30 September 2023: Clinical Research
The Impact of Implementing the Vortex Approach on Airway Management Performance in Stressed Medical Students: A Randomized Controlled Simulation Study
Michał StarosolskiDOI: 10.12659/MSM.940372
Med Sci Monit 2023; 29:e940372
Abstract
BACKGROUND: The ability to manage airways in emergencies is paramount, especially for less experienced medical students. Although the Vortex Approach, a useful scheme to support decision-making during airway management, promises structured guidance, there’s limited research on its benefits among students. Our study aimed to evaluate student proficiency in a simulated difficult airway scenario and assess the advantages of the Vortex Approach.
MATERIAL AND METHODS: Medical students initially practiced on low-fidelity mannequins. Subsequently, they were divided into Vortex (n=48) and control groups (n=48). The Vortex group received specialized training. Both groups encountered a simulated scenario focusing on proper ventilation and supraglottic device insertion when traditional intubation failed. Performance was assessed using the airway management outcome score (AMOS).
RESULTS: The Vortex-trained group demonstrated superior capabilities. Fewer participants exceeded 3 lifeline interventions (4.2% vs 16.7%, P=0.046). The Vortex group consistently optimized subsequent attempts (31.3% vs 10.4%, P=0.01) and reduced prolonged apnea episodes (47.9% vs 81.3%, P=0.0009). Their AMOS scores were notably higher (56.3% vs 27.1%, AMOS=2, P=0.002), reflecting better patient outcomes (41.7% vs 10.4%, P=0.0005).
CONCLUSIONS: There is a marked need to enhance airway management skills among senior medical students. The Vortex Approach, even after brief exposure, yields significant skill improvements, underscoring its potential as a pivotal component in medical training. Integrating it into the curriculum could bridge the evident skill gap, optimizing future patient care.
Keywords: airway management, Algorithms, Education, Medical, Intubation, Simulation Training, Humans, Students, Medical, Curriculum, Manikins, Clinical Competence
Background
Anxiety, compulsion, and cognitive overload are integral to the work of medical professionals and are especially noticeable when providing respiratory protection in cases in which not all things work out as planned and the situation requires an immediate reaction and the ability to make the right decisions [1].
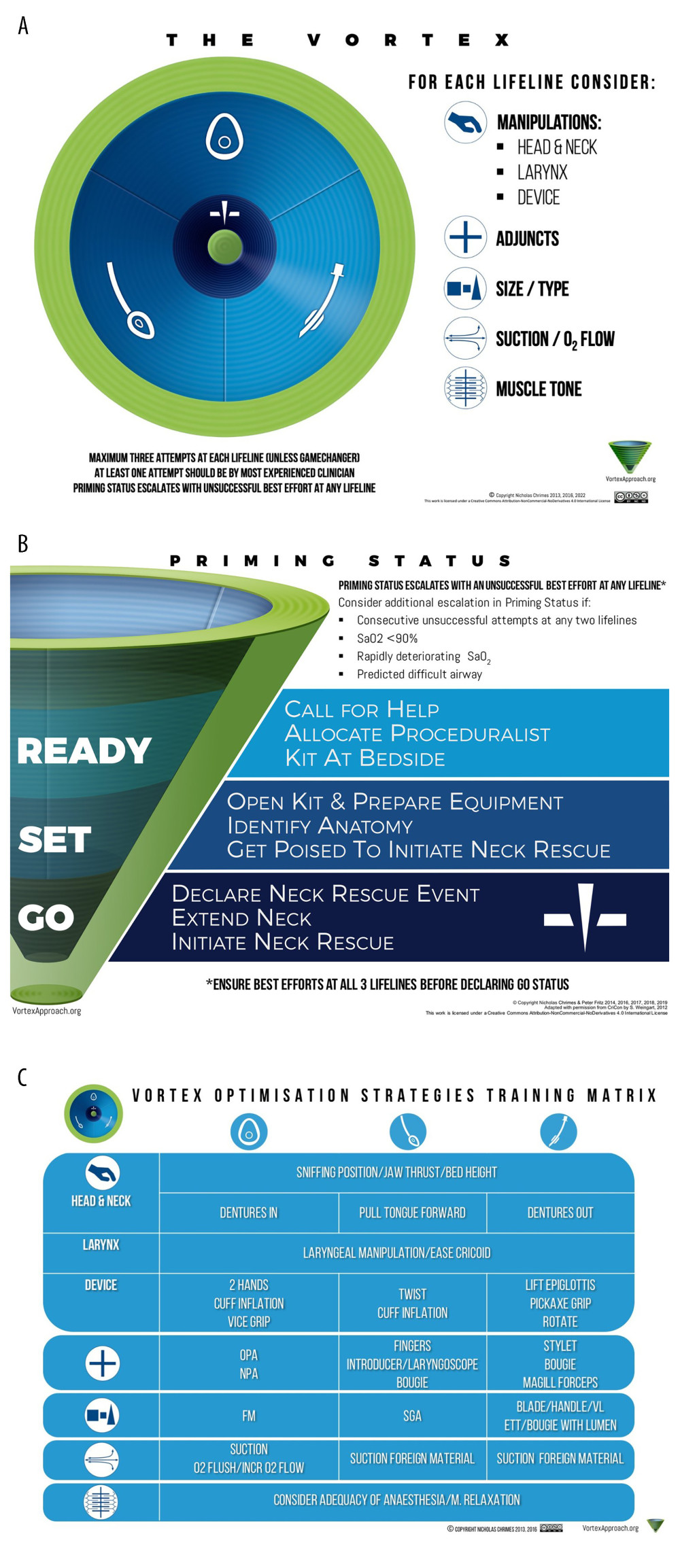
According to the available literature, the incidence of difficult intubation (3.2–4.9%) and cannot intubate–cannot oxygenate situations (up to 0.4%) are relatively rare, and the consequences of hypoxia, such as brain damage, are inexorable [2–7]. Nevertheless, every medical practitioner regardless of specialty should be prepared for these emergency situations. Algorithms are particularly helpful to reduce stress and relieve life-saving mental overload in urgent cases. The algorithms allow an increased focus on the clinical condition and treatment of the patient. The Vortex Approach is one of the useful schemes to support decision-making during airway management. It is based on the premise that there are 3 upper airway nonsurgical techniques for ventilation and coaches the practitioner to use the face mask, supraglottic airway, or endotracheal tube in any sequence, as the clinical circumstance dictates. If a “best effort” at each of these 3 techniques is not successful, then a cannot intubate–cannot oxygenate situation exists and a surgical airway must be initiated. The Vortex Approach was constructed as a simple and flexible implementation tool “to be used in real time by teams of potentially highly stressed individuals” during airway crises [8]. The Vortex Approach is presented as a funnel diagram, which consists of 3 circles that draw 3 zones. The outer part of the funnel is represented as the green zone and indicates the situation in which the patient has adequate alveolar oxygenation. The central blue zone contains the previously mentioned upper airway nonsurgical techniques between which one can move freely. The inner dark blue zone represents situations in which nonsurgical techniques have failed and an emergency surgical airway should be used. Securing the airway is one of the skills that every medical graduate should master to the extent that it can be performed in real life, avoiding critical errors. For medical students, who have a lack of clinical experience, simulations are crucial in learning these practical abilities, allowing students to improve their performance in future work with patients [9].
There is a paucity of studies that present the spectrum of benefits of the Vortex algorithm for the student population. The studies presented so far have presented comparisons of the Vortex algorithm to other airway management algorithms [10]. Mainly, they were conducted on physicians. Our work will broaden the perception of the Vortex algorithm, which is not only an algorithm to reduce cognitive overload but also a good basis for teaching students effective airway management. Nevertheless, we also intended to highlight a certain limitation of this work, which is the differences in the level of knowledge presented by the students.
The main objective of the study was to analyze the behavior and method choice of airway management among medical students in a simulated setting with a scenario of a patient with a difficult airway. The second goal was to evaluate whether the implementation of the Vortex Approach would result in more effective airway management, defined as a composite overall outcome. Based on the literature and our experience in working with students, we expected that medical students acquainted with the Vortex algorithm would perform better in the simulation and the rate of inappropriate intubations, and that the incidence of prolonged apnea would be lower in that group.
Material and Methods
ETHICS STATEMENT:
This prospective simulation study did not require bioethics committee approval because it was performed on mannequins. All participants voluntarily consented to participate in the study and the written informed consent was obtained from each of them. There was no compensation for participation in the study.
EQUIPMENT USED DURING THE SIMULATION:
The equipment used in the survey included the Simman 3G mannequin (Laerdal Medical AS, Norway), laryngeal mask airway, endotracheal tube, oropharyngeal airways (in various sizes), bag valve mask with different mask sizes, tracheal intubation stylet, and bougie intubation stylet.
The mannequin provided functions of multiple airway skills/features, airway complications, and breathing features (simulated spontaneous breathing). More information on the features of the simulator is available on the manufacturer’s website (
The aforementioned functions and simulation parameters were controlled and recorded by the Laerdal Learning Application (LLEAP), the original software of the simulator manufacturer.
SELECTION OF PARTICIPANTS:
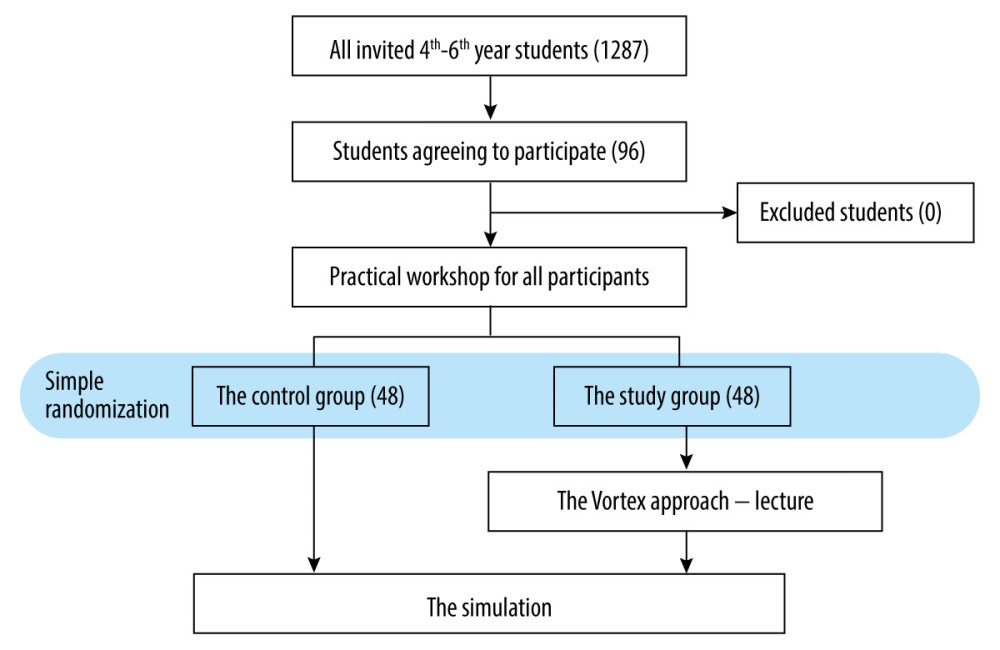
Initially, each student from the 4th to 6th year of medical studies at the Medical University of Silesia in Katowice was invited to participate in the simulation (Figure 1). Students with at least 1 year of clinical classes completed were included in the study. The invitation did not include any information about the course and topic of the simulation; the participants were only informed that it concerned emergency medicine. To limit the bias resulting from the students’ ability to prepare, the topics of the study were not disclosed until the training began. Graduates of nursing and emergency medical studies were excluded from the study due to their possible work experience. Everyone who voluntarily responded to our invitation and appeared to participate was informed about the workshop and the survey. Participation in the workshop phase was guaranteed for all who came. Students were verbally asked about their willingness to participate in the survey and were informed that they could withdraw from it at any time. After the workshop phase, willing students were asked to give written consent to participate in the study. The control group was informed that they could participate in the remainder of the Vortex translation lecture if they wished. No student was forced to participate, nor were they compensated for their participation. We tried to ensure that every participant in the study/workshop would benefit educationally.
TRAINING PHASE:
In the workshop phase, all students received task training on low-fidelity airway mannequins. The training was conducted in groups of 4 in order to provide participants with the most optimal access to the instructor. Each group had workshops conducted with one and the same instructor. It included familiarization and practical use of available instruments. This included bag/mask ventilation, use of oropharyngeals, placement of supraglottic devices, direct laryngoscopy with a Macintosh blade, basics of endotracheal intubation, and cricothyrotomy. During this workshop, both groups learned the technique of using the above-mentioned instruments and had the opportunity to practice the skills they had acquired. All participants received tips on what to do in crisis moments, but the knowledge was not systematized in the form of an algorithm. Students received 60 min to practice under the supervision of the instructor to improve basic airway skills and acquire a comfort level for these skills.
ASSIGNMENT TO VORTEX GROUP AND CONTROL GROUP:
When the first phase was completed, participants were assigned to a control group or a Vortex (research) group. For these purposes, simple randomization was applied using the Research Randomizer. Those assigned to the control group proceeded to the simulation stage, while the research group was presented with the Vortex Approach. For this purpose, we used publicly available engravings (Figure 2A#x02013;2C). The Vortex group was introduced to the Vortex algorithm through a short lecture lasting up to 10 min. The lecture was based on a presentation with engravings. It was strictly theoretical, describing the main concepts of the algorithm. Students were given a lecture without practicing or discussing the topic with the instructor. The students in the Vortex group were not suggested any desirable behaviors.
SIMULATION:
Before the simulation, the students were given the following general preliminary instructions: (1) take charge of a patient in the Emergency Department (ED); (2) think aloud; and (3) ask for anything needed at any time. In addition, students had the opportunity to ask questions about the scenario and the equipment used in the simulation. Classes conducted in the course of the medical studies were performed on the same model of the simulator, and therefore students were familiar with its functions. Moreover, each student had a briefing, which consisted of introducing them to the simulation scenario. The premise of the scenario was to secure the airway. The patient could be ventilated, and supraglottic devices could be placed. The settings we used on the Simman completely prevented intubation in its normal range of use. The settings included degeneration of the mandibular joint and the cervical spine. This resulted in neck stiffness and little ability to open the mouth. The settings were checked by the study authors in such a way that it was confirmed that the simulator could not be intubated within its normal range of use. However, the mannequin is just a piece of equipment. With a very large amount of force, the participant was able to break through the simulator’s resistance. This was audible through crackling and deformed flexible material of simulated teeth, among other things.
The scenario began with the student, as the only available doctor in the ED at the moment, being asked to help with airway management in an obese 70-year-old man with an exacerbation of chronic lung disease. Respiratory fatigue was evident in the patient. Students were informed of the possibility of administering rapid sequence intubation to the patient. However, to increase the focus on the goals of the scenario, specific medications with dosages were not required to be administered. The participant was accompanied in the simulation only by an assistant, who remained in the room throughout the scenario. If requested by the student, the assistant was able to help in monitoring the patient and obtaining and preparing, but not using, any required equipment. The assistant did not prompt the student, ask questions, or suggest any course of action.
Simulating the ED setting, an emergency cart containing only the materials needed during the simulation was available. The top drawer contained all the instruments needed during the simulation: 7.0-mm, 7.5-mm, and 8.0-mm endotracheal tubes, laryngoscope equipped with #1, #2, #3, and #4 Macintosh blades, supraglottic airways (size 3 and 4 laryngeal mask airway), and oropharyngeal tubes in various sizes. On the cart were face masks and an Ambu bag with stylets. If a student verbally requested the needed instrument, the assistant immediately provided it.
Time zero for the scenario was the participant’s declaration of readiness. The patient’s initial vital signs were blood pressure 150/95 mmHg, respiratory rate 34 breaths per min, heart rate 110 beats per min, and SpO2 80%. With the respiratory maneuvers performed correctly and the simulator recording the appropriate volumes, the patient’s vital parameters were adjusted accordingly. The patient poorly tolerated the attempt to place the laryngeal mask airway and perform intubation if no drugs were administered. Therefore, the students decided to use rapid sequence intubation (simplifying the simulation, the effect of the drugs was immediate). Performing rapid sequence intubation was synonymous with the patient’s apnea; from that point on, the patient’s SpO2 dropped by 1% in 3 s if no respiratory support was provided. This entailed the development of bradycardia and hypotension. The scenario lasted maximally for 7 min or ended earlier when the student successfully secured the airway. The end time of the scenario was chosen because cerebral hypoxia lasting longer than 3 to 5 min is associated with permanent brain damage.
After the simulation was completed, debriefing was conducted with each participant, aimed at drawing attention to and discussing the mistakes made by the participant. The instructor and evaluators were both blinded to the assignment of participants to the Vortex group and the control group throughout the study. In contrast, the person making the random assignment to groups and analyzing the data was not blinded.
DATA ACQUISITION:
For each participant, we collected the data about the course of the simulation, including duration of the simulation, oxygen saturation, equipment and optimizations used during the airway management attempts, duration of apnea, presence and duration of effective ventilation, respiratory rate and volume, technique and effectiveness of applied attempts in different lifelines, number of attempts in each lifeline, and the number of same attempts. We used Session Viewer, an application produced by Laerdal Medical AS, Norway, for this purpose. The definitions of an attempt were derived from the Vortex Approach website (
OUTCOMES DEVELOPMENT:
The concept of the airway management outcome score (AMOS) was created primarily to evaluate the performance of students. Its criteria were defined mainly on general 3 components: actions taken, their effectiveness, and their impact on the patient. In the first conception, the AMOS was to be a 2-point scale, evaluating the participant’s performance on a good/bad basis. However, during the course of the study, we encountered difficulties in explicitly evaluating the students’ actions. Our original approach depicted extreme behavior, so we had to adjust the AMOS by adding an intermediate score. This allowed us to evaluate the participants more objectively. We have included the criteria for AMOS scoring in Table 1.
AMOS=0: the patient was not obtaining effective intervention by which the clinical condition got worse; participants made significant or multiple errors: persistent, repeated attempts at a single lifeline (3 upper airway lifelines of face mask, supraglottic airway, and endotracheal tube are equally able to fulfil the goal of alveolar oxygen delivery) without optimization; traumatic endotracheal intubation; use of cricothyrotomy too early and incorrectly; or apnea.
AMOS=1: the participant’s actions were partially successful; or the patient’s condition was partially improving, but there were still errors in the participants’ technique.
AMOS=2: the participant provided effective interventions; the patient benefited significantly from the interventions.
In cases that did not conform to the AMOS definitions listed above, the authors decided to assign a score according to the principles of the Vortex Approach. In case of disagreement, the third blinded author carried out an independent, conclusive assessment (Table 1).
Traumatic intubation was defined as an intubation attempt in which participants, despite the limitations of our patient-simulator, forcibly intubated and simultaneously harmed the patient. Whereas, apnea was defined as a continuous time without effective patient ventilation of more than 1 min.
STATISTICAL ANALYSIS:
The database was collected in Microsoft 365 Excel, Microsoft Corporation, and statistical analyses were performed using the program Statistica 13.3. The distribution of the continuous variables was verified with the Shapiro-Wilk test, and homogeneity of variance was tested with the Levene test. Continuous variables with a normal distribution were presented as mean and standard deviation, and variables with a non-normal distribution were expressed as median and interquartile range. Quantitative variables were expressed as absolute values and percentages. We compared the study group and the control group in terms of the following nominal data: applied method of airway management and course of the simulation, composite airway management score, identical attempts, use of optimizations, number of attempts in 1 lifeline, and proper technique/mistakes during applying particular devices and effectiveness of ventilation (including tidal volume and frequency). Based on data from the study of Ambardekar et al, indicating an approximate 30.5% improvement in airway management after learning the Vortex algorithm, we determined the number of participants in each group. Including a 5% type α error and a 20% type β error, the minimum number of participants in each group was determined as 34 [11]. Analysis of nominal variables was performed using the chi-square test or Fisher’s exact test. Analysis of continuous variables was performed using the t test or Mann-Whitney U test. A P value of <0.05 was considered statistically significant.
Results
In total, 96 students (29%, n=28 men) in the 4th to 6th year of medical studies participated in the study. The students were enrolled in the Vortex group and in the control group. Table 2 shows the main characteristics of the participants.
It was possible to distinguish several repeated pathways of airway management, which are described in Table 3. Most students in the control group (13/48, 27%) performed a traumatic endotracheal intubation, defined as an intubation attempt in which participants, despite the limitations of our patient-simulator, forcibly intubated and simultaneously harmed a patient. While, after the Vortex Approach lecture, most of them used different lifelines (3 upper airway lifelines of face mask, supraglottic airway, and endotracheal tube are equally able to fulfil the goal of alveolar oxygen delivery) or optimizations (according to the Vortex model, these are actions (including manipulations, additives, size/type, suction/O2 flow, muscle tone) that can be applied to increase success in entering the green zone through any of the lifelines, without identical attempts (14/48, 29%). This approach was used significantly less often in the control group (2/48, 4%,
After the analysis of the course of simulations, in total 26/96 (27%) participants were rated as AMOS=0; 30/96 (31%) as AMOS=1; and 40 (42%) as AMOS=2. The Vortex group coped with airway management significantly better than the control group. In comparison with the control group, participants after the Vortex lecture less often applied more than 3 attempts in 1 lifeline (4.2% vs 16.7%,
Discussion
LIMITATIONS:
Our study had limitations. Regarding organizational difficulties, one serious limitation was the small group of respondents. The study was based on the participation of volunteer students. The consequence of this is the lack of stratified randomization. The lack of blinding of the person doing the data analysis is also a limitation and may have resulted in unconscious bias. Therefore, conclusions drawn from the results of the study should be interpreted with caution. One of the biggest limitations remains the simulator. Despite the use of the Simman 3G features that made intubation impossible, our participants succeeded in breaking the simulator’s persistence. Also, even such a good simulator cannot imitate the variability and difficulty of securing an airway in a human being. Despite this, we believe that learning through simulation remains the best method of learning in medical studies. It makes it possible to evaluate student behavior in a controlled manner and enables precise reference to mistakes made and high-quality debriefing.
Another limitation is the possible difference in the level of knowledge, experience, and interests of the participants. For this reason, we asked about their specialized future plans. Although the participants were at a similar stage of training, their knowledge regarding airway management or the equipment used may have differed. Given this, we cannot exclude prior knowledge of the Vortex Approach; however, the randomization should have prevented the impact of this variable on the results. The stress induced in the participants due to decision-making may also have limited the students’ cognitive functions. However, we claim that this is a beneficial phenomenon that allows students to become accustomed to difficult situations that will occur in their future work.
Conclusions
The overall efficacy of airway management among students in the last years of medical college is not satisfactory. The implementation of the Vortex Approach resulted in better airway management by medical students. Even a short training with an introduction of the Vortex Approach can lead to improvement of these important skills and should therefore be included in the learning plan.
References
1. Quek TT, Tam WW, Tran BX, The global prevalence of anxiety among medical students: A meta-analysis: Int J Environ Res Public Health, 2019; 16(15); 2735
2. Thoeni N, Piegeler T, Brueesch M, Incidence of difficult airway situations during prehospital airway management by emergency physicians – a retrospective analysis of 692 consecutive patients: Resuscitation, 2015; 90; 42-45
3. Heinrich S, Birkholz T, Irouschek A, Incidences and predictors of difficult laryngoscopy in adult patients undergoing general anesthesia: A single-center analysis of 102,305 cases: J Anesth, 2013; 27(6); 815-21
4. Cook TM, MacDougall-Davis SR, Complications and failure of airway management: Br J Anaesth, 2012; 109(Suppl 1); i68-i85
5. Kheterpal S, Healy D, Aziz MFMulticenter Perioperative Outcomes Group (MPOG) Perioperative Clinical Research Committee, Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: A report from the multicenter perioperative outcomes group: Anesthesiology, 2013; 119(6); 1360-69
6. Tachibana N, Niiyama Y, Yamakage M, Incidence of cannot intubate-cannot ventilate (CICV): Results of a 3-year retrospective multicenter clinical study in a network of university hospitals: J Anesth, 2015; 29(3); 326-30
7. Caplan RA, Posner KL, Ward RJ, Cheney FW, Adverse respiratory events in anesthesia: A closed claims analysis: Anesthesiology, 1990; 72(5); 828-33
8. Chrimes N, The Vortex: A universal ‘high-acuity implementation tool’ for emergency airway management: Br J Anaesth, 2016; 117(Suppl 1); i20-i27
9. Meyer MN, Connors H, Hou Q, Gajewski B, The effect of simulation on clinical performance: A junior nursing student clinical comparison study: Simul Healthc, 2011; 6(5); 269-77
10. Ambardekar AP, Rosero EB, Bhoja R, A randomized controlled trial comparing learners’ decision-making, anxiety, and task load during a simulated airway crisis using two difficult airway aids: Simul Healthc, 2019; 14(2); 96-103
11. Apfelbaum JL, Hagberg CA, Connis RT, 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway: Anesthesiology, 2022; 136(1); 31-81
12. Hubert V, Duwat A, Deransy R, Effect of simulation training on compliance with difficult airway management algorithms, technical ability, and skills retention for emergency cricothyrotomy: Anesthesiology, 2014; 120(4); 999-1008
13. Borges BC, Boet S, Siu LW, Incomplete adherence to the ASA difficult airway algorithm is unchanged after a high-fidelity simulation session: Can J Anaesth, 2010; 57(7); 644-49
14. Davies PR, Tighe SQ, Greenslade GL, Evans GH, Laryngeal mask airway and tracheal tube insertion by unskilled personnel: Lancet, 1990; 336(8721); 977-79
15. Deakin CD, Peters R, Tomlinson P, Cassidy M, Securing the prehospital airway: A comparison of laryngeal mask insertion and endotracheal intubation by UK paramedics: Emerg Med J, 2005; 22(1); 64-67
16. Komatsu R, Kasuya Y, Yogo H, Learning curves for bag-and-mask ventilation and orotracheal intubation: An application of the cumulative sum method: Anesthesiology, 2010; 112(6); 1525-31
17. Massoth C, Röder H, Ohlenburg H, High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students: BMC Med Educ, 2019; 19(1); 29
18. Buis ML, Maissan IM, Hoeks SE, Defining the learning curve for endotracheal intubation using direct laryngoscopy: A systematic review: Resuscitation, 2016; 99; 63-71
19. Joffe AM, Aziz MF, Posner KL, Management of difficult tracheal intubation: A closed claims analysis: Anesthesiology, 2019; 131(4); 818-29
20. Herbstreit F, Fassbender P, Haberl H, Learning endotracheal intubation using a novel videolaryngoscope improves intubation skills of medical students: Anesth Analg, 2011; 113(3); 586-90
Figures
Tables
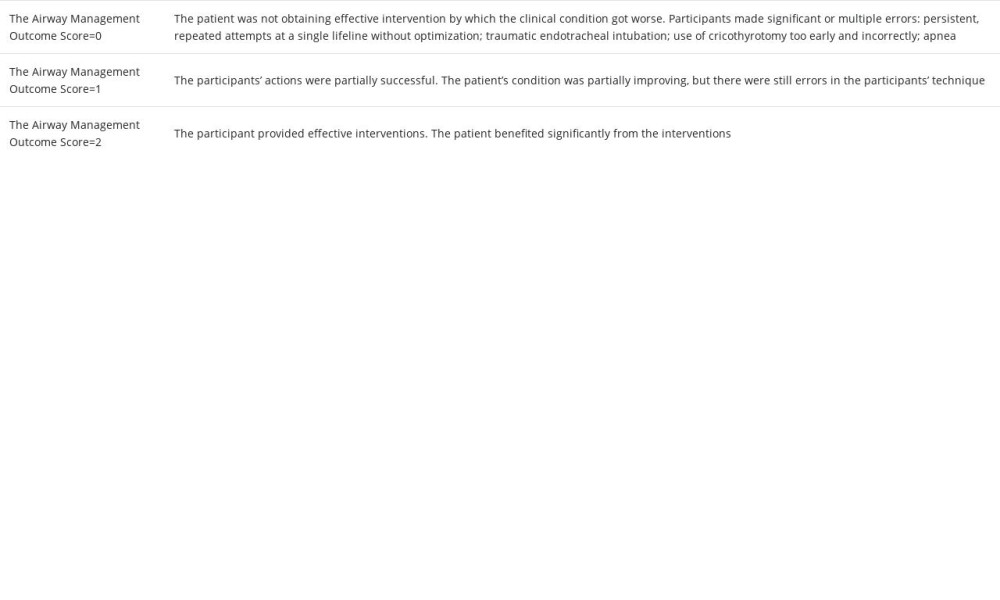 Table 1. The airway management outcome score (AMOS).
Table 1. The airway management outcome score (AMOS).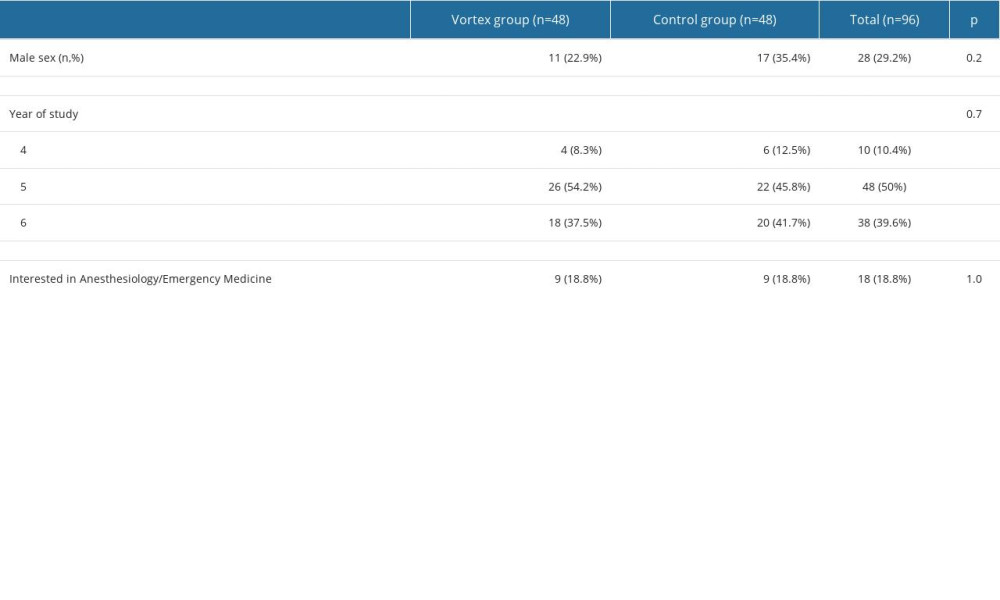 Table 2. Main characteristics of the participants.
Table 2. Main characteristics of the participants.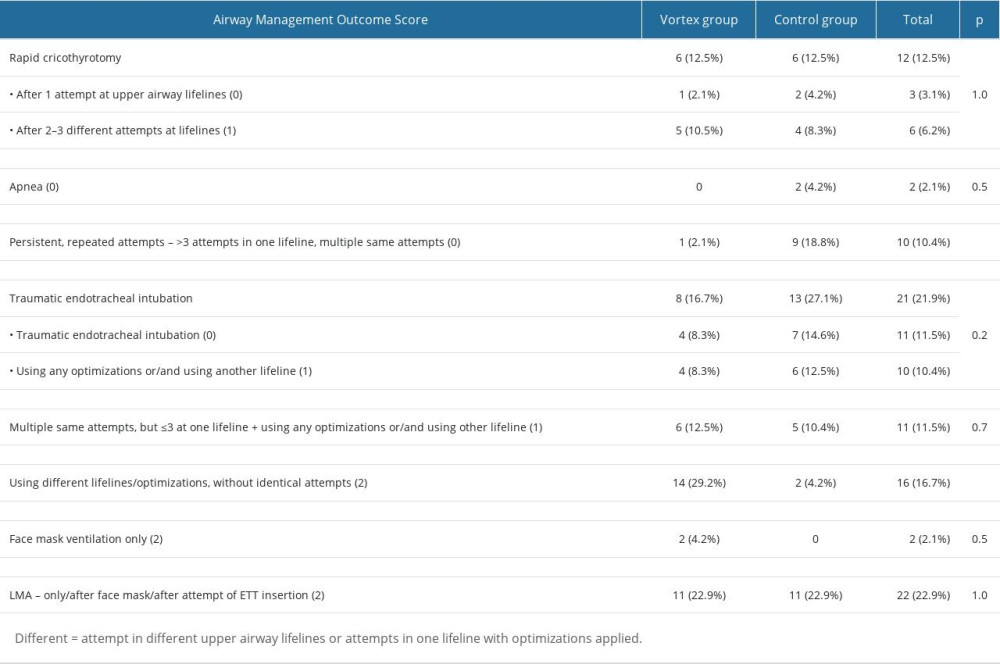 Table 3. Pathways of airway management.
Table 3. Pathways of airway management.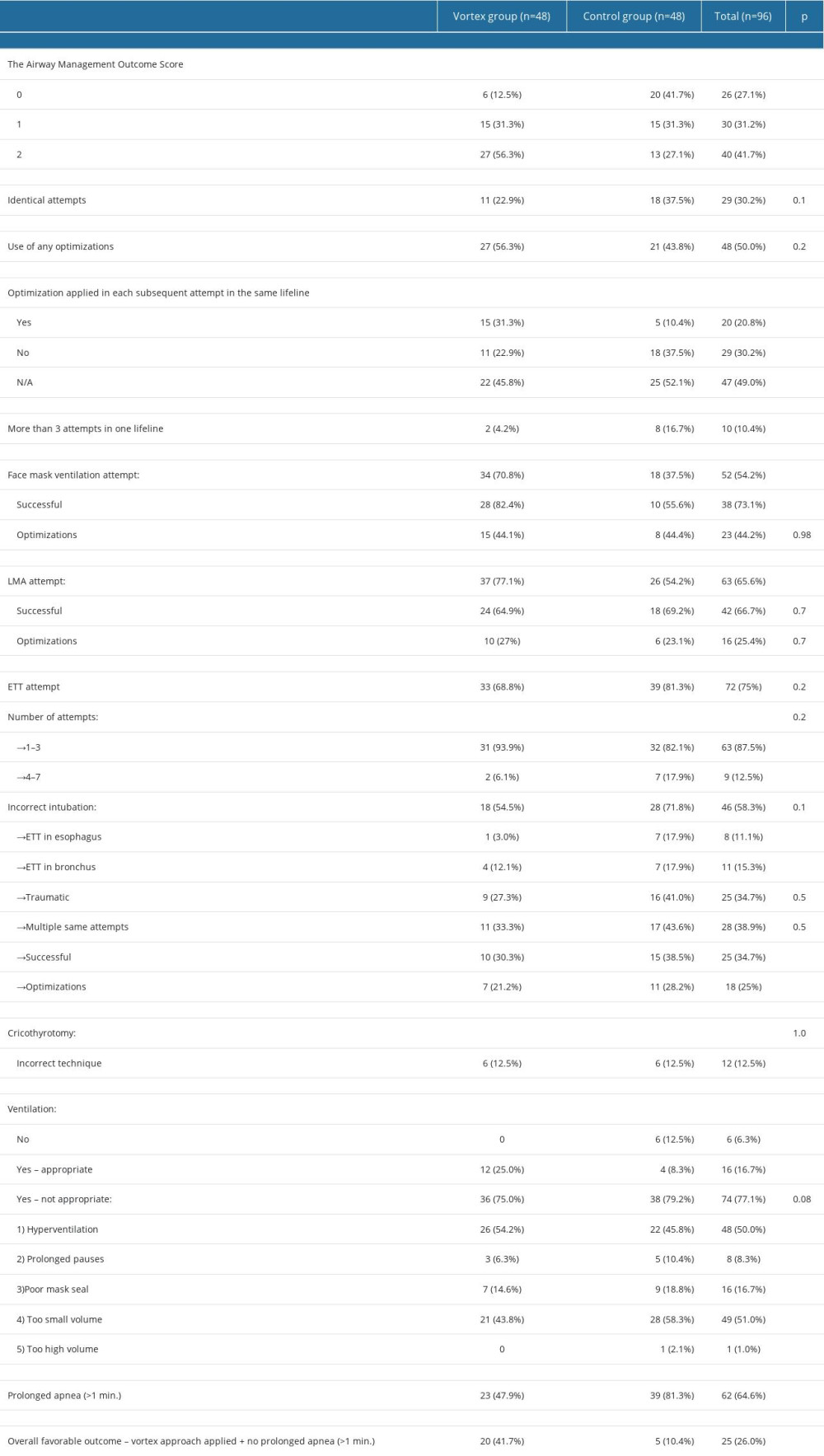 Table 4. Comparison of the Vortex group and control group.
Table 4. Comparison of the Vortex group and control group.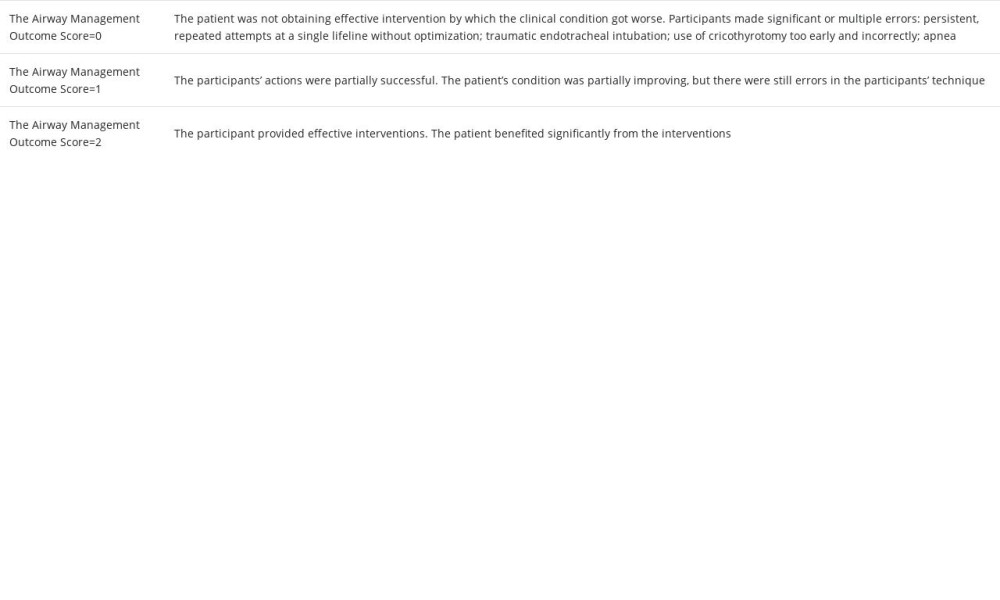 Table 1. The airway management outcome score (AMOS).
Table 1. The airway management outcome score (AMOS).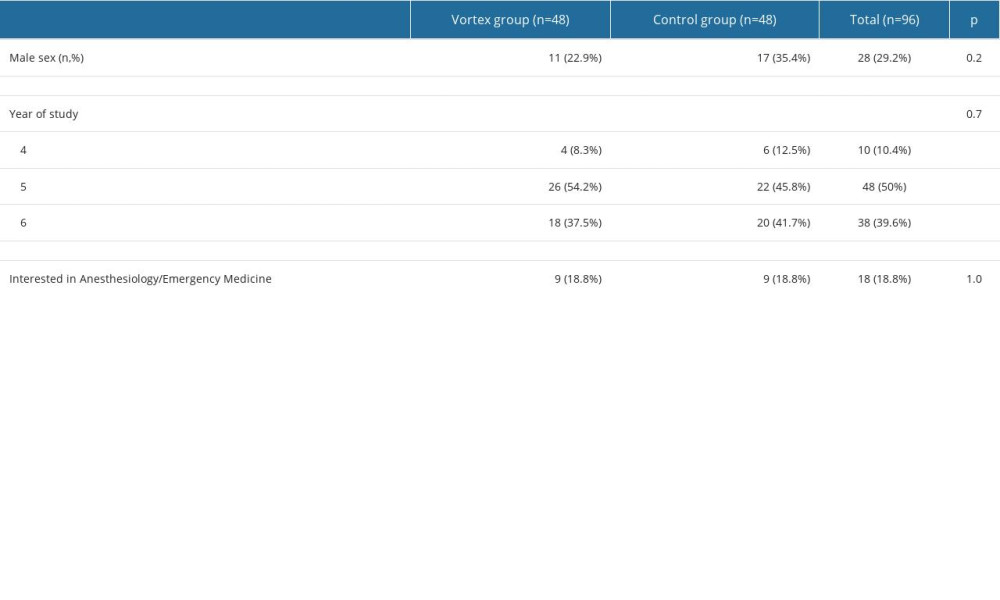 Table 2. Main characteristics of the participants.
Table 2. Main characteristics of the participants.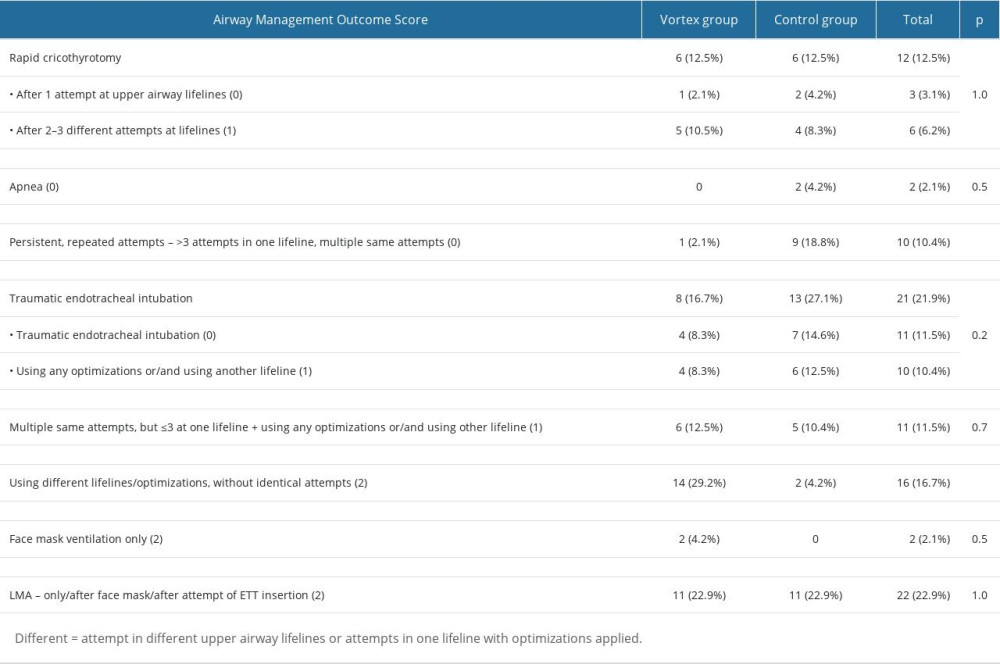 Table 3. Pathways of airway management.
Table 3. Pathways of airway management.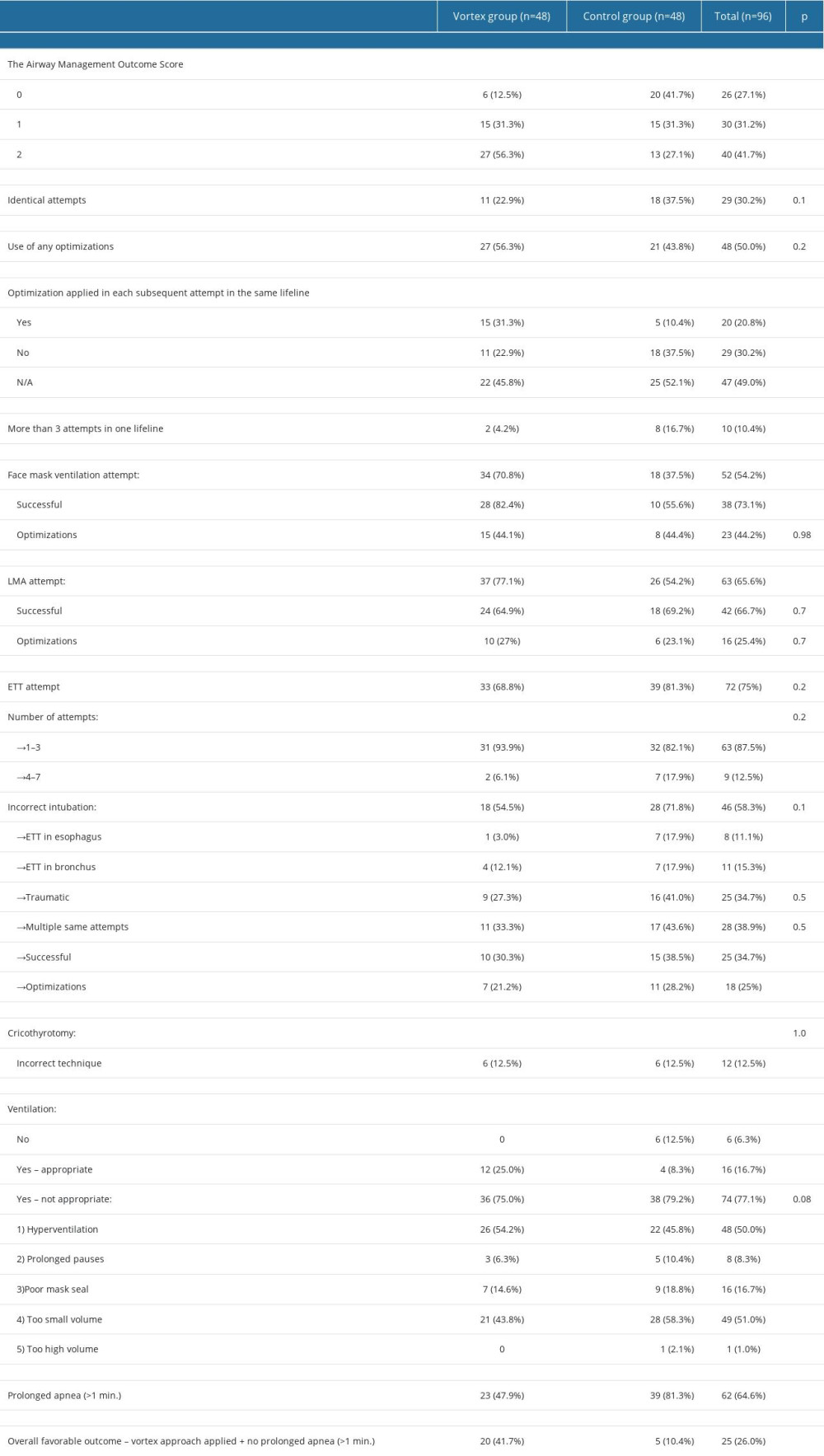 Table 4. Comparison of the Vortex group and control group.
Table 4. Comparison of the Vortex group and control group. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952