18 October 2023: Meta-Analysis
Suggested Electroacupuncture for Postoperative Nausea and Vomiting: A Comprehensive Meta-Analysis and Systematic Review of Randomized Controlled Trials
Zhenxu Han1AB, Xi Zhang1CE, Huan Yang2BC, Ping Yuan2CDF, Huanyuan Wang3CF, Guangzhong Du3AG*DOI: 10.12659/MSM.941262
Med Sci Monit 2023; 29:e941262
Abstract
BACKGROUND: The purpose of this meta-analysis was to evaluate the effectiveness of electroacupuncture in preventing and treating postoperative nausea and vomiting (PONV) after general anesthesia.
MATERIAL AND METHODS: We searched for papers on randomized controlled trials on electroacupuncture for PONV prevention after general anesthesia published in PubMed, Web of Science, and China National Knowledge Infrastructure (CNKI) since October 1, 2016. Primary outcome was incidence of PONV; secondary outcomes were incidence of postoperative nausea (PON) at 6 h, postoperative vomiting (POV) at 6 h, and postoperative antiemetic requirement. Data were combined and analyzed using RevMan 5.4.1 software.
RESULTS: Eight randomized controlled trials, with 899 total participants, were included. Findings showed (1) there was no significant difference in occurrence rate of PONV between electroacupuncture and control groups (OR=0.31, 95% CI [0.06, 1.49], P=0.14, I²=82%); (2) electroacupuncture reduced incidence of PON at 6 h postoperatively, compared with controls (OR=0.43, 95% CI [0.27, 0.67], P=0.0002, I²=0%); (3) compared with control group, electroacupuncture reduced POV incidence 0-6 h postoperatively (OR=0.38, 95% CI [0.23, 0.63], P=0.0001, I²=0%); (4) electroacupuncture group demonstrated a significant reduction in postoperative requirement for antiemetic medications (OR=0.44, 95% CI [0.25, 0.78], P=0.005, I²=61%); (5) one study reported adverse reactions during observation, with 3 patients experiencing pain and itching at acupuncture site and 2 patients refusing a second acupuncture treatment; all symptoms lasted less than 2 h.
CONCLUSIONS: Based on current evidence, electroacupuncture significantly reduces the occurrence rate of PON and POV at 6 h after surgery and the use of antiemetic medication postoperatively. However, more high-quality, large-sample randomized controlled trials are needed to further validate its efficacy.
Keywords: Anesthesia, General, Electroacupuncture, Meta-Analysis, Postoperative Nausea and Vomiting, Humans, Antiemetics, Randomized Controlled Trials as Topic, Acupuncture Therapy
Background
Postoperative nausea and vomiting (PONV) refers to a series of symptoms such as nausea, retching, and vomiting that occur in a specific period after surgery. It is one of the common complications during the perioperative period, with an incidence rate of approximately 30% [1]. In high-risk individuals, the incidence rate can reach 70% to 80% [2], making PONV the second most common postoperative complication after pain [3]. The exact mechanism of PONV has not been fully elucidated, but current understanding suggests that it is the result of the interaction between various receptors and neurotransmitters in the central and visceral nervous systems [4]. The occurrence of PONV increases the incidence of postoperative complications and prolongs hospital stay [5,6], leading to increased healthcare costs and a significant economic burden on the medical system. Therefore, finding the optimal method for treating PONV following general anesthesia has become an urgent clinical challenge.
In recent years, acupuncture has been widely used as a non-pharmacological therapy for the prevention and treatment of PONV. Some studies have indicated that acupuncture at the Neiguan point (PC6) can effectively prevent the occurrence of PONV [7,8]. Currently, most meta-analyses on intervention measures include acupuncture or transcutaneous electrical acupoint stimulation (TEAS) [9–11]. However, there is a lack of meta-analyses specifically focusing on electroacupuncture for PONV. TEAS is a therapy that combines the theory of meridian acupoints in acupuncture with transcutaneous electrical nerve stimulation (TENS). The main difference between TEAS and electroacupuncture lies in the technique used. Electroacupuncture involves needle insertion into the skin, whereas TEAS applies electrodes on the acupoints, making it a non-invasive procedure. Electroacupuncture refers to a contemporary form of acupuncture in which pulsed current stimulation at varying frequencies and techniques is incorporated to enhance the therapeutic effects. This approach has gained widespread acceptance and is extensively used in clinical practice [12]. Compared with traditional acupuncture, electroacupuncture provides objective and precise control over stimulation parameters, allowing for quantitative, stable, and prolonged stimulation of acupoints. However, there is currently a lack of meta-analyses on the use of electroacupuncture for the prevention and treatment of PONV after general anesthesia. Therefore, we conducted this meta-analysis to evaluate the effectiveness of electroacupuncture in PONV after general anesthesia.
Material and Methods
INCLUSION AND EXCLUSION CRITERIA:
Two authors used the following inclusion criteria to assess the articles: The study adhered to the Patient, Intervention, Control, Outcome, and Study Design (PICOS) criteria. It involved patients undergoing surgery under general anesthesia. The intervention consisted of electroacupuncture in conjunction with perioperative conventional therapy. The control group consisted of patients receiving only perioperative conventional therapy. The primary outcome of the study focused on the incidence of PONV. The secondary outcomes included the incidence of postoperative nausea (PON) at 6 h, the incidence of postoperative vomiting (POV) at 6 h, and the postoperative antiemetic requirement. Finally, the study design had to be a randomized controlled clinical trial, with a study period between 2016 and 2023. The exclusion criteria were article categories of comments, case reports, crossover studies, letters, editorials, review articles, meta-analysis, and retrospective studies; studies of animal experiments; and studies that involved data that could not be extracted or that lacked sufficient data. If there was any disagreement about the eligibility of an included article, the disagreement was resolved through a discussion session or by the corresponding author.
SEARCH STRATEGY:
The study protocol was registered with PROSPERO, and the findings have been reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. We conducted a comprehensive search on PubMed, Web of Science, and China National Knowledge Infrastructure (CNKI) to identify relevant studies published from October 1, 2016, to 2023, focusing on the use of electroacupuncture for the prevention of PONV. The search strategy used for PubMed was as follows: (electroacupuncture) AND (postoperative nausea and vomiting OR PONV OR nausea and vomiting postoperative OR vomiting, postoperative OR postoperative emesis OR postoperative vomiting OR emesis, postoperative OR emeses, postoperative OR postoperative emeses OR postoperative nausea OR nausea, postoperative) AND (randomized controlled trial). The search strategy employed for Web of Science and CNKI was: (electroacupuncture) AND (postoperative nausea and vomiting) AND (randomized controlled trial). There were no restrictions based on language, sex, age, or type of surgery. No filters were applied during the search process.
STUDY SELECTION:
Two researchers, Zhenxu Han and Huan Yang, conducted independent reading and screening of the article, extracted the data, and cross-checked it for any discrepancies. The screening process involved initially reading the title and abstract of the article. After excluding irrelevant articles, the full text was examined to determine whether the inclusion criteria were met. Data were collected using a predefined table that included details such as the first author, country, year, sample size per group, age, patient sex, type of procedure, American Society of Anesthesiologists classification, experimental and control interventions, duration of intervention, outcome, and risk of bias.
RISK OF BIAS ASSESSMENT:
The methodological quality of the included studies was evaluated by 2 reviewers (Zhenxu Han and Huan Yang) according to the Cochrane Risk of Bias Assessment Tool provided by Cochrane Reviewer’s Handbook 5.3 [14]: (a) selection bias: whether the random allocation method was adopted, type of random allocation method, and type of allocation hiding method was adopted; (b) implementation bias: whether a blinding method was applied on implementers and participants; (c) measurement bias: whether the blinding method was implemented in the outcome evaluation; (d) follow-up bias: whether there was a loss to follow-up or withdrawal and type of analysis method used; (e) report bias: whether there was a selective reporting of results; and (f) other bias: whether there were other sources of bias.
STATISTICAL ANALYSIS:
Meta-analysis was conducted using RevMan 5.4.1 software, developed by the Cochrane Collaboration in Oxford, UK. For categorical variables, odds ratios (OR) with 95% confidence intervals (CI) were used. These variables included the incidence of PONV, incidence of PON at 6 h, incidence of POV at 6 h, and the requirement for postoperative antiemetic medication (including only events starting from 0). The χ2 test and
SUBGROUP ANALYSIS:
To examine the impact of anesthesia mode and the presence or absence of intraoperative antiemetics on the efficacy of electroacupuncture, subgroup analyses were conducted:
Results
STUDY SELECTION PROCESS:
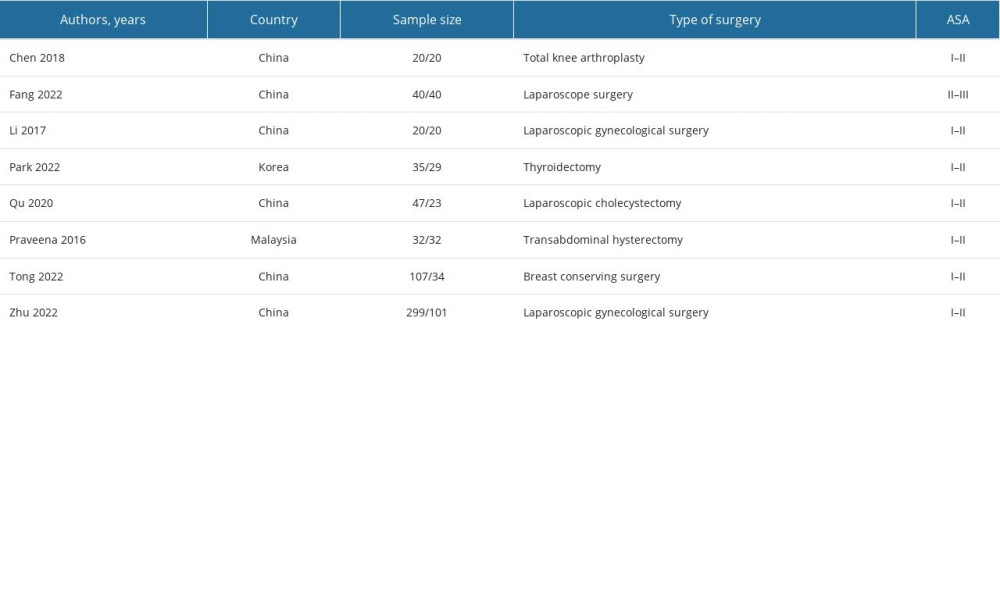
Initially, we retrieved a total of 68 articles, and after conducting a hierarchical screening process, 8 randomized controlled trials [15–22] were included. The selection process is illustrated in Figure 1.
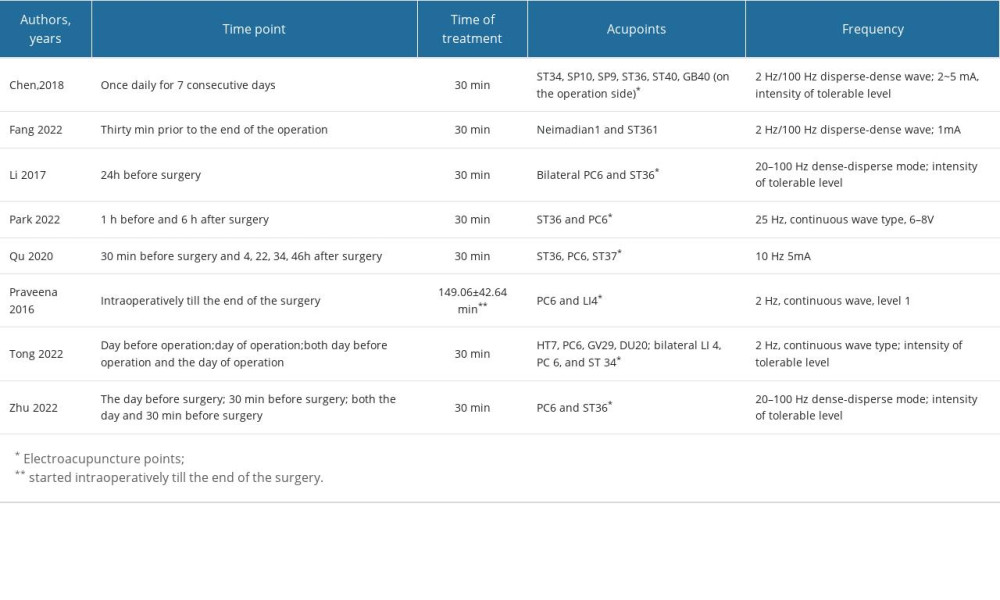
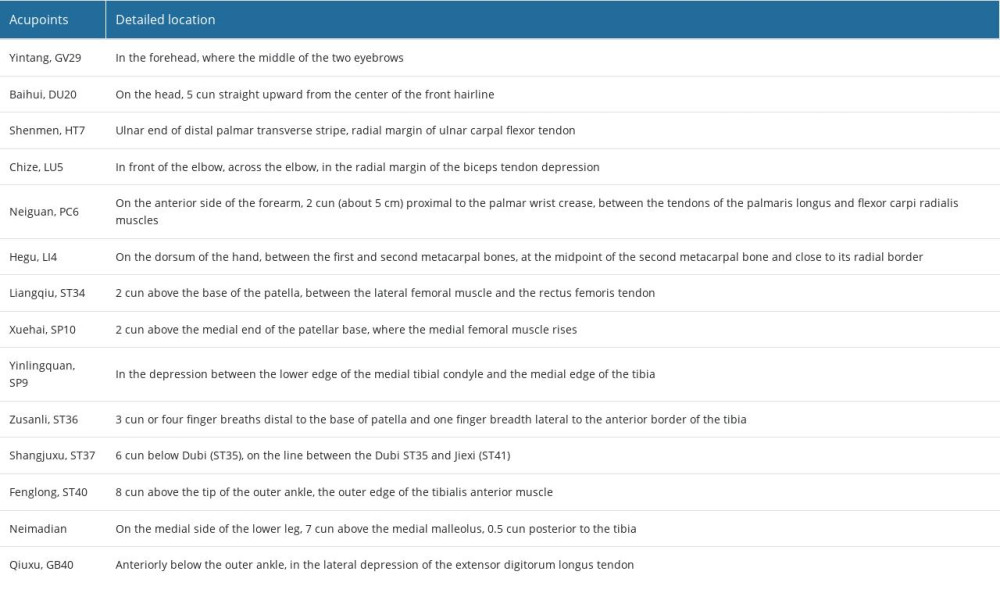
STUDY CHARACTERISTICS:
The characteristics of the included studies are presented in Tables 1–3. These 8 studies investigated the impact of electroacupuncture and standard care on PONV following general anesthesia. In all the studies, the interventions consisted of electroacupuncture along with routine perioperative care in the experimental group, while the control group received only routine perioperative care. Opioid analgesics were administered in all studies. Two studies employed additional antiemetic drugs during the surgery [18,19]. Six of the studies were conducted in China, 1 in Korea, and 1 in Malaysia. A total of 899 participants were included in these 8 studies, with 600 individuals receiving electroacupuncture intervention. In 5 studies [15,16,18–20], preoperative electroacupuncture interventions were used, while 3 studies [15,17,21] used intraoperative electroacupuncture interventions, and 3 studies [16,20,22] used postoperative electroacupuncture interventions. Two studies [16,18] used measurement tools to assess the severity of PON and POV, 1 study used the visual analog scale (VAS) score, and the other 2 studies used the 4-point Likert-type severity scale [18].
STUDY QUALITY:
Among the 8 studies included, 4 studies [15,18,19,21] provided descriptions of allocation concealment methods and used blinding techniques. All 8 studies reported comprehensive information on random sequence generation, and 4 studies [15,18,19,21] provided detailed explanations of allocation concealment methods. The risk of bias is presented in Figure 2.
INCIDENCE OF PONV:
A total of 4 randomized controlled trials [16,20,21,22] reported on the occurrence of PONV in 254 total patients, with 142 patients receiving electroacupuncture and 112 patients not receiving it. The study results revealed no significant difference in the incidence of PONV between the electroacupuncture group and the control group. (OR=0.31, 95% CI [0.06, 1.49], P=0.14, I2=82%; Figure 3).
INCIDENCE OF PON AT 6 H:
A total of 4 randomized controlled trials [15,17–19] reported the incidence of PON at 6 h in a total of 645 patients, with 458 patients receiving electroacupuncture and 187 patients not receiving it. The study results indicated that the electroacupuncture group exhibited significant improvement in reducing the incidence of PON at 6 h, compared with the control group (OR=0.43, 95% CI [0.27, 0.67], P=0.0002 I2=0; Figure 4).
INCIDENCE OF POV AT 6 H:
A total of 3 randomized controlled trials [15,18,19] reported the incidence of POV at 6 h in a total of 581 patients, with 426 patients receiving electroacupuncture and 155 patients not receiving it. The study findings demonstrate that electroacupuncture significantly reduced the incidence of POV within the first 6 h after surgery, compared with the control group (OR=0.38, 95% CI [0.23, 0.63], P=0.0001, I2=0%; Figure 5).
ANTIEMETIC REQUIREMENT:
A total of 3 randomized controlled trials [16,18,19] reported on the requirement for antiemetic medications in a total of 504 patients, with 354 patients receiving electroacupuncture and 150 patients not receiving it. Compared with the control group, the electroacupuncture group demonstrated a significant reduction in the postoperative requirement for antiemetic medications. (OR=0.44, 95% CI [0.25, 0.78], P=0.005, I2=61%; Figure 6).
SUBGROUP ANALYSIS:
Through subgroup analysis, it appeared that the administration of intraoperative antiemetics can influence the efficacy of electroacupuncture, particularly with regard to postoperative antiemetic needs. However, due to the limited number of included articles, the reliability of this result was not high, and further research is required. Regarding the impact of the type of anesthesia used during general anesthesia, based on the restricted number of articles included, we concluded that it had minimal or no effect on the effectiveness of electroacupuncture. Additionally, the waveform of electroacupuncture appeared to affect its therapeutic effectiveness in reducing the incidence of PONV and the requirement for postoperative antiemetic medications, while not significantly impacting other aspects (Figures 7–10).
SENSITIVITY ANALYSIS:
For the outcome of the incidence of PONV, the included studies were excluded on a study-by-study basis, and the heterogeneity in the results of the meta-analysis changed after the exclusion of the study Park et al [16]. The forest plot after exclusion of this study is shown in Figure 11. After analysis, it was found that the sex of the patients included in the study [16] was female, whereas the patients included in other studies [20–22] were of both sexes; therefore, the sex of the included patients may be the main reason for the study heterogeneity. However, due to the small number of articles included in the present study, the included articles could not be analyzed in subgroups according to patient sex.
Discussion
Clinical investigations have substantiated that the primary etiology of PONV involves the administration of inhalation anesthesia and opioid analgesics [23]. PONV represents one of the most distressing postoperative symptoms experienced by patients, and inadequate management of PONV leads to prolonged hospital stays and increased healthcare costs [5]. Current clinical strategies for preventing and treating PONV primarily rely on pharmaceutical interventions [24], yet the effectiveness of pharmacological agents in preventing and managing PONV remains unsatisfactory. Reports from certain studies indicate an efficacy rate of only 55.1% for drugs belonging to the ondansetron class [25]. Recent investigations have demonstrated the pivotal role of acupuncture in managing postoperative pain, yielding notable reductions in postoperative pain levels and opioid consumption, thereby mitigating the occurrence of opioid-induced adverse effects, such as nausea and vomiting [26,27]. Both animal and human studies have revealed that preoperative electroacupuncture facilitates an elevation in enkephalin and β-endorphin levels, thereby conferring beneficial analgesic effects [28–30]. Furthermore, additional research has elucidated how acupuncture modulates serotonin and dopamine levels, which are targeted by common antiemetic drugs [31,32], potentially contributing to the suppressive impact of acupuncture on PONV. In comparison with antiemetic drugs, acupuncture offers distinct advantages, including minimal physiological perturbation and a lower incidence of adverse effects [33]. Manual acupuncture, involving manual manipulation of needles to elicit the de qi sensation, represents a therapeutic modality. Electroacupuncture, derived from manual acupuncture, boasts the ability to quantitatively and repetitively administer stimulation, facilitating objective control of the degree of stimuli for quantitative analysis [34]. Furthermore, an investigation examining resting-state fMRI findings revealed distinct enduring effects of manual acupuncture and electroacupuncture on the Zusanli (ST36) acupoint, with electroacupuncture demonstrating a broader range of activation [35]. Therefore, the aim of the present study was to evaluate and investigate the clinical efficacy of electroacupuncture in mitigating PONV after general anesthesia, with the intention of making a valuable contribution to the existing literature.
This meta-analysis indicated that there was no significant difference in reducing the incidence of PONV between the electroacupuncture group and the postoperative conventional care group. However, the study findings showed statistically significant differences between the electroacupuncture group and the control group in preventing PON and POV at 6 h, as well as reducing the usage of antiemetic medication after surgery. One study included in the analysis reported adverse events. Therefore, electroacupuncture is considered a safe adjunctive therapy for preventing PONV following general anesthesia.
However, our study has several limitations: (1) The number of randomized controlled trials included in this study and the sample size of participants were insufficient to draw specific conclusions. We recommend conducting a multicenter randomized controlled trial with a larger sample to mitigate bias. (2) Additionally, there are certain issues with the reporting of efficacy indicators for the prevention of PONV using electroacupuncture. For instance, variations exist in the timing of PONV observation across different articles, thereby making it challenging to incorporate certain results into this systematic study and provide a higher level of evidence for clinical trials. (3) Out of the 8 studies analyzed, only 2 studies, involving 128 total patients, were conducted in other countries, with the majority of the study population being from China. This highlights a lack of similar large-scale international multicenter clinical trials. (4) During the sensitivity analysis of the PONV indicator in this study, sex was identified as a significant factor contributing to heterogeneity and influencing the results. However, due to limited relevant studies, subgroup analysis could not be performed. (5) The potential cofounders influencing the efficacy of electroacupuncture were not thoroughly investigated, and variables such as the type of procedure and its duration were not further explored.
Conclusions
In summary, we conducted a comprehensive statistical analysis of outcome data regarding the use of electroacupuncture for the prevention and treatment of PONV after general anesthesia. The pooled data from a randomized controlled trial indicate that electroacupuncture significantly reduces the incidence of PON and POV at 6 h after surgery, as well as the antiemetic requirement. However, there is no significant difference between the electroacupuncture group and the control group in terms of the incidence of PONV. Regarding safety, electroacupuncture carries a minimal risk of pain and itching at the needle insertion site. To provide more precise guidance for clinical practice, it is necessary to conduct longer-duration and larger-scale randomized controlled trials to evaluate the effectiveness and safety of electroacupuncture in the prevention and treatment of PONV.
Figures
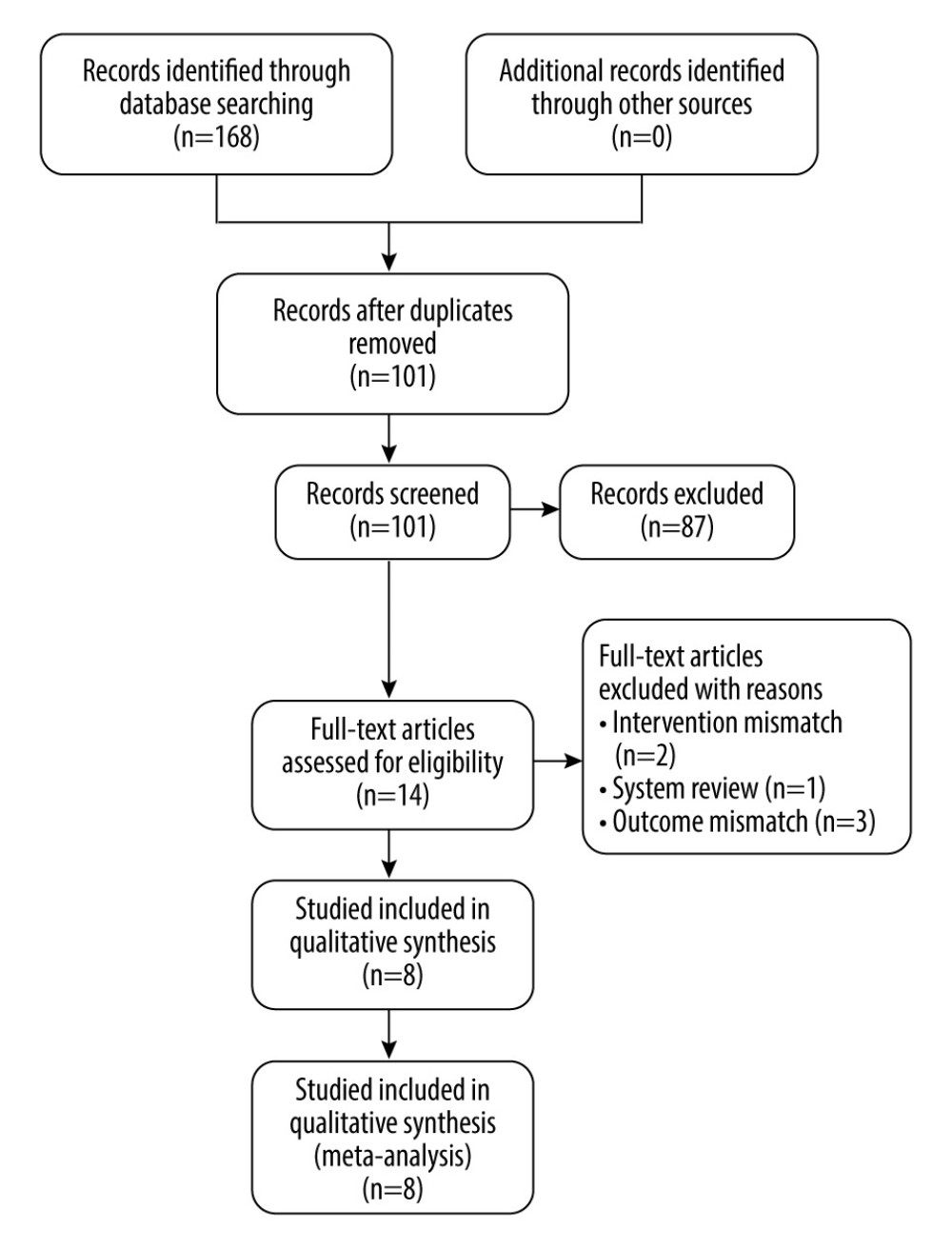 Figure 1. PRISMA flowchart.
Figure 1. PRISMA flowchart. 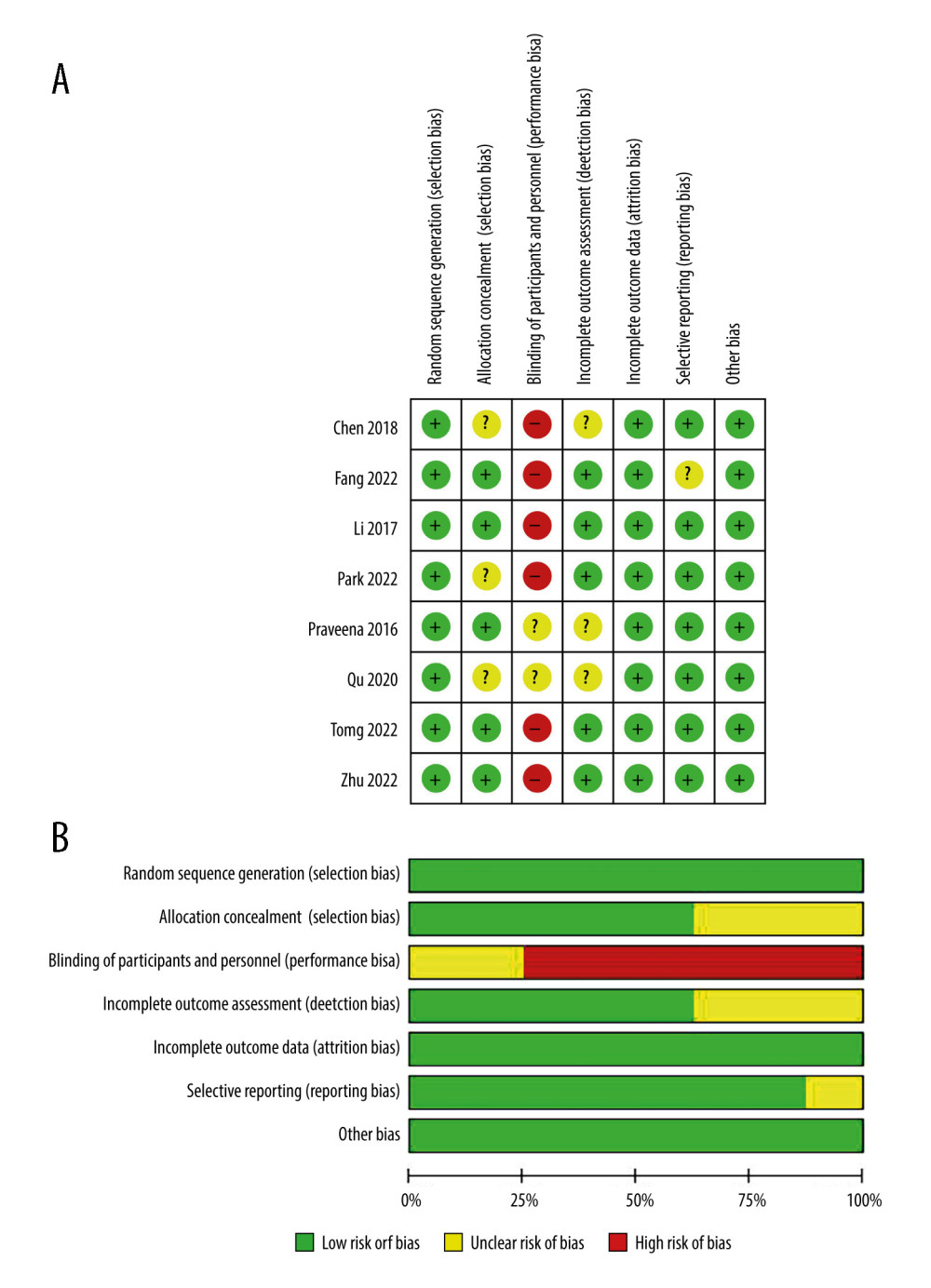 Figure 2. (A, B) Quality assessment of included studies.
Figure 2. (A, B) Quality assessment of included studies. 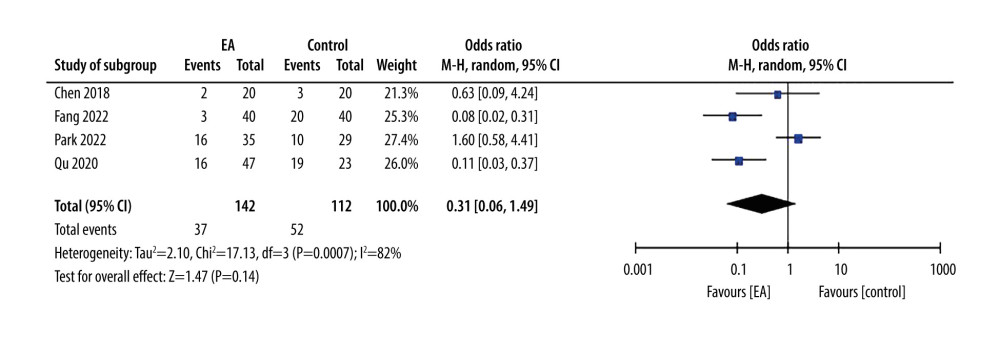 Figure 3. Forest plot showing incidence of postoperative nausea and vomiting.
Figure 3. Forest plot showing incidence of postoperative nausea and vomiting. 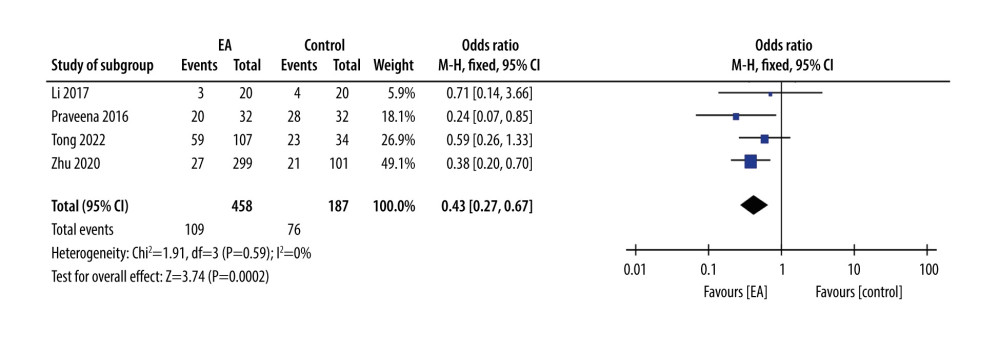 Figure 4. Forest plot showing incidence of postoperative nausea and at 6 h.
Figure 4. Forest plot showing incidence of postoperative nausea and at 6 h. 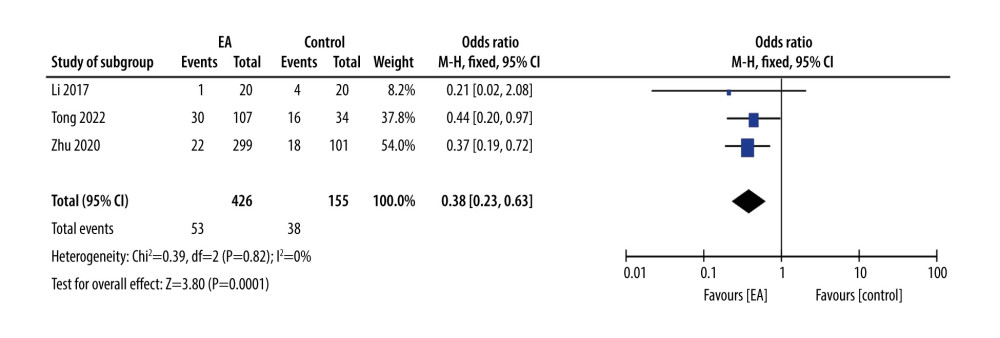 Figure 5. Forest plot showing incidence of postoperative vomiting at 6 h.
Figure 5. Forest plot showing incidence of postoperative vomiting at 6 h. 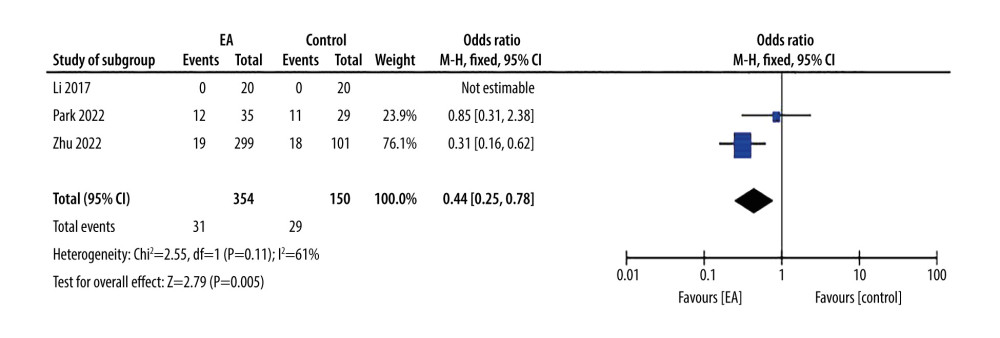 Figure 6. Forest plot showing antiemetic requirement.
Figure 6. Forest plot showing antiemetic requirement. 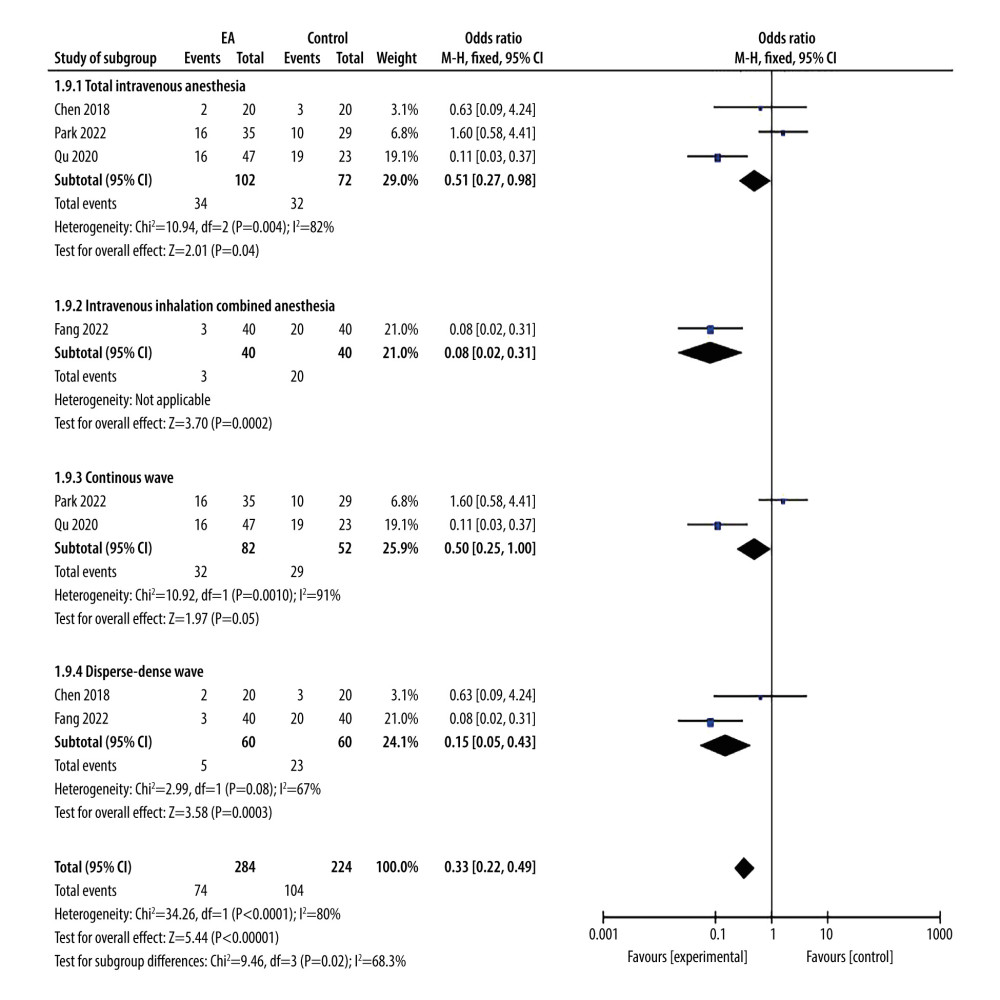 Figure 7. Forest plot showing incidence of postoperative nausea and vomiting. Total intravenous anesthesia vs combined intravenous-inhalation anesthesia. Continuous wave vs disperse-dense wave.
Figure 7. Forest plot showing incidence of postoperative nausea and vomiting. Total intravenous anesthesia vs combined intravenous-inhalation anesthesia. Continuous wave vs disperse-dense wave. 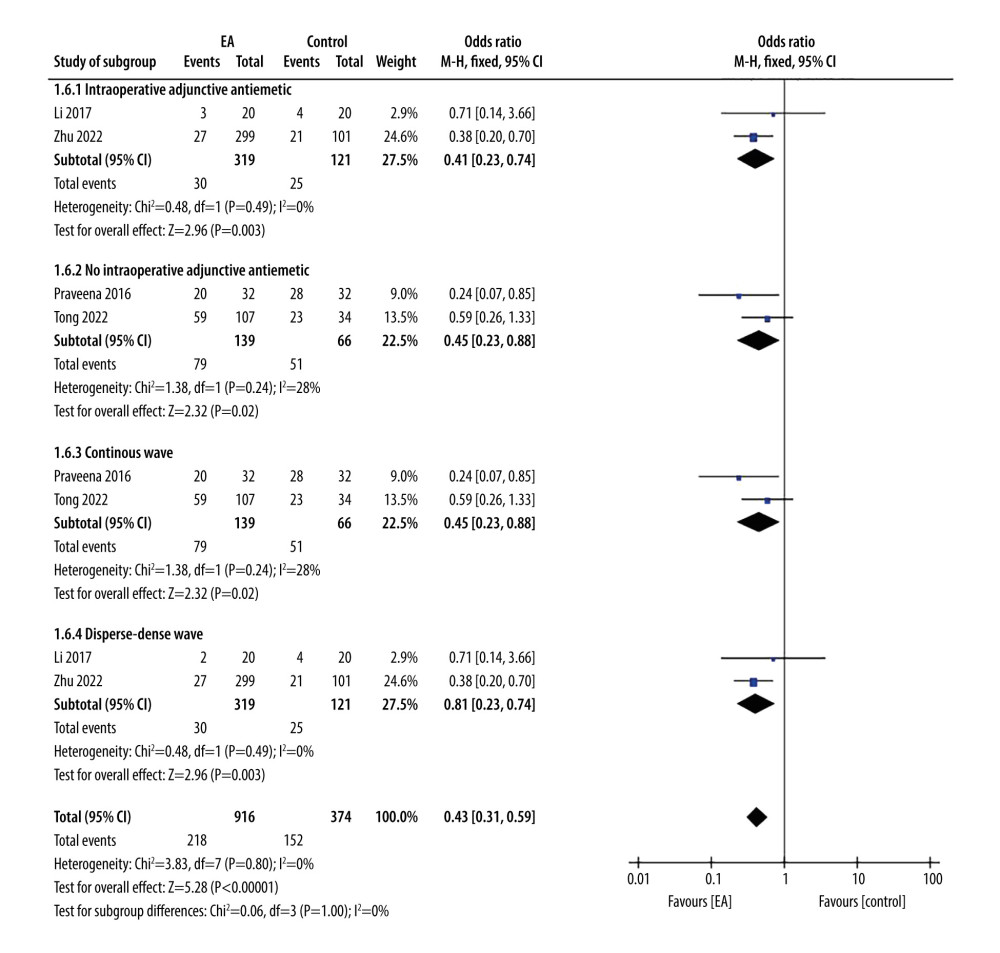 Figure 8. Forest plot showing postoperative nausea at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 8. Forest plot showing postoperative nausea at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave. 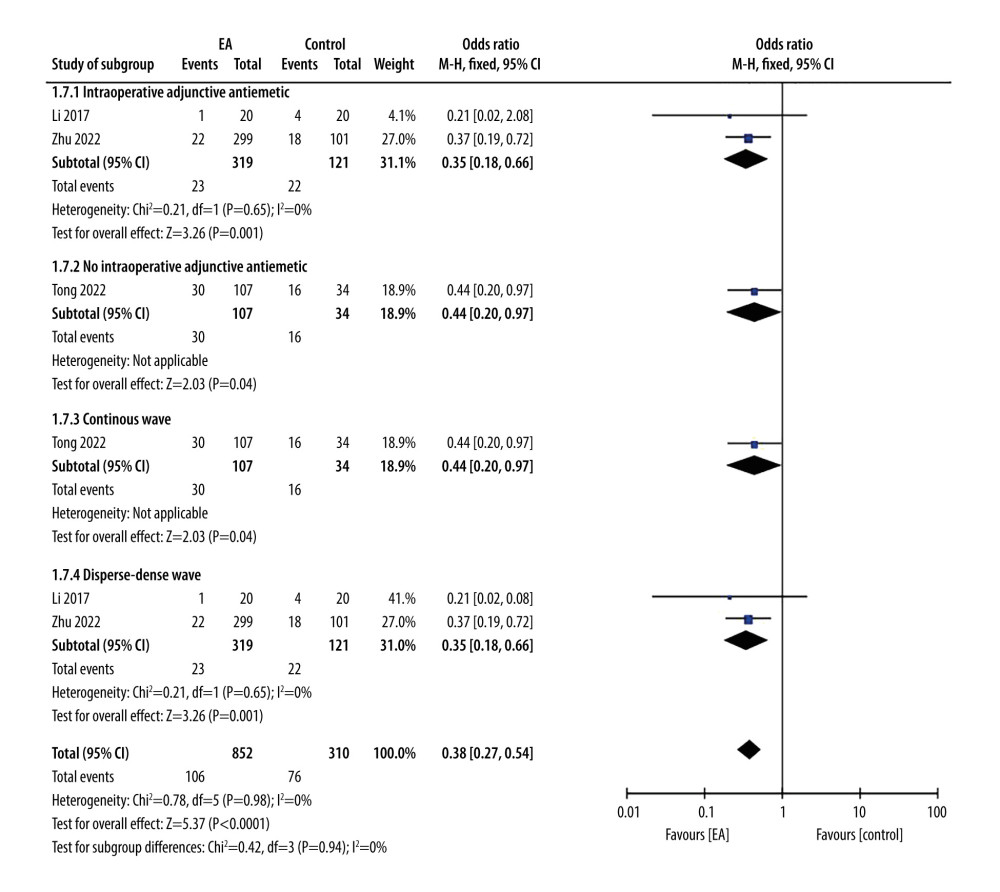 Figure 9. Forest plot showing postoperative vomiting at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 9. Forest plot showing postoperative vomiting at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave. 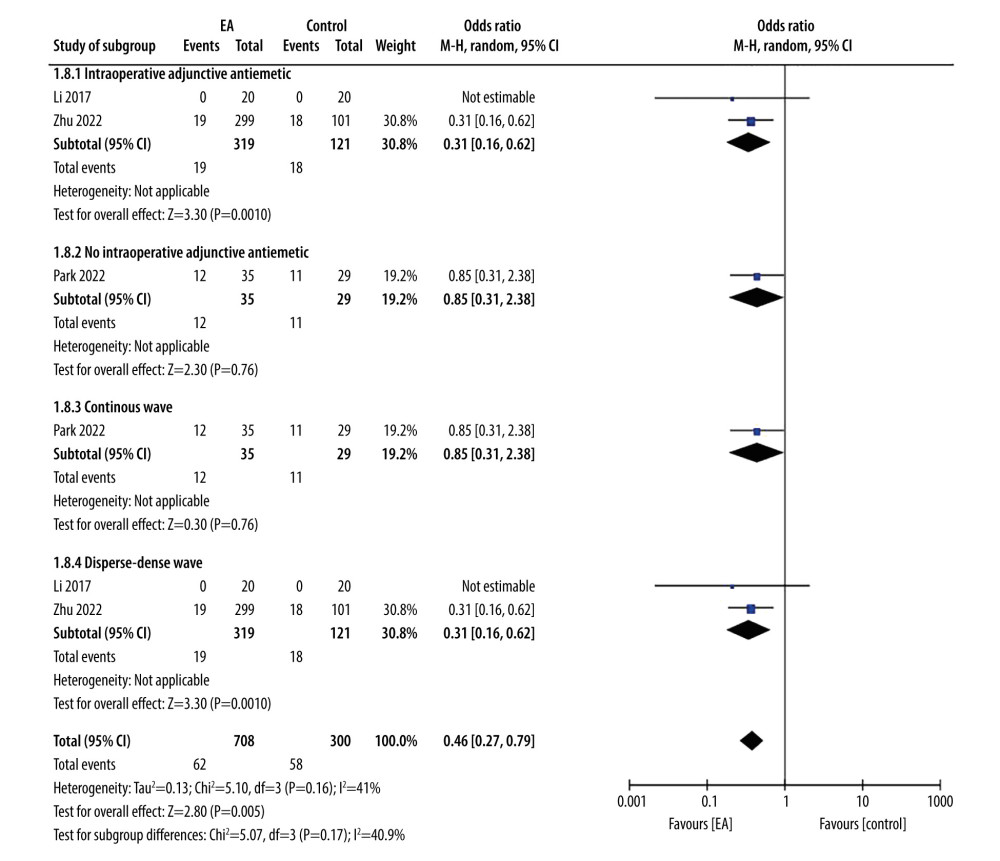 Figure 10. Forest plot showing antiemetic requirement. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 10. Forest plot showing antiemetic requirement. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave. 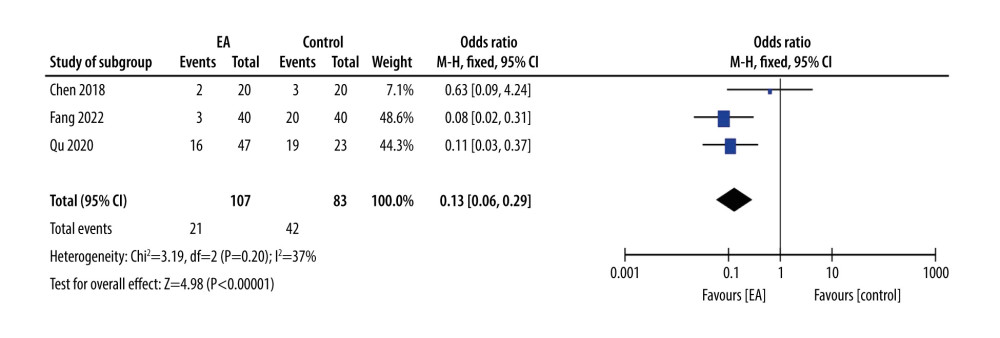 Figure 11. Forest plot showing incidence of postoperative nausea and vomiting after exclusion.
Figure 11. Forest plot showing incidence of postoperative nausea and vomiting after exclusion. References
1. Gan TJ, Belani KG, Bergese S, Fourth consensus guidelines for the management of postoperative nausea and vomiting: Anesth Analg, 2020; 131(2); 411-48 [Erratum in: Anesth Analg. 2020;131(5):e241]
2. Rajan N, Joshi GP, Management of postoperative nausea and vomiting in adults: Current controversies: Curr Opin Anaesthesiol, 2021; 34(6); 695-702
3. Horn CC, Wallisch WJ, Homanics GE, Williams JP, Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting: Eur J Pharmacol, 2014; 722; 55-66
4. Kovac AL, Postoperative nausea and vomiting in pediatric patients: Paediatr Drugs, 2021; 23(1); 11-37
5. Naz R, Özyazıcıoğlu N, Kaya M, Effects of menthol gum chewing on postoperative nausea, vomiting, and length of hospital stay in children undergoing appendectomy: A randomized controlled trıal: J Pediatr Nurs, 2023; 72; 92-98
6. Schwartz J, Gan TJ, Management of postoperative nausea and vomiting in the context of an Enhanced Recovery after Surgery program: Best Pract Res Clin Anaesthesiol, 2020; 34(4); 687-700
7. Rüsch D, Eberhart LH, Wallenborn J, Kranke P, Nausea and vomiting after surgery under general anesthesia: An evidence-based review concerning risk assessment, prevention, and treatment: Dtsch Arztebl Int, 2010; 107(42); 733-41
8. Lee A, Chan SK, Fan LT, Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting: Cochrane Database Syst Rev, 2015; 2015(11); CD003281
9. Chen J, Tu Q, Miao S, Transcutaneous electrical acupoint stimulation for preventing postoperative nausea and vomiting after general anesthesia: A meta-analysis of randomized controlled trials: Int J Surg, 2020; 73; 57-64
10. Shin HC, Kim JS, Lee SK, The effect of acupuncture on postoperative nausea and vomiting after pediatric tonsillectomy: A meta-analysis and systematic review: Laryngoscope, 2016; 126(8); 1761-67
11. Cheong KB, Zhang JP, Huang Y, Zhang ZJ, The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis: PLoS One, 2013; 8(12); e82474
12. Cheng RD, Tu WZ, Jiang SH, Progress in the study of the role of purines and their receptors in the analgesic effect of electroacupuncture: Chinese Journal of Pain Medicine, 2012; 18(01); 53-56
13. Panic N, Leoncini E, de Belvis G, Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses: PLoS One, 2013; 8(12); e83138
14. Higgins JPT, Altman DG, Sterne JAC, Chapter 8: Assessing risk of bias in included studies: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011), 2011, The Cochrane Collaboration Available from URL: www.cochranehandbook.org
15. Tong QY, Liu R, Gao Y, Effect of electroacupuncture based on ERAS for preoperative anxiety in breast cancer surgery: A single-center, randomized, controlled trial: Clin Breast Cancer, 2022; 22(7); 724-36
16. Park MS, Park WS, Nam D, Efficacy of electroacupuncture in preventing nausea and vomiting after thyroidectomy: A prospective randomized controlled trial: Asian J Surg, 2022 [Online ahead of print]
17. Praveena Seevaunnamtum S, Bhojwani K, Abdullah N, Intraoperative electroacupuncture reduces postoperative pain, analgesic requirement and prevents postoperative nausea and vomiting in gynaecological surgery: A randomised controlled trial: Anesth Pain Med, 2016; 6(6); e40106
18. Zhu J, Li S, Wu W, Preoperative electroacupuncture for postoperative nausea and vomiting in laparoscopic gynecological surgery: A randomized controlled trial: Acupunct Med, 2022; 40(5); 415-24
19. Li S, Zheng M, Wu W, Effects of electroacupuncture administered 24 hours prior to surgery on postoperative nausea and vomiting and pain in patients undergoing gynecologic laparoscopic surgery: A feasibility study: Explore (NY), 2017; 13(5); 313-18
20. Qu LZ, Zhao HC, Shen HXElectroacupuncture of both single- and multi-acupoints promotes recovery of gastrointestinal function in laparoscopic cholecystectomy patients: Zhen Ci Yan Jiu, 2020; 45(2); 136-40 [in Chinese]
21. Fang R, Zhou MT, Zhang CJ, Fu JHEffect of electroacupuncture on laparoscope postoperative shivering in patients undergoing general anesthesia: Zhongguo Zhen Jiu, 2022; 42(3); 257-60 [in Chinese]
22. Chen D, Sheng D, Xu JLElectroacupuncture intervention reduces post-surgical pain of patients undergoing total knee arthroplasty: Zhen Ci Yan Jiu, 2018; 43(10); 616-21 [in Chinese]
23. Schlesinger T, Weibel S, Kranke P, Postoperative/postdischarge nausea and vomiting: Evidence-based prevention and treatment: Curr Opin Anaesthesiol, 2023; 36(1); 109-16
24. Tateosian VS, Champagne K, Gan TJ, What is new in the battle against postoperative nausea and vomiting?: Best Pract Res Clin Anaesthesiol, 2018; 32(2); 137-48
25. Gralla R, Lichinitser M, Van Der Vegt S, Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: Results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron: Ann Oncol, 2003; 14(10); 1570-77
26. Shah S, Godhardt L, Spofford C, Acupuncture and postoperative pain reduction: Curr Pain Headache Rep, 2022; 26(6); 453-58
27. Usichenko TI, Henkel BJ, Klausenitz C, Effectiveness of acupuncture for pain control after cesarean delivery: A randomized clinical trial: JAMA Netw Open, 2022; 5(2); e220517 Erratum in: JAMA Netw Open. 2022;5(4):e229622
28. Jiang Y, He X, Yin XAnti-inflammatory and synovial-opioid system effects of electroacupuncture intervention on chronic pain in arthritic rats: Zhongguo Zhen Jiu, 2015; 35(9); 917-21 [in Chinese]
29. Wang Y, Gehringer R, Mousa SA, CXCL10 controls inflammatory pain via opioid peptide-containing macrophages in electroacupuncture: PLoS One, 2014; 9(4); e94696 [Erratum in: PLoS One. 2014;9(8):e105841]
30. Sun Y, Gan TJ, Dubose JW, Habib AS, Acupuncture and related techniques for postoperative pain: A systematic review of randomized controlled trials: Br J Anaesth, 2008; 101(2); 151-60
31. Hsieh YL, Hong CZ, Liu SY, Acupuncture at distant myofascial trigger spots enhances endogenous opioids in rabbits: A possible mechanism for managing myofascial pain: Acupunct Med, 2016; 34(4); 302-9
32. Zhang X, Jin HF, Fan YH, Effects and mechanisms of transcutaneous electroacupuncture on chemotherapy-induced nausea and vomiting: Evid Based Complement Alternat Med, 2014; 2014; 860631
33. Shah S, Godhardt L, Spofford C, Acupuncture and postoperative pain reduction: Curr Pain Headache Rep, 2022; 26(6); 453-58
34. Fu HW, Yan LJ, Liu YY, Research on the effects of the different electroacupuncture parameters on analgesia effect an overview: Journal of Shanghai Journal of Acupuncture and Moxibustion, 2018; 37(11); 1331-35
35. Tan JH, Wang YY, Long XJ, fMRI investigation of the sustained-effect of manual acupuncture and electro-acupuncture: Journal of Hunan University Natural Sciences, 2013; 40(7); 64-68
Figures
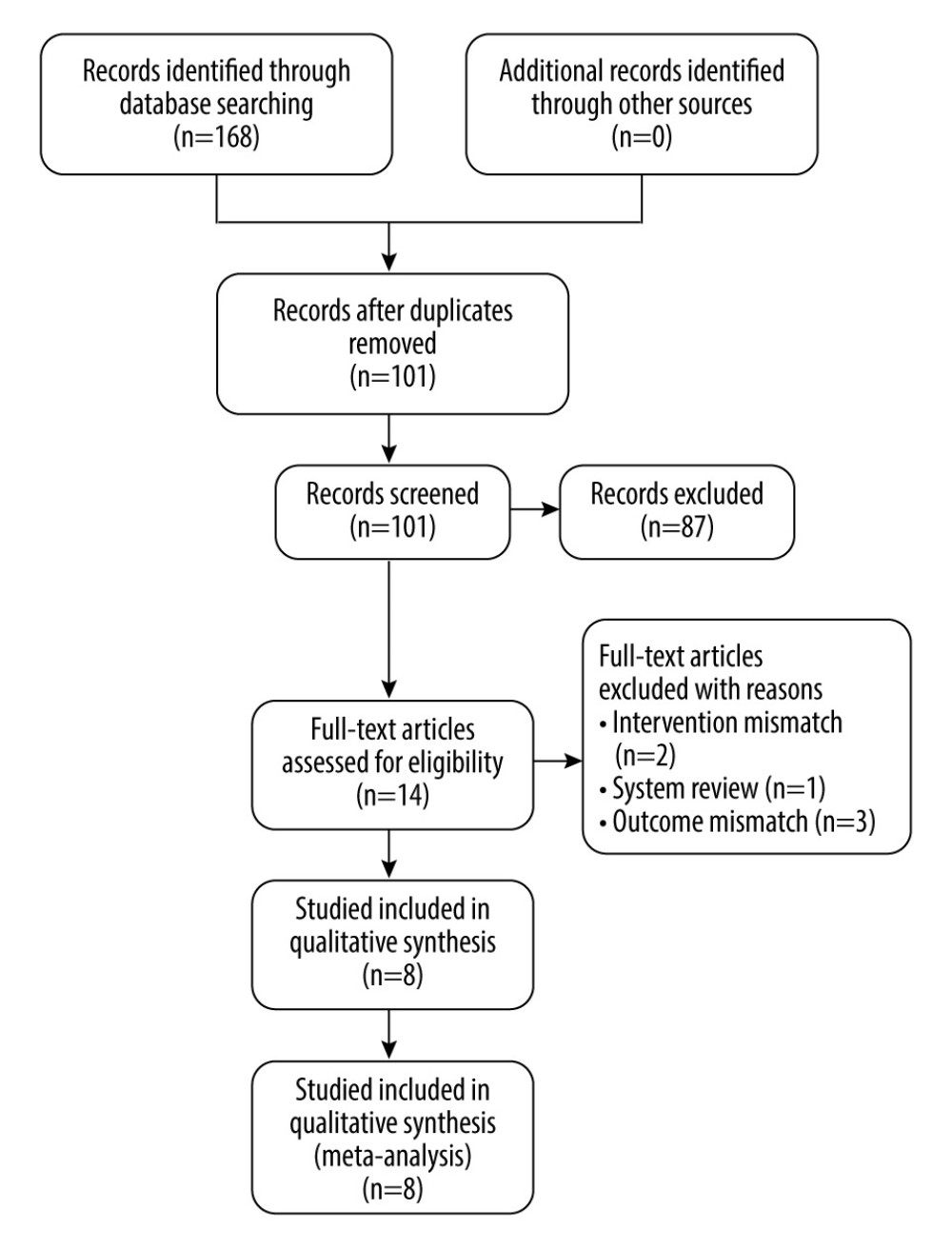 Figure 1. PRISMA flowchart.
Figure 1. PRISMA flowchart.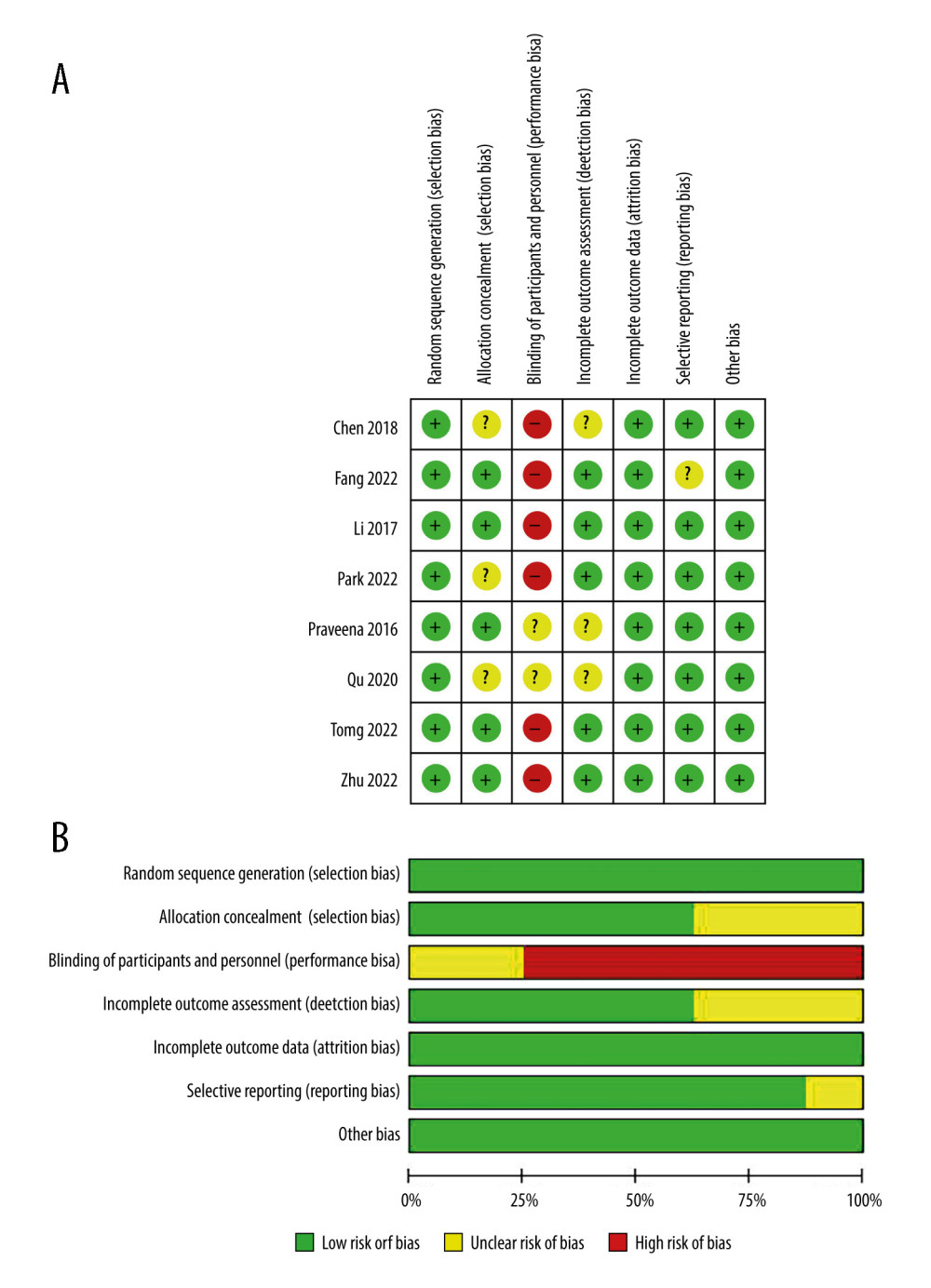 Figure 2. (A, B) Quality assessment of included studies.
Figure 2. (A, B) Quality assessment of included studies.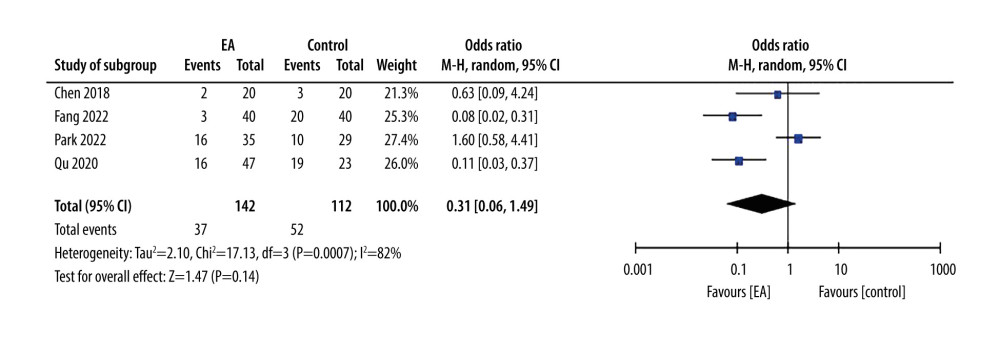 Figure 3. Forest plot showing incidence of postoperative nausea and vomiting.
Figure 3. Forest plot showing incidence of postoperative nausea and vomiting.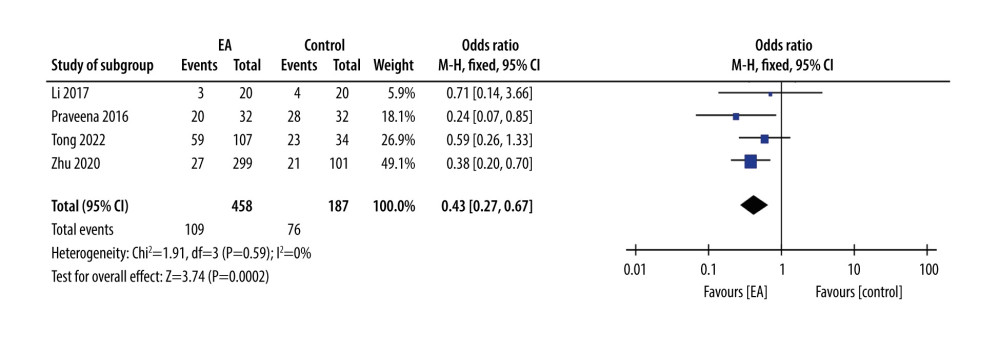 Figure 4. Forest plot showing incidence of postoperative nausea and at 6 h.
Figure 4. Forest plot showing incidence of postoperative nausea and at 6 h.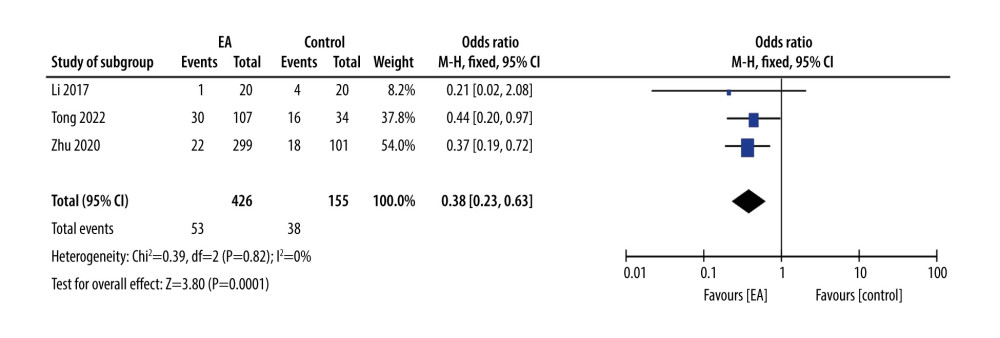 Figure 5. Forest plot showing incidence of postoperative vomiting at 6 h.
Figure 5. Forest plot showing incidence of postoperative vomiting at 6 h.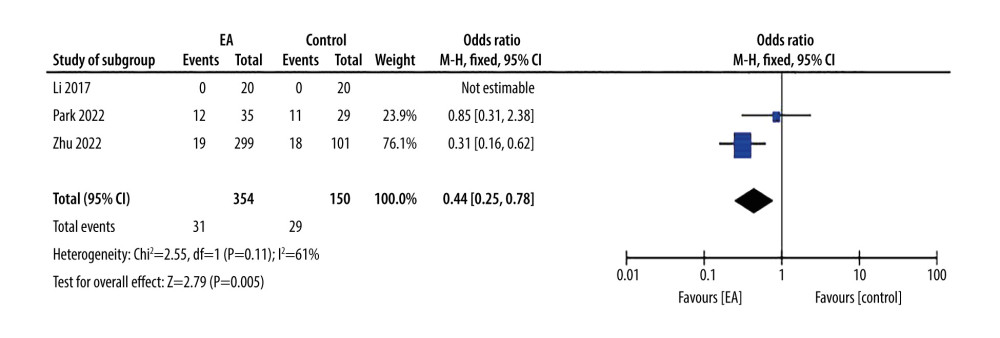 Figure 6. Forest plot showing antiemetic requirement.
Figure 6. Forest plot showing antiemetic requirement.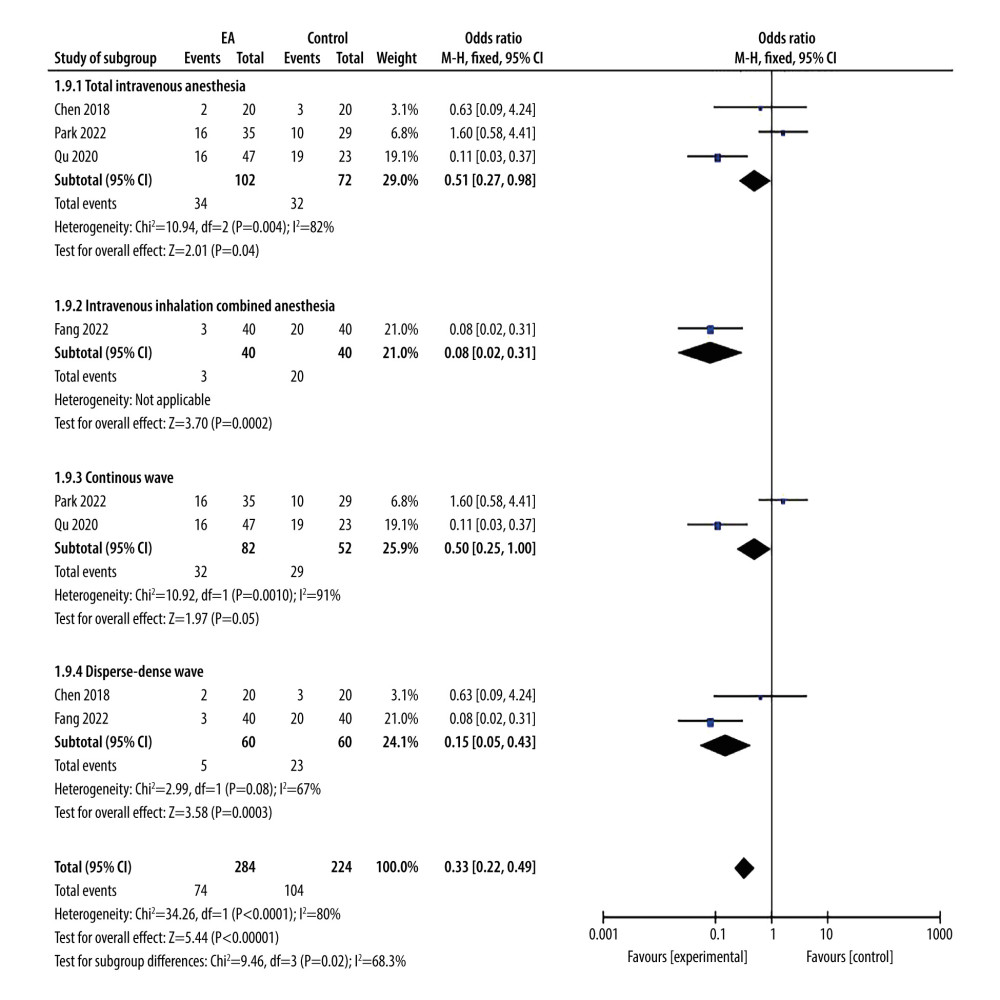 Figure 7. Forest plot showing incidence of postoperative nausea and vomiting. Total intravenous anesthesia vs combined intravenous-inhalation anesthesia. Continuous wave vs disperse-dense wave.
Figure 7. Forest plot showing incidence of postoperative nausea and vomiting. Total intravenous anesthesia vs combined intravenous-inhalation anesthesia. Continuous wave vs disperse-dense wave.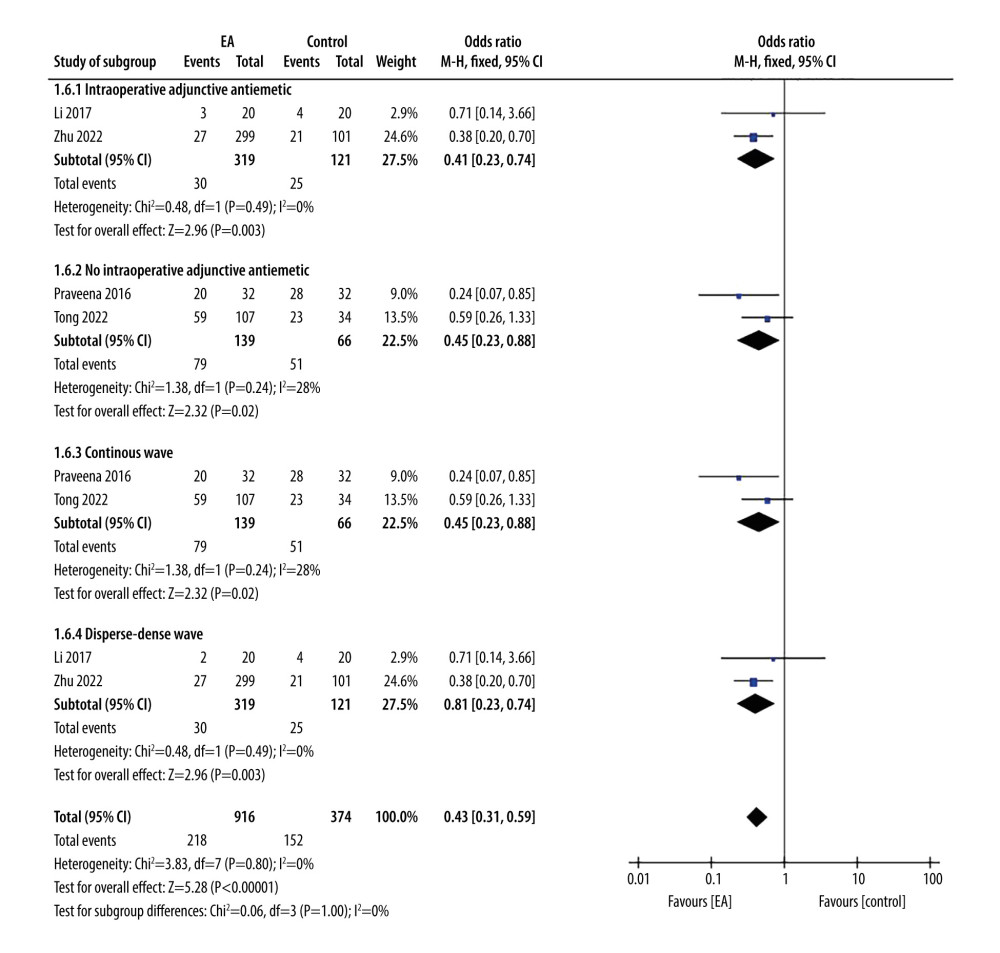 Figure 8. Forest plot showing postoperative nausea at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 8. Forest plot showing postoperative nausea at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.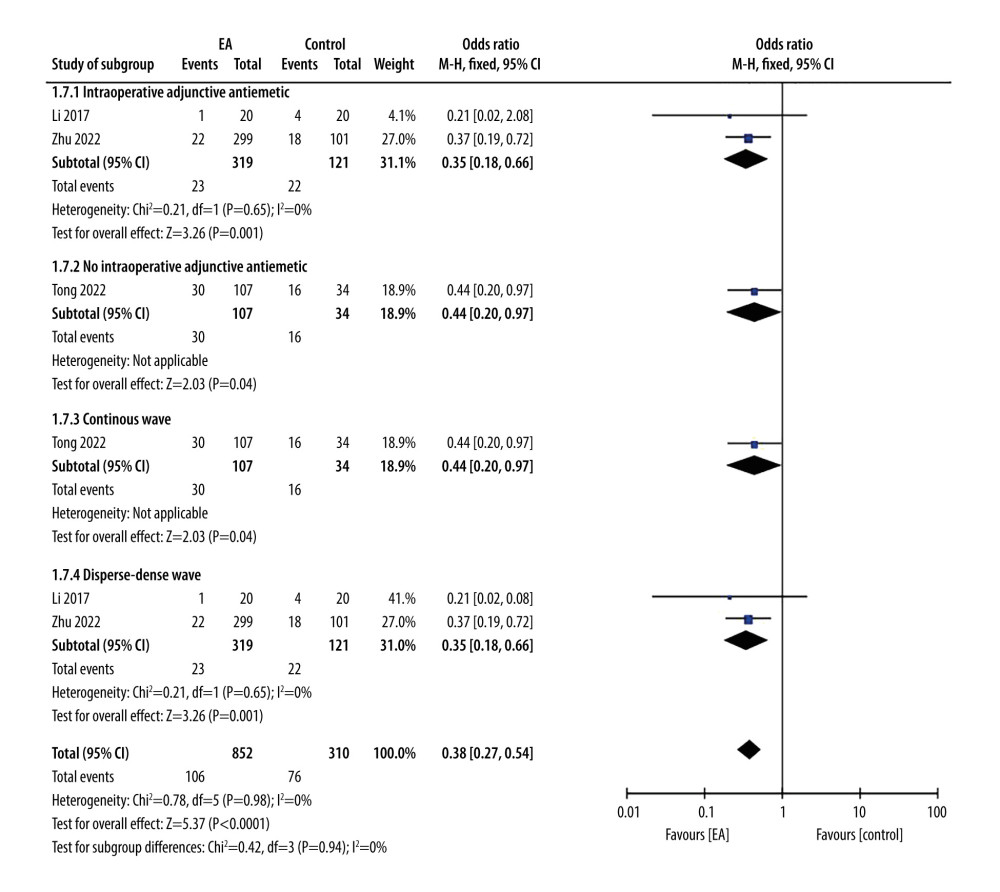 Figure 9. Forest plot showing postoperative vomiting at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 9. Forest plot showing postoperative vomiting at 0–6 h. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.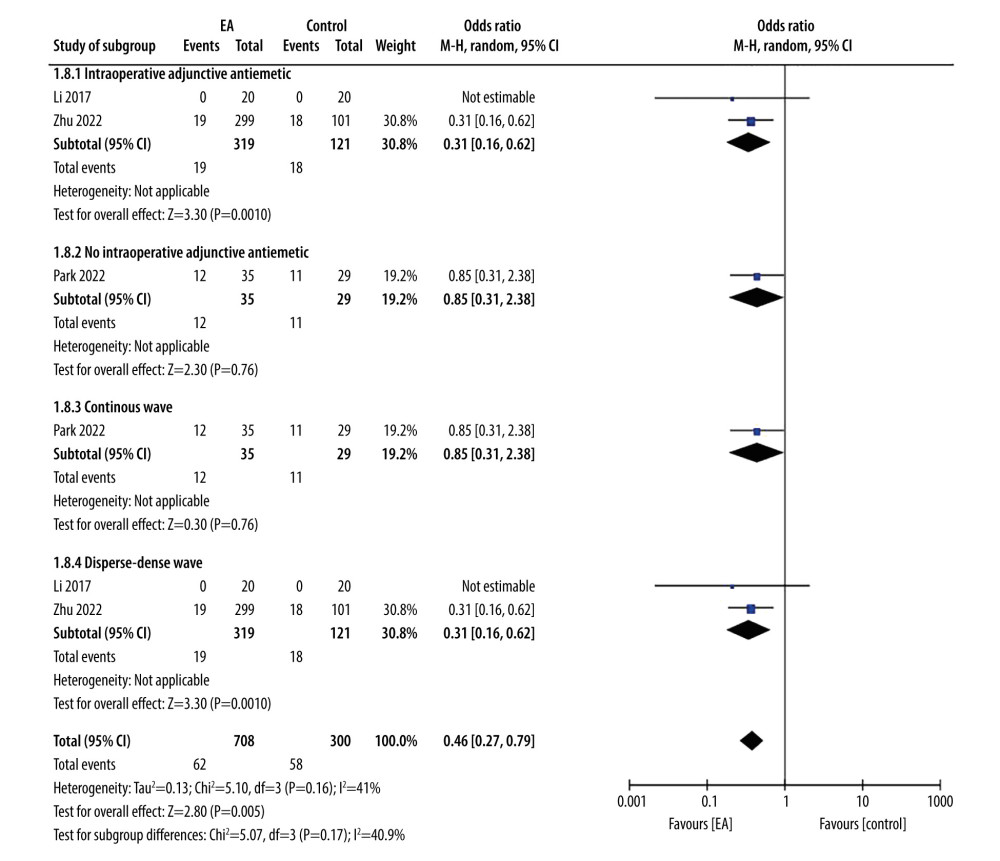 Figure 10. Forest plot showing antiemetic requirement. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.
Figure 10. Forest plot showing antiemetic requirement. Intraoperative adjunctive antiemetic vs no intraoperative adjunctive antiemetic. Continuous wave vs disperse-dense wave.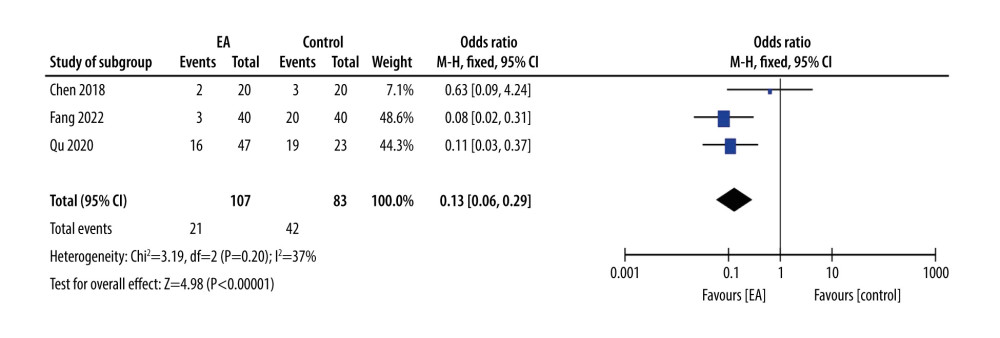 Figure 11. Forest plot showing incidence of postoperative nausea and vomiting after exclusion.
Figure 11. Forest plot showing incidence of postoperative nausea and vomiting after exclusion. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952