08 September 2023: Clinical Research
Determinants of Attitude to a Humanoid Social Robot in Care for Older Adults: A Post-Interaction Study
Sławomir TobisDOI: 10.12659/MSM.941205
Med Sci Monit 2023; 29:e941205
Abstract
BACKGROUND: While there is a growing body of research examining opinions on social robots in elderly care, there is a lack of comprehensive studies investigating the underlying factors influencing these opinions. The Godspeed Questionnaire Series (GQS) measures perceptions related to human-robot interactions (HRIs). The Comprehensive Geriatric Assessment (CGA) is widely used to evaluate physical, cognitive, and social functions of older patients. The EASYCare 2010 Standard (EC) is a tool for assessing unmet needs in older individuals. TIAGo, a social humanoid robot, integrates perception, navigation, and HRI capabilities. This study aimed to identify the determinants of perception following interactions between older individuals and TIAGo, utilizing the GQS, selected CGA items, and EC.
MATERIAL AND METHODS: We analyzed a database of opinions from older individuals who interacted with TIAGo, based on the Users’ Needs, Requirements, and Abilities Questionnaire. We examined the relationships between the robot’s roles (companion/assistant/useful device), its assistive/social functions, and various characteristics of the older participants.
RESULTS: The study included 161 participants (mean age: 75.2±9.8 years), comprising 89 women and 113 institutionalized individuals. Positive correlations were observed between the robot’s role, its functions, and the participants’; perceptions across most evaluated parameters (Anthropomorphism, Animacy, Likeability, Perceived intelligence, Perceived safety). Only a few individual correlations were found for other parameters.
CONCLUSIONS: The primary determinant of older individuals’ opinions was their perception of the robot. Therefore, involving older adults in the co-design process of such robots is crucial. Additionally, a paradigm shift is needed in the study of humanoid social robots, focusing on successful aging rather than deficits associated with aging
Keywords: Aged, Geriatric Assessment, Needs Assessment, Patient Care, Robotics, Humans, Female, Aged, 80 and over, social interaction, Aging, Databases, Factual
Background
Aging of societies presents an increasing challenge [1]. The rising percentage of older people, especially the “oldest-old,” needs attention on many levels since a substantial fraction of these persons requires support in everyday functioning [2,3]. Simultaneously, the ability to employ working-age people, particularly trained caregivers, is more and more limited, which means that securing this support is increasingly difficult [4]. The current paradigm of “aging in place” requires that all possible actions be taken to enable the aging persons to live in their homes for as long as possible instead of institutionalization [5,6]. One of the ways to achieve this goal, given the shortage of potential caregivers, which is not likely to improve anytime soon, may be a deployment of technological solutions [7], therein, especially the ones using socially-assistive robots [8].
Older people constitute a heterogeneous societal group with widely differing characteristics of health and independence [9]. This also means that the abilities and needs of individual persons differ, sometimes significantly. Since there reportedly is no “one-size-fits-all” technological solution for the analyzed area [10], investigating the determinants of perception and acceptance of robots in elder care may be a good way to provide tailored interventions that meet the future users’ needs and expectations and thus enhance the chances for a successful implementation. Although there are numerous acceptance studies related to older subjects in the literature [11,12], to the best of our knowledge, no effort has so far been undertaken to comprehensively analyze the results of the geriatric assessment as potential determinants of attitudes to robots in care for older adults.
We previously analyzed the attitudes of various stakeholders to the TIAGo robot (PAL Robotics, Barcelona, Spain): first, by presenting them with a static picture of a humanoid social robot and then by letting the potential users interact with it. We developed and validated a dedicated assessment tool – the Users’ Needs, Requirements, and Abilities Questionnaire. With its help, we observed consistently high acceptance of the idea of using social robots in care for older people. We also demonstrated that a real-world interaction with the machine influences some of the aspects of potential users’ opinions. In the current study, we focused on factors widely used in clinical and care practice: sociodemographic and self-assessment items, as well as selected scores from the Comprehensive Geriatric Assessment and needs assessed with a dedicated tool (EASYCare Standard 2010). Therefore, this study aimed to analyze these factors and users’ perceptions as potential determinants for the attitudes of older adults toward the roles and functions of the robot.
Material and Methods
ETHICS STATEMENT:
The study was based on the analysis of a database of older people’s opinions about the use of robots in eldercare after interacting with the robot. The study was approved by the Bioethics Committee of Poznań University of Medical Sciences (Protocol No. 711/18). All studied subjects gave their consent for participation after receiving a full explanation of the nature of the study.
THE PROCEDURE OF THE STUDY:
The investigation involved 161 older subjects with an average age of 75.2±9.8 years, including 59 aged at least 80 years (36.6%). In the participating group, there were 89 women (55.3%); 113 people lived in long-term care institutions (70.2%), and 48 were participants of daycare units, living in the community.
The inclusion criteria were at least 60 years of age, cognitive status ensuring understanding of questions and providing adequate answers, as well as the completeness of the data record for the current analysis.
THE TIAGO ROBOT:
During the study, the subjects had an opportunity to interact with the TIAGo robot (Figure 1). We used a customized version of the TIAGo, equipped with a range of sensors (an RGB-D camera for depth recognition, a thermal camera for following humans, an RFID antenna for tracing lost objects, a laser scanner, environment sensors, and radar sensors), a microphone, a loudspeaker, and a touch tablet for communication with the user. The robot used a wireless network to communicate with a remote computer (AIS – Ambient Intelligence System) connected via the Internet to a cloud-based Networked Care Platform). During the interaction, the participants could select options from cognitive games, reminders, safety measures, physical exercises, dietary recommendations, audio/video connectivity, news, and weather, as well as presentation of environmental values (eg, temperature, humidity, air pressure, air quality) [13].
The interaction sessions lasted from approximately 60 to 150 minutes, until every participant felt they had sufficient time to operate the machine, and included 11–23 older subjects, depending on the number of persons willing to interact and their degree of interest. Detailed rules for the data collection on the role of the robot in care for older adults were presented in a previous paper based on a study conducted in 6 long-term care institutions [13].
THE USERS’ NEEDS, REQUIREMENTS, AND ABILITIES QUESTIONNAIRE: The opinions on the use of the robot in care for older adults were analyzed using the Users’ Needs, Requirements, and Abilities Questionnaire (UNRAQ). The questionnaire has been validated, and its good psychometric properties have been demonstrated [14]. It consists of affirmative statements grouped in 4 areas (A – Interaction with the robot and technical issues, B – Assistive role of the robot, C – Social aspects, and D – Ethical issues), to which the respondents are expected to respond on a 5-point Likert scale (I completely disagree, etc.). In the current study, the scores of the following statements were examined:
Opinions on assistive and social functions were also analyzed. In the UNRAQ, there are 13 statements describing the assistive functions and 6 describing the social ones (a detailed description of the tool can be found in [14]). Mean scores of assistive and social functions were calculated for each participant – for the social functions, the calculation scheme was as follows:
where C was the resulting mean value for opinions on the social functions of the robot and C1,…, C6 represented numerical scores of the 6 individual statements on the Likert scale (1–5) for a given person. Analogous calculations were performed for the assistive functions.
GODSPEED QUESTIONNAIRE SERIES: The perception of the robot was measured with the Godspeed Questionnaire Series (GQS). GQS consists of 5 scales that assess features such as Anthropomorphism, Animacy, Likeability, Perceived intelligence, or Perceived safety of robots on a scale of 1 to 5 [15]. It has been broadly used in research on humanoid robots, as shown in the meta-analysis by Weiss and Bartneck [16].
The participants were also asked to fill out a basic personal data form and to declare their computer skills, ease of use of technology, and feeling of loneliness, and also to provide self-assessment of health and physical independence, all rated on a scale of 1 to 5.
COMPREHENSIVE GERIATRIC ASSESSMENT: The study included selected elements of Comprehensive Geriatric Assessment (CGA) and needs assessment for each subject. Within the CGA, evaluations of cognitive functions, mood, and functional capacity were performed. An overview of CGA assessments has been given by Parker et al [17], and an example of CGA implementation can be found in Conroy et al [18].
MINI-MENTAL STATE EXAMINATION: Cognitive functions were measured using the Mini-Mental State Examination (MMSE), according to Folstein [19]. The results were adjusted for age and education [20]. Only people who scored at least 15 on the MMSE scale were included in the analysis, as it is accepted that subjects meeting this criterion are able to understand questions and provide adequate answers [21,22].
GERIATRIC DEPRESSION SCALE: Mood was assessed using the 15-item Geriatric Depression Scale (GDS), which is a screening tool for depression; positive screening: scores above 5, out of 15 possible [23].
BARTHEL INDEX, LAWTON SCALE: The Barthel Index (BI) was used to evaluate independence in activities of daily living (ADL) [24]. The possible score is 0–100 points, and higher scores mean greater independence. Independence in the instrumental activities of daily living (IADL) was measured using the Lawton scale, which includes 8 activities [25]. Each of them is rated on a scale of 0/1, where 1 means that it is performed independently.
EASYCARE STANDARD 2010: Unmet needs were assessed with the EASYCare Standard 2010 (EC) tool. The authors have experience in using this questionnaire from previous studies [26–29]. This tool includes 49 items reflecting 49 needs in 7 domains:
The particular strengths of this tool are its summarizing indexes: Independence score, Risk of breakdown in care, and Risk of falls, derived from the analysis of needs in the above domains [30]. For each participant, the number of areas in which needs were present, as well as the total number of needs from all areas (with the maximum possible count of 49), were also calculated.
DATA ANALYSIS:
The following factors were taken into account as possible determinants of the analyzed opinions about the robot as a potential caregiver for older adults:
STATISTICAL ANALYSIS:
Statistical analysis was performed with STATISTICA 13 software (TIBCO Software, Poland). Normality was analyzed with the Shapiro-Wilk test. Due to lack of normality of some of the studied parameters, non-parametric tests were used in further analyses. For binary data, the analysis was done with the χ2 (chi-square) test with Yates correction for small groups; for others, the Spearman coefficient was used as a measure of correlation in data. Values are thus presented as means±SD and median or percentage, where applicable.
Results
CHARACTERISTICS OF THE STUDIED GROUP:
The largest group of respondents had secondary education (62 people, 38.5%); only 27 (16.8%) had education above secondary, including 17 with higher education (10.6%).
The respondents declared (on a scale of 1–5) their computer use skills only at the level of 1.7±1.3 (median 1.0) because as many as 120 people (74.2%) reported that they did not use a computer at all, and only 17 (8.7%) had no problem with that. Notably, for the ease of use of technology, the average score was 3.2±1.6 (median 3). On a scale of 1–5, the subjects assessed their health status at 3.1±1.0 (median 3), fitness at 3.2±1.0 (median 3), and loneliness at 2.6±1.5 (median 3).
The average MMSE score of the respondents was 23.3±4.1 points (median 24). Only 31 subjects scored below 20 points. The average GDS score was 3.8±2.8 points (median 3); 37 people scored above 5 points, which indicated the presence of symptoms of depression. The average value of BI was 82.2±20.5 points (median 90); none of the respondents was extremely dependent (score of 20 points or less). On the Lawton scale, the subjects obtained an average of 4.9±2.4 points (median 5).
As for the assessment of needs, according to the EC questionnaire, the existence of needs was found on average in 5 domains (5.1±1.4, median 5). All the respondents had unmet needs – the lowest number of needs was 3, reported in domain 7 (occurrence of pain and loss of a loved one, low self-assessment of health). The average number of reported needs was 15.8±6.8, median 15, and in terms of individual domains, the mean values were as follows:
For the EC summarizing indexes, the Independence score had an average value of 23.6±20.6 points (median 20), the Risk of breakdown in care was 3.9±2.1 (median 4), and the Risk of falls was 1.8±1.4 (median 2): 42 people (26.1%) had increased risk of falls (score greater than 2).
The mean scores of the Godspeed Questionnaire Series, measuring the perception of the robot, were as follows: Anthropomorphism was 3.0±0.9 (median 3.0), Animacy was 3.2±1.1 (median 3.2), Likeability was 4.3±0.9 (median 4.8), Perceived intelligence was 4.4±0.7 (median 4.6), and Perceived safety was 3.0±0.9 (median 3.0).
DETERMINANTS OF RESULTS OBTAINED FOR THE ROLE OF THE ROBOT IN THE CARE OF OLDER ADULTS:
Older people rated the role of the robot as a useful device significantly higher than that of a companion (4.6±0.9 vs 4.3±1.2;
In terms of demographic parameters, only gender was found to be related to the assessment of the companion role of the robot – the rating of men was higher in this respect (P<0.05, Table 1). Education was found to be significant for the social functions of the robot (P<0.05).
We observed no relationship between the opinions of older people on the role of the robot in care for older people with any of the self-assessment parameters (Computer use, Ease of use of technology, Loneliness, Health status, Fitness). For functional capacity factors, only an inversely proportional relationship was found between the scores of the robot as an assistant and independence on the ADL scale (ie, people with a higher value, and therefore being more independent, had lower expectations towards the robot as an assistant; r =−0.1800, P<0.05). This was additionally reflected in the relationship between the assessment of this role and the independence score index of the EC questionnaire (P<0.05; Table 2). This phenomenon is a reflection of the strong negative correlation between the Barthel Index and the Independence score (r=−0.8763, P<0.0001, data not shown).
A detailed analysis of the role of the robot in the context of the number of needs reported by the participants in the domains of the EC questionnaire revealed a weak positive correlation between the number of needs in domain 5 (Accommodation and finances) and higher results in terms of the robot as a useful device (r=0.1745,
A relationship between the role of the robot declared by the participants and the perception of the robot assessed with the Godspeed Questionnaire Series was found. The only exception was the Anthropomorphism series, for which no relationship with the useful device perspective was observed (Table 3).
DETERMINANTS OF RESULTS OBTAINED FOR THE ROBOT’S ASSISTIVE AND SOCIAL FUNCTIONS:
Older subjects (the whole studied group) rated the robot’s assistive functions significantly higher than social functions (4.6±0.7 vs 4.4±0.8;
For sociodemographic parameters, only education was found to be related to the opinions expressed about the robot as a useful device; the assessment of people with higher education levels was lower (
No relationship was found between the self-assessment parameters and the opinions of older people either on the assistive or social functions of the robot. Similarly, no correlation was found for the parameters describing functional capacity.
The analysis of needs based on the EC questionnaire showed that the scores of assistive functions were related to the number of declared needs in domain 4 (Safety) – the more needs in this area, the higher the assessment of assistive functions (r=0.1763, P<0.05). No relationships were observed between the number of needs in other areas or the results of the questionnaire’s summarizing indexes and the assessment of assistive and social functions (Table 2).
As was the case with the role of the robot, we found relationships between the scores of assistive and social functions of the robot and the perception of the robot measured with the GQS. The exceptions were Anthropomorphism for assistive functions and Perceived safety series for social functions (Table 3).
Discussion
FUTURE DIRECTIONS:
The opinions of older people about the projected roles and functions of the robot – after experiencing an interaction with the TIAGo robot – are shaped by multiple factors, including gender, education, ADL, and unmet needs. Still, undoubtedly, the main determinant of these opinions is the perception of the robot. Henceforth, virtually all aspects of perception (eg, anthropomorphism and likeability) appear to determine its role and functions in the eyes of potential end-users, which, in turn, may constitute an important factor in the success of the implementation of the robot in care for older adults.
Notably, we observed no relationship between the robot’s anthropomorphism and its strictly utilitarian role (that is, that of a tool) and its assistive functions, while there was such a relationship with the social aspects of its use. This indicates that studied subjects did expect specific features of the robot’s appearance when considering its social functions.
The lack of strong relationships between self-assessment values, CGA items, and unmet needs and attitudes toward robots in elder care seems to suggest that humanoid social robots require a study model that concentrates on successful aging rather than on deficits related to aging, as also suggested by other researchers [51,52]. A model of successful aging does not view it as a process of continuing losses and older adults as needing more and more assistance – which restricts the design of new technologies – but rather focuses on preservation of the user’s autonomy and making use of their resources. This approach can and should be applied to designing, implementing, and using socially-assistive robots.
Our results indicate the need for further research in the field, which may be viewed as an intersection of geriatrics/gerontology, psychology, and engineering, using validated research tools. At the same time, in the practical aspect, they confirm the necessity to involve older adults in the co-design of technological solutions [53].
Conclusions
The opinions of older people about the roles and functions of TIAGo were mainly due to their perception of the robot. Older adults should be involved in root design to improve quality of life rather than problems associated with aging.
Tables
Table 1. Opinions of participants (n=161) on the role of the robot in care for older adults and its functions, grouped by sociodemographic parameters (mean±SD).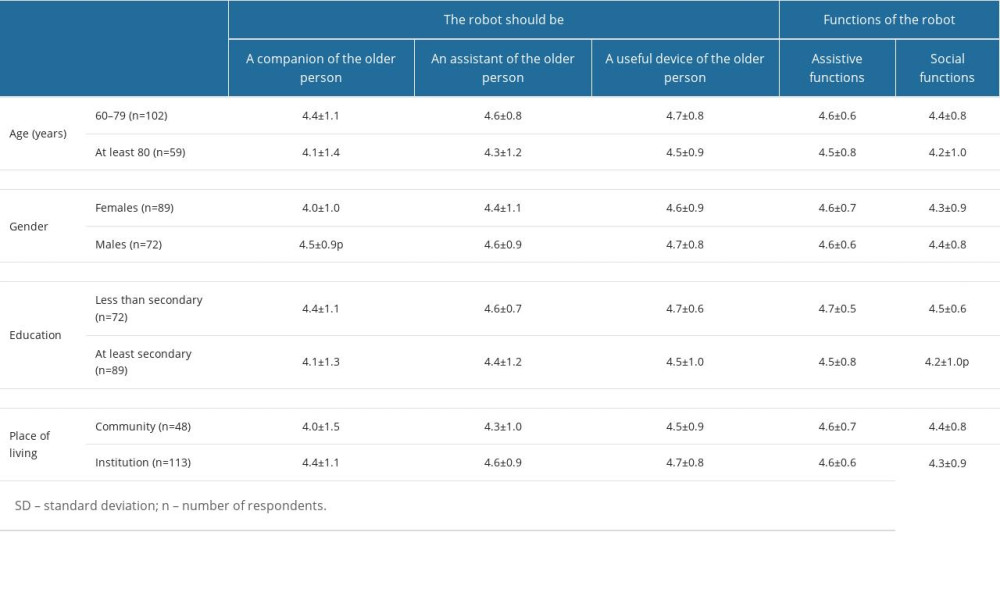 Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis.
Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis. Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series.
Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series.
References
1. The National Institute on Aging: Strategic directions for research, 2020-2025. NIA Strategic Directions, 2020 Available fromhttps://www.nia.nih.gov/about/aging-strategic-directions-research
2. Guay M, Dubois MF, Corrada M, Exponential increases in the prevalence of disability in the oldest old: A Canadian national survey: Gerontology, 2014; 60(5); 395-401
3. Hagberg JE: Being the oldest old in a shifting technology landscape, 2016; 107-24, Routledge, Generational use of new media
4. European Commission. Economy and Finance: The 2018 ageing report: economic and budgetary projections for the EU member states (2016-2070), 2018 Available fromhttps://economy-finance.ec.europa.eu/publications/2018-ageing-report-economic-and-budgetary-projections-eu-member-states-2016-2070_en
5. Wiles JL, Leibing A, Guberman N, The meaning of “aging in place” to older people: Gerontologist, 2012; 52(3); 357-66
6. Iecovich E, Aging in place: From theory to practice: Anthropological notebooks, 2014 Available fromhttp://www.drustvo-antropologov.si/AN/PDF/2014_1/Anthropological_Notebooks_XX_1_Iecovich.pdf
7. Queirós A, Santos M, Rocha NP, Cerqueira M, Technologies for ageing in place to support community-dewlling older adults: Semantic Scholar, 2017
8. Matarić MJ, Scassellati B: Socially assistive robotics. Springer handbook of robotics, 2016; 1973-94, Cham, Springer
9. Tobis S, Jaracz K, Kropinska S, Needs of older persons living in long-term care institutions: On the usefulness of cluster approach: BMC Geriatr, 2021; 21(1); 316
10. Greenhalgh T, Procter R, Wherton J, What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services: BMC Med, 2015; 13(1); 91
11. Asgharian P, Panchea AM, Ferland F, A review on the use of mobile service robots in elderly care: Robotics, 2022; 11(6); 127
12. Beuscher LM, Fan J, Sarkar N, Socially assistive robots: Measuring older adults’ perceptions: J Gerontol Nurs, 2017; 43(12); 35-43
13. Tobis S, Piasek J, Cylkowska-Nowak M, Robots in eldercare: How does a real-world interaction with the machine influence the perceptions of older people?: Sensors, 2022; 22(5); 1717
14. Tobis S, Neumann-Podczaska A, Kropinska S, UNRAQ – A questionnaire for the use of a social robot in care for older persons. A multi-stakeholder study and psychometric properties: Int J Environ Res Public Health, 2021; 18(11); 6157
15. Bartneck C, Kulić D, Croft E, Measurement instruments for the anthropomorphism, animacy, likeability, perceived intelligence, and perceived safety of robots: Int J Soc Robot, 2008; 1(1); 71-81
16. Weiss A, Bartneck C, Meta analysis of the usage of the Godspeed Questionnaire Series, 2015
17. Parker SG, McCue P, Phelps K, What is comprehensive geriatric assessment (CGA)? An umbrella review: Age Ageing, 2018; 47(1); 149-55
18. Conroy SP, Bardsley M, Smith P: Comprehensive geriatric assessment for frail older people in acute hospitals: The HoW-CGA mixed-methods study, 2019, Southampton (UK), NIHR Journals Library
19. Folstein MF, Folstein SE, McHugh PR, “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician: J Psychiatr Res”, 1975; 12(3); 189-98
20. Mungas D, Marshall SC, Weldon M, Age and education correction of Mini-Mental State Examination for English and Spanish-speaking elderly: Neurology, 1996; 46(3); 700-6
21. Chopra MP, Sullivan JR, Feldman Z, Self-, collateral- and clinician assessment of depression in persons with cognitive impairment: Aging Ment Health, 2008; 12(6); 675-83
22. Henneges C, Reed C, Chen YF, Describing the sequence of cognitive decline in Alzheimer’s disease patients: Results from an observational study: J Alzheimers Dis, 2016; 52(3); 1065-80
23. Marc LG, Raue PJ, Bruce ML, Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population: Am J Geriatr Psychiatry, 2008; 16(11); 914-21
24. Mahoney FI, Barthel DW, Functional evaluation: The Barthel Index: Md State Med J, 1965; 14; 61-65
25. Lawton MP, Brody EM, Assessment of older people: Self-maintaining and instrumental activities of daily living: Gerontologist, 1969; 9(3); 179-86
26. Tobis S, Jaracz K, Talarska D, Validity of the EASYCare Standard 2010 assessment instrument for self-assessment of health, independence, and well-being of older people living at home in Poland: Eur J Ageing, 2018; 15(1); 101-8
27. Talarska D, Tobis S, Kotkowiak M, Determinants of quality of life and the need for support for the elderly with good physical and mental functioning: Med Sci Monit, 2018; 24; 1604-13
28. Talarska D, Strugala M, Szewczyczak M, Is independence of older adults safe considering the risk of falls?: BMC Geriatr, 2017; 17(1); 66
29. Talarska D, Kropińska S, Strugała M, The most common factors hindering the independent functioning of the elderly at home by age and sex: Eur Rev Med Pharmacol Sci, 2017; 21(4); 775-85
30. Philip KE, Alizad V, Oates A, Development of EASY-Care, for brief standardized assessment of the health and care needs of older people; With latest information about cross-national acceptability: J Am Med Dir Assoc, 2014; 15(1); 42-46
31. Louie WY, McColl D, Nejat G, Acceptance and attitudes toward a human-like socially assistive robot by older adults: Assist Technol, 2014; 26(3); 140-50
32. Torta E, Werner F, Johnson DO, Evaluation of a small socially-assistive humanoid robot in intelligent homes for the care of the elderly: J Intell Robot Syst, 2014; 76(1); 57-71
33. Piasek J, Wieczorowska-Tobis K, Acceptance and long-term use of a social robot by elderly users in a domestic environment, 2018, Gdańsk, Poland, IEEE
34. Carros F, Meurer J, Löffler D, Exploring human-robot interaction with the elderly: Results from a ten-week case study in a care home Available from: https://dl.acm.org/doi/10.1145/3313831.3376402
35. Chu L, Chen HW, Cheng PY, Identifying features that enhance older adults’ acceptance of robots: A mixed methods study: Gerontology, 2019; 65(4); 441-50
36. Shourmasti ES, Colomo-Palacios R, Holone H, User experience in social robots: Sensors (Basel), 2021; 21(15); 5052
37. Bedaf S, Marti P, Amirabdollahian F, A multi-perspective evaluation of a service robot for seniors: The voice of different stakeholders: Disabil Rehabil Assist Technol, 2018; 13(6); 592-99
38. Caleb-Solly P, Dogramadzi S, Huijnen CAGJ, Exploiting ability for human adaptation to facilitate improved human-robot interaction and acceptance: Inf Soc, 2018; 34(3); 153-65
39. Hebesberger D, Koertner T, Gisinger C, A long-term autonomous robot at a care hospital: A mixed methods study on social acceptance and experiences of staff and older adults: Int J Soc Robot, 2017; 9(3); 417-29
40. Pinney J, Carroll F, Newbury P, Human-robot interaction: The impact of robotic aesthetics on anticipated human trust: PeerJ Comput Sci, 2022; 8; e837
41. Vandemeulebroucke T, Dzi K, Gastmans C, Older adults; experiences with and perceptions of the use of socially assistive robots in aged care: A systematic review of quantitative evidence: Arch Gerontol Geriatr, 2021; 95; 104399
42. Suwa S, Tsujimura M, Kodate N, Exploring perceptions toward home-care robots for older people in Finland, Ireland, and Japan: A comparative questionnaire study: Arch Gerontol Geriatr, 2020; 91; 104178
43. May DC, Holler KJ, Bethel CL, Survey of factors for the prediction of human comfort with a non-anthropomorphic robot in public spaces: Int J Soc Robot, 2017; 9(2); 165-80
44. Naneva S, Sarda Gou M, Webb TL, A systematic review of attitudes, anxiety, acceptance, and trust towards social robots: Int J Soc Robot, 2020; 12(6); 1179-201
45. Carradore M, Social robots in the home: What factors influence attitudes towards their use in assistive care?: Ital Sociol Rev, 2021; 11(3); 879-901
46. Chen K, Chan AH, Gerontechnology acceptance by elderly Hong Kong Chinese: A senior technology acceptance model (STAM): Ergonomics, 2014; 57(5); 635-52
47. Ke C, Lou VW, Tan KC, Changes in technology acceptance among older people with dementia: the role of social robot engagement: Int J Med Inform, 2020; 141; 104241
48. Kobb R, Hilsen P, Ryan P, Assessing technology needs for the elderly: finding the perfect match for home: Home Healthc Nurse, 2003; 21(10); 666-73
49. Broadbent E, Stafford R, MacDonald B, Acceptance of healthcare robots for the older population: review and future directions: Int J Soc Robot, 2009; 1(4); 319-30
50. Broadbent E, Tamagawa R, Patience A, Attitudes towards health-care robots in a retirement village: Australas J Ageing, 2012; 31(2); 115-20
51. Papadopoulos I, Koulouglioti C, Lazzarino R, Enablers and barriers to the implementation of socially assistive humanoid robots in health and social care: A systematic review: BMJ Open, 2020; 10(1); e033096
52. Lee HR, Riek LD, Reframing assistive robots to promote successful aging: ACM Transactions on Human-Robot Interaction (THRI), 2018; 7(1); 1-23
53. Sumner J, Chong LS, Bundele A, Co-designing technology for aging in place: A systematic review: Gerontologist, 2021; 61(7); e395-e409
Tables
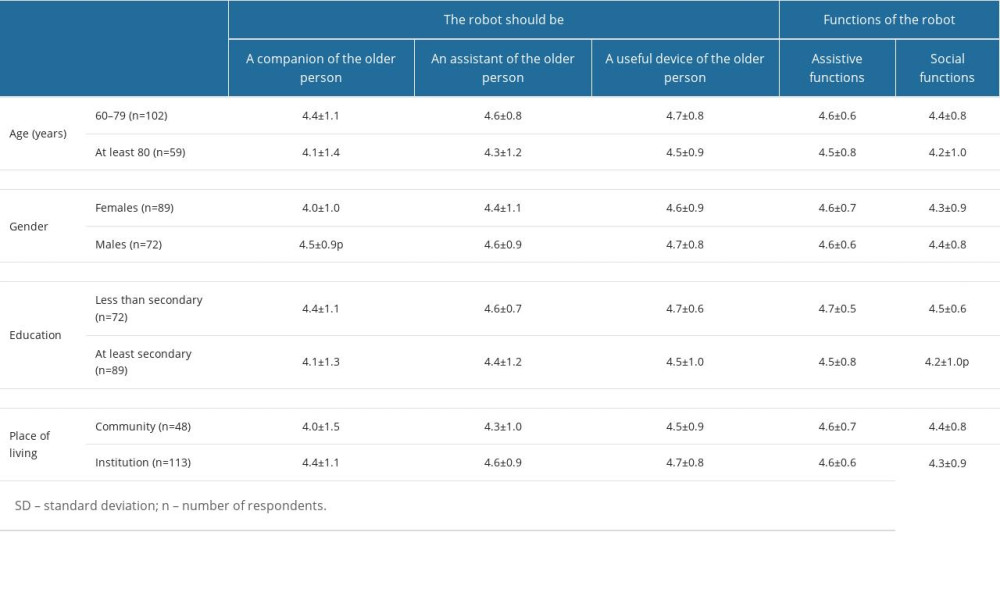 Table 1. Opinions of participants (n=161) on the role of the robot in care for older adults and its functions, grouped by sociodemographic parameters (mean±SD).
Table 1. Opinions of participants (n=161) on the role of the robot in care for older adults and its functions, grouped by sociodemographic parameters (mean±SD). Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis.
Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis. Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series.
Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series.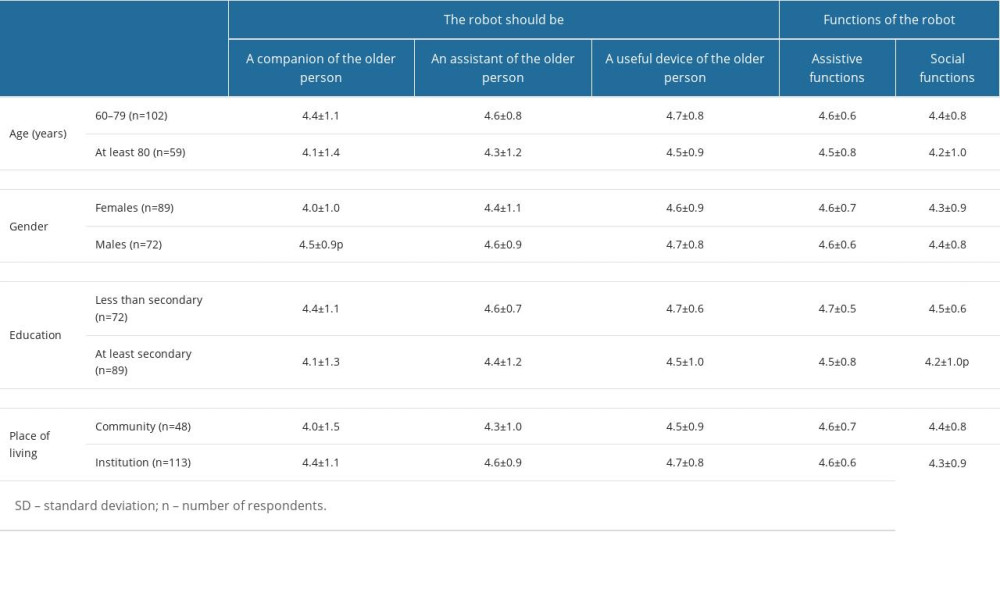 Table 1. Opinions of participants (n=161) on the role of the robot in care for older adults and its functions, grouped by sociodemographic parameters (mean±SD).
Table 1. Opinions of participants (n=161) on the role of the robot in care for older adults and its functions, grouped by sociodemographic parameters (mean±SD). Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis.
Table 2. Assessment of the correlation between the participants’ opinions (n=161) on the role of the robot and the robot’s functions in care for older adults grouped by self-assessment, functional capacity, and needs analysis. Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series.
Table 3. Correlations between the participants’ opinions (n=161) on the role of the robot and its functions in care for older people, grouped on the perception of the robot according to Godspeed Questionnaire Series. In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









