21 September 2023: Clinical Research
Anatomical Features of the Tarsal Sinus in Patients with Pes Planus: Implications for Clinical Management
Taiyuan Guan12BCDE, Yong Ma1AFG*DOI: 10.12659/MSM.940687
Med Sci Monit 2023; 29:e940687
Abstract
BACKGROUND: In the treatment of pes planus, if the implant does not match the anatomical structures of the sinus tarsi, synovitis can develop, causing pain symptoms. In the interest of making clinical recommendations for extra-osseous talotarsal stabilization, the goal of the present study was to characterize the anatomical characteristics of the sinus tarsi in patients with pes planus using magnetic resonance imaging (MRI) scans.
MATERIAL AND METHODS: This was a retrospective study involving 56 pes planus patients and 56 healthy volunteers from January 2014 to May 2022. The sinus tarsi was measured for length and width, for angle with the coronal and sagittal axes, and for length of the subtalar implant.
RESULTS: All examined metrics showed a difference between pes planus patients and healthy participants, with the exception of the subtalar implant’s length. The average sinus tarsi length and width among pes planus patients were 19.23 mm and 2.91 mm, respectively. The angle between the sinus tarsi and the coronal and sagittal axes was 21.418° and 25.077°, while the length of approach was 33.06 mm and 0.76°. The only gender differences that were statistically significant were in the length and width of the sinus tarsi. There were no notable variations between the left and right sides.
CONCLUSIONS: Sinus tarsi morphology may be impacted by pes planus. When treating patients with pes planus, clinicians should take these anatomical factors into consideration since they might more completely characterize the anatomical features of the sinus tarsi.
Keywords: Ankle, Diagnostic Imaging, Flatfoot, Humans, Heel, Retrospective Studies, Benchmarking, Bone and Bones
Background
Pes planus is among the most common diseases requiring foot and ankle surgery in clinical practice [1–3]. Flattening of the normal medial longitudinal arch is a complicated foot malformation that causes foot pain [4–7]. The arch curvature during non-weight bearing classifies pes planus as flexible or stiff. Flexible pes planus has a regular arch when not weight bearing, but the arch disappears when weight bearing, and the subtalar joint has more mobility. Severe deformity, low medial longitudinal arch, and ankle injuries might affect pes planus patients’ lifestyles.
Clinicians now prioritize early treatment of flexible pes planus patients. Flexible pes planus can be treated via conservative or surgical treatments [8]. Conservative therapies have low patient compliance, long clinical cycles, and cannot fully rectify the abnormal talar position [9]. Invasive surgery can entail long recovery times and cause problems such as nonunion and infection [10,11]. Flexible pes planus may be treated with extra-osseous talotarsal stabilization (EOTTS). A sinus tarsi implant may stabilize the gap, enabling foot arch repair [12,13]. The sinus tarsi is a slightly tapered space located between the inferior posterior joint and the anterior and middle subtalar joints, running anteriorly, from posteromedially to anteriorly [14]. The sinus tarsi is composed of a long tubular tarsal canal on the medial side, a funnel-shaped sinus tarsi, and a tarsal ostium located below the tail of the sustentaculum, which is filled with neuronal cells, small blood vessels, and fat [7].
When pes planus develops, the sinus tarsi closes, the pressure in the sinus tarsi rises, the nerve endings in the sinus tarsi are compressed, and localized pain occurs around the sinus tarsi. Without treatment, it can result in sinus tarsi syndrome, pes valgus, and metatarsal pain, as well as a poor quality of life for patients. After receiving EOTTS treatment, some patients may experience severe foot pain. Up to 40% of patients may decide to remove the tarsal sinus implant because of pain, primarily because the implant does not match the anatomical structure of the tarsal sinus and is either too deep or too shallow. Implantation of the brake can lead to the development of synovitis and the occurrence of vascular and neurodegenerative problems, causing pain symptoms [15]. The tarsal sinus has not been the subject of enough study, to the authors’ knowledge, to provide trustworthy information. The present study was therefore conducted to collect more detailed anatomical and morphological parameters of the tarsal sinus to confirm that there are differences between healthy persons and patients who have flat feet. Additionally, the objective of this study was to obtain more specific anatomical and morphological parameters of the tarsal sinus. This research offers clinicians new ideas for investigating the anatomical features of the tarsal sinus in patients with flat feet, as well as diagnostic and therapeutic anatomical data in an attempt to hasten patients’ recoveries. Additionally, this study provides clinicians with new ideas for studying the anatomical characteristics of the tarsal sinus in patients with flat feet.
Material and Methods
ETHICS:
This research was carried out in adherence with the Declaration of Helsinki, following ethical approval from the Ethics Committee of the Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University (BY2022022). All patients gave their informed consent for their clinicopathologic data to be evaluated and published for scientific objectives.
GENERAL DATA OF PATIENTS:
From January 2014 to May 2022, 56 healthy volunteers and 56 patients with pes planus were enrolled (57 male and 55 female, 54 left feet and 58 right feet, age range: 10–72). All of the study participants supplied written informed consent before enrollment in the studies. All MRI scans were performed with 1.5-T scanners (Philips Ingenia) with an extremity coil, using the sagittal, axial, and coronal planes with standard pulse sequences and proton density–weighted images with fat saturation (PD-WI FAT SAT), and turbo inversion recovery magnitude; both T2-weighted and T1-weighted. The slice thickness was 3 mm.
INCLUSION CRITERIA:
(1) Patients must have met the diagnostic criteria for flexible pes planus. (2) No obvious ankle deformity was observed in the outward appearance. (3) Complete clinical data and MRI imaging data were available for each patient.
EXCLUSION CRITERIA:
Patient exclusion criteria were: (1) patients with other lower limb injury, previous ankle fractures, or surgery; (2) patients with peripheral neuropathy of the ankle joint.
CONFIRMATION OF PES PLANUS:
Two researchers independently measured lateral ankle X-rays to diagnose pes planus in patients [16–18]. The talo-first metatarsal (Meary angle) is the normal angle of 0±4 degrees between the long axis of the talus and the first metatarsal. The calcaneal inclination angle is the angle between the lower border of the calcaneus and the sagittal axis, which is typically between 10 and 30 degrees [19]. The talocalcaneal angle (Kites angle) is the angle between the long talus and calcaneus, which is typically between 25 and 45 degrees. The talar tilt angle is the angle between the longitudinal axis of the talus and the sagittal axis, which is typically between 0 and 5 degrees. Patients with the aforementioned abnormalities were deemed to have pes planus (Figure 1).
MORPHOLOGICAL PARAMETERS MEASURED:
MRI scans of 56 patients and 56 healthy volunteers were retrospectively reviewed. The maximal cross section of the sinus tarsi was selected for analysis. In the horizontal plane, the length and diameter of the sinus tarsi and the angle of the sinus tarsi with the coronal axis were measured. The length of the subtalar implant refers to extending the long axis of the sinus tarsi to the skin surface. In the coronal plane, the angle between the sinus tarsi and the sagittal axis was measured. The measurement data are shown in Figures 2 and 3.
The parameters measured included the following:
STATISTICAL ANALYSIS:
Data analysis was performed in SPSS (SPSS Statistics 25.0; IBM). The normality assumption for the data was tested using the Shapiro-Wilk test. The data that conformed to a normal distribution were analyzed using
Results
In Table 1, demographic parameters have been summarized. The patient group and controls were comparable with respect to age and body mass index. No differences between patients and healthy volunteers were observed with regard to gender, feet, and age.
In Table 2, the length of the sinus tarsi was significantly larger in patients compared with healthy volunteers (19.23±2.91 mm vs 17.51±1.81 mm,
As detailed in Table 3, no statistically significant difference was seen between right and left feet.
Discussion
The purpose of this study was to measure the structure of the sinus tarsi using MRI images and to investigate the sinus tarsi characteristics in patients with pes planus. MRI has numerous advantages over computed tomography (CT), including no radioactivity in the human body, no biological adverse effects, and high resolution of soft tissue. Therefore, not only is it secure, but it also ensures that the experimental results are scientific [20–22]. In the present study, the length, diameter, angle in the coronal axis, and angle in the sagittal axis of the sinus tarsi were measured using MRI in patients with pes planus to determine the optimal length, diameter, and trajectory of the EOTTS implant. This study is the first to demonstrate through data that the parameters of the sinus tarsi in patients with pes planus differ from those in healthy volunteers, with the aim of providing clinicians with new treatment parameters that are more consistent with the sinus tarsi in patients with pes planus, thereby reducing the incidence of postoperative complications and facilitating the individualized treatment of patients with pes planus. EOTTS can effectively stabilize the distance by inserting a subtalar joint brake in the sinus tarsi to increase subtalar joint stability. It corrects the ectropion of the subtalar joint and reconstructs the arch to preserve the arch’s stability [12,23]. When treating flexible pes planus with a lower distance joint brake, strephenopodia predisposes prolapse of the brake, accounting for surgical failure. Even if the dimension is marginally off from the sinus tarsi, it is necessary to reimplant the matching brake [24]. In addition, the surgeon sequentially positions the trial in the order of the extent of the subtalar implant, until the foot ankle joint is passively extended by 10° as the correction standard. However, the method of placement is subjective, and it is unknown if the placement location and profundity correspond to the anatomical location of the sinus tarsi.
In the present study, patients with pes planus and healthy volunteers exhibited statistically significant differences in sinus tarsi length, diameter, angle in the sagittal axis, and angle in the coronal axis. Therefore, we would contend that the sinus tarsi of pes planus patients differs from the ordinary volunteer. Unquestionably, the use of sinus tarsi data from the general population in the study of subtalar joint stabilization may contribute to complications due to the presence of errors. Our study revealed that the length of the sinus tarsi in patients with pes planus was 19.23±2.91 mm, the diameter was 2.93±0.66 mm, and the angles in the coronal and sagittal axes were 21.418±3.973° and 25.077±3.253°, respectively. Consequently, we recommend using this parameter as a standard for subtalar implant dimensions. We discovered a significant difference in the length of the sinus tarsi between the male and female subjects (19.04±1.96 mm vs 17.67±2.92 mm,
Several limitations should be acknowledged in this paper. First, the complex structure of the ankle ligament makes it challenging to display the complete length of the ligament at the same level on MRI images, leading to measurement errors. Second, the MRI image resolution of the sinus tarsi in some patients may not be crystal clear. Third, this study’s sample size is relatively modest. In addition, there was a paucity of body mass index (BMI) data, and all the images in this study were collected from a single center in the Southwest region of China, so there was no multi-center research or in-depth analysis.
Conclusions
The structure of the sinus tarsi may be affected by pes planus, and it is hoped that clinicians will refer to this fact during diagnosis and treatment. For subtalar implants in adults, we recommend a length of 33.06±3.71 mm and a diameter of 2.93±0.666 mm. The present research not only enriched the anatomical and morphological database of the sinus tarsi, but also provided foundation and reference information for clinical surgery, such as subtalar joint stabilization. However, the information in this study is only an estimate, and patients should be treated individually.
Figures
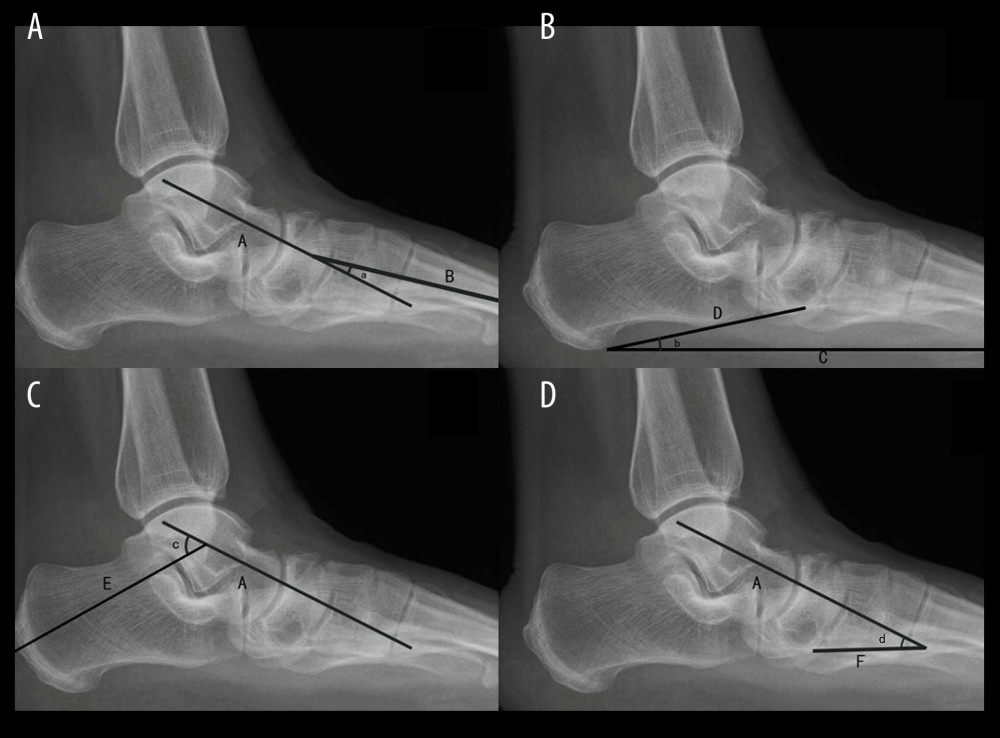 Figure 1. (A–D) Lateral X-rays of the ankles: A) the axis of the talus; B) the axis of the first metatarsal; C, D, E, F) the sagittal axis of the participants’ body; a) the talo-first metatarsal; b) the calcaneal pitch angle; c) the talocalcaneal angle; d) the talar tilt angle.
Figure 1. (A–D) Lateral X-rays of the ankles: A) the axis of the talus; B) the axis of the first metatarsal; C, D, E, F) the sagittal axis of the participants’ body; a) the talo-first metatarsal; b) the calcaneal pitch angle; c) the talocalcaneal angle; d) the talar tilt angle. 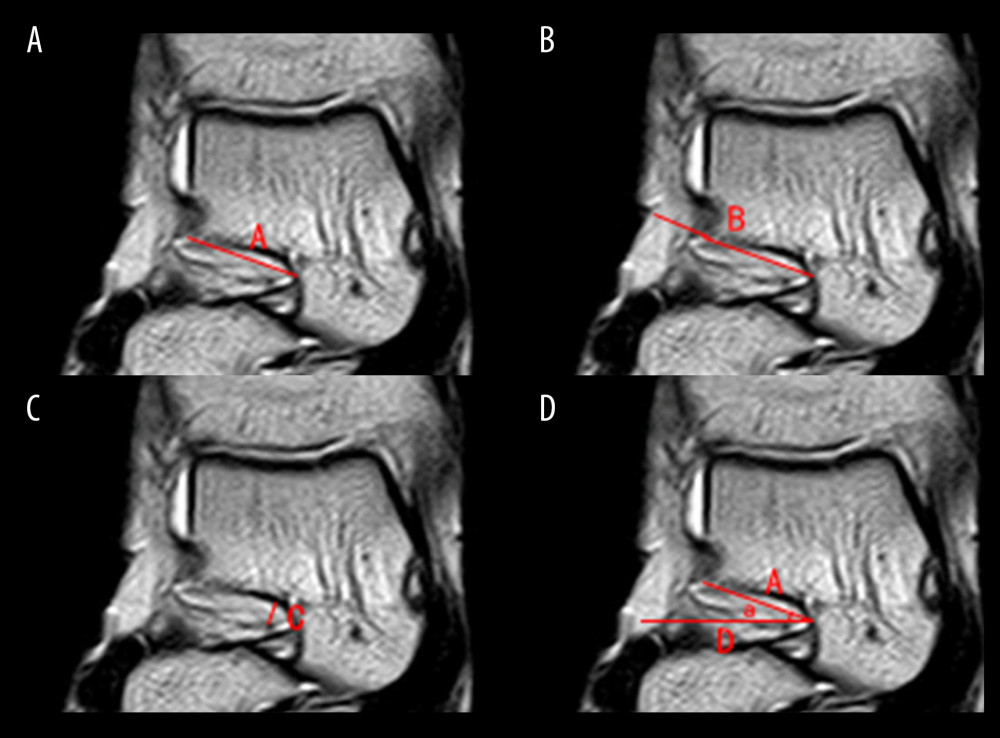 Figure 2. (A–D) Horizontal plane in MRI. A) The length of the sinus tarsi; B) the length of the subtalar implant; C) the diameter of the sinus tarsi; D) the coronal axis; a) the angle of the sinus tarsi in the coronal axis. MRI – magnetic resonance imaging.
Figure 2. (A–D) Horizontal plane in MRI. A) The length of the sinus tarsi; B) the length of the subtalar implant; C) the diameter of the sinus tarsi; D) the coronal axis; a) the angle of the sinus tarsi in the coronal axis. MRI – magnetic resonance imaging. 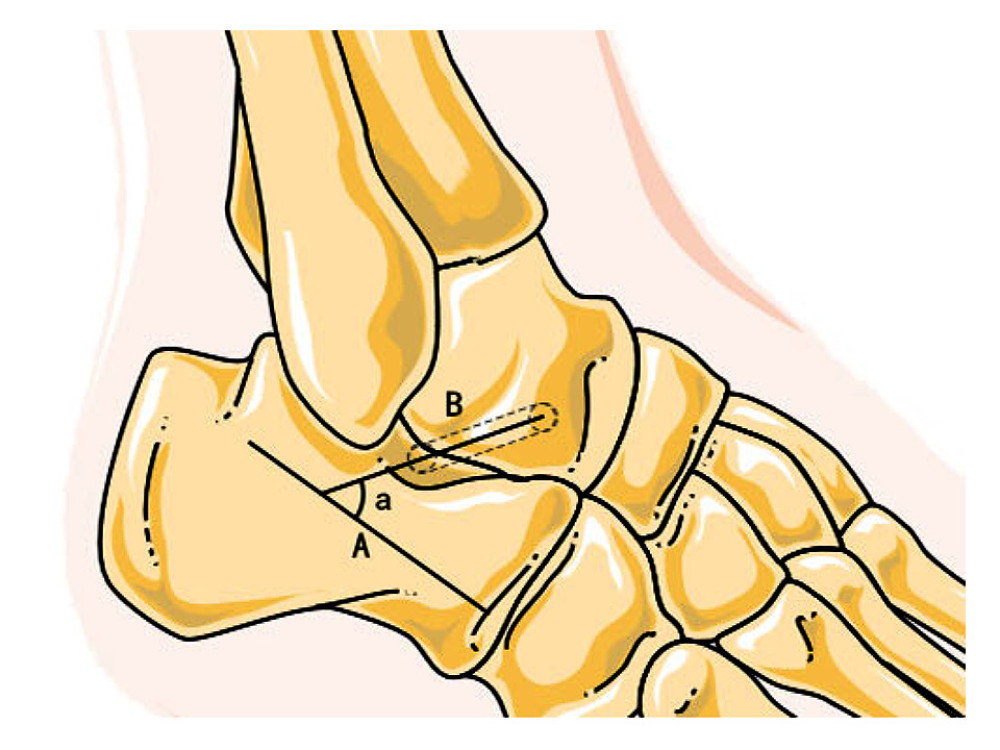 Figure 3. Image illustrating MRI coronal plane measurement. A) The sagittal axis; B) the long axis of sinus tarsi; a) the angle between the sinus tarsi and the sagittal axis. MRI – magnetic resonance imaging. (Image realized by applying Servier Medical ART illustration: http://smart.servier.com).
Figure 3. Image illustrating MRI coronal plane measurement. A) The sagittal axis; B) the long axis of sinus tarsi; a) the angle between the sinus tarsi and the sagittal axis. MRI – magnetic resonance imaging. (Image realized by applying Servier Medical ART illustration: http://smart.servier.com). References
1. Lee HJ, Lim KB, Yoo J, Effect of custom-molded foot orthoses on foot pain and balance in children with symptomatic flexible flat feet: Ann Rehabil Med, 2015; 39(6); 905-13
2. Pita-Fernandez S, Gonzalez-Martin C, Seoane-Pillado T, Validity of footprint analysis to determine flatfoot using clinical diagnosis as the gold standard in a random sample aged 40 years and older: J Epidemiol, 2015; 25(2); 148-54
3. Das SP, Das PB, SG , Sahu MC, Effectiveness of surgically treated symptomatic plano-valgus deformity by the calcaneo stop procedure according to radiological, functional and gait parameters: J Taibah Univ Med Sci, 2017; 12(2); 102-29
4. Baghdadi T, Mazoochy H, Guity M, Heidari Khabbaz N, Evaluation of clinical and radiological results of calcaneal lengthening osteotomy in pediatric idiopathic flexible flatfoot: Arch Bone Jt Surg, 2018; 6(5); 402-11
5. Elataar FF, Abdelmajeed SF, Abdellatif NMN, Mohammed MM, Core muscles’ endurance in flexible flatfeet: A cross – sectional study: J Musculoskelet Neuronal Interact, 2020; 20(3); 404-10
6. Dars S, Uden H, Banwell HA, Kumar S, The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: A systematic review: Update: PLoS One, 2018; 13(2); e0193060
7. Zhang L, Peng X, He S, Association between subtalar articular surface typing and flat foot deformity: Which type is more likely to cause flat foot deformity: BMC Musculoskelet Disord, 2021; 22(1); 979
8. Chen KC, Chen YC, Yeh CJ, The effect of insoles on symptomatic flatfoot in preschool-aged children: A prospective 1-year follow-up study: Medicine (Baltimore), 2019; 98(36); e17074
9. Powell M, Seid M, Szer IS, Efficacy of custom foot orthotics in improving pain and functional status in children with juvenile idiopathic arthritis: A randomized trial: J Rheumatol, 2005; 32(5); 943-50
10. Faldini C, Nanni M, Traina F, Surgical treatment of hallux valgus associated with flexible flatfoot during growing age: Int Orthop, 2016; 40(4); 737-43
11. Van Gestel L, Van Bouwel S, Somville J, Surgical treatment of the adult acquired flexible flatfoot: Acta Orthop Belg, 2015; 81(2); 172-83
12. Prachgosin T, Chong DY, Leelasamran W, Medial longitudinal arch biomechanics evaluation during gait in subjects with flexible flatfoot: Acta Bioeng Biomech, 2015; 17(4); 121-30
13. Bresnahan PJ, Juanto MA, Pediatric flatfeet – a disease entity that demands greater attention and treatment: Front Pediatr, 2020; 8; 19
14. Sergot L, Kho JSB, Chakraverty J, The frondiform ligament sling: A sonographic landmark for injection into the sinus tarsi: J Ultrasound, 2022; 25; 777-81
15. Wong DW, Wang Y, Niu W, Zhang M, Finite element analysis of subtalar joint arthroereisis on adult-acquired flexible flatfoot deformity using customised sinus tarsi implant: J Orthop Translat, 2021; 27; 139-45
16. Meyr AJ, Sansosti LE, Ali S, A pictorial review of reconstructive foot and ankle surgery: Evaluation and intervention of the flatfoot deformity: J Radiol Case Rep, 2017; 11(6); 26-36
17. Henry JK, Shakked R, Ellis SJ, Adult-acquired flatfoot deformity: Foot Ankle Orthop, 2019; 4(1); 2473011418820847
18. Hamel J, Horterer H, Harrasser N, Is it possible to define reference values for radiographic parameters evaluating juvenile flatfoot deformity? A case-control study: BMC Musculoskelet Disord, 2020; 21(1); 838
19. Gentili A, Masih S, Yao L, Seeger LL, Pictorial review: Foot axes and angles: Br J Radiol, 1996; 69(826); 968-74
20. Yu SS, Scherer RL, Ortega RA, Enzymatic- and temperature-sensitive controlled release of ultrasmall superparamagnetic iron oxides (USPIOs): J Nanobiotechnology, 2011; 9; 7
21. Ji S, Wei B, Yu Z, A new multistage medical segmentation method based on superpixel and fuzzy clustering: Comput Math Methods Med, 2014; 2014; 747549
22. Qian K, Arichi T, Price A, An eye tracking based virtual reality system for use inside magnetic resonance imaging systems: Sci Rep, 2021; 11(1); 16301
23. Jain A, Gupta G, Gupta A, Short term clinico-radiological outcome of Extra Osseous Talo-Tarsal Stabilization (EOTTS) in flat foot: An Indian perspective: Indian J Orthop, 2021; 56(1); 94-102
24. Cao L, Miao XD, Wu YP, Therapeutic outcomes of Kalix II in treating juvenile flexible flatfoot: Orthop Surg, 2017; 9(1); 20-27
Figures
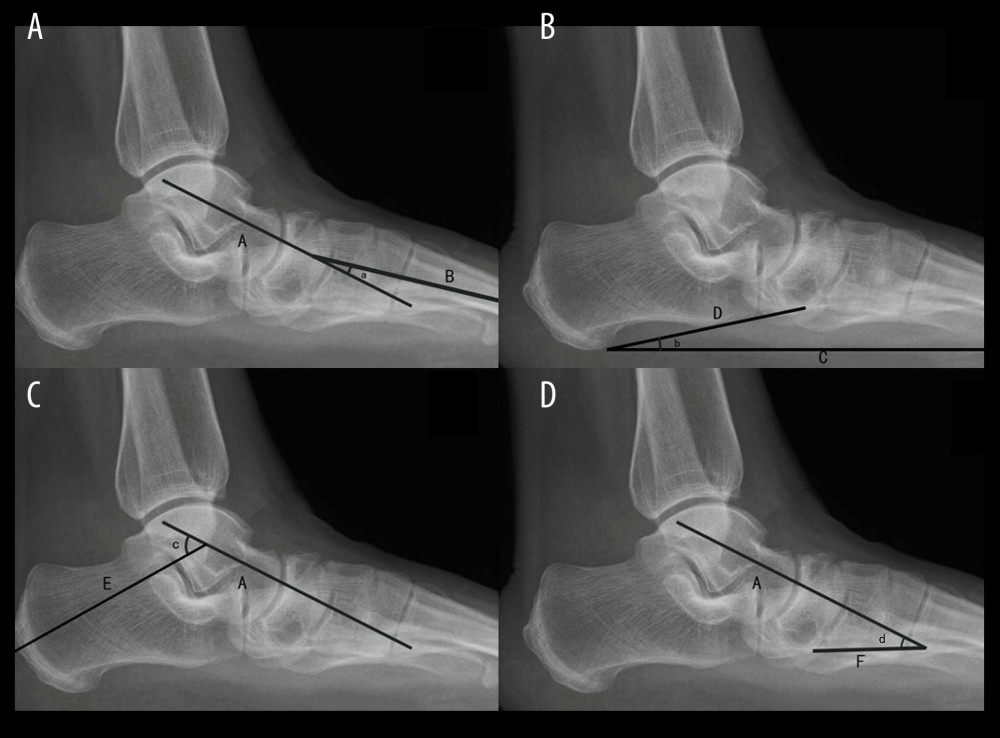 Figure 1. (A–D) Lateral X-rays of the ankles: A) the axis of the talus; B) the axis of the first metatarsal; C, D, E, F) the sagittal axis of the participants’ body; a) the talo-first metatarsal; b) the calcaneal pitch angle; c) the talocalcaneal angle; d) the talar tilt angle.
Figure 1. (A–D) Lateral X-rays of the ankles: A) the axis of the talus; B) the axis of the first metatarsal; C, D, E, F) the sagittal axis of the participants’ body; a) the talo-first metatarsal; b) the calcaneal pitch angle; c) the talocalcaneal angle; d) the talar tilt angle.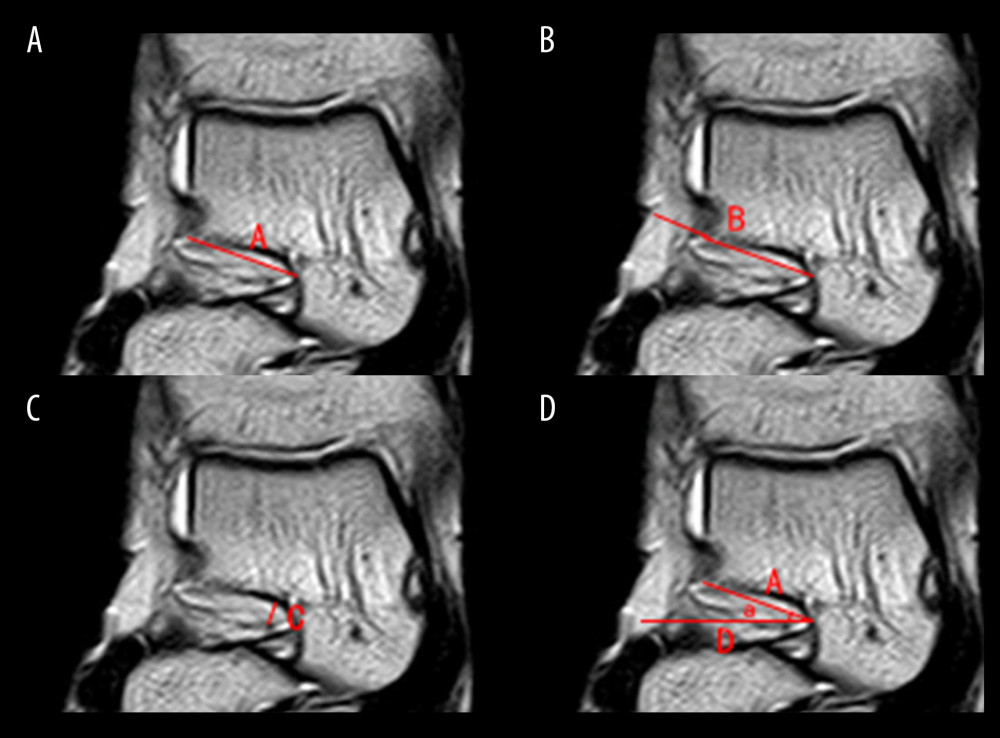 Figure 2. (A–D) Horizontal plane in MRI. A) The length of the sinus tarsi; B) the length of the subtalar implant; C) the diameter of the sinus tarsi; D) the coronal axis; a) the angle of the sinus tarsi in the coronal axis. MRI – magnetic resonance imaging.
Figure 2. (A–D) Horizontal plane in MRI. A) The length of the sinus tarsi; B) the length of the subtalar implant; C) the diameter of the sinus tarsi; D) the coronal axis; a) the angle of the sinus tarsi in the coronal axis. MRI – magnetic resonance imaging.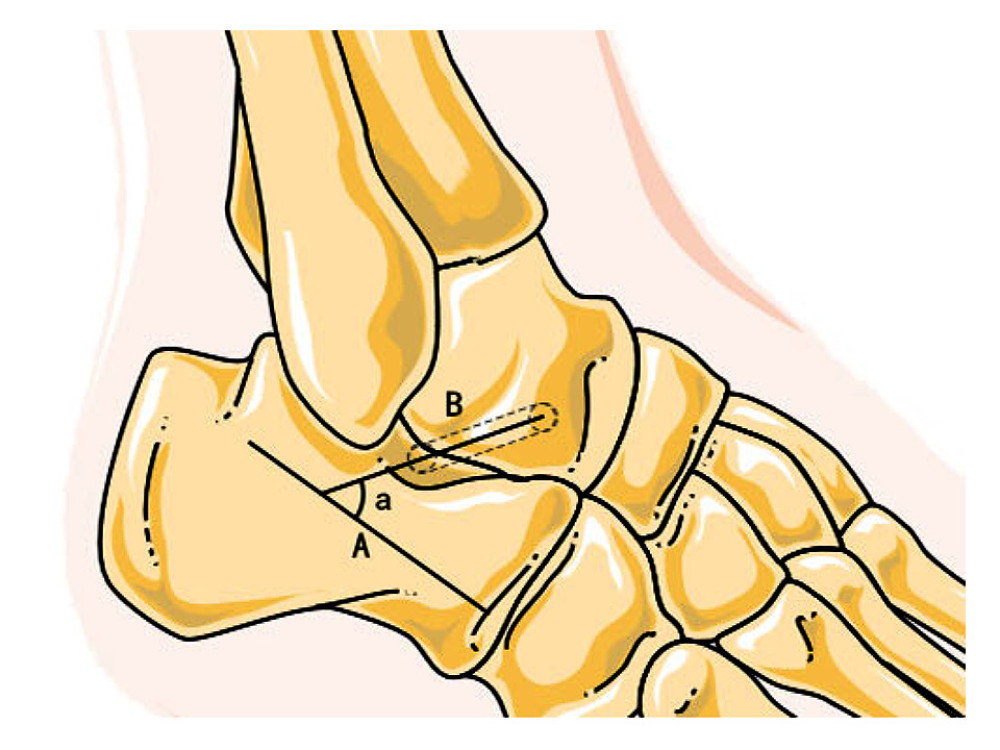 Figure 3. Image illustrating MRI coronal plane measurement. A) The sagittal axis; B) the long axis of sinus tarsi; a) the angle between the sinus tarsi and the sagittal axis. MRI – magnetic resonance imaging. (Image realized by applying Servier Medical ART illustration: http://smart.servier.com).
Figure 3. Image illustrating MRI coronal plane measurement. A) The sagittal axis; B) the long axis of sinus tarsi; a) the angle between the sinus tarsi and the sagittal axis. MRI – magnetic resonance imaging. (Image realized by applying Servier Medical ART illustration: http://smart.servier.com). Tables
 Table 1. Demography of patients and volunteers.
Table 1. Demography of patients and volunteers.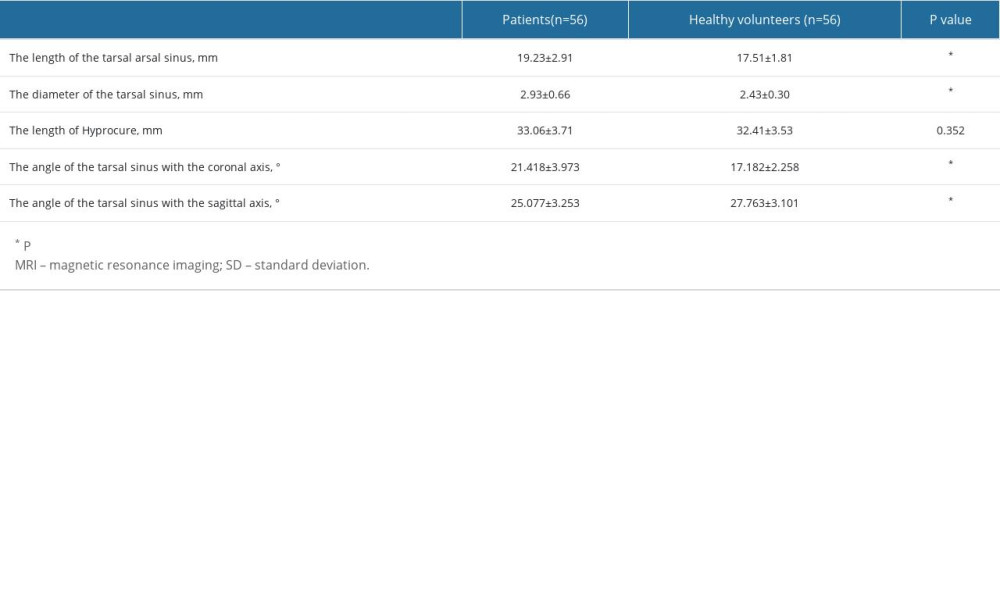 Table 2. Classified measurement on MRI image of the sinus tarsi (mean±SD or mean).
Table 2. Classified measurement on MRI image of the sinus tarsi (mean±SD or mean).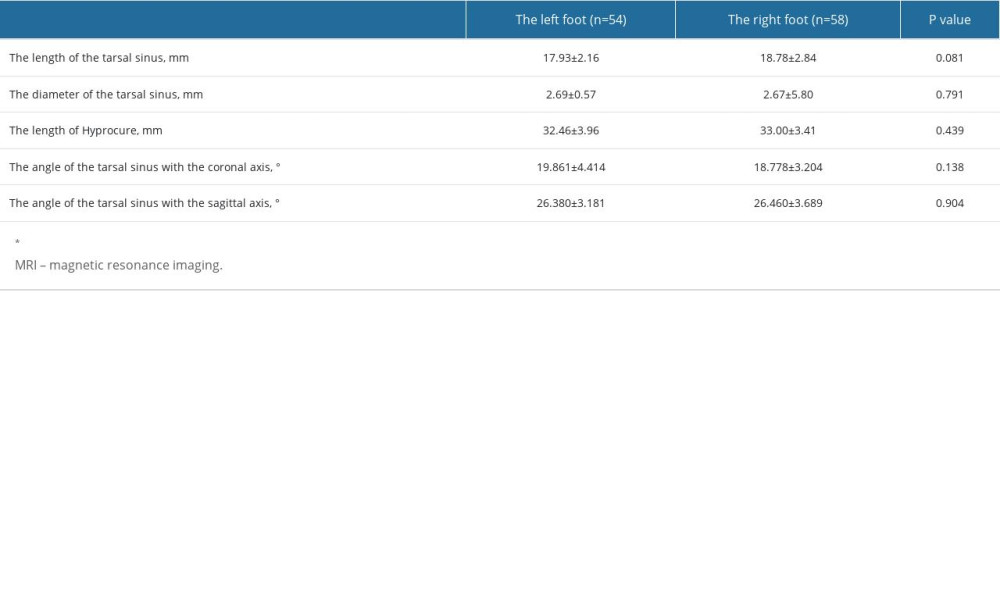 Table 3. Classification and measurement of sinus tarsi from MRI images of the left and right feet.
Table 3. Classification and measurement of sinus tarsi from MRI images of the left and right feet. Table 1. Demography of patients and volunteers.
Table 1. Demography of patients and volunteers.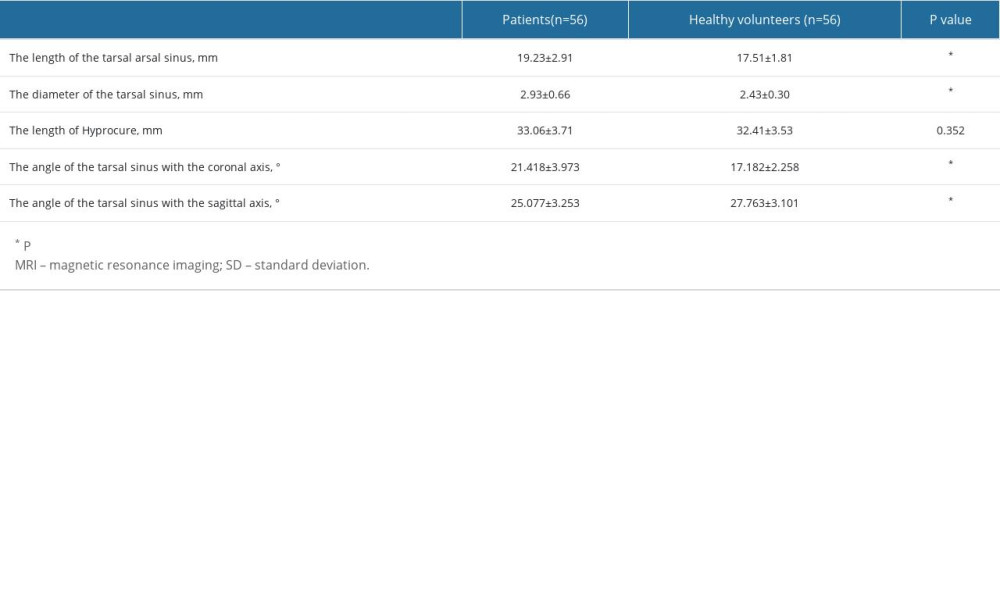 Table 2. Classified measurement on MRI image of the sinus tarsi (mean±SD or mean).
Table 2. Classified measurement on MRI image of the sinus tarsi (mean±SD or mean).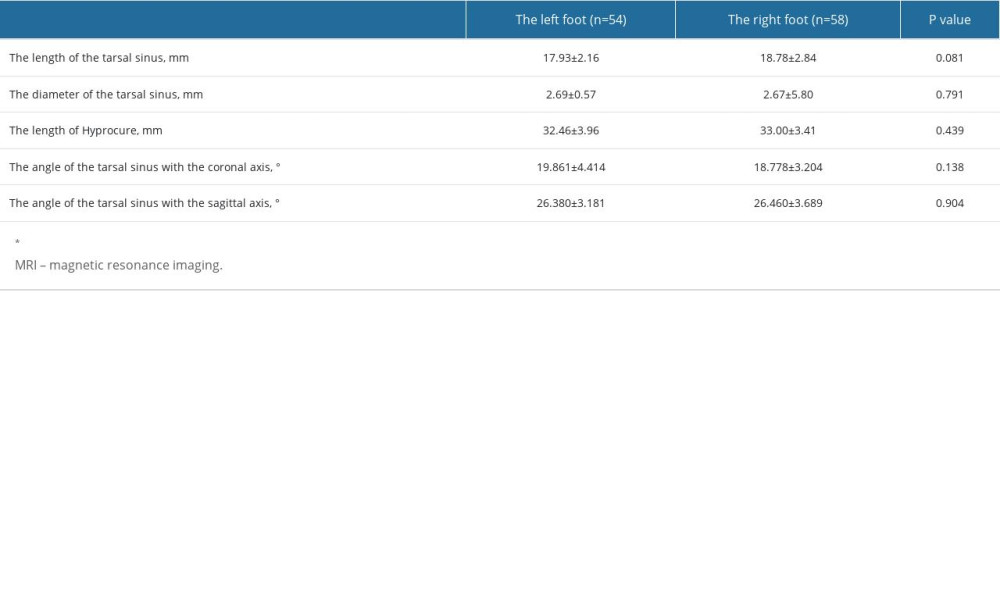 Table 3. Classification and measurement of sinus tarsi from MRI images of the left and right feet.
Table 3. Classification and measurement of sinus tarsi from MRI images of the left and right feet. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








