05 July 2023: Clinical Research
Immunomodulatory Effects in Healthy Individuals Following a 4-Week Taoist Qigong Intervention: A Comparative Study
Juan M. ManzanequeDOI: 10.12659/MSM.940450
Med Sci Monit 2023; 29:e940450
Abstract
BACKGROUND: Qigong, an ancient health preservation technique forming part of Traditional Chinese Medicine, combines slow body movements, breathing, and meditation. While this meditative movement system has been reported to offer various physical and psychological benefits, studies on the Taoist school of qigong are sparse. This study, therefore, aimed to investigate the effects of Taoist qigong on white blood cells and other immune parameters in healthy individuals.
MATERIAL AND METHODS: Thirty-eight participants were recruited for the study, with 21 assigned to the experimental group and 17 to the control group. Participants in the experimental group engaged in a four-week Taoist qigong program. Blood samples for immune parameter quantification, including leukocyte count, neutrophil, eosinophil, basophil, lymphocyte, and large unstained cell (LUC) counts, as well as concentrations of IgG, IgA, IgM, C3, and C4, were collected one day before the experiment started and one day after it ended.
RESULTS: Post-program, the experimental group exhibited significantly lower total leukocyte counts, and reduced numbers of lymphocytes and LUCs. Additionally, a higher percentage of monocytes was noted in this group.
CONCLUSIONS: Taoist qigong practice induced a distinct immunomodulatory profile, characterized by decreased counts of several white blood cell parameters and increased percentages of certain agranulocytes. This outcome presents intriguing implications from a psychobiological perspective and highlights the need for further research into the immune effects of Taoist mind-body practice.
Keywords: Immunomodulation, Mind-Body Therapies, qigong, Humans, Immunity, Medicine, Chinese Traditional, Respiration, healthy volunteers, Leukocytes, Breathing Exercises
Background
Qigong is a traditional method of mind-body training, dating back thousands of years, which is part of Traditional Chinese Medicine [1–3]. The main aim of this classical discipline, of which there are various systems, is to achieve mind-body harmony through the coordinated use of slow body movements, breathing, and meditation in a single exercise [4–6]. Considering its peculiar combination of practices, Qigong has been said to be meditative movement [7,8]. The different methods of Qigong are each associated either with the philosophical schools of Taoism, Buddhism, or Confucianism, and there are also Qigong systems linked to Chinese medicine and martial arts [9]. The Taoist school of Qigong in particular is based on the principles of
Although Taoist Qigong has been found to have an immunomodulatory effect, this action has only been reported immediately after practice [11]. The changes induced by Qigong on immune parameters accrue after practice, but can disappear as time from the last practice elapses. While the reach of this effect over time is unknown, a longer-lasting immunomodulatory action could presumably lead to more stable physical and perhaps psychological changes. Consequently, the aim of the present study was to evaluate the specific effects of Taoist Qigong practice on leukocyte count, as well as on the concentration of immunoglobulins (IgA, IgG, IgM) and complement (C3 and C4), 1 day after completion of the 4-week programme. Given that these parameters are to be measured 1 day after the last practice session, the sustained effects of Qigong 24 hours after practice could be assessed. The specific underlying mechanisms by which Qigong might influence these parameters, however, lies beyond the scope of this research.
Due to the integrative nature of Qigong, researchers have become increasingly interested in the potential therapeutic benefits of its practice [1,12–16]. In fact, there is a considerable body of empirical evidence in support of the clinical utility of Qigong, particularly with respect to improvements in overall physical and mental health [2,17–20]. In this respect, research has documented a wide range of physiological benefits [1,21–27], as well as relief of anxiety and depression symptoms even in patients with chronic disease [2,28,29]. Likewise, improvement has been shown on specific medical conditions such as hypertension [30–32], diabetes [33–35], chronic heart disease [36–38], fibromyalgia [39–41], movement disorders [42–45], and cancer [46–49].
Given that the practice of Qigong has a wide range of beneficial effects, it is important to elucidate its underlying mechanisms. In this sense, it is interesting to note that some of the health benefits associated with Qigong may be mediated by immuno-modulation [13]. Not surprisingly, a number of studies have documented changes of immune parameters following Qigong practice [50], including increases in the number of specific lymphocyte sub-populations such as T and/or B cells [11,51,52], enhanced neutrophil function [53] and cytolytic/tumoricidal activities [54], as well as increased antibody response to influenza vaccine [55,56]. However, results of how Qigong impact the immune system are not consistent among different studies. In addition, there are no data available linking Qigong with changes of specific immune parameters such as the large unstained cells (LUC). This is an interesting issue, since this parameter has been said to be of particular clinical relevance in immunocompromised patients [57,58]; in addition, changes of this immune parameter have been linked to some disorders [59,60]. Therefore, our study can provide significant evidence of the impact of Qigong on the immune system, which may hold potential clinical implications. In fact, this research might provide evidence to support the use of Qigong as an intervention to modulate immune function.
Material and Methods
ETHICS STATEMENT:
We confirm that any aspect of the work covered in this manuscript, which involved humans, has been conducted with the ethical approval of all relevant bodies. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The nature of the study and the procedure was explained to all participants, and written informed consent was obtained from all subjects. Subjects did not receive any financial remuneration or course credits for their participation. All data, including full statistics data, as well as every single immunological measure from each and all of the subjects, are readily available upon request.
PARTICIPANTS:
Participants in this study were all Psychology students from the University of Malaga who volunteered to take part following a preliminary interview by means of which they were checked about health issues, lifestyle habits, including sleep quality, eating and drinking routines, as well as physical and leisure activities. The main inclusion criteria for both the experimental and control groups were being in good health, not having serious medical conditions that might limit their participation, and following regular lifestyle habits, with no significant changes between weekdays and weekends. Potential participants were excluded if they had any diagnosed health condition and/or had taken prescribed medication during the 3 months prior to the study period. All the females included were within the first 10 days of their menstrual cycle at the time of the study. This prerequisite was due to the fact that the present study was part of a larger investigation dealing with other biological measures and psychological variables, which could be influenced by the hormonal changes that occur throughout the menstrual cycle. Consequently, our purpose was to homogenize the sample of female participants, all of them being in the first days of their menstrual cycle, when specific hormone levels are lower and, therefore, less prone to influence other psychobiological parameters.
None of the selected participants regularly practiced sports or had previous experience of Qigong, yoga, or other similar activities. This information was obtained from the preliminary interview, wherein subjects were checked if they practiced any sports, and if so, how often. Likewise, subjects were asked if they regularly practiced Qigong, yoga, or other similar activity, and whether they had had any previous past experience with any of these psychosomatic methods. All subjects were instructed to maintain their usual lifestyle throughout the study period so as to ensure that the only difference between the experimental and control groups was that the former followed the Qigong program.
The final sample comprised 38 individuals (8 males and 30 females), aged between 18 and 21 years. Of these, 21 were randomly assigned to the experimental group (17 females and 4 males) and 17 to the control group (13 females and 4 males). The difference in gender distribution between the 2 groups was therefore only 2.2%.
INTERVENTION:
The particular method of Taoist Qigong investigated in this research involves a single sequence of movements composed of 7 exercises, each of which is repeated 6 times. For all the exercises, individuals adopt a standard body posture with their feet apart and parallel to one another, approximately in line with their shoulders. The movements that make up the entire sequence require the person to stretch his or her hands, arms, trunk, waist and legs, without moving the basic position of the feet. These movements must be accompanied by natural, relaxed and rhythmic breathing.
The Qigong programme lasted for 4 weeks and comprised 3 group and 2 individual sessions per week. The group sessions typically involved the practice of the whole Qigong form for 2 times, with a few minutes’ break in between. This training, which took place on Monday, Wednesday, and Friday afternoons in a room next to our laboratory, lasted for 25–30 minutes, and was supervised by an instructor of this Qigong style. The instructor’s role was to demonstrate the movements so that subjects could follow and learn them correctly. Likewise, while subjects performed the exercises, the instructor would make corrections and adjustments of the positions displayed by subjects if those diverged from the standard ones. These corrections were typically done by the instructor on the first week of training. In addition to the group sessions, experimental subjects were asked to perform 2 similar sessions at home (one on either Tuesday or Thursday and one at the weekend); for the individual sessions, they were required to practice the Qigong form one single time, which involved 10–15 minutes of practice. During the 4 weeks Qigong program, participants in the control group were asked simply to follow their regular daily routines and habits.
BLOOD SAMPLING:
Blood samples for the quantification of immune parameters were drawn from all subjects (experimental and control) 1 day before the Qigong program began and 1 day after the final session (4 weeks later). Blood was collected by venipuncture at 9:00 a.m. and was immediately centrifuged in a refrigerated centrifuge before storage at −20°C. Samples were transported in isothermal fridges, with controlled temperature, using dry ice. Once in the laboratory, those parameters needing immediate processing (ACTH and blood counts) were processed accordingly. For the rest of the biological measures, serum samples were frozen and processed within 48–72 hours. The immune parameters considered included the number of leukocytes, the number and percentage of neutrophils, eosinophils, basophils, lymphocytes, and LUC, as well as the concentrations of IgG, IgA, IgM, C3, and C4. For the white series count (total leukocytes, monocytes, neutrophils, eosinophils, basophils, total lymphocytes and LUC), the procedure involved placing 5 ml of whole blood into EDTA tubes and analyzing the samples by means of a Siemens ADVIA 2010 flow cytometry analyzer. This analyzer combines flow cytometry with an automatic dyer-extensor using standard peroxidase dyeing of reference for leukocyte differential count. The concentrations of immunoglobulins and complement factors were analyzed by an immunoturbidimetric method whereby complement anti-proteins and anti-immunoglobulin antibodies react with the antigen of the sample, forming an antigen-antibody complex. Subsequent agglutination in both cases may then be measured by turbidimetry. All the parameter analyses were performed using the Modular Analytics E170 system (Roche Diagnostics). Reference values were calculated by the laboratory itself, considering its population. The reference value includes 95% of the population values, which will be considered normal for the parameters measured.
STATISTICAL ANALYSIS:
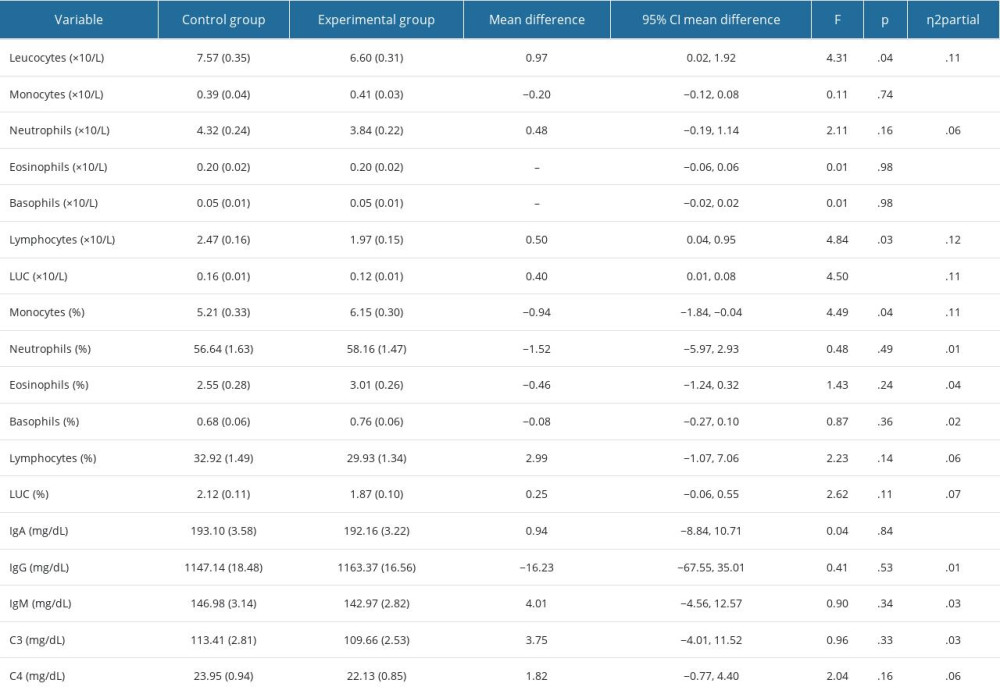
Data were collected according to a pretest-posttest design with random assignment to the control and experimental groups. Accordingly, a between-group analysis of covariance (ANCOVA) was performed on the dependent variables listed in Table 1. The Qigong program was considered as an independent variable with 2 levels (absence or control group, and presence or experimental group), while the respective pretest scores of each dependent variable were treated as covariates. Thus, the posttest differences between groups were estimated with the differences in pretest scores removed, with a significance level of .05. All analysis fulfilled the assumptions of homogeneity of variance and homogeneity of regression slopes. Partial eta squared was used as a measure of effect size. Following Cohen’s criterion [61], we considered a value of 0.01 as a small, 0.06 as medium, and 0.14 as large effect size. There were no missing data. Statistical analysis was carried out by IBM-SPSS 25.
Results
The results obtained in this research are shown in Table 1. The table reveals that following a Taoist Qigong program with a duration of 1 month, statistically significant differences were found between the experimental and control groups with regard to total leukocyte, lymphocyte, and LUC counts; in this sense, experimental subjects displayed lower values of these parameters as compared to controls. Monocytes (%) was also statistically significant, with a greater mean in the experimental group than in the control group. All partial eta squared were close to a large effect size. Statistical significance was not reached, however, in the concentrations of IgA, IgG, IgM, C3, and C4, the number and percentage of neutrophils, eosinophils, and basophils, the number of monocytes, or in the percentage of lymphocytes and LUC.
Discussion
The main finding of this study is that Taoist Qigong can induce a significant and sustained immunomodulatory effect in healthy individuals after just a short period of practice of 4 weeks. It is interesting to point out that the ability of this type of Qigong to influence immune parameters in a baseline of 24 hours had never been reported up to now. Likewise, it is also noteworthy that this is the first study measuring and reporting a significant change in the number of LUC, a very specific count parameter, following a Qigong program.
Our results revealed that, 1 day after the Taoist Qigong program concluded, the total number of leukocytes was lower in the experimental group than in controls. These data, the first to be published in relation to Taoist Qigong, are consistent with the results of a previous study by our group, in which we observed a decrease in the total number of leukocytes among healthy individuals who practiced another form of Qigong [57]. In addition, our result of a lower leukocyte count also coincide with what has been reported in subjects engaging in tai chi, another method of Qigong [62]. Nevertheless, it should be noted that not all research in this area reported an immunomodulatory response characterized by a decrease in the total number of leukocytes. In fact, several studies that examined the total leukocyte count in relation to mind-body practices have either found no change or even an increase of this parameter [63–67], with a similar discrepancy being observed in studies of physical exercise [68,69]. These differences could be due to the distinct and heterogeneous nature of the various Qigong systems employed, the different methodology followed, etc. In this sense, the different length of the programs, which varies considerably across the studies, and the time points in which measures were taken, can play an important part in the discrepancy in results. In addition, factors such as age, level of physical activity and dietary habits, which are not always controlled in the studies, could have a relevant influence on leukocyte count [70].
Another interesting finding of the present study is the significant decrease in the total number of lymphocytes following participation in the Taoist Qigong program. This contrasts with the results of a previous study by our group in which adaptive immune response cells (eg, total lymphocytes) remained unaffected after Qigong practice [57]. The duration of the programs was similar in both of our studies, but the Qigong methods investigated were different, and this may likely account for the discrepancy in results. However, other studies have found an increased lymphocyte count after the practice of Qigong or other such mind-body methods [51,67,71–74]. Likewise, a study of patients with HIV infection reported augmented lymphocyte proliferative function after 10 weeks of tai chi [75]. Therefore, our results are peculiar in that a decrease of the total number of lymphocytes following the practice of Taoist Qigong was found. The difference between our result of lymphocyte count and that of the other studies may be owing to the particular features of Taoist Qigong, the difference in experimental designs, including, as previously indicated, the various length of the programs, as well as the distinct time intervals in which measures were taken.
Mention should also be made of a recent study by our group concerning the same form of Qigong used in the present research. In that previous study, while we did not find any change in the total number of lymphocytes as such, interestingly, we did observe an increase in the number and percentage of B lymphocytes [11]. The different measurement points used in these 2 studies probably account for the differences observed, both in the immune parameters showing a significant change, as well as in the direction of the effect. Thus, in the previous research, final measurements were taken 1 hour after the last session of Qigong, while in the present one these measures were obtained 1 day after the completion of the Qigong program. The findings from our present research seem to reflect a more enduring immunomodulatory effect of Qigong, whereas the previous investigation revealed a rather acute effect. In future studies it would therefore be interesting to take measurements at both time points so as to capture the continuity and persistence of any observed changes. In addition, it would be useful to analyze the different lymphocytes subgroups, since some of them have been shown to be more sensitive to the time factor [11].
The large unstained cells have not been, to date, studied in relation to any form of Qigong, mind-body method, or physical exercise. However, this immune parameter has been studied in the context of infectious diseases [58,76,77]. Thus, Shin et al [77], in a study of patients with varicella, found that the percentage of LUC increased significantly during the acute phase, but then showed a significant decrease once the patient improved clinically. This decrease presumably reflects a stabilization within the immune system, returning to an optimum state once the patient’s symptoms improve. A similar result was observed in a study on the effects of chemotherapy in cancer patients [76], which revealed that the highest LUC values coincided with the nadir of neutropenia, this being the point at which the patient is most susceptible to infections. The authors, therefore, concluded that a decrease of LUC values might predict the end of this phase of vulnerability, adding that this decrease would have a certain prognostic value.
Consistent with results mentioned above, an investigation designed to assess the immune activation levels in HIV infection found that the number of LUC was significantly increased in the HIV-infected group, as compared with uninfected controls [58]. Likewise, in a study of COVID-19-positive patients, with and without diabetes mellitus, the number of large stained cells was found to be higher in the diabetic patients compared to the non-diabetic group [78]. In light of these results, our finding that the number of LUC decreased following a 4-week Taoist Qigong program seems compatible with a stabilization or even optimization taking place within the immune system. However, given the general lack of information with respect to the effects of Qigong on LUC, more research is certainly needed to be able to fully assess the impact of this ancient mind-body method on this particular immune parameter.
The percentage of monocytes, which was higher in the experimental group than in controls, seems to contrast with the rest of the results from this study, since a higher value of this parameter was exhibited in the subjects that followed the Qigong program. While the number of monocytes as such remained unaffected, the increase in the percentage of this type of agranulocyte is a significant result in this study due to the direction of the change, as well as due to the very nature of the change, affecting the percentage rather than the number, as with the rest of immune parameters.
Taking together, the decrease in the number of leukocytes, lymphocytes, and LUC, and the increase in the percentage of monocytes, that we observed after the 4-week Taoist Qigong program, reflects quite an interesting psychobiological profile. These results, therefore, confirm that Taoist Qigong can indeed induce significant changes in the number of certain white blood cells. Given the nature of these results, it would be interesting to hypothesize the biological mechanisms whereby Qigong can impact the immune system. In this sense, it is well known that Qigong exerts noteworthy physiological [20,22,31] and psychological [2,18,26] effects. This broad psychophysiological action of Qigong is likely to influence the neuroendocrine system, thereby inducing endocrine effects [10,12,34,35] that may, ultimately, account for the changes in immune parameters, given the link between the immune and endocrine systems [79,80].
Although, in general, lower levels of leukocytes and lymphocytes, at first glance, might appear to be a sign of a detrimental effect of Qigong on the immune system, several aspects, which indicate a beneficial and more coherent interpretation of results, should be taken into consideration. In this sense, it is a known fact that physical and psychological stress, among other factors, may increase the number of some white blood cells in peripheral blood [81–85]; but on the other hand, the pathogenesis of numerous diseases has been said to be characterized by a heightened immune response [86–89]. Consequently, in this context, the lower count of these parameters found in our experimental subjects may be of clinical relevance, as they are consistent with a beneficial action of Qigong on the immune system. Furthermore, given the influence that emotional and behavioral changes have on the immune system, one might wonder whether the boosting of certain psychological factors may have played a determining role in the immune modulation observed in this study. Nonetheless, to ascertain this possibility would be beyond the scope of this research. Based on our results it would certainly be interesting to consider how Taoist Qigong could be applied to a clinical setting to foster health by immunomodulation. While it may still be tentative to do so, it is our opinion that Qigong has the potential to exert beneficial effects by virtue of its immunoregulatory effects. Therefore, behavioral interventions based on Qigong geared towards specific pathologies affecting the immune system should be studied and implemented.
The small number of subjects in the sample may be considered, to a certain extent, a limitation of its overall results; thus, it is possible that statistical significance may not have been reached in some variables because of the limited number of subjects. In addition, the relatively short length of the Qigong program (4 weeks), as well as the measuring of immune parameters at only 2 time points throughout the study, may also represent, to some degree, a limitation. Likewise, other possible confounding variables, which have not been strictly controlled in this study, are age and diet, among others. At any rate, future studies should certainly include a larger sample size, with a broader and more diverse profile (eg, age), longer practice programs (over 1 month), more than 2 measures throughout time (including measures in between the program), as well as a strict control of those possible confounding factors. This control could be carried out by means of a more detailed interview or a diary to be completed throughout the program, which would provide a broader and more consistent perspective of the sustained effects of Taoist Qigong on immune parameters.
Conclusions
Taoist Qigong exerts a significant and sustained effect on the immune system, inducing changes in the count of several white blood cell parameters, after a short period of practice of 1 month. This peculiar immunomodulatory profile, apart from its psychobiological interest, has interesting clinical implications. Further research is needed to shed light on the full scope of the effects of Taoist Qigong on the immune system, the mechanisms underlying these effects, as well as the reach of its clinical relevance.
References
1. Vera FM, Manzaneque JM, Maldonado EF, Biochemical changes after a Qigong program: Lipids, serum enzymes, urea, and creatinine in healthy subjects: Med Sci Monit, 2007; 13(12); 560-66
2. Wang CW, Chan CL, Ho RT, The effect of Qigong on depressive and anxiety symptoms: A systematic review and meta-analysis of randomized controlled trials: Evid Based Complement Alternat Med, 2013; 2013; 716094
3. Matos LC, Machado JP, Monteiro FJ, Understanding traditional Chinese medicine therapeutics: An overview of the basics and clinical applications: Healthcare, 2021; 9(3); 257
4. Dorcas A, Yung P, Harmonizing the breath, the body and the mind: Complement Ther Nurs Midwifery, 2003; 9; 198-202
5. Kemp CA, Qigong as therapeutic intervention with older adults: J Holist, 2004; 22; 351-73
6. Casuso-Holgado MJ, Heredia-Rizo AM, Gonzalez-Garcia P, Mind-body practices for cancer-related symptoms management: An overview of systematic reviews including one hundred twenty-nine meta-analyses: Support Care Cancer, 2022; 30(12); 10335-57
7. Pölönen P, Lappi O, Tervaniemi M, Effect of meditative movement on affect and flow in Qigong practitioners: Front Psychol, 2019; 10; 2375
8. Klein P, Picard G, Baumgarden J, Schneider R, Meditative movement, energetic, and physical analyses of three Qigong exercises: Unification of Eastern and Western mechanistic exercise theory: Medicines (Basel), 2017; 4(4); 69
9. Breslau J, Pathways through the border of biomedicine and traditional Chinese medicine: A meeting of medical systems in a Japanese psychiatry department: Cult Med Psychiatry, 2001; 25(3); 251-75
10. Vera FM, Manzaneque JM, Rodriguez-Peña FM, Assessment of hormonal parameters and psychological well-being in healthy subjects after a Taoist Qigong program: An exploratory study: Scand J Psychol, 2019; 60(1); 43-49
11. Vera FM, Manzaneque JM, Rodríguez FM, Acute effects on the counts of innate and adaptive immune response cells after 1 month of Taoist Qigong practice: Int J Behav Med, 2016; 3(2); 198-203
12. Maldonado EF, Vera FM, Manzaneque JM, Efectos de la práctica de Qigong sobre los parámetros hormonales, síntomas de ansiedad, presión arterial y calidad subjetiva de sueño en estudiantes universitarios: Cuad Med Psicosom Psiquiatr Enlace, 2005; 76; 9-15
13. Manzaneque JM, Vera FM, Rodriguez FM, Serum cytokines, mood and sleep after a Qigong program: Is Qigong an effective psychobiological tool? J: Health Psychol, 2009; 14(1); 60-67
14. Chang MYThe theory and practice of health cultivation Qigong exercise in traditional Chinese medicine: Hu Li Za Zhi, 2015; 62(6); 13-19 [in Chinese]
15. Rodrigues JM, Lopes LT, Gonçalves M, Perceived health benefits of taijiquan and Qigong: Altern Ther Health Med, 2022; 23; AT7241
16. Toneti BF, Barbosa RFM, Mano LY, Benefits of Qigong as an integrative and complementary practice for health: A systematic review: Rev Lat Am Enfermagem, 2020; 28; e3317
17. Jahnke R, Larkey L, Rogers C, Comprehensive review of health benefits of Qigong and tai-chi: Am J Health Promot, 2010; 24(6); 1-25
18. Ismail K, Tsang HW, Qigong and suicide prevention: Br J Psychiatry, 2003; 182; 266-70
19. Yeh ML, Lee TI, Chen HH, The influences of Chan-Chuang qi-gong therapy on complete blood cell counts in breast cancer patients treated with chemotherapy: Cancer Nurs, 2006; 29; 149-55
20. Chang PS, Lu Y, Nguyen CM, Effects of Qigong exercise on physical and psychological health among African Americans: West J Nurs Res, 2021; 43(6); 551-62
21. Dorcas A, Chinese Qigong research: An overview: Asian perspectives on psychology, 1997, USA & India, Sage publications
22. Fong SS, Wong JY, Chung LM, Changes in heart-rate variability of survivors of nasopharyngeal cancer during Tai Chi Qigong practice: J Phys Ther Sci, 2015; 27(5); 1577-79
23. Litscher G, Wenzel G, Niederwieser G, Effects of Qigong on brain function: Neurol Res, 2001; 23(5); 501-5
24. Xu M, Tomotake M, Ikuta , The effects of Qigong and acupuncture on human cerebral evoked potentials and electroencephalogram: J Med Invest, 1998; 44; 163-71
25. Anderson JG, Rogers CE, Bossen A, Mind-body therapies in individuals with dementia: An integrative review: Res Gerontol Nurs, 2017; 10(6); 288-96
26. Rodrigues JM, Matos LC, Francisco N, Assessment of Qigong effects on anxiety of high-school students: A randomized controlled trial: Adv Mind Body Med, 2021; 35(3); 10-19
27. Kurt Z, Sice P, Krajewska K, A pilot study on the impacts of lung-strengthening Qigong on wellbeing: Complement Ther Med, 2022; 71; 102891
28. Oh B, Choi SM, Inamori A, Effects of Qigong on depression: A systemic review: Evid Based Complement Altern Med, 2013; 2013; 134737
29. Yeung A, Chan JSM, Cheung JC, Qigong and Tai-Chi for mood regulation: Focus (Am Psychiatr Publ), 2018; 16(1); 40-47
30. Lee MS, Pittler MH, Guo R, Qigong for hypertension: A systematic review of randomized clinical trials: J Hypertens, 2007; 25(8); 1525-32
31. Dong X, Shi Z, Ding M, The effects of Qigong for hypertension: A meta-analysis of randomized controlled trials: Evid Based Complement Alternat Med, 2021; 2021; 5622631
32. Liu D, Yi L, Sheng M, The efficacy of Tai Chi and Qigong exercises on blood pressure and blood levels of nitric oxide and endothelin-1 in patients with essential hypertension: A systematic review and meta-analysis of randomized controlled trials: Evid Based Complement Alternat Med, 2020; 2020; 3267971
33. Lee MS, Chen KW, Choi TY, Qigong for type 2 diabetes care: A systematic review: Complement Ther Med, 2009; 17(4); 236-42
34. Putiri AL, Close JR, Lilly HR, Qigong exercises for the management of type 2 diabetes mellitus: Medicines (Basel), 2017; 4(3); 59
35. Li X, Si H, Chen Y, Effects of fitness Qigong and tai chi on middle-aged and elderly patients with type 2 diabetes mellitus: PLoS One, 2020; 15(12); e0243989
36. Chan CL, Wang CW, Ho RT, A systematic review of the effectiveness of Qigong exercise in cardiac rehabilitation: Am J Chin Med, 2012; 40(2); 255-67
37. Zhao F, Liang C, Zaslawski CJ, Effects of Qigong therapy on the anaerobic threshold in patients with stable coronary artery disease: A randomized controlled trial: Evid Based Complement Alternat Medn, 2022; 2022; 5690569
38. Chen X, Savarese G, Cai Y, Tai Chi and Qigong practices for chronic heart failure: A systematic review and meta-analysis of randomized controlled trials: Evid Based Complement Alternat Med, 2020; 2020; 2034625
39. Chan CL, Wang CW, Ho RT, Qigong exercise for the treatment of fibromyalgia: A systematic review of randomized controlled trials: J Altern Complement Med, 2012; 18(7); 641-46
40. Sawynok J, Lynch ME, Qigong and fibromyalgia circa 2017: Medicines (Basel), 2017; 4(2); 37
41. Sarmento CVM, Moon S, Pfeifer T, The therapeutic efficacy of Qigong exercise on the main symptoms of fibromyalgia: A pilot randomized clinical trial: Integr Med Res, 2020; 9(4); 100416
42. Lee MS, Ernst E, Qigong for movement disorders: A systematic review: Mov Disord, 2009; 24(2); 301-3
43. Wassom DJ, Lyons KE, Pahwa R, Qigong exercise may improve sleep quality and gait performance in Parkinson’s disease: A pilot study: Int J Neurosci, 2015; 125(8); 578-84
44. Li X, Lv C, Liu X, Effects of health Qigong exercise on lower limb motor function in Parkinson’s disease: Front Med (Lausanne), 2022; 8; 809134
45. Chen S, Zhang Y, Wang YT, The effect of Qigong-based therapy on patients with Parkinson’s disease: A systematic review and meta-analysis: Clin Rehabil, 2020; 34(12); 1436-48
46. Chan CL, Wang CW, Ho RT, A systematic review of the effectiveness of Qigong exercise in supportive cancer care: Support Care Cancer, 2012; 20(6); 1121-33
47. Oh B, Butow P, Mullan B, A critical review of the effects of medical Qigong on quality of life, immune function, and survival in cancer patients: Integr Cancer Ther, 2012; 11; 101-10
48. Kuo CC, Wang CC, Chang WL, Clinical effects of baduanjin Qigong exercise on cancer patients: A systematic review and meta-analysis on randomized controlled trials: Evid Based Complement Alternat Med, 2021; 2021; 6651238
49. Xu J, Li H, Sze DM, Effectiveness of Qigong and tai chi in the quality of life of patients with cancer: Protocol for an umbrella review: BMJ Open, 2022; 12(4); e057980
50. Oh B, Bae K, Lamoury G, The effects of Tai Chi and Qigong on immune responses: A systematic review and meta-analysis: Medicines (Basel), 2020; 7(7); 39
51. Ryu H, Jun CD, Lee BS, Effect of Qigong training on proportions of T lymphocyte subsets in human peripheral blood: Am J Chin Med, 1995; 23; 27-36
52. Tai H-C, Chou Y-S, Tzeng I-S, Effect of Tai Chi synergy T1 exercise on autonomic function, metabolism, and physical fitness of healthy individuals: Evid Based Complement Alternat Med, 2018; 2018; 6351938
53. Lee MS, Kim MK, Ryu H, Qi-training (Qigong) enhanced immune functions: What is the underlying mechanism?: Int J Neurosci, 2005; 115(8); 1099-104
54. Liu J, Chen P, Wang R, Yuan , Effect of Tai Chi on mononuclear cell functions in patients with non-small cell lung cancer: Complement Altern Med, 2015; 15; 3
55. Yang Y, Verkuilen J, Rosengren KS, Effects of a traditional Taiji/Qigong curriculum on older adults immune response to influenza vaccine: Med Sport Sci, 2008; 52; 64-76
56. Dinas PC, Koutedakis Y, Ioannou LG, Effects of exercise and physical activity levels on vaccination efficacy: A systematic review and meta-analysis: Vaccines (Basel), 2022; 10(5); 769
57. Manzaneque JM, Vera FM, Maldonado EF, Assessment of immunological parameters following a Qigong training program: Med Sci Monit, 2004; 10(6); 264-70
58. Vanker N, Ipp H, Large unstained cells: A potentially valuable parameter in the assessment of immune activation levels in HIV infection: Acta Haematol, 2014; 131(4); 208-12
59. Gomez-Llorente MA, Martínez Cañavate A, Chueca N, Multi-omics approach reveals new signatures in obese allergic asthmatic children: Biomedicines, 2020; 8(9); 359
60. Rosniak-Bąk K, Jelen A, Bak M, Analysis of separation of white blood cells in peripheral blood as an indicator of MPO deficiency: Ann Clin Lab Sci, 2017; 47(4); 422-31
61. Cohen J: Statistical power analysis for the behavioral sciences, 1988, Lawrence Erlbaum Associates
62. Liao P-C, Lin H-H, Chiang B-L, Tai Chi chuan exercise improves lung function and asthma control through immune regulation in childhood asthma: Evid Based Complement Alternat Med, 2019; 2019; 9146827
63. Solberg EE, Halvorsen R, Sundgot-Borgen J, Meditation: A modulator of the immune response to physical stress? A brief report: Br J Sports Med, 1995; 29(4); 255-57
64. Solberg EE, Halvorsen R, Holen A, Effect of meditation on immune cells: Stress Med, 2000; 16; 185-90
65. Taylor DN, Effects of a behavioral stress-management program on anxiety, mood, self-esteem, and T-cell count in HIV positive men: Psychol Rep, 1995; 76; 451-57
66. Raghunath K, Sumathi CH, Rajappa Senthil J, Impact of naturopathy, yoga, and dietary interventions as adjuvant chemotherapy in the management of stage II and III adenocarcinoma of the colon: J Colorectal Dis, 2020; 35(12); 2309-22
67. Infante JR, Peran F, Rayo JI, Levels of immune cells in transcendental meditation practitioners: Int J Yoga, 2014; 7(2); 147-51
68. Pedersen BK, Toft AD, Effects of exercise on lymphocytes and cytokines: Br J Sports Med, 2000; 34(4); 246-51
69. Matthews CE, Ockene IS, Freedson PS, Moderate to vigorous physical activity and risk of upper-respiratory tract infection: Med Sci Sports Exerc, 2002; 34(8); 1242-48
70. Zaldivar F, McMurray RG, Nemet D, Body fat and circulating leukocytes in children: Int J Obes (Lond), 2006; 30(6); 906-11
71. Lee MS, Huh HJ, Jeong SM, Effects of Qigong on immune cells: Am J Chin Med, 2003; 31(2); 327-35
72. Yao BSA preliminary study on the changes of T-cell subsets in patients with aplastic anemia treated with Qigong: Zhong Xi Yi Jie He Za Zhi, 1989; 9(6); 341-42 [in Chinese]
73. Ng BHP, Tsang HWT, Psychophysiological outcomes of health Qigong for chronic conditions: A systematic review: Psychophysiology, 2009; 46(2); 257-69
74. Jiang T, Hou J, Sun R, Immunological and psychological efficacy of meditation/yoga intervention among people living with HIV (PLWH): A systematic review and meta-analyses of 19 randomized controlled trials: Ann Behav Med, 2021; 55(6); 505-19
75. McCain NL, Gray DP, Elswick RK, A randomized clinical trial of alternative stress management interventions in persons with HIV infection: J Consult Clin Psychol, 2008; 76(3); 431-41
76. Bononi A, Lanza F, Dabusti M, Increased myeloperoxidase index and large unstained cell values can predict the neutropenia phase of cancer patients treated with standard dose chemotherapy: Cytometry, 2001; 15(46); 92-97
77. Shin D, Lee MS, Kimdo Y, Increased large unstained cells value in varicella patients: A valuable parameter to aid rapid diagnosis of varicella infection: J Dermatol, 2015; 42(8); 795-99
78. Keskin M, Burcak Polat S, Ateş I, Are neutrophil-to-lymphocyte ratios and large unstained cells different in hospitalized COVID-19 PCR-positive patients with and without diabetes mellitus?: Eur Rev Med Pharmacol Sci, 2022; 26(16); 5963-70
79. Zefferino R, Di Gioia S, Conese M, Molecular links between endocrine, nervous and immune system during chronic stress: Brain Behav, 2021; 11(2); e01960
80. Carvalho LA, Gerdes JM, Strell C, Interplay between the endocrine system and immune cells: Biomed Res Int, 2015; 2015; 986742
81. Millard AL, Valli PV, Stussi G, Brief exercise increases peripheral blood NK cell counts without immediate functional changes, but impairs their responses to ex vivo stimulation: Front Immunol, 2013; 4; 1-12
82. Atanackovic D, Nowottne U, Freier E, Acute psychological stress increases peripheral blood CD3+CD56+ natural killer T cells in healthy men: Possible implications for the development and treatment of allergic and autoimmune disorders: Stress, 2013; 16(4); 421-28
83. Schwindt CD, Zaldivar F, Wilson L, Do circulating leucocytes and lymphocyte subtypes increase in response to brief exercise in children with and without asthma?: Br J Sports Med, 2007; 41(1); 34-40
84. Cvitanovic H, Milosevic M, Bukvic-Beslic I, Determination of psychological stress, serum immune parameters, and cortisol levels in patients with human papilloma virus: AG Clin Ther, 2020; 42(5); 783-99
85. Poller WC, Downey J, Mooslechner AA, Brain motor and fear circuits regulate leukocytes during acute stress: Nature, 2022; 607; 578-84
86. Van Craenenbroek AH, Van Ackeren K, Hoymans VY, Acute exercise-induced response of monocyte subtypes in chronic heart and renal failure: Mediators Inflamm, 2014; 2014; 216534
87. Schreiber S, Monocytes or T cells in Crohn’s disease: Does IL-16 allow both to play at that game?: Gut, 2001; 49(6); 747-48
88. Rabah H, Itani A, Chalhoub M, Leukocytes in critical patients with asthma exacerbation: Cureus, 2021; 13(12); e20520
89. Fang W, Zhang Y, Chen Z, Innate lymphoid cells in inflammatory arthritis: Arthritis Res Ther, 2020; 22(1); 25
In Press
07 May 2024 : Clinical Research
Treatment of AVN-Induced Proximal Pole Scaphoid Nonunion Using a Fifth and Fourth Extensor Compartmental Ar...Med Sci Monit In Press; DOI: 10.12659/MSM.944553
16 Mar 2024 : Clinical Research
Diagnostic Efficiency of ACR-TIRADS Score for Differentiating Benign and Malignant Thyroid Nodules of Vario...Med Sci Monit In Press; DOI: 10.12659/MSM.943228
08 May 2024 : Clinical Research
Effect of Individualized PEEP Guided by Driving Pressure on Diaphragm Function in Patients Undergoing Lapar...Med Sci Monit In Press; DOI: 10.12659/MSM.944022
21 Mar 2024 : Clinical Research
Impact of Serum Vitamin D, B6, and B12 and Cognitive Functions on Quality of Life in Peri- and Postmenopaus...Med Sci Monit In Press; DOI: 10.12659/MSM.943249
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952