20 August 2023: Clinical Research
Correlation Between Third Molar Mineralization and Midpalatal Suture Maturity: A Cone Beam Computed Tomography Study
Simona Šefeldaitė1ABCDEF, Austėja Mitalauskienė1BCDF, Giedrė Trakinienė1E, Arunas VasiliauskasDOI: 10.12659/MSM.940539
Med Sci Monit 2023; 29:e940539
Abstract
BACKGROUND: Midpalatal suture ossification varies in patients of different ages, which can lead to making inaccurate presumptions when considering effective treatment timing based on chronological age. Chronological age provides only general information, whereas dental development correlates with skeletal growth, which suggests that tooth mineralization could be considered to be a precise criterion for determining the midpalatal suture’s maturity. The present study was conducted to investigate the association between third-molar mineralization and midpalatal suture’s maturation stages using cone-beam computed tomography (CBCT) images.
MATERIAL AND METHODS: The study involved 97 CBCT images of patients aged 8-37 years with normal growth and development. Subjects with cleft lip and palate, caries treatment, or present cavities in the third molars were not included in the study. The stages of midpalatal suture ossification were evaluated according to the protocol suggested by Angelieri et al, and the third-molar mineralization degree was measured by the Demirjian index. Statistical analysis was performed to evaluate correlations between the variables.
RESULTS: Patients with advanced third-molar mineralization stages were found to have greater midpalatal suture maturity. A statistically significant positive correlation was found between the stages of third-molar mineralization and midpalatal suture maturation (R=0.814, P<0.01). Third-molar development was also found to be associated with chronological age (R=0.883, P<0.01).
CONCLUSIONS: A measure of third-molar mineralization does not allow for accurate determination of the midpalatal suture maturation stage.
Keywords: Age Factors, Cone-Beam Computed Tomography, Cranial Sutures, Maxilla, Molar, Third, Palatal Expansion Technique, Palate, Hard, Tooth Calcification, Humans, Cleft Lip, Cleft Palate, Sutures, Calcinosis
Background
Transversal maxillary deficiency is a common skeletal discrepancy that leads to discordant growth of the facial and dentoalveolar structures [1]. This discrepancy is characterized by an inadequate transversal relationship of maxillary and mandibular teeth, also defined as a cross-bite [2]. Maxillary expansion (ME) is one of the most common procedures used in orthodontics to treat cross-bites and dental crowding. The main goal of ME is to separate the midpalatal suture and achieve mostly skeletal expansion with the least possible dentoalveolar changes. ME provides increased dental arch perimeter and balance between the width of the upper and lower jaws. However, this procedure has to be performed before the midpalatal suture fuses. Once advanced ossification begins, invasive and expensive surgically assisted techniques are required to provide skeletal expansion [3]. Identifying the midpalatal suture (MPS) maturation stage can play an essential role in preventing treatment complications such as expansion failure, pain, periodontal problems, and undesired buccal tipping with extrusion of the posterior teeth [4–7]. Several attempts have been made to predict midpalatal suture ossification based on the patients’ chronological age, although a few recent studies found that MPS ossification does not depend on age in young adults and demonstrated cases where skeletal maturity exceeded chronological age [8–13].
With the widespread application of three-dimensional (3D) imaging techniques in everyday dental practice, CBCT has become an accessible tool for evaluating MPS fusion and morphology [14]. In 2013, Angelieri et al developed a 5-stage system that classifies the midpalatal suture by observing the suture in CBCT images [9,10]. Despite constructive results, there is debate about the application of CBCT in every case, as it means exposure to ionizing radiation and the resulting radiation doses of three-dimensional (3D) images are higher compared to two-dimensional (2D) radiographs [15,16]. This is why new, effective, safe alternatives to evaluate the suture by using CBCT imaging are needed. In this regard, attempts were made to find the relationship between MPS maturation and other commonly used indices in orthodontics. A less invasive method, known as the hand-wrist method (HWM), has been used as the criterion standard for evaluating skeletal maturity [3]; it involves taking a wrist radiograph and assessing the characteristic features of the selected metaphyseal phalangeal cartilages and the radial bone. The cervical vertebral maturation (CVM) method also eliminates additional patient radiation since it only requires a cephalometric radiograph [17]. Demirjian et al proposed another practical and easily implementable diagnostic method to evaluate dental age based on tooth mineralization degree seen in panoramic radiographs (Figure 1). To summarize, the author proposed 8 stages (A to H) of tooth calcification, ranging from calcification of the cusp tip to the closure of the apex [18,19]. The third molars are the last teeth to develop in the dental arch and complete their formation when the skeletal growth is finished. Therefore, their mineralization might be related to an individual’s skeletal development [20–22].
There is limited research on the relationship between midpalatal suture mineralization and the development stages of mandibular third molars, creating a need for this study. Used as a diagnostic tool to estimate the timing of the pubertal growth spurt and to select the best possible treatment for patients with transverse maxillary deficiency, the Demirjian index could become part of a regular small effective dose 2D radiographs in orthodontic practice. Combining the mandibular third molars and midpalatal suture maturation diagnostics could make possible a low-radiation diagnostic technique for individual evaluation before orthodontic treatment of transverse maxillary deficiencies for adolescents and young adults.
The null hypothesis is that midpalatal suture mineralization is not associated with the development stages of mandibular third molars. The primary aim of this study was to evaluate the relationship between maturity of the midpalatal suture and the third-molar mineralization stages.
Material and Methods
STUDY DESIGN AND ETHICS APPROVAL:
Ninety-seven diagnostic CBCTs acquired for clinical purposes were examined in this retrospective, cross-sectional study. The CBCT images were randomly selected and stratified based on patient age. The sample size was calculated using G*Power 3 for a single-sample
ELIGIBILITY CRITERIA:
The study involved good-quality CBCT images taken between 2008 and 2019 in 1 dental clinic in Kaunas, Lithuania, using consistent techniques. Based on the inclusion criteria, we selected patients of both sexes, aged 8–37 years, who had undergone a CBCT for diagnostic purposes prior to dental treatment. Subjects with previous or ongoing orthodontic treatment, cleft lip and palate, caries treatment, or present cavities in the mandibular third molars were excluded from the study. All selected CBCT images were taken using an i-CAT scanner (Imaging Sciences International, Inc., Hatfield, PA, USA; 120 kVp, 3–8 mA, 8–11 cm field of view, 0.2–0.40 mm voxel resolution, 26.9 acquisition time). The head of the patient was fixed to the headrest with a strap to minimize movement. The images were analyzed using the i-CAT viewing (Imaging Science International, Inc.) software program. The best-quality panoramic images were saved from the same scans.
EVALUATION OF MIDPALATAL SUTURE’S OSSIFICATION:
The MPS assessment from the CBCT images was performed according to the protocol suggested by Angelieri et al [9,10]. The head was positioned in the axial, sagittal, and transversal planes. An axial cross-section was used to evaluate the suture. A middle cross-section in the sagittal plane was applied to assess the palate’s horizontal layout (parallel to the horizontal line of the software program). After establishing a horizontal line along the palate, a central cross-section from the upper and lower dimensions (from the nose to the mouth’s surface) was used to classify the stages of midpalatal suture. For individuals with curved palate (ie, anterior and posterior palatal areas not correspondingly distributed in the same section), the suture was divided into 2 central axial cross-sections, with the anterior and posterior suture’s areas assessed separately. The final image of the MPS was evaluated in the axial plane. All CBCT images were examined by experienced investigators (S.Š and T.V). Based on the MPS maturation stage, patients were divided into 4 groups: A and B stages were combined into 1 AB group because the expansion of the suture is the most effective in those stages; groups C, D, and E were evaluated separately (Figure 2).
ASSESSMENT OF THIRD-MOLAR MINERALIZATION:
Mineralization of the mandibular third-molar (M3) was determined according to Demirjian et al’s classification of mineralization stages A through H, using panoramic images [18,19]. The mandibular left third-molar mineralization stages that mark the completion of the crown formation up to the cemento-enamel junction (A, B, and C) were considered as 1 group, whereas other stages were not grouped (Figure 3). All panoramic images were examined by orthodontists (G.T. and A.V.). Following previous research, the stage of mineralization was evaluated for M3, and stage D was decided to represent the time right before adolescent growth was completed [22]. The mandibular right third-molar was chosen for assessment when it was impossible to assess the left molar (ie, it was missing).
SUBJECTS’ DISTRIBUTION:
Patients were randomly selected and divided into 4 age groups: younger than 14, 14–18, 19–25, and over 25 years, as in the original study conducted by Angelieri et al [9,10]. The CBCT scans were coded to hide the individual’s identity from the observers. The evaluation of the CBCT images was carried out twice by each of the 2 examiners 2 weeks apart.
STATISTICAL ANALYSIS:
Statistical analyses were performed using the IBM SPSS 20 (IBM Corp., Armonk, NY, USA) statistical software package. The correlations between the stages of midpalatal suture maturation and the third-molar mineralization were evaluated by Spearman’s rank correlation coefficient (R) for the significance of relationship.
The intra-examiner and inter-examiner measured error was evaluated with the weighted Cohen’s kappa coefficient, and the results were interpreted using the method of Landis and Koch. The intra-observer kappa coefficient value was 0.937, and the inter-observer value was 0.862.
Patient distribution was calculated in percentage. A significance level of 5% was considered, meaning that the results were considered statistically significant when the significance level was less than 0.05 (
Results
SAMPLE DEPICTION:
The study sample consisted of 97 patients, 59 females and 38 males, aged 8–37 years (mean age 18.4 years, SD 7.4). Patients’ distribution among age groups was the following: 23 patients were younger than 14 years, 24 patients were 14–18 years, 25 patients were 19–25 years, and 25 patients were older than 25 years. Age groups were homogenous and subjects were distributed almost in the same percentage (χ2=0.361, df=3,
MIDPALATAL SUTURE’S OSSIFICATION:
Table 1 describes the distribution of the MPS maturation stages among different age groups. The most frequently observed MPS maturation stage was stage E, followed by stage D, then C and AB. The nonparametric Kruskal-Wallis test showed a statistically significant difference between the mean age of patients in stages AB–E 5.8 years (P<0.001, SE 1.99) and C–E 6.5 years (P<0.05, SE 1.80).
THE RELATIONSHIP BETWEEN THE THIRD MOLARS’ MINERALIZATION DEGREE, CHRONOLOGICAL AGE, AND MIDPALATAL SUTURE’S MATURITY:
Table 2 shows distribution of the M3 mineralization stages and MPS maturation stages among patients. The most frequent molar mineralization stage, H, was observed only in adults (ages 19 and older). The second most frequent stage, D, was observed only among adolescent patients. Stage G was observed in all patients older than 14 years. The third molar development was found to be associated with chronological age (R=0.833, P<0.01). All participants with an open midpalatal suture (stage AB) had their third molars formed only up to the cemento-enamel junction (stages ABC and D). Statistically significant Spearman’s rank correlation (R=0.814, P<0.01) was found between third-molar mineralization and MPS maturation. According to sex, MPS maturation stage AB was significantly more common in boys (χ2=10.749, df=3, P=0.013), while stage D was more common in girls, although the distribution was not significantly different by sex and age groups.
Discussion
The midpalatal suture evaluation and patient’s chronological age influences the decision of whether to perform conventional or surgically assisted maxillary expansion. The results of our study showed that MPS ossification increased with patient age, although recent studies found no significant relationship between closure of the suture and age. A study by Haghanifar et al evaluated suture morphology in 10-year age groups, which revealed wide variations in subjects over 20 years of age, with 50% of the subjects over 20 years of age having completely open sutures [23]. N’Guyen et al carried out a study on 20 patients over 70 years of age and reported that midpalatal suture could potentially remain incompletely closed, even in the elderly [24]. The interpretations of the results, suggested diagnostic tools, and treatment timing vary among researchers. While a few years ago maxillary expansion was considered successful in patients younger than 16 years, recent studies show results of effective maxillary expansion to patients up until 20 years old [25]. In adults, the ossification of MPS differs significantly, and, correspondingly, chronological age does not reliably predict treatment outcome. Considering MPS maturation stage C being the borderline of the successful palatal expansion, 33 out of 97 of our study subjects (34%) had an open suture. The interdigitations may be regarded as the expression of a functional phenomenon, as they do not occur if the suture develops without being influenced by functional forces. According to Angelieri et al, patients in MPS maturation stages A through C could be managed by conventional expansion, but in the more matured groups (D and E), surgical expansion should be considered [26]. The literature also describes sex-based differences in evaluating MPS maturity and third-molar mineralization, although authors disagree and more studies need to be conducted. Our study did not subdivide results according to sex considering no significant difference between age groups when accounted for sex was found.
Since the borderline for the shift from conventional to surgical expansion performance is not clear, more attention to MPS diagnostics is required. A few of the most commonly applied diagnostic tools for the evaluation of the MPS maturity are cone-beam computed tomography, hand-wrist maturation, and cervical vertebrae maturation indices, although their implications as presented in the literature are limited, mostly due to young patients’ exposure to ionizing radiation and difficulty in analyzing suggested landmarks [27].
Dental and skeletal maturity has been a common investigation subject in many studies, as tooth mineralization stages seen in radiographic images appear to be correlated with skeletal growth [28]. Trakinienė et al conducted a twin study, which concluded that mineralization of the third molars’ roots was determined more by genetic factors (60–63%) than by general environmental factors (20–27%) [20,21]. Therefore, the stages of dental mineralization in panoramic radiographs could be used as a diagnostic tool to estimate the timing of the pubertal growth spurt. A study conducted by Al-Balbeesi et al suggested that the third molars’ mineralization stage D corresponded mainly with the CVM stage III, meaning that the mineralization stage D could be an indicator for predicting a patient’s growth spurt [29]. Similar results were presented by Mehta et al, who found that the M3 stage D was mostly seen in patients with CVM stage III [22]. A study by Duangto et al proposed that the third molars’ mineralization stages A–C, measured by the Demirjian index, could represent a patient’s age younger than 15 years, and stages A–D could represent an age younger than 18 years [30]. These findings match our study’s results because most patients in stages A–C were younger than 14, and none of the patients over age 18 had a stage D or above measured.
One of the reasons why third molars were used in this research is that they continue developing after puberty. Another aspect to consider is the common absence of third molars. Genetics play an important role in third molar absence, and agenesis of third molars was more often observed in the mandible than in the maxilla. If third molars are missing, our method cannot be applied and tested. The results of our study emphasize the importance of the Demirjian index, a measure of third-molar mineralization, in predicting the degree of midpalatal suture maturation. The Demirijian index is a convenient, easy-to-use tool that only requires a 2-dimensional panoramic radiograph, which is easily accessible to every dental practitioner. Future longitudinal research studies with larger and more extensive populations and more dental age estimation methods (eg, Nolla and Willems) should be conducted to investigate the utility of this method for midpalatal suture evaluation.
Conclusions
The present findings demonstrate a strong, statistically significant positive correlation between the Demirjian index and midpalatal suture maturation stage. Although within the limitations of the study a measure of third-molar mineralization does not allow for accurate determination of the midpalatal suture maturation stage, the Demirjian index has the potential to become diagnostic tool to evaluate midpalatal suture maturity, according to patient’s third-molar mineralization as shown in 2D panoramic images.
Figures
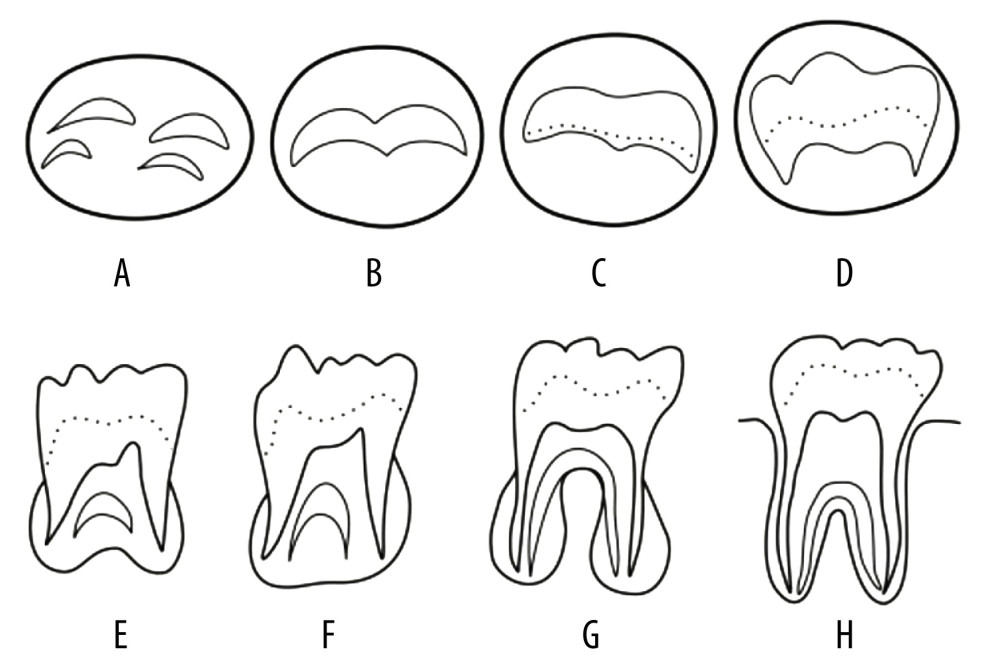 Figure 1. Tooth mineralization stages according to Demirjian et al. (1973). Stage A: Calcification of the occlusal surface occurs without fusion; Stage B: Formation of occlusal surface by fusion of the mineralization points; Stage C: Enamel is formed and the formation of dentin has started, with no pulp horns in the pulp chamber; Stage D: Crown is formed up to the cement–enamel junction, with commencement of root formation; Stage E: The roots are shorter than the crown height and the radicular bifurcation is calcified; Stage F: The roots are equal or longer than the crown height; Stage G: The walls of the root canal are parallel, with the apical ends open; Stage H: The apexes of the roots are closed.
Figure 1. Tooth mineralization stages according to Demirjian et al. (1973). Stage A: Calcification of the occlusal surface occurs without fusion; Stage B: Formation of occlusal surface by fusion of the mineralization points; Stage C: Enamel is formed and the formation of dentin has started, with no pulp horns in the pulp chamber; Stage D: Crown is formed up to the cement–enamel junction, with commencement of root formation; Stage E: The roots are shorter than the crown height and the radicular bifurcation is calcified; Stage F: The roots are equal or longer than the crown height; Stage G: The walls of the root canal are parallel, with the apical ends open; Stage H: The apexes of the roots are closed. 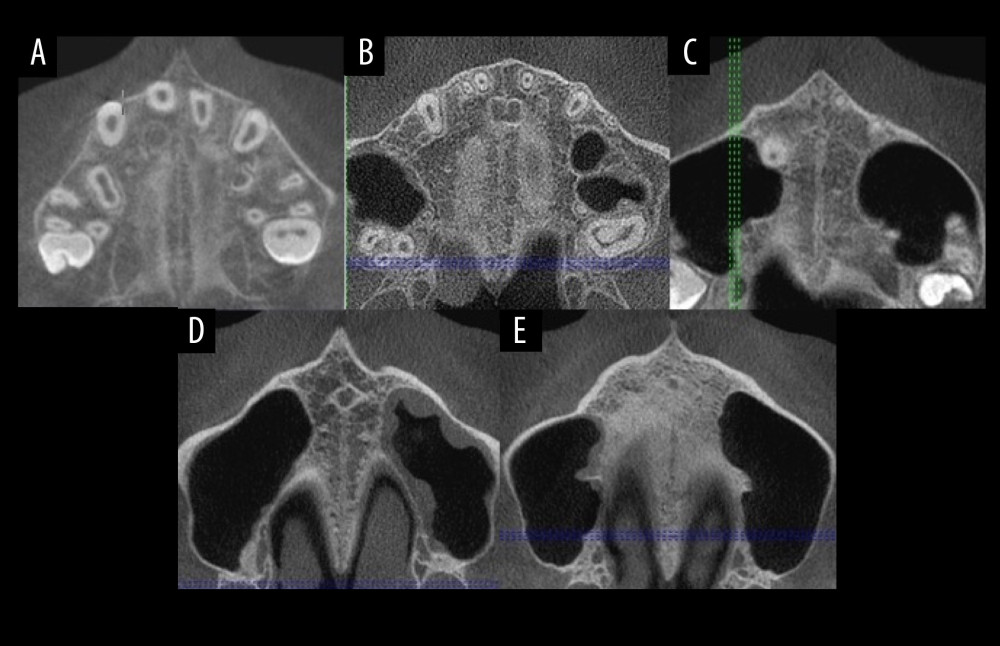 Figure 2. (A–E) Midpalatal suture maturation stages.
Figure 2. (A–E) Midpalatal suture maturation stages. 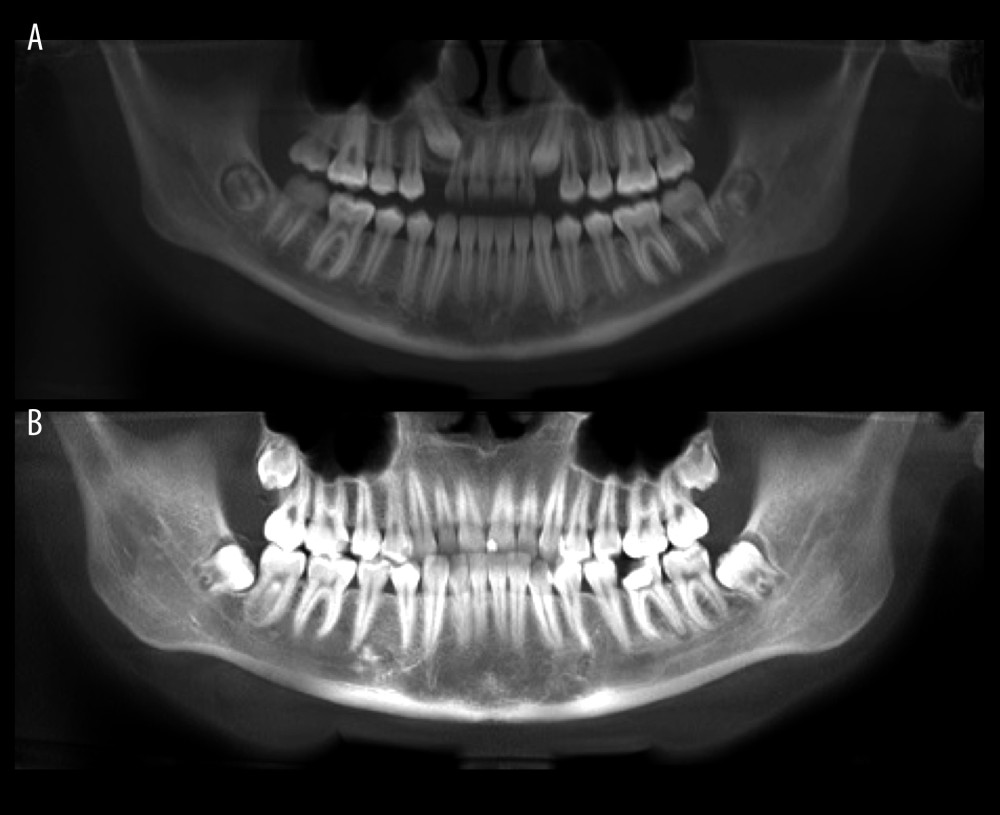 Figure 3. Panoramic images for assessment of the third-molar mineralization: stage C (A) and stage F (B).
Figure 3. Panoramic images for assessment of the third-molar mineralization: stage C (A) and stage F (B). References
1. Andrucioli MCD, Matsumoto MAN, Transverse maxillary deficiency: Treatment alternatives in face of early skeletal maturation: Dental Press J Orthod, 2020; 25(1); 70-79
2. lmeida RR, Almeida MR, Oltramari-Navarro PV, Posterior crossbite – treatment and stability: J Appl Oral Sci, 2012; 20(2); 286-94
3. Shayani A, Sandoval Vidal P, Garay Carrasco I, Merino Gerlach M, Midpalatal suture maturation method for the assessment of maturation before maxillary expansion: A systematic review: Diagnostics (Basel), 2022; 12(11); 2774
4. Krooks L, Pirttiniemi P, Kanavakis G, Lähdesmäki R, Prevalence of malocclusion traits and orthodontic treatment in a Finnish adult population: Acta Odontol Scand, 2016; 74(5); 362-67
5. Feldmann I, Bazargani F, Pain and discomfort during the first week of rapid maxillary expansion (RME) using two different RME appliances: A randomized controlled trial: Angle Orthod, 2017; 87(3); 391-96
6. Izuka EN, Feres MF, Pignatari SS, Immediate impact of rapid maxillary expansion on upper airway dimensions and on the quality of life of mouth breathers: Dental Press J Orthod, 2015; 20(3); 43-49
7. Bazargani F, Magnuson A, Ludwig B, Effects on nasal airflow and resistance using two different RME appliances: A randomized controlled trial: Eur J Orthod, 2018; 40(3); 281-84
8. Calfee RP, Sutter M, Steffen JA, Goldfarb CA, Skeletal and chronological ages in American adolescents: Current findings in skeletal maturation: J Child Orthop, 2010; 4(5); 467-70
9. Angelieri F, Cevidanes LH, Franchi L, Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion: Am J Orthod Dentofacial Orthop, 2013; 144(5); 759-69
10. Angelieri F, Franchi L, Cevidanes LH, Prediction of rapid maxillary expansion by assessing the maturation of the midpalatal suture on cone beam CT: Dental Press J Orthod, 2016; 21(6); 115-25
11. Korn EL, Baumrind S, Transverse development of the human jaws between the ages of 8.5 and 15.5 years, studied longitudinally with use of implants: J Dent Res, 1990; 69(6); 1298-306
12. Knaup B, Yildizhan F, Wehrbein H, Age-related changes in the midpalatal suture. A histomorphometric study: J Orofac Orthop, 2004; 65(6); 467-74
13. Korbmacher H, Schilling A, Püschel K, Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture: J Orofac Orthop, 2007; 68(5); 364-76
14. Isfeld D, Flores-Mir C, Leon-Salazar V, Lagravère M, Evaluation of a novel palatal suture maturation classification as assessed by cone-beam computed tomography imaging of a pre- and postexpansion treatment cohort: Angle Orthod, 2019; 89(2); 252-61
15. Garib DG, Calil LR, Leal CR, Janson G, Is there a consensus for CBCT use in Orthodontics?: Dental Press J Orthod, 2014; 19(5); 136-49
16. Colceriu-Şimon IM, Băciuţ M, Ştiufiuc RI, Clinical indications and radiation doses of cone beam computed tomography in orthodontics: Med Pharm Rep, 2019; 92(4); 346-51
17. Szemraj A, Wojtaszek-Słomińska A, Racka-Pilszak B, Is the cervical vertebral maturation (CVM) method effective enough to replace the hand-wrist maturation (HWM) method in determining skeletal maturation? – a systematic review: Eur J Radiol, 2018; 102; 125-28
18. Demirjian A, Goldstein H, New systems for dental maturity based on seven and four teeth: Ann Hum Biol, 1976; 3(5); 411-21
19. Demirjian A, Goldstein H, Tanner JM, A new system of dental age assessment: Hum Biol, 1973; 45(2); 211-27
20. Trakinienė G, Smailienė D, Kučiauskienė A, Evaluation of skeletal maturity using maxillary canine, mandibular second and third molar calcification stages: Eur J Orthod, 2016; 38(4); 398-403
21. Trakinienė G, Andriuškevičiūtė I, Šalomskienė L, Genetic and environmental influences on third molar root mineralization: Arch Oral Biol, 2019; 98; 220-25
22. Mehta N, Patel D, Mehta F, Evaluation of skeletal maturation using mandibular third molar development in Indian adolescents: J Forensic Dent Sci, 2016; 8(2); 112
23. Haghanifar S, Mahmoudi S, Foroughi R, Assessment of midpalatal suture ossification using cone-beam computed tomography: Electron Physician, 2017; 9(3); 4035-41
24. N’Guyen T, Ayral X, Vacher C, Radiographic and microscopic anatomy of the mid-palatal suture in the elderly: Surg Radiol Anat, 2008; 30(1); 65-68
25. Jimenez-Valdivia LM, Malpartida-Carrillo V, Rodríguez-Cárdenas YA, Midpalatal suture maturation stage assessment in adolescents and young adults using cone-beam computed tomography: Prog Orthod, 2019; 20(1); 38
26. Sayar G, Kılınç DD, Rapid maxillary expansion outcomes according to midpalatal suture maturation levels: Prog Orthod, 2019; 20(1); 27
27. Lurie AG, Doses, benefits, safety, and risks in oral and maxillofacial diagnostic imaging: Health Phys, 2019; 116(2); 163-69
28. Chertkow S, Tooth mineralization as an indicator of the pubertal growth spurt: Am J Orthod, 1980; 77(1); 79-91
29. Al-Balbeesi HO, Al-Nahas NW, Baidas LF, Correlation between skeletal maturation and developmental stages of canines and third molars among Saudi subjects: Saudi Dent J, 2018; 30(1); 74-84
30. Duangto P, Iamaroon A, Prasitwattanaseree S, New models for age estimation and assessment of their accuracy using developing mandibular third molar teeth in a Thai population: Int J Legal Med, 2017; 131(2); 559-68
Figures
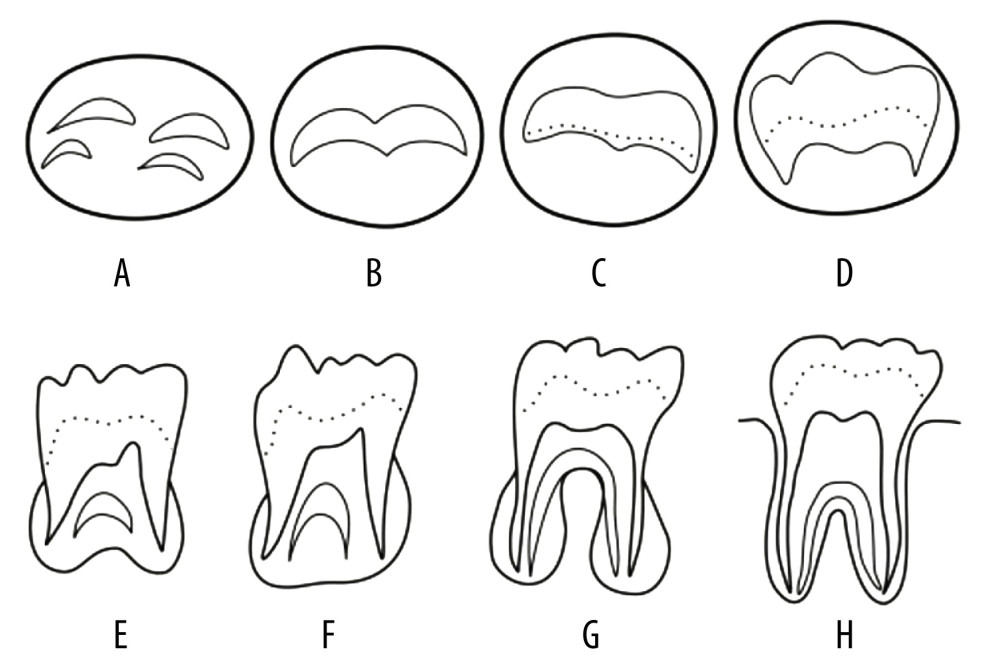 Figure 1. Tooth mineralization stages according to Demirjian et al. (1973). Stage A: Calcification of the occlusal surface occurs without fusion; Stage B: Formation of occlusal surface by fusion of the mineralization points; Stage C: Enamel is formed and the formation of dentin has started, with no pulp horns in the pulp chamber; Stage D: Crown is formed up to the cement–enamel junction, with commencement of root formation; Stage E: The roots are shorter than the crown height and the radicular bifurcation is calcified; Stage F: The roots are equal or longer than the crown height; Stage G: The walls of the root canal are parallel, with the apical ends open; Stage H: The apexes of the roots are closed.
Figure 1. Tooth mineralization stages according to Demirjian et al. (1973). Stage A: Calcification of the occlusal surface occurs without fusion; Stage B: Formation of occlusal surface by fusion of the mineralization points; Stage C: Enamel is formed and the formation of dentin has started, with no pulp horns in the pulp chamber; Stage D: Crown is formed up to the cement–enamel junction, with commencement of root formation; Stage E: The roots are shorter than the crown height and the radicular bifurcation is calcified; Stage F: The roots are equal or longer than the crown height; Stage G: The walls of the root canal are parallel, with the apical ends open; Stage H: The apexes of the roots are closed.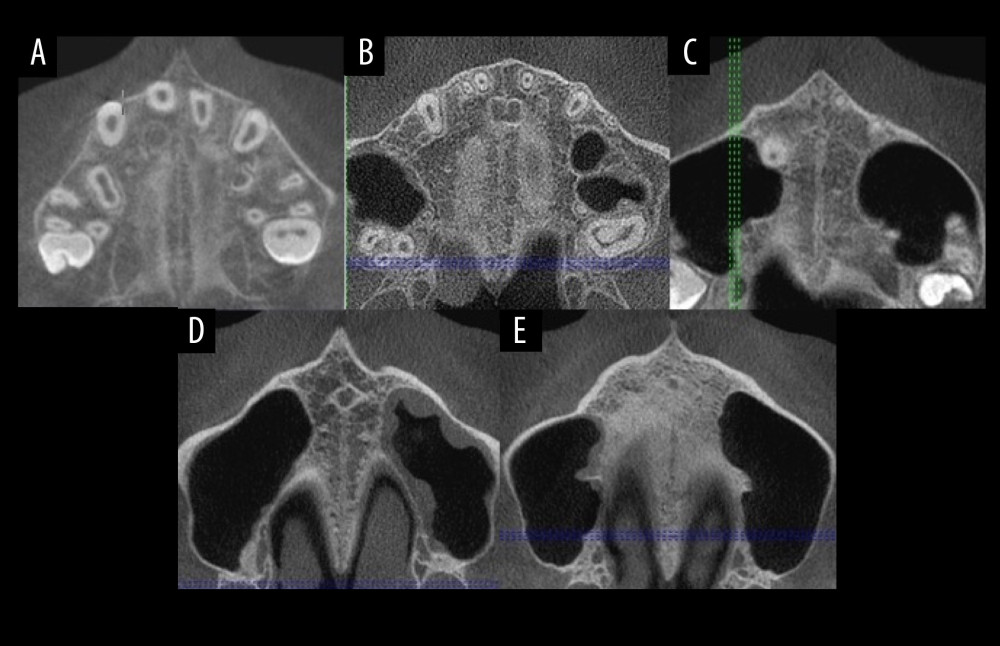 Figure 2. (A–E) Midpalatal suture maturation stages.
Figure 2. (A–E) Midpalatal suture maturation stages.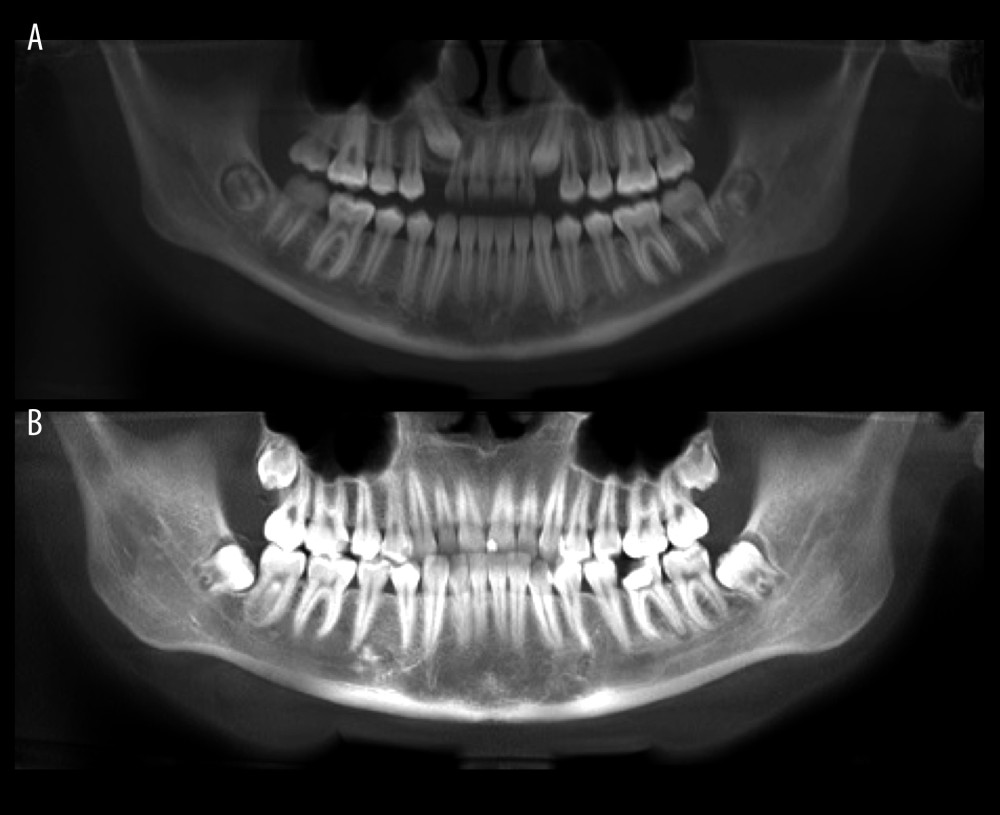 Figure 3. Panoramic images for assessment of the third-molar mineralization: stage C (A) and stage F (B).
Figure 3. Panoramic images for assessment of the third-molar mineralization: stage C (A) and stage F (B). Tables
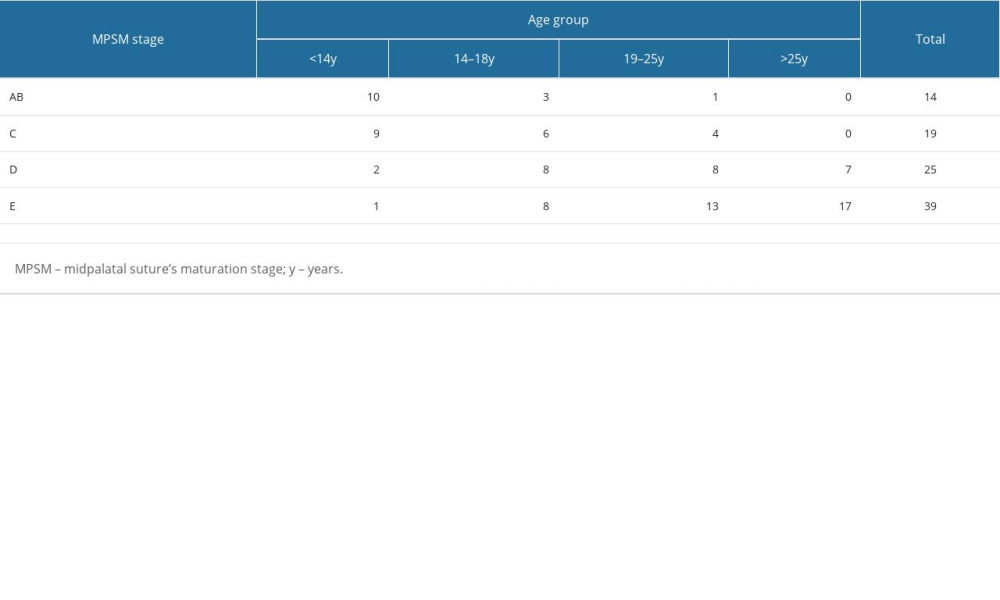 Table 1. Frequency of midpalatal suture maturation stages in different patient age groups.
Table 1. Frequency of midpalatal suture maturation stages in different patient age groups.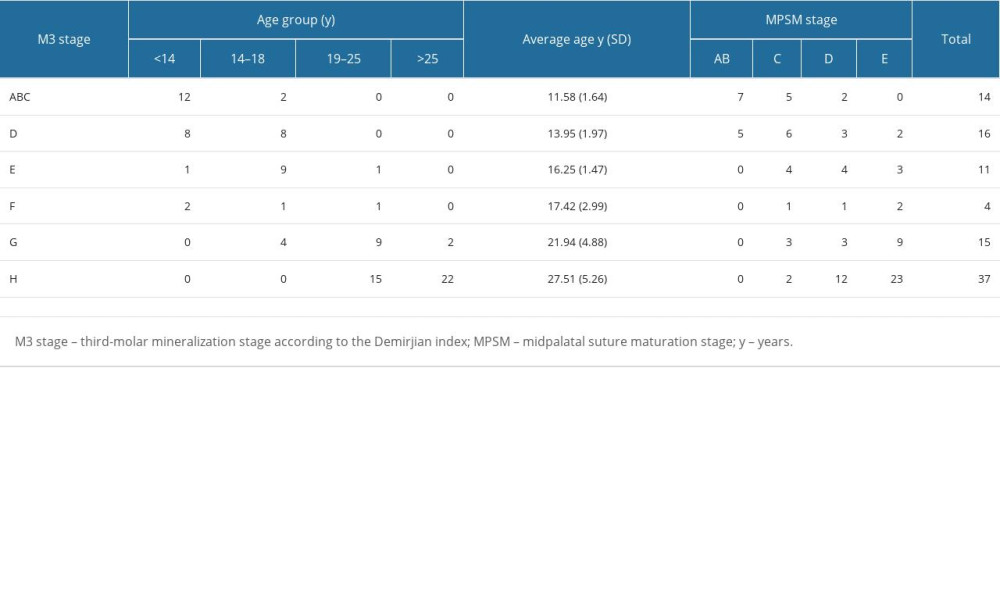 Table 2. Distribution of patients according to mandibular third-molar mineralization, age groups, and MPS maturation stages.
Table 2. Distribution of patients according to mandibular third-molar mineralization, age groups, and MPS maturation stages.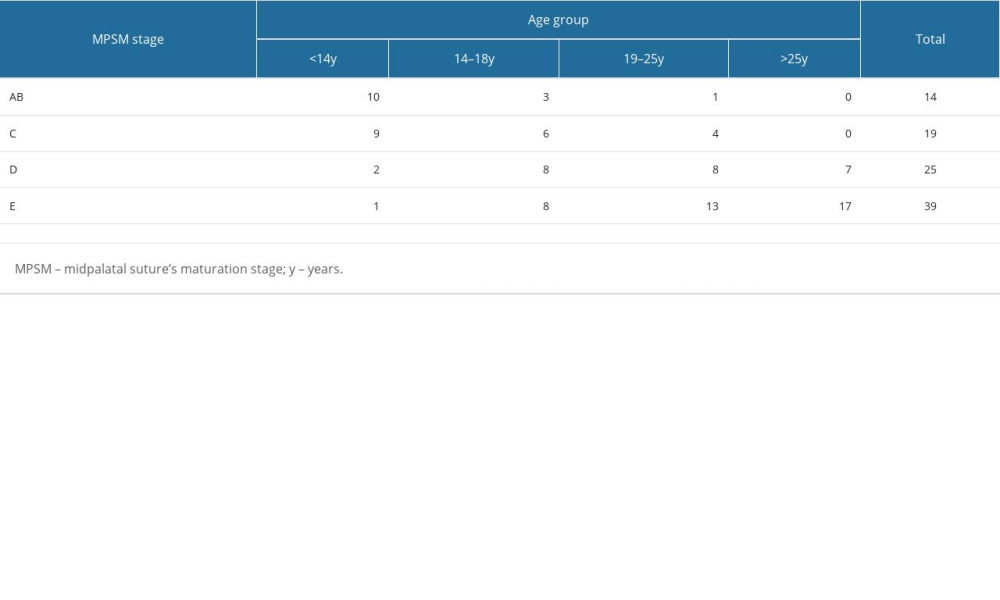 Table 1. Frequency of midpalatal suture maturation stages in different patient age groups.
Table 1. Frequency of midpalatal suture maturation stages in different patient age groups.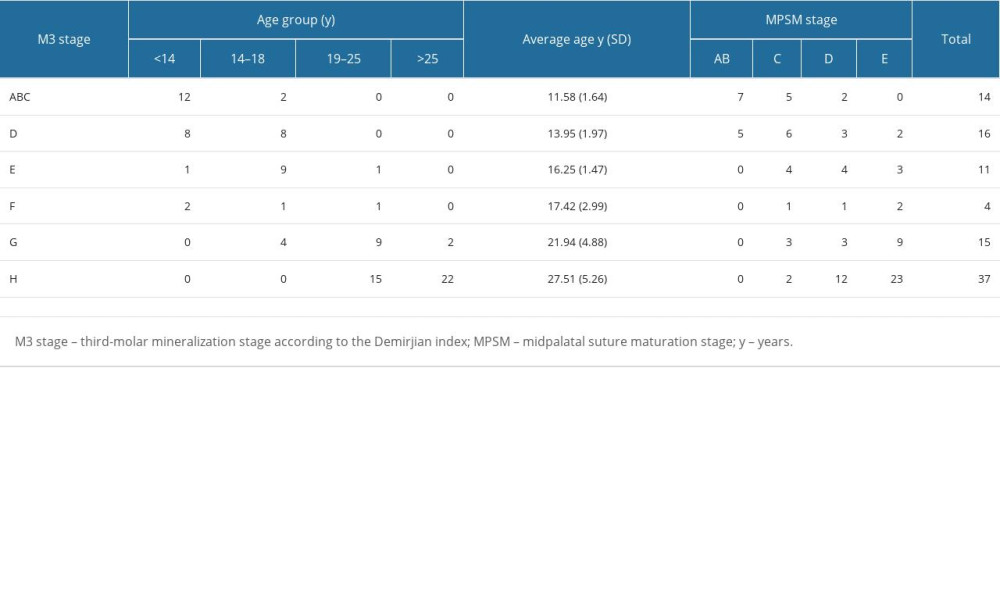 Table 2. Distribution of patients according to mandibular third-molar mineralization, age groups, and MPS maturation stages.
Table 2. Distribution of patients according to mandibular third-molar mineralization, age groups, and MPS maturation stages. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








