23 June 2023: Clinical Research
Comparative Analysis of Percutaneous Excision and Radiofrequency Ablation for Osteoid Osteoma
Ramazan Atiç1ABCDEFG*, Celil Alemdar2BC, Serhat Elçi3ABCDF, Abdurrahim Dusak4AB, Mehmet Akif Çaçan5ABCD, Emin Özkul1EFG, Mahmut Nedim AytekinDOI: 10.12659/MSM.940292
Med Sci Monit 2023; 29:e940292
Abstract
BACKGROUND: This retrospective study aims to compare the efficacy of computed tomography-guided percutaneous excision and radiofrequency ablation in the treatment of osteoid osteoma.
MATERIAL AND METHODS: We evaluated 40 patients with osteoid osteoma who underwent either percutaneous excision or radiofrequency ablation between 2012 and 2015. The cohort consisted of 10 female and 30 male patients, with a mean age of 15.1 years (range: 4-27 years) and a mean follow-up time of 19.02 months (range: 11-39 months). Percutaneous excision was performed in 20 patients, while radiofrequency ablation was performed in the remaining 20 patients.
RESULTS: The success rates of percutaneous excision and radiofrequency ablation were comparable, with unsuccessful outcomes observed in 10% and 5% of patients, respectively. The reasons for failure in the percutaneous excision group were attributed to a marking error and incomplete excision of the wide-based nidus. Complications were limited to pathological fracture (n=1) and deep infection (n=1) in the percutaneous excision group, while no complications were encountered in the radiofrequency ablation group.
CONCLUSIONS: Both percutaneous excision and radiofrequency ablation demonstrate high success rates in treating osteoid osteoma. However, radiofrequency ablation offers the advantage of a quicker return to daily activities without the need for activity restrictions or splints. While being a more cost-effective option, percutaneous excision should be considered cautiously to minimize potential complications.
Keywords: radiofrequency ablation, Osteoma, Osteoid, Orthopedic Procedures, Humans, Male, Female, Adolescent, Bone Neoplasms, Retrospective Studies, Catheter Ablation
Background
Osteoid osteoma (OO) is the most common benign bone tumor. It constitutes 10–12% of benign bone tumors and 2–3% of primary bone tumors. It predominantly affects men and usually occurs in the second or third decade of life [1]. This tumor, which has a low growth potential, is mostly smaller than 1 cm. Histologically, nidus was found in 85% of osteoid osteoma cases [2]. Osteoid osteoma is usually located in the long bones of the lower extremity (femur, tibia, fibula), but can occur in almost all bones in the body [3].
Pain, which increases especially at night and responds dramatically to aspirin therapy, is the main symptom of osteoid osteoma. Depending on the age of the patient and the location of the nidus, daily activities may be restricted, and gait and posture disorders may occur.
The first examination that should be applied in patients with suspected osteoid osteoma is plain radiography. Computed tomography (CT) is generally used to confirm the diagnosis. CT provides excellent information about the location and size of the nidus and the condition of the bony cortex. Magnetic resonance imaging (MRI) does not provide as clear information about the nidus as CT, but provides better information about bone marrow and soft-tissue edema, joint effusion, and synovitis [4]. In addition, MRI can be useful in differential diagnosis.
Open surgical methods such as curettage, en-bloc resection, and wide resection have been used in the treatment of this tumor for many years. The success of classical surgical methods is reported to be 88–100%. Minimally invasive treatment methods have been rapidly popularized due to the disadvantages of open surgery such as high complication rate (20–45%), long surgical time, tissue damage, scarring, and morbidity [5].
Recent studies have shown that CT-guided percutaneous RFA is beneficial and may be preferred for treatment of OO [6–9]. There are also studies showing the success and safety of CT-assisted percutaneous excision [10]. The aim of this study was to compare these 2 closed methods in terms of treatment success, complication rates, cost, and time to return to work.
Material and Methods
PARTICIPANTS:
In this study, 40 patients with osteoid osteoma who underwent computed tomography-guided percutaneous nidus excision or radiofrequency ablation between 2012 and 2015 were evaluated retrospectively. Ten of the patients were female and 30 were male. Mean age was 15.1 (range 4–27 years) and the mean follow-up time was 19.02 months (range 11–39 months).
Percutaneous excision was performed in 20 patients and radiofrequency ablation was performed in 20 patients.
In both groups, a total of 19 patients had nidus in the tibia and 15 in the femur (Table 1).
PROCEDURE:
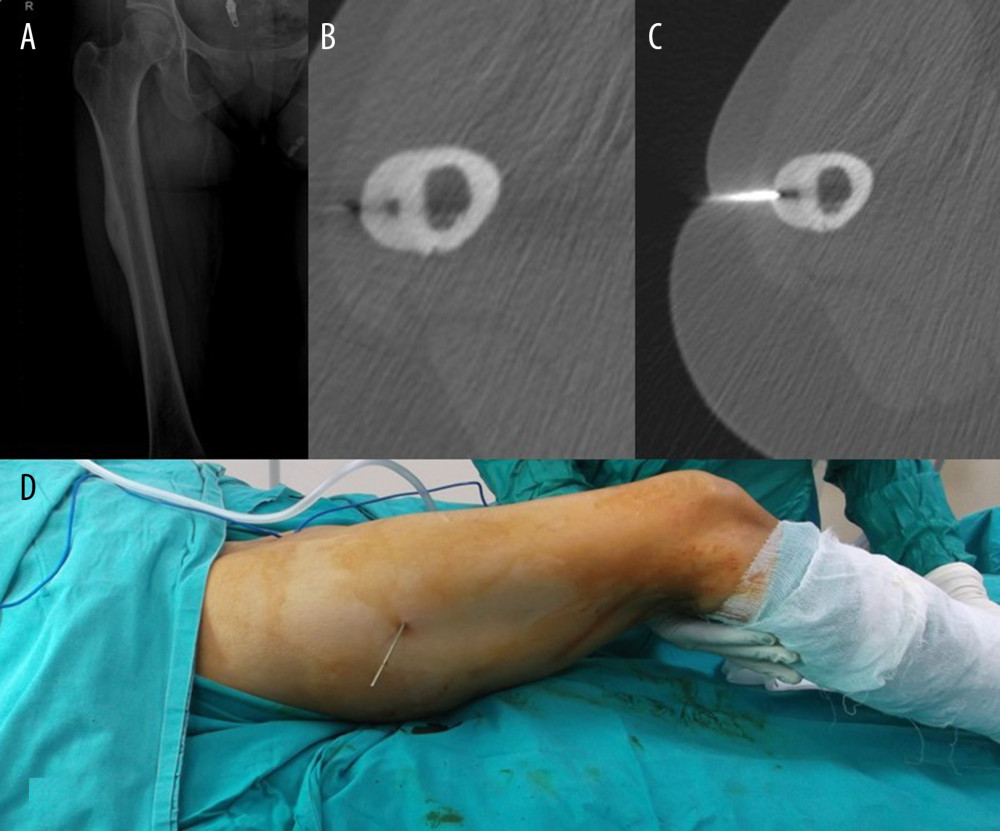
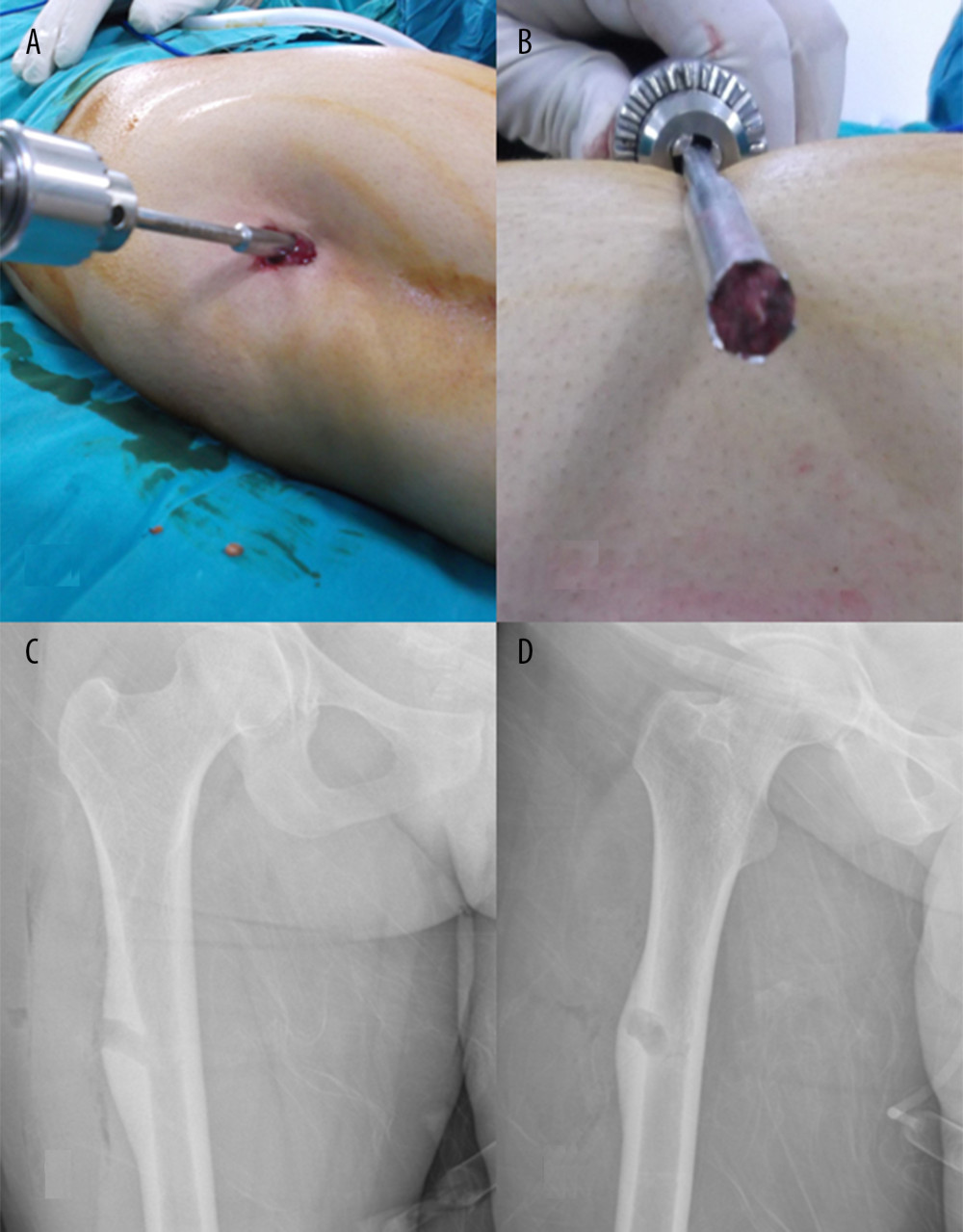
In percutaneous excision, a thin wire was sent towards the center of the nidus after the location of the nidus was determined under the guidance of tomography. The thick cortical frame, including the nidus, was cut in the form of a block with a trephine sent percutaneously over the wire (Figures 1, 2).
In patients who underwent, a bone biopsy needle or a thicker K wire than the radiofrequency probe was sent to the nidus under CT accompaniment. Afterwards, the radiofrequency probe was inserted into the nidus from the same channel. Care was taken to keep the active tip in the bone. Radiofrequency ablation was performed for 8 minutes at 85°.
In both groups, recurrence or persistent pain was considered an unsuccessful outcome.
Results
STATISTICAL ANALYSIS:
Unsuccessful results were obtained in 2 (10%) patients who underwent percutaneous excision and in 1 (5%) patient who underwent radiofrequency ablation. There was no statistically significant difference between the 2 methods in terms of success rate (p>0.05).
Discussion
Osteoid osteoma is a common benign bone tumor and the main goal of treatment is complete removal of the tumor without weakening the bone [6]. En-bloc resection is an effective method that has been used for a long time in osteoid osteoma. In the operations performed with the help of c-arm fluoroscopy, the incision is large, a large bone resection is performed, and post-procedure infection was associated with the risk of fracture. In addition, the length of hospital stays and the time required for weight bearing were longer. Errors in marking the lesion also brought the possibility of recurrence. In recent years, with the use of computed tomography in the treatment of osteoid osteoma, it has become possible to make more accurate marking with less bone resection, which requires less incision. Many methods such as CT-guided drilling, en-bloc resection, ethanol injection, radiofrequency ablation have been used. With these methods, smaller incisions, more accurate marking, lower morbidity, and shorter hospital stay have become possible [11–17].
First described in 2014, microwave ablation emits microwaves to thermally destroy the nidus. Under CT guidance, a needle is inserted into the lesion, and the microwaves produced by the needle create a small heat zone that heats and destroys the tumor [18,19]. Microwave ablation is less affected by tissue type or tissue impedance than radiofrequency ablation [20] and is quite successful [18].
Magnetic resonance guided focused ultrasound is a new imaging-guided technique that provides radiation-free treatment of osteoid osteoma. This method is an effective and safe alternative in the treatment of osteoid osteoma in both children and adults [21,22]. Geiger et al published the results of 29 patients with osteoid osteoma treated with this method, reporting 90% complete clinical success and 10% partial clinical success in patients [21].
In recent years, studies on CT-guided radiofrequency ablation method have become dominant in the literature. Rosenthal was the first to pave the way for the use of radiofrequency in the treatment of osteoid osteoma. Since then, this technique has achieved very good results in terms of efficacy and safety, so that percutaneous CT-guided radiofrequency ablation has become the standard therapeutic technique, replacing surgical treatment [14–16].
Also, compared to surgery, CT-guided radiofrequency ablation allows access to difficult anatomical sites and provides shorter operative and hospital stays [16]. In a comparative series of 24 patients by Goksel et al, 11 (45.83%) patients underwent surgical curettage and 13 (54.17%) radiofrequency ablation. The mean operative time was 69.5 minutes and the mean hospital stay was 1.3 days in the surgical resection group, while the mean operative time was 49.6 minutes and the mean hospital stay was 0.3 days in the radiofrequency ablation group. The length of hospital stay and procedure time were significantly shorter when compared with surgical resection [17].
The main problem with radiofrequency ablation is the high cost involved in the procedure as well as the need for specialized instrumentation and probes. Another disadvantage is that anatomical pathological confirmation is not possible, especially in suspicious cases. There was also a theoretical possibility of physical damage that would preclude the use of this method in lesions very close to the physis due to radiofrequency waves [23].
CT-guided percutaneous excision is an alternative surgical technique. A guide wire is sent to the nidus under CT guidance. Then, a small incision is made and the nidus is excised with the help of the trephine sent over the guide wire. Postoperative CT is performed to confirm that the nidus is completely drained. Finally, a pathological examination is performed to confirm the diagnosis. Correct placement of the needle in the nidus is very important as it reduces the amount of bone to be removed during surgery and reduces the risk of postoperative fracture [24,25]. The success rate of this method is 83–100% [26,27].
Engel et al showed a primary cure rate of 95% in their series of 15 patients. This success rate is similar to the success rates of other percutaneous CT-guided procedures. The resection segment is also very limited due to tomographic guidance. The recurrence rates are also comparable to other methods. With CT-guided percutaneous excision, the tumor can also be confirmed histopathologically. Another important advantage of this procedure is that its cost is extremely low. This surgery can only be performed using routine orthopedic instrumentation, and there is no need for any additional special devices [23–28].
The data we obtained in our study were compatible with the data in the literature. The success rate was 95% in the radiofrequency ablation group and 90% in the percutaneous excision group. In terms of complication rates, the 2 methods had similar results.
Conclusions
Both methods have a high success rate. However, patients who underwent radiofrequency ablation return to their daily lives earlier as there is no activity restriction or splint.
Although percutaneous excision therapy is less expensive and does not require special equipment, it may involve more hospitalizations and a higher risk of complications.
While percutaneous excision is a cheaper and easily accessible method, shorter hospital stay and earlier return to daily life are possible with radiofrequency ablation therapy. Both methods can be applied safely with a high success rate.
Tables
Table 1. Localization table.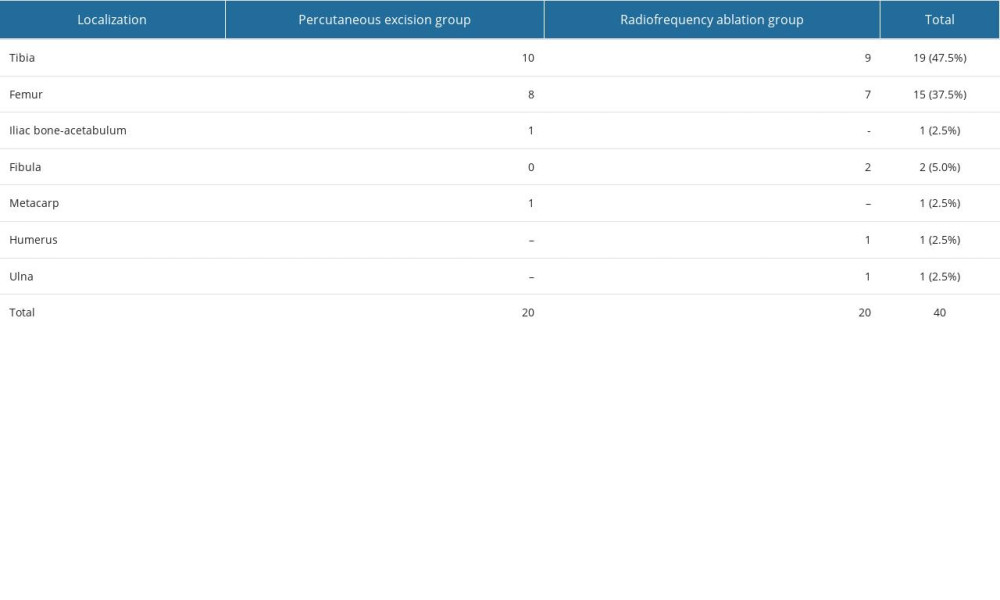
References
1. Dahlin DC, Unni KK: Bone tumors: General aspects and data on 8,542 cases, 1986, Springfield. Ill, USA, Charles C Thomas
2. Schulman L, Dorfman HD, Nerve fibers in osteoid osteoma: J Bone Joint Surg Am, 1970; 52(7); 1351-56
3. Mirra M, Gold RH, Picci P, Osseous tumors of intramedullary origin: Bone tumors: Clinical, Radiologic, and pathologic Correlations, 1989; 248-438, Philadelphia, Pa, USA
4. Davies M, Cassar-Pullicino VN, Davies AM, The diagnostic accuracy of MR imaging in osteoid osteoma: Skeletal Radiol, 2002; 31(10); 559-69
5. Cantwell CP, Obyrne J, Eustace S, Current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation: Eur Radiol, 2004; 14(4); 607-17
6. Rosenthal DI, Springfield DS, Gebhardt MC, Rosenberg AE, Mankin HJ, Osteoid osteoma: percutaneous radio-frequency ablation: Radiology, 1995; 197(2); 451-54
7. Parlier-Cuau C, Nizard R, Champsaur P, Osteoid osteoma of the acetabulum. Three cases treated by percutaneous resection: Clin Orthop Relat Res, 1999; 365; 167-74
8. Weber MA, Sprengel SD, Omlor GW, Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection: Skelet Radiol, 2015; 44(7); 981-93
9. Motamedi D, Learch TJ, Ishimitsu DN, Thermal ablation of osteoid osteoma: overview and step-by-step guide: Radiographics, 2009; 29(7); 2127-41
10. Reverte-Vinaixa MM, Velez R, Alvarez S, Percutaneous computed tomography-guided resection of non-spinal osteoid osteomas in 54 patients and review of the literature: Arch Orthop Trauma Surg, 2013; 133(4); 449-55
11. Lassalle L, Campagna R, Corcos G, Therapeutic outcome of CT-guided radiofrequency ablation in patients with osteoid osteoma: Skelet Radiol, 2017; 46(7); 949-56
12. Miyazaki M, Arai Y, Myoui A, Phase I/II multi-institutional study of percutaneous radiofrequency ablation for painful osteoid osteoma (JIVROSG0704): Cardiovasc Intervent Radiol, 2016; 39(10); 1464-70
13. Cioni R, Armillotta N, Bargellini I, CT-guided radiofrequency ablation of osteoid osteoma: Long-term results: Eur Radiol, 2004; 14(7); 1203-8
14. Rosenthal DI, Alexander A, Rosenberg AE, Springfield D, Ablation of osteoid osteomas with a percutaneously placed electrode: A new procedure: Radiology, 1992; 183(1); 29-33
15. Tordjman M, Perronne L, Madelin G, Mali RD, Burke C, CT-guided radiofrequency ablation for osteoid osteomas: A systematic review: Eur Radiol, 2020; 30(11); 5952-63
16. Parvinian A, Welch BT, Callstrom MR, Kurup AN, Trends in musculoskeletal ablation: emerging indications and techniques: Tech Vasc Interv Radiol, 2020; 23(2); 100678
17. Göksel F, Aycan A, Ermutlu C, Gölge UH, Sarısözen B, Comparison of radiofrequency ablation and curettage in osteoid osteoma in children: Acta Ortop Bras, 2019; 27(2); 100-3
18. Kostrzewa M, Diezler P, Michaely H, Rathmann N, Microwave ablation of osteoid osteomas using dynamic MR imaging for early treatment assessment: Preliminary experience: J Vasc Interv Radiol, 2014; 25(1); 106-11
19. Basile A, Failla G, Reforgiato A, The use of microwaves ablation in the treatment of epiphyseal osteoid osteomas: Cardiovasc Intervent Radiol, 2014; 37(3); 737-42
20. Hinshaw JL, Lubner MG, Ziemlewicz TJ, Percutaneous tumor ablation tools: Microwave, radiofrequency, or cryoablation – what should you use and why: Radiographics, 2014; 34(5); 1344-62
21. Geiger D, Napoli A, Conchiglia A, MR-guided focused ultrasound (MRgFUS) ablation for the treatment of nonspinal osteoid osteoma: A prospective multicenter evaluation: J Bone Joint Surg Am, 2014; 96(9); 743-51
22. Yarmolenko PS, Eranki A, Partanen A, Technical aspects of osteoid osteoma ablation in children using MR-guided high intensity focussed ultrasound: Int J Hyperthermia, 2018; 34(1); 49-58
23. Engel EE, Gava NF, Nogueira-Barbosa MH, Botter FA, CT guided percutaneous drilling is a safe and reliable method of treating osteoid osteomas: SpringerPlus, 2013; 2(1); 34
24. Atar D, Lehman WB, Grant AD, Tips of the trade. Computerized tomography – guided excision of osteoid osteoma: Orthop Rev, 1992; 21(12); 1457-58
25. Towbin R, Kaye R, Meza MP, Osteoid osteoma: Percutaneous excision using a CT-guided coaxial technique: Am J Roentgenol, 1995; 164(4); 945-49
26. Roger B, Bellin MF, Wioland M, Grenier P, Osteoid osteoma: CT-guided percutaneous excision confirmed with immediate follow-up scintigraphy in 16 outpatients: Radiology, 1996; 201(1); 239-42
27. Raux S, Abelin-Genevois K, Canterino I, Osteoid osteoma of the proximal femur: treatment by percutaneous bone resection and drilling (PBRD). A report of 44 cases: Orthop Traumatol Surg Res, 2014; 100(6); 641-45
28. Fenichel I, Garniack A, Morag B, Percutaneous CT-guided curettage of osteoid osteoma with histological confirmation: A retrospective study and review of the literature: Int Orthop, 2006; 30(2); 139-42
Figures
In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952