17 September 2023: Clinical Research
Impact of Remimazolam versus Sevoflurane Anesthesia on Cerebral Oxygenation and Intracranial Pressure during Gynecological Laparoscopy with Mild Hypercapnia
Chun Gon ParkDOI: 10.12659/MSM.941315
Med Sci Monit 2023; 29:e941315
Abstract
BACKGROUND: Remimazolam has the advantage of better hemodynamic stability compared with other anesthetics. We compared the effects of remimazolam and sevoflurane on cerebral oxygenation, intracranial pressure, and intraoperative hemodynamic parameters during mild hypercapnia in patients undergoing laparoscopy in the Trendelenburg position.
MATERIAL AND METHODS: Sixty-two patients (20-65 years old) scheduled for gynecological laparoscopy were randomly allocated to either the remimazolam (n=31) or sevoflurane (n=31) group. Respiratory and hemodynamic parameters and regional cerebral oxygen saturation (rSO₂) were recorded. Intracranial pressure was measured using the optic nerve sheath diameter (ONSD).
RESULTS: The change over time in rSO₂ did not differ between groups (P=0.056). The change in ONSD over time showed a significant intergroup difference (P=0.002). ONSD significantly changed over time (P=0.034) in the sevoflurane group but not in the remimazolam group (P=0.115). The changes in mean arterial pressure and heart rate over time showed significant intergroup differences (P=0.045 and 0.031, respectively). The length of stay and the use of rescue antiemetics and analgesics in the postanesthetic care unit were significantly lower in the remimazolam group than in the sevoflurane group (P=0.023, 0.038, and 0.018, respectively).
CONCLUSIONS: Remimazolam can provide a favorable hemodynamic profile and attenuate the increase in ONSD during gynecological laparoscopy compared with sevoflurane anesthesia during lung-protective ventilation with mild hypercapnia. Remimazolam can provide faster and better postoperative recovery than sevoflurane anesthesia.
Keywords: Anesthesia, Hemodynamics, Intracranial Pressure, Laparoscopy, Humans, young adult, Adult, Middle Aged, Aged, sevoflurane, Hypercapnia, Lung
Background
With the advantages of being minimally invasive and allowing for rapid recovery, laparoscopy has been progressively performed for most intra-abdominal surgeries rather than laparotomy. However, carbon dioxide (CO2) pneumoperitoneum and Trendelenburg position for laparoscopic surgery can increase intracranial pressure (ICP) and cause temporary cognitive impairment [1]. According to a previous clinical study on laparoscopic surgery, the change in ICP measured using the optic nerve sheath diameter (ONSD), transcranial Doppler-based pulsatility index, and diastolic component of the transcranial Doppler-based cerebral blood flow velocity was shown to significantly increase during pneumoperitoneum in the Trendelenburg position [2]. In addition, changes in hemodynamic parameters and blood CO2 concentration during laparoscopic surgery result in changes in the cerebral perfusion pressure and regional cerebral oxygen saturation (rSO2) [3].
Hypercapnia commonly occurs during laparoscopic surgery because of intra-abdominal CO2 insufflation and changes in respiratory mechanics [4]. Rather than overcorrection of hypercapnia, a previous study showed that permissive hypercapnia, a part of lung-protective ventilation, improves respiratory function after laparoscopic surgery [4]. Although hypercapnia is well known to induce cerebral vasodilation and increase ICP, previous studies that used propofol/remifentanil total intravenous anesthesia have shown that mild hypercapnia does not exacerbate the increase in ONSD during pneumoperitoneum in the Trendelenburg position but rather improves rSO2 compared with normocapnia [5].
In a previous animal study, sevoflurane dilated the pial vessels in rats in a dose-dependent manner and enhanced cerebrovascular dilation induced by hypercapnia [6]. In a clinical study of brain tumors, subdural ICP and arteriovenous oxygen differences were significantly higher in the inhalation anesthesia group than in the propofol anesthesia group [7]. In addition, CO2 reactivity is significantly higher under inhalation anesthesia than under propofol anesthesia [7]. Inhalational anesthetics have the risk of increasing ICP, and intravenous anesthetics are preferred for controlling ICP. However, propofol can significantly inhibit blood circulation, and midazolam, a type of benzodiazepine, has the disadvantage of causing delayed awakening [8]. Remimazolam, a recently introduced benzodiazepine, is a “soft” drug with a rapid onset/offset, no active metabolite formation, and hemodynamic stability [9].
We expected that the use of remimazolam for the induction and maintenance of anesthesia during lung-protective ventilation with permissive hypercapnia would alleviate the hemodynamic instability and increase ICP that can occur during pneumoperitoneum in the Trendelenburg position for laparoscopic surgery during sevoflurane anesthesia. Therefore, we hypothesized that remimazolam would have a beneficial effect on cerebral physiology during laparoscopic surgery for mild hypercapnia in the Trendelenburg position. We compared the effects of remimazolam and sevoflurane anesthesia on cerebral oxygenation (using rSO2), ICP (using ONSD), and intraoperative hemodynamic parameters during lung-protective ventilation with mild hypercapnia in patients undergoing gynecological laparoscopy in the Trendelenburg position.
Material and Methods
The Ethics Committee of Gachon University Gil Hospital approved this study (GCIRB2021-471), which was registered with the Clinical Research Information Service (KCT0006900; cris.nih.go.kr) before patient recruitment. All eligible participants provided written informed consent prior to participating in the study, which was conducted in accordance with the Helsinki Declarartion-2013. This prospective study included 62 patients with an American Society of Anesthesiologists physical status of 1 or 2 and who were 20–65 years of age and scheduled for gynecological laparoscopy. We excluded patients with a body mass index ≥30 kg/m2, uncontrolled hypertension, uncontrolled diabetes mellitus, active pulmonary disorder, cerebrovascular disease, glaucoma, ongoing ophthalmic infection, or a previous history of ophthalmic surgery. The randomization list generated in Excel 2017 (Microsoft Office, Redmond, WA, USA) without stratification was used to assign participants to the sevoflurane (n=31) or remimazolam (n=31) group. Except for the anesthesiologists who conducted this study, the participants, caregivers, and postoperative outcome assessors were unaware of the group assignment.
No sedatives were administered for premedication prior to anesthesia induction. Electrocardiography, noninvasive arterial blood pressure, pulse oximetry, rSO2 sensor, and CONOX (Quantium Medical, Spain/Fresenius Kabi, Germany) electrodes were employed prior to anesthesia induction. In the sevoflurane group, anesthesia was inducted with propofol 1.5–2.0 mg/kg after administration of remifentanil 0.5–1.0 μg/kg. In the remimazolam group, remifentanil 0.5–1.0 μg/kg was administered, then remimazolam was infused at 6 mg/kg/h and the dose was reduced to 1 mg/kg/h after loss of consciousness. In both groups, rocuronium 0.8 mg/kg was injected after loss of consciousness for tracheal intubation. Anesthesia was maintained with sevoflurane 2–2.5 vol% and remifentanil 0.05–0.2 μg/kg/min in the sevoflurane group, and with remimazolam 1–2 mg/kg/h and remifentanil 0.05–0.2 μg/kg/min in the remimazolam group. The concentrations of sevoflurane and remimazolam were adjusted to between 30 and 55 of the quantium consciousness index (qCON) value of CONOX, and the concentration of remifentanil was adjusted to between 30 and 50 of the quantium nociception index (qNOX) value of CONOX.
Volume-controlled ventilation was set at FiO2 of 0.5 in air, tidal volume of 6 ml per kg of ideal body weight (0.919×(height in cm − 152.4)+45.5), an inspiratory to expiratory ratio (I: E ratio) of 1: 1, and a positive end-expiratory pressure of 5 cmH2O. To maintain the target end-tidal CO2 (ETCO2) of 43±2 mmHg (target PaCO2 of 50 mmHg), the respiratory rate was adjusted.
Hemodynamic parameters were recorded before anesthesia induction (baseline), 1 min after induction (IND), 1, 15, and 30 min after CO2 pneumoperitoneum in the Trendelenburg position (PP1, PP15, and PP30, respectively), and at the end of surgery in the supine position (END). Respiratory parameters and rSO2 were recorded at baseline, IND, PP15, PP30, and END. The mean of the left and right rSO2 values was used to analyze the results. When the mean arterial pressure (MAP) decreased to less than 60 mmHg or more than 20% of the baseline value, hypotension was defined, and ephedrine or phenylephrine was appropriately administered.
ONSD was measured using a 6–15 Hz high-frequency ultrasonic probe with a lubricant after attaching tape for eye protection. ONSD was measured in a vertical plane at 3 mm from the papilla. The measurements were performed 3 times at a single time point, and the mean values were calculated. The ONSD was measured at IND, PP1, PP30, and END. Intra-abdominal CO2 insufflation was limited to 15 mmHg, and the Trendelenburg position was adopted at 30°.
Hemodynamic variables, postoperative nausea and vomiting (PONV), severity of pain, and requirements for antiemetics and rescue analgesics were obtained from the postanesthetic care unit (PACU). For antiemetics, 0.3 mg of ramosetron was administered when the numerical rating scale (NRS; 0–10) score of PONV was 5 or higher. For rescue analgesics, 50 μg of fentanyl was administered when the NRS score of pain was 5 or higher, or if the patient requested it. Patients were discharged from the PACU with a modified Aldrete score of 9 or higher.
The primary outcome was the difference in rSO2 during pneumoperitoneum, and the secondary outcome was the difference in ONSD changes during surgery. The sample size was calculated based on a previous study [5] that compared the rSO2 between mild hypercapnia and normocapnia during total intravenous anesthesia. When rSO2 was 72.9±8.3 during pneumoperitoneum in the Trendelenburg position during mild hypercapnia [5], 31 participants were required for each group considering a power of (1−β) of 90% and an α-error of 0.05 with 10% of possible drop-outs.
Statistical analyses were performed using SPSS (version 22.0; SPSS, Inc., Chicago, IL, USA). Results are expressed as mean±standard deviation, median [interquartile range] or number of patients (%). The Kolmogorov-Smirnov test was performed to investigate the normality of the distribution of continuous variables. An independent
Results
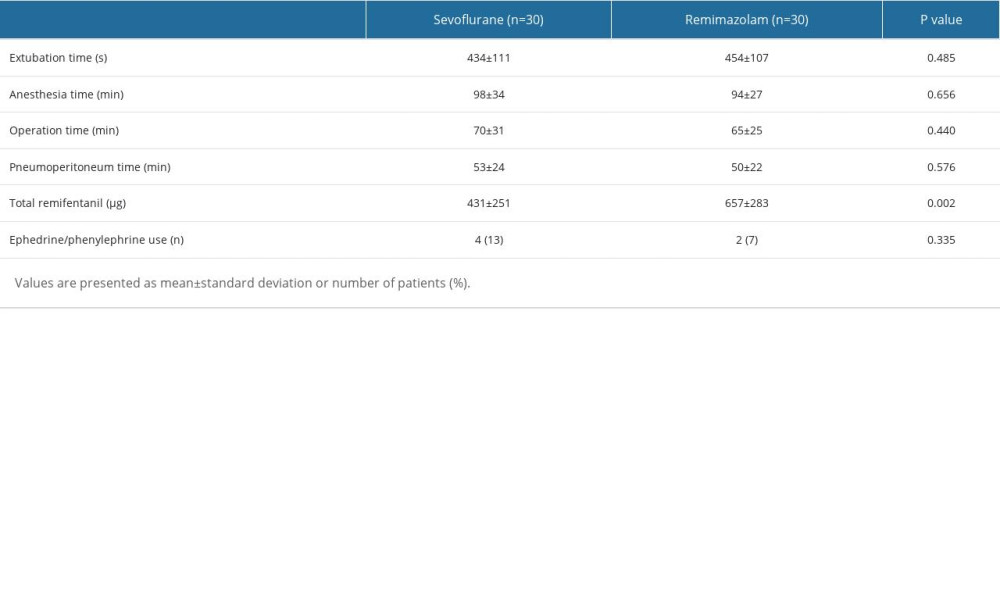
A total of 62 patients were enrolled in this study, and 1 from each group was excluded from the analysis because of the conversion of the surgical method from laparoscopy to laparotomy. Sixty patients completed this prospective study (Figure 1).
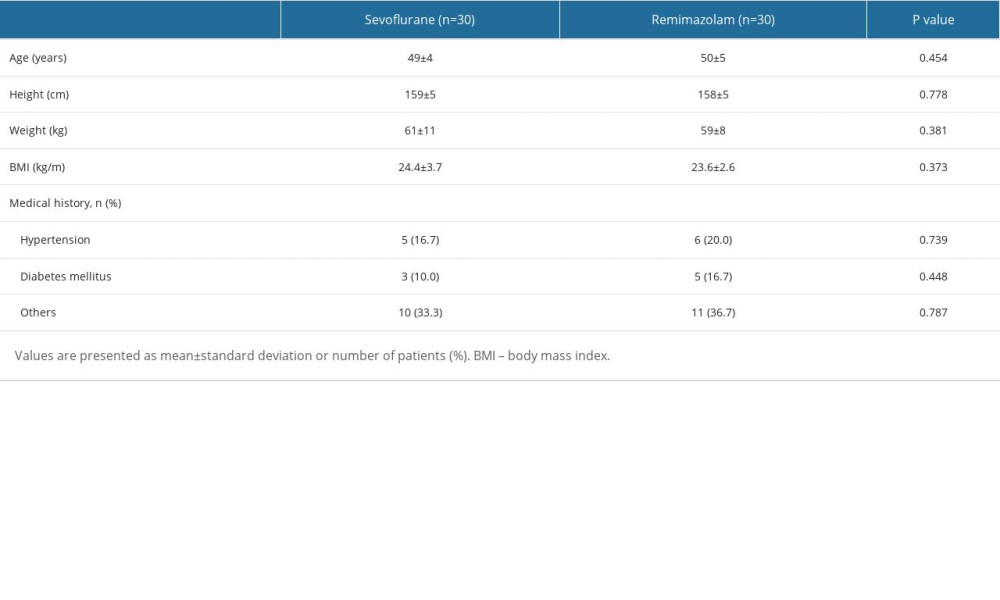
The demographic data were not statistically different (Table 1). The mean age was similar between the sevoflurane and remimazolam groups (49±4 vs 50±5 years,
Changes in ETCO2, rSO2, and ONSD during surgery are shown in Figure 2. No significant intergroup differences were observed in changes over time in ETCO2 and rSO2 (
The changes in MAP and heart rate (HR) are shown in Figure 3. The change in MAP over time was significantly different between the groups (
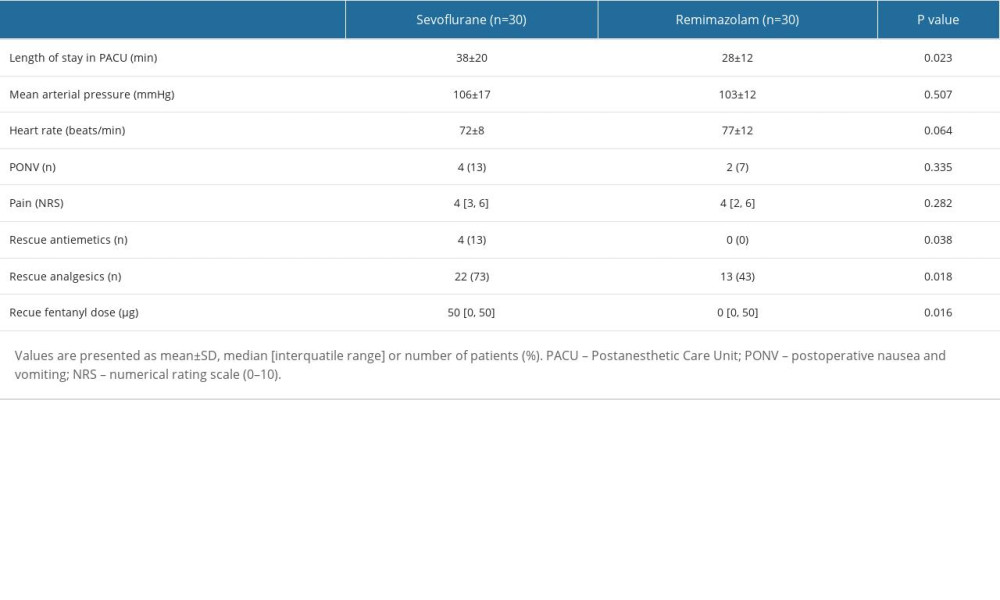
The PACU data are summarized in Table 3. The length of stay in the PACU was significantly shorter in the remimazolam group than in the sevoflurane group (38±20 min vs 28±12 min,
Discussion
This prospective randomized trial showed that remimazolam attenuated the increase in ONSD compared with sevoflurane anesthesia during lung-protective ventilation with mild hypercapnia in patients undergoing gynecological laparoscopy in the Trendelenburg position, although no difference was found in rSO2. In addition, remimazolam anesthesia improved hemodynamic changes during surgery and showed better recovery profiles compared with sevoflurane anesthesia.
The effect of anesthetic agents on rSO2 remains controversial. rSO2 reflects the balance between cerebral blood flow (CBF) and the cerebral metabolic rate of oxygen (CMRO2) [10]. Since volatile anesthetics increase CBF and suppress CMRO2, intravenous anesthetics that enhance r-aminobutyric acid (GABA), such as propofol and benzodiazepine, decrease both CMRO2 and CBF; thus, volatile anesthetics are theoretically expected to show higher rSO2 than iv anesthetics [11]. However, when the drug concentration is adjusted to an identical sedation level, the results of the effect of the type of anesthetic agent on rSO2 are not consistent from study to study [12–14]. In a comparative study of the effects of propofol and sevoflurane anesthesia on rSO2 during one-lung ventilation, no intergroup differences were found in the alteration of rSO2 [12]. By contrast, in another clinical study on gynecological laparoscopic surgery, a significantly lower rSO2 was observed in the propofol group [13]. In a study comparing the effects of propofol and sevoflurane anesthesia on rSO2 values according to the difference in blood CO2 concentration, both normocapnia and mild hypercapnia showed similar rSO2 values, regardless of the anesthetic agent used, during laparoscopic cholecystectomy [14]. However, higher rSO2 values were observed in the propofol group than in the sevoflurane group at the time of stimulation, including intubation, skin incision, and CO2 insufflation [14].
We observed similar rSO2 values in both groups throughout the study period. Our results also showed that rSO2 changed with changes in ETCO2 rather than in MAP. In a previous clinical study on changes in rSO2 during pneumoperitoneum in the Trendelenburg position under propofol anesthesia, rSO2 changed along with changes in MAP and PaCO2, but not in HR, PaO2, or SaO2 [3]. Mild hypercapnia seems to improve rSO2 regardless of the anesthetic agents [5,15]. Mild hypercapnia during laparoscopic gynecological surgery with total intravenous anesthesia using propofol and remifentanil showed improved rSO2 values compared with those in the normocapnia group [5]. In addition, in major surgeries using sevoflurane, the mild hypercapnia group showed a stable increase in rSO2, whereas the normocapnia group showed a decrease in rSO2 [15].
ONSD is a noninvasive method that can effectively predict changes in ICP [16]. ONSD increases with pneumoperitoneum, and Trendelenburg position exacerbates its increase in ONSD [17]. In the present study, we observed an increase in ONSD during pneumoperitoneum in the Trendelenburg position. In addition, changes in ONSD were significantly different between the remimazolam and sevoflurane groups. Although results of studies on the selection of anesthetic agents for rSO2 are inconsistent, studies on the effects of anesthetics on ONSD have shown consistent results. In a comparative study on the effects of propofol and sevoflurane on ONSD during laparoscopic surgery, propofol alleviated the increase in ONSD during pneumoperitoneum more than sevoflurane [17]. A meta-analysis of 7 studies showed the superiority of propofol over sevoflurane anesthesia in terms of changes in ONSD [18]. According to a previous clinical study, anesthetic induction with remimazolam decreased CBF, similar to other benzodiazepines or propofol, but did not alter cerebral blood volume in uncomplicated patients [19]. A previous clinical study found that while the rSO2 value is affected by the presence or absence of permissive hypercapnia, ONSD tends to increase during CO2 pneumoperitoneum in the Trendelenburg position, regardless of the presence or absence of hypercapnia [5].
Remimazolam exhibits excellent hemodynamic stability. A recent meta-analysis that analyzed 8 randomized controlled studies involving 998 patients demonstrated that remimazolam has superior hemodynamic stability with a lower incidence of hypotension than propofol anesthesia [20]. In a propensity score-matched analysis of remimazolam and sevoflurane anesthesia during robotic gastrectomy in the reverse Trendelenburg position, remimazolam anesthesia showed better hemodynamic stability, with less frequent vasopressor use [21]. In the present study, MAP and HR were more stable in the remimazolam group than in the sevoflurane group after CO2 insufflation. Although sedatives such as sevoflurane and remimazolam were adjusted according to the identical target qCON and remifentanil was adjusted according to the identical target qNOX in our study, arithmetically determining which drug is hemodynamically superior is difficult because the infused amount of remifentanil was different. However, despite the significantly larger amount of remifentanil used in the remimazolam group, the lack of a significant difference in vasopressor demand suggests that remimazolam is not inferior to sevoflurane in terms of hemodynamic stability. In the present study, the total infused amount of remifentanil was significantly higher in the remimazolam group than in the sevoflurane group. The results of a previous analysis of robot gastrectomy were consistent with our results [21]. In a propensity score-matched analysis between sevoflurane and remimazolam groups, the amount of remifentanil administered was 700 (interquartile range, 600–900) vs 1405 (1023–1990), which was statistically significant [21].
The ultrashort-acting properties of remimazolam are considered suitable for enhanced recovery after surgery. In the present study, the remimazolam group had a significantly shorter duration of PACU stay than the sevoflurane group. In our study, the recovery profile was superior in the remimazolam group compared with the sevoflurane group, with a shorter length of PACU stay and fewer rescue antiemetic and analgesic requirements. In a previous comparative study of desflurane and remimazolam, anesthesia with remimazolam significantly reduced the incidence of PONV, with a better quality of recovery-40 score compared with desflurane [22]. In addition, after gynecological laparoscopic surgery, remimazolam reduced the incidence of PONV and rescue antiemetics used during the first 2 h after surgery [23]. A meta-analysis of 8 randomized controlled studies comparing propofol and remimazolam showed a lower incidence of nausea, vomiting, dizziness, and injection site pain in the remimazolam group than in the propofol group [20].
This study has several limitations. First, we only included relatively young and healthy patients without severe underlying diseases. Therefore, generalizing the results of this study to all patient groups is difficult. Patients with cerebrovascular disease or autonomic dysfunction may experience different outcomes. Second, since measurements of rSO2 and ONSD are not variables that directly represent a single physiological change or pressure changes in the brain, but rather are affected by various variables such as hemodynamics, respiratory parameters, and hematologic status, an increase in ONSD might not mean a clinically meaningful increase in ICP. Interpreting changes in rSO2 simply as changes in CMRO2 or CBF is also unreasonable. Third, although we adjusted the remifentanil dose targeting the identical target qNOX in our study, the possibility that remifentanil use was significantly higher in the remimazolam group than in the sevoflurane group also influenced the difference in ONSD change between groups cannot be ruled out. A previous study on the effects of remifentanil on ICP demonstrated that the infusion of remifentanil decreased ICP with slight changes in cerebral perfusion pressure [24]. Finally, since it was not possible for the anesthesiologist to be blinded to group assignments due to the design of this study, the possibility that the anesthesiologist might influence the patient’s hemodynamic management cannot be ruled out. However, the assigned anesthesiologist made efforts to ensure that hemodynamic management was performed according to the defined protocol in this study.
Conclusions
In conclusion, remimazolam anesthesia can provide better hemodynamic profiles and attenuate the increase in ONSD during lung-protective ventilation with mild hypercapnia compared with sevoflurane anesthesia in patients undergoing gynecological laparoscopy. In addition, remimazolam anesthesia can provide rapid and better postoperative recovery than sevoflurane anesthesia.
Figures
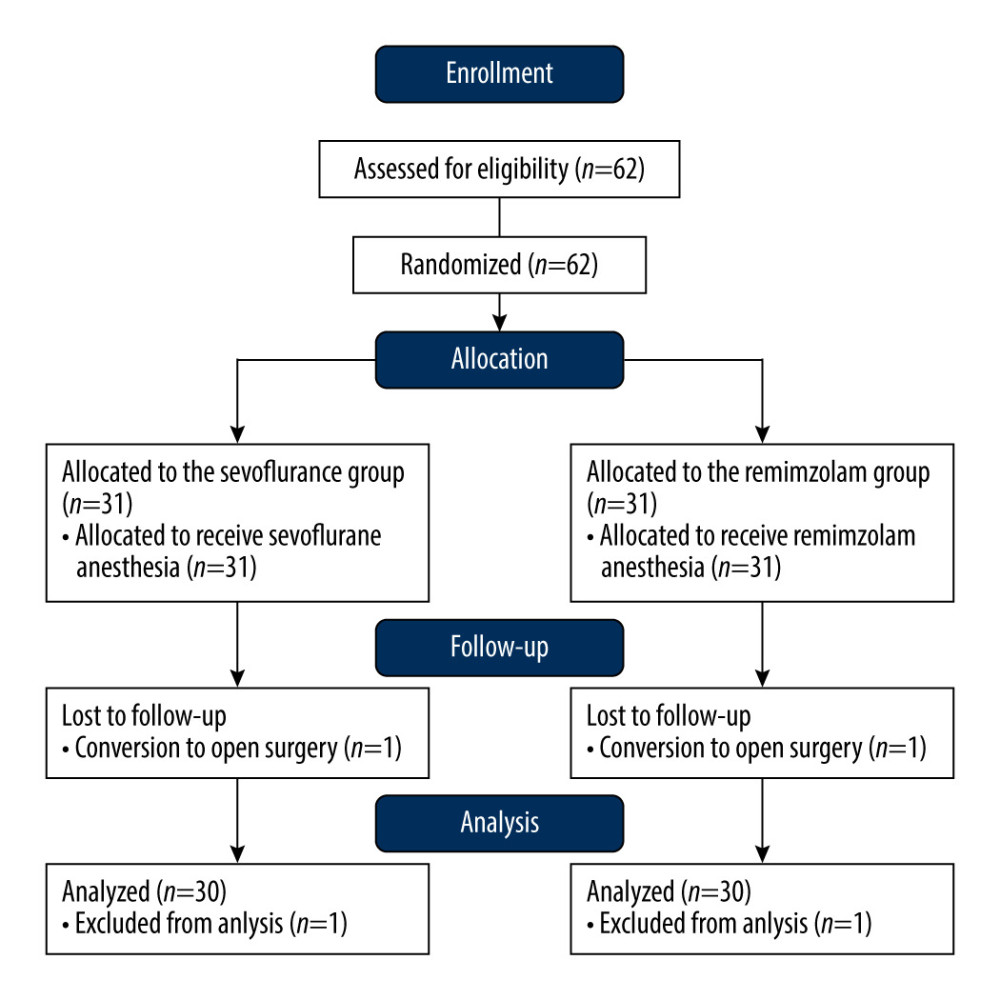 Figure 1. Flow chart of patient allocation. Created using Word 2017 (Microsoft Office, Redmond, WA, USA).
Figure 1. Flow chart of patient allocation. Created using Word 2017 (Microsoft Office, Redmond, WA, USA). 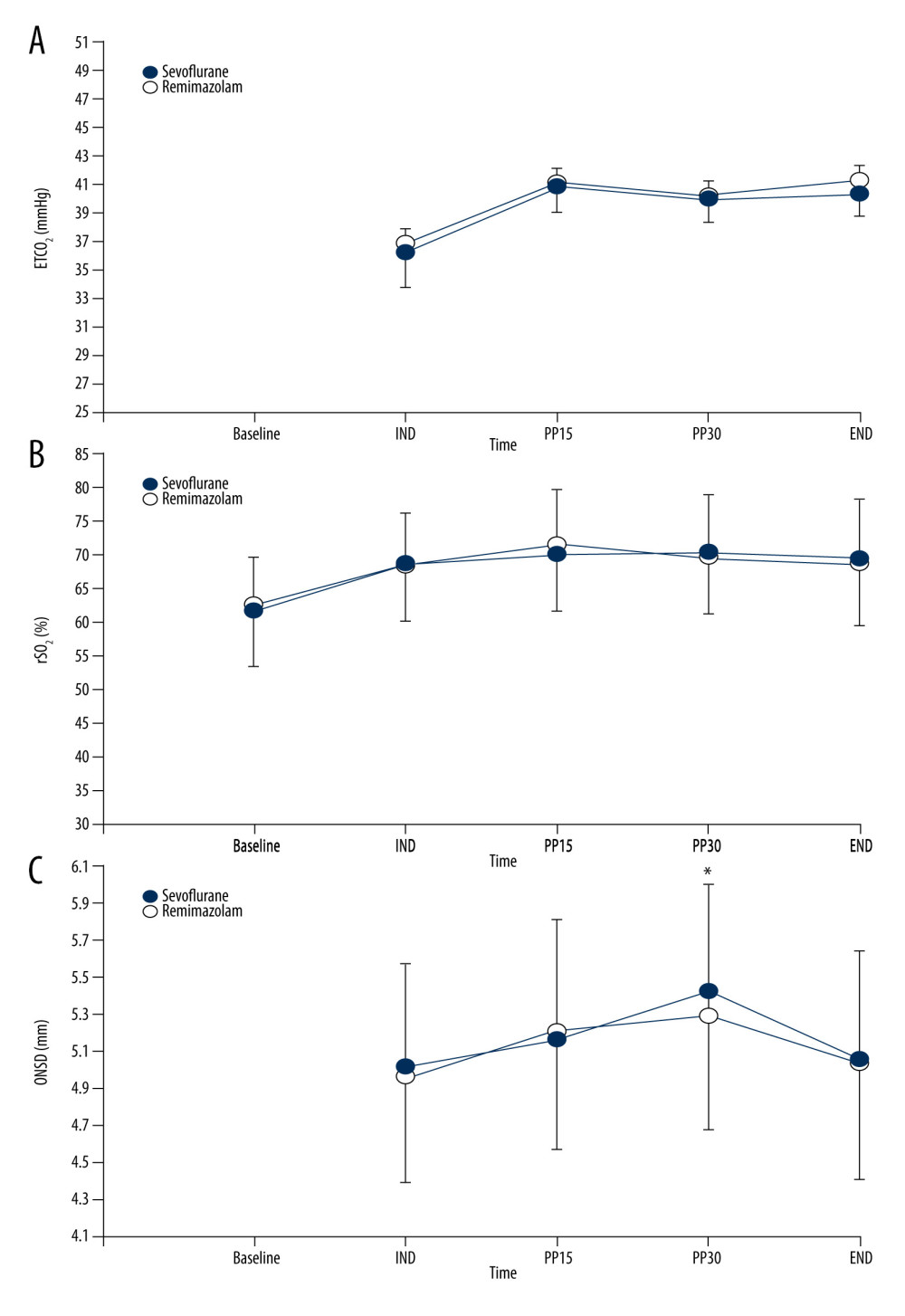 Figure 2. (A–C) Changes in end-tidal carbon dioxide tension (ETCO2), regional cerebral oxygen saturation (rSO2), and optic nerve sheath diameter (ONSD) during surgery. Baseline – before induction; IND – 1 min after induction; PP1, PP15, and PP30, 1, 15, and 30 min after pneumoperitoneum, respectively; END – the end of surgery. * P<0.05, vs IND within the group. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA).
Figure 2. (A–C) Changes in end-tidal carbon dioxide tension (ETCO2), regional cerebral oxygen saturation (rSO2), and optic nerve sheath diameter (ONSD) during surgery. Baseline – before induction; IND – 1 min after induction; PP1, PP15, and PP30, 1, 15, and 30 min after pneumoperitoneum, respectively; END – the end of surgery. * P<0.05, vs IND within the group. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA). 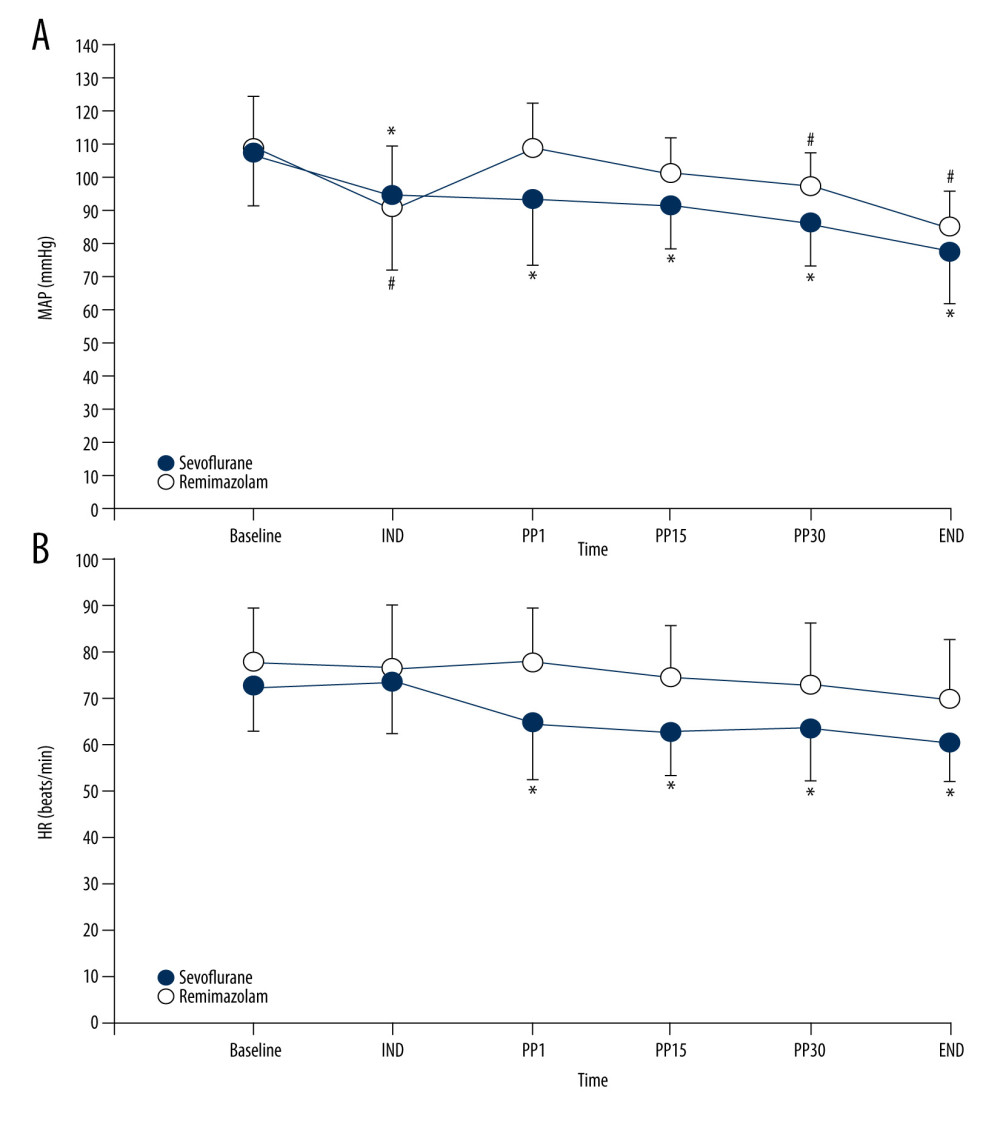 Figure 3. (A) Changes in mean arterial pressure (MAP). * P<0.05, vs IND within the remimazolam group. # P<0.05, vs IND within the sevoflurane group. (B) Changes in heart rate (HR). * P<0.05, vs IND within the remimazolam group. Baseline – before induction; IND – 1 min after induction; PP1, PP15 and PP30 – 1, 15 and 30 min after pneumoperitoneum, respectively; END – the end of surgery. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA).
Figure 3. (A) Changes in mean arterial pressure (MAP). * P<0.05, vs IND within the remimazolam group. # P<0.05, vs IND within the sevoflurane group. (B) Changes in heart rate (HR). * P<0.05, vs IND within the remimazolam group. Baseline – before induction; IND – 1 min after induction; PP1, PP15 and PP30 – 1, 15 and 30 min after pneumoperitoneum, respectively; END – the end of surgery. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA). References
1. Chen K, Wang L, Wang Q, Effects of pneumoperitoneum and steep Trendelenburg position on cerebral hemodynamics during robotic-assisted laparoscopic radical prostatectomy: A randomized controlled study: Medicine (Baltimore), 2019; 98(21); e15794
2. Robba C, Cardim D, Donnelly J, Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods: Br J Anaesth, 2016; 117(6); 783-91
3. Matsuoka T, Ishiyama T, Shintani N, Changes of cerebral regional oxygen saturation during pneumoperitoneum and Trendelenburg position under propofol anesthesia: A prospective observational study: BMC Anesthesiol, 2019; 19(1); 72
4. Wang L, Yang L, Yang J, Shan S, Effects of permissive hypercapnia on laparoscopic surgery for rectal carcinoma: Gastroenterol Res Pract, 2019; 2019; 3903451
5. Park CG, Jung WS, Park HY, Comparison of the effects of normocapnia and mild hypercapnia on the optic nerve sheath diameter and regional cerebral oxygen saturation in patients undergoing gynecological laparoscopy with total intravenous anesthesia: J Clin Med, 2021; 10(20); 4707
6. Sakata K, Kito K, Fukuoka N, Cerebrovascular reactivity to hypercapnia during sevoflurane or desflurane anesthesia in rats: Korean J Anesthesiol, 2019; 72(3); 260-64
7. Petersen KD, Landsfeldt U, Cold GE, Intracranial pressure and cerebral hemodynamic in patients with cerebral tumors: A randomized prospective study of patients subjected to craniotomy in propofol-fentanyl, isoflurane-fentanyl, or sevoflurane-fentanyl anesthesia: Anesthesiology, 2003; 98(2); 329-36
8. Shi M, Chen J, Liu T, Protective effects of remimazolam on cerebral ischemia/reperfusion injury in rats by inhibiting of NLRP3 inflammasome-dependent pyroptosis: Drug Des Devel Ther, 2022; 16; 413-23
9. Kim SH, Fechner J, Remimazolam – current knowledge on a new intravenous benzodiazepine anesthetic agent: Korean J Anesthesiol, 2022; 75(4); 307-15
10. Kurth CD, Levy WJ, McCann J, Near-infrared spectroscopy cerebral oxygen saturation thresholds for hypoxia-ischemia in piglets: J Cereb Blood Flow Metab, 2002; 22(3); 335-41
11. Slupe AM, Kirsch JR, Effects of anesthesia on cerebral blood flow, metabolism, and neuroprotection: J Cereb Blood Flow Metab, 2018; 38(12); 2192-208
12. Yamada N, Nagata H, Sato Y, Tomoyasu MEffects of propofol or sevoflurane on cerebral regional oxygen saturation (rSO2) during one-lung ventilation: Masui, 2008; 57(11); 1388-97 [in Japanese]
13. Kim SJ, Kwon JY, Cho AR, The effects of sevoflurane and propofol anesthesia on cerebral oxygenation in gynecological laparoscopic surgery: Korean J Anesthesiol, 2011; 61(3); 225-32
14. Sen P, Izdes S, But A, Effects of sevoflurane and propofol anaesthesia on cerebral oxygenation during normocapnia and mild hypercapnia: A pilot study: Br J Anaesth, 2013; 110(2); 318-19
15. Wong C, Churilov L, Cowie D, Randomised controlled trial to investigate the relationship between mild hypercapnia and cerebral oxygen saturation in patients undergoing major surgery: BMJ Open, 2020; 10(2); e029159
16. Munawar K, Khan MT, Hussain SW, Optic nerve sheath diameter correlation with elevated intracranial pressure determined via ultrasound: Cureus, 2019; 11(2); e4145
17. Yu J, Hong JH, Park JY, Propofol attenuates the increase of sonographic optic nerve sheath diameter during robot-assisted laparoscopic prostatectomy: A randomized clinical trial: BMC Anesthesiol, 2018; 18(1); 72
18. Yang J, Yang X, Li X, Ou S, Effects of propofol and inhalational anesthetics on the optic nerve sheath diameter in patients undergoing surgery in the steep Trendelenburg position: A systematic review and meta-analysis: Ann Palliat Med, 2021; 10(10); 10475-85
19. Soejima T, Ueda K, Hasegawa S, Change in cerebral circulation during the induction of anesthesia with remimazolam: J Anesth, 2023; 37(1); 92-96
20. Wu X, Wang C, Gao H, Comparison of remimazolam and propofol about safety outcome indicators during general anesthesia in surgical patients: A systematic review and meta-analysis: Minerva Anestesiol, 2023; 89(6); 553-64
21. Lee B, Kim MH, Kong HJ, Effects of remimazolam vs. sevoflurane anesthesia on intraoperative hemodynamics in patients with gastric cancer undergoing robotic gastrectomy: A propensity score-matched analysis: J Clin Med, 2022; 11(9); 2643
22. Song SW, Jang YN, Yoon MW, Jeon YG, Quality of recovery in patients administered remimazolam versus those administered an inhalant agent for the maintenance of general anesthesia: A randomized control trial: BMC Anesthesiol, 2022; 22(1); 226
23. Hari Y, Satomi S, Murakami C, Remimazolam decreased the incidence of early postoperative nausea and vomiting compared to desflurane after laparoscopic gynecological surgery: J Anesth, 2022; 36(2); 265-69
24. Tipps LB, Coplin WM, Murry KR, Rhoney DH, Safety and feasibility of continuous infusion of remifentanil in the Neurosurgical Intensive Care Unit: Neurosurgery, 2000; 46(3); 596-602
Figures
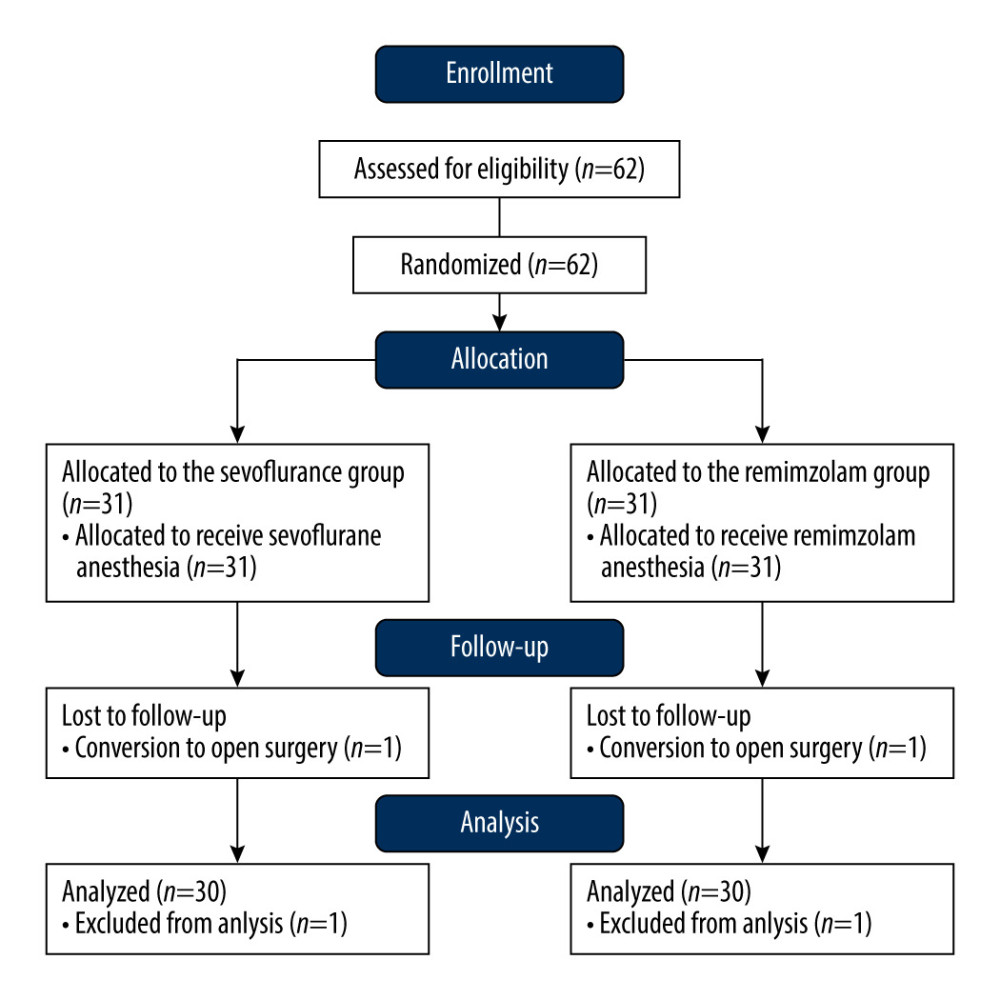 Figure 1. Flow chart of patient allocation. Created using Word 2017 (Microsoft Office, Redmond, WA, USA).
Figure 1. Flow chart of patient allocation. Created using Word 2017 (Microsoft Office, Redmond, WA, USA).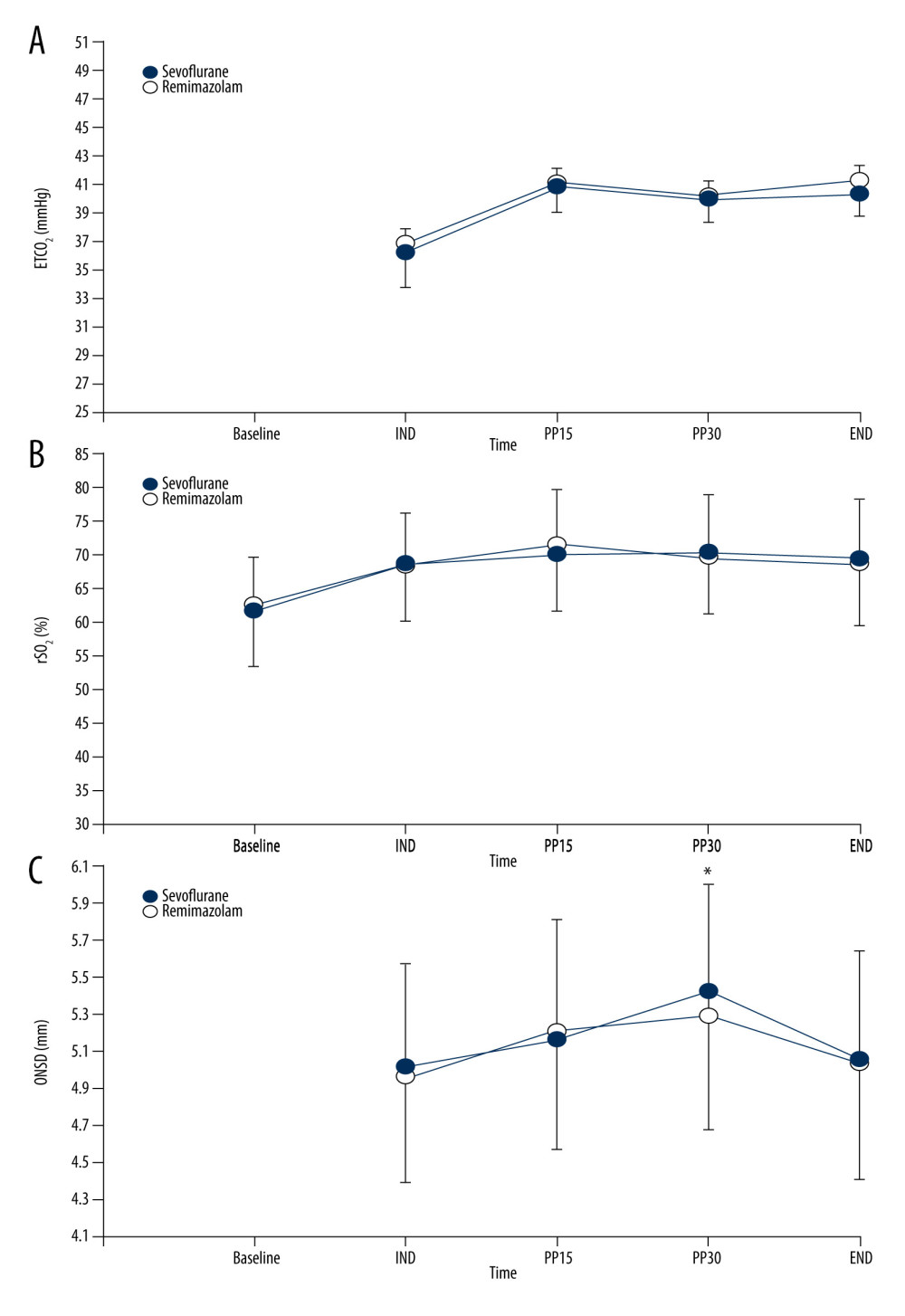 Figure 2. (A–C) Changes in end-tidal carbon dioxide tension (ETCO2), regional cerebral oxygen saturation (rSO2), and optic nerve sheath diameter (ONSD) during surgery. Baseline – before induction; IND – 1 min after induction; PP1, PP15, and PP30, 1, 15, and 30 min after pneumoperitoneum, respectively; END – the end of surgery. * P<0.05, vs IND within the group. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA).
Figure 2. (A–C) Changes in end-tidal carbon dioxide tension (ETCO2), regional cerebral oxygen saturation (rSO2), and optic nerve sheath diameter (ONSD) during surgery. Baseline – before induction; IND – 1 min after induction; PP1, PP15, and PP30, 1, 15, and 30 min after pneumoperitoneum, respectively; END – the end of surgery. * P<0.05, vs IND within the group. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA).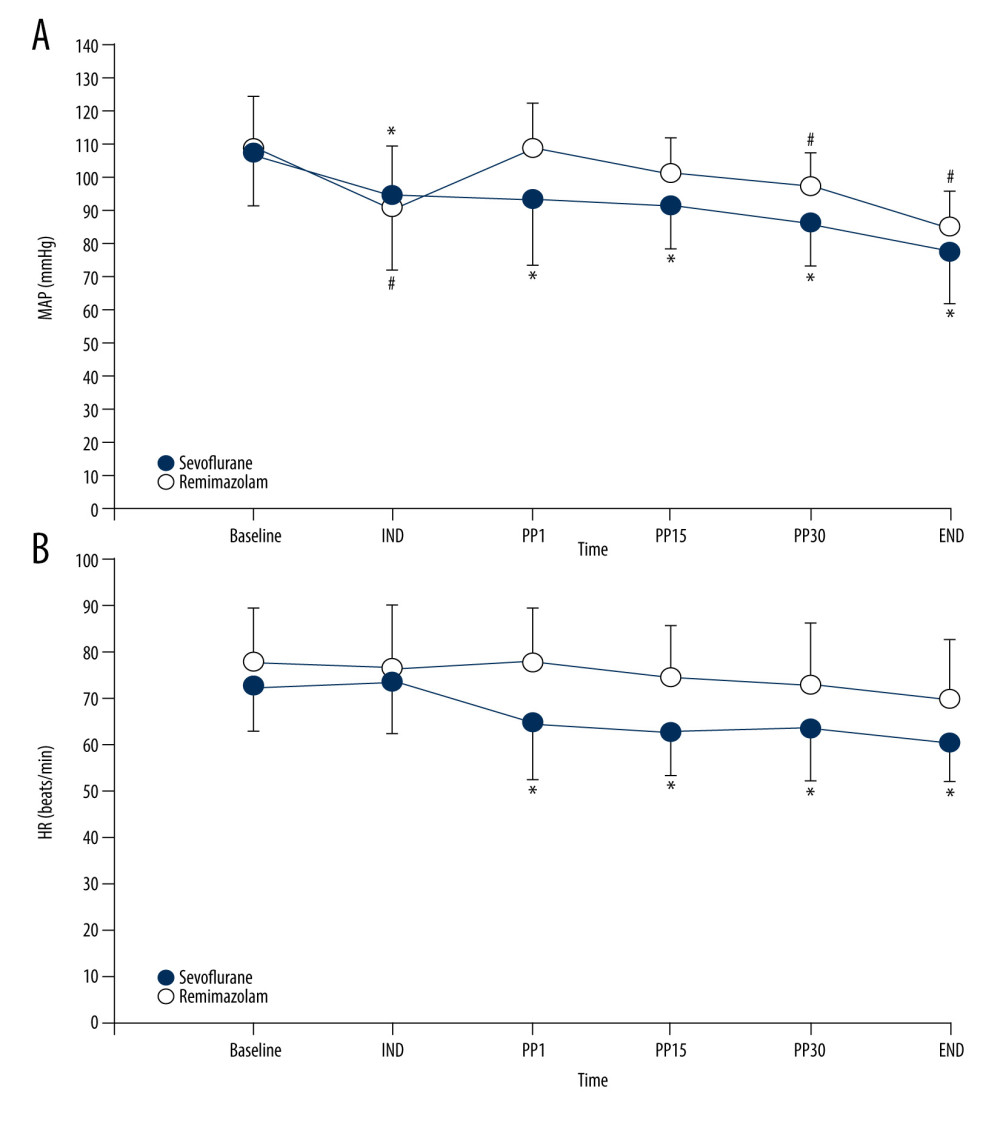 Figure 3. (A) Changes in mean arterial pressure (MAP). * P<0.05, vs IND within the remimazolam group. # P<0.05, vs IND within the sevoflurane group. (B) Changes in heart rate (HR). * P<0.05, vs IND within the remimazolam group. Baseline – before induction; IND – 1 min after induction; PP1, PP15 and PP30 – 1, 15 and 30 min after pneumoperitoneum, respectively; END – the end of surgery. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA).
Figure 3. (A) Changes in mean arterial pressure (MAP). * P<0.05, vs IND within the remimazolam group. # P<0.05, vs IND within the sevoflurane group. (B) Changes in heart rate (HR). * P<0.05, vs IND within the remimazolam group. Baseline – before induction; IND – 1 min after induction; PP1, PP15 and PP30 – 1, 15 and 30 min after pneumoperitoneum, respectively; END – the end of surgery. Created using Excel 2017 (Microsoft Office, Redmond, WA, USA). In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952