25 October 2023: Clinical Research
Improving Bowel Function Recovery and Quality of Life in Han Chinese Patients with Spinal Cord Injuries: A Quantitative Assessment-Based Nursing Intervention Study
Xiaohong TaoDOI: 10.12659/MSM.939695
Med Sci Monit 2023; 29:e939695
Abstract
BACKGROUND: Neurological bowel dysfunction (NBD) due to spinal cord injuries (SCIs) is common and significantly impacts patients’ quality of life. This study evaluated the efficacy of quantitative assessment-based nursing interventions on bowel function recovery, quality of life, and caregivers’ satisfaction with SCI patients with NBD.
MATERIAL AND METHODS: The study included 418 SCI patients with NBD. Patients were categorized into 3 cohorts: quantitative assessment-based nursing intervention (QN, n=114), conventional nursing intervention (CN, n=125), or no nursing intervention (DN, n=189). The 3 cohorts were followed over a 6-month period.
RESULTS: At 6 months post-intervention, patients in the QN and CN cohorts showed significant reductions in symptoms of fecal incontinence, constipation, and abdominal distension compared to the DN cohort. Additionally, defecation time decreased significantly in the QN and CN cohorts compared to both initial measures and the DN cohort. Notably, patients in the QN cohort demonstrated substantial improvement in overall quality of life scores compared to baseline, CN, and DN cohorts. The QN cohort also reported marked improvement in caregivers’ satisfaction, surpassing that of caregivers in the CN and DN cohorts.
CONCLUSIONS: Six months of quantitative assessment-based nursing interventions significantly improved bowel function, quality of life, and caregiver satisfaction in SCI patients with NBD. This intervention appears beneficial for managing NBD in SCI patients and improving their quality of life and caregiver satisfaction.
Keywords: Constipation, Defecation, Fecal Incontinence, Quality of Life, Spinal Cord Injuries, Standardized Nursing Terminology, Humans, East Asian People, Intestines, Recovery of Function, Intestinal Diseases
Background
Neurological bowel dysfunctions are common and generally occurred in 70% to 80% of patients after spinal cord injuries4[1,2]. Severe bowel dysfunctions in patients with spinal cord injuries have worse effects on the quality of life of patients [3–5]. Persistent bowel dysfunctions lead to other complications, for example, urinary incontinence, constipation, and uncoordinated defecation [6,7]. Social [8] and economic [9] factors are also associated with the worse quality of life due to spinal cord injuries.
Generally, clinicians focus on treatments of intestinal functions [10]. However, it is necessary to focus on effective non-treatment intervention(s) to improve the quality of life of patients after spinal cord injuries. Nursing non-treatment intervention(s) are helpful in the improvement of the quality of life of patients after spinal cord injuries [11]. Conventional nursing non-treatment intervention(s) focuses on the basics and treatment of disease(s) [10], but do not consider the effects and severity of diseases on the quality of life of patients with spinal cord injuries [12]. Therefore, conventional nursing non-treatment intervention(s) is not sufficient to improve the quality of life of patients with spinal cord injuries. Quantitative assessment-based nursing non-treatment intervention(s) could improve bowel functions and the quality of life of patients with spinal cord injuries [10,12].
The objectives of this longitudinal study were an assessment of recovery of bowel functions, quality of life, and caregivers’ satisfaction of Han Chinese patients with spinal cord injuries from Shaoxing, Zhejiang province, China with neurological bowel dysfunctions due to spinal cord injuries who received quantitative assessment-based nursing non-treatment interventions compared with those of patients with spinal cord injuries who received conventional nursing non-treatment interventions for rehabilitation.
Material and Methods
ETHICS APPROVAL AND CONSENT TO PARTICIPATE:
The designed protocol of the established study was approved by the institutional review board. The study follows the law of China. Informed consent was not required throughout the study.
INCLUSION CRITERIA:
Patients who had ischemic or traumatic spinal cord injuries and neurological bowel dysfunctions after spinal cord injuries and were available at rehabilitation center of institutes were included in the study.
EXCLUSION CRITERIA:
Patients who had not completed the non-treatment intervention(s) were excluded from the study.
SAMPLE SIZE CALCULATION:
On basis of the assumption that besides conventional nursing interventions, quantitative assessment-based nursing interventions improved bowel functions in 20% of patients, 90% of power, β=0.1, and α=0.05, the sample size (minimum patients required in each cohort) was 100.
COHORTS:
A total of 114 patients received quantitative assessment-based non-treatment nursing interventions for 6 months (QN cohort). A total of 125 patients received conventional non-treatment nursing interventions for 6 months (CN cohort). A total of 189 patients did not receive any kind of nursing intervention and they received education materials only (DN cohort). Non-treatment nursing interventions were provided for rehabilitations of patients in the centers. Continuous follow-up was performed by nursing staff of the institute.
CONVENTIONAL NON-TREATMENT NURSING INTERVENTIONS:
Conventional non-treatment nursing interventions included education regarding disease(s) and psychological nursing. Patients were instructed to eat fruits, vegetables, food containing higher dietary fibers, drink more water, and eat less gas-producing materials.
QUANTITATIVE ASSESSMENT-BASED NON-TREATMENT NURSING INTERVENTIONS:
Based on the severity of dysfunction(s), patients were divided into mild, moderate, and severe conditions of dysfunction(s). For 3 patients with mild dysfunction(s), 1 nurse was allocated, for 2 patients with moderate- dysfunction(s) 1 nurse was allocated, and for 1 patient with severe dysfunction(s) 1 nurse was allocated. Patients received non-treatment nursing interventions according to the severity of dysfunction(s). Patients were educated regarding disease(s) and psychological nursing. Patients were instructed to eat fruits, vegetables, and food containing higher dietary fibers, drink more water, and eat less gas-producing materials (like conventional nursing). Patients were instructed to drink at least 2 L of water per day. Nurses provided abdominal massages to speed defecation. Massages were provided to the patients in supine positions. Twenty minutes of abdominal massage for improving bowel dysfunction was performed every day. Nurses guided patients in exercises of abdominal muscles (lumbar stabilization exercise). Deep breathing and abdominal breathing were used for exercises of abdominal muscles. Patients were guided for exercises of anal contraction (spreading of legs of patients safely, try to squeeze pelvic floor muscles). Anal action was implemented by nurses daily for 2 min. Anal action included lubrication of the anus with liquid paraffin.
DEMOGRAPHICAL AND CLINICAL PARAMETERS:
Demographical and clinical parameters of patients were collected from patients’ hospital records.
BOWEL DYSFUNCTIONS: Patients were questioned before intervention(s) and 6 months after intervention(s). Fecal incontinence was defined as unplanned defecation outside of bowel maintenance time. Straining more than one-quarter of stools and/or lumpy or hard stools were considered constipation. Expansion of the abdomen due to gas or fluid was considered abdominal distension. The time for bowel evacuation (defecation time) was evaluated [7].
QUALITY OF LIFE: The 36-Item Short-form Health Survey (SF-36) Chinese version [13] was used for evaluation of quality of life of patients with spinal cord injuries. A trained instructor evaluated the quality of life of patients. Overall, of quality of life of patients of all dimensions was evaluated. The score for overall quality of life ranges from 0 to 100. A higher score indicates higher quality of life.
CAREGIVERS’ SATISFACTION: The Caregivers’ Satisfaction with Stroke Care Questionnaire was used for the evaluation of caregivers’ satisfaction [14]. Overall, the personal satisfaction of patients’ caregivers of all dimensions was evaluated. The score ranged from 0 to 4, scored as 0: unsatisfied, 1: mild satisfied, 2: moderately satisfied, 3: moderately to fully satisfied, and 4: fully satisfied.
STATISTICAL ANALYSIS:
InStat 3.01 GraphPad, Software, San Diego, CA, USA was used for statistical analysis. The chi-square test (χ2 test) or Fisher’s exact test was used for statistical analysis of categorical data. The Kolmogorov-Smirnov test was used to check the linearity of continuous or ordinal data. Bartlett’s test was used to check the linearity of standard deviations (SDs) of continuous or ordinal data. One-way analysis of variance (ANOVA) was used for linear continuous or ordinal data for statistical analysis. The Kruskal-Wallis test was used for non-linear continuous or ordinal data for statistical analysis. Dunn’s multiple comparisons test was used for post hoc analysis of non-linear continuous or ordinal data. All results were considered significant if the
Results
STUDY POPULATION:
From 11 January 2011 to 15 January 2021, a total of 433 patients with neurological bowel dysfunctions due to spinal cord injuries (ischemic or traumatic) from Shaoxing, Zhejiang province, China, and outside the province were available at the Affiliated Hospital of Shaoxing University, Shaoxing, Zhejiang, China, and the referring hospitals. Among 433 patients, 15 patients had started non-treatment intervention(s) but did not complete them; therefore, they were excluded from the study. Data on bowel dysfunctions and quality of life of 418 patients from Shaoxing, Zhejiang province, China with spinal cord injuries and their caregivers’ satisfaction were included in the analysis. The summary chart is presented in Figure 1.
FOR PATIENTS: Age, gender, problems associated with bowel care, overall quality of life score before the intervention, type of spinal cord injuries, and marital status of patients were comparable among cohorts (P>0.05 for all). Traumatic spinal cord injuries were mostly caused by falls and motor vehicle accidents (Table 1).
FOR CAREGIVERS: There were fewer female caregivers than male caregivers. Caregivers were younger than patients. Caregivers were generally relatives of patients. Gender, age, and education levels of caregivers, and caregivers’ satisfaction before intervention were comparable among cohorts (P>0.05 for all). Caregivers’ satisfaction was mildly satisfied (unsatisfied-moderate satisfied, Table 2).
PROBLEMS ASSOCIATED WITH BOWEL CARE:
After 6 months, the number of patients with fecal incontinence, constipation, and abdominal distension decreased in the QN cohort (P<0.05 for all, χ2 test). After 6 months, the number of patients with constipation and abdominal distension decreased in the CN cohort (P<0.05 for both, χ2 test). After 6 months, the number of patients with fecal incontinence, constipation, and abdominal distension was not decreased in the DN cohort (P>0.05 for all, χ2 test). At 6 months after interventions, the numbers of patients with fecal incontinence, constipation, and abdominal distension were lower in the QN and the CN cohorts than in the DN cohort (P<0.05 for all, Fisher’s exact test). The defecation time was decreased after 6 months in all cohorts as compared to before non-treatment intervention(s) (P<0.05 for all, Kruskal-Wallis test/Dunn’s multiple comparisons test). The defecation time was shorter after 6 months in the QN and the CN cohorts as compared to the initial stages (before non-treatment intervention(s)) and those of the DN cohort (P<0.01 for all, Kruskal-Wallis test/Dunn’s multiple comparisons test). The defecation time of patients was shorter after 6 months in the CN cohort as compared to the DN cohort (P<0.05, Kruskal-Wallis test/Dunn’s multiple comparisons test). The details of the problems associated with the bowel care of patients are reported in Table 3.
QUALITY OF LIFE:
After 6 months, the overall quality of life score was higher for the QN, CN, and DN cohorts as compared to the initial stage (P 0.05 for all, Kruskal-Wallis’ test/Dunn’s multiple comparisons test). After 6 months, the overall quality of life score was higher in the QN cohort than in the CN and DN cohort as compared to the initial stage (P<0.001 for both, Kruskal-Wallis’ test/Dunn’s multiple comparisons test). After 6 months, the overall quality of life score increased for the CN cohort than those of the DN cohort (P<0.001, Kruskal-Wallis test/Dunn’s multiple comparisons test). The overall quality of life score is presented in Figure 2.
CAREGIVERS’ SATISFACTION:
After 6 months, caregivers’ satisfaction scores increased for the QN and the CN cohorts as compared to the initial stage (P<0.05 for both, Kruskal-Wallis test/Dunn’s multiple comparisons test). After 6 months, caregivers’ satisfaction scores increased more for the QN cohort than those of the CN and the DN cohorts (P<0.001 for both, Kruskal-Wallis test/Dunn’s multiple comparisons test). After 6 months, caregivers’ satisfaction scores were not higher in the CN cohort than in the DN cohort (P>0.05, Kruskal-Wallis test/Dunn’s multiple comparisons test). The caregivers’ satisfaction scores are presented in Figure 3.
Discussion
After 6 months of non-treatment intervention(s), problems associated with bowel care were decreased for patients with spinal cord injuries who received quantitative assessment-based non-treatment nursing interventions. The results of the bowel function of the current study were consistent with those of a randomized trial [12], but the randomized trial had a small sample size and a deficiency in study design. The role of the abdominal and pelvic muscles is important in effective bowel movements [15]. Nurses provided abdominal massages during quantitative assessment-based non-treatment nursing interventions, which improve bowel movement [12]. Six months of quantitative assessment-based non-treatment nursing interventions improved the bowel function of patients with neurological bowel dysfunctions due to spinal cord injuries.
Constipation, abdominal distension, and defecation time were improved with conventional non-treatment nursing interventions. Eating fruits, vegetables, food containing higher dietary fibers, drinking more water, and eating less gas-producing materials improved constipation, abdominal distension, and defecation time. Changes in eating and drinking habits can improve the bowel functions of patients with spinal cord injuries.
After 6 months of non-treatment intervention(s), the overall quality of life was better for patients with spinal cord injuries who received quantitative assessment-based non-treatment nursing interventions than for those who received conventional non-treatment nursing interventions. The results of the quality of life of the current study were consistent with those of a randomized trial [12]. Improvement in bowel functions of patients with spinal cord injuries allow them to have more participation in social activities and better quality of life [16]. Six months of quantitative assessment-based non-treatment nursing interventions improve the quality of life of patients with neurological bowel dysfunctions due to spinal cord injuries.
After 6 months of non-treatment intervention(s), personal satisfaction was better for caregivers of patients with spinal cord injuries who received quantitative assessment-based non-treatment nursing interventions than in those who received conventional non-treatment nursing interventions. Satisfaction of caregivers is related to the formal care of the patient [17]. Improvement in patient health can increase the personal satisfaction of caregivers [4]. Six months of quantitative assessment-based non-treatment nursing interventions can improve the personal satisfaction of caregivers.
In a randomized trial [12], non-treatment nursing interventions were provided during the hospital stay of patients with spinal cord injuries. Moreover, in a longitudinal, prospective cohort study [4], non-treatment nursing interventions were provided for 1.5 years for patients with spinal cord injuries. However, the current study provided 6 months of non-treatment nursing interventions. Patients in the current study were comparatively older (55 years: median value) and required more non-treatment nursing interventions than those younger patients [18]. Also, 1.5 years of non-treatment nursing interventions are not required for better clinical outcomes because patients with spinal cord injuries included in the study had worsened bowel functions and quality of life, and had worsened satisfaction of caregivers of patients with spinal cord injuries due to the severity of diseases [4]. A total of 6 months of non-treatment nursing interventions are required for better clinical outcomes for patients with spinal cord injuries, problems associated with bowel functions, and worse quality of life.
Caregivers’ satisfaction was worse before non-treatment nursing interventions. Most caregivers were male and caregivers may have difficult challenges and have decreased physical and/or psychological health [19] because most males from Shaoxing, Zhejiang province, China were had professional responsibilities. Caregivers of Han Chinese patients from Shaoxing, Zhejiang province, China with spinal cord injuries had low satisfaction.
All included patients before the intervention(s) had an overall quality of life score of ~50. Moderate to large disability is associated with less happiness and lower quality of life [20]. The included patients had recent bowel dysfunctions (~4-week history). Therefore, they were unable to adapt to the situation they faced.
The limitations of the study include its retrospective design and lack of randomization. The date of recruiting patients ranges from 10 years because participating institutes did not have enough patients in a short time. The study did not include any patients from Mongolia, Tibet, or rural or suburban regions. The Han Chinese patients included in the study were mainly from Shaoxing, Zhejiang province, China, and some patients lived outside the province. The results of our study may not be generalizable to other populations.
Conclusions
Six months of quantitative assessment-based non-treatment nursing interventions improved the bowel functions, the quality of life, and personal satisfaction of caregivers of Han Chinese patients from Shaoxing, Zhejiang province, China with neurological bowel dysfunctions due to spinal cord injuries. Changes in eating and drinking habits may improve the bowel functions of patients with spinal cord injuries. A total of 6 months of non-treatment nursing interventions are required for better clinical outcomes for patients with spinal cord injuries, problems associated with bowel functions, and worse quality of life. Caregivers of Han Chinese patients from Shaoxing, Zhejiang province, China with neurological bowel dysfunctions due to spinal cord injuries had low satisfaction levels.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Figures
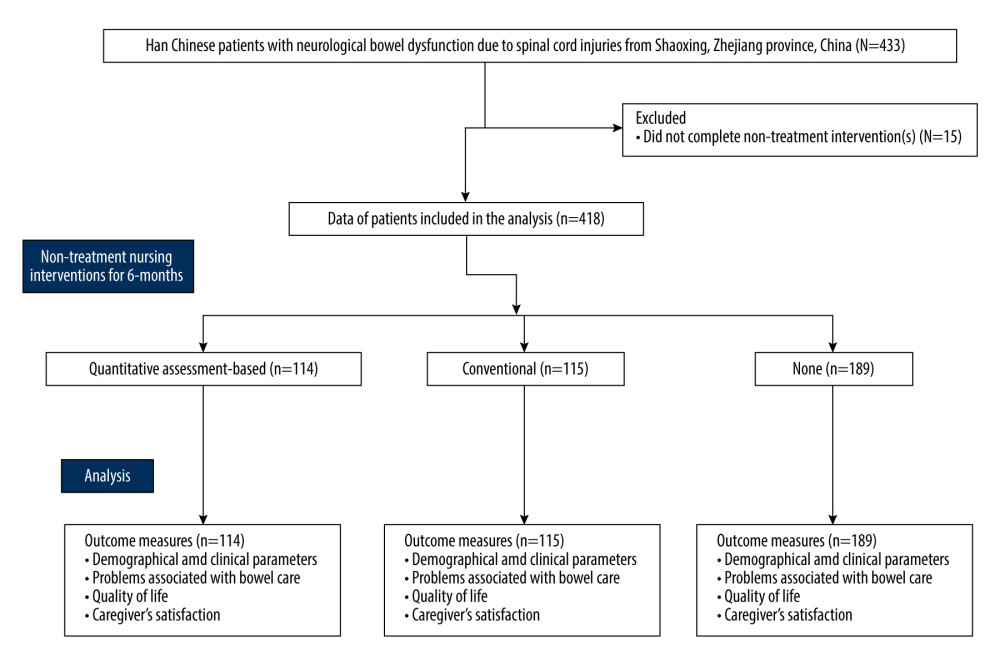 Figure 1. The summary chart of the study.
Figure 1. The summary chart of the study. 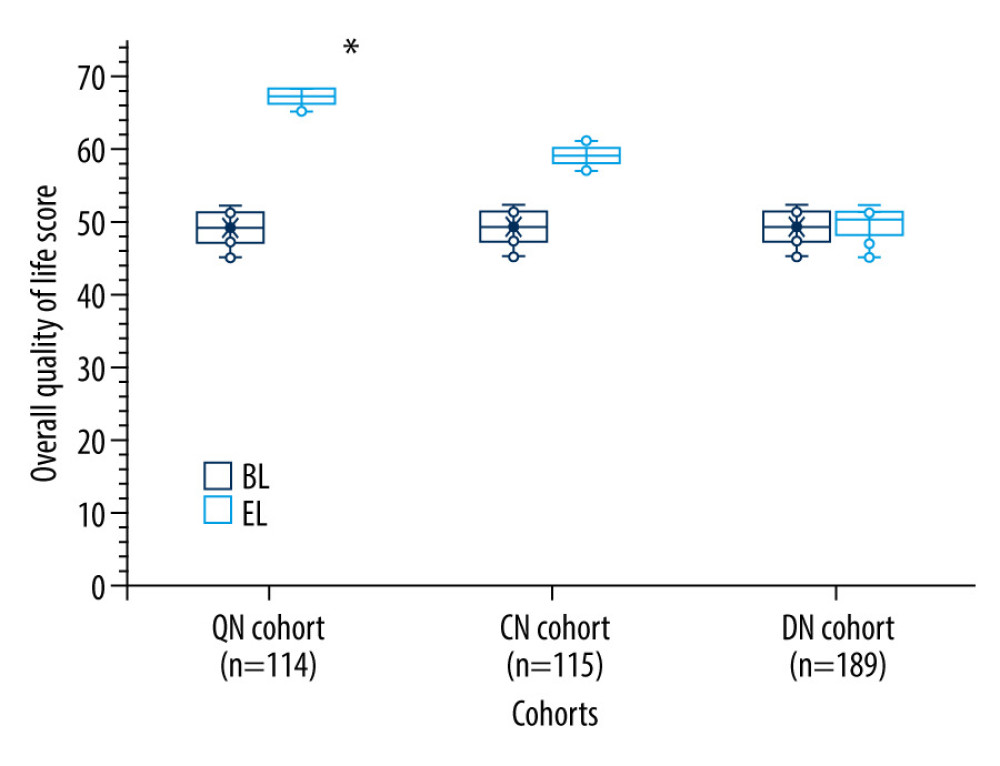 Figure 2. The overall quality of life score. The score for overall quality of life ranges from 0 to 100. The higher the score, the higher the quality of life. * Higher than those of the CN and the DN cohorts.
Figure 2. The overall quality of life score. The score for overall quality of life ranges from 0 to 100. The higher the score, the higher the quality of life. * Higher than those of the CN and the DN cohorts. 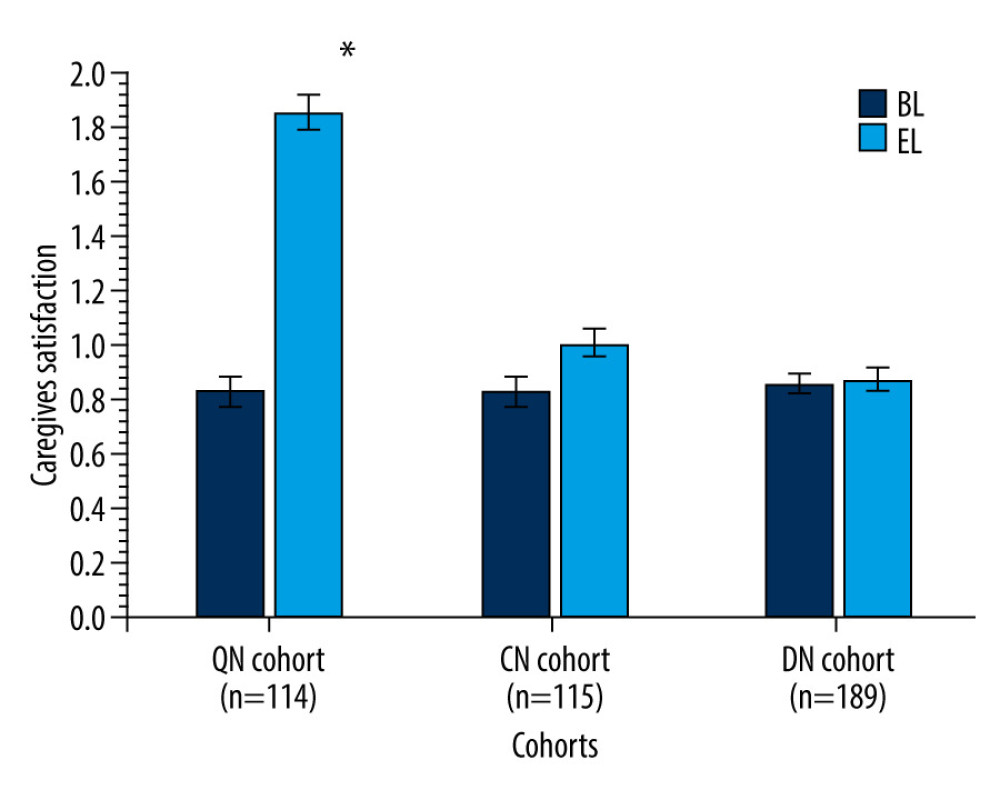 Figure 3. Caregivers’ satisfaction. Data are presented as mean±standard error. 0: unsatisfied, 1: mildly satisfied, 2: moderately satisfied, 3: moderately to fully satisfied, and 4: fully satisfied. * Higher than those of the CN and the DN cohorts.
Figure 3. Caregivers’ satisfaction. Data are presented as mean±standard error. 0: unsatisfied, 1: mildly satisfied, 2: moderately satisfied, 3: moderately to fully satisfied, and 4: fully satisfied. * Higher than those of the CN and the DN cohorts. References
1. Qi Z, Middleton JW, Malcolm A, Bowel dysfunction in spinal cord injury: Curr Gastroenterol Rep, 2018; 20(10); 47
2. Holmes GM, Blanke EN, Gastrointestinal dysfunction after spinal cord injury: Exp Neurol, 2019; 320; 113009
3. Gómara-Toldrà N, Sliwinski M, Dijkers MP, Physical therapy after spinal cord injury: A systematic review of treatments focused on participation: J Spinal Cord Med, 2014; 37(4); 371-79
4. Backx APM, Spooren AIF, Bongers-Janssen HMH, Bouwsema H, Quality of life, burden and satisfaction with care in caregivers of patients with a spinal cord injury during and after rehabilitation: Spinal Cord, 2018; 56(9); 890-99
5. Zürcher C, Tough H, Fekete CSwiSCI Study Group, Mental health in individuals with spinal cord injury: The role of socioeconomic conditions and social relationships: PLoS One, 2019; 14(2); e0206069
6. Pires JM, Ferreira AM, Rocha F, Assessment of neurogenic bowel dysfunction impact after spinal cord injury using the International Classification of Functioning, Disability and Health: Eur J Phys Rehabil Med, 2018; 54(6); 873-79
7. Ozisler Z, Koklu K, Ozel S, Unsal-Delialioglu S, Outcomes of bowel program in spinal cord injury patients with neurogenic bowel dysfunction: Neural Regen Res, 2015; 10(7); 1153-58
8. Newman SD, Li C, Krause JS, Social isolation after spinal cord injury: Indicators from the Longitudinal Aging Study: Rehabil Psychol, 2016; 61(4); 408-16
9. Squair JW, White BA, Bravo GI, The economic burden of autonomic dysreflexia during hospitalization for individuals with spinal cord injury: J Neurotrauma, 2016; 33(15); 1422-27
10. Yin Q, Wang C, Yu J, Zhang Q, Quantitative assessment-based nursing intervention improves bowel function in patients with neurogenic bowel dysfunction after spinal cord injury: Study protocol for a randomized controlled study: Medicine, 2020; 99(51); e23354
11. Coggrave M, Norton C, Wilson-Barnett J, Management of neurogenic bowel dysfunction in the community after spinal cord injury: A postal survey in the United Kingdom: Spinal Cord, 2009; 47(4); 323-30
12. Zhang Y, Xia X, Zhuang X, Effect of quantitative assessment-based nursing intervention on the bowel function and life quality of patients with neurogenic bowel dysfunction after spinal cord injury: J Clin Nurs, 2018; 27(5–6); e1146-e51
13. Hu J, Gruber KJ, Hsueh KH, Psychometric properties of the Chinese version of the SF-36 in older adults with diabetes in Beijing, China: Diabetes Res Clin Pract, 2010; 88(3); 273-81
14. Shen YL, Zhang ZQ, Zhu LJ, Liu JH, Timing theory continuous nursing, resistance training: Rehabilitation and mental health of caregivers and stroke patients with traumatic fractures: World J Clin Cases, 2022; 10(5); 1508-16
15. Sharma A, Herekar A, Yan Y, Dyssynergic defecation and other evacuation disorders: Gastroenterol Clin North Am, 2022; 51(1); 55-69
16. Zhi-hua L, Fei G, Qing XDiagnosis and surgical treatment of adhesive intestinal obstruction after spinal cord injury: 35 Cases report: Chinese Journal of Rehabilitation Theory and Practice, 2015; 21(8); 982-85 in Chinese
17. Morishita M, Kamibeppu K, Quality of life and satisfaction with care among family caregivers of patients with recurrent or metastasized digestive cancer requiring palliative care: Support Care Cancer, 2014; 22(10); 2687-96
18. Hsieh CH, DeJong G, Groah S, Comparing rehabilitation services and outcomes between older and younger people with spinal cord injury: Arch Phys Med Rehabil, 2013; 94(4 Suppl); S175-S86
19. Adelman RD, Tmanova LL, Delgado D, Caregiver burden: A clinical review: JAMA, 2014; 311(10); 1052-60
20. Lucas RE, Long-term disability is associated with lasting changes in subjective well-being: Evidence from two nationally representative longitudinal studies: J Pers Soc Psychol, 2007; 92(4); 717-30
Figures
 Figure 1. The summary chart of the study.
Figure 1. The summary chart of the study.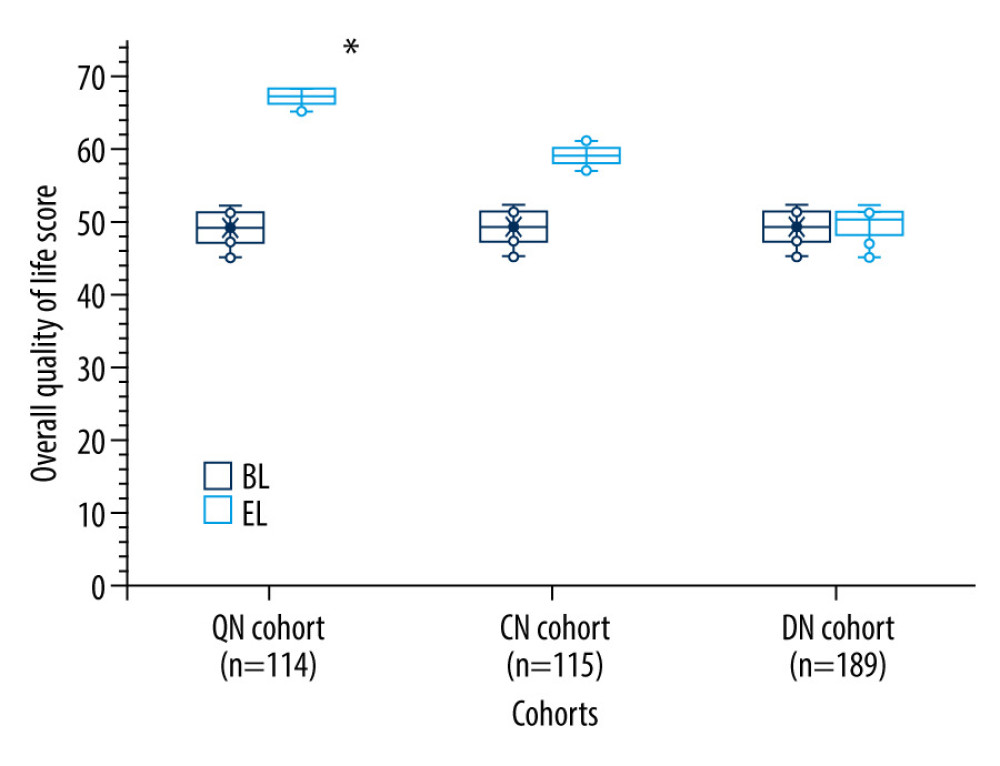 Figure 2. The overall quality of life score. The score for overall quality of life ranges from 0 to 100. The higher the score, the higher the quality of life. * Higher than those of the CN and the DN cohorts.
Figure 2. The overall quality of life score. The score for overall quality of life ranges from 0 to 100. The higher the score, the higher the quality of life. * Higher than those of the CN and the DN cohorts.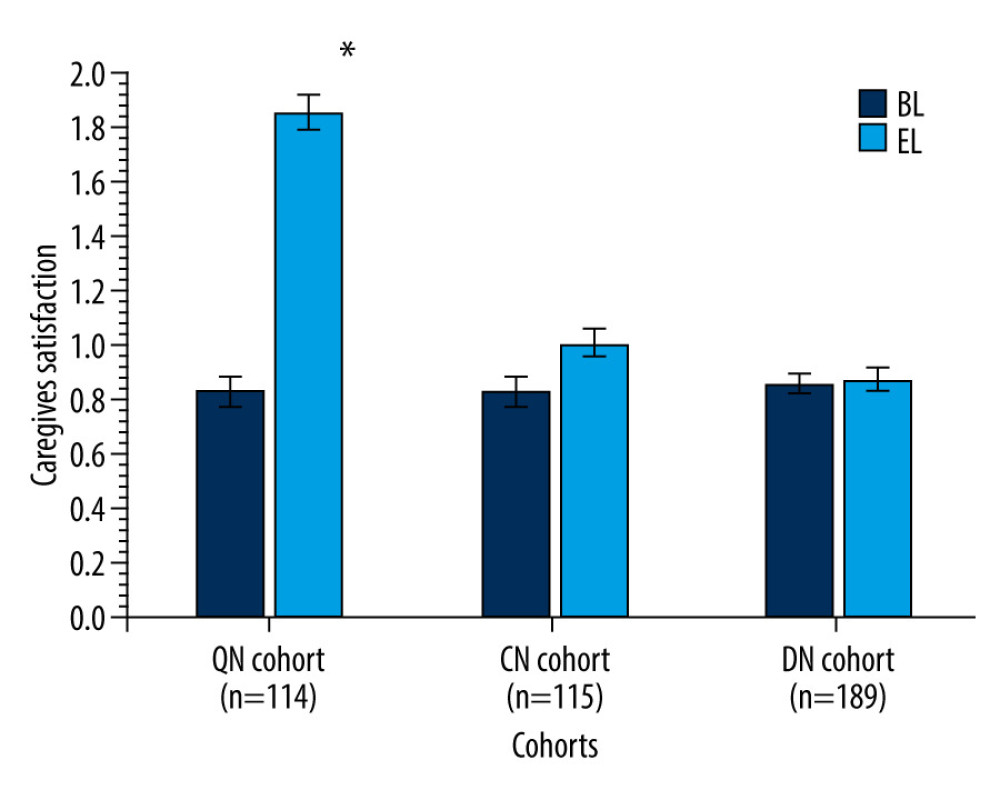 Figure 3. Caregivers’ satisfaction. Data are presented as mean±standard error. 0: unsatisfied, 1: mildly satisfied, 2: moderately satisfied, 3: moderately to fully satisfied, and 4: fully satisfied. * Higher than those of the CN and the DN cohorts.
Figure 3. Caregivers’ satisfaction. Data are presented as mean±standard error. 0: unsatisfied, 1: mildly satisfied, 2: moderately satisfied, 3: moderately to fully satisfied, and 4: fully satisfied. * Higher than those of the CN and the DN cohorts. Tables
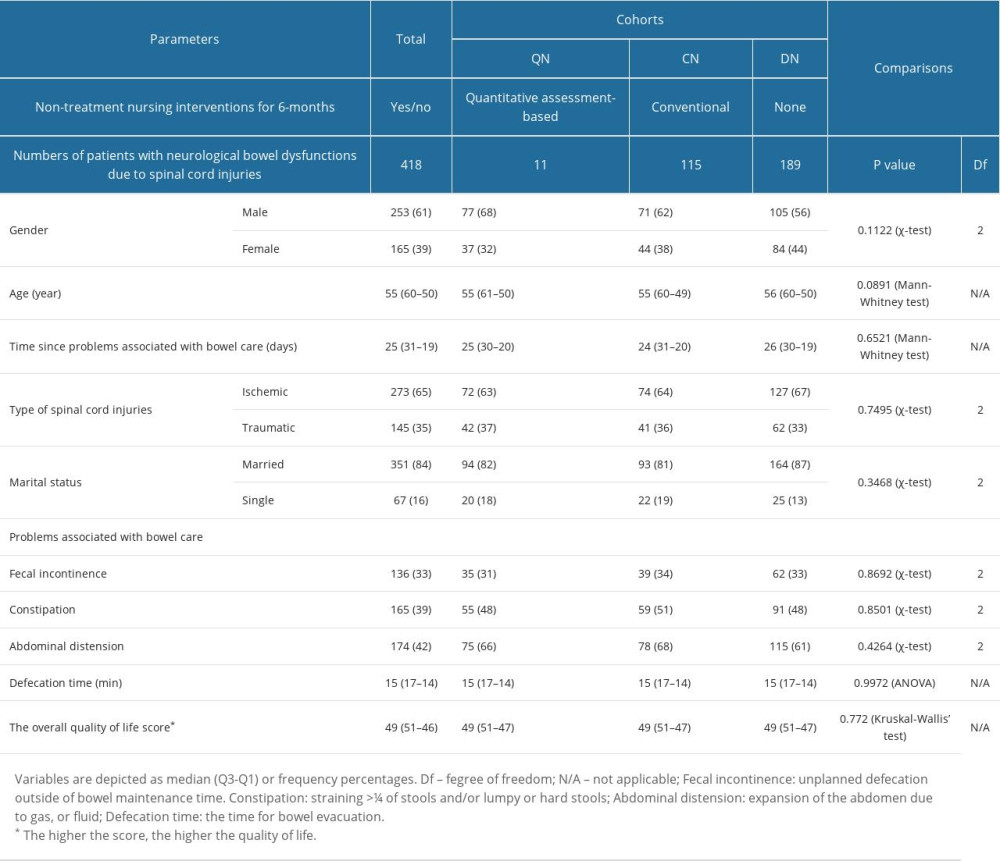 Table 1. Demographical, clinical, and social parameters of patients before non-treatment nursing interventions.
Table 1. Demographical, clinical, and social parameters of patients before non-treatment nursing interventions.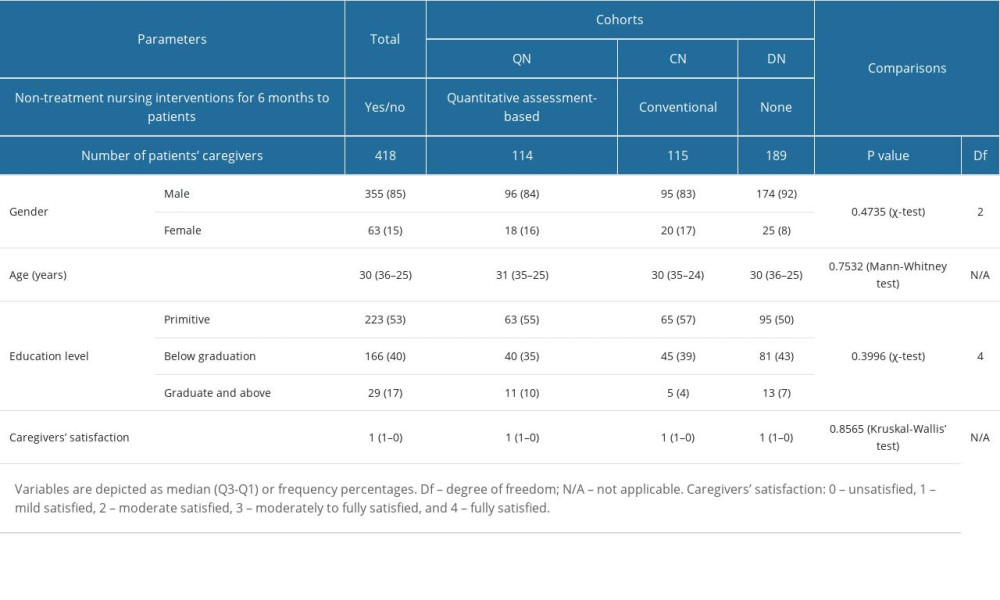 Table 2. Available parameters of patients’ caregivers before non-treatment nursing interventions.
Table 2. Available parameters of patients’ caregivers before non-treatment nursing interventions.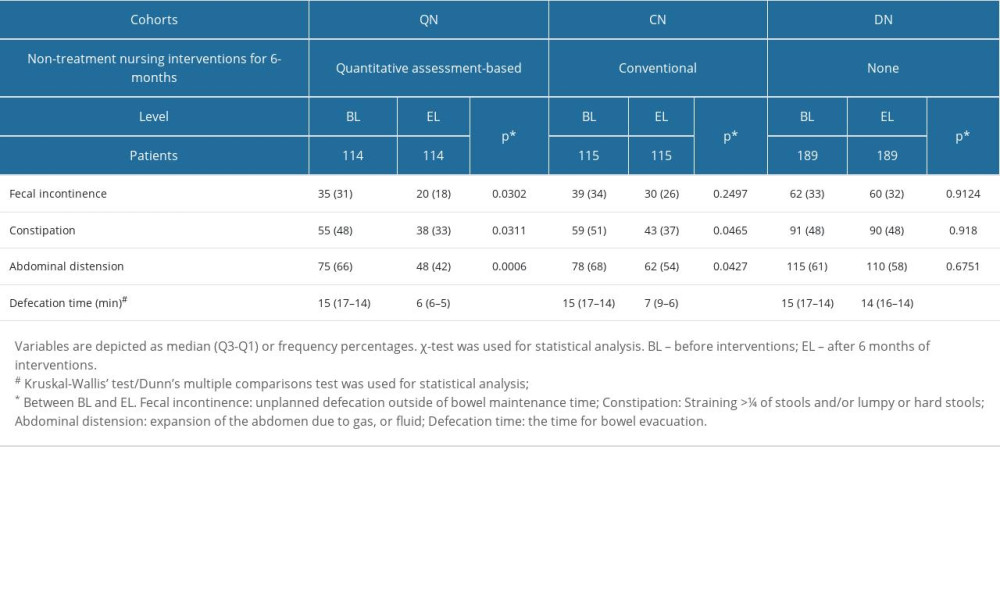 Table 3. Problems associated with bowel care.
Table 3. Problems associated with bowel care.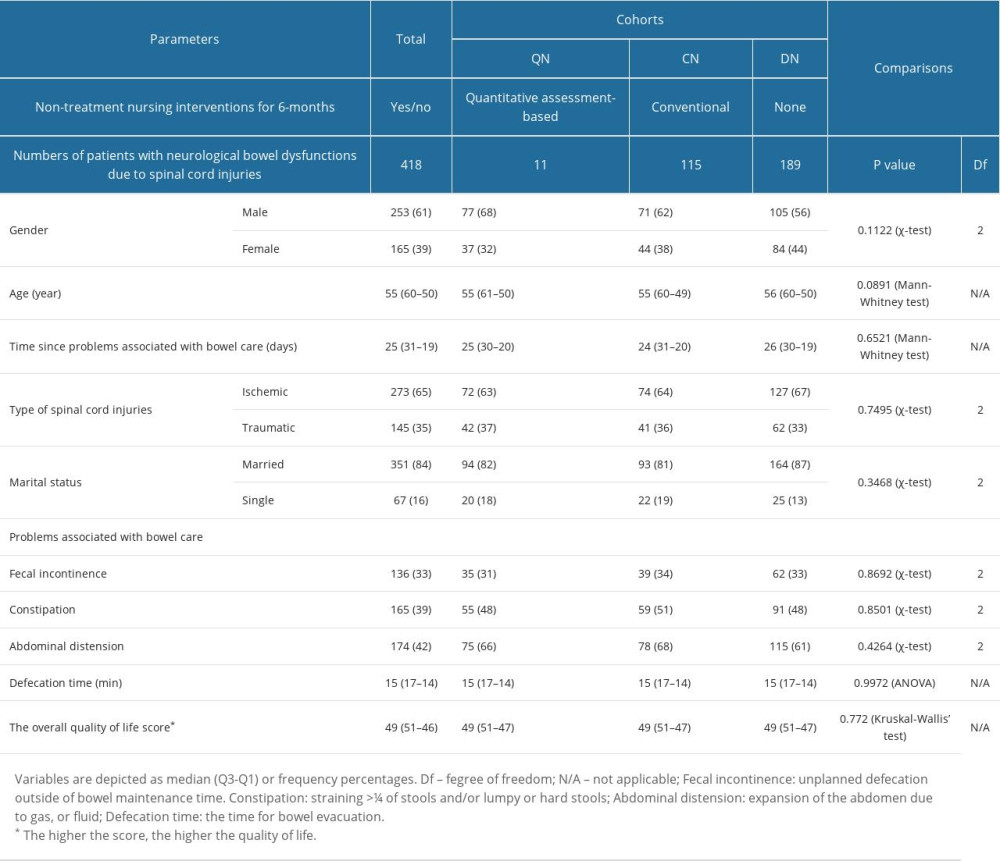 Table 1. Demographical, clinical, and social parameters of patients before non-treatment nursing interventions.
Table 1. Demographical, clinical, and social parameters of patients before non-treatment nursing interventions.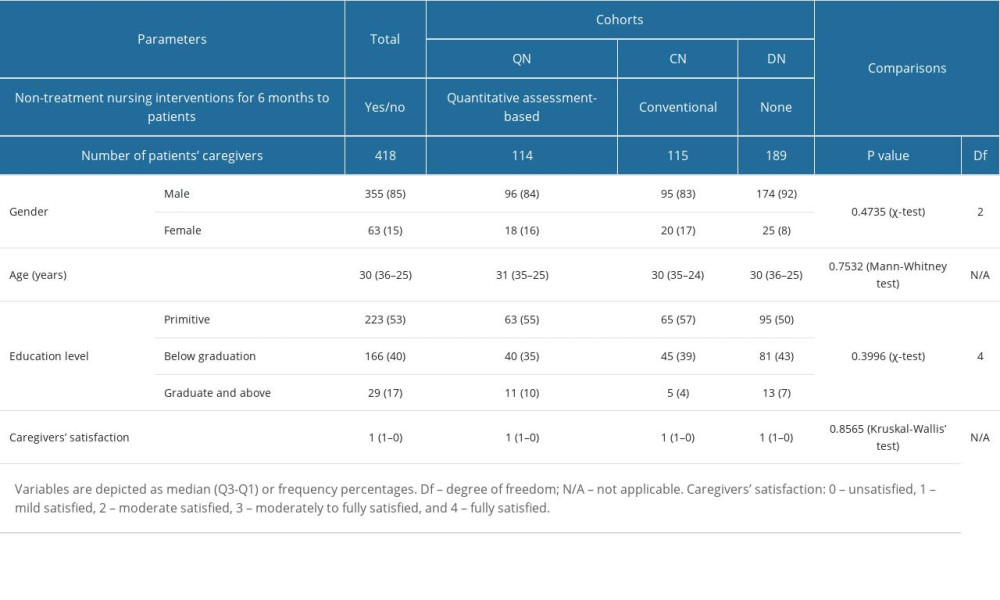 Table 2. Available parameters of patients’ caregivers before non-treatment nursing interventions.
Table 2. Available parameters of patients’ caregivers before non-treatment nursing interventions.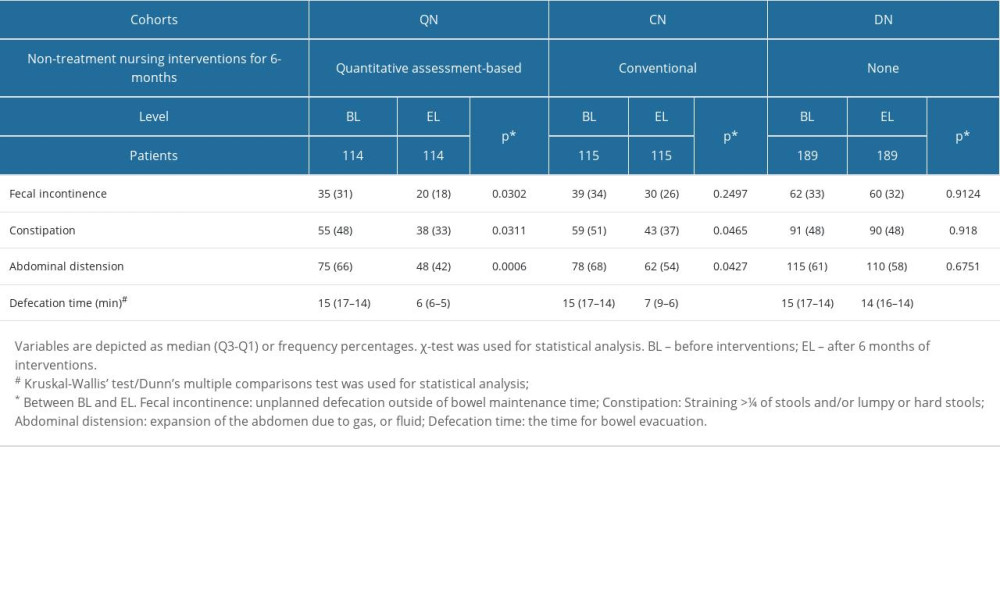 Table 3. Problems associated with bowel care.
Table 3. Problems associated with bowel care. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








