11 September 2023: Clinical Research
A Retrospective Study of Far Lateral Midline Microlumbar Discectomy in 20 Patients at a Single Center in Turkey
Serdal AlbayrakDOI: 10.12659/MSM.941257
Med Sci Monit 2023; 29:e941257
Abstract
BACKGROUND: Microdiscectomy is a minimally-invasive surgical technique for treating far lateral lumbar disc herniation (FLLDH). This retrospective study from a single center in Turkey aimed to evaluate midlinelumbar discectomy in 20 patients with far lateral lumbar disc herniation.
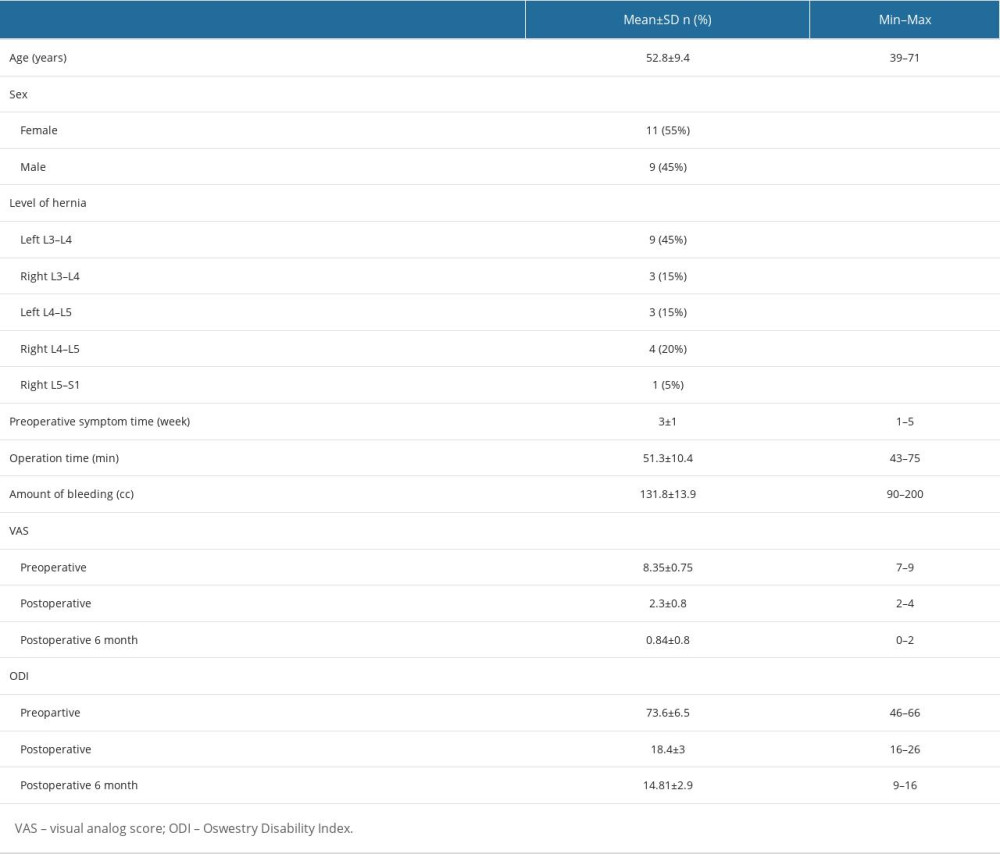
MATERIAL AND METHODS: We collected clinical data of 20 patients (11 men, 9 women) operated for FLDDH between January 2006 and January 2022. Patients’ age, sex, surgical level, examination findings, motor deficit, duration of operation, complications during the operation and preoperative/postoperative 6 month visual analogue Scala (VAS), preoperative/postoperative 6th month Oswestry Disability Index (ODI) scores were evaluated.
RESULTS: The patients were 11 men (55%) and 9 women (45%), with a mean age of 52.08±11.21 years. The mean duration of symptoms before the operation was 3.4 weeks. Laseque sign positivity was found in 86.4% of the patients. Motor deficit was present in 30% of the patients. After 6-month follow-up, preoperative VAS value decreased from 9.35±0.75 to 0.84±0.75. Preoperative and postoperative VAS score averages were significantly different (P=0.0001). Operation ODI values were 73.63±3.76 before and after surgery, and decreased to 14.81±3.63 at 6 months.
CONCLUSIONS: The term distal lateral disc herniation was first defined in the literature in 1974 when the disc was seen in a different location than the normal location compared to the facet. Far lateral disc herniation can be operated on successfully with midline skin incision.
Keywords: Lumbar Vertebrae, Spine, Spinal Cord, Intervertebral disc disease, Male, Humans, Female, Adult, Middle Aged, Retrospective Studies, Turkey, Intervertebral Disc Displacement, Dermatologic Surgical Procedures, Diskectomy
Background
ANATOMY:
Far lateral region anatomically; anteriorly the disc distance, medially the edge of the superior articular facet, posteriorly the facet joint itself and defined as the area lateral to the inferior pedicles. In far lateral disc herniation, the disc is attached to the root emerging lateral to the foramen and presses on the dorsal root ganglion, causing root displacement.
DIAGNOSIS:
Magnetic resonance imaging (MRI) is the criterion standard method for diagnosis. Distant lateral disc herniations lateral to the pedicle are either isointense or hypointense. Sagittal cross-sectional MRI is the most effective way to image distal lateral disc hernias, and has been shown to be a useful test.
Material and Methods
SURGICAL PROCEDURE:
Surgical technique is defined for L4–L5 far lateral disc as an example. Patients were positioned prone under general or spinal anesthesia after necessary monitoring and intravenous connections were provided in the sterile operating room. After level detection with scopy, sterile staining, and dressing, the relevant level was entered with a midline skin incision of approximately 3–4 cm. The paravertebral muscle fascia was opened from the midline and the paravertebral muscles were dissected by blunt dissection. Two Taylor retractors were placed to expose the upper and lower facet junction. After determining the level with fluoroscopy, under the microscope, the L3–L4 facet junction, L4–L5 facet junction, and L4 pars interarticularis were revealed. After L4 hemi-laminectomy with the help of high-speed drill and Kerrison ronjer, first the L4 root was found and followed. The medial facet was removed with the help of high-speed drill and Kerrison ronjer and progressed downwards. Then, the L5 root was found. After the disc space was found, it was palpated with a blunt nerve hook at the exit level of the exiting root. Then, the lateral part of the disc level was palpated with the help of the hook, and visualization of the disc was attempted. The posterior longitudinal ligament was incised, and the far lateral and foraminal disc fragments at the L4–5 intervertebral disc distance were excised. Then, the fascia was closed surgically and the skin was closed subcutaneously.
STATICAL ANALYSIS:
Statistical analysis was performed with Friedman test in the evaluation of Oswesttry scores before and after the operation. The Siegel Castellan test was used in the analysis of binary non-parametric values. A
Results
The mean age of these patients 11 men (55%) and 9 women (45%) was 52.08±11.21 years. Three patients hadiabetes mellitus (DM), 2 had hypertension (HT), and 1 had both HT and DM. No rheumatic disease was detected in any patient. One patient had participated in a 10-day rehabilitation program before the operation. The mean duration of symptoms before the operation was 3.4 weeks. Laseque sign positivity was found in 86.4% of the patients. 16.6% of the patients had motor deficits without leg and low back pain. Leg pain and motor deficit were present in 56.3%. Sensory deficit was present in 81.5% of the patients (Table 1). Far lateral disc herniation was found in 66.6% of the patients and far lateral and foraminal disc herniation was found in 33.3% of the patients on preoperative MR images.
Sequestrectomy was performed in 58.3% of the patients, and both sequestrectomy and discectomy were performed in 41.6%. The mean operation time was 51.03±10.71 minutes. None of the patients had nerve root injury, cerebrospinal fluid complications such as (CSF) fistula, or hematoma at the operation site.
After the 6-month follow-up, preoperative VAS values decreased from 9.35±0.75 to 0.84±0.75. When the preoperative and postoperative VAS values were compared, the difference in the postoperative VAS values was statistically significant (
Postoperative results after 6 months according to satisfaction of patients after surgery was classified as excellent (no pain), good (mild pain), moderate (moderate pain), and poor (unchanged or more severe pain) according to the MacNab classification. Eight patients were excellent (40%), 7 patients were good (35%), and 3 patients were moderately satisfied (15%).
Discussion
Twenty cases operated on with midline incision were included in our study. The procedure of finding the upper root after hemilaminectomy and limited facet removal after midline incision are methods that neurosurgeons are familiar with. As a result of this surgery, statistically significant pain regression was achieved and a statistically significant positive contribution was made to the quality of life index. In our study, this surgical method was found to be effective and reliable.
The definition of far lateral disc herniation was first introduced in the literature in 1974, when it was defined as lateral and below the facet in an abnormal location. Although it is rare, it may occur with severe pain and nerve deficit due to nerve root and ganglion compression. Its treatment is usually surgical, and different techniques have been described for surgical intervention [5,6].
Possible surgical procedures include the following: a far lateral intertransverse approach with midline incision, an approach with midline limited or total facetectomy, lateral and paramedian transmuscular approaches, minimally-invasive techniques with microdiscectomy using an ipsilateral and contralateral tubular retractor, and percutaneous posterolateral transforaminal endoscopic surgical methods [7].
Midline incision after subperiosteal dissection is the method most familiar to spine surgeons. With this method, the upper root can be exposed in a conventional way, thus minimizing the risks of nerve damage and complications that can occur in surgery. In the surgery performed with a midline incision in the context of root damage, the root and ganglion are encountered early when the pars and/or facet joint laterals are turned, and this may be an advantage to reduce rupture. However, excessive removal of the facet joint to reach the upper root and pass to the lateral of the disc can in some cases cause low back pain and instability [7].
Ipsilateral tubuler endoscopic surgery is started by targeting the lateral of the disc with fluoroscopy control. From the incision, after gentle stripping of the para-spinal muscles, the endoscope system is inserted and guided by fluoroscopy up to the bony attachment of the pars interarticularis. It is then drilled at the lateral end of the pars interarticularis-lamina junction. By exposing the lateral part of the ligamentum flavum, a laminotomy field is created along the lateral aspect of the pars interarticularis and lamina. Then, the nerve and adipose tissue emerging after using the the Kerrison ronjer, and the intertransverse ligament is recognized and the disc is removed [8]. Endoscopic methods are more comfortable surgeries for postoperative patients, as their bone removal rates and muscle stripping levels are low. Operations can be performed through a small incision, but the learning process is long for surgeons. Therefore, it may be difficult to recognize anatomical landmarks during surgery and to distinguish between the upper root and disc.
The paramedian approach described by Wiltse and Spencer requires muscle stripping with less bone resection and provides a more direct approach to the neural foramen [9]. According to the position of the extruded disc part, the lateral surface of the facet joint and the isthmus are drilled. If the disc herniation is displaced cranially, the lateral surface of the pars interarticularis is drilled further. If far lateral disc herniation is not directed superiorly and inferiorly, the lateral surface of the isthmus is drilled less and the lateral surface of the facet joint is drilled more. Then, the intertransverse ligament is found and the root is found with the help of the Kerrision ronjer and the disc is removed [10]. However, this method is not a method that many spine surgeons are familiar with. It can increase the chance of nerve damage during surgery. However, combined lateral and medial approaches have also been described in the literature [11].
Far lateral disc disease is generally seen in older patients. In elderly patients, the duration of the operation and the amount of bleeding in the surgical procedure are important. For this reason, the short operation time in this surgery and the low amount of bleeding in the surgery can be considered advantages. The average age in previous reports was 55–56 years. In the current study, the mean age was 52.9 years [12]. The mean operative time for far lateral disc surgery has been reported to be 41–70 minutes [12]. However, in this study, the mean operation time was 51.3 minutes [13]. The amount of bleeding during surgery has been reported as 124–131.32 mL for FLDH [14], and this was 110.8 mL in the current study.
Long-term pressure on the dorsal root can affect the nerve fibers here and cause neuropathic pain. Therefore, shortening the operation time after diagnosis in far lateral disc herniation cases with surgical indication can reduce the risk of postoperative neuropathic pain. The patients were operated on within 20 days at the latest after the indication for surgery. Moderate neuropathic pain lasting for 5 months developed in 3 patients postoperatively, and pregabalin was administered to these patients for neuropathic pain, 150 mg twice a day, and was gradually tapered off after 5 months.
Several limitations should be considered when interpreting the results of the present study. The number of patients and the follow-up period werere not sufficient. In the future, our clinic will work on this subject again by increasing the number of cases and extending the follow-up period. We think that with more patients and a longer follow-up period, more precise information can be obtained about the surgical success of the long-term midline incision, postoperative low back pain, and instability levels.
Conclusions
Spinal surgery with midline skin incision is a method familiar to neurosurgeons. Far lateral disc herniation can be successfully operated on with this method by visualizing the upper nerve root. Our study is limited by the small number of cases and the short follow-up period.
References
1. Tessitore E, de Tribolet N, Far-lateral lumbar disc herniation: The microsurgical transmuscular approach: Neurosurgery, 2004; 54; 939-42
2. Porchet F, Chollet-Bornand A, de Tribolet N, Long-term follow up of patients surgically treated by the far-lateral approach for foraminal and extraforaminal lumbar disc herniations: J Neurosurg, 1999; 90; 59-66
3. Abdullah A, Ditto E, Byrd EB, Extreme-lateral lumbar disc herniations: Clinical syndrome and special problems of diagnosis: J Neurosurg, 1974; 41; 229-34
4. Quaglietta P, Cassitto D, Corriero AS, Paraspinal approach to the far lateral disc herniations: Retrospective study on 42 cases: Acta Cir Bras, 2005; 92; 115-19
5. Abdullah A, Ditto EW, Byrd EB, Extremelateral lumbar disc herniations: Clinical syndrome and special problems of diagnosis: J Neurosurg, 1974; 41; 229-34
6. Kotil K, Akcetin M, Bilge T, A minimally invasive transmuscular approach to far-lateral L5–S1 level disc herniations: A prospective study: J Spinal Disord Tech, 2007; 20; 132-38
7. Yeom JS, Kim KH, Hong SW, A minimally invasive technique for L5–S1 intraforaminal disc herniations: microdiscectomy with a tubular retractor via a contralateral approach: J Neurosurg Spine, 2008; 8(2); 193-98
8. Yoshimoto M, Iwase T, Takebayashi T, Microendoscopic discectomy for far lateral lumbar disk herniation: Less surgical invasiveness and minimum 2-year follow-up results: J Spinal Disord Tech, 2014; 27; E1-7
9. Wiltse LL, Spencer CW, New uses and refinements of the paraspinal approach to the lumbar spine: Spine, 1988; 13(6); 696-706
10. Kaya M, Keskin E, Ceylan D, Surgical treatment of far lateral lumbar disc herniation: Outcomes of the safe and simple midline approach: Cureus, 2022; 14(8); e27907
11. Kunogi J, Hasue M, Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression: Spine, 1991; 16(11); 1312-20
12. Aydın AL, Sasani M, Sasani H, Comparison of two minimally invasive techniques with endoscopy and microscopy for extraforaminal disc herniations: World Neurosurg, 2020; 144; e612-e21
13. Yüce I, Kahyaoğlu O, Çavuşoğlu H, Surgical outcomes of extraforaminal microdiskectomy by midline incision for far-lateral lumbar disk herniation: Neurol Surg A Cent Eur Neurosurg, 2021; 82; 27-33
14. Shawky Abdelgawaad A, Babic D, Siam AE, Extraforaminal microscopic assisted percutaneous nucleotomy for foraminal and extraforaminal lumbar disc herniations: Spine J, 2018; 18; 620-25
In Press
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952