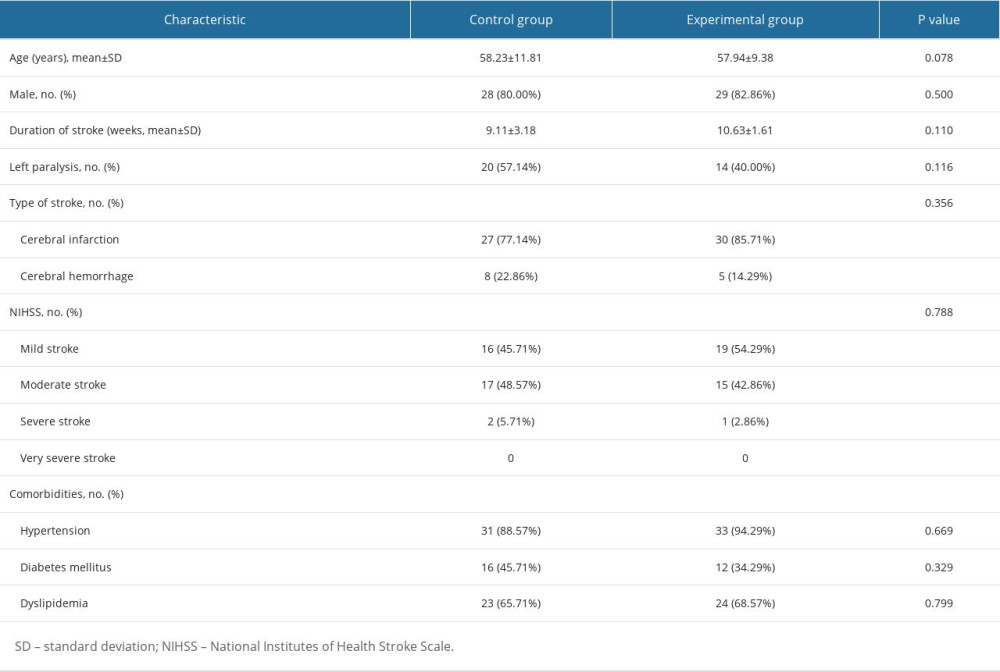 Table 1. Participant characteristics at baseline (n=35).
Table 1. Participant characteristics at baseline (n=35).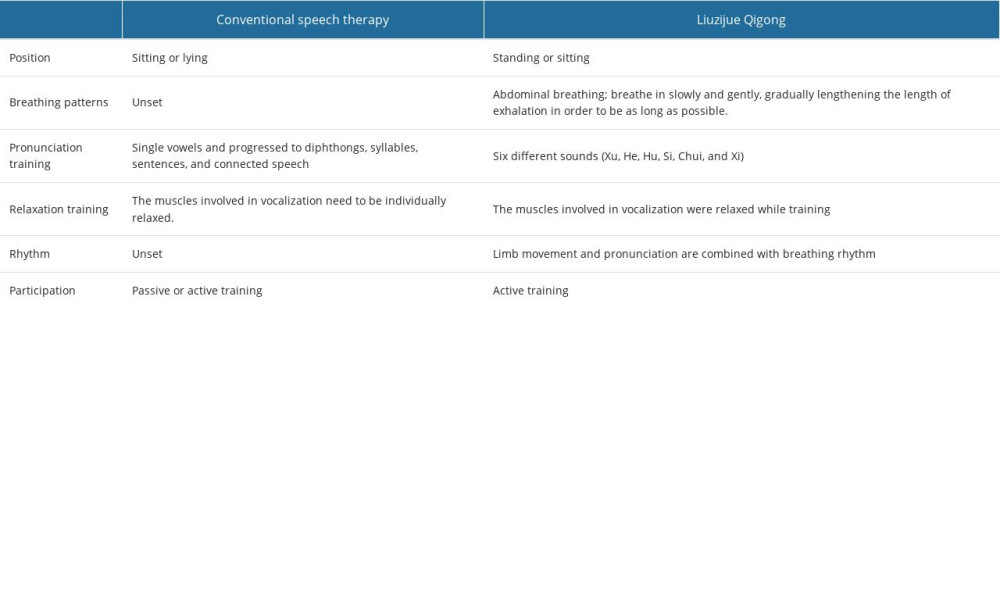 Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.
Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.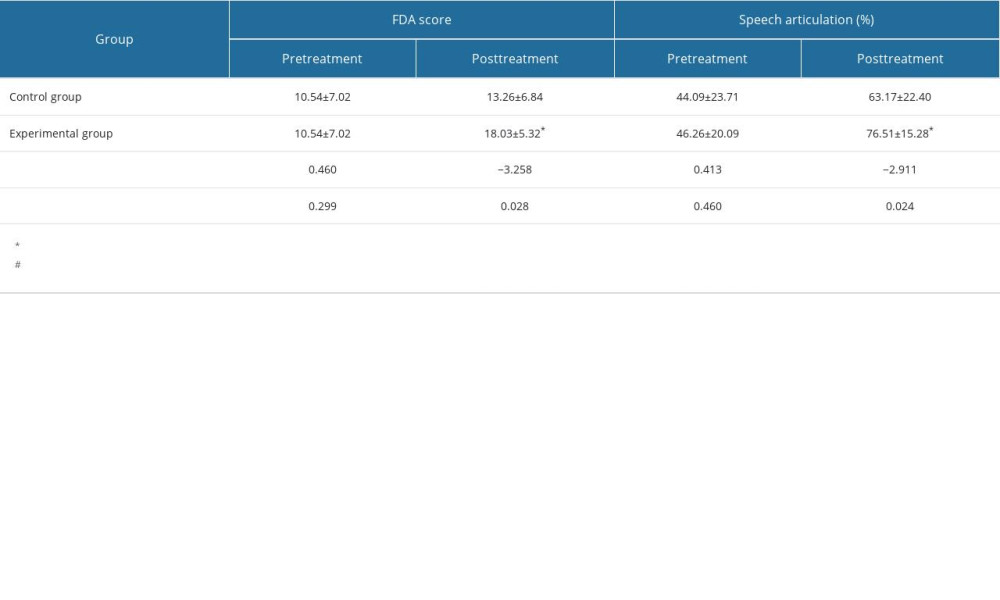 Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).
Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).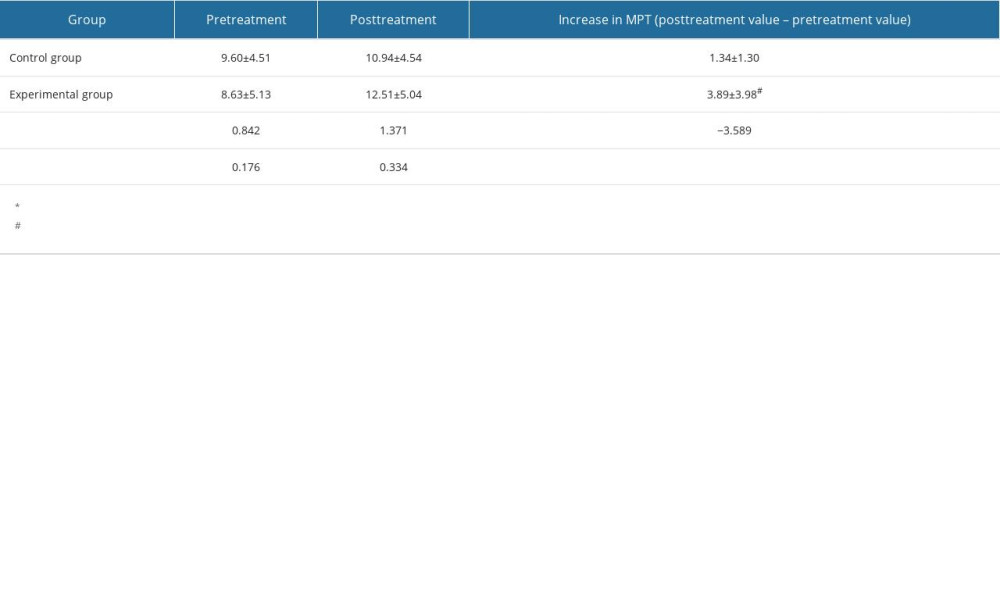 Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35).
Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35). Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups.
Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups. Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35).
Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35).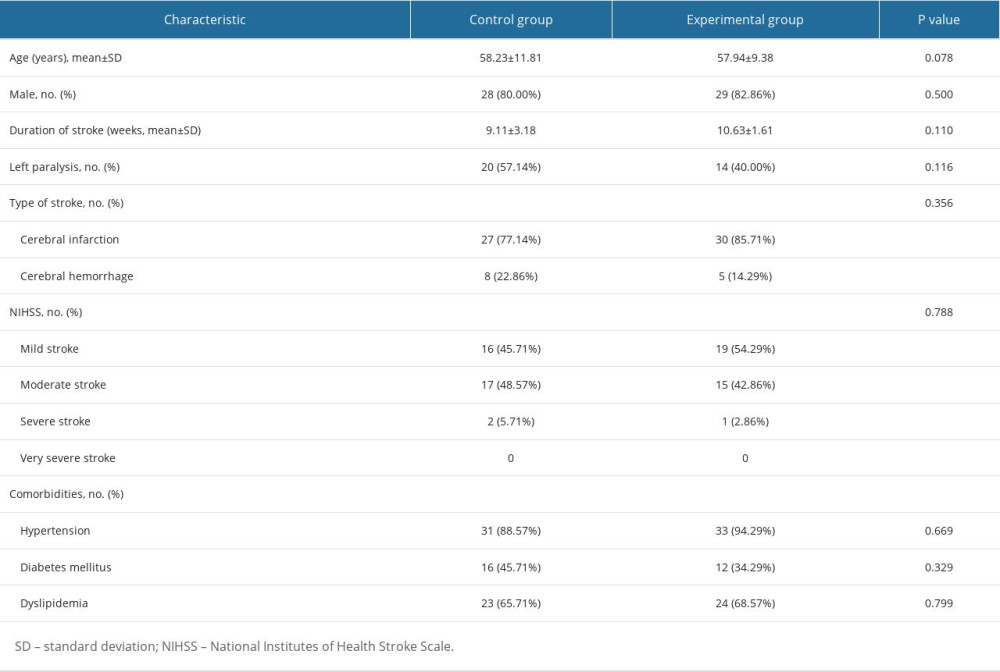 Table 1. Participant characteristics at baseline (n=35).
Table 1. Participant characteristics at baseline (n=35).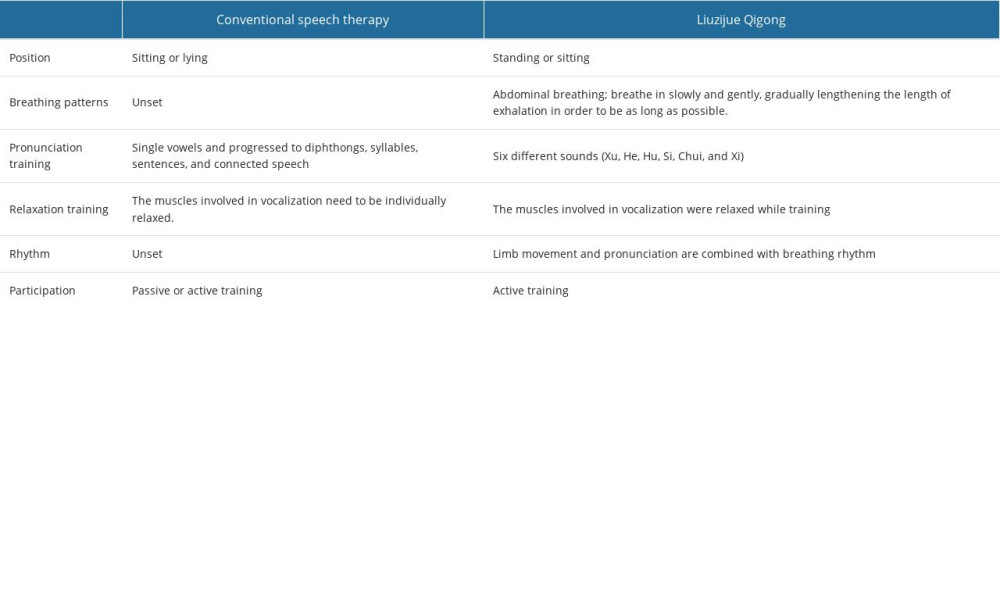 Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.
Table 2. Description and comparison of conventional speech therapy and Liuzijue Qigong.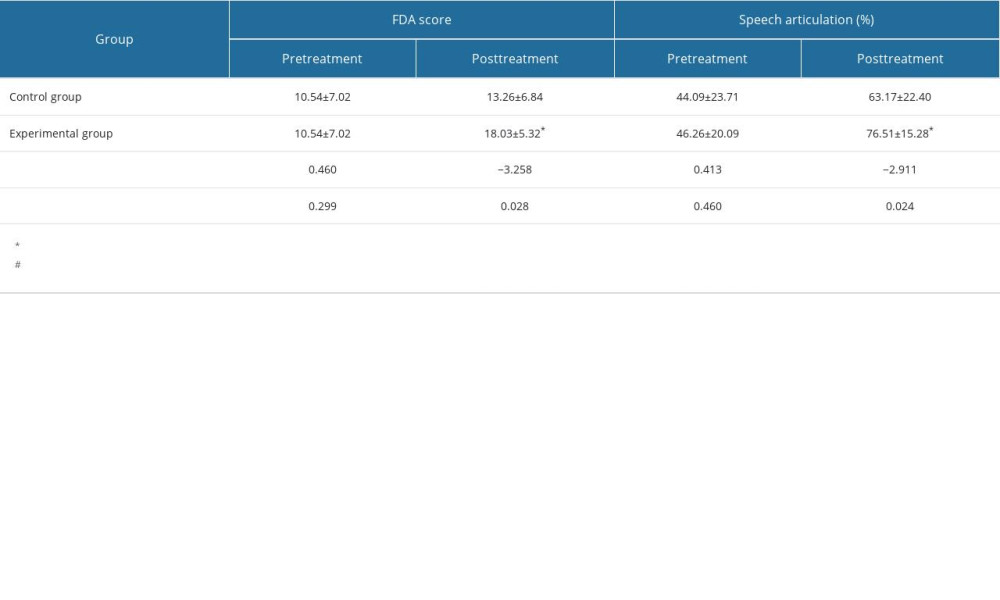 Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).
Table 3. Comparison of Frenchay Dysarthria Assessment (FDA) and speech articulation (mean±standard deviation, n=35).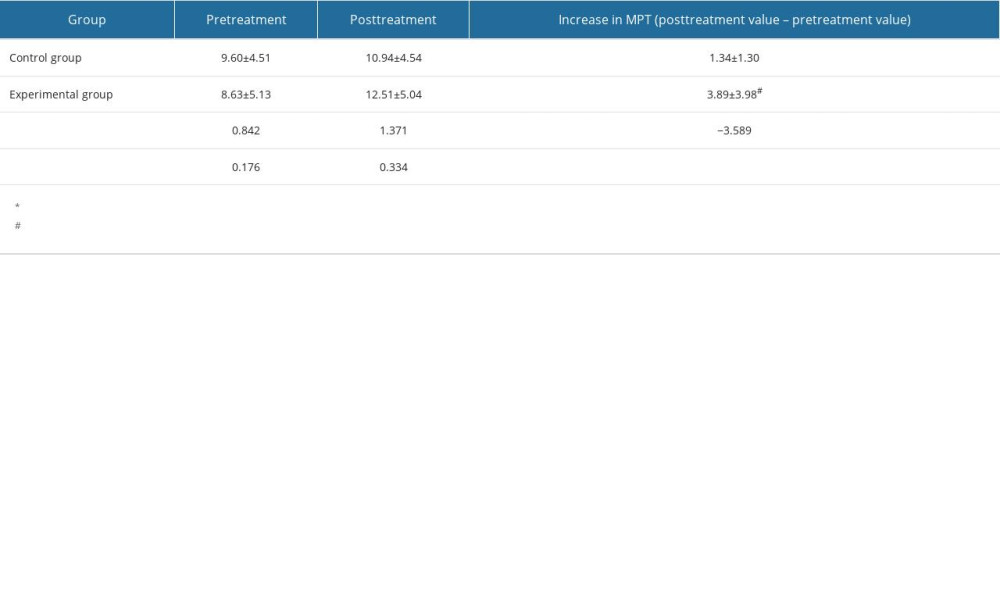 Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35).
Table 4. Comparison of maximum phonation time (MPT) duration (in seconds) between the 2 groups before and after treatment (mean±standard deviation, n=35). Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups.
Table 5. Comparison of the pretreatment and posttreatment loudness in calm communication (dB; mean±standard deviation; n=35) between the 2 groups. Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35).
Table 6. Comparison of the pretreatment and posttreatment Montreal Cognitive Assessment scale scores between the 2 groups (mean±standard deviation, n=35). In Press
07 May 2024 : Clinical Research
Treatment of AVN-Induced Proximal Pole Scaphoid Nonunion Using a Fifth and Fourth Extensor Compartmental Ar...Med Sci Monit In Press; DOI: 10.12659/MSM.944553
16 Mar 2024 : Clinical Research
Diagnostic Efficiency of ACR-TIRADS Score for Differentiating Benign and Malignant Thyroid Nodules of Vario...Med Sci Monit In Press; DOI: 10.12659/MSM.943228
08 May 2024 : Clinical Research
Effect of Individualized PEEP Guided by Driving Pressure on Diaphragm Function in Patients Undergoing Lapar...Med Sci Monit In Press; DOI: 10.12659/MSM.944022
21 Mar 2024 : Clinical Research
Impact of Serum Vitamin D, B6, and B12 and Cognitive Functions on Quality of Life in Peri- and Postmenopaus...Med Sci Monit In Press; DOI: 10.12659/MSM.943249
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952