19 July 2023: Clinical Research
Pubertal Stage-Dependent Anthropometric Variations in Turkish Children with Adolescent Idiopathic Scoliosis: An In-Depth Analysis
Keziban Aslı BalaDOI: 10.12659/MSM.940864
Med Sci Monit 2023; 29:e940864
Abstract
BACKGROUND: Identifying predictive factors for anthropometric changes during puberty in adolescent idiopathic scoliosis (AIS) is critical for prognosis and management. This study aimed to discern these factors in the Turkish AIS population, by analyzing variations against female breast development stages and male testicular volume, benchmarked against national standards.
MATERIAL AND METHODS: A cross-sectional study was conducted between 2018 and 2022, involving children aged 10 to 18 years from the Orthopedics and Pediatrics Clinics. AIS patients and controls were assessed concerning pubertal status (Tanner stage), chronological age, skeletal maturation (Tanner-Whitehouse), and anthropometric parameters (height, weight, and body mass index).
RESULTS: AIS patients were compared to controls, stratified by pubertal stages. In girls across all stages, significant differences emerged in bone age, BMI, and weight between AIS and controls (p<0.01). In boys, AIS patients significantly differed in bone age from controls across all stages (p<0.001). At stage V, controls demonstrated higher BMI than AIS boys (p<0.001), while at stage I, AIS boys had significantly higher height and weight compared to controls (p<0.001).
CONCLUSIONS: AIS patients demonstrate distinctive pubertal growth abnormalities, with males and females presenting divergent patterns. Understanding these variations could inform better management of AIS during the critical pubertal growth period.
Keywords: Adolescent, Anthropometry, Puberty, Scoliosis, Humans, Male, Female, Child, Cross-Sectional Studies, Body Mass Index, Kyphosis
Background
Adolescent idiopathic scoliosis (AIS) represents a complex 3-dimensional structural disorder affecting the spine. It appears in children, predominantly between the age of 10 years and the end of their skeletal maturity [1]. A myriad of factors, including genetic, intrinsic, and environmental elements, play a critical role in the onset and progression of AIS. Notably, researchers have suggested a connection between growth and development in children, hormone release, posture, and physical activity [2,3].
Historically, different prognostic indices and regression equations have been proposed to understand and predict the progression of AIS. One such approach was proposed by Lonstein and Carlson [4], focusing on 3 factors: the initial Cobb angle, which reflects the degree of scoliosis; the Risser degree, an indicator of skeletal maturity; and chronological age. Further advancement in this field saw Peterson and Nachemson [5] introducing a 4-factor regression equation [6]. However, many subsequent studies still need to fully consider Tanner’s staging, a measure of physical development, leading to a primary reliance on changes in the Cobb angle to define curve progression [7,8].
Realizing that an increase in the Cobb angle may not have direct clinical implications, a need emerged to refine these predictive factors, encompassing elements such as age at onset, menarchal status, and the Cobb angle itself [9]. This need was underscored by evidence suggesting a strong correlation between AIS progression and growth spurts during puberty [10–15]. Thus, a more nuanced understanding of pubertal growth patterns in AIS patients, in terms of both sexes, is crucial.
Peak height velocity predicts residual growth more accurately than do Risser sign or chronological age [16]. Recognizing puberty onset and measuring its progression in boys can be challenging. For instance, boys lack physiological events such as menarche, which marks specific stages of puberty in girls. Nevertheless, elements like secondary sex characteristics and changes in bone age and testicular volume can provide practical markers to establish correlations between somatic signs of puberty and its stages [17].
The criterion for the onset of puberty in boys is the testicular volume. In boys, the increase in testicular volume begins at a mean age of 12 years (range, 9.5–13.5 years) [18,19]. This process lasts an average of 3.5 years [20]. Since the average age at the onset of puberty and duration of puberty [21] in boys and the average age at the onset of puberty and duration of puberty in girls in Turkish society differ [22], the growth spurt in boys occurs 2 years later than in girls and continues until the age of 18 [23]. A boy has reached 99% of his adult height at a bone age of 17 years [24]. In girls, height growth decreases after menarche and the average height gain is 7 cm per year. A girl reaches 99% of her adult height at a bone age of 15 years [20].
Height measured during physical examination and the annual growth rate calculated for a child at follow-up are the most important criteria used to evaluate growth. The calculated values are measured against national reference values to determine the child’s growth status [25].
Given the notable differences in growth histories between boys and girls with AIS, we hypothesize that boys with AIS exhibit abnormal growth patterns during puberty, distinct from those observed in girls with AIS. Although the progression of AIS in female patients has been extensively studied [13,14,26,27], the same cannot be said for male patients [28]. Previous studies have often relied on anthropometric measurements, without adhering to national standards or considering standard deviations.
This gap in the literature underscores the need for this study. We aim to investigate and compare anthropometric parameters and growth patterns in adolescent boys and girls with AIS within the Turkish population. We intend to adhere to national standards and consider standard deviations in our analysis. Ultimately, we aspire to shed light on the influence of sexual development on physical growth and progression of AIS, gauging breast development in girls and testicular volume in boys. This study could contribute valuable insights for both research and clinical practice by offering a more sex-inclusive understanding of AIS.
Material and Methods
MEASUREMENT OF COBB ANGLE:
The Cobb angle was measured by a single experienced orthopedist using (standing) radiographs of the thoracic and lumbar spine. Scoliosis was defined as a spinal curvature with a Cobb angle of 10° or greater. Measurements were made using the classical vertebra endplate method using erect and bending radiographs [1].
MEASUREMENT OF TESTICULAR VOLUME:
In boys, the first sign of puberty is a testicular long axis of ≥2.5 cm or a testicular volume of ≥4 cm3. Testicular volume was measured using Prader’s orchidometer [29], the most widely used instrument for measuring testicular size, and was staged according to the Male External Genitalia Scale [30].
Testicular volume index per square centimeter was calculated as follows: (length×width of right testes+length×width of left testes)/2 [17].
ANTHROPOMETRIC MEASUREMENTS:
Weight and height were measured using standard measurement techniques. Measurements were read to the nearest 0.1 value (cm). The height without shoes was measured while the participants were standing upright against a wall-mounted stadiometer, head in the Frankfort horizontal plane and heels against a Harpenden stadiometer (Holtain, Crosswell, Crymych, Pembs., SA41 3UF, UK).
Measurements were read to the nearest 0.1 value (kg). Weight was measured using a digital scale (Seca pediatric digital scale, Hammer Steindamm 3–25, 22089 Hamburg, Germany), while participants were in light clothing and without shoes. Standard deviation scores were calculated for height, weight, and BMI according to the 2015 Turkish national population standards [31]. BMI was calculated using weight (in kg) divided by the squared height (m2).
BONE AGE:
Bone age was calculated using radiographs of the left hand and wrist using the standard Greulich and Pyle atlas by a single experienced pediatric endocrinologist.
STAGING OF PUBERTY:
Pubertal development was assessed using descriptive standards developed by Tanner and Marshall. According to Tanner, stage 1 refers to the prepubertal stage, while stage 5 refers to the last stage of puberty [20]. Puberty was evaluated using Tanner staging for pubic hair and breast development and Prader’s technique for testicular volume [31–33].
When adrenarche and gonadarche differed, puberty was staged after gonadarche, namely, breast development in girls and testicular volume in boys.
BMI CALCULATION:
BMI was adjusted for age and sex, and the BMI z-score was used for diagnosis. The BMI z-score was expressed as a range of standard deviations from the 50th percentile (median) value. BMI z-scores were derived from 2015 Turkish national population standards [34]. BMI (kg/m2) was calculated based on weight in kilograms divided by the square of height in meters.
STATISTICAL ANALYSIS:
Descriptive data are presented as median and interquartile ranges (25th and 75th percentiles) or mean±standard deviation, according to the data distribution. The normality of data was assessed with the Shapiro-Wilk test and histogram plots. The non-parametric Mann-Whitney U test was used for non-normal data. For the analyses of normally distributed continuous variables, independent-sample
Results
CORRELATION:
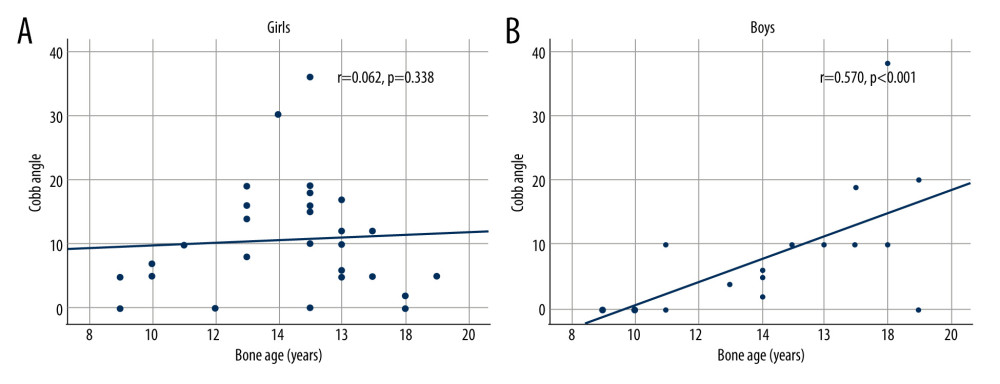
Figure 1 displays the results of correlation analysis assessing the relationship between Cobb angle and bone age stratified by sex. A significant positive correlation was found between Cobb angle and bone age in boys (r=0.570, P<0.001), while no such correlation was observed in girls (Figure 1).
REGRESSION:
Univariate and multivariate analyses were conducted to identify factors associated with AIS, stratified by sex (Table 5). Both analyses showed that advancing pubertal stage was significantly associated with increased odds of AIS. In girls, after controlling for pubertal stage and height, bone age was negatively and significantly associated with AIS (OR: 0.763, 95% CI: 0.625–0.932, P=0.008). In boys, age and bone age were found to be significant predictors of AIS. When controlled for age, the association between bone age and AIS was negative (OR: 0.558, 95% CI: 0.318–0.979, P=0.042).
In the univariate analysis for boys, age (OR: 1.808, 95% CI: 1.483–2.203,
Discussion
Our study illuminated the sexually dimorphic nature of AIS progression during puberty[35–37], underscoring the importance of assessing anthropometric parameters in tandem with pubertal staging. We found unique patterns of anthropometric parameters in AIS patients, distinct from those of healthy controls, which fluctuated with pubertal progression.
During adolescence, curve progression in AIS has been reported to occur during the peak of growth in female [10,11,38] and male patients [12–15,39,40]. Previous studies have reported that female patients with AIS exhibit a trend of greater curve progression [35–37,41], while male patients with AIS have a lower curve progression [4,41,42]. Probably, these studies considered skeletal maturity in both sexes only in relation to pre-menarche and menarche and not according to Tanner staging. This may also be attributed to the fact that male patients with AIS grow differently and have abnormal growth patterns during puberty compared with healthy males.
In female patients with AIS, BMI was higher than that of controls in the prepubertal phase and during the pubertal growth spurt, but it declined after puberty. This agrees with the previous studies that reported similar BMI trends in girls with AIS [43–46]. Conversely, our male patients with AIS exhibited lower BMI than their healthy counterparts only at stage 5. This novel finding has not been reported in the literature before, warranting further investigation to ascertain the biological underpinnings of this phenomenon.
Notably, our results diverged from those of previous studies, such as that by Dangerfield et al, which reported that girls with scoliosis were shorter than their healthy counterparts [47]. We found girls with AIS to be shorter during pubertal stages 1 and 5 but taller during the premenarchal stage. This discrepancy warrants further exploration.
Further analysis revealed that bone age and chronological age emerged as independent predictors of scoliosis in boys with AIS. Furthermore, a significant relationship was identified between chronological age and the Cobb angle. Our findings echo the results of Wei-Jun et al, who recognized body weight and chronological age as critical variables affecting curve size in male patients with AIS [28].
Our findings also stress the significance of pubertal staging as an essential parameter to be considered in patients with AIS. The present study adds to the growing body of evidence suggesting abnormal growth patterns in AIS patients [27], which are potentially driven by neuro-hormonal dysregulation at various biological levels.
However, the cross-sectional nature of our study constrains our ability to establish a clear temporal relationship between anthropometric parameters and AIS progression. Future longitudinal studies could provide invaluable insights into the evolution of these parameters and their correlation with curve progression in patients with AIS.
Ultimately, understanding these growth patterns and their relationship to AIS could be instrumental in establishing early intervention strategies and personalized treatment plans. Further research is required to delineate the complex interplay of factors contributing to AIS and to explore the clinical implications of these anthropometric findings.
Our findings highlight the importance of considering the pubertal stage and various anthropometric parameters in managing AIS. They also point to a possible link between AIS progression and growth patterns, providing a novel avenue for future research into the pathogenesis and management of AIS.
Conclusions
The results strongly support our hypothesis that although both male and female patients with AIS show abnormal pubertal development, male patients with AIS exhibit a different pattern of abnormality than do female patients with AIS. However, it is not entirely clear whether the results found in this study are the cause or the consequence of the deformity.
Tables
Table 1. Comparison of girls with adolescent idiopathic scoliosis and normal controls by pubertal stage.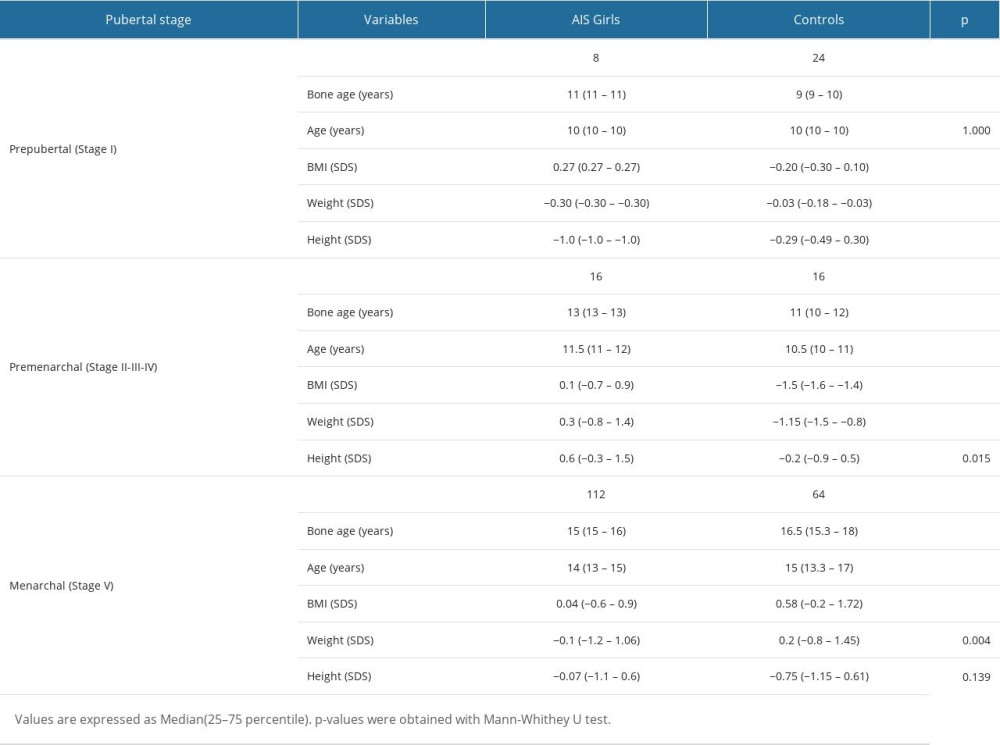 Table 2. Comparison of AIS boys and normal controls by pubertal stage.
Table 2. Comparison of AIS boys and normal controls by pubertal stage.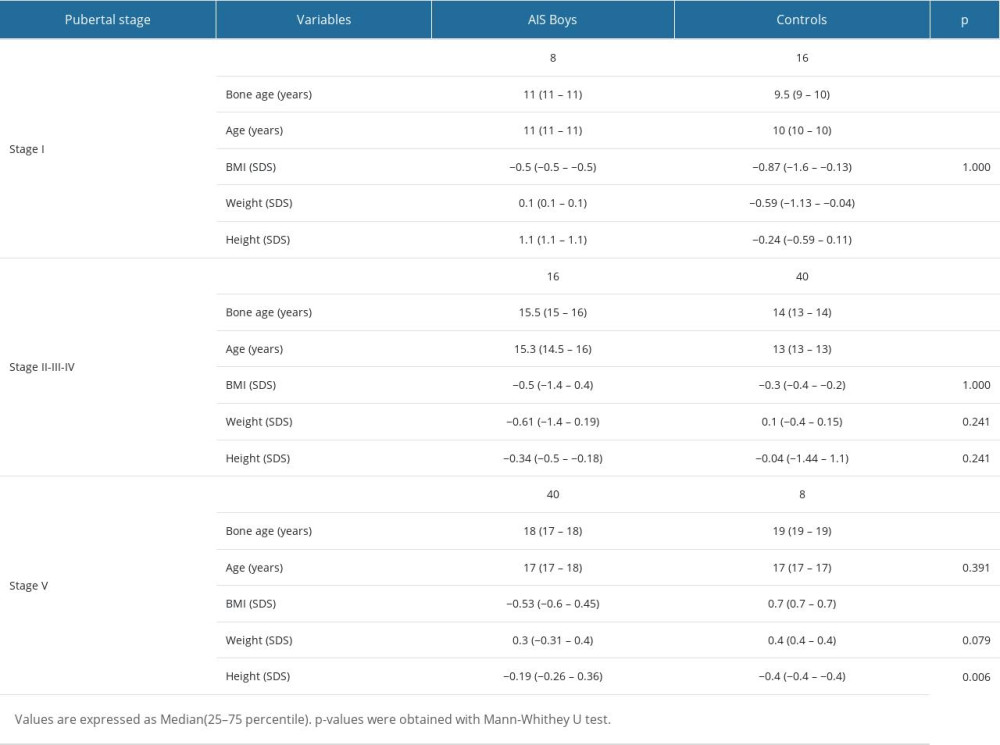 Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.
Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.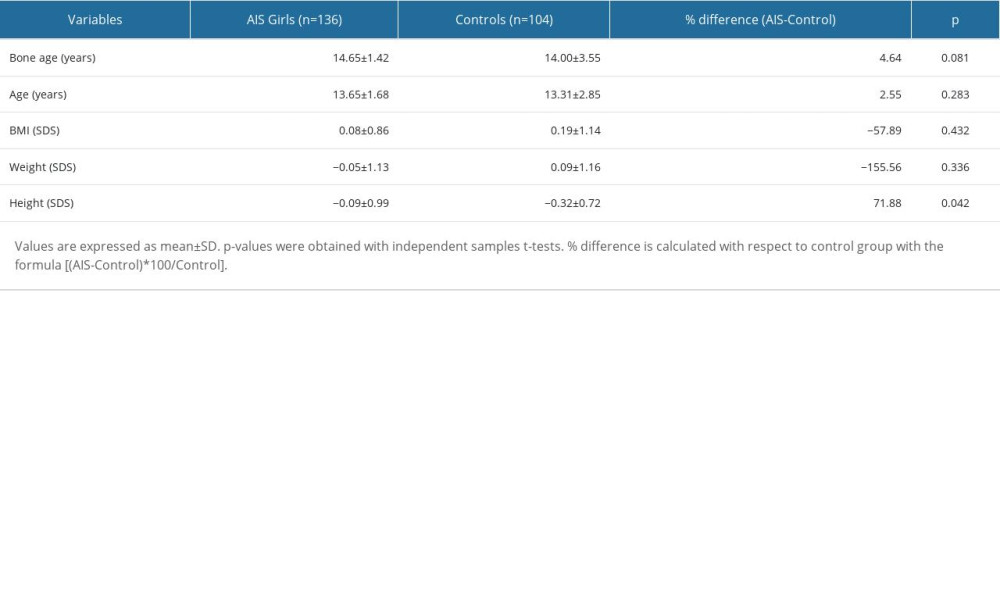 Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.
Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.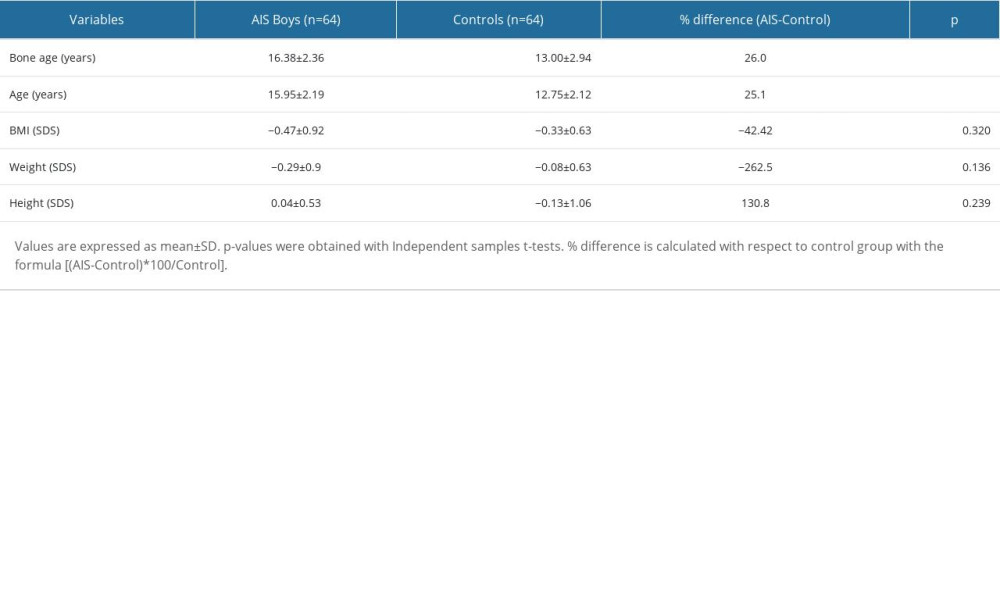 Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys.
Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys.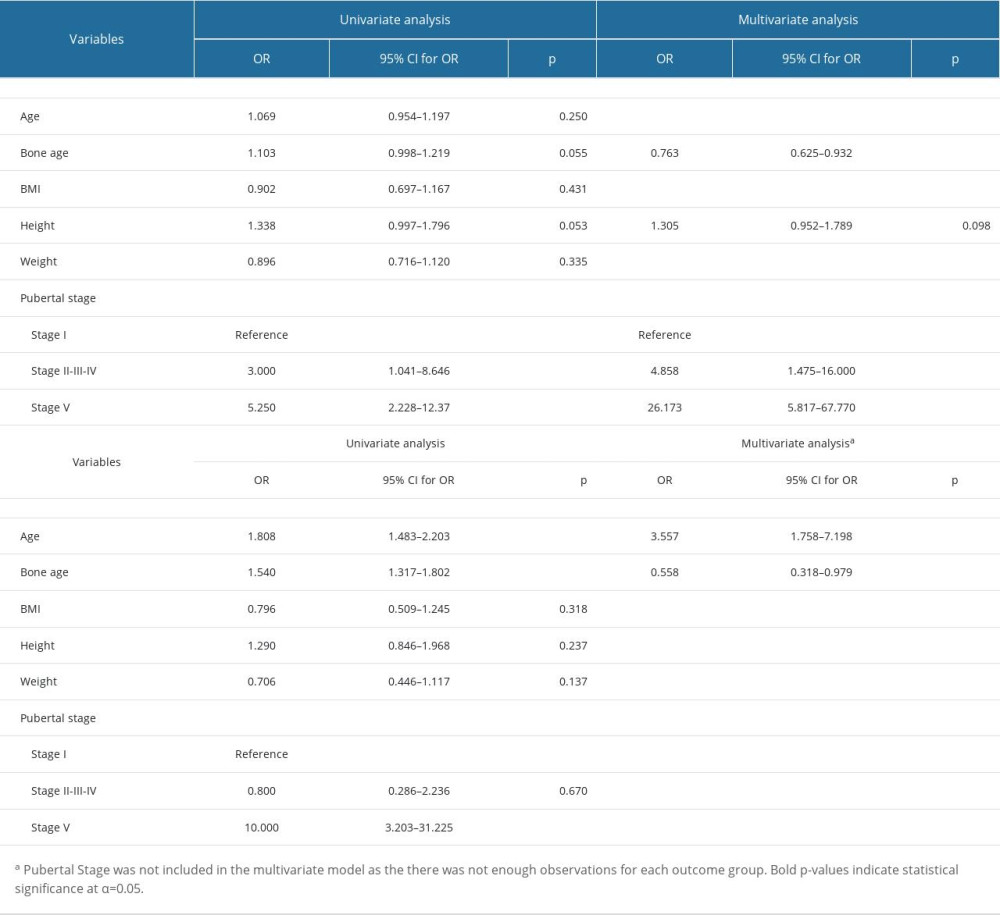
References
1. Bala MM, Bala KA, Association among complete blood count parameters, bone mineral density, and Cobb angle in cases of adolescent idiopathic scoliosis: Med Sci Monit, 2023; 29; e940355
2. Burwell RG, Aetiology of idiopathic scoliosis: Current concepts: Pediatr Rehabil, 2003; 6(3–4); 137-70
3. Kikanloo SR, Tarpada SP, Cho W, Etiology of adolescent idiopathic scoliosis: A literature review: Asian Spine J, 2019; 13(3); 519-26
4. Lonstein JE, Carlson JM, The prediction of curve progression in untreated idiopathic scoliosis during growth: J Bone Joint Surg Am, 1984; 66(7); 1061-71
5. Peterson LE, Nachemson AL, Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from The Brace Study of the Scoliosis Research Society: J Bone Joint Surg Am, 1995; 77(6); 823-27
6. Sadat-Ali M, Al-Othman A, Bubshait D, Al-Dakheel D, Does scoliosis causes low bone mass? A comparative study between siblings: Eur Spine J, 2008; 17(7); 944-47
7. Hung VWY, Qin L, Cheung CSK, Osteopenia: A new prognostic factor of curve progression in adolescent idiopathic scoliosis: J Bone Joint Surg Am, 2005; 87(12); 2709-16
8. Zhang Y, Yang Y, Dang X, Factors relating to curve progression in female patients with adolescent idiopathic scoliosis treated with a brace: Eur Spine J, 2015; 24(2); 244-48
9. Yip BHK, Yu FWP, Wang Z, Prognostic value of bone mineral density on curve progression:A longitudinal cohort study of 513 girls with adolescent idiopathic scoliosis: Sci Rep, 2016; 6; 39220
10. Escalada F, Marco E, Duarte E, Growth and curve stabilization in girls with adolescent idiopathic scoliosis: Spine (Phila Pa 1976), 2005; 30(4); 411-17
11. Goldberg CJ, Fogarty EE, Moore DP, Dowling FE, Scoliosis and developmental theory: Adolescent idiopathic scoliosis: Spine (Phila Pa 1976), 1997; 22(19); 2228
12. Song KM, Little DG, Peak height velocity as a maturity indicator for males with idiopathic scoliosis: J Pediatr Orthop, 2000; 20(3); 286-88
13. Little DG, Song KM, Katz D, Herring JA, Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls: J Bone Joint Surg Am, 2000; 82(5); 685-93
14. Ylikoski M, Height of girls with adolescent idiopathic scoliosis: Eur Spine J, 2003; 12(3); 288-91
15. Yrjönen T, Ylikoski M, Effect of growth velocity on the progression of adolescent idiopathic scoliosis in boys: J Pediatr Orthop B, 2006; 15(5); 311-15
16. Song KM, Little DG, Peak height velocity as a maturity indicator for males with idiopathic scoliosis: J Pediatr Orthop, 2000; 20(3); 286-88
17. August GP, Grumbach MM, Kaplan SL, Hormonal changes in puberty. 3. Correlation of plasma testosterone, LH, FSH, testicular size, and bone age with male pubertal development: J Clin Endocrinol Metab, 1972; 34(2); 319-26
18. Wang Y-N, Zeng Q, Xiong F, Zeng Y, Male external genitalia growth curves and charts for children and adolescents aged 0 to 17 years in Chongqing, China: Asian J Androl, 2018; 20(6); 567
19. Nathan BM, Palmert MR, Regulation and disorders of pubertal timing: Endocrinol Metab Clin North Am, 2005; 34(3); 617-41
20. Bordini B, Rosenfield RL, Normal pubertal development: Part II: Clinical aspects of puberty: Pediatr Rev, 2011; 32(7); 281-92
21. Bundak R, Darendeliler F, Gunoz H, Analysis of puberty and pubertal growth in healthy boys: Eur J Pediatr, 2007; 166(6); 595-600
22. Bundak R, Darendeliler F, Günöz H, Puberty and pubertal growth in healthy Turkish girls: No evidence for secular trend: J Clin Res Pediatr Endocrinol, 2008; 1(1); 8-14
23. Marshall WA, Tanner JM, Variations in pattern of pubertal changes in girls: Arch Dis Child, 1969; 44(235); 291-303
24. Traggiai C, Stanhope R, Delayed puberty: Best Pract Res Clin Endocrinol Metab, 2002; 16(1); 139-51
25. Neyzi O, Günöz H, Furman A, Türk çocuklarında vücut ağırlığı, boy uzunluğu, baş çevresi ve vücut kitle indeksi referans değerleri: Çocuk Sağlığı ve Hast Derg, 2008; 51(1); 1-14 [in Turkish]
26. Hägglund G, Karlberg J, Willner S, Growth in girls with adolescent idiopathic scoliosis: Spine (Phila Pa 1976), 1992; 17(1); 108-11
27. Siu King Cheung C, Tak Keung Lee W, Kit Tse Y, Abnormal peri-pubertal anthropometric measurements and growth pattern in adolescent idiopathic scoliosis: A study of 598 patients: Spine (Phila Pa 1976), 2003; 28(18); 2152-57
28. Wei-Jun W, Xu S, Zhi-Wei W, Abnormal anthropometric measurements and growth pattern in male adolescent idiopathic scoliosis: Eur Spine J, 2012; 21(1); 77-83
29. Antoniazzi F, Zamboni G, Central precocious puberty: Current treatment options: Paediatr Drugs, 2004; 6(4); 211-31
30. Sizonenko PCMartini LBT-E of ED, Sexual maturation, male: Encyclopedia of Endocrine Diseases Elsevier, 2004; 240-44
31. Zachmann M, Prader A, Kind HP, Testicular volume during adolescence. Cross-sectional and longitudinal studies: Helv Paediatr Acta, 1974; 29(1); 61-72
32. Albertsson-Wikland K, Rosberg S, Karlberg J, Groth T, Analysis of 24-hour growth hormone profiles in healthy boys and girls of normal stature: relation to puberty: J Clin Endocrinol Metab, 1994; 78(5); 1195-201
33. Wheeler MD, Physical changes of puberty: Endocrinol Metab Clin North Am, 1991; 20(1); 1-14
34. Neyzi O, Bundak R, Gökçay G, Reference values for weight, height, head circumference, and body mass index in Turkish children: JCRPE J Clin Res Pediatr Endocrinol, 2015; 7(4); 280-93
35. Bunnell WP, The natural history of idiopathic scoliosis before skeletal maturity: Spine (Phila Pa 1976), 1986; 11(8); 773-76
36. Weinstein SL, Ponseti IV, Curve progression in idiopathic scoliosis: J Bone Joint Surg Am, 1983; 65(4); 447-55
37. Weinstein SL, Zavala DC, Ponseti IV, Idiopathic scoliosis: Long-term follow-up and prognosis in untreated patients: J Bone Joint Surg Am, 1981; 63(5); 702-12
38. Ylikoski M, Growth and progression of adolescent idiopathic scoliosis in girls: J Pediatr Orthop B, 2005; 14(5); 320-24
39. Raggio CL, Sexual dimorphism in adolescent idiopathic scoliosis: Orthop Clin North Am, 2006; 37(4); 555-58
40. Wang WJ, Yeung HY, Chu WC-W, Top theories for the etiopathogenesis of adolescent idiopathic scoliosis: J Pediatr Orthop, 2011; 31(1 Suppl); S14-27
41. Karol LA, Johnston CE, Browne RH, Madison M, Progression of the curve in boys who have idiopathic scoliosis: J Bone Joint Surg Am, 1993; 75(12); 1804-10
42. Suh PB, MacEwen GD, Idiopathic scoliosis in males. A natural history study: Spine (Phila Pa 1976), 1988; 13(10); 1091-95
43. Barrios C, Cortés S, Pérez-Encinas C, Anthropometry and body composition profile of girls with nonsurgically treated adolescent idiopathic scoliosis: Spine (Phila Pa 1976), 2011; 36(18); 1470-77
44. Qui Y, Qiu X, Sun XBody mass index in girls with adolescent idiopathic scoliosis: Zhonghua Wai Ke Za Zhi, 2008; 46(8); 588-91 [in Chinese]
45. Qiu Y, Sun X, Qiu X, Decreased circulating leptin level and its association with body and bone mass in girls with adolescent idiopathic scoliosis: Spine (Phila Pa 1976), 2007; 32(24); 2703-10
46. Willner S, Growth in height of children with scoliosis: Acta Orthop Scand, 1974; 45(6); 854-66
47. Dangerfield PH, Anthropometry and scoliosis: J Bone Jt Surg Br, 1974; 56; 382
Tables
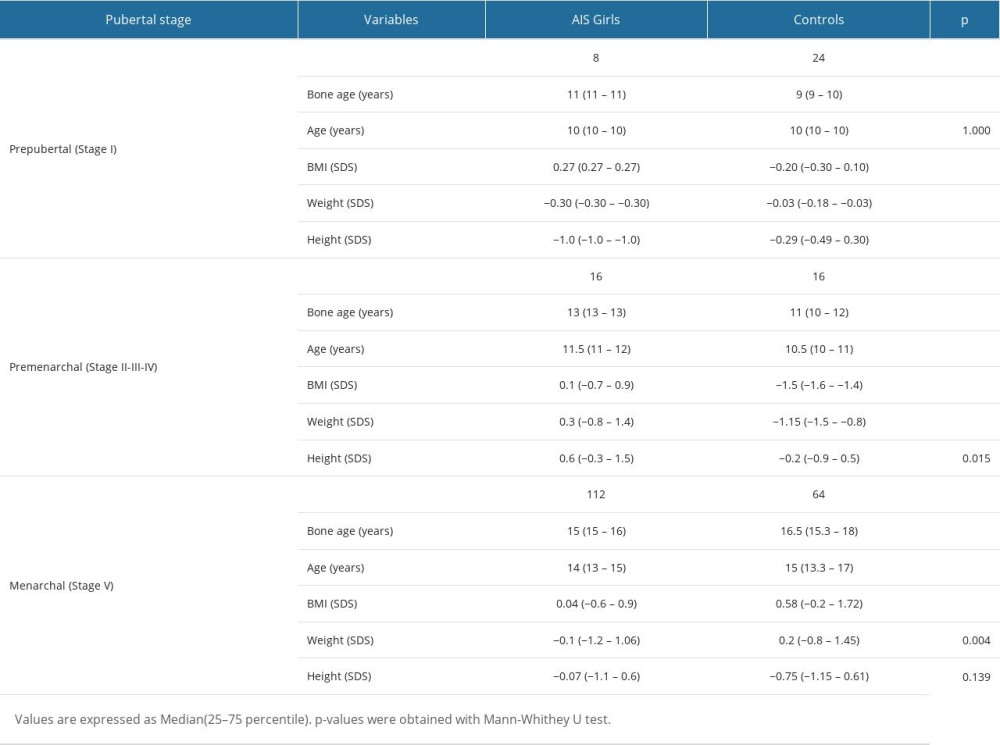 Table 1. Comparison of girls with adolescent idiopathic scoliosis and normal controls by pubertal stage.
Table 1. Comparison of girls with adolescent idiopathic scoliosis and normal controls by pubertal stage.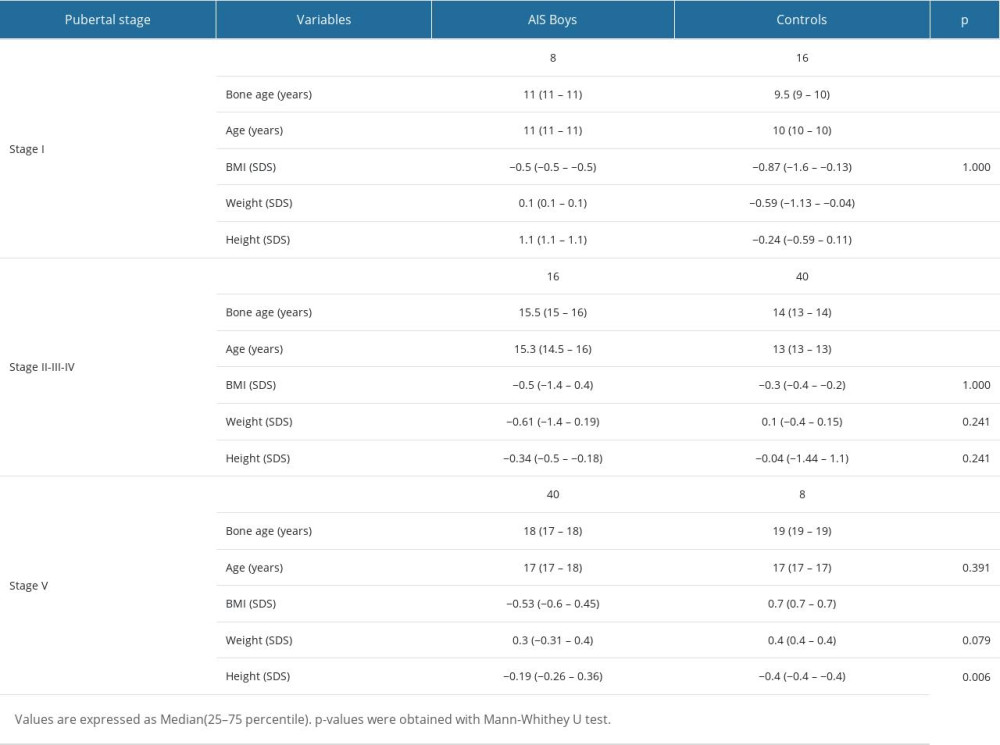 Table 2. Comparison of AIS boys and normal controls by pubertal stage.
Table 2. Comparison of AIS boys and normal controls by pubertal stage.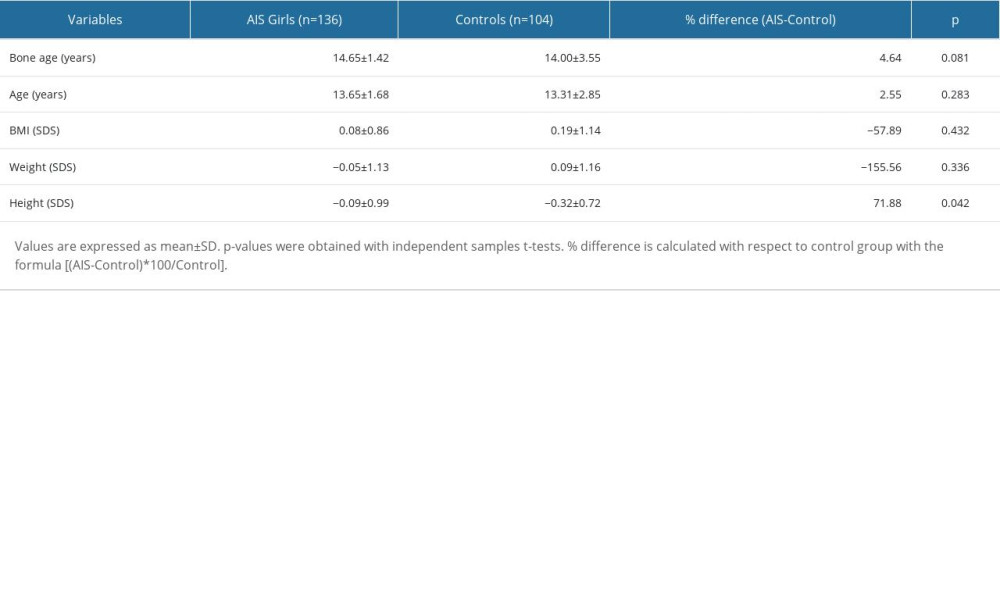 Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.
Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.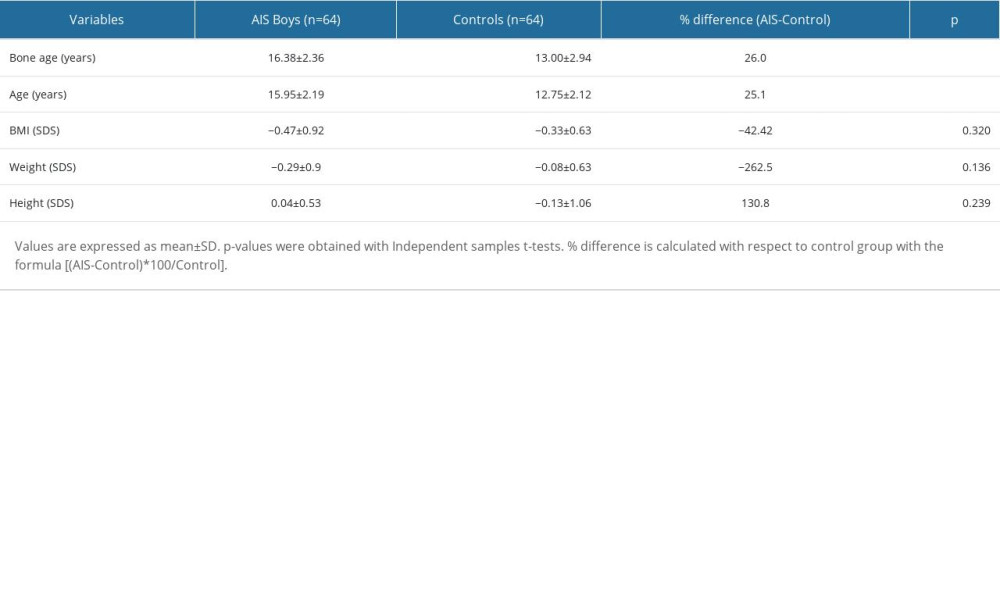 Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.
Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.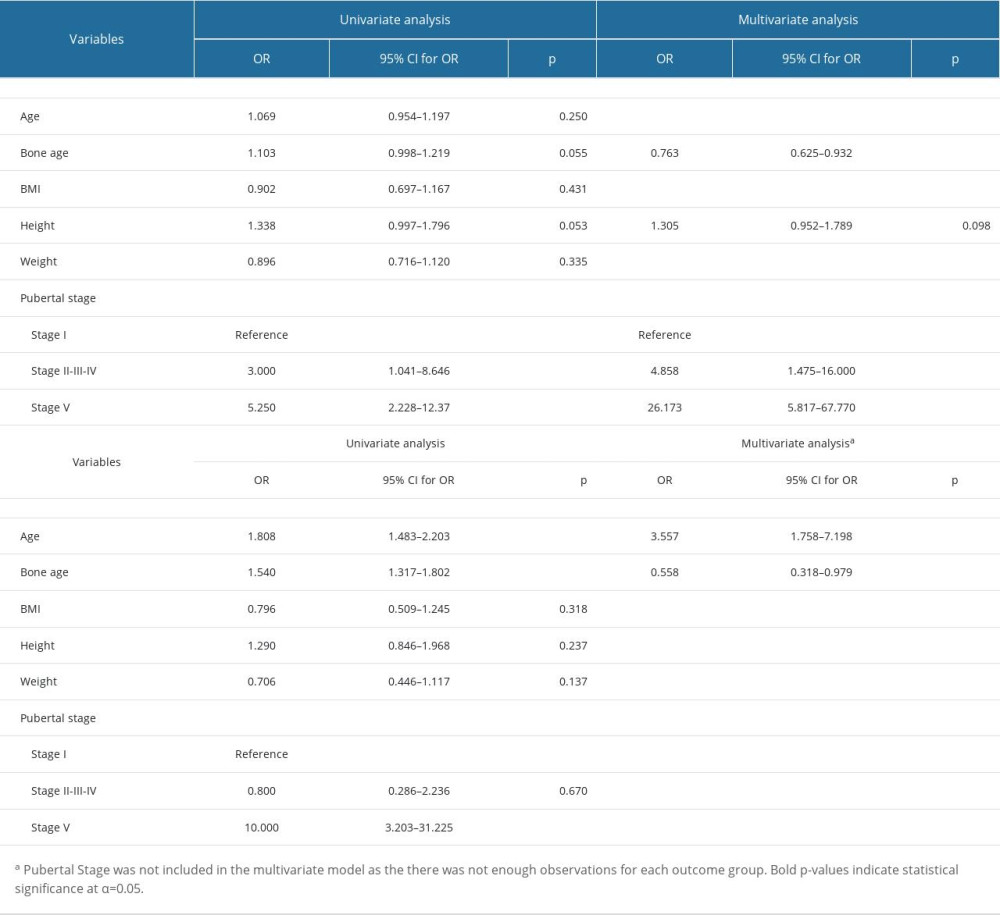 Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys.
Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys.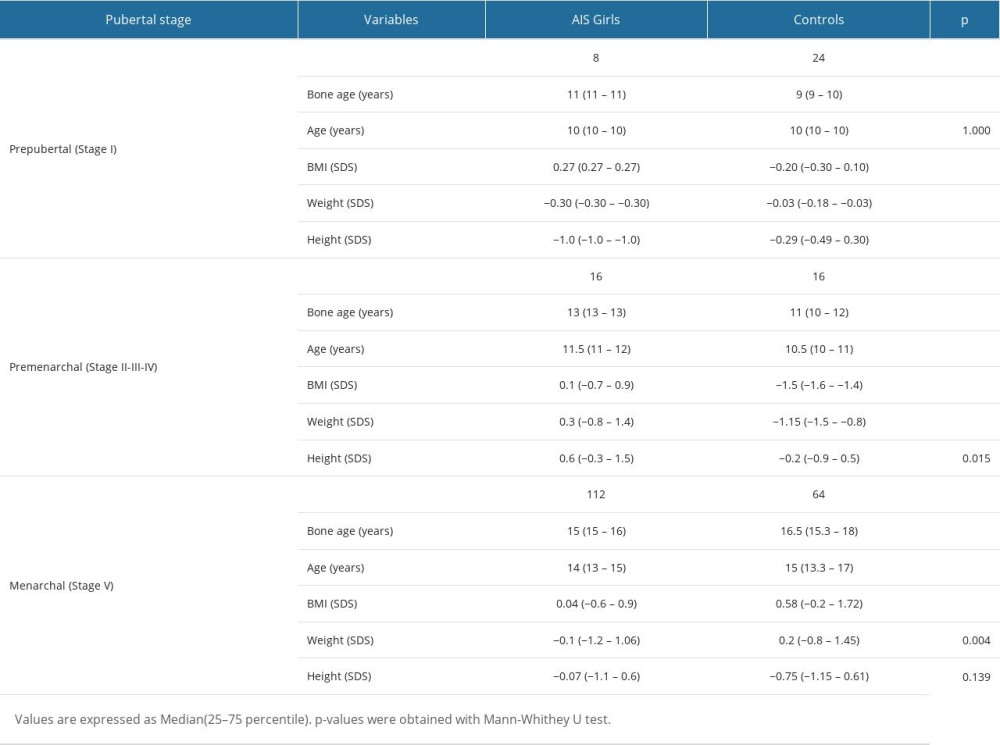 Table 1. Comparison of girls with adolescent idiopathic scoliosis and normal controls by pubertal stage.
Table 1. Comparison of girls with adolescent idiopathic scoliosis and normal controls by pubertal stage.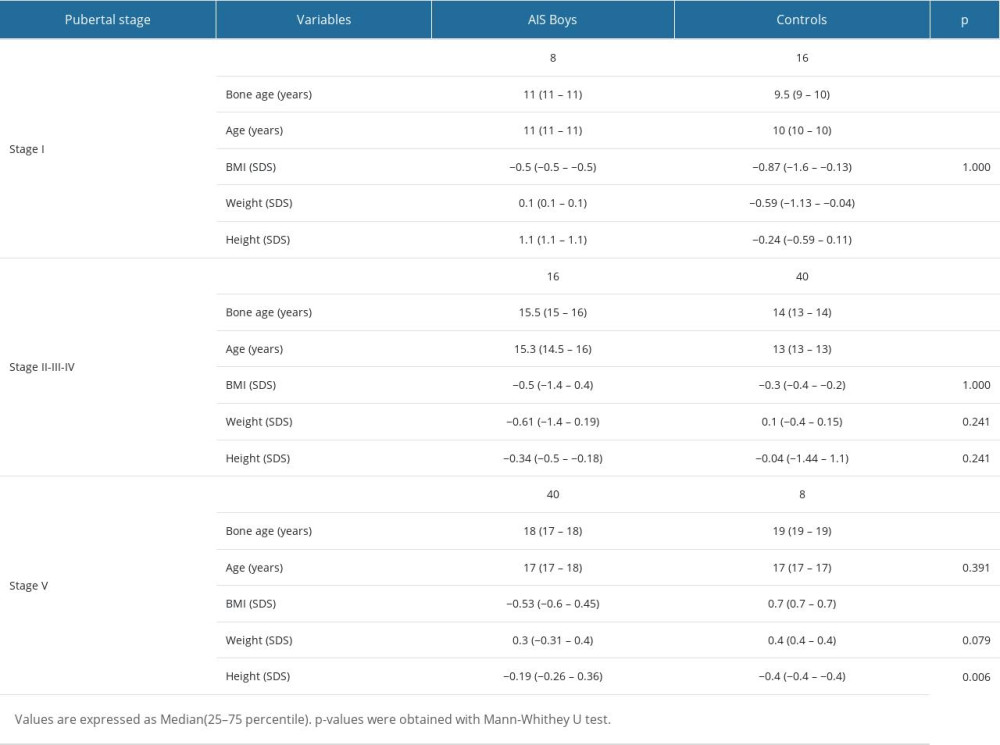 Table 2. Comparison of AIS boys and normal controls by pubertal stage.
Table 2. Comparison of AIS boys and normal controls by pubertal stage.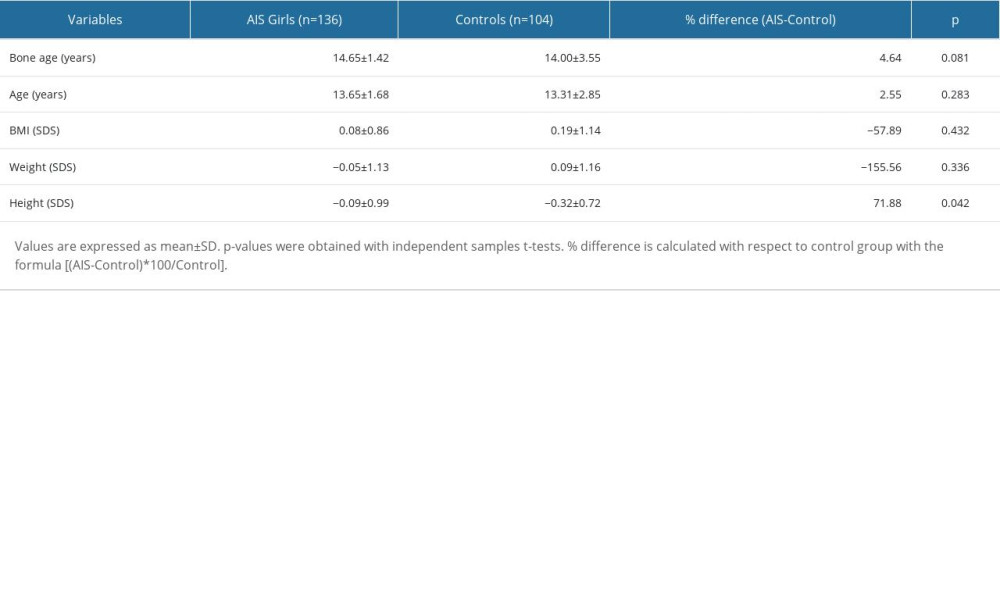 Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.
Table 3. Overall mean differences between girls with adolescent idiopathic scoliosis and controls.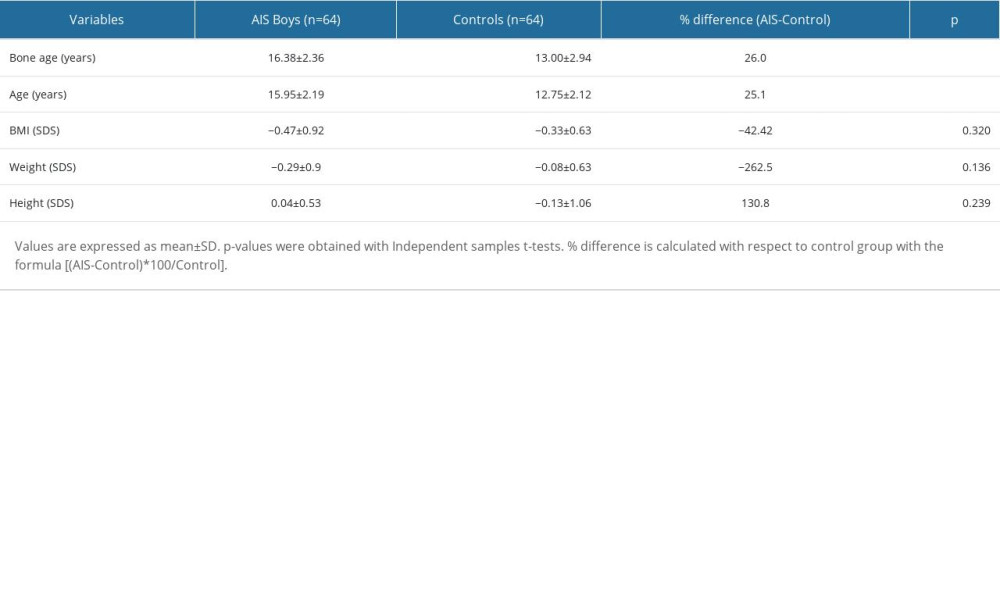 Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.
Table 4. Overall mean differences between boys with adolescent idiopathic scoliosis and controls.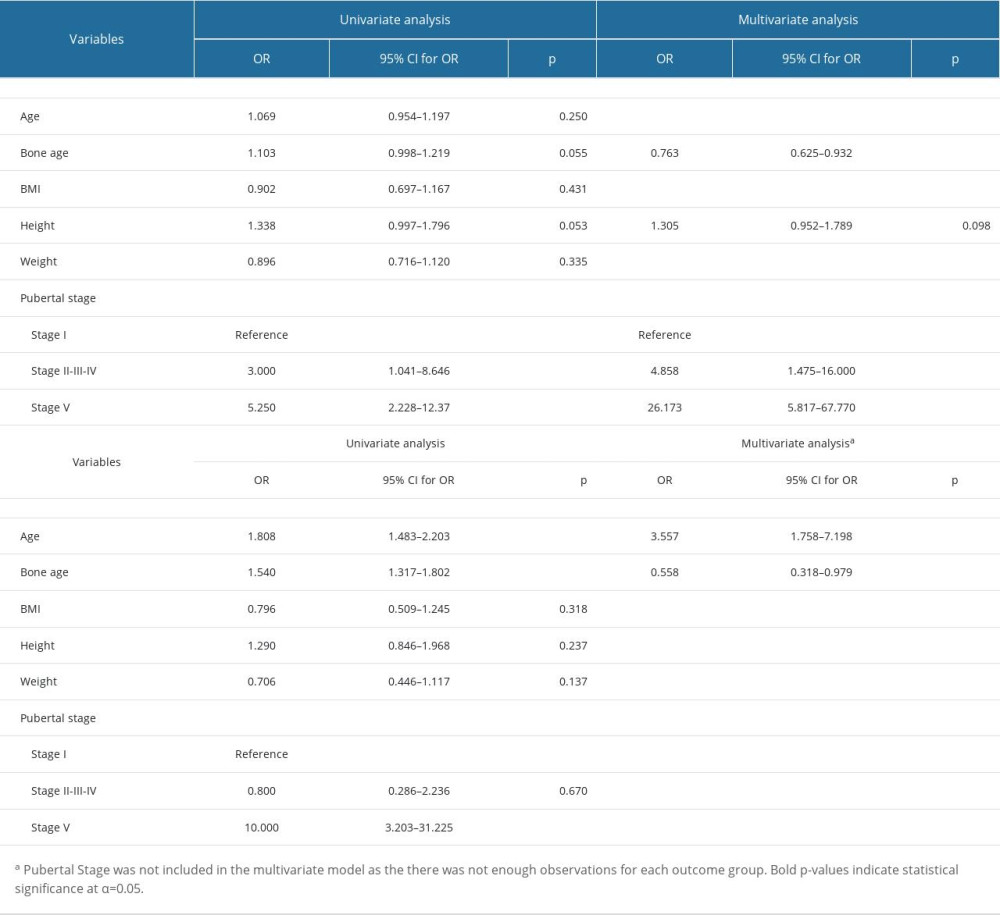 Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys.
Table 5. Logistic regression analysis to assess factors related to adolescent idiopathic scoliosis in girls and boys. In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952